MRI Spine Protocols This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: The American Chiropractor ~ September 25, 2013 ~ FULL TEXT
by Mark Studin, D.C., F.A.S.B.E.(C), D.A.A.P.M., D.A.A.P.L.M.
Your pateint has radicular pain in the lumbosacral distribution that is status post-motor vehicle accident and you order a lumbar MRI. The report rendered by a board certified general radiologist concludes mild disc bulging at L5-S1. However, upon further review by both a neuroradiologist and yourself (once you have been certified and trained to interpret MRI), you realize the general radiologist erred and the scan reveals a protrusion-type herniation compressing the left L5 nerve root correlating to your pateint’s clinical presentation.
Herein lies multiple potential culprits for an inaccurate diagnosis. First, as I have discussed previously, general radiologists have a 42.2% error rate as reported by Lurie, Doman, Spratt, Tosteson, and Weinstein (2009), which makes it virtually imperitive that we, as practitioners, must take control of a critical component in diagnosing our patients. At the very least, we must understand the basics of MRI spine interpretation to verify the findings or lack thereof. We also must be congnizant of the fact that we often rely on the MRI when ordering and delivering high velocity thrusts into our pateints. At this level, accuracy matters in determining a correct prognosis and treatment plan to ensure the safety of our patients when adjusting the spine. It is imperative for chiropractic.
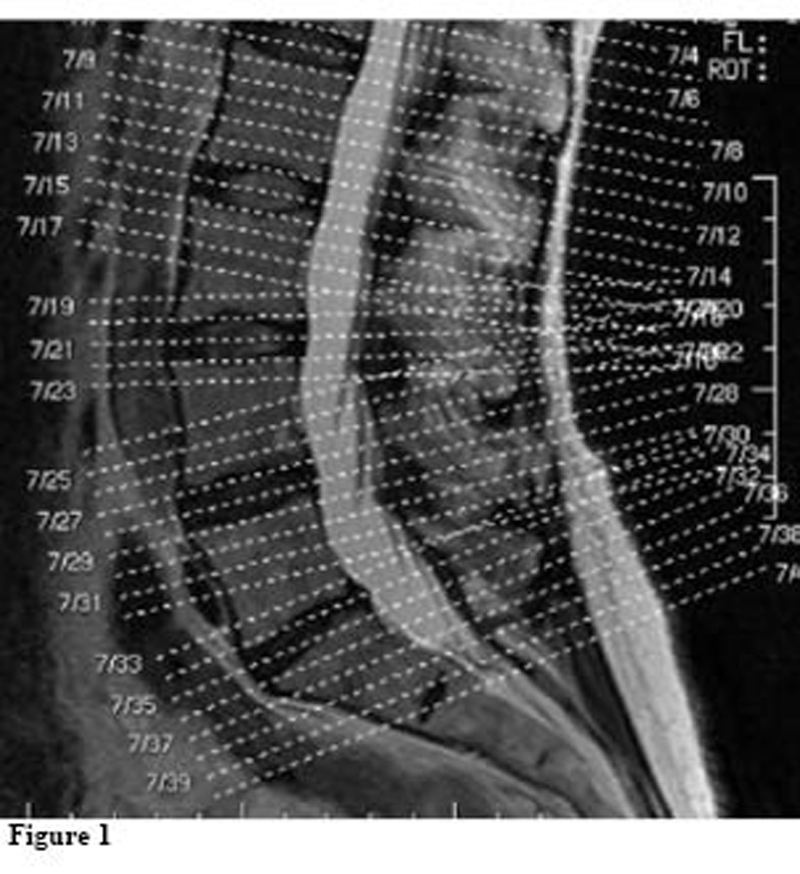
A second factor in accurate MRI reporting is the precise acquisition of slices. Too many MRI technicians are not meticulous in positioning where the slices are taken and often catch too much of the end plates or the vertebrae, and sometimes do not catch the disc at all. After reviewing thousands of MRIs in the last few months, I can report that almost 75% of images are not done to the required standard, and in many cases radiologists must guess with incomplete image acquisitions. A case in point is image 1, which has both good and bad slice acquisitions.
Referencing Figure 1, the slices should be through the disc and not catching the end plates or the vertebrae when diagnosing the disc. If we look at L5-S1 and slices 734, 735, and 736, you will notice that all of the slices catch the end plates and not one clean slice of the disc was acquired. If we go to the level above at L4-L5 and slices 727, 728, and 729, the top two slices are 100% through the disc (good), while 729 misses the disc entirely. Although acquisition of bone is necessary, that was not the intented purpose of that slice.
If we compare L5-S1 to L4-L5, it illustrates this problem in one patient. Every disc ideally should have a minimum of three clean slices through the disc without catching the end plates. There should then be slices through the bone as well to diagnose any osseous issues. The lack of clean slices is nothing more than the MRI technician “missing the target” and the radiologists accepting inferior images to interpret. In teaching hospitals, as with my patients, I demand clean slices or I mandate the center redo the scan if I feel that I am missing pathology. Should your imaging company offer 3-D technology, as mine does (a topic for another article), you can get 24 slices through one disc. However, most MRI centers do not yet have this technology available.
Many will argue that, based on either the scout image or the sagittal view, it does not warrant thin slices or that thin slices will create too much signal-to-noise ratio and cause poor quality images. That is a great argument to take thick slices and result in fewer images increasing the profit margin of the imaging center. Otherwise, the argument is moot and centered on the bottom line versus quality patient care.
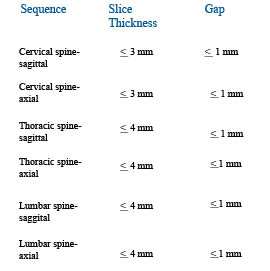
Slice thickness is another critical component of a quality MRI. The American College of Radiology (ACR) has set forth the following guidelines for maximum thicknesses:
The key to this graph is the concept “maximum” and it does not illustrate a complete sequence to ensure that most pathologies are not missed. In addition, most MRI centers tout that they are ACR accredited and that is factual. However, being ACR accredited does not mean that they use ACR guidelines in their scans. In addition, there are no regulatory standards in any state enforcing those guidelines for imaging centers. That “ruse” is quite profitable for those centers at both you and your patients’ expense because this often leads to many missed pathologies. So it also leaves you exposed to hurting your patients—caveat emptor!
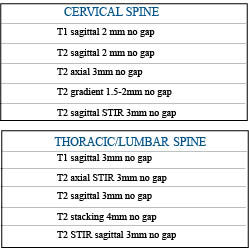
According to Robert Peyster, MD, neuroradiologist and section chief of neuroradiology of State University of New York at Stony Brook Medicine who acquired his neuroradiology education at Mass General (Harvard) and has been published more than sixty times on MRI, the following sequences should be considered:
Please note that all of the scenarios involve “no gap.” They are no longer necessary with today’s technology. These recommendations exceed the ACR guidelines and are meant to do so. As I have already articulated, those guidelines are minimum standards with maximum slice thicknesses. The thinner the slice, the more you see with “volume averaging” in image acquisition.
Understanding that this article is intended to serve as a guide, I urge every DC worldwide to learn the significance of each sequence and be able to interpret MRIs (or at least the basics) to protect patients from any of the above scenarios. Dr. Peyster and other world-class specialists teach MRI to DCs at www.teachdoctors.com. This course carries a certification from the University of Bridgeport, College of Chiropractic and State University of New York at Buffalo, School of Medicine and Biomedical Sciences. This is the only program that offers a “cross certification” through both chiropractic and medical academia. Although this has had significant positive ramifications for chiropractic in the courts nationally by allowing DCs to testify as experts when challenged, the real winners are the patients.
Do not be taken advantage of by unscrupulous imaging centers when ordering MRIs. Winning through clinical excellence is the only solution and DCs now have the opportunity to learn how to interpret MRIs from the same educators who have taught thousands of medical neuroradiologists to interpret spinal MRIs. This level of clinical excellence has nothing to do with your philosophy of practice or method of delivery of care. It is purely about accurately triaging your patients with an accurate diagnosis, prognosis, and treatment plan.
References:
- Lurie, J. D., Doman, D. M., Spratt, K. F., Tosteson, A. N. A., & Weinstein, J. N. (2009).
Magnetic resonance imaging interpretation in patients with symptomatic lumbar spine disc herniations.
Spine, 34(7), 701-705
- American College of Radiology (2011).
MRI practice guideline for the performance of magnetic resonance imaging (MRI) of the adult spine.
Last retrieved July 11, 2013 from
http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/MRI_Adult_Spine.pdfMark Studin, D.C., F.A.S.B.E.(C), D.A.A.P.M., D.A.A.P.L.M.
Dr. Mark Studin is just one voice, a chiropractor seeking to attain 95% of the entire population under chiropractic care in his lifetime. He can be reached at DrMark@TeachDoctors.com or 631-786-4253.
Return to RADIOLOGY
Since 1-25-2014


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |