

Efficacy of Selected Complementary and Alternative
Medicine Interventions For Chronic PainThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Rehabil Res Dev. 2007; 44 (2): 195222 ~ FULL TEXT
OPEN ACCESS Gabriel Tan, PhD, ABPP, Michael H. Craine, PhD, Matthew J. Bair, MD, MS,
M. Kay Garcia, DrPH, MSN, RN, LAc, James Giordano, PhD,
Mark P. Jensen, PhD, Shelley M. McDonald, MD
Department of Anesthesiology,
Michael E. DeBakey Department of Veterans Affairs (VA) Medical Center (VAMC),
2002 Holcombe Blvd,
Houston, TX 77030, USA.
tan.gabriel@med.va.govComplementary and alternative medicine (CAM) is a group of diverse medical and healthcare systems, therapies, and products that are not presently considered part of conventional medicine. This article provides an up-to-date review of the efficacy of selected CAM modalities in the management of chronic pain. Findings are presented according to the classification system developed by the National Institutes of Health National Center for Complementary and Alternative Medicine (formerly Office of Alternative Medicine) and are grouped into four domains: biologically based medicine, energy medicine, manipulative and body-based medicine, and mind-body medicine. Homeopathy and acupuncture are discussed separately as "whole or professionalized CAM practices." Based on the guidelines of the Clinical Psychology Division of the American Psychological Association, findings indicate that some CAM modalities have a solid track record of efficacy, whereas others are promising but require additional research. The article concludes with recommendations to pain practitioners.
From the FULL TEXT Article:
INTRODUCTION
Definition of Complementary and Alternative Medicine
Complementary and alternative medicine (CAM) is a group of diverse medical and healthcare systems, therapies, and products that are not presently considered part of conventional medicine. They are not generally provided by U.S. hospitals and clinics or widely taught in medical schools [1].
Prevalence and Popularity of Complementary and Alternative Medicine Use
CAM modalities are widely used by the U.S. public. According to the Centers for Disease Control and Prevention (CDC), 62 percent of adults used some form of CAM during the past 12 months when the definition of CAM included prayer specifically for health reasons and 36 percent when prayer was excluded [2]. The most frequent conditions associated with CAM use included back pain, neck pain, joint pain, stiffness, anxiety, and depression (the latter two are commonly associated with chronic pain). CAM use increased substantially during the 1990s. The U.S. public spent an estimated $36 to $47 billion on CAM in 1997 alone [3]; between $12.2 and $19.6 billion were paid out-of-pocket for the services of CAM providers such as chiropractors, acupuncturists, and massage therapists. These fees are more than the U.S. public paid out-of-pocket for all hospitalizations in 1997 and half the amount of all out-of-pocket physician services for traditional care [4].
Purpose of This Article
Despite the immense popularity of CAM, its efficacy is controversial. Many view CAM as encompassing unproven therapies of questionable efficacy. This article comprehensively reviews the efficacy of various CAM modalities in the management of chronic pain. The review has been restricted to chronic pain because of the wider availability of efficacious traditional interventions for acute pain. However, as our effort progressed, we realized that the relevant literature encompasses a wide range of CAM modalities and a large variety of chronic pain conditions. Thus, great variation exists regarding the number, type, and quality of trials for each specific CAM approach, with some modalities (e.g., acupuncture) possessing a large literature and many other modalities (e.g., craniosacral therapy) having been the subject of very few trials. Certain specific pain complaints (e.g., low back pain [LBP]) have been extensively investigated, whereas other chronic pain conditions (e.g., complex regional pain syndrome [CRPS]) have only been studied in a handful of trials. In light of the inherent inconsistencies and vastness of the extant literature, we modified the aim of this article to a more conservative and manageable goal: to summarize the evidence for selected CAM modalities that have been applied to the management of a wide range of chronic pain complaints, highlight areas for future study, and provide general guidelines for clinicians. Thus, we reviewed and summarized the empirical evidence for each selected modality.
In addition to reviewing the efficacy data, we reviewed the mechanism of action for each selected modality, although this is not a major focus of the article. Similar to their counterparts in more traditional chronic pain interventions, very little is known about the actual mechanism of action for CAM modalities. Most of what we provide here is a summary of the purported or suspected mechanisms of action.
The selection of modalities for inclusion in this review was based on several factors: the modality had been the subject of at least one controlled study or several strong primary efficacy studies, was commonly known and publicly available, and was not already a common service in typical healthcare settings. Thus, prayer and spirituality, despite their popularity according to the CDC study [2], were excluded because of the lack of published efficacy studies on chronic pain. Transcutaneous electrical stimulation (TENS), cognitive-behavioral therapy (CBT), and relaxation therapy, despite being listed on the Web site of the National Center for Complementary and Alternative Medicine (NCCAM) (formerly the Office of Alternative Medicine [OAM]), were excluded since they are widely used and no longer considered CAM by practitioners.
Methodology
To synthesize the vast amount of data on the efficacy of CAM, we used combined methods to select studies for inclusion in this review. We searched computerized databases including MEDLINE, PsychINFO, CINAHL, and the Cochrane Library between 1966 and July 2006 using the search terms "pain" and the specific CAM modality of interest (e.g., "acupuncture"). To be as inclusive as possible, we did not use search terms that specified the type of pain complaint. Each article uncovered by this search strategy was manually checked to determine whether the study focused on a chronic pain condition. Articles that investigated acute pain (e.g., pain related to injury or medical procedures) or disease-related pain (e.g., cancer pain) were excluded. Only studies that included pain severity and/or functional disability as key outcomes were included. Only findings from controlled trials, including randomized controlled trials (RCTs), review articles, and meta-analyses (limited to human studies reported in English) were included. Because of the very large number of studies uncovered by this search strategy, we condensed and synthesized the literature using the following steps. For those CAM modalities and chronic pain conditions in which peer-reviewed systematic reviews (e.g., Cochrane reviews, meta-analyses) were identified, the findings were summarized and the authors' conclusions described. Primary trials that were excluded by these review authors because of methodo-logical or other limitations were not included. However, findings from relevant primary studies published since these reviews appeared were included. Only those CAM modalities and chronic pain conditions that were the subject of at least one controlled trial were included in this article.
Criteria for Evaluation of Efficacy
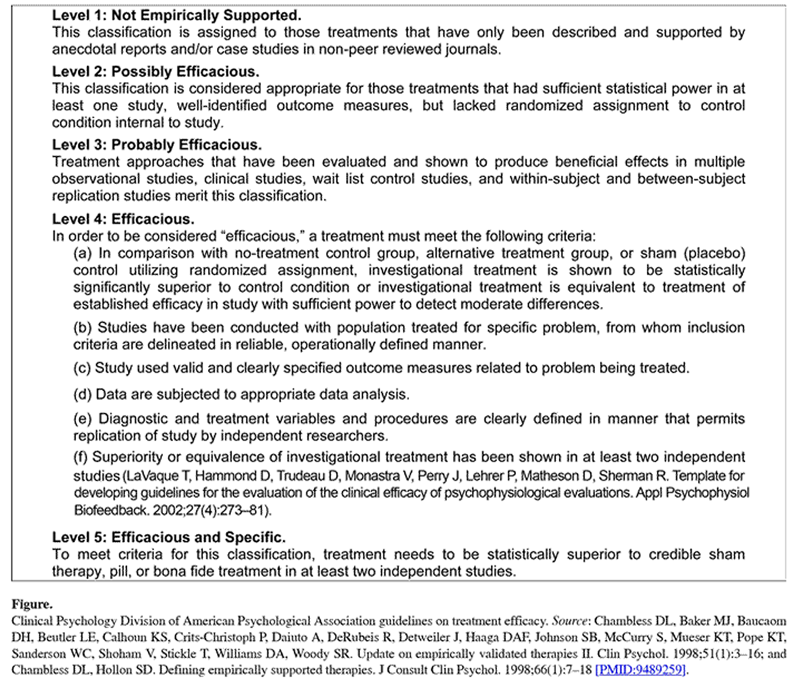
Figure 1 Based on the guidelines of the Clinical Psychology Division of the American Psychological Association (APA) (Figure), this review evaluates evidence for the efficacy of various CAM modalities for treatment of chronic pain [56]. One should note that most prior reviews in this area have focused on only one or two CAM modalities and have included only one type of chronic pain complaint. Since we aimed to cover a broad range of CAM modalities and chronic pain conditions, we did not incorporate specific criteria typically used for evaluation of the methodological quality of individual trials (e.g., Jadad scores). This decision was based on the fact that the various reviews and meta-analyses included in this article used different rating systems to evaluate the quality of the trials and we could not determine the best way to reconcile these different systems. Ratings for the efficacy of each reviewed CAM modality based on APA guidelines are depicted in the Figure.
Organization of This Article
The findings are presented according to the classification system developed by the OAM/NCCAM that grouped CAM therapies into four domains: biologically based medicine, energy medicine, manipulative and body-based medicine, and mind-body medicine. Home-opathy and acupuncture are discussed separately since they are recognized by NCCAM as "whole or professionalized CAM practices." For each modality, the findings of comprehensive reviews and/or meta-analyses are summarized first (where available) and followed by the results of primary trials published after these reviews appeared.
BIOLOGICALLY BASED MEDICINE
This section focuses on dietary supplements for treating chronic pain. As defined by NCCAM, dietary supplements include vitamins, minerals, herbal preparations, botanicals, amino acids, enzymes, and glandulars. A recently published systematic review evaluated three different herbal remedies for treating LBP: devil's claw, white willow bark, and topical cayenne [7]. Several trials in the review found devil's claw to be superior to placebo for short-term pain relief in patients with acute exacerbations of chronic LBP. A single trial found white willow bark superior to placebo for short-term pain relief. Evidence on the efficacy of cayenne was mixed. Long-term outcomes were not included in this review.
The 84 additional studies that we identified addressed chronic pain conditions including rheumatoid arthritis and osteoarthritis (OA) (50 studies), back pain (7 studies), neuropathic pain (4 studies), and various other conditions, such as prostatitis and sickle cell pain (23 studies). The most commonly tested supplement was combined glucosamine and chondroitin sulfate (22 studies). A recent large-scale trial investigating glucosamine and chondroitin sulfate suggested that the combination may be safe and effective for patients with moderate to severe knee OA pain [8]. Other commonly tested supplements included aromatherapy/aromatic oils (9 studies), fatty acids/fish oils (7 studies), and cannabis derivatives (4 studies).
The 84 trials ranged in length from 2 days to 3 years and included from 8 to 555 subjects. Sixty-three studies compared supplements with placebo, and the rest involved comparisons with an active treatment control. Of the 84 trials, 53 indicated that pain significantly improved with the dietary supplement compared with the control or comparison group. Twenty-four studies demonstrated no significant difference between treatment and control or favored active treatment, such as ibuprofen or rofecoxib, and seven studies had mixed results.
In summary, studies on the efficacy of dietary supplements varied extensively in the remedies tested and pain conditions treated. A recent systematic review found clinical trial evidence for the efficacy of devil's claw and white willow bark in acute exacerbations of chronic LBP but mixed results with the use of cayenne [7]. Most clinical trials (63%) showed a statistically significant effect on pain compared with placebo. However, many studies were limited by small sample sizes and short trial lengths. A recent large-scale trial suggested that combined glucosamine and chondroitin sulfate may be safe and effective for patients with moderate to severe knee OA pain [8]. Thus, the evidence tends to favor glucosamine and chondroitin sulfate for management of knee pain. Other biologically based therapies were not included because of the absence of primary studies and/or at least one controlled study.
ENERGY MEDICINE
According to NCCAM, the two types of energy therapies are bioelectromagnetic-based therapies that involve the unconventional use of electromagnetic fields, such as pulsed fields, magnetic fields, or alternating-current/direct-current fields, and biofield therapies that are intended to affect the energy fields that purportedly surround and penetrate the human body. NCCAM notes that the existence of biofields has not been scientifically proven. TENS has been excluded since it is widely used in hospitals and pain-care settings and is no longer considered CAM by most pain practitioners.
Pulsed Electromagnetic Fields
Pulsed electromagnetic field (PEMF) generators come in two major types. The relatively low-power devices are usually wearable, battery-powered, and designed for nearly continuous use throughout a patient's treatment. Relatively high-power devices, such as the Diapulse Model 103 (Diapulse Corporation of America, Great Neck, New York) that produces sufficient power to light a 40 W lightbulb placed within its field, are designed for use several times a day. All the studies using relatively high-power PEMF used a Diapulse Model 103 set to produce 975 W at 27.12 MHz in 65 ms bursts pulsing 600 times a second. The head of the device is set so that its cone-shaped field points at each inner thigh for a half hour each (1 hour total) once a day.
In reviewing the published research on the use of PEMF for headache, Vincent et al. concluded that combined small double-blind, placebo-controlled and open clinical trials showed that PEMF could significantly reduce chronic migraine headache activity by at least 80 percent. Subsequent follow-ups showed that the effects could be sustained for at least 16 months.1 Two reviewers discussed the use of PEMF for OA. Fini et al. reviewed the PEMF literature and found positive effects on cartilage cell and tissue cultures in in vitro and in vivo animal studies and cited three RCTs that found improvements in OA in clinical studies [9]. They concluded that PEMF can potentially modify the complex pathological processes that occur in tissue damaged by OA. Hulme et al. reviewed studies involving the use of PEMF in OA treatment [10]. They found small to moderate but significant results in knee OA patients and more limited but positive results in cervical spine OA patients. Hulme et al. concluded that PEMF may significantly improve knee OA pain but suggested that further studies be conducted.
Several randomized, placebo-controlled trials were conducted with low-power PEMF devices that were worn near the head for approximately 1 month [1112]. One study found symptom relief for 77 percent of participants in the treatment group, with 8 percent of controls reporting minor relief and 1 percent reporting moderate relief [11]. The study did not report any follow-up data. In another study, one-half of the subjects receiving the PEMF treatment reported at least a 25 percent decrease in days with headache, whereas one-quarter of the controls reported a similar reduction [12]. Again, no follow-up data were reported.
Four studies were identified that examined the effects of high-power PEMF on migraine headaches [1314]. The first demonstrated a nearly tenfold decrease in headache activity that was maintained from 6 to 18 months follow-up. The second study was a double-blind, placebo-controlled crossover study that failed when all but one participant who received PEMF first refused to cross over because his or her headaches had decreased dramatically. As in the first study, headache activity substantially decreased and this decrease was maintained at 3 months follow-up. The third study was a double-blind, placebo-controlled study in which PEMF reduced headaches substantially more than placebo. Finally, a fourth study demonstrated that patients could use the device in their homes with good clinical results.
In these studies, tension-headache patients showed little change in headache activity after exposure to the device and patients with mixed tension-migraine headaches only showed changes in the migraine component. Moreover, these studies showed a clear dose-response relationship: migraine patients exposed for only 2 weeks showed fewer decrements in headache activity than those exposed for 3 weeks, and migraine patients exposed to the device's half-power showed less effect than similar patients exposed for the same amount of time to the device's full power. None of the studies reported negative side effects. PEMF has now been in use for more than 3 decades and no negative side effects have been reported [15].
Four RCTs applied PEMF to the treatment of knee OA [1619], two to patients with cervical spine OA [18,20], and one to patients with temporomandibular joint (TMJ) disorder [21]. All RCTs were double-blind treatments that used sham PEMF in the control group. The first study that used PEMF to treat knee OA included 83 patients and found significant improvements in pain and stiffness in the patients under age 65 [16]. The second knee OA study applied PEMF to 36 patients and found reduced impairment in activities of daily living and improved knee function [17]. The third knee OA study applied PEMF to 86 patients and found significant improvements in pain and pain on motion [18]. The final knee OA study applied PEMF to 25 patients and found decreased pain and improved functional performance [19]. The authors concluded that the method warrants further investigation as a means of improving symptoms in patients with OA. Trock et al. also treated 81 patients with cervical spine OA but found somewhat lesser improvements among cervical spine versus knee OA patients [18]. In another study of cervical pain, Sutbeyaz et al. applied PEMF to 34 patients with cervical spine OA and found significant improvements in neck pain and disability among the experimental but not the sham-treatment control group [20]. Finally, one author applied PEMF to the treatment of 42 patients with TMJ disorder and found that PEMF had no specific treatment effects [21]. Despite the relatively small number of patients treated in these studies, this research suggests that PEMF is probably efficacious for treatment of knee OA and possibly efficacious for treatment of cervical spine OA.
In summary, although relatively few studies have examined the efficacy of PEMF, the research to date suggests that this treatment may be highly effective for patients with migraine, but not tension-type, headaches. However, given the paucity of controlled studies, the small number of participants, and the rarity of follow-up data, the overall efficacy of PEMF treatments for headache would still only be rated as probably efficacious based on the APA criteria for efficacy. PEMF is probably efficacious for treatment of knee OA and possibly efficacious for treatment of cervical spine OA. Moreover, the device is relatively inexpensive, appears to have no short-term side effects, and can be easily applied by patients or technicians.
Cranial Electrotherapy Stimulation
Cranial electrotherapy stimulation (CES) involves the delivery of a low-level electrical current via external skin-surface electrodes (usually placed on the ear[s]). The low-level current is ordinarily subthreshold for sensory detection and appears to engage electrical and neurochemical mechanisms that affect network electrophysiological activity of brain systems and mediate arousal, sensory processing, and thus, pain and pain modulation.
No systematic reviews of the use of CES with chronic pain were identified. However, several well-designed studies of CES treatment have been conducted with various patient populations. In a double-blind study, CES was compared to dental anesthesia, and while results varied, favorable outcomes were generally reported for CES versus sham CES [22]. Another study examined electroencephalogram (EEG) spectra and pain relief with a two-part double-blind approach that compared CES with sham control and other forms of central stimulation (i.e., Liss Stimulator) [23]. In this study, results also varied, yet the authors concluded that CES produced EEG spectral smoothing and pain relief that was superior to the sham control or comparison treatment. Naveau et al. used a randomized double-blind protocol to evaluate the capacity of CES to reduce the required analgesic dose of fentanyl in rectal cancer patients undergoing Nd:YAG laser treatment [24]. The authors reported that CES treatment enabled a 31 percent decrease in the dose of fentanyl required for pain relief.
A double-blind, placebo-controlled study of 60 patients with fibromyalgia indicated that CES, as compared with sham treatment or waiting-list control, reduced tender points by 28 percent and self-rated pain by 27 percent [25]. More recently, a double-blind control study comparing CES with sham treatment for 38 patients with pain associated with spinal cord injury concluded that CES effectively reduces pain and pain interference [26]. To summarize, several studies have found that CES effectively reduces pain. Although this work is somewhat incipient, CES shows considerable promise as both a complementary modality to other forms of therapeutic interventions and as a stand-alone approach to the treatment of particular types of pain. Consequently, CES would be rated as possibly efficacious for pain relief.
Therapeutic Touch/Healing Touch
Therapeutic touch (TT) or "healing touch" is derived from the ancient technique of laying on of hands. The goal is promotion or maintenance of the balance of vital energy fields in the body. It is based on the notion that the therapist's healing force affects the patient's recovery. Typically, the therapist passes his or her hands over the patient (without direct physical contact) to identify and correct energy imbalances. Several reviews of TT exist [27-30], but none focused specifically on its value for pain relief. In addition, many of the studies included in these reviews were uncontrolled and/or unpublished (e.g., abstracts, dissertations) or not peer reviewed (e.g., book chapters).
The results of one study [31] included in the Cochrane review on noninvasive treatments for headache pain [32] led the review authors to conclude that moderate evidence shows that TT is superior to placebo TT for reduction of tension-type headache pain within a few hours of a single treatment. Other published controlled trials have revealed greater reductions in pain for TT, relative to mock TT, for knee OA [33] and mixed chronic musculoskeletal problems [34]. However, negative findings have also been reported. One study found that progressive muscle relaxation (PMR) was more effective than TT for pain related to degenerative arthritis [35], another found that TT was not superior to education for fibromyalgia pain [36], and a third found that TT was not more beneficial than relaxation when both were delivered as adjuncts to CBT in 12 patients with mixed chronic pain [37]. In general, the quality of the positive studies was poor because of numerous methodological limitations (e.g., insufficient sample size). Taking into account the null findings just discussed, one can conclude that insufficient evidence exists for the use of TT for chronic pain, with the exception of tension-type headaches. Future studies should include larger sample sizes, and if mixed groups of patients are studied, care should be taken to ensure equivalence of clinical factors across groups.
Reiki
Reiki is a Japanese term that refers to "universal life energy." Reiki is based on the notion that when spiritual energy is channeled through a Reiki practitioner, the patient's spirit is healed, which in turn heals the patient's physical body. The main distinction between Reiki and TT is that Reiki therapists have physical contact with the body. We located three studies on the application of Reiki for pain, although only one study included a control group. The uncontrolled studies found improvements in mixed chronic pain symptoms [38] and pain related to human immunodeficiency virus [39]. In the only controlled trial, Reiki showed modest evidence for short-term reduction of cancer pain [40]. To summarize, little evidence from controlled trials currently supports the use of Reiki for pain.
Qigong/Qi Therapy
The Chinese term qi means "vital energy," and the term gong means "training." Thus, qigong is a component of traditional Chinese medicine (TCM) that combines movement, meditation, and regulation of breathing for enhanced flow of qi in the body. The improved flow of qi is thought to lead to health benefits including pain reduction. Four studies were located that examined the effects of qigong or qi therapy on pain. In the first study, patients with CRPS type I showed short-term benefits from training with a qigong master compared with a sham master but these gains were attenuated by the 6 to 10week follow-ups [41]. The other three studies on qi therapy were conducted by the same research group on elderly participants (60 years or older) with mixed chronic pain symptoms. In these studies, the qi therapy involved a practitioner adjusting the patients' qi; patients did not engage in exercises or movement. In two of these studies [4243], patients who received qi therapy reported less pain than usual-care controls. The third study found that patients who received qi therapy reported less pain, anxiety, depression, and fatigue and exhibited lower blood pressure compared with those who received sham qi therapy [44]. Overall, qi therapy could be rated as possibly to probably efficacious for treatment of chronic pain.
MANIPULATIVE AND BODY-BASED MEDICINE
As defined by NCCAM, manipulative and body-based medicine includes chiropractic and massage therapy, which are subsequently reviewed. Chiropractic manipulation and various forms of massage therapies are included since they are modalities commonly known to the public and available to patients.
Chiropractic Manipulation
Spinal manipulation therapy (SMT), practiced primarily by chiropractors, is the most popular CAM therapy for LBP [45]. SMT has been licensed in all 50 states since 1974 and is covered by most insurance plans. However, conflicting results of studies evaluating the efficacy of SMT have led to confusion about whether SMT is superior to standard therapy.
A recent systematic Cochrane review of SMT for LBP found that SMT had clinically and statistically significant benefits when compared with either sham manipu-lation or various LBP therapies previously determined to be ineffective or harmful (e.g., traction, bed rest, home care, topical gel, or no treatment) [46]. When compared with other recommended treatments for LBP, including analgesics, physical therapy, exercises, or back school, SMT did not show any statistically significant benefits. Another recent review also found that SMT had statistically significant benefits only when compared with sham or ineffective therapies [47]. No evidence was found that SMT was any more or less effective than conventional therapies for acute or chronic LBP.
A total of 47 studies met our search criteria. The majority (25 studies) evaluated SMT for subacute or chronic LBP. Cervical spine pain was also commonly studied (13 studies). Nine articles reported on SMT for various pain conditions, including fibromyalgia, carpal tunnel syndrome, migraine and tension-type headaches, coccydynia, dysmenorrhea, shoulder dysfunction, and total abdominal hysterectomy. Of the 47 studies, 20 tested SMT combined with other modalities such as heat, exercise, or medication. Control or comparison groups varied across studies. Placebo-controlled or sham SMT was compared in one-third of studies (15 studies). Thirteen studies involved exercise or stabilization, nine involved usual care as prescribed by a primary or specialty care physician, and ten included medication or electrical stimulation. Overall, 18 studies demonstrated a beneficial effect of SMT over the comparison group for pain or pain-related disability. In studies comparing SMT with placebo or sham, five showed statistically significant improvement in pain or disability as a result of SMT. The results demonstrated the benefit of SMT over exercise or stabilization, usual care, and medication or electrical stimulation in 23, 44, and 60 percent of studies, respectively.
In summary, evidence from two recent systematic reviews indicates that SMT is more effective than sham manipulation and treatments such as bed rest and traction but no more effective than other recommended LBP treatments. Consequently SMT should be considered probably efficacious for treating LBP. Multiple studies have shown that SMT may reduce pain severity and disability in chronic pain conditions other than LBP but should be viewed cautiously at this time. Future studies of SMT for pain conditions should adhere to rigorous methodological guidelines and identify which patients are most likely to benefit from this pain-management approach.
Massage Therapy
Massage therapy is defined as soft-tissue manipulation by trained therapists for therapeutic purposes [48]. Massage therapy may take different forms, including Swedish, reflexology, Shiatsu, Rolfing, and craniosacral. Massage is typically used as adjunct therapy that prepares the patient for exercise or other interventions rather than as the main treatment [49].
Our search identified 21 studies on the application of massage for LBP (8 studies), headache pain (2 studies), neck pain (1 study), shoulder pain (3 studies), fibromyalgia (4 studies), and mixed chronic pain (3 studies). In their comprehensive review, the Cochrane Collaboration recently reported that massage was (1) superior to relaxa-tion [50], acupuncture [45], and self-care education [45] for LBP; (2) equal to corsets [5152] and exercises [53]; and (3) inferior to SMT [5152, 5455] and TENS [56]. One should note, however, that in some cases, such as acupuncture, these conclusions are based on only one RCT. The Cochrane Collaboration also reviewed noninvasive physical treatments for chronic/recurrent headache [32] but only one trial (reported in two studies [5758]) examined massage. This trial found SMT to be superior to massage for cervicogenic headache [5758], whereas another trial not included in the Cochrane review found greater pain reduction for massage relative to acupuncture in patients with migraine but not tension-type or combined headaches [59]. Thus, the findings for headaches are mixed.
The single study on neck pain found that by 3month follow-up, pain reduction did not differ between acupuncture and massage [60]. All three studies on shoulder pain reported significant improvements in pain compared with the no-treatment control [6163]. For fibromyalgia, two studies conducted by the same group found massage to be superior to TENS [64] and PMR [65]. The two other fibromyalgia studies revealed greater pain reduction for massage versus no treatment by 6month follow-up [66] and no benefits for massage compared with usual care (i.e., standard care provided by physicians including medications) [67]. For mixed chronic pain, one study found that massage led to less pain than usual care [68] but the other two studies reported no benefits of massage over relaxation (at 3month follow-up) [69] or mediation and usual care (at 1month follow-up) [70].
To summarize, massage therapy is useful for pain relief in numerous chronic pain conditions, particularly LBP and shoulder pain. The authors of a Cochrane review concluded that massage therapy may benefit patients with subacute and chronic nonspecific LBP, particularly when combined with exercise and education [49]. Less support exists for the use of massage therapy for patients with headache pain, neck pain, or fibromyalgia, although one study found that massage may be superior to acupuncture for migraine but not tension-type headaches. On this basis, massage therapy is rated as efficacious for LBP, probably efficacious for shoulder pain, and possibly efficacious for fibromyalgia and neck pain.
Craniosacral Therapy
Proponents of craniosacral therapy maintain that movement restrictions in the cranial structures of the skull adversely affect impact rhythmic impulses conveyed through the cerebral spinal fluid from the cranium to the sacrum [71]. Thus, craniosacral therapy is a form of massage that uses gentle pressure on the plates of the patient's skull. Few controlled studies have been conducted on craniosacral therapy, and a recent review concluded that evidence to support its use is insufficient [71]. However, none of the studies in this review included pain as an outcome measure. Only one study relevant to the current review was located. This study examined the CV4 craniosacral technique for tension-type headaches [72]. The CV4 technique moves with the narrowing and widening of the skull, or the cranial rhythm; the basis of the technique is compression of the fourth ventricle [72]. For additional details regarding the CV4 technique, see the book by Upledger and Vredevoogd [73]. Patients who received CV4 reported less pain intensity and negative affect than the controls. The authors of a recent review of manual therapies for tension-type headaches concluded that moderate evidence indicates that the CV4 technique exerts a beneficial effect on pain related to tension-type headaches [74]. Nevertheless, additional large-scale trials that include follow-up assessments are warranted before recommendations regarding application of the CV4 technique to pain relief can be made.
MIND-BODY MEDICINE
Mind-body therapies (MBTs) cover a wide array of modalities and procedures. Relaxation is a common element of many MBTs and will not be covered as a separate modality in this review. CBTs are now widely accepted in pain management and therefore also will not be covered.
Meditation
Meditation has its roots in spiritual practice [7577]. Meditation can be defined as intentional self-regulation of attention to promote a specific mental focus and awareness of internal or external experiences [78]. The two general types of meditation are concentrative and mindfulness [79]. Concentrative meditation uses a specific focus as the object of attention, such as a visual image, the counting of breaths, or the repetition of a specific word or phrase. Mindfulness meditation does not limit attention to a particular object but involves increased attention and awareness to the fullness of the current experience and present reality [80]. In chronic pain, mindfulness meditation is used for promoting detached observation of the pain and awareness of the moment-to-moment primary sensations as separate events with accompanying thoughts about pain [81]. A model of Mindfulness-Based Stress Reduction (MBSR) was introduced for pain management more than 20 years ago [82]. A systematic review of MBT for pain management [83] concluded that MBSR is a promising intervention for chronic LBP and heterogeneous pain [8182, 84]. A recent meta-analysis of MBSR included five studies of physical conditions, including two studies of fibromyalgia and one of general chronic pain [85]. The meta-analysis estimated a mean effect size of 0.53 (95% confidence interval 0.230.81), indicating moderate effects of MBSR.
Our search also discovered five additional RCTs that examined the effects of meditation on LBP (two studies), fibromyalgia (one study), mixed musculoskeletal pain (one study), and irritable bowel syndrome (IBS) (one study). One LBP study found significant improvements among patients who engaged in meditation compared with no improvements in a standard-care group [86]. Because of attrition rates of 44 and 17 percent in the meditation and control groups, respectively, power for between-group comparisons was inadequate. The other study on LBP showed no significant differences in pain reduction between patients who received breath therapy (i.e., integrated approach of body awareness, breathing, meditation, and movement) compared with physical therapy [87]. The single study on fibromyalgia compared MBSR and qigong with an education control group [78,88]. Nearly 50 percent of patients from both groups dropped out and no group differences in pain were found at any assessment point. For mixed musculoskeletal pain, MBSR was compared with massage and standard care [70]; by 1month follow-up, the groups did not differ in pain intensity or pain unpleasantness. The single study on IBS found significant improvements in general gastrointestinal symptoms [89] but no differences in pain symptoms in patients assigned to concentrative meditation versus wait-list control [90].
In summary, existing evidence is not strong enough to support routine use of meditation for pain management but supports its probable efficacy for patients interested in it as an adjunct to other care. Meditation is thus similar to other MBTs, and outcomes are likely to be improved by assessment of patient variables such as expectations and readiness to change [91]. The current studies used mainly female samples and may not generalize to males. A study of concentrative meditation conducted at the San Diego Department of Veterans Affairs Medical Center with a predominately male group demonstrated improvement on stress, anxiety, quality of life, and spiritual well-being measures [92]. With the exception of breath therapy, which used touch in the intervention, none of the studies reviewed indicated adverse reactions to meditation training. However, clinicians should be aware of the potential for some increased anxiety, which has been shown in relaxation studies [93].
Hypnosis
Hypnosis ". . . typically involves an introduction to the procedure during which the subject is told that suggestions for imaginative experiences will be presented" and that following this introduction ". . . one person (the subject) is guided by another (the hypnotist) to respond to suggestions for changes in subjective experience, alterations in perception, sensation, emotion, thought, or behavior" [94]. Hypnosis for pain management usually begins with an induction (e.g., suggestions for focused attention or relaxation) and is followed by suggestions for altering how pain is viewed or experienced. Posthypnotic suggestions are often included and usually involve suggestions about experiences outside a session (e.g., suggestions that pain relief experienced during sessions will last and/or become permanent). Hypnotic treatment for chronic pain typically lasts 4 to 10 sessions; virtually all clinicians encourage patients to practice self-hypnosis for chronic pain outside of treatment sessions [95].
Three recent reviews cover the bulk of published RCTs of hypnotic analgesia [9596]. In the first study, the authors performed a meta-analysis of 18 studies of laboratory and clinical pain [96]. The average effect size across studies was 0.67, which lies squarely between a medium (0.50) and large (0.80) effect. This effect size can be interpreted as indicating that the average person treated with hypnosis obtains a greater analgesic response than 75 percent of individuals who are given standard care or no treatment. Patterson and Jensen identified 12 RCTs of hypnotic treatment of chronic pain [95]. In the studies comparing hypnosis with no treatment, standard care, or attention, hypnosis usually resulted in significantly greater reductions in pain than the other treatments. However, when hypnosis was compared with treatments that share many of its characteristics (e.g., PMR), hypnosis was usually not found to be superior to the competing treatments. But, in no case was hypnosis for chronic pain found to be less effective than other treatments, which led the authors to conclude that hypnosis is a viable intervention for chronic pain.
Most recently, Jensen and Patterson identified 19 studies that examined the efficacy of hypnotic analgesia for headache pain (8 studies), mixed chronic pain (3 studies), LBP (2 studies), TMJ pain (2 studies), and cancer-related pain, sickle cell disease pain, fibromyalgia, OA pain, and disability-related pain (1 study each) [90]. As previously found in a review of a subset of these studies, hypnotic treatment produced greater pain reductions relative to standard care and no treatment but had similar effects as PMR and autogenic training [95]. The authors also reported that hypnosis was more effective than medication management (for headache), physical therapy (for fibromyalgia), and education (for TMJ pain). They concluded that ". . . hypnotic treatment for chronic pain results in significant reductions in perceived pain that maintain for at least several months, and possibly longer" [90].
Clinically, hypnosis and hypnotic analgesia has been greatly underutilized. Hypnosis is almost always a benign treatment with very little likelihood of negative side effects. In fact, the "side effects" that occur appear to be overwhelmingly positive and include a greater sense of control over pain, as well as increased overall well-being and decreased tension, stress, and anxiety [97]. To provide this treatment, clinicians need to obtain appropriate training in hypnosis and apply this training to reduce their patients' pain and suffering. Consequently, hypnosis is rated as efficacious for treating chronic pain.
Yoga
Yoga is a Sanskrit term for a group of spiritual practices thought to have originated in India more than 7,000 years ago. Raja Yoga, also known as Astanga Yoga, is the most familiar Western form of yoga. Raja Yoga is described in a codification of yoga philosophy comprising 196 aphorisms, the Yoga Sutras, which were composed by Pantanjali approximately 2,000 years ago. It includes eight stages or limbs: yama (ethical principles), niyama (self-restraint), asana (postures), pranayama (breath control), pratyahara (withdrawal of the senses), dharana (concentration), dyhana (meditation), and samadhi (liberation). The Hathayoga Pradipika is another primary source for yoga practitioners. It was written in the 15th century by Svatmarama and teaches postures and breathing techniques [98]. The term Hatha Yoga is generally used for the postures and breathing techniques used by yoga practitioners.
Our search identified six RCTs on yoga for chronic pain: LBP (four studies) [99102], carpal tunnel syndrome (one study) [103], and hand OA (one study) [104]. One LBP study was discarded because it only provided baseline data and no outcomes [102]. The three remaining LBP studies suggested a positive benefit of yoga. The first study found that patients who practiced yoga demonstrated significantly decreased pain and improvements in functional disability compared with an education control group [99]. The effect sizes for functional disability and pain intensity for the yoga group were 2.60 (strong effect) and 0.50 (moderate effect), respectively. The second study reported that yoga, compared with exercise and self-help, yielded significant improvement in functional disability but not symptom "bothersomeness" (including pain) at 12 weeks. Yoga remained superior to self-care but not to exercise at 26 weeks [99]. The third study had inadequate power to detect differences between yoga versus wait-list control but reported trends in favor of the yoga intervention [101]. The single study on carpal tunnel syndrome found that yoga participants demonstrated statistically significant differences in grip strength, pain intensity, and Phalen's sign compared with the control group [103]. Another study reported that patients with hand OA showed statistically significant improvements in pain, joint tenderness, and finger range of motion following yoga [104]. No-treatment controls did not demonstrate significant changes from baseline, although between-group differences were not analyzed.
In summary, the limited studies suggest the potential benefit of yoga therapy and indicate that it is probably efficacious for some cases of LBP and carpal tunnel syndrome, but not enough evidence exists to routinely recommend this intervention. The overall sample demographics of the reviewed studies may not match the usual chronic-pain population. The self-referral sample selection likely resulted in a generally healthier and less disabled sample with less unemployment, more education, and relatively lower pain-intensity scores. Further research with a broader, more representative sample is recommended for efficacy determination and appropriate patient selection.
Biofeedback
Biofeedback is the process of providing real-time information from psychophysiological recordings about the levels at which physiological systems are functioning. Electronic biofeedback devices objectively and noninvasively record tiny changes in physiological functions that cannot be readily detected by other means. Most record from the skin surface. The information recorded by surface sensors is sent to a computer for processing and then displayed on the monitor and/or through speakers. The patient and therapist attend to the display of information and incorporate it into the processes they are attempting to modify. The physiological parameters most often recorded for biofeedback include muscle tension (the surface electromyogram [sEMG]), near-surface blood flow (done by recording skin temperature), heart rate, sweating or galvanic skin response, brain waves (EEG), and respiration.
The available literature on biofeedback for pain control is so extensive that a comprehensive discussion of the efficacy studies is beyond the scope of this review [105106].2 Thus, only the findings for selected pain conditions are briefly discussed. Numerous studies have demonstrated the efficacy of psychophysiological interventions, including biofeedback, for migraine and tension-type headaches [107109]. Rains et al. reviewed the meta-analyses and found that biofeedback is highly efficacious for these conditions [110]. Comparative studies have shown that biofeedback is at least as or more effective than standard interventions [111].
Regarding muscle-related orofacial pain, a comprehensive review concluded that biofeedback treatment is effective when the pain is muscle-related rather than originating in the TMJ [112]. Several studies have shown that biofeedback was as or more effective than splint therapy and that the gains were maintained for longer periods [113114]. A recent review of 12 RCTs concluded that sEMG training with adjunctive CBT is an efficacious treatment for TMJ disorders and that sEMG training as the sole intervention and biofeedback-assisted relaxation training are probably efficacious treatments [115]. For musculoskeletal back pain, reviews indicate that mixed behavioral interventions including biofeedback can be very successful for chronic LBP [116119]. Reviews of studies on the efficacy of biofeedback for LBP generally concluded that biofeedback helps some patients with muscle-related back pain, with an overall improvement rate of about 65 percent versus 33 percent for placebo and no improvement for no-treatment controls [120].
Additional studies have investigated phantom limb pain and two types have been found to be amenable to biofeedback: burning and cramping pain. Studies have shown that nearly all people with amputations who have cramping pain are helped by sEMG [121]. Unfortunately, about half of the patients with burning pain have not benefited from biofeedback [121]. Many authors do not differentiate between types of phantom limb pain when applying biofeedback but still achieve success [122123]. Regarding fibromyalgia, a series of studies have confirmed that a psychophysiological intervention combining sEMG biofeedback and EEG-driven stimulation effectively treats fibromyalgia [124126]. These investigators identified diffuse muscular coactivation as a potential source of pain in fibromyalgia and successfully used sEMG biofeedback to reduce the pain in these tender points [124125].
Biofeedback for pain generally works because it first identifies the patient's individual physiological dysfunctions causing the pain and helps the patient recognize when those dysfunctions are occurring and correct them by watching the display and trying various corrective strategies. For example, most people with chronic muscle-related pain have more difficulty judging the tension in the muscles in the painful area than people without pain [127]. Thus, they tend to keep the muscles too tense for too long and then pain develops. Biofeedback calibrates the sensations coming from the muscles with actual levels of tension.
Side effects of biofeedback therapy for pain are rarely an issue. However, other behavioral therapies commonly used conjointly with biofeedback, such as PMR training, have potentially serious side effects. Side effects may occur when biofeedback is used for treating conditions other than pain. For example, PMR may precipitate panic attacks or hyperventilation when respiratory alterations are induced in some individuals with significant anxiety or asthma and may trigger cardiac events when used with individuals with underlying cardiac problems. One should note that many clinicians who use biofeedback incorporate behavioral techniques such as breathing or relaxation training into their clinical protocols and thus increase the likelihood of side effects.
To conclude, biofeedback is a nonpharmacological intervention that can directly or indirectly help patients cope with their pain. The direct approach, which teaches patients to correct the physiological problem causing their pain, is efficacious for several pain problems. The indirect approach helps patients modulate their pain experience and how pain affects their functioning. Biofeedback used for pain treatment has relatively few known side effects when compared with traditional pain interventions such as medication; it can be the sole pain treatment or an adjunctive treatment combined with other interventions. Sufficient meta-analyses, detailed reviews, assessments by U.S. government-sponsored panels, and high-quality studies with long follow-ups of significant numbers of patients have demonstrated that biofeedback can be efficacious for assessing and treating a variety of disorders characterized by pain.
WHOLE OR PROFESSIONALIZED COMPLEMENTARY AND
ALTERNATIVE MEDICINE PRACTICES
Two systems of whole or professionalized practices will be discussed: homeopathic medicine and acupuncture. These two have been selected because of their popularity and common acceptance by the U.S. public.
Homeopathy
Homeopathy is a form of alternative medicine based on the principle of "like cures like." This principle postulates that administering a small amount of a substance that causes illness in a healthy person can also treat the same illness in a sick person. While homeopathy has been used frequently to treat chronic pain, it has seen high levels of controversy and debate because its treatment concepts seem contradictory to the laws of science. Furthermore, controlled trials of homeopathic remedies for painful conditions have produced contradictory results.
In the absence of extant reviews, five studies were found that used homeopathic remedies to treat chronic pain conditions (headaches, arthritis, and back pain) [128132]. The homeopathic remedies tested were "spiroflor" or homeopathic gel, "rheus-tox," or an individualized menu of homeopathic medicines. Three studies compared a homeopathic remedy with a placebo and two compared homeopathy with active treatments (e.g., anti-inflammatory medication or pain-relieving gel). Studies were relatively short, ranging in length from 1 week to 6 months. While three studies demonstrated greater mean pain reduction from the homeopathic remedy compared with the comparison groups, only one reached statistical significance.
To conclude, relatively few RCTs have investigated homeopathic remedies for pain management. Furthermore, these studies are relatively small (i.e., underpowered to show effect), of short duration, and have methodological shortcomings. Most studies found no significant improvement in pain. Thus, evidence for homeopathic remedies in pain conditions is lacking. Future efforts should focus on larger studies of standardized treatments with more rigorous methodology.
Acupuncture
Acupuncture involves penetration of the skin by thin, solid, metallic needles that are stimulated either manually or electrically. It is one of several TCM therapies that have been used for thousands of years in the treatment of a variety of health problems. Today, acupuncture therapy is commonly used for pain control throughout the world, although the putative mechanisms are complex and unclear. Practitioners apply many different models and approaches in acupuncture practice, ranging from the metaphysical paradigm used by traditionally trained practitioners to the strictly neurophysiologic approach more commonly used by physicians treating patients exclusively for pain.
TCM is a complete system of healthcare delivery. Therefore, a discussion of the efficacy of acupuncture must be prefaced with an understanding of the problems that occur when researchers attempt to evaluate treatments from one diagnostic paradigm (i.e., TCM) to diagnoses made with a different paradigm (i.e., allopathic medicine). Many studies have evaluated the use of acupuncture for symptoms that are either side effects of biomedical treatment (e.g., pain, fatigue) or related to a specific disease process (e.g., OA). TCM syndromes, however, are not equivalent to either of these side effect types as defined by a biomedical model. One must therefore use caution when interpreting results from studies that apply a TCM treatment to anything other than a TCM-related diagnosis or syndrome.
TCM syndromes, such as yin/yang deficiencies or qi stagnation, are unique symptom complexes that result from imbalances between the body's various functional systems. Since TCM is based on functional relationships and TCM diagnoses involve syndromes not diseases, no one-to-one correlation of signs and symptoms between TCM diagnoses and biomedical diseases exists. The diagnostic symptom complexes used in TCM differ from an allopathic model, and treatment is given according to individual patterns of system imbalances. As a result, certain aspects of human physiological functional relationships are emphasized that are not directly addressed by a biomedical paradigm. Results from RCTs of acupuncture will continue to be equivocal and show little more than a comparison of "apples to oranges" until studies are designed that recognize and include evaluation of the underlying TCM syndrome.
Since the 1970s, hundreds of clinical trials evaluating the efficacy of acupuncture for various conditions have been conducted. Many, however, were poorly designed and few included treatment protocols as applied in actual clinical practice. Nevertheless, in some areas related to pain management, reviews provide sufficient evidence of efficacy to draw clear conclusions. For example, acupuncture is generally agreed to effectively treat postoperative dental pain, as well as postoperative and chemotherapy-related nausea and vomiting [133]. More recently, substantial evidence indicates that acupuncture is also effective in treating chronic LBP [134135] and support for the efficacy of acupuncture for premenstrual syndrome has been published in China [136]. One reviewer found that results from studies on efficacy are considered (1) positive by some and difficult to interpret by others for the treatment of migraine and TMJ disorders; (2) promising for fibromyalgia, knee OA, and tennis elbow, although additional research is needed; and (3) inconclusive or difficult to interpret for neck pain [137].
To summarize, acupuncture has traditionally been used as adjunctive therapy for a variety of conditions. Although hard data from modern research methods are sparse regarding the synergistic effects of acupuncture combined with other therapies, a great deal of literature has evaluated its safety [138141] and efficacy for certain conditions. For patients at risk for adverse reactions to pharmaceutical therapy or for any patient who prefers acupuncture over drugs, acupuncture should be used as an adjunct in pain management. Its relatively low cost, low risk for serious adverse events, and ease of application make it particularly suitable in patients for whom standard treatment methods have failed. More specific recommendations for integrating acupuncture into clinical care will become available as our understanding of its putative mechanisms evolves. In the meantime, acupuncture can be considered probably efficacious for treating LBP and possibly efficacious for treating premenstrual syndrome.
CONCLUSIONS ON EFFICACY OF COMPLEMENTARY AND
ALTERNATIVE MEDICINE MODALITIES FOR
CHRONIC PAIN MANAGEMENT

Table 1

Table 2A

Table 2B This review has evaluated existing evidence for the efficacy of various CAM modalities for treatment of chronic pain based on the APA guidelines (Figure) [5]. A summary of the evidence for the efficacy of each selected CAM modality is provided in Table 1, while ratings for the efficacy of each CAM modality are provided in Table 2.
Evidentiary data must be used to (1) guide clinicians' consideration of the risk and burden-to-benefit ratios of particular CAM therapies, (2) afford knowledge that can be provided to patients for genuine informed consent to treatment, and (3) facilitate potential CAM integration into the mainstream model of healthcare [142]. Yet several challenges to the study of CAM therapies exist, such that the basic question is not simply which CAM interventions should be studied but rather how they should be studied. Therefore, Giordano et al. recently proposed the use of hierarchical research approaches that use mixed methods (i.e., quantitative as well as qualitative techniques) together with forms of RCT, adapted to best meet the contextual factors inherent to the use and "real-world" application(s) of various CAM therapies [143].
Several methodological limitations were found in the trials we reviewed. Among the most serious of these were (1) small sample sizes, (2) lack of follow-up data, (3) inadequate blinding of assessors, (4) paucity of trials that included comparison conditions that controlled for nonspecific effects (e.g., therapist time/attention, physical contact), (5) lack of replication studies in independent research groups, and (6) for certain nonpharmacological approaches (e.g., massage, TT), little information on the extent to which procedures were standardized. Future trials should remedy these limitations and provide a more rigorous evidence base for the use of CAM in pain management.
RECOMMENDATIONS TO PRACTITIONERS
Available evidence indicates that the public has been using CAM modalities for many years and will likely continue to do so with or without the blessing of pain or other clinical practitioners. Therefore, pain practitioners must become more familiar with the efficacy of CAM modalities and consider incorporating those CAM treatments with evidence supporting their efficacy into daily practice whenever indicated and/or appropriate.
This review indicates that CAM modalities, as a group, have a mixed efficacy track record, with some approaches having more evidence to support their efficacy than others (Table 1). For example, although not everyone responds to these treatments and the immediate efficacy of the treatments is not always maintained, support for the efficacy of hypnosis, biofeedback, and massage therapies for LBP and shoulder pain is greater than that for numerous control conditions and, in some cases, other treatments. The efficacy of PEMF has been demonstrated for migraine headaches and OA of the knee and cervical spine but no other pain condition. CES, massage therapies for neck and other pain conditions, SMT, meditation, and yoga appear to be promising treatments, but more research is needed to replicate preliminary findings. The CAM treatments that showed mixed results include herbal and dietary interventions (perhaps because these represent hundreds of interventions, so mixed results are expected), TT, craniosacral therapy, Reiki, qigong, and homeopathy. However, even these interventions might help a subgroup of patients.
Acupuncture appears to belong in its own category. While multiple meta-analyses and clinical trials support the efficacy of acupuncture as an analgesia and treatment for many medical conditions, relatively few studies have focused on chronic pain conditions. As discussed in the acupuncture section, the lack of studies on chronic pain may be partially due to acupuncture being originally an integral part of TCM, which conceptualizes health and illness from a very different paradigm. In short, the efficacy of acupuncture as analgesia is not disputed, but studies of its efficacy in treating chronic-pain diagnoses as defined by Western nomenclature have mixed results.
In addition to efficacy, other issues are relevant to practitioners making decisions about using or incorporating CAM modalities into their pain practice. These issues include additional time and energy investments, the need for specially trained personnel to administer the modalities, known or potential side effects, safety in combining CAM and other modalities, likely acceptance by clients and the public (and hence the issue of long-term adherence), and ease of incorporation into traditional pain-management practices.
Additional Requirements
Biofeedback requires equipment and specialized training. Many treatments, including acupuncture, homeopathy, massage, and chiropractic care, require a licensed practitioner. Also, some CAM modalities may produce concrete results in just a few sessions for some patients (e.g., CES, hypnosis, biofeedback), while others may require more time and effort (e.g., yoga, meditation). In general, CAM modalities as a group take longer than traditional medical pain interventions to achieve results.
Side and Toxic Effects
Another important issue is that, compared with traditional pain interventions, CAM modalities as a group have fewer known, documented side and toxic effects. For example, the "side effects" of training in self-hypnosis for chronic pain are overwhelmingly positive [97]. This fact may explain, at least in part, the popularity of CAM modalities relative to traditional medical interventions, which tend to be invasive and undermine patient self-efficacy and control.
Combining Complementary and Alternative Medicine and Other Modalities
Another issue that clinicians should consider is that some CAM modalities can be combined safely with each other and with traditional pain interventions to produce additive or synergistic effects. For example, CES can be administered easily with self-hypnosis or biofeedback training or with psychotherapy. In this way, any potential benefits of the individual treatments can combine for maximum pain relief for the patient.
Interest in combined traditional medical treatments for maximum pain relief is increasing, but no reason exists that more established CAM modalities should not at least be considered during development of multimodal treatment plans [137]. Additional research must examine the use of individual CAM therapies with other CAM approaches and with traditional interventions in terms of safety and synergistic effects. Recently, some concerns have arisen regarding the combined use of medication and herbal preparations [144145]. Some herbal preparations should be avoided completely because of their very rapid, irreversible actions [144145].
Acceptance, Adherence, and Ease of Incorporation
The popularity of CAM therapies for chronic pain has been partially fueled by the current lack of efficacious treatments for chronic pain. However, after the initial desperation for relief and the curiosity and novelty of new treatments have worn off, long-term compliance may emerge as a potential road block to successful positive outcome. Little data indicate which CAM therapies would more likely incur acceptance and compliance and which would not. In the absence of empirical data, one might assume that those CAM modalities that resonate with current ideas of medical treatments would be more readily accepted. Thus, herbal and dietary supplements may have an advantage in adherence since the public has become acculturated to the idea of taking medications to get and stay well. Treatments that use sophisticated equipment, such as biofeedback, CES, PEMF, and acupuncture (perhaps only the electrical stimulation activity, not as part of TCM) may also have an advantage. The idea of "massaging" away tension and pain and the use of chiropractic manipulations for reducing pain are ingrained in the human psyche. Hypnosis for "mind control" might be more effective for people who believe that the brain modulates pain. Yoga, meditation, healing touch, and qigong may have foreign connotations and would more likely appeal only to a subsample of the general public. Ease of incorporation into pain practices is likely influenced by the level of acceptance of and subsequent compliance with the CAM modalities.
Other Advantages of Complementary and Alternative Medicine Use
The use of CAM may lead to greater acceptance of traditional interventions. A case in point is the use of CES for increased acceptance of psychological interventions such as CBT. Tan et al. showed that the use of CES could lead veterans to engage in psychological therapy or MBT because they perceived CES to be a "real" physical treatment that could rapidly reduce pain and credibly treat "real" pain [146]. Once engaged, the veterans became more amenable to participating and benefiting from other MBTs or psychological therapies.
Overall, this review indicates that some CAM modalities provide significant relief for individuals with chronic pain and that, for some individuals, this relief is maintained over time. While more research is needed to specify the mechanisms of different CAM treatments, enough evidence supports offering at least a subset (in particular, biofeedback and self-hypnosis training) to patients who express interest. As more is learned about the efficacy of CAM approaches and as those approaches with established efficacy are provided more consistently to individuals with chronic pain, we can anticipate greater reductions in the disability and suffering associated with chronic pain conditions.
MECHANISM OF ACTION
Giordano's recent review of pain modulatory mechanisms described the involvement of several systems, including, but not limited to, intraspinal-segmental pain modulation, bulbospinal pain modulation, centrifugal pain modulation involving midbrain and descending inhibitory controls, opioid and nonopioid hypothalamic-pituitary analgesia, and corticolimbic inhibitory processing [147]. Literature supports the concept that particular CAM therapies may engage one or more of these systems to evoke analgesia. Clearly, a detailed discussion of the putative mechanisms subserving each CAM approach addressed is beyond the scope of this article. As well, we must note that each system represents part of a hierarchy of neural pathways that function as nonlinear, parallel, and serial processing networks. Thus, one must understand that pain modulation may involve both temporal and anatomical reorientation/redirection of these networks, rather than simply a change in activity at a single neuro-anatomical site or within a unitary tract or pathway [148]. A brief summary follows of the known or purported mechanism of action for the CAM modalities covered in this review. Similar to traditional therapies, the actual mechanisms responsible for the pain-modulating effects are putative and ongoing methodologically progressive but no less rigorous research is required for a fuller definition of which anatomical pathways and chemical systems are involved and how these substrates actually change the mental state (i.e., sensation, perception, and/or cognition) of pain [143,149150].
Biologically Based Medicine: Supplements
Glucosamine and chondroitin sulfate are the most widely used dietary supplements for pain secondary to OA. The supplements' mechanisms of action in relieving arthritic pain and repairing cartilage are still speculative [151]. Setnikar and Rovati demonstrated that after oral administration, glucosamine sulfate is bioavailable and reaches the articular cartilage, which is the purported site of action [152]. Glucosamine sulfate is involved in glycoprotein metabolism and is preferentially incorporated by chondrocytes into the components of glycosaminoglycan chains of intact cartilage [151, 153].
Additional evidence suggests that glucosamine sulfate reverses some of the negative inflammatory effects of interleukin-1 on cartilage metabolism, which possibly explains the long-term benefits on joint structural changes [153]. Furthermore, early effects observed during shorter treatment periods with glucosamine sulfate may be explained by the anti-inflammatory effects mediated by suppressing superoxide radical generation, inhibiting nitric oxide synthesis, or selectively inhibiting the cyclo-oxygenase-2 pathway [153].
Like glucosamine sulfate, chondroitin sulfate is derived from animal products and its mechanism of action remains uncertain. Chondroitin sulfate is a glycosaminoglycan found in the proteoglycans of articular cartilage. It has demonstrated anti-inflammatory activities, anti-arthritic effects, and favorable effects on cartilage metabolism in vitro [154]. Animal studies have shown that both parenterally and orally administered chondroitin sulfate are incorporated into cartilage and articular tissue. Orally administered chondroitin sulfate increases hyaluronic acid and synovial fluid viscosity, which possibly explains its favorable effect on joint pain and mobility [155].
In addition to glucosamine and chondroitin sulfate, numerous other dietary supplements and herbal substances have been used for treating painful conditions. Some of the most commonly used supplements include fatty acids, fish oils, aromatic oils, and cannabis derivatives. Because of the paucity of high-quality research involving these supplements, drawing conclusions about their mechanisms of action is difficult. More methodo-logically rigorous studies and greater standardization of supplements and herbal medications are needed before their mechanisms of action can be accurately elucidated.
Energy MedicinePulsed Electromagnetic Field Therapy Relatively high-power PEMF generators have been shown to increase blood flow in the areas exposed to the fields [156], which, at least in the case of rabbits, can last for up to 3 years [157]. Increased peripheral blood flow commonly results in reduced migraine activity through yet undiscovered mechanisms [158].
Cranial Electrotherapy Stimulation Some evidence indicates changes in neurotransmitters, including serotonin and norepinephrine, as a result of CES treatment. Giordano provides a further discussion of the putative mechanism of action of CES [159].
Therapeutic Touch The purported mechanism of action for TT is based on the assumption that we live in a pandimensional, unitary world wherein energy fields are the fundamental units of humans and their environment, and linear time and separation of human and environmental fields do not exist [160]. Pain and other symptoms occur when energy is imbalanced, and therapists are purported to identify and correct energy imbalances in the patient's body to affect the pain experience. TT is viewed as a purposeful patterning of therapist-environmental/patient-environmental energy-field mutual processes that promotes maximum patient healing and well-being [161].
Reiki Two main mechanisms of action for Reiki have been proposed: gate theory (see the subsequent discussion of massage therapy) and coverage of the main meridians treated in acupuncture [38].
Qigong Qigong literally means "working on the qi or `vital energy' in the body." To better understand the purported mechanism of action, one has to accept the basic tenet of TCM that pain and other symptoms are related to the quality, flow, and imbalance of qi in the human body [41]. Qigong may involve not only the patient cultivating his or her qi to achieve optimal health in mind and body but also qigong healers or practitioners directing or emitting their qi energy to help patients clear qi imbalances or blockages or to move bad qi out of the body for pain relief [43]. Further specification of the mechanism of action is inexplicable within the Western medical model.
Manipulative and Body-Based MedicineChiropractic Manipulation Chiropractors use hands-on therapy called manipulation as their core clinical procedure. Chiropractic manipulation is a form of spinal manipulation. The term SMT is often reserved for thrust manipulation: a passive movement of a joint(s) and its components (i.e., ligaments, tendons, and cartilage) beyond their normal physiological range. Manipulation involves low-amplitude and high-velocity maneuvers [162]. While both mobilization and manipulation aim to reduce pain and increase joint range of motion, the techniques used vary significantly. This variability has led to uncertainty about the underlying mechanism of action.
Numerous hypotheses have been proposed to explain the efficacy of SMT [163]. The research to date suggests that SMT has three primary anatomic effects:(1) separation of facet joint surfaces,
(2) relaxation of the paraspinal muscles, and
(3) lowering of intradiscal pressure.Most of these changes are short-lived, and an explanation of the long-term therapeutic effects has not yet been established. Further research should delineate the biomechanical consequences of specific manipulative techniques on vertebral motion.
Massage Therapy The main mechanistic theories for the analgesic effects of massage are gate theory [164], the serotonin hypothesis [165], and the restorative-sleep hypothesis [27]. Gate theory proposes that because pressure receptors are longer and more myelinated than pain fibers, pressure signals from massage are transmitted faster and close the gate to pain signals. The serotonin hypothesis purports that massage increases serotonin levels, which is thought to modulate the pain-control system. The restorative-sleep hypothesis maintains that because substance P, a neurotransmitter associated with pain, is released in the absence of deep sleep, promotion of restorative sleep by massage reduces substance P and pain [64].
Craniosacral Therapy Proponents of craniosacral therapy maintain that movement restrictions in the cranial structures of the skull adversely affect rhythmic impulses conveyed through the cerebral spinal fluid from the cranium to the sacrum [71]. Craniosacral therapists propose that gentle pressure on external areas, including the head and back, enhance the motion of tissue and cerebral spinal fluid and thus restore the flexibility of the autonomic response, which leads to reduced symptoms, including pain.
Mind-Body MedicineMeditation Meditation effects are thought to be based in changes in awareness of pain behaviors. These changes in awareness create flexible attention that allows individuals to observe their habitual emotional and cognitive reactions to pain and then change them to more adaptive reactions [8081]. Related to this shift in cognitive and emotional processing away from a habitual alarm state are increased self-efficacy, improved coping capacities, and general attenuation of stress [83]. Another potential mechanism is the relaxation that often accompanies meditation and is often a goal of concentrative meditation techniques [166]. Meditation may also share a mechanism thought to be common to several MBTs: the release of nitric oxide that stimulates vasodilatation, anti-inflammatory, and morphinergic and/or endocannabinoid activity [167168].
Hypnosis No clear mechanism for hypnotic analgesia has been identified, although evidence exists that brain activity in the sensory cortex and limbic system are differentially affected as a function of the type of suggestion given (i.e., decreased pain sensations vs decreased bothersomeness of pain) [169171] and that hypnotic-analgesia suggestions can alter sensory information processing at the level of the spinal cord [172173].
Yoga No specific mechanism of action for yoga has been established by existing studies. In the yogic tradition, benefits are thought to be related to the quieting of the negative impulses of the mind, which improves the individual's functioning of the organ and musculoskeletal systems and increases his or her ability to use breath energy or prana [98]. General mechanisms of action associated with yoga could include physical effects, such as improved flexibility and strength and reduced postural guarding and other habitual physical behaviors associated with chronic pain. Mental effects could include increased mental focus, improved body awareness, and changed beliefs about physical ability and pain. General stress reduction through activity and relaxation exercises is also a potential mechanism.
Biofeedback The mechanism of action for biofeedback in pain management has not been fully established. However, evidence is increasing that for chronic muscle or myofascial pain syndrome, pain modulation with biofeedback is achieved via decatastrophizing and learning lowered arousal techniques that prevent the maintenance of sympathetic pathways to trigger points [112,174]. For pain conditions such as fibromyalgia, phantom, and other centrally mediated pain, biofeedback may counter the effect of central sensitization through decreasing sympathetic overload, parasympathetic withdrawal, and stress hormones. Some evidence also exists that changing improper muscle contraction and blood flow patterns directly affect pain caused by these problems [105,127].
Whole or Professionalized Complementary and Alternative Medicine PracticesHomeopathy A key premise of homeopathy is that each person has innate energy called a "vital force" or a self-healing response. When a person's energy is disrupted or imbalanced, health problems such as chronic pain may develop. Therefore, the overriding goal of homeopathic practice is the recommendation of remedies that stimulate the body's own healing responses. The primary mechanism of homeopathy is based on the law of "similars" or the "like cures like" principle. This theory proclaims that if a large amount of a certain substance can cause specific symptoms in a healthy person, smaller amounts of that same substance can treat symptoms in an ill person [175]. Thus, the practitioner of homeopathy would attempt to stimulate the healing responses by providing a smaller amount of the same substance that caused the symptoms. Unfortunately, no published empirical evidence supports this theory [176].
Acupuncture Although many studies have documented the efficacy of acupuncture for pain and other medical conditions, understanding how it works within a Western medical paradigm remains challenging. Like qigong, acupuncture originated in TCM. In TCM, regulation of qi is the major source of health problems and illness and acupuncture purportedly treats pain and other conditions by improving the quality, balance, and flow of qi. In Western medical nomenclature, the proposed mechanisms involve regulation of the nervous system, stimulation of the immune system, and alteration of the brain chemistry and cause the release of various neurotransmitters and hormones. Thus, acupuncture affects parts of the central nervous system related to sensation and involuntary body functions, such as immune reactions and processes that regulate a person's blood pressure, blood flow, and body temperature [177178].
CONCLUSIONS
We reviewed the published research on commonly used CAM treatments for chronic pain. Our findings show that CAM therapies, as a group, have a mixed track record for efficacy. Not only do the different CAM modalities show different levels of efficacy but one modality may work for one pain condition but not others. The CAM modalities with the best track records for pain management are biofeedback, hypnosis, and massage (particularly for low back and shoulder pain). In selecting a CAM modality either as an alternative or complement to traditional pain interventions, such as medication, practitioners must weigh the pros and cons of the modality and tailor the interventions to the needs of the chronic pain patient. In addition to efficacy, other issues that practitioners must consider when making decisions about CAM use include additional time and energy investments, the need for specialized trained personnel to administer the modalities in question, known side effects or potential toxic effects, safety in combining CAM and other modalities, likely acceptance by clients and the public (and hence issues of long-term compliance), and ease of incorporation into traditional pain management practices.
ACKNOWLEDGMENTS
We wish to acknowledge the financial support provided by the National Headache Foundation, the U.S. Army Medical Command's Department of Clinical Investigation, the National Institutes of Health, the National Institute of Child Health and Human Development, the National Center for Medical Rehabilitation Research, the National Institute on Drug Abuse, the National Institute of Mental Health, and the Department of Veterans Affairs Health Services Research and Development Service.
Contributions to this article are reflected in the order of authorship as follows: Dr. Tan, Dr. Tsao, Dr. Craine, Dr. Bair; remaining authors shown in alphabetical order.
This material was based on work supported in part by the National Headache Foundation (Dr. Sherman), the U.S. Army Medical Command's Department of Clinical Investigation (Dr. Sherman), the National Institutes of Health (grant R01 GM42725-09A1, Drs. Patterson and Jensen), the National Institute of Child Health and Human Development, the National Center for Medical Rehabilitation Research (grant P01 HD33988, Drs. Patterson and Jensen), the National Institute on Drug Abuse (grant 5R03 DA17026-2, Dr. Tsao), the National Institute of Mental Health (grant 5R01 MH063779-03, Dr. Tsao), and a Department of Veterans Affairs Health Services Research and Development Career Development Award (Dr. Bair).
The authors have declared that no competing interests exist
References:
Please refer to the Full Text article (in a separate screen)

Return to ALT-MED/CAM ABSTRACTS
Return to SPINAL PAIN MANAGEMENT
Since 7-04-2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |