

Best Practices for Chiropractic Care for Older Adults:
A Systematic Review and Consensus UpdateThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2017 (May); 40 (4): 217–229 ~ FULL TEXT
OPEN ACCESS Cheryl Hawk, DC, PhD, Michael J. Schneider, DC, PhD, Mitchell Haas, DC, MA,
Paul Katz, MD, Paul Dougherty, DC, Brian Gleberzon, DC, MHSc,
Lisa Z. Killinger, DC, John Weeks
Texas Chiropractic College,
Pasadena, TX.This is an update of the 2010 Consensus Document titled:
Recommendations for Chiropractic Care for Older Adults: Results of a Consensus ProcessOBJECTIVE: The purpose of this study was to update evidence-based recommendations on the best practices for chiropractic care of older adults.
METHODS: The project consisted of a systematic literature review and a consensus process. The following were searched from October 2009 through January 2016: MEDLINE, Index to Chiropractic Literature, CINAHL (Cumulative Index to Nursing and Allied Health Literature), AMED (Allied and Complementary Medicine Database), Alt HealthWatch, Cochrane Database of Systematic Reviews, and Cochrane Registry of Controlled Trials. Search terms were: (manipulation, spinal OR manipulation, chiropractic OR chiropract*) AND (geriatric OR "older adult*"). Two reviewers independently screened articles and abstracts using inclusion and exclusion criteria. The systematic review informed the project steering committee, which revised the previous recommendations. A multidisciplinary panel of experts representing expertise in practice, research, and teaching in a variety of health professions serving older adults rated the revised recommendations. The RAND Corporation/University of California, Los Angeles methodology for a modified Delphi consensus process was used.
RESULTS: A total of 199 articles were found; after exclusion criteria were applied, 6 articles about effectiveness or efficacy and 6 on safety were added. The Delphi process was conducted from April to June 2016. Of the 37 Delphi panelists, 31 were DCs and 6 were other health care professionals. Three Delphi rounds were conducted to reach consensus on all 45 statements. As a result, statements regarding the safety of manipulation were strengthened and additional statements were added recommending that DCs advise patients on exercise and that manipulation and mobilization contribute to general positive outcomes beyond pain reduction only.
CONCLUSIONS: This document provides a summary of evidence-informed best practices for doctors of chiropractic for the evaluation, management, and manual treatment of older adult patients.
KEYWORDS: Aging; Chiropractic; Spinal Manipulation
From the Full-Text Article:
Introduction
Aging of the general population is a global phenomenon; the United States is similar to other developed countries in the rapid growth of older age groups. [1] About 15% of people who seek chiropractic care are aged 65 and older. [2] Like other age groups, older adults use chiropractic services most often for musculoskeletal complaints. In addition, as people live longer, increasing emphasis is being placed on their ability to function independently. The World Health Organization states that a key feature of promotion of “healthy aging” is to increase or maintain functional ability. [3] This may allow older people to live independently, which may be of utmost importance to them. Thus, any health care intervention that contributes to a patient’s ability to overcome activity limitations imposed by chronic pain should have a role in the care of older adults. [4]
In addition to managing musculoskeletal symptoms, doctors of chiropractic (DCs) may also provide a diverse range of services to aging patients and may play an important role as a member of the health care team. [5] One role for DCs may be as a first-contact provider, managing both the initial assessment and management of the older adult’s complaint. One recent study indicated that when the supply of DCs in a particular geographic region is greater, primary care medical visits decrease in the Medicare population in that region. [6] This supports that older adults may use chiropractic as the sole management for common musculoskeletal complaints. [7] However, chiropractors co-manage patients’ conditions with other providers, particularly for older adults, who often have multiple comorbidities. [6] Doctors of chiropractic may play a role as members of a health care team, either in a small clinical setting or in a large system such as the Veterans Affairs (VA) clinical system. [8, 9] Regardless of the role that the DC is providing, she or he must provide care that is both evidence based and patient centered. [10]
To provide older adults with the best possible care, the body of evidence for both safety and effectiveness of chiropractic care should be evaluated. This is true for musculoskeletal conditions and the other roles that the DC may play in assessing and managing disease prevention. [11–13] At this time, the scientific evidence has important gaps for chiropractic management of the aging population. In such cases, expert opinion may be useful in establishing best practices. In the current era of evidence-based practice, guidelines and best practice documents must be re-evaluated at regular intervals to remain current with the evidence base. [14] The purpose of this study was to update previously published evidence-based recommendations [5] on the best practices for chiropractic care of older adults.
Methods
Project Overview
The project was composed of a systematic literature review and a formal consensus process to update the 2010 recommendations. An investigator experienced in systematic reviews (M.H.) led the review process to rate and summarize the relevant literature, emphasizing new evidence published after the original consensus document was developed. Based on the results of the systematic review, the Project Steering Committee revised the previous recommendations. A multidisciplinary panel of experts representing expertise in practice, research, and teaching in a variety of health professions serving the older adult population rated the revised set of recommendations. The RAND Corporation/University of California, Los Angeles (UCLA) methodology for a modified Delphi process was used to reach consensus. We chose an a priori level of agreement of 80% for acceptance.
Human Subject Considerations
The project was approved by the University of Western States Institutional Review Board. Participants signed a consent form prior to the start of the Delphi process.
Steering Committee
The Steering Committee (SC) was responsible for drafting and approving the original seed statements and for revising statements as per the Delphi panelists’ comments, for statements on which agreement was not reached. The SC was composed of the project director and co-director, 3 DCs either teaching geriatrics courses or working with geriatric patients, a medical physician specializing in geriatrics, and a journal editor.
Systematic Review
Literature that had been published since the beginning of the original consensus project was reviewed; thus, the start date for the search was October 1, 2009, and the end date was January 31, 2016. Our literature search was designed to answer 2 general questions:(1) “What is the effectiveness of chiropractic care, including spinal manipulation, for conditions
experienced by older adults?”
(2) “What are the adverse events associated with chiropractic care including spinal manipulation
among older adults?”To state question 1 in terms of PICO (Population, Intervention, Comparison, Outcome): the population was older adults (aged 65 and older); the interventions were chiropractic care or spinal manipulation; type of comparison group and outcome were unspecified so as not to be exclusive. We did not specify outcomes in great detail because we intended only to summarize relevant findings; we did not plan to pool data because of the expected heterogeneity of studies. Actual outcomes included changes in pain, function, and/or quality of life.
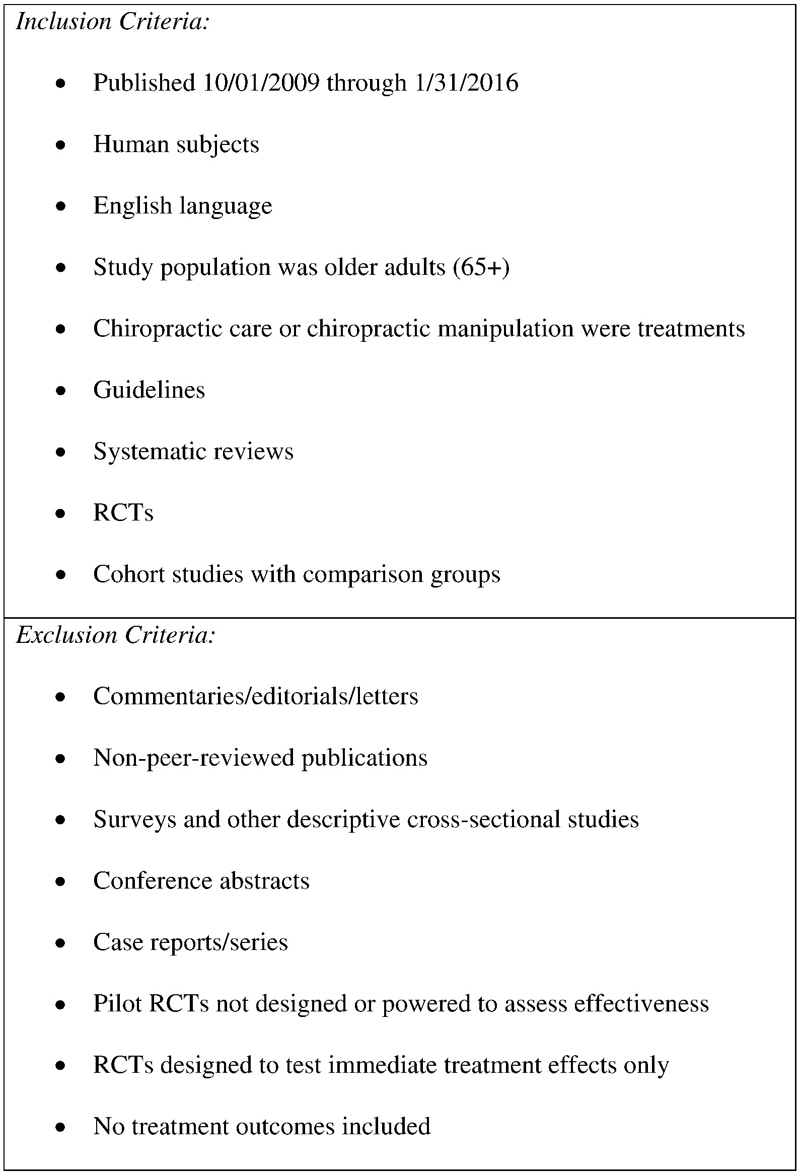
Figure 1 The inclusion and exclusion criteria for effectiveness and efficacy studies are illustrated in Figure 1.
Search Strategy The following databases were included in the search: MEDLINE Complete, Index to Chiropractic Literature, CINAHL, AMED (Allied and Complementary Medicine Database), Alt HealthWatch, Cochrane Database of Systematic Reviews, and Cochrane Registry of Controlled Trials. Search terms were: (manipulation, spinal OR manipulation, chiropractic OR chiropract*) AND (geriatric OR “older adult*”). Two reviewers independently screened articles and abstracts. We did not extract further data.
The literature search on safety was conducted at the same time as the search effectiveness, using the same databases. The rationale for broadening the inclusion criteria was that studies of harm are not typically designed as randomized trials and often are published as individual case reports or cases series. Search terms were: (manipulation, spinal OR manipulation, chiropractic OR chiropract* OR manual therapies) AND (geriatric OR "older adult*") AND (harm OR risk OR adverse event* OR adverse effect*). An additional hand search was conducted.
Evaluation of Articles
To address the general question about effectiveness, we evaluated the literature using several validated rating tools, depending on the type of study. Systematic reviews were rated with the AMSTAR checklist [15, 16]; randomized controlled trials (RCTs) with the risk of bias tool from the Cochrane Collaboration [17]; and cohort studies with the Newcastle-Ottawa Quality Assessment Scale. [18] These same rating tools were used to assess the quality of the studies retrieved on the general question of safety. Individual case reports and case series were not formally rated. Two investigators reviewed each paper, and disagreements in their ratings were resolved by discussion.
Seed Document and Background Materials
We began to develop the seed document using the 49 seed statements from the previous set of recommendations verbatim. [5] The SC reviewed the document and made some revisions based on new literature, with a resultant set of 45 seed statements. Background materials were also developed to succinctly summarize the literature review and its results.
Delphi Process
As in previous projects, [5, 19–21] we conducted the consensus electronically with a panel of experts. This method saves on the time and expense of conducting in-person meetings and reduces the bias introduced by panelists influencing one another’s ratings. With an electronic process, panelists can remain anonymous during the process.
Our consensus methodology was that of RAND Corporation/UCLA-consensus methodology. [22] Panelists rate the appropriateness of each statement. They are told to consider “appropriateness” to mean that the expected health benefit is greater to the patient than any expected negative consequences, excluding cost. [22]
An ordinal rating scale of 1–9 is used, anchored by“highly inappropriate” = 1, 2, 3
“uncertain” = 4, 5, 6 and
“highly appropriate” = 7, 8, 9Panelists were instructed that if they rated a statement as “inappropriate,” they had to give a reason and, if possible, a citation from peer-reviewed literature, to facilitate revision of the statement.
Ratings were entered into an Excel file, and comments were entered verbatim and anonymously into an MS Word table. We calculated percentage agreement on each statement. Consensus was considered to be reached if at least 80% of panelists rated a statement as “highly appropriate.” The SC reviewed all comments and revised statements on which consensus was not reached, basing the revisions on both the panelists’ comments and the current literature. Revised statements were recirculated until consensus was reached.
Delphi Panel
We invited all panelists on the original project to participate. The SC nominated additional panelists to provide broad representation and multidisciplinary input. Forty-four people were invited, and 37 accepted (84%).
Results
Systematic Review: Effectiveness
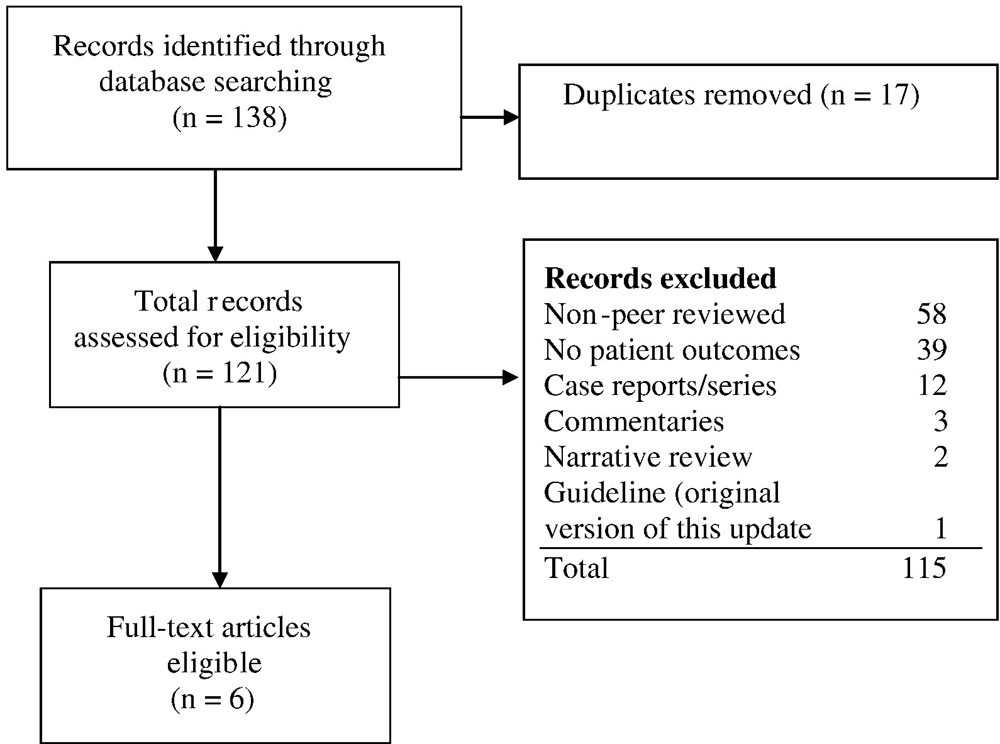
Figure 2

Table 1 The review of selected articles was conducted from January to March 2016. The numbers of articles resulting from the literature search for effectiveness are summarized in Figure 2. We evaluated 6 articles for quality; 3 were RCTs, [23–25] 2 were cohort studies, [26, 27] and 1 was a systematic review, [28] as outlined in Table 1.
A high-quality RCT found that, although spinal manipulation did not result in greater reduction in pain than sham, disability was slightly more improved at 12 weeks. [23] One low-quality [24] and 1 medium-quality RCT [25] found improvements in pain among older adults receiving manipulation. Two high-quality cohort studies found that, although Medicare users of chiropractic care had a slightly increased risk for declines in lower body function and self-rated health, chiropractic use was protective against 1–year decline in all outcomes, and users were satisfied with their care. [26, 27] A fair-quality systematic review found insufficient evidence for the effect of manipulation on balance and falls. [28]
Systematic Review: Safety
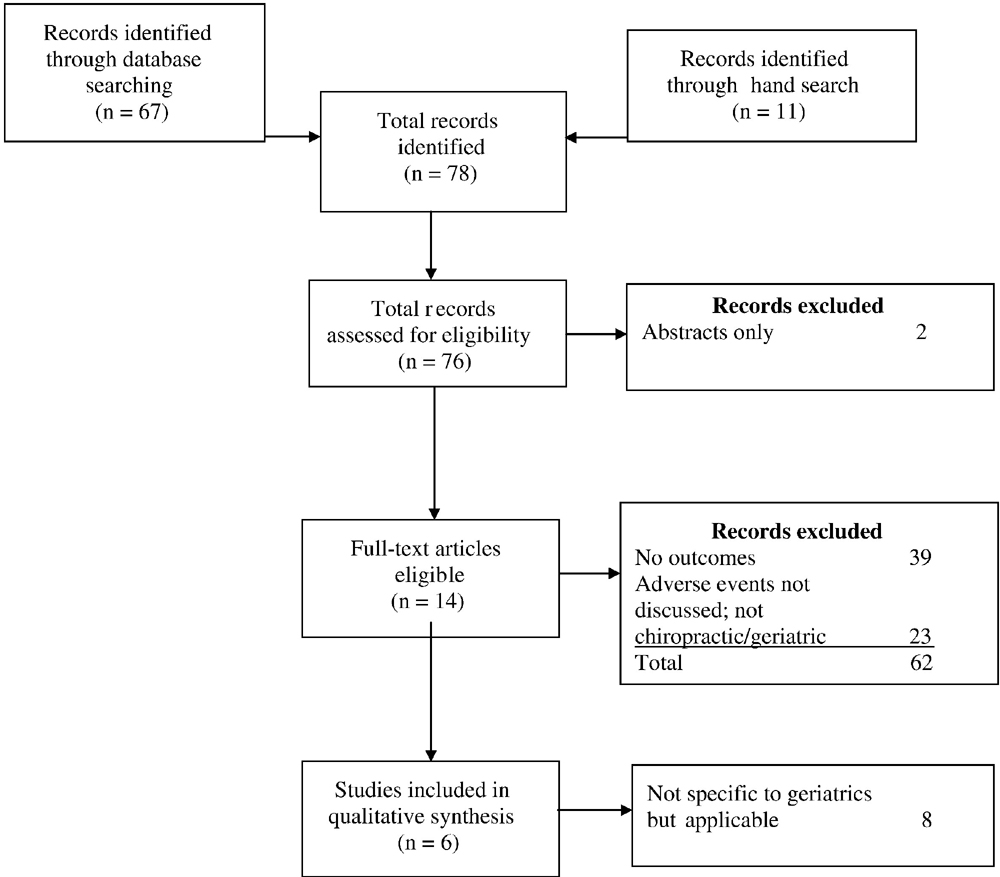
Figure 3

Table 2 Seventy-eight articles were retrieved. Sixty-four articles were excluded (abstracts, not applicable to older adults, not chiropractic, no treatment outcomes, adverse events not reported), leaving 14 articles. Six of these were studies specifying older adults, [23, 29–33] and 8 addressed adverse events in adults in general but were considered applicable to older adults as well and were retained [34–41] (Fig 3).
Safety and Adverse Events in Older Adults Table 2 summarizes the 6 studies addressing safety issues, specifically in older adults. No serious adverse events related to the intervention were reported in any of the studies. The articles on adverse events related to spinal manipulation in general (not specifically in older adults) found that serious adverse events are very rare [34, 35] and challenge a causal relationship with spinal manipulation. [34–41]
The main findings from these 8 articles, which did not focus specifically on older adults, were as follows:
A 2015 systematic review stated: “We found no evidence for a causal link between chiropractic care
and CAD [cervical artery dissection].” [34]A 2015 case-control study found no significant association between the risk of vertebrobasilar artery
(VBA) stroke and use of chiropractic. [35]A 2014 review found no epidemiologic studies demonstrating an association between cervical
manipulation and internal carotid artery (ICA) dissection. [36]A 2015 study indicated that “maximal ICA strains imparted by cervical spinal manipulative
treatments were well within the normal ROM” and did not cause strains in excess of those
experienced with normal everyday neck movements. [37]A 2014 study suggested that vertebral artery (VA) strains during global head and neck movements,
including spinal manipulation, were considerably smaller than published VA failure strains. [38]A 2014 biomechanical study found no significant changes in blood flow in the vertebral arteries
of healthy young adult males after cervical spine manipulations. [39]A 2014 statement from the American Heart Association suggested that patients should be informed of
the risk of cervical arterial dissection prior to undergoing manipulation of the cervical spine. [40]A systematic review on the incidence of serious adverse events following lumbopelvic spinal manipulative
therapy found only anecdotal cases (including cauda equina and disc herniation), so causation cannot
be inferred. Similar risks of adverse events occur with exercise compared with manual therapy;
risk is lower comparing manual therapy with drugs. [41]
Delphi Process
The Delphi process was conducted from April to June of 2016. Of the 37 panelists, 31 were DCs and 6 were other types of health professionals. There were 3 medical physicians; 1 was a geriatrician, 1 a faculty member of a Geriatric Education Center, and 1 an Ayurvedic physician and acupuncturist. One panelist was an registered nurse, another a PhD psychologist, and another a physical therapist (DPT). Three DCs were cross-trained, 1 as a physical therapist and 2 as massage therapists. Panelists represented 18 US states (AZ, CA, CT, GA, IA, IL, MA, MN, MO, MS, NH, NY, OH, OR, PA, TX, VA, WA) and 3 Canadian provinces (MB, QC, ON). Those who were practitioners [29] had been in practice an average of 19.4 years (range: 1–42). Seventeen were faculty (either full- or part-time) at chiropractic colleges, and 11 were full- or part-time faculty at non-chiropractic colleges.
Three Delphi rounds were conducted to reach consensus on all 45 statements; in the first round, 6 statements required revision, and in the second round, 2 required revision.
The following statements are the result of the consensus process.
Consensus Statements on “Best Practices” for Chiropractic Care for Older Adults
Introduction
The purpose of this best practice document is to define the parameters of an appropriate approach to chiropractic care for older adults, which is in both the patient’s and the public’s interest. The potential benefits of any health care intervention must consider patient preference and should be weighed against the associated risks and the costs in terms of population health, time, and money.
General Clinical Principles in the Care of Older Adults
In a biopsychosocial approach to treating older adults, it is recognized that there are age-related changes that may affect the delivery of a given intervention. [42] The age-related changes in the neurologic and musculoskeletal systems of older adults create unique findings and presentations that may require specific consideration during the physical examination (such as peripheral neuropathy, age-related muscle loss, and loss of flexibility).
The Chiropractic Clinical Encounter
Chiropractic management of the older patient should follow the 3 basic principles of evidence-based practice, which are to(1) make clinical judgments based on use of the best available evidence combined with
(2) the clinician’s experience and expertise and
(3) the patient’s preference, based on their values and goals (consistent with patient centered care). [43, 44]
Informed Consent Informed consent by the patient or legal representative is required before performing an examination or diagnostic tests or initiating a management program. Consent must be fully informed, voluntary, related to the patient’s condition, and not be obtained by misrepresentation. The patient must have the capacity to understand the information to provide informed consent. If there is impairment in their ability to make decisions, then an appropriately designated surrogate/substitute decision maker must be consulted. Providers must be alert for indications of cognitive or affective issues that might influence the patient’s capacity for providing informed consent. [45] Consent is a process and not a one-time, specific event and should be modified as warranted. [46]
Risks and Benefits Among adult chiropractic patients, minor transient side effects (24–72 hours), usually muscle soreness or stiffness, are common. However, evidence indicates that serious adverse events are very rare. [34, 35, 41, 47] Among older adult chiropractic patients recent studies indicate no evidence of higher risk for serious adverse events and no evidence for causation of strokes. [32, 33] Furthermore, there is emerging evidence indicating older patients receiving chiropractic care (particularly mobilizations and manipulative procedures of the spine and peripheral joints) experience a variety of positive clinical outcomes and a high level of satisfaction with their care. [23, 25, 27] In the absence of conclusive evidence it is imperative that the clinician use a patient-centered approach that combines clinical experience and patient preference for a time-limited, outcome-based therapeutic trial of chiropractic care.
Management Approaches
The 3 basic chiropractic management approaches to the care of the geriatric patient are:(1) sole management by a chiropractic physician;
(2) co-management with other appropriate health care providers; and
(3) referral to a recognized licensed or certified health care provider/specialist.Co-management with or referral to other appropriate health care providers is common in older adults and may be appropriate under any number of conditions.
These include but are not limited to the following:
The patient is not showing clinically significant improvement, or is showing a worsening of
symptoms, after a time-limited initial trial of chiropractic care.The patient requests a referral or co-management approach.
There are significant comorbidities that could be outside the scope of chiropractic practice for
which the patient requests a referral or co-management approach.Older adult patients often have multiple health care conditions being managed by multiple health care providers. The chiropractor, as part of this team, should make every reasonable attempt to obtain copies of all relevant clinical records and files and to communicate his or her findings to other health care providers. The chiropractor should, if at all possible, communicate directly with that health care provider to provide important clinical information. This communication should adhere to jurisdictional legislation governing patient confidentiality as well as the maintenance, distribution, and protection of patient health records.
Clinical History Changes in an older adult’s hearing, sight, coordination, and cognition may create a challenge in obtaining a history and performing a physical examination. If these impairments are thought to compromise the integrity of the findings, the chiropractor should obtain permission to have the patient’s family member or caregiver accompany him or her. [45]
The comprehensive case history at the initial visit should include a review of systems, family history, health care history, concurrent health care, and both prescription and nonprescription medication use, including supplements, herbs, and nutraceuticals. Information on health habits, including tobacco use, alcohol use, diet, sleep, physical activity, falls, and other injuries, should be included. [48] Activities of daily living (ADLs), which are basic tasks involving bodily issues such as bathing, toileting, eating, and walking, and instrumental activities of daily living (IADLs), which are a higher level of function than ADLs, such as cooking, writing, and driving, should be reviewed. Prior occurrence of the chief complaint should be recorded, including length of time to recovery, type of treatment, and previous diagnosis.
Additional factors that must be considered during the case history for this age group include atypical presentation of many clinical conditions, underreporting of disease, overestimation of cognitive function, polypharmacy, and ageist attitudes held by patients, caregivers, family, and health care providers.
It is recommended that chiropractors inform appropriate social services if they reasonably suspect an older person is the victim of any form of abuse, even if statutes do not require such referral. Key features on history or physical examination are unexplained injuries in different stages of healing and a history of abuse. Many jurisdictions’ mandatory reporting laws include issues in addition to sexual or physical abuse, including financial abuse, emotional/psychological abuse, and self- or caregiver neglect. Doctors of chiropractic should be conversant with the particulars of laws in their jurisdiction.
Chiropractors should be alert to signs and symptoms of emotional and mental health issues. Depression with suicidal ideation mandates referral to a mental health provider. Acute confusion (delirium) often requires hospitalization, and cognitive impairments may necessitate involvement of a substitute decision maker.
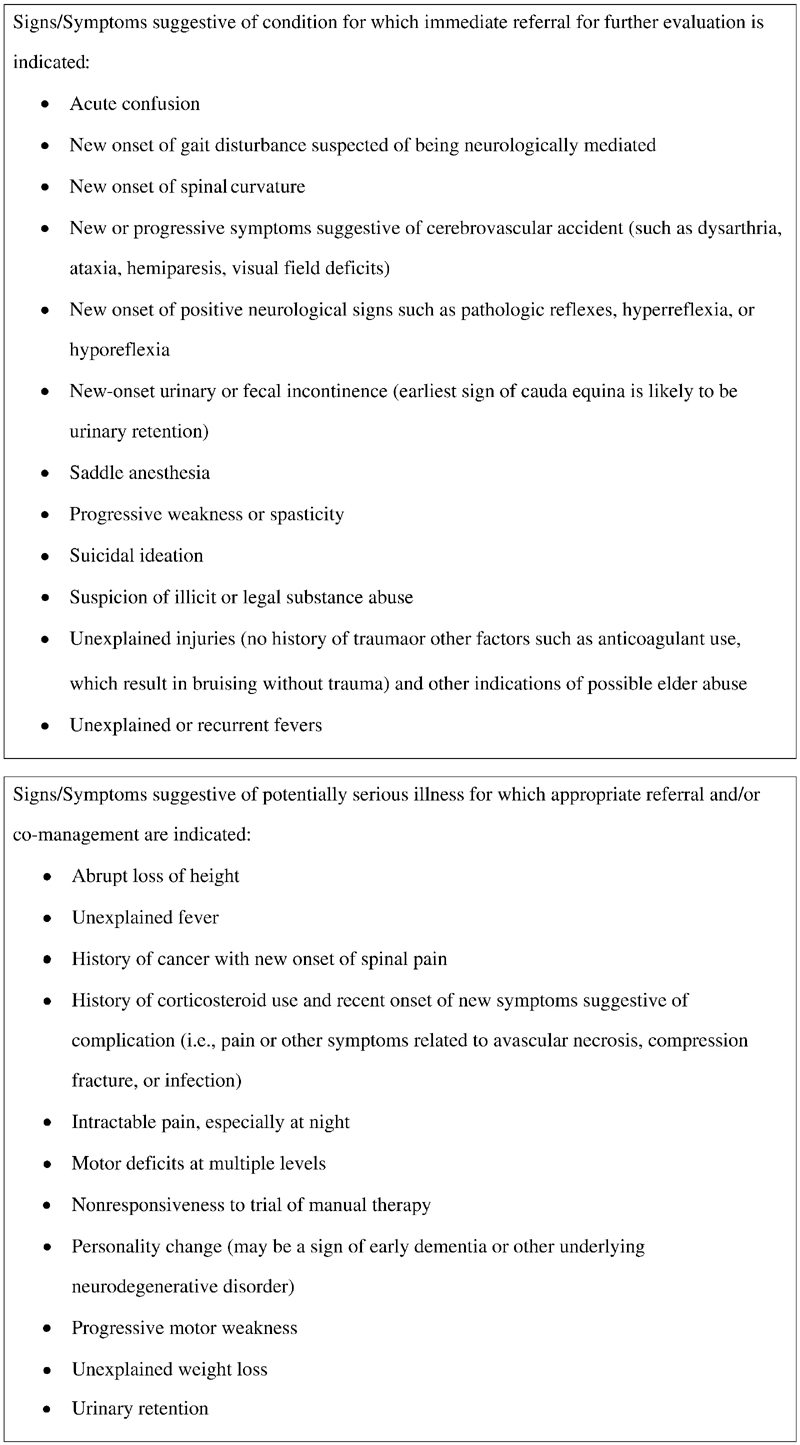
Figure 4 Red Flags If the history and/or examination reveal “red flags,” that is, absolute contraindications to care, or if these emerge during the course of care, the patient should be referred to an appropriate provider for further evaluation and/or care. See Figure 4 for a list of red flags.
Examination Physical examination should be based on case presentation, to identify potentially serious pathology and to support management decisions. Necessary diagnostic or examination procedures outside the practitioner’s scope of practice or range of experience should be referred to an appropriately qualified and experienced health professional.
Vital signs should be recorded, including temperature, heart rate, respiratory rate, weight, height, and blood pressure. The doctor should consider the need for measurement of sitting and standing blood pressure to rule out orthostatic hypotension. Although pain is often the predominant complaint of the older adult seeking care, it is important to assess function and quality of life in considering response to treatment.
Comprehensive geriatric assessment, considered a best practice, should include assessment of physical health, functional health, cognitive health, oral/nutritional health, and home-environmental safety.
Diagnostic Imaging—Conventional Radiography The use of radiography or repeated radiographs is not recommended without clear clinical justification. [49] Advanced age alone is not necessarily a clinical indication for diagnostic imaging. The use of conventional radiography and other imaging procedures should be based on current evidence-informed clinical practice guidelines and the clinical judgment of the managing clinician. [50]
Appropriate diagnostic imaging and/or referral for specialty consultation should be considered in patients who fail to respond to an initial brief trial of chiropractic care. In the patient who has failed to respond to this trial of care, the decision to pursue appropriate diagnostic imaging may be required to rule out serious conditions. The decision to pursue these tests should be based on a thorough history, physical exam, and any previous diagnostic testing that has been performed. [50]
Conventional radiographs may be indicated in cases of clinically suspected trauma-induced injury, such as fracture or dislocation, and in cases of suspected compression fracture (even in absence of significant trauma), as in patients with spinal pain that is not related to posture or position. [50]
Advanced Diagnostic Imaging Bone densitometry (BD) (not conventional radiography) is the most appropriate modality for the quantitative measurement of bone mass in patients with suspected metabolic bone disease such as osteoporosis and osteomalacia. BD should be performed in appropriate patients based on patient characteristics, including history, physical exam, patient preference, and availability of treatment options. [51]
Manual Procedures
The following considerations apply to treating older adults with manual procedures:
Biomechanical force should be modified as clinically warranted based on the history and physical
examination of the older adult.Higher-force manual techniques that may put strain on osseous structures are contraindicated
in the presence of severe osteoporosis or other bone-weakening processes.- [52]
When considering the application of soft tissue techniques for patients on anticoagulants or
steroids that exceed maintenance doses, the patient should be counseled on the risk of
bruising and/or bleeding.Patient preferences: The clinician should adapt manipulation and soft tissue techniques and
procedures to support the needs and comfort of the patient.Because of the current scarcity of research evidence, the doctor must rely on his or her clinical
experience when determining the appropriate high-velocity low-amplitude manipulative
procedure to use, in terms of patient positioning, to achieve the desired clinical effect.In cases where the application of high-velocity low-amplitude manipulation of the spine or peripheral
joints is contraindicated, the chiropractor may choose to use other low-force or minimal-force
chiropractic techniques to achieve the desired clinical effect.Care Planning
Care planning should also take into consideration such factors as whether the patient lives alone; his or her competence with activities of daily living; the availability of a competent caregiver, if needed; and the patient’s access to transportation and other necessary resources.
Routine manipulation of asymptomatic patients without clinical indicators is not recommended for therapeutic correction when maximal medical improvement has been reached. However, older adults often have significant musculoskeletal degeneration with chronic symptoms which may benefit from supportive management in the form of periodic evaluation and interventions that enable the older adult to maintain functional activities. Currently there is a paucity of data to support or deny this type of care. [53–55] Therefore this should be approached on an individual basis, taking patient preferences into account and encouraging self-management strategies.
Disease Prevention and Health Promotion
Health promotion in older adults is an emerging concept in preventive medicine. This would include advice to stay physically active, maintain a healthy diet, and engage in social activities. Doctors should also discuss “safe sun” (minimize sun exposure and use sun blocks) and “safe sex” (use of condoms for disease prevention) with patients for whom these are relevant issues. [56, 57]
There is a growing body of robust clinical evidence in support of the concept of “exercise as medicine.” [58] Older adult patients should be “prescribed” exercise with proper dose, intensity, and frequency suitable for the types of exercise (strength training, endurance, flexibility, proprioception/balance) in which each individual should engage. [59]
Immunization is a well-established medical approach to disease prevention, and older adult patients may ask their chiropractor for information about immunizations. Chiropractors should provide balanced, evidence-based information from credible resources, such as the Centers for Disease Control and Prevention, and/or recommend the patient consult his or her primary care physician or other provider whose scope of practice includes immunization. [60]
Older adults should be provided an opportunity to follow evidence-based recommendations for disease and risk factor screening and counseling, such as those of the U.S. Preventive Services Task Force. Doctors of chiropractic should stay current on these recommendations so that they can assist patients by either providing those services or making appropriate referrals. [61]
Discussion
As the population around the world ages, we see an increasing burden of musculoskeletal pain syndromes. [62] It is imperative in this time of increasing fiscal demands on global health care systems that there be an emphasis on effective and efficient care. The care of older adults is challenging, given the significant incidence of comorbidities that complicate both the assessment and management of their musculoskeletal conditions. In our original manuscript, we discussed the need for additional postgraduate training opportunities and for additional research studies. [5] Since that time the American Chiropractic Association has established a Council on Aging, which may be an important resource for the practicing chiropractor. In addition, 3 RCTs [23–25] and 2 cohort studies [26, 27] have been completed that investigated the role of chiropractic care in managing spinal pain in older adults.
Although several studies on the safety of chiropractic care for older adults have been published since our original paper, [29, 31–33 ]there remains a need to further investigate the safety of managing older adults with the use of manual therapy procedures. In addition, there is a need to investigate the role of the practicing chiropractor in the management of the overall health of the older adult. It is important to note that chiropractic management involves much more than the delivery of a manual therapy procedure. Management must involve appropriate clinical assessment of the patient to determine what the best course of care will be for this individual patient. Patient-centered care must focus on patient-specific goals (focusing on what is important to the patient) and an emphasis on self-management strategies that create patient independence.
There is growing evidence that the biopsychosocial model of pain must influence the management of older adults. [42] The results of the current best practice document emphasize that there is a need to further investigate this topic and to better train chiropractors in an approach to assessment and management that acknowledges this important topic.
The purpose of a consensus process is to inform the practicing clinician on best practices for the treatment of older adults where there is a lack of definitive data. We feel that the current project, although not different from the previously published best practices document, adds new and important language. The new statements are relevant to the areas of patient assessment, potential harm with manual therapy, and disease prevention. We continue to encourage investigation of the effectiveness of specific modalities of care in the older adult through the use of traditional RCTs, nonrandomized comparison studies, and retrospective reviews of large administrative databases. Another area for future investigation is the effectiveness of ongoing care in reinforcing treatment effects and encouraging compliance. Some studies on the effects of “booster sessions” suggest that this may be a promising avenue of research. [55] Observational studies on harm are important, and one of the most pressing areas requiring investigation is the appropriate selection of patients to undergo specific interventions. As providers manage older adults’ pain syndromes from a biopsychosocial perspective, it is important to acknowledge and appropriately manage the psychosocial aspects of pain.
Older adults continue to seek care from DCs for the management of their musculoskeletal complaints. Older adults are a complex population, requiring a thorough and conscientious approach to clinical assessment and management. Manual therapy, including spinal manipulation, is a reasonable and evidence-based approach to management of the older adult. However, there is a need for the practicing clinician to use patient-centered, self-management strategies to optimally manage this population. There remains a need for further development of postgraduate training specific to the management of older adults, as well as a need to increase the emphasis on unique challenges of management at the undergraduate level. In addition, there is a need to investigate the efficacy of biopsychosocial management strategies in the older adult population.
The literature on this topic is more plentiful for this updated study than for the earlier one from 2010, particularly in the area of safety. However, there remain many gaps in the literature required to answer both efficacy and effectiveness questions concerning the role of chiropractors in the management of older adults. The authors feel that the current document has addressed some of the concerns about the safety of SMT. The RCTs that have been performed since the last document give additional support for use of SMT in the older adult population, particularly with respect to its safety. Specifically, the data indicated that a higher incidence of adverse events is not associated with SMT as compared with other techniques [63] or sham interventions. [20, 22, 26] This document also provides additional guidance on the importance of tailored approaches to the evaluation of the older adult, specifically in the areas of cognitive impairment and preventive screening. [41]
Limitations and Strengths
The chief limitation of this study was that there was a heavy reliance on expert opinion through a consensus process because of the sparse literature on the effectiveness of chiropractic care specifically for older adults. Other limitations include the composition of the consensus panel, which consisted mainly of doctors of chiropractic and other health care providers and did not include payers, patients, or other stakeholders.
A strength of the current project was the addition of members with geriatric expertise outside the chiropractic profession, thus providing a perspective that will be more generalizable to the health care system as a whole. We feel that although much work remains to be done, some of the important gaps required to guide the practicing chiropractor were filled by this Delphi panel of experts.
Conclusion
This document provides a summary of evidence-informed best practices for doctors of chiropractic for the evaluation, management, and manual treatment of older adult patients.
Practical Applications
The consensus process using a multidisciplinary panel was successful in
updating a set of recommendations on key issues related to chiropractic
care for older adults.This document provides a general framework for an evidence-based and
reasonable approach to the chiropractic management of older adults.It should be seen not as a final product, but as a living document that
requires updates as new evidence emerges in the future.
Funding Sources and Conflicts of Interest
This study was funded by a grant from the NCMIC Foundation. All Delphi panelists served without compensation. The authors report no conflicts of interest.
Contributorship Information
Concept development (provided idea for the research): C.H., M.J.S.
Design (planned the methods to generate the results): C.H., M.J.S., M.H.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): C.H., M.J.S., M.H., P.K., P.D., B.G., L.Z.K., J.W.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): C.H., M.J.S., M.H.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): C.H., M.J.S., M.H.
Literature search (performed the literature search): C.H., M.J.S., M.H.
Writing (responsible for writing a substantive part of the manuscript): C.H., M.J.S., M.H., P.K., P.D., B.G., L.Z.K., J.W.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): C.H., M.S., M.H., P.K., P.D., B.G., L.K., J.W.
Acknowledgments
The authors thank Rachael Duwe, MPH, Project Coordinator, for keeping the consensus process on time and for organizing project communications, data, and documents in such a way that the project always ran smoothly. They also thank the Delphi panelists for their generous contribution of time and expertise, and without whom the project could not have been done: Michael Barbato, DC; André Bussières, DC, MSc, PhD; Jerrilyn Cambron, DC, PhD; Michael B. Clay, DC, MPH; Ezra Cohen, DC; Catherine Cummins, DC; Connie D’Astolfo, DC, PhD; Mark D. Dehen, DC; Ronald J. Farabaugh, DC; Kimary L. Farrar, MS, DC; Suzanne M. Gillespie, MD, MA, PhD; Brian Giuliani, DC; Jordan Gliedt, DC; Justin M. Goehl, DC, MS; Kathryn T. Hoiriis, DC; Jurgis Karuza, MA, PhD; Yasmeen Khan, DC; Robert A. Leach, DC, MS; K. Sean Mathers, DC, DPT; Teresa McCarthy, MD, MS; George B. McClelland, DC; Robert D. Mootz, DC; Paul J. Osterbauer, DC, MPH; David Paris, DC; Steven Passmore, DC, MS, PhD; Stephen M. Perle, DC, MS; Mark Pfefer, RN, MS, DC; Julie Plezbert, DC; Eric Roseen, DC; Stacie A. Salsbury, PhD, RN, MSN; Leonard Suiter, DC; Sivarama Prasad Vinjamury, MD (Ayurveda), MAOM, MPH; Carol Ann Weis, MSc, DC; Susan Wenberg, MA, DC; Wayne M. Whalen, DC; James M. Whedon, DC, MS.
References:
Centers for Disease Control and Prevention.
The State of Aging and Health in America 2013
Centers for Disease Control and Prevention,
US Dept of Health and Human Services, Atlanta, GA; 2013National Board of Chiropractic Examiners.
Practice Analysis of Chiropractic 2015
Author, Greeley, CO; 2015World Health Organization.
World Report on Ageing and Health.
Author, Geneva, Switzerland; 2015Weigel, PA, Hockenberry, JM, and Wolinsky, FD.
Chiropractic Use in the Medicare Population: Prevalence, Patterns, and Associations
With 1-Year Changes in Health and Satisfaction With Care
J Manipulative Physiol Ther. 2014 (Oct); 37 (8): 542-551Hawk C, Schneider M, Dougherty P, Gleberzon BJ, Killinger LZ.
Best Practices Recommendations for Chiropractic Care for Older Adults:
Results of a Consensus Process
J Manipulative Physiol Ther 2010 (Jul); 33 (6): 464–473Davis, MA, Yakusheva, O, Gottlieb, DJ, and Bynum, JP.
Regional Supply of Chiropractic Care and Visits to
Primary Care Physicians for Back and Neck Pain
J American Board of Family Medicine 2015 (Jul); 28 (4): 481–490Hawk, C, Long, CR, Boulanger, KT, Morschhauser, E, and Fuhr, AW.
Chiropractic care for patients aged 55 years and older: report from a practice-based research program.
J Am Geriatr Soc. 2000; 48: 534–545Lisi, AJ and Brandt, CA.
Trends in the Use and Characteristics of Chiropractic Services in the
Department of Veterans Affairs
J Manipulative Physiol Ther. 2016 (Jun); 39 (5): 381–386Eisenberg, DM, Kaptchuk, TJ, Post, DE et al.
Establishing an integrative medicine program within an academic health center: essential considerations.
Acad Med. 2016; 91: 1223–1230Council on Chiropractic Education.
Accreditation Standards, Principles, Processes & Requirements for Accreditation.
Author, Scottsdale, AZ; 2013Johnson, C, Rubinstein, SM, Cote, P et al.
Chiropractic care and public health: answering difficult questions about safety, care through the lifespan, and community action.
J Manipulative Physiol Ther. 2012; 35: 493–513Johnson, C and Green, BN.
Public Health, Wellness, Prevention, and Health Promotion:
Considering the Role of Chiropractic and Determinants of Health
J Manipulative Physiol Ther. 2009 (Jul); 32 (6): 405–412Johnson, C, Baird, R, Dougherty, PE et al.
Chiropractic and public health: current state and future vision.
J Manipulative Physiol Ther. 2008; 31: 397–410Shekelle, P, Woolf, S, Grimshaw, JM, Schunemann, HJ, and Eccles, MP.
Developing Clinical Practice Guidelines: Reviewing, Reporting, and Publishing Guidelines;
Updating Guidelines; and the Emerging Issues of Enhancing Guideline Implementability
and Accounting for Comorbid Conditions in Guideline Development
Implementation Science 2012 (Jul 4); 7: 62Shea, BJ, Bouter, LM, Peterson, J et al.
External validation of a measurement tool to assess systematic reviews (AMSTAR).
PLoS One. 2007; 2: e1350Shea, BJ, Grimshaw, JM, Wells, GA et al.
Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews.
BMC Med Res Methodol. 2007; 7: 10Higgins, JP, Altman, DG, Gotzsche, PC et al.
The Cochrane Collaboration's tool for assessing risk of bias in randomised trials.
BMJ. 2011; 343: d5928Wells, GA, Shea, B, Higgins, JP, Sterne, J, Tugwell, P, and Reeves, BC.
Checklists of methodological issues for review authors to consider when including non-randomized studies in systematic reviews.
Res Synth Methods. 2013; 4: 63–77Hawk C, Schneider M, Evans MW Jr, Redwood D:
Consensus Process to Develop a Best-Practice Document on the Role of Chiropractic Care
in Health Promotion, Disease Prevention, and Wellness
J Manipulative Physiol Ther. 2012 (Sep); 35 (7): 556–567Hawk, C, Schneider, M, Ferrance, RJ, Hewitt, E, Van Loon, M, and Tanis, L.
Best Practices Recommendations for Chiropractic Care for Infants, Children,
and Adolescents: Results of a Consensus Process
J Manipulative Physiol Ther. 2009 (Oct); 32 (8): 639–647Hawk, C, Schneider, MJ, Vallone, S, and Hewitt, EG.
Best Practices for Chiropractic Care of Children: A Consensus Update
J Manipulative Physiol Ther. 2016 (Mar); 39 (3): 158–168Fitch, K, Bernstein, SJ, Aquilar, MS et al.
The RAND UCLA Appropriateness Method User's Manual.
Santa Monica, CA, RAND Corp.; 2003Dougherty P, Karuza J, Dunn A, Savino D, Katz P:
Spinal Manipulative Therapy for Chronic Lower Back Pain in Older Veterans:
A Prospective, Randomized, Placebo-Controlled Trial
Geriatric Orthopaedic Surgery and Rehabilitation 2014 (Dec); 5 (4): 154–164Learman, KE, Showalter, C, O'Halloran, B, and Cook, CE.
Thrust and nonthrust manipulation for older adults with low back pain: an evaluation of pain and disability.
J Manipulative Physiol Ther. 2013; 36: 284–291Enix DE, SK, Malmstrom, TK, and Flaherty, JH.
A randomized controlled trial of chiropractic compared to physical therapy for chronic low back pain in community dwelling geriatric patients.
Top Integr Health Care. 2015; 6: 6.1002Weigel, PA, Hockenberry, J, Bentler, S, and Wolinsky, FD.
Chiropractic Use and Changes in Health Among Older Medicare Beneficiaries:
A Comparative Effectiveness Observational Study
J Manipulative Physiol Ther 2013 (Nov); 36 (9): 572-584Weigel, P.A., Hockenberry, J., Bentler, S.E., Wolinsky, F.D., 2014.
The Comparative Effect of Episodes of Chiropractic and
Medical Treatment on the Health of Older Adults
J Manipulative Physiol Ther 2014 (Mar); 37 (3): 143–154Holt, KR, Haavik, H, and Elley, CR.
The Effects of Manual Therapy on Balance and Falls: A Systematic Review
J Manipulative Physiol Ther. 2012 (Mar); 35 (3): 227–234Dougherty, PE, Engel, RM, Vemulpad, S, and Burke, J.
Spinal manipulative therapy for elderly patients with chronic obstructive pulmonary disease: a case series.
J Manipulative Physiol Ther. 2011; 34: 413–417Gleberzon, BJ.
A narrative review of the published chiropractic literature regarding older patients from 2001-2010.
J Can Chiropr Assoc. 2011; 55: 76–95Cambron, JA, Schneider, M, Dexheimer, JM et al.
A pilot randomized controlled trial of flexion-distraction dosage for chiropractic treatment of lumbar spinal stenosis.
J Manipulative Physiol Ther. 2014; 37: 396–406Whedon, JM, Mackenzie, TA, Phillips, RB, and Lurie, JD.
Risk of Traumatic Injury Associated with Chiropractic Spinal Manipulation
in Medicare Part B Beneficiaries Aged 66-99
Spine (Phila Pa 1976) 2015 (Feb 15); 40 (4): 264–270Whedon, JM, Song, Y, Mackenzie, TA, Phillips, RB, Lukovits, TG, and Lurie, JD.
Risk of Stroke After Chiropractic Spinal Manipulation in Medicare B Beneficiaries
Aged 66 to 99 Years With Neck Pain
J Manipulative Physiol Ther. 2015 (Feb); 38 (2): 93–101Church, EW, Sieg, EP, Zalatimo, O, Hussain, NS, Glantz, M, and Harbaugh, RE.
Systematic Review and Meta-analysis of Chiropractic Care and Cervical Artery Dissection:
No Evidence for Causation
Cureus 2016 (Feb 16); 8 (2): e498Kosloff, TM, Elton, D, Tao, J, and Bannister, WM.
Chiropractic Care and the Risk of Vertebrobasilar Stroke: Results of a Case-control Study
in U.S. Commercial and Medicare Advantage Populations
Chiropractic & Manual Therapies 2015 (Jun 16); 23: 19Chung, CL, Cote, P, Stern, P, and L'Esperance, G.
The association between cervical spine manipulation and carotid artery dissection: a systematic review of the literature.
J Manipulative Physiol Ther. 2015; 38: 672–676Herzog, W, Tang, C, and Leonard, T.
Internal Carotid Artery Strains During High-Speed, Low-Amplitude
Spinal Manipulations of the Neck
J Manipulative Physiol Ther. 2015 (Nov); 38 (9): 664–671Piper, SL, Howarth, SJ, Triano, J, and Herzog, W.
Quantifying strain in the vertebral artery with simultaneous motion analysis of the head and neck: a preliminary investigation.
Clin Biomech (Bristol, Avon). 2014; 29: 1099–1107Quesnele, JJ, Triano, JJ, Noseworthy, MD, and Wells, GD.
Changes in Vertebral Artery Blood Flow Following Various Head Positions
and Cervical Spine Manipulation
J Manipulative Physiol Ther. 2014 (Jan); 37 (1): 22–31Biller J, Sacco RL, Albuquerque FC, et al.:
Cervical Arterial Dissections and Association With Cervical
Manipulative Therapy A Statement for Healthcare Professionals
From the American Heart Association/ American Stroke Association
Stroke. 2014 (Oct); 45 (10): 3155–3174Hebert JJ, Stomski NJ, French SD, et al.
Serious Adverse Events and Spinal Manipulative Therapy
of the Low Back Region: A Systematic Review of Cases
J Manipulative Physiol Ther 2015 (Nov); 38 (9): 677–691Morone, NE, Greco, CM, Moore, CG et al.
A mind-body program for older adults with chronic low back pain: a randomized clinical trial.
JAMA Intern Med. 2016; 176: 329–337Sackett, DL, Straus, SE, Richardson, WS et al.
Evidence-Based Medicine: How to Practice and Teach EBM. 2nd ed.
Edinburgh, Church Livingstone; 2000Stewart, M, Brown, JB, Donner, A et al.
The impact of patient-centered care on outcomes.
J Fam Pract. 2000; 49: 796–804Moye, J and Marson, DC.
Assessment of decision-making capacity in older adults: an emerging area of practice and research.
J Gerontol B Psychol Sci Soc Sci. 2007; 62: P3–P11Langworthy, JM and Cambron, J.
Consent: its practices and implications in United Kingdom and United States chiropractic practice.
J Manipulative Physiol Ther. 2007; 30: 419–431Clar C, Tsertsvadze A, Court R, Hundt G, Clarke A, Sutcliffe P.
Clinical Effectiveness of Manual Therapy for the Management of
Musculoskeletal and Non-Musculoskeletal Conditions:
Systematic Review and Update of UK Evidence Report
Chiropractic & Manual Therapies 2014 (Mar 28); 22 (1): 12Gleberzon, B.
Geriatric Chiropractic Care as a Health Promotion and Disease Prevention Initiative:
Focus on Fall Prevention
Topics in Integrative Health Care 2010 (Dec 30); 1 (2)Chou, R, Fu, R, Carrino, JA, and Deyo, RA.
Imaging strategies for low-back pain: systematic review and meta-analysis.
Lancet. 2009; 373: 463–472Bussieres, AE, Taylor, JA, and Peterson, C.
Diagnostic Imaging Practice Guidelines for Musculoskeletal Complaints in Adults —
An Evidence-Based Approach
J Manipulative Physiol Ther. 2008; 31: 33–88Celi, M, Rao, C, Scialdoni, A et al.
Bone mineral density evaluation in osteoporosis: why yes and why not?.
Aging Clin Exp Res. 2013; 25: S47–S49Manchikanti, L, Falco, FJ, Benyamin, RM et al.
Assessment of bleeding risk of interventional techniques: a best evidence synthesis of practice patterns and perioperative management of anticoagulant and antithrombotic therapy.
Pain Physician. 2013; 16: SE261–SE318Eklund, A, Axen, I, Kongsted, A, Lohela-Karlsson, M, Leboeuf-Yde, C, and Jensen, I.
Prevention of low back pain: effect, cost-effectiveness, and cost-utility of maintenance care—study protocol for a randomized clinical trial.
Trials. 2014; 15: 102Axen, I and Bodin, L.
The Nordic Maintenance Care Program:
The Clinical Use of Identified Indications for Preventive Care
Chiropractic & Manual Therapies 2013 (Mar 6); 21: 10Fleig, L, Pomp, S, Schwarzer, R, and Lippke, S.
Promoting exercise maintenance: how interventions with booster sessions improve long-term rehabilitation outcomes.
Rehabil Psychol. 2013; 58: 323–333US Preventive Services Task Force (USPSTF).
Guide to Clinical Preventive Services.
Agency for Healthcare Research and Quality (AHRQ),
Washington, DC; 2012Wernli, KJ, Henrikson, NB, Morrison, CC, Nguyen, M, Pocobelli, G, and Blasi, PR.
Screening for skin cancer in adults: updated evidence report and systematic review for the US Preventive Services Task Force.
JAMA. 2016; 316: 436–447Pedersen, BK and Saltin, B.
Exercise as medicine: evidence for prescribing exercise as therapy in 26 different chronic diseases.
Scand J Med Sci Sports. 2015; 25: 1–72American Geriatric Society.
Exercise prescription for older adults with osteoarthritis pain: consensus practice recommendations. A supplement to the AGS Clinical Practice Guidelines on the management of chronic pain in older adults.
J Am Geriatr Soc. 2001; 49: 808–823Khorsan, R, Smith, M, Hawk, C, and Haas, M.
A public health Immunization Resource web site for chiropractors: discussion of current issues and future challenges for evidence-based initiatives for the chiropractic profession.
J Manipulative Physiol Ther. 2009; 32: 500–504Hawk, C and Evans, MW Jr.
A framework for chiropractic training in clinical preventive services.
Chiropr Man Ther. 2013; 21: 28Briggs, AM, Cross, MJ, Hoy, DG et al.
Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 World Health Organization World Report on Ageing and Health.
Gerontologist. 2016; 56: S243–S255Hondras MA, Long CR, Cao Y, et al.
A Randomized Controlled Trial Comparing 2 Types of Spinal Manipulation
and Minimal Conservative Medical Care for Adults 55 Years and Older
With Subacute or Chronic Low Back Pain
J Manipulative Physiol Ther. 2009 (Jun); 32 (5): 330–343
Return to MEDICARE
Return to SENIOR CARE
Return to BEST PRACTICES
Since 4–07–2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |