

Spinal Pain in Adolescents: Prevalence, Incidence,
and Course: A School-based Two-year Prospective
Cohort Study in 1,300 Danes Aged 11-13This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: BMC Musculoskelet Disord. 2014 (May 29); 15: 187 ~ FULL TEXT
OPEN ACCESS Ellen Aartun, Jan Hartvigsen, Niels Wedderkopp, and Lise Hestbaek
Department of Sports Science and Clinical Biomechanics,
University of Southern Denmark,
Odense, DenmarkBACKGROUND: The severity and course of spinal pain is poorly understood in adolescents. The study aimed to determine the prevalence and two-year incidence, as well as the course, frequency, and intensity of pain in the neck, mid back, and low back (spinal pain).
METHODS: This study was a school-based prospective cohort study. All 5th and 6th grade students (11-13 years) at 14 schools in the Region of Southern Denmark were invited to participate (N=1,348). Data were collected in 2010 and again two years later, using an e-survey completed during school time.
RESULTS: The lifetime prevalence of spinal pain was 86% and 89% at baseline and follow-up, respectively. A group of 13.6% (95% CI: 11.8, 15.6) at baseline and 19.5% (95% CI: 17.1, 22.0) at follow-up reported that they had pain frequently. The frequency of pain was strongly associated with the intensity of pain, i.e., the majority of the participants reported their pain as relatively infrequent and of low intensity, whereas the participants with frequent pain also experienced pain of higher intensity. The two-year incidence of spinal pain varied between 40% and 60% across the physical locations. Progression of pain from one to more locations and from infrequent to more frequent was common over the two-year period.
CONCLUSIONS: Spinal pain is common at the age of 11-15 years, but some have more pain than others. The pain is likely to progress, i.e., to more locations, higher frequency, and higher pain intensity over a two-year period.
From the Full-Text Article:
Background
It is now widely acknowledged that neck pain (NP), mid back pain (MBP), and low back pain (LBP) (spinal pain) start early in life and that the lifetime prevalence increases rapidly during adolescence to reach adult levels at the age of 18 [1, 2]. In adults, LBP is now the leading cause of years lived with disability on a global level [3] and the societal burden due to disability pensions and treatment costs for this disorder are high and increasing [4]. Even amongst adolescents, consequences of pain are common, e.g., 8% of all 13 year olds and 34% of all 15–year olds seek health care for spinal pain in Denmark [5], and among those reporting recurrent LBP, 31% have refrained from participating in sport and physical activity and 26% have been absent from school [6], indicating that spinal pain in adolescence is not a negligible problem. In addition, spinal pain in adolescence is strongly associated with spinal pain and generalised pain in adulthood [7, 8] so, the young population is a group of special interest when exploring the incidence, progression, and severity of spinal pain.
The incidence of NP, MBP, and LBP reported in adolescents is based on various definitions of pain, i.e., weekly pain in the past 3 or 6 months [9–12], frequent pain [13], quite bad pain [14], and pain in the past week [15]. Incidence is however defined as new cases of a disease during a specified time period and prior studies have rarely been based on a group that has never had pain. In addition, the severity of spinal pain in adolescents has previously been assessed by describing the consequences of the pain and not directly by describing the pain characteristics such as frequency and intensity [16]. In addition, the aspect of multiple pain sites and the extent to which the pain dissipates or changes location in the spine over time has not been addressed in this population, which is of interest because multiple pain sites are associated with high disability in adolescents [17], and in adults, they are a predictor of work disability [18]. Consequently, there has been a call for more longitudinal studies [19], but to our knowledge, there are no population-based longitudinal studies that describe pain characteristics and changes in spinal pain in adolescence.
Therefore, the overall aims of this longitudinal cohort study were to determine the prevalence, severity and course of spinal pain in Danish adolescents. The specific objectives were to:a) Determine the lifetime, one-week, and point prevalence of NP, MBP, and LBP (separately and combined) at age 11–13 and age 13–15,
b) Determine the frequency and intensity of NP, MBP, and LBP and explore the associations between the two,
c) Estimate the two-year incidence of NP, MBP, and LBP, and
d) Describe the changes in pain location and the changes in frequency of spinal pain from baseline to follow-up.
Methods
Participants
This study was nested within the SPACE study. SPACE was a school-based cluster-randomised controlled trial involving 14 schools in the Region of Southern Denmark [20]. The main aim of SPACE was to investigate how physical environment combined with organisational initiatives could promote physical activity in adolescents aged 11–13 years. All 1,348 5th and 6th grade students (aged 11–13 years) at the 14 schools were invited to participate. There were no exclusion criteria. For a comprehensive description, see the SPACE protocol [20]. There were no differences between the control group and the intervention group at baseline or follow-up with regard to adiposity, physical fitness or musculoskeletal strength [21]. Therefore, it did not seem likely that the intervention had an impact on the presence of spinal pain and so, we decided to use the pooled cohort rather than the control group only.
Prior to the study, the parents of the involved students received a letter including information about the project. Participation did not require parental consent, but the parents were informed that they could initially, or at any time later, withdraw their child’s participation. This form of passive consent was reviewed by the Regional Committee for Health Research Ethics together with the rest of the project protocol. The conclusion was that the project was acceptable according to Danish legislation and did not require formal approval because all tests were non-invasive and there were no physical interventions involved [22]. Approval from the Danish Data Protection Agency was obtained (#2010-41-5147).
Data collection
The participants completed an electronic questionnaire (e-survey) during school time, observed by a teacher who also ensured that there were no interactions between participants. For a detailed description of the e-survey, see the SPACE protocol [20]. Baseline data were collected from April to June 2010 and two-year follow-up data from April to June 2012.
The e-survey contained parts of the Young Spine Questionnaire [23], which included identical questions for the three spinal regions separately. Using the neck questions as an example, the first question was: "Have you ever had pain in your neck?" ("often"/"sometimes"/ "once or twice"/"never"). If so, the next questions were: "Have you had neck pain in the last week?" ("yes"/"no") and "Do you have neck pain today?" ("yes"/"no"). Finally, they noted the worst pain ever in the neck using the revised version of the Faces Pain Scale (FPS-R) [24]. This scale is based on six faces with expressions illustrating progressively worse pain. The questions were repeated for the mid back and low back. A diagram with the three spinal areas clearly shaded and labelled was shown alongside the questions. The e-survey was designed in such a way that there was a jump to the next spinal region if the participant answered "never" to a question because any subsequent questions about pain last week or today, and pain intensity then became irrelevant for that particular spinal region. Immediately following the questions, an open field for comments was provided. The questionnaire was developed for 9–11–year olds and has shown satisfactory results for feasibility, content validity, and item agreement between questionnaire scores and interview findings [23].
Variables
Lifetime, one week, and point prevalence of NP, MBP, and LBP were defined as a positive response to the first, second and third questions respectively for each spinal region. If the student answered "never" to the lifetime question, it was assumed that the answers to the one week and point prevalence questions were "no". Spinal pain was defined as pain in any of the three locations.
Frequency of NP, MBP, and LBP were "often", "sometimes", "once or twice", or "never". Frequency of spinal pain was defined as "often", "sometimes", "once or twice", or "never" in any of the three locations. If the frequency of pain differed in the three locations, the location with the highest frequency was used. A missing value in any region resulted in a missing value for this variable.
Pain intensity was based on the FPS-R with six faces scaled from 1 to 6 where 1 was labelled "no pain" and 6 as "very much pain" in the questionnaire. Then, the pain intensity was rescaled into a 0–10 scale (1 → 0, 2 = 2, 3 → 4, 4 → 6, 5 → 8, and 6 → 10).
Incidence cases were defined as those who reported "never" having had pain at baseline but reporting pain at follow-up. Incidence proportions were reported separately for each spinal location.
Pain locations were defined as none, NP only, MBP only, LBP only, NP + MBP, NP + LBP, MBP + LBP, and NP + MBP + LBP based on answers to the lifetime question. A missing value in any region resulted in a missing value for all the pain combinations that included this region.
Descriptive statistics
The prevalence, frequency, two-year incidence, and changes in pain locations and frequency of spinal pain from baseline to follow-up were reported using percentages and 95% confidence intervals (CI). The pain intensity was reported using the mean with 95% CI. Cross-sectional descriptions were reported by gender, but due to smaller cell sizes, the longitudinal descriptions were presented for the combined cohort only. The associations between frequency and pain intensity were illustrated graphically by histograms with 95% CI bars.
Post-hoc analysis: There was a technical problem at one school where some of the students were unable to respond "never" at the LBP question at baseline. The lifetime, one week and point prevalence of LBP were therefore calculated also with this school excluded in order to investigate how much this technical problem had affected the prevalence of LBP. All statistics were calculated using STATA version 11.2.
Results
The participation rate was 95.8% (n = 1,291) at baseline and 82.4% (n = 1,064) at follow-up. Seventy-seven percent (n = 1,042) filled in both questionnaires. The participation rate for the follow-up was lower, primarily because a number of students had changed school (n = 156). Nineteen students refused to participate at baseline, and a further 14 refused to participate at follow-up. There were 51.6% (n = 666) boys at baseline and 53.1% (n = 565) at follow-up. The mean age was 12.6 years (SD = 0.63) at baseline. There were some statistically significant differences in baseline characteristics of those who completed both questionnaires and those who just completed the baseline questionnaire. Among the drop-outs, there was a predominance of girls and participants who had a history of NP and LBP, and participants who had pain at more pain sites, but who did not have higher frequency or intensity of pain.
Prevalence

Table 1 At baseline, the lifetime prevalence of spinal pain was 86% (95% CI: 84.0, 87.8), the one-week prevalence was 35.9% (95% CI: 33.3, 38.6) and the point prevalence was 16.9% (95% CI: 14.9, 19.0). At follow-up, the lifetime, one-week and point prevalence of spinal pain was 88.8% (95% CI: 86.9, 90.7), 48.5% (95% CI: 45.4, 51.5) and 22.9% (95% CI: 20.4, 25.5) respectively. NP was consistently the most common spinal pain site followed by MBP, and lastly LBP (Table 1). The lifetime, one week and point prevalence at baseline and follow-up are for all locations presented by gender in Table 1.
Frequency, pain intensity, and the association between them

Table 2

Table 3
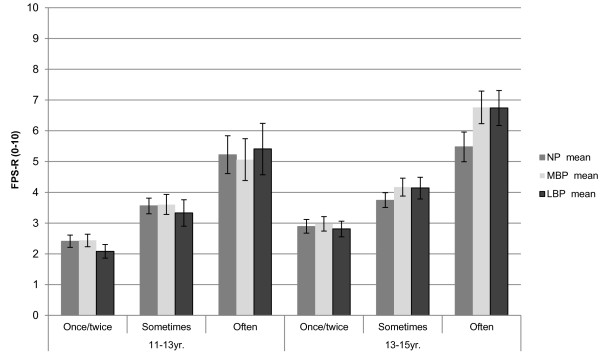
Figure 1 NP, MBP, and LBP were mostly experienced only "once or twice" at both time-points (Table 2). A group of 13.6% (95% CI: 11.8, 15.6) of the participants reported that they often had spinal pain at baseline and this group increased to 19.5% (95% CI: 17.1, 22.0) at follow-up. Detailed results for the frequency of NP, MBP, and LBP are presented by gender in Table 2.
The mean pain intensity was relatively low at baseline for all three spinal regions: 3.1 (95% CI: 2.9, 3.3) for NP, 3.1 (95% CI: 2.9, 3.2) for MBP and 2.7 (95% CI: 2.5, 3.0) for LBP. At follow-up, the mean pain intensity was higher in all locations. See Table 3 for gender-specific details.The mean pain intensity was lowest for students reporting pain "once or twice" with a statistically significant progressive increase across the "sometimes" and "often" groups. Thus the largest group had pain that was both of low frequency and low intensity, but a smaller group reported pain of both high frequency and intensity. This pattern was seen for all spinal regions and at both time-points (Figure 1).
Changes in pain locations
The two-year incidence of NP (no NP at baseline followed by NP at follow-up) was 60.1% (95% CI: 54.1, 66.0), for MBP 49.8% (95% CI: 45.0, 54.5), and for LBP 42.1% (95% CI: 38.2, 46.1).
Changes in pain locations

Table 4 Both at baseline and follow-up, pain in all three locations combined was most common followed by the combination of NP and MBP (Table 4). We observed that changes in pain location were common over the two-year period (Table 4). We also observed that regardless of pain location at baseline, they were most likely to report pain in all three locations at follow-up. An exception to this was those with MBP only, who were more likely to have the combination of NP and MBP at follow-up (Table 4). In total, 378 (51.8%) participants had pain in more locations at follow-up than at baseline, whereas 262 (29.8%) had pain in fewer locations.
Changes in frequency of spinal pain

Table 5 It appears that the spinal pain progressed from "never" to "once or twice" and further to "sometimes" and "often". Only a very small proportion of participants shifted from "never" to "often" (1.9%) (Table 5) and half of those reporting spinal pain "often" at baseline continued to have it at follow-up (Table 5). Paradoxically, a small proportion (7.7%) of those who reported pain at baseline did not do so at follow-up. We ascribe this to poor recall, and it is worth noting that this proportion was lower for those who reported spinal pain "often" (3.9%) than those who reported spinal pain "once or twice" (9.3%) at baseline (Table 5).
Post-hoc analysis
When the school with the technical failure was excluded from analysis, the lifetime prevalence of LBP at baseline was two percentage points lower than reported in Table 1, but there were no differences in the one-week and point prevalence.
Discussion
Pain in the spine affected almost nine out of ten 11–15–year olds and among those who did not report spinal pain at age 11–13, around half had experienced pain two years later. For the majority, the pain appears to be relatively mild, i.e., mostly reported as "once or twice" and of low intensity. However, 14–20% reported more frequent pain which was also of higher intensity. In addition, localised spine pain in early adolescence appears to spread to involve other areas of the spine over time.
This study reports higher prevalence and incidence of spinal pain than previous studies. A systematic review has shown that the lifetime prevalence of NP in adolescents ranged from 3% to 8%, MBP from 9.5% to 72%, and LBP from 7% to 72% [1]. Earlier reporting of incidence has been based on varying definitions including weekly pain in the past 3 or 6 months [9–12], frequent pain [13], quite bad pain [14], and pain in the past week [15]. Nissinen et al. reported a one–year incidence of LBP, based on ‘LBP ever’, in 18% of adolescents from age 13 to 14 [25], which appears comparable to our result of 42% for a two–year incidence. However, because of the large variation in pain reporting in the past, comparison between estimates should be made with caution [1]. A reasonable explanation for the high lifetime prevalence and incidence in this study is related to the response options of the first question ("Have you ever had neck pain?") which were "often"/"sometimes"/"once or twice"/"never". We assume some of those answering "once or twice" might have answered "no" if the only options were "yes" or "no". This assumption is based on an issue detected during the development of the questionnaire. In the first version, there was not a "once or twice" response option. During interviews, it became obvious that many children did not know whether to answer "never" or "sometimes" if the pain was experienced only once or twice, as they did not consider this frequency enough to be categorised as "sometimes". Therefore, the option "once or twice" was included in the questionnaire [23]. The theory of the "once or twice" response option as an explanation of the high lifetime prevalence could be supported by another observation. If the variable of lifetime prevalence was dichotomised differently, i.e., if "once or twice" was included as "no", the results were more similar to previous reported lifetime prevalence. Although it makes comparisons with previous studies difficult, we recommend this approach in the future as it might result in more precise estimates. Also, some considerations need to be taken into account when presenting incidence rates. We observed that some students at follow–up reported that they had "never" had pain, despite a report of pain at baseline. Therefore, it is likely that some of those who reported never having had pain at baseline could have had an experience of pain previously. Since incidence is defined as new cases of a disease over a specified time period, we are sceptical of the use of this term.
The literature about frequency, pain intensity and the association between them is currently limited, but supports the findings from this study. Investigating back pain frequency, Brattberg et al. reported that 22% of the boys in their study and 47% of the girls aged 13 years had back pain often [13]. A similar association between frequency and intensity was reported in another study for NP [10], but no studies of such an association were found in relation to MBP and LBP.
The report of pain in multiple locations was more common than reporting pain in one location only. We know that multiple pain sites are associated with disability in adolescents [17], but it is unknown if there is a difference in disability between those who experience pain simultaneously at the three locations or those with pain that shifts from one location to another. The association between disability and concurrent/non–concurrent pain at multiple sites, and the influence of other pain characteristics such as frequency and intensity should be investigated in future research.
The strengths of this study were the school–based population and the longitudinal design. A follow–up period of two years is relatively short from a life course perspective, but enough to be able to observe an increase in all measured parameters and a noticeable change in pain location and frequency of spinal pain. Another strength was that the questionnaire used was developed for the target population [23] and answered by the participants without parental or peer influence. We know that this age group is not very discriminative when reporting pain, e.g., scratches can be reported as back pain if they are located on the back, so comparison of prevalence with the adult population should be done with caution [23]. This is one of the reasons why we included other descriptive variables like frequency and pain intensity in the study; we wanted other variables to determine the severity of the pain.
The technical problem at one of the schools slightly inflated the lifetime prevalence of LBP at baseline, but did not influence the conclusions that can be drawn from this study. Finally, biological age might be a better predictor than chronological age as used in this study, but unfortunately we do not have data to illustrate this. We recommend that pubertal stage is considered in future studies.
Conclusions
Neck, mid back, and low back pain are common at the age of 11–15 years. For the majority of the participants, the pain seems to be mild in nature, relatively infrequent and of low intensity. A group of 14–20% was more severely affected with frequent pain which was also more intense. The two–year course showed a progressive development in pain, and that pain was likely to spread to more locations over a two–year period, regardless of initial pain location.
Abbreviations
CI: Confidence interval;
FPS-R: Faces pain scale – revised;
LBP: Low back pain;
MBP: Mid back pain;
NP: Neck pain.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
EA: Conception and design, analysis, drafting the manuscript. JH: Conception and design, analysis, revising the manuscript. NW: Conception and design, revising the manuscript. LH: Conception and design, data collection, analysis, revising the manuscript. All authors have read and approved the manuscript.
Acknowledgements
This work was supported by the Danish Chiropractic Research Stipend, University of Southern Denmark, the Norwegian Chiropractic Association, and Nordic Institute for Chiropractic and Clinical Biomechanics. The SPACE study was provided by the Centre for Intervention Research. The Centre is funded by TrygFonden and the Danish Cancer Society. The SPACE study was funded by TrygFonden.
REFERENCES:
Jeffries LJ, Milanese SF, Grimmer-Somers KA:
Epidemiology of Adolescent Spinal Pain:
A Systematic Overview of the Research Literature
Spine (Phila Pa 1976). 2007 (Nov 1); 32 (23): 2630–2637Leboeuf-Yde C, Kyvik KO:
At What Age Does Low Back Pain Become a Common Problem?
A Study of 29,424 Individuals Aged 12-41 Years
Spine (Phila Pa 1976). 1998 (Jan 15); 23 (2): 228–234Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, et al.:
Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases and Injuries 1990-2010:
A Systematic Analysis for the Global Burden of Disease Study 2010
Lancet. 2012 (Dec 15); 380 (9859): 2163–2196Martin, BI, Deyo, RA, Mirza, SK et al.
Expenditures and Health Status Among Adults With Back and Neck Problems
JAMA 2008 (Feb 13); 299 (6): 656–664Kjaer P, Wedderkopp N, Korsholm L, Leboeuf-Yde C.
Prevalence and Tracking of Back Pain From Childhood to Adolescence
BMC Musculoskelet Disord. 2011 (May 16); 12: 98Jones MA, Stratton G, Reilly T, Unnithan VB:
A school-based survey of recurrent non-specific low-back pain prevalence and consequences in children.
Health Educ Res 2004, 19:284-289Hestbaek L, Leboeuf-Yde C, Kyvik KO, Manniche C:
The Course of Low Back Pain from Adolescence to Adulthood:
Eight-year Follow-up of 9600 Twins
Spine (Phila Pa 1976). 2006 (Feb 15); 31 (4): 468–472Brattberg G:
Do pain problems in young school children persist into early adulthood? A 13-year follow-up.
Eur J Pain 2004, 8:187-199El-Metwally A, Salminen JJ, Auvinen A, Macfarlane G, Mikkelsson M:
Risk factors for development of non-specific musculoskeletal pain in preteens and early adolescents: a prospective 1-year follow-up study.
BMC Musculoskelet Disord 2007, 8:46Stahl M, Mikkelsson M, Kautiainen H, Hakkinen A, Ylinen J, Salminen JJ:
Neck pain in adolescence. A 4-year follow-up of pain-free preadolescents.
Pain 2004, 110:427-431Feldman DE, Shrier I, Rossignol M, Abenhaim L:
Risk factors for the development of low back pain in adolescence.
Am J Epidemiol 2001, 154:30-36Ehrmann Feldman D, Shrier I, Rossignol M, Abenhaim L:
Risk factors for the development of neck and upper limb pain in adolescents.
Spine 2002, 27:523-528Brattberg G:
The incidence of back pain and headache among Swedish school children.
Qual Life Res 1994, 3(Suppl 1):S27-S31Burton AK, Clarke RD, McClune TD, Tillotson KM:
The natural history of low back in adolescents.
Spine 1996, 21:2323-2328Grimmer K, Nyland L, Milanese S:
Repeated measures of recent headache, neck and upper back pain in Australian adolescents.
Cephalalgia 2006, 26:843-851Calvo-Munoz I, Gomez-Conesa A, Sanchez-Meca J:
Prevalence of low back pain in children and adolescents: a meta-analysis.
BMC Pediatr 2013, 13:14Hoftun GB, Romundstad PR, Rygg M:
Factors associated with adolescent chronic non-specific pain, chronic multisite pain, and chronic pain with high disability: the young-HUNT study 2008.
J Pain 2012, 13:874-883Kamaleri Y, Natvig B, Ihlebaek CM, Bruusgaard D:
Does the number of musculoskeletal pain sites predict work disability? A 14-year prospective study.
Eur J Pain 2009, 13:426-430Jones GT:
Pain in children - a call for more longitudinal research.
Pain 2011, 152:2202-2203Toftager M, Christiansen LB, Kristensen PL, Troelsen J:
SPACE for physical activity–a multicomponent intervention study: study design and baseline findings from a cluster randomized controlled trial.
BMC Public Health 2011, 11:777Christiansen LB, Toftager M, Boyle E, Kristensen PL, Troelsen J:
Effect of a school environment intervention on adolescent adiposity and physical fitness.
Scand J Med Sci Sports 2013, 23:e381Guidelines about notification etc. of a biomedical research project to the committee system on biomedical research ethics, No 9154, 5 May 2011
http://www.cvk.sum.dk/English/guidelinesaboutnotification.aspx webciteLauridsen HH, Hestbaek L.
Development of the Young Spine Questionnaire
BMC Musculoskelet Disord 2013 (Jun 12); 14: 185Hicks CL, von Baeyer CL, Spafford PA, van Korlaar I, Goodenough B:
The faces pain scale-revised: toward a common metric in pediatric pain measurement.
Pain 2001, 93:173-183Nissinen M, Heliovaara M, Seitsamo J, Alaranta H, Poussa M:
Anthropometric measurements and the incidence of low-back-pain in a cohort of pubertal children.
Spine 1994, 19:1367-1370
Return to PEDIATRICS
Return to NECK AND BACK PAIN
Return to SPINAL PAIN MANAGEMENT
Since 11–24–2014


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |