

Chiropractic Use in the Medicare Population:
Prevalence, Patterns, and Associations With
1-Year Changes in Health and Satisfaction With CareThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther. 2014 (Oct); 37 (8): 542-551 ~ FULL TEXT
OPEN ACCESS Paula A.M. Weigel, PhD, Jason M. Hockenberry, PhD, Fredric D. Wolinsky, PhD
Research Associate,
Department of Health Management and Policy,
College of Public Health,
The University of Iowa, Iowa City, IA.
OBJECTIVE: The purpose of this study was to examine how chiropractic care compares to medical treatments on 1–year changes in self-reported function, health, and satisfaction with care measures in a representative sample of Medicare beneficiaries.
METHODS: Logistic regression using generalized estimating equations is used to model the effect of chiropractic relative to medical care on decline in 5 functional measures and 2 measures of self-rated health among 12,170 person-year observations. The same method is used to estimate the comparative effect of chiropractic on 6 satisfaction with care measures. Two analytic approaches are used, the first assuming no selection bias and the second using propensity score analyses to adjust for selection effects in the outcome models.
RESULTS: The unadjusted models show that chiropractic is significantly protective against 1–year decline in activities of daily living, lifting, stooping, walking, self-rated health, and worsening health after 1 year. Persons using chiropractic are more satisfied with their follow-up care and with the information provided to them. In addition to the protective effects of chiropractic in the unadjusted model, the propensity score results indicate a significant protective effect of chiropractic against decline in reaching.
CONCLUSION: This study provides evidence of a protective effect of chiropractic care against 1–year declines in functional and self-rated health among Medicare beneficiaries with spine conditions, and indications that chiropractic users have higher satisfaction with follow-up care and information provided about what is wrong with them.
From the Full-Text Article:
Introduction
National surveys and other data show chiropractic use prevalence rates among those 18 years and older, ranging between 5.6% and 8.6% in the United States. [1–3] Among Medicare beneficiaries 70 years and older, chiropractic use is less prevalent, with 2 studies indicating annual rates ranging between 4.1% and 5.4%. [4, 5] For younger Medicare beneficiaries, chiropractic prevalence rates are closer to national rates, ranging between 6% and 7%. [6] Although informative, these estimates are not reflective of the population that commonly seeks care from doctors of chiropractic — namely, persons seeking treatment of spine-related health conditions. [2, 7–9] Prevalence of chiropractic use is likely higher in the population of Medicare beneficiaries with back and neck conditions, but how much higher is not known.
Spine-related problems are common in the general adult population, and there is evidence of increasing prevalence as people age. [10–14] As a result, spine conditions reflect a growing portion of health services use and expenditures, particularly under Medicare. [6, 15, 16] More significantly, these problems are associated with increased disability by impeding a person's capacity to perform everyday mobility tasks such as walking, stooping, lifting, or reaching. Those mobility tasks can subsequently limit a person's ability to perform basic activities of daily living (ADLs), all of which are crucial to prolonging independence among older adults living in a community setting. [17–22]
Medicare covers several treatment options ranging from the noninvasive like chiropractic and physical therapy to the more invasive, such as steroidal injections and surgery. Studies have shown that the technologically intensive treatment types have grown more dramatically, both in use and in expenditures, than the noninvasive kind over the past 15 to 20 years. [3, 6, 12, 16, 23–26] Although these studies document the increasing use of interventional treatments, they also note that population-level improvements in outcomes and disability have not improved commensurately.
Recent research, however, suggests that chiropractic use benefits older Medicare beneficiaries (>70 years) by protecting them against decline in function and self-rated health (SRH). [27] Because that study used Medicare claims to compare outcomes between users of chiropractic and users of medical care treatments in uncomplicated back conditions over a 2–year period, it represents a real-world approximation of the relative benefit of chiropractic use on health outcomes.
Given the escalating costs of treatment and the ramifications of disability on future dependency, [28, 29] it is important to understand the prevalence and the relative effect on health and care, costs of chiropractic use among age-eligible Medicare beneficiaries with spine-related problems. Equally important is how patients view the quality of care received from different treatment types. If treatments have comparable effects on health, but disparate care costs or satisfaction, then policy makers may consider incentives or disincentives to promote particular treatments for certain conditions.
This study uses the Medicare Current Beneficiary Survey (MCBS) linked to Medicare provider claims to examine chiropractic use among Medicare beneficiaries with spine conditions. This research study has 3 objectives:(1) to describe the prevalence of chiropractic use among age-eligible Medicare beneficiaries in general and among those with spine problems in particular;
(2) to describe treatment patterns, service trends, and Medicare expenditures among persons who mostly use chiropractic vs those that are users of medical care only; and
(3) to determine the comparative effect of chiropractic relative to medical care only on 1–year changes in function, self-rated health (SRH), and satisfaction with care.
Methods
Study Population
A detailed description of the Medicare Current Beneficiary Survey (MCBS), associated technical documentation, and its sample design can be found elsewhere. [30, 31] We used the MCBS survey linked to provider claims between 1997 and 2006 to construct nine person-year observations for Medicare beneficiaries, which were then pooled to examine changes in health outcomes. The MCBS is a continuous, rotating panel survey of a nationally representative sample of Medicare beneficiaries sponsored by the Centers for Medicare and Medicaid Services (CMS). The Access to Care file contains survey participants’ demographic and socioeconomic information, their health and functional status, health care use history, and satisfaction with care responses. The matched claims data includes Medicare payment for physician services. [32]
Sample
Our sample includes fee-for-service Medicare beneficiaries who were age-eligible (≥65) and living in the community at the time of their first and second interviews. We excluded persons with end-stage renal disease (ESRD) because their functional health trajectory differs from those who do not have permanent kidney failure, and we excluded those that did not survive to the end of the second interview year because of their imminent mortality. Survey participants had to have two consecutive interviews one-year apart to determine changes in health outcomes. Self- or proxy-respondents were included in each person-year panel.
To be included in the spine condition subsample, MCBS participants had to have at least one claim with an International Classification of Diseases, Clinical Modification (ICD-9 CM) diagnosis code falling under the category of “Diseases of the Musculoskeletal System and Connective Tissue” or “Dislocation” or “Sprains and Strains of Joints and Adjacent Muscles” between first and second interviews (see Appendix 1 for the ICD-9 CM diagnosis codes used). Diagnoses by medical doctors that contraindicated chiropractic (e.g., 839.1 “Cervical Vertebra, open” or 839.3 “Thoracic and Lumbar Vertebra, open”) were excluded.
Outcome Measures
We examined thirteen outcomes, five measuring functional decline, two measuring changes in self-assessed health, and six reflecting satisfaction with discrete aspects of care. Of the five functional health outcomes, the first is decline in ADLs. The ADL measure was the sum of five daily activities that the participant reported difficulties in or the inability to perform at the time of their interview: bathing, getting in or out of a chair, dressing, eating, and walking across a room. A decline is reflected by a person adding at least one new ADL limitation between interviews. The remaining functional decline measures reflect going from one level of difficulty to a greater difficulty level (e.g., from ‘little difficulty’ to ‘some difficulty’) on four tasks: lifting or carrying ten pounds (lifting), extending arms above shoulder (reaching), stooping/crouching/kneeling (stooping), and walking ¼ mile or 2–3 blocks (walking).
The two self-reported health outcomes are decline in self-rated health (SRH) and changes in comparative health after one year. Decline in SRH occurred if a person rated their general health at a worse level in the second interview compared to the first. The five response options were excellent (1), very good (2), good (3), fair (4), and poor (5). The comparative health measure was in response to the question “Health compared to one year ago is ________”, where response options were ‘much better’, ‘somewhat better’, ‘about same’, ‘somewhat worse’, or ‘much worse’. Responses were collapsed into “worse comparative health” relative to “same comparative health” and “better comparative health”.
The six satisfaction outcome measures address quality of care received over the past year, doctor’s concern for overall health, out of pocket costs for services, ease of getting to doctor, satisfaction with follow-up care, and satisfaction with information about what was wrong. Responses were dichotomized to ‘satisfied’ (1) or ‘dissatisfied’ (0).
Focal Variable
The focal variable is chiropractic use. If a participant used any chiropractic services during the year between survey interviews indicated by a provider specialty code of ‘35’ in the Medicare Part B claims, s/he was designated a chiropractic user and coded 1 on the treatment variable. If not, the person was assigned to medical care only status and coded 0. While a participant in the chiropractic treatment group could also use other non-chiropractic services for spine treatment, prior research has indicated that conditional upon choosing chiropractic for a particular care episode, the vast majority of services used during that episode are chiropractic.27,33
Covariates
Using Andersen and Aday’s behavioral model of health services use, [34, 35] we included a set of covariates in all analyses to account for potential risk factors. [4, 5] Predisposing factors include age, sex, and race. Enabling factors are marital status, education, income, and metro/non-metro location of residence. Need factors include disease history markers (arthritis, broken hip, cancer, coronary heart disease, chronic obstructive pulmonary disease (COPD), diabetes, heart attack, hypertension, osteoporosis, psychological problems, rheumatoid arthritis, and stroke), as well as functional status at time of first interview (ADLs, difficulty lifting, reaching, stooping, and walking), self-rated health, vision and hearing acuity, and health worries.
Other need factors influenced by lifestyle and prior health services use include four weight categories based on BMI cut-offs (underweight, normal, overweight, and obese), two smoking status measures (‘ever smoke’ and ‘currently smoke’), and two measures of health services use in the prior year (hospitalized or not, and a three-level categorization of office visits—none, 1 to 5, and 6 or more).
Finally, we included a marker of whether a person participated in managed care or not during the year and indicators of whether a person was a self-respondent at both interviews, a proxy at both interviews, or a combination of self- and proxy at either interview. These variables were included because (1) the claims experience of persons in managed care would be different than those in fee-for-service (under-represented), and (2) the assessments of change in function and health are affected by whom (self-respondent vs. proxy respondent) is answering the survey questions.18
Analysis
The prevalence of chiropractic use among all Medicare beneficiaries and among those with spine conditions are described. Treatment patterns are characterized by the average number of services provided and the portion that are chiropractic, as well as by the mix of providers seen each year. Average Medicare Part B expenditures on behalf of beneficiaries with spine conditions are calculated for each treatment group each year, as is the sub-set of spending on chiropractic services. Spending for spine conditions from institutional-based services (such as inpatient stays) or Part D benefits, however, are not characterized here. Trends are described for mean service volume, provider distribution, and mean expenditures. The comparative effect of care for persons incorporating chiropractic into their treatment plan relative to care among persons using only medical or non-chiropractic services (e.g., physical therapy) on one-year changes in health and satisfaction is modeled. Because each person may contribute several person-period observations, we used Generalized Estimating Equations (GEE) logistic regression methods to adjust for within-person correlation. To account for potential selection bias inherent in comparing different treatment effects in observational data, [36–39] propensity score weighted models are also estimated on the health and satisfaction outcomes. The propensity score models used state chiropractor supply data for the interview start year, in addition to other known risk factors to estimate a probability of chiropractic use for each person-year observation. [4, 5, 40–42] Once the propensity scores were estimated, the inverse probability of treatment weights (IPTW) were calculated and multiplied by the one-year sample weight provided in the MCBS to obtain a propensity score adjusted sample weight.
Human Subjects Approval This research was supported by grant R21 AT004578 from the National Institutes of Health (NIH) to Dr. Wolinsky. The human subject protocol was fully approved by the University of Iowa Institutional Review Board (IRB) in March 2003 and annually thereafter. A Restricted Data Agreement with the University of Michigan Survey Research Center (2003–006), and subsequent completion and approval of a Data Use Agreement with the Centers for Medicare and Medicaid Services (DUA 14807) was approved in March 2005 with subsequent modifications and extensions through 2014. Written informed consent was obtained from all AHEAD participants.
Results
Prevalence

Table 1

Table 2 The average annual population prevalence of community-dwelling and age-eligible Medicare beneficiaries using chiropractic was 7.4% (range 6.3% to 8.9%). Among persons with spine conditions, the average annual prevalence was 34.5% (range 32.4% to 35.7%). Year-by-year prevalence rates are shown in Table 1.
Sample Descriptives
Table 2 compares persons who used chiropractic with those that did not for treatment of spine conditions. People who chose chiropractic for their spine care were significantly younger, male, white, and married. They were high school graduates, in the highest income category (> $25K), and comparatively less likely to live in metropolitan areas. Chiropractic users were also relatively healthier than the medical only group based upon presence of disease conditions, having significantly lower proportions of arthritis and rheumatoid arthritis; heart disease, heart attacks, and stroke; and diabetes, hypertension, and osteoporosis, though among these last three conditions the prevalence among users of chiropractic increased over time.
Chiropractic users also had significantly less functional limitation as reflected by fewer ADLs and less self-reported difficulty lifting, reaching, stooping, and walking several blocks. Vision was better and self-rated health higher among those using chiropractic. The proportion of chiropractic users worried about their health was significantly lower than those using medical only care, which could be a reflection of the relative disease burden for each group.
Finally, chiropractic users had proportionately fewer hospitalizations in the year prior to their first interview and were less prevalent in the highest category of office visits (> 6 per year) compared to medical only users. Again, this difference in health services use could be a reflection of the disparity in disease conditions. The chiropractic use group also had significantly higher representation in the category of self-respondent at both first and second interviews.
Unadjusted Differences in Outcomes

Table 3 Table 3 presents unadjusted differences on the outcomes. The chiropractic user group experienced proportionately less functional decline as reflected by limitations in ADLs and difficulty in lifting, reaching and walking several blocks. They were also less likely to rate their health worse over the year compared to those in the medical services only group. Among the satisfaction measures, persons in the chiropractic use group were more satisfied with care quality, out of pocket costs, follow-up after the initial visit, and with information provided about what was wrong with them. There were no differences between treatment groups on decline in self-rated health, satisfaction with providers’ concern, and ease of getting to doctor from where participant lives.
Patterns of Use by Treatment Group
The average annual volume of services used to treat spine conditions grew between 1997 and 2006 among both treatment groups. The chiropractic user group had nearly double the average service volume of the medical only group (mean 15.2 services per year vs. 7.7, respectively) over the nine person-year panels. On average, 82% of the service volume among chiropractic users was chiropractic with primary care (internal medicine, general practice, family practice) being only 5%. Over time, however, the percentage of services that were chiropractic decreased as other non-chiropractic services were used to treat spine conditions.
The mix of providers also changed over time and within treatment groups. Among chiropractic users, services sought from physical therapists grew from 0.7% in the 1997–1998 panel to 9.2% in the 2003–2004 panel. Likewise, among the medical only group, physical therapy services as a portion of all services grew markedly between the 1997–1998 panel and the 2004–2005 panel (from 12.1% to 32.2%). In the medical care only group there was greater provider heterogeneity, ranging from primary care providers delivering 21% of services to physical therapists/physical medicine and rehabilitation (28%) to specialists such as orthopedists and anesthesiologists (18.3%). Neurology and neurosurgery services also grew over the period in the medical only group. The heterogeneity may be due to patient preferences, clinical indication, condition severity or chronicity, or a combination of these factors, all of which are unobservable from claims data. Detailed data on provider distributions by treatment group are available from the first author upon request.
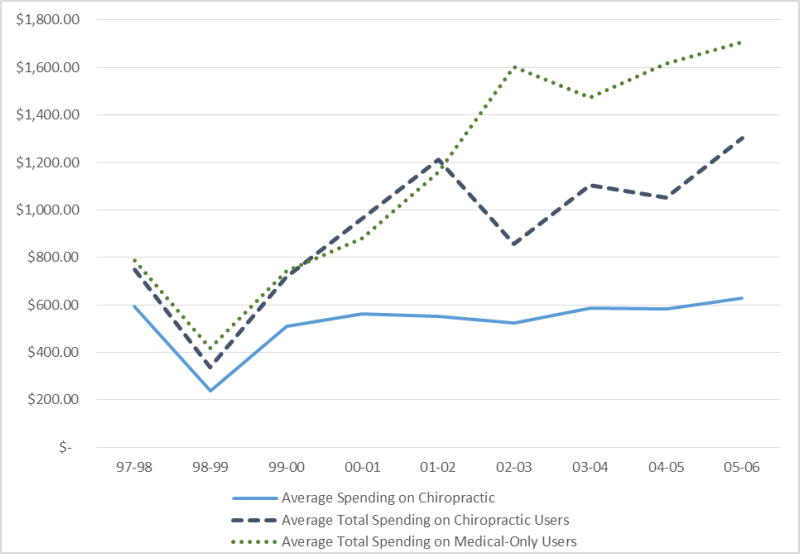
Figure 1 Average annual Medicare spending on spine-related conditions roughly doubled over the nine-year period. Spending trends for both treatment groups were similar between 1997 and 2002, but diverged after 2002 when spending in the chiropractic user group grew at a slower rate than that of the medical group (Figure 1). Medicare spending on chiropractic remained flat between 1999 and 2006, decreasing from 71% of total spending on spine conditions in 1999–2000 to 48% of total spending in 2005–2006.
Effect of Chiropractic on Outcomes

Table 4

Table 5 Table 4 shows the results for both the unadjusted and adjusted health outcome models. Without adjusting for selection bias, we found that chiropractic was significantly protective against declines in ADLs, lifting, stooping, and walking several blocks. After adjusting for potential selection bias using IPTWs, we observed a protective effect of chiropractic against decline in all five functional outcomes, including reaching. Chiropractic was also found to be protective against one-year declines in self-rated health and worsening health compared to one year ago in both the unadjusted and adjusted models. Table 5 shows the results for both the unadjusted and adjusted satisfaction outcome models Participants in the chiropractic use group had higher satisfaction with follow-up after initial visit and with information provided about what was wrong with them. These results were consistent in magnitude regardless of whether the models adjusted for selection using the IPTWs or not.
Discussion
We investigated chiropractic use among community-dwelling age-eligible Medicare beneficiaries over a 9–person-year period (1997–2006). We found annual prevalence rates similar to those reported from the National Health Interview Surveys. [1, 2] Our prevalence estimates for chiropractic use among beneficiaries with spine diagnoses, however, are much higher (35%), indicating that chiropractic is a commonly sought treatment among those with back and neck problems. Furthermore, chiropractic users appear to have strong preferences for chiropractic treatment once they choose chiropractic compared with other types of services based on the percent of overall service volume for chiropractic relative to other care, although the data on provider mix suggest a trend toward service provision by others.
Service volume trends were similar between treatment groups, with average yearly service volume steadily increasing between the 1997 to 1998 panel and the 2005 to 2006 panels. On a percentage basis, however, service volume in the medical only group grew slightly more between the 1997 to 1998 panel and the 2005 to 2006 panel (58% vs 41% for the chiropractic use group). Chiropractic volume grew at a lesser rate than the overall average volume, and consequently, chiropractic volume as a percentage of all services used to treat spine conditions declined over time (from 90% in 1997–1998 to 78% in 2005–2006). This trend is also evident in the distribution of provider data, where a growing proportion of services among the chiropractic use group went to physical therapists.
As a byproduct of the service volume growth and differences in prices between general and specialty care, average spending per year by Medicare also increased between the first and last panels in both groups. Once again, this occurred at a faster rate in the medical only group relative to the chiropractic user group (117% vs 74%, respectively). Furthermore, the percent growth in average chiropractic spending per year from 1997–1998 to 2005–2006 was only 6%, which is remarkably lower than the growth in overall spending in each group. Inflation-adjusted spending on chiropractic was essentially flat over the period and was accompanied by a declining portion of total spending among persons using chiropractic (from 79% to 48% in 1997–1998 and 2005–2006, respectively). In support of conclusions by Whedon et al. [6] about trends in use and costs of chiropractic spinal manipulation in the Medicare population, our results suggest Medicare payments for chiropractic services (at least among those with spine conditions) are relatively less of a payment vulnerability for the Medicare program than has been implied in the past. [43]
We found that chiropractic use is comparatively protective against 1–year declines in function and self-assessed health among Medicare beneficiaries with spine conditions and is also associated with higher satisfaction on measures of follow-up care and with information provided. Furthermore, we found that the models measuring the effect of chiropractic on functional health, self-rated health (SRH), and satisfaction with care using IPTWs are consistent with the models that are not adjusted for potential selection to treatment. By using propensity score methods, we accounted for potential selection bias using the data available. In so doing, we demonstrated that the causal effects using IPTWs were similar to those observed without such adjustments.
Limitations and Future Research
The decision to combine back and neck conditions in these analyses introduces clinical condition heterogeneity that could make indistinguishable the comparative effect of chiropractic on health changes for certain specific conditions. However, we felt that expanding the number and types of conditions for which people consistently choose chiropractic was important to the overall picture of how chiropractic is used in this population.
We did not aggregate service use into episodes of care but rather looked at overall service use and spending over the course of a year. Whether chiropractic treatment is comparatively effective at slowing functional decline is a function of how it is delivered in practice for a particular clinical presentation. Evidence of chiropractic efficacy has shown a minimally effective “dosing” level of up to 12 treatments over a several week period, with some studies suggesting that an additional monthly treatment thereafter prolongs the benefit. [44–46] Combining related service claims into episodes of care could further refine treatment effect estimates, although it would likely introduce analytical complexity due to care that is proximal but outside the 1–year interview window (left and right censoring).
Another limitation is related to the satisfaction with care outcomes. Questions regarding satisfaction in the MCBS are not specific to a particular treatment delivered for an identifiable health condition but rather are about the medical services received since the time of the last interview. Accordingly, a distinction cannot be made between health services delivered for a back condition vs those delivered for a heart condition. Persons seeking treatment of spine conditions had health services use for other conditions as well, thus confounding satisfaction perceptions across a variety of providers. Had the questions been related only to care received for spine conditions, a better distinction between treatment groups could be made.
Despite attempts to adjust for potential selection bias using IPTWs, it remains possible that unobserved confounders affected the treatment effect on declines in health.
Future research will focus on distinguishing further among specific types of spine conditions to better determine the comparative effect of chiropractic relative to medical only care on the health and well-being of Medicare beneficiaries with specific clinical conditions.
Conclusion
This study found prevalence of chiropractic use among age-eligible Medicare beneficiaries consistent with that of the US adult population, but among those seeking care for spine problems, we observed a much higher prevalence rate. Service volume trends between 1997 and 2006 showed growth in the average number of services used to treat spine conditions, although the percentage growth of chiropractic services was nearly flat compared with overall service volume growth. Medicare spending on spine conditions grew as a consequence of higher service volume and more expensive services, although spending on chiropractic was relatively flat and declined as a percentage of total spending among those choosing chiropractic.
This study provides evidence of a protective effect of chiropractic against 1–year declines in functional and self-rated health (SRH) among Medicare beneficiaries with spine conditions, and indications that chiropractic users have higher satisfaction with follow-up care and information provided about what is wrong with them.
Return to MEDICARE
Return to INITIAL PROVIDER/FIRST CONTACT
Since 1–18–2014


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |