The Efficacy of Forward Head Correction on Nerve
Root Function and Pain in Cervical Spondylotic
Radiculopathy: A Randomized TrialThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Clinical Rehabilitation 2012 (Apr); 26 (4): 351–361 ~ FULL TEXT
Aliaa A Diab and Ibrahim M Moustafa
Basic Science Department,
Faculty of Physical therapy,
Cairo University, Egypt.
OBJECTIVE: To investigate the effect of forward head posture correction on pain and nerve root function in cases of cervical spondylotic radiculopathy.
DESIGN: A randomized controlled study with six months follow-up.
SETTING: University research laboratory.
SUBJECTS: Ninety-six patients with unilateral lower cervical spondylotic radiculopathy (C5-C6 and C6-C7) and craniovertebral angle measured less than or equal to 50° were randomly assigned to an exercise or a control group.
INTERVENTIONS: The control group (n = 48) received ultrasound and infrared radiation, whereas the exercise group (n = 48) received a posture corrective exercise programme in addition to ultrasound and infrared radiation.
MAIN OUTCOME MEASURES: The peak-to-peak amplitude of dermatomal somatosensory evoked potentials, craniovertebral angle, visual analogue scale were measured for all patients at three intervals (before treatment, after 10 weeks of treatment, and at follow-up of six months).
RESULTS: There was a significant difference between groups adjusted to baseline value of outcome at 10 weeks post-treatment for craniovertebral angle, pain, C6 and C7 peak-to-peak amplitude of dermatomal somatosensory evoked potentials P = 0.000, 0.01, 0.000, 0.001 respectively and at follow-up for all previous variables (P = 0.000).
CONCLUSION: Forward head posture correction using a posture corrective exercise programme in addition to ultrasound and infrared radiation decreased pain and craniovertebral angle and increased the peak-to-peak amplitude of dermatomal somatosensory evoked potentials for C6 and C7 in cases of lower cervical spondylotic radiculopathy.
From the Full-Text Article:
Introduction
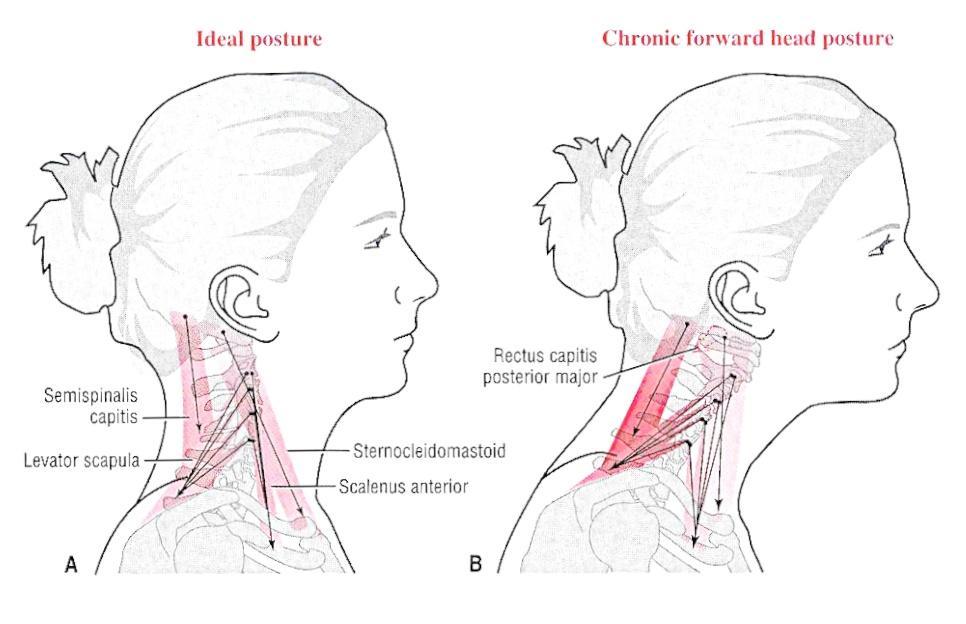
Although age appears to be the major risk factor for degenerative changes, mechanical disturbance of the cervical spine is considered as one of the most deteriorative factors for cervical spondylosis. [1] In this regard, forward head posture has been shown to be a common postural displacement, with a conservative estimate being 66% of the patient population. [2] It is generally believed that this abnormal posture is associated with the development and persistence of many disorders including cervicogenic and migraine headaches, [3] myofacial pain syndrome, [4] abnormal scapular movement, [5] and even temporomandibular disorders, [6] which justify the growing interest with the importance of normal posture as clinical outcome of health care as supported by many authors. [7, 8]
The association between forward head posture and neck pain has been investigated in many studies. However, the literature does not give concrete information on this relationship. Two recent systematic reviews did not find an association between head posture and neck pain. [9, 10] Conversely, two other systematic reviews have shown a significant differences in the cervical posture of an adult neck pain patient population when compared to a matched asymptomatic group. [11, 12]
More important, while the adverse effect that forward head posture has on the nervous system was supported by several studies, [13–15] there is a limited amount of literature and overall lack of controlled studies evaluating the effect of forward head posture correction in cervical nerve root function.
Specifically, despite the widespread inclusion of postural correction in therapeutic interventions, 16 there are limited experimental data to support its effectiveness. Accordingly, the purpose of this study was to investigate the effect of forward head posture correction on nerve root function and pain in cases of lower cervical spondylotic radiculopathy. In the current study we used a combination of strengthening, stretching, and behavioural/biofeedback training to correct the abnormal forward head posture as supported by Harman et al. [17] The highly reliable craniovertebral angle was used to assess the forward head position. [18] For measuring the nerve root function, we used dermatomal somatosensory evoked potential to minimize the inherent problems associated with mixed nerve stimulation as in F wave or mixed nerve somatosensory-evoked potentials. Moreover, it provides reliable information about segmental nerve root function that corresponds to clinical symptoms more closely than did the other electrophysiological examinations. [19, 20]
Methods
A prospective, randomized, controlled study was conducted in the research laboratory of our university. All the patients were conveniently selected from our institution’s outpatient clinic. They participated in the study after signing an informed consent form prior to data collection. Recruitment began after approval was obtained from the local institutional review board. Patients were recruited from September 2009 to July 2010 with six months of follow-up. They were screened prior to inclusion by measuring the craniovertebral angle, if the angle was less than 50°, then a participant was referred to the study (selection of 50° as a reference angle was guided by the study of Yib et al. [21] who reported 55:02±2:86 as a normal range and, as it well known, subjects with forward head had a significant smaller craniovertebral angle when compared with normal subjects [21, 22]). Patients were included if they had unilateral radiculopathy due to spondylotic changes of the lower cervical spine (C5–C6 and C6–C7), side-to-side amplitude differences of 50% or more in dermatomal somatosensory-evoked potentials measurement, duration of symptoms was more than three months to avoid acute stage of inflammation. Exclusion criteria included spinal canal stenosis, rheumatoid arthritis and vestibulobasilar insufficiency.
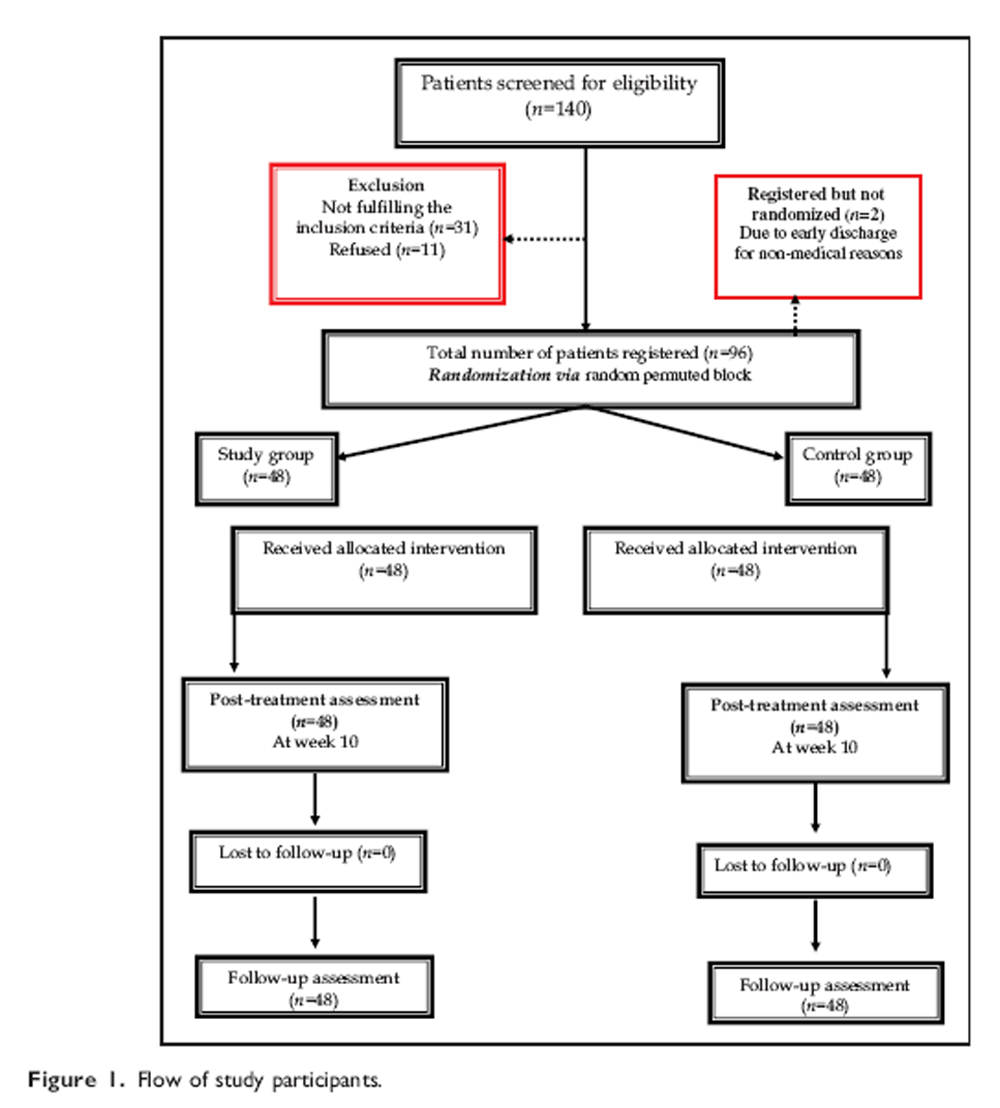
Figure 1 Patients were randomly assigned into two groups of equal number using the roll of a dice, an exercise group (odd number) and a control group (even number). Random permuted size 4 blocks were employed to achieve a balance of the sample sizes between the two groups. A resident who was blinded to the research protocol and was not otherwise involved in the trial, operated the random assignment. A diagram of patients’ retention and randomization throughout the study is shown in Figure 1. The figure shows that 140 patients were initially screened, after the screening process 98 were eligible to participate in, and 96 completed, the study.
Patients in both the experimental (n = 48) and the control group (n = 48) received superficial heat in the form of infrared radiation on the neck for 10 minutes followed by continuous ultrasound application on upper trapezius, for 10 minutes with 1.5 w/cm2 intensity. This conventional treatment was to be repeated three times per week for 10 weeks. [23] Those in the control group received this conventional treatment only. The exercise group additionally received a posture corrective exercise programme in the form of two strengthening (deep cervical flexors and shoulder retractors) and two stretching (cervical extensors and pectoral muscles) exercises. The exercise programme was done according to Harman et al.’s protocol [17] and based on Kendall et al.’s approach. [24] It involved:
Strengthening deep cervical flexors through chin tucks in supine lying with the head in contact with the floor, the progression of this exercise was to lift the head off the floor in a tucked position and hold it for varying lengths of time (this was to progress by twosecond holds starting at two seconds i.e. 2, 4, 6, and 8 seconds).
Stretching cervical extensors through a chin drop while sitting (the progression of this exercise was to drop the chin with hand assistance).
Strengthen shoulder retractors first while standing using a theraband by pulling the shoulder back. The patient was asked to pinch scapulae together without elevation or extension in the shoulder holding this position for at least six seconds then relaxing. The first progression was by conducting the shoulder retraction from a prone position by using weights. The second progression was through using elastics resistance and weights. Participants performed each progression for two weeks. At the consultation, if they could complete three sets of 12 repetitions correctly for the strengthening, they were progressed to the second progression.
Unilateral and bilateral pectoralis stretches alternating each two-week period. For bilateral pectoralis stretching, the patient was seated comfortably with their hand behind their head, from this position, the patient’s elbow was moved up and out to the end of the available range. For unilateral stretching, the arm on the involved site was moved into abduction and external rotation. To stretch the costal division, the ram should be elevated to approximately 135 degrees. For sternal division, the arm abducted to 90 degrees. For clavicular division, the arm was rested at the side.
Participants were instructed to complete three sets of 12 repetitions of the strengthening exercises and three stretching exercises held for 30 seconds each. This exercise programme was to be repeated four times per week for 10 weeks. Patients in both groups were instructed to avoid any other exercise programmes that could interfere with the results. The therapist telephoned the patients weekly to supervise and guide them.
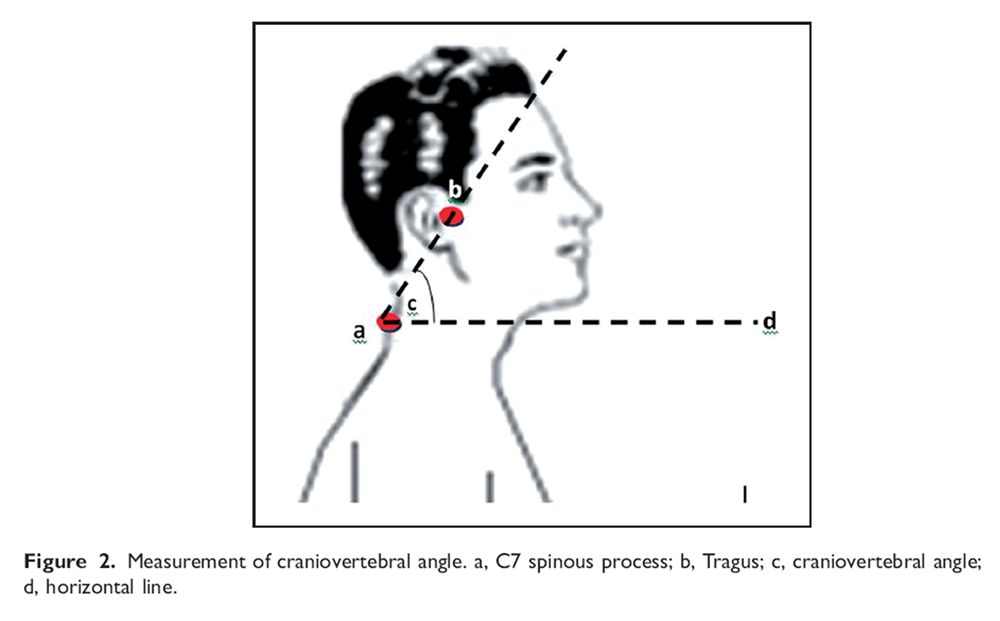
Figure 2 The main outcome measurement used to assess the forward head posture was the craniovertebral angle which was considered to be a valid and reliable assessment tool. [19] All the measurement procedures were done following Falla et al.’s protocol. [22] The craniovertebral angle was measured by taking a lateral photograph. The patients were asked to sit on a chair as usual and a lateral photograph was taken. A digital camera was positioned on a tripod at a distance of 0.8 m from the subject. The axis of the lens of the camera was placed orthogonal to the sagittal plane of the patient at a height that corresponded with the seventh cervical vertebra. Adhesive markers were fixed on the tragus of the ear and the spinous processes of the seventh cervical vertebra. The head forward angle was measured as an angle between a line drawn from the tragus of the ear to the seventh cervical vertebra and horizontal line (Figure 2).
The main outcome measurement used to assess the nerve root function was the peakto- peak amplitude of dermatomal somatosensory evoked potentials. An electromyogram device (Tonneis neuroscren plus version 1.59, Germany) was used to measure this variable for all patients before starting the treatment, at the end of 10 weeks, and at follow-up period of six months. All testing procedures were done following Liguori et al.’s protocol. [20] The patient was lying supine on a softly padded table with a pillow under the head and the knees. After the skin was abraded and cleaned with alcohol, the stimulating electrodes were placed overlying dermatomes of C6 about 7 cm above the styloid process of the radius and C7 between the second and the third metacarpal bones. A bipolar electrode was used for stimulation with an interelectrode distance of 2.5 cm with the stimulation cathode placed proximally.
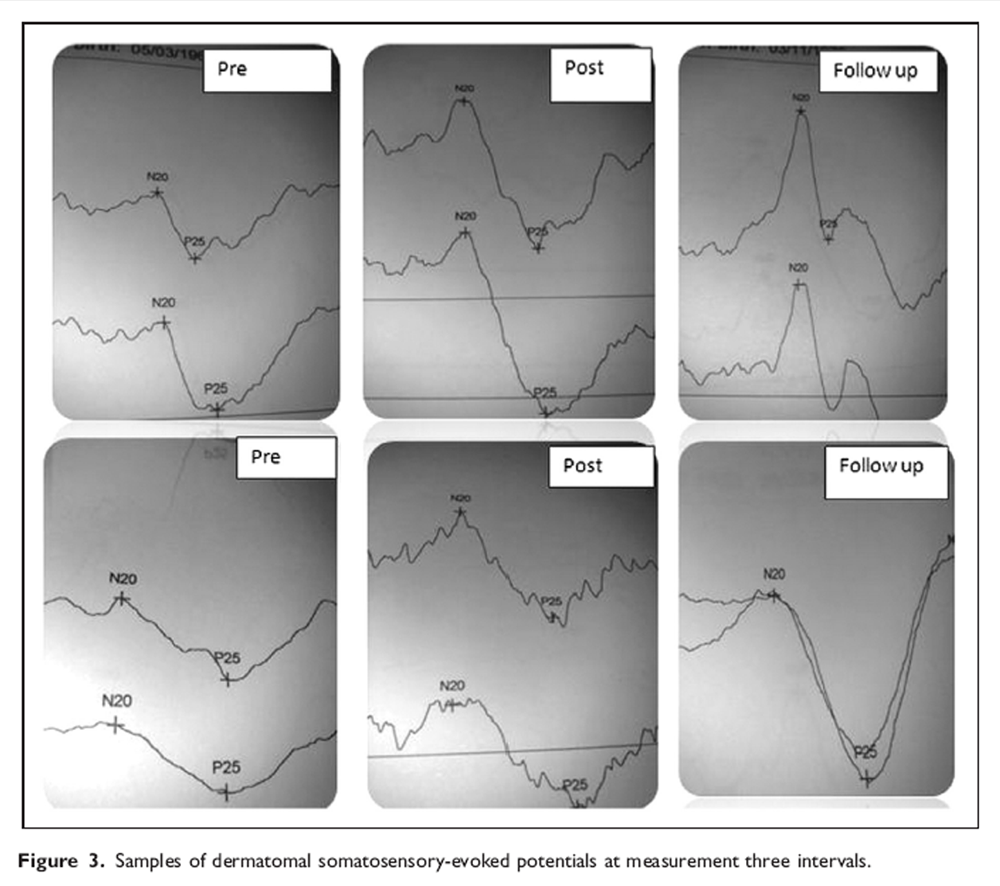
Figure 3 The sensory threshold for the electrical stimulation was determined by increasing the intensity of electrical current until the patient reported its sensation. Tolerable and painless stimulus intensity was usually set at 2.5 times above this level. Stimulation was accomplished with a constant current square wave pulse, 0.2 ms duration, delivered at 3.1 Hz, 200 sweeps preadjusted. Recoding was made with 9-mm diameter tin/lead electrodes affixed with electrolyte paste to abraded skin. The recording electrodes were placed at C3' and C4' (between C3 and P3 and C4 and P4 of the international electroencephalogram 10–20 system), while the reference electrode was placed at Fz and the ground electrode at Fpz. The cortical responses were amplified, average and displayed using an analysis time of 50 ms. A filters setting of 2 Hz to 1KHz was used. After the stimulation was performed and traces were superimposed to ensure reproducibility, negative near field potentials were detected to measure the peakto- peak amplitude. A representative example of dermatomal somatosensory evoked potentials at three intervals of measurement is given graphically in Figure 3.
Measurement of pain was performed by using a visual analogue scale (VAS). It is a responsive pain scale that yields reliable and valid data. [25] The patients were asked about the perception of pain using a 10-cm line with 0 (no pain) on one end and 10 (worst pain) on the other. Patients were asked to place a mark along the line to denote their level of pain. The outcome assessor, who also applied the treatment intervention programmes, was not masked during the study.
Sample size determination
To determine the required number of samples in this study, estimates of mean difference and standard deviation for craniovertebral angle were collected from a pilot study consisting of 10 patients who received the same programme between 1 January 2009 and 30 June 2009. The mean difference value and standard deviation were estimated as 4.1 and 4.3, respectively, a two-tailed test, an alpha level of 0.05, and a desired power of 90%. These assumptions generated a sample size of 29 patients per each group. To account for high drop-out rates, the sample size was increased by 40%.
Data analysis
Both the mean and standard deviation were calculated for each variable. The differences in the baseline data between the exercise and control group were analysed using t-test for the continuous variables and Chi-square test for the categorical variables. To compare the exercise group and the control group, analysis of covariance (ANCOVA) at two follow-up points (after 10 weeks of treatment and at follow-up of six months) was performed for craniovertebral angle, pain, peak-to-peak amplitude of dermatomal somatosensory-evoked potentials. The outcome variables were continuous and all settings/ circumstances were normally distributed. The baseline value of the outcome as covariates was used to assess between group differences. (Baseline outcome in the model = baseline value – overall mean baseline value). For all statistical tests the level of significance was set at P<0.05. SPSS (version 10) was used in this study.
Results
Baseline and demographic data

Table 1 The clinical and demographic features of the patients at inception are presented in Table 1. The exercise and control groups were similar with regard to age, height, weight, gender, smoking, history of neck pain, and past use of physiotherapy. The study specific measurements (C6 and C7 amplitude of dermatomal somatosensory- evoked potentials, pain and craniovertebral angle) were also well balanced between the groups at baseline (P = 0.85, P = 0.9, P = 0.87 and P = 0.37, respectively).
Between groups analysis

Table 2 Results are summarized and presented as mean (SD) in Table 2. After 10 weeks of treatment, the analysis of covariance (ANCOVA) revealed a significant difference between the exercise and control groups adjusted to baseline value of outcome for all measured variables; craniovertebral angle, pain, C6 and C7 peak-to-peak amplitude of dermatomal somatosensoryevoked potentials where the (F = 47.5, P = 0.000), (F = 6.5, P = 0.01), (F = 39.2, P = 0.000), (F = 13.6, P = 0.001) for all previous variables respectively. At six-month follow-up, the analysis showed that there were still significant differences between the study and control groups where (F = 23.1, P = 0.000), (F = 22.4, P = 0.000), (F = 71.5, P = 0.000), (F = 48.8, P = 0.000) for all the variables respectively.
Discussion
This study demonstrates that 10 weeks of a posture corrective exercise programme in addition to ultrasound and infrared radiation decrease the pain intensity and increase the craniovertebral angle and peak-to-peak amplitude of dermatomal somatosensory-evoked potentials for C6 and C7 levels in patients with cervical spondylotic radiculopathy. The changes in the study group were significantly greater than any changes in the control group which received infrared radiation and therapeutic ultrasound only. Furthermore, after six months, these significant changes were maintained.
However, our analysis has some potential limitations, each of which points toward directions of future study. The primary limitation was the lack of investigator blinding. In addition, the sample was a convenient sample rather than a random sample of the whole population. Furthermore, we did not use functional outcome measures since we were primarily interested in assessing the subjective pain experience alone. Despite the limitations, the present randomized, controlled study indicates that correction of biomechanical dysfunction, especially in terms of forward head posture, is essential in management of cervical spondylotic radiculopathy.
The improvement in the forward head posture recorded by the exercise group is similar to those reported in other studies which showed the effectiveness of the exercise programme in reducing this abnormal posture. [17, 26] Correction of forward head posture in the current study may be achieved by restoring the normal muscle balance through strengthening the week muscles and stretching the tight muscles. This concept was further supported by many studies which reported the muscle imbalance represented in weakness in the deep cervical short flexor muscles and mid-thoracic scapular retractors (i.e. rhomboids, serratus anterior, middle and lower fibres of the trapezius) and shortening of the opposing cervical extensors and pectoralis muscles as etiological factor for this abnormal posture. [27, 28]
It may be that improving forward head posture attributed to pain relief by the traditional treatment in the form of ultrasound and infrared radiation. However, we found no statistically significant differences in the control group which was subjected to traditional treatment only.
The second outcome assessment that has been studied in the present study was the pain. Overall, our findings are consistent with many studies which investigated the association between forward head posture and neck pain, concluded that individuals experiencing pain demonstrated a more severe forward head posture than those who did not experience pain. [11, 12, 29] In contrast, the findings of the present study stand in contrast to other studies. In particular, Willford et al. [30] found that there was no significant difference in the forward head posture between groups of subjects with different levels of neck pain. In addition, Hanten et al. [31] found that the resting head posture was not significantly different between patients and the normal population. These findings were further supported by a systematic review conducted by Silva et al. [9] who found that eight out of the 11 studies demonstrated a lack of association between forward head posture and pain. Similarly, Straker et al. [10] found no difference between the neck posture of adolescents with prolonged neck pain and symptom-free adolescents.
The discrepancy and conflict found in the results obtained by the previous studies cannot be directly compared with the current study. All of these studies, for example, were correlational studies and not true experimental studies which look for a degree of association between variables without the ability to ascribe cause and effect. The previous studies which investigated the relationship between head posture and pain have also identified subjects with neck pain retrospectively, or have included heterogeneous sample.
In the control group, while there was a significant decrease in post-treatment VAS scores, the follow-up measures revealed a significant increase in the VAS scores towards initial baseline values. The temporal reduction of pain came in agreement with many studies which reported the beneficial effects of infrared radiation and therapeutic ultrasound in management of pain. [32, 33] However, the sustained postural imbalance represented in forward head posture may be directly or indirectly responsible for recurrence of cervical pain. [34] This highlights the importance of our current results, which indicate that the structural rehabilitation is mandatory if we seek long-lasting effects.
Concerning the peak-to-peak amplitude of dermatomal somatosensory-evoked potentials, to the best of our knowledge, this is the first study to explicitly examine the relationship between forward head posture and nerve root function in detail. Forward head posture is most often described as excessive anterior positioning of the head, involving extension of upper cervical and flexion of lower cervical spine. [35]
Mechanically, it seems logical and is generally admitted that ventroflexion, especially for lower cervical spine, is more beneficial in improving the nerve root function. This opinion is further supported by many studies which reported that flexion of lower cervical spine will improve the nerve root function through increasing the foraminal volume and area at the foraminal isthmus. [36, 37] In contrast to the previous mechanical principles, the present study revealed remarkable improvement in dermatomal somatosensory- evoked potentials following forward head correction and consequently decreased the flexion posture of lower cervical spine.
Restoring the normal mechanics for the nervous system is the likely explanation for significant improvement in amplitude of dermatomal somatosensory-evoked potentials. This concept is supported largely by Harrison et al. [15] who reported that flexion of any part of the spinal column will induce abnormal stresses in the entire cord and nervous system while the extension position will minimize these stresses. This explanation make sense and agrees with Schnebel et al. [38] who investigated the role of spinal flexion and extension in changing nerve root compression and showed that the amount of compressive force and tension in the nerve root increased with flexion of the spine and decreased with extension of the spine.
Additionally, The relevance of lower cervical flexion posture to nerve root function has been questioned by Albert et al. [39] and Brian et al. [40] who reported a non-significant association between foraminal height and foraminal area and relief of clinical symptoms in cases of cervical radiculopathy, which support the role of nervous system biomechanics in cervical rehabilitation as reported by Brieg. [13]
The unique contribution of our study is that it evaluated the independent effect of structural rehabilitation in the form of forward head correction on long-term neural function, which, to our knowledge, has not been previously reported. In conclusion, the effectiveness of forward head correction in reducing pain and improving the nerve root function in cases of cervical spondylotic radiculopathy introduces yet another treatment option to a list that already includes physical agent modalities and manual therapies such as massage and myofascial stretch. Its unique appeal lies in its long-lasting effect.
Clinical messages
Posture corrective exercise programme in the form of stretching and strengthening exercises is beneficial in correcting the forward head posture in cervical sondylotic patients.
Correction of forward head posture is essential in the management of cervical spondylotic radiculopathy.
All of the improvements were still present six months after termination of treatment.
Acknowledgement
The authors express their sincere gratitude to all the patients who kindly participated in the study. They are grateful to the management and staff of El-Farouk Hospital, Cairo, Egypt, for supporting this trial.
Competing interests
None
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References:
Stephen J, Troyanovich SJ, Harrison DE, Harrison DD.
Structural Rehabilitation of the Spine and Posture:
Rationale for Treatment Beyond the Resolution of Symptoms
J Manipulative Physiol Ther 1998 (Jan); 21 (1): 37–50Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA.
Incidence of Common Postural Abnormalities in the Cervical, Shoulder, and Thoracic Regions
and their Association with Pain in Two Age Groups of Healthy Subjects
Phys Ther 1992 (Jun); 72 (6): 425–431Fernandez-de-las-Peñas C, Cuadrado ML, Pareja JA.
Myofascial Trigger Points, Neck Mobility, and Forward Head Posture
in Episodic Tension-Type Headache
Headache 2007 (May); 47 (5): 662—672Cimbiz A, Beydemir F, Manisaligil U.
Evaluation of trigger points in young subjects.
J Musculoskelet Pain 2006; 14: 27–35Weon JH, Oh JS, Cynn HS, et al.
Influence of Forward Head Posture on Scapular Upward Rotators During Isometric Shoulder Flexion
J Bodyw Mov Ther. 2010 (Oct); 14 (4): 367—374Evcik D, Aksoy O.
Relationship between head posture and temporomandibular dysfunction syndrome
J Musculoskelet Pain 2004; 12: 19–24Weigand R, Kettner NW, Brahee D, Marquina N.
Cervical Spine Geometry Correlated to Cervical Degenerative Disease in a Symptomatic Group
J Manipulative Physiol Ther 2003 (Jul); 26 (6): 341–346Harrison DE, Jones EW, Janik TJ, Harrison DD.
Evaluation of the axial and flexural stresses in the vertebral body cortex and trabecular bone
in lordosis and two sagittal cervical translation configurations with an elliptical shell model.
J Manipulative Physiol Ther 2002; 25: 391–401Silva A, Sharples P, Johnson M.
Studies comparing surrogate measures for head posture in individual with and without neck pain.
Phys Ther Rev 2010; 15: 12–22Straker L, O’Sullivan P, Smith A, Perry M.
Relationship between prolonged neck/shoulder pain and sitting spinal posture in male and female adolescents.
Man Ther 2009; 14: 321–329Lau K, Cheung K, Chan K, et al.
Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain,
neck pain severity and disability.
Man Ther 2010; 15: 457–462Silva A, Punt T, Sharples P, Vilas-Boas JP, Johnson M.
Head posture and neck pain of chronic non traumatic origin:
A comparison between patients and pain-free persons.
Arch Phys Med Rehabil 2009; 90: 669–674Breig A.
Adverse mechanical tension in the central nervous system.
Analysis of cause and effect. Relief by functional neurosurgery.
New York: John Wiley and Sons, 1978Harriosn DE, Gailliet R, Harriosn DD, Troyanovich SJ, Harriosn SO.
A review of biomechanics of the central nervous system: Part I:
spinal canal deformation from changes in posture.
J Manipulative Physiol Ther 1999; 22: 227–234Harrison DE, Cailliet R, Harrison DD, Troyanovich SJ, Harrison SO.
A review of biomechanics of the central nervous system-part II:
spinal cord strains from postural loads.
J Manipulative Physiol Ther 1999; 22: 322–332Morningstar MW, Strauchman MN, Weeks DA.
Spinal manipulation and anterior headweighting for the correction of forward head posture
and cervical hypolordosis: a pilot study.
J Chiropr Med 2003; 2: 51–54Harman K, Hubley-Kozey C, Butler H.
Effectiveness of an exercise program to improve forward head posture in normal adults:
a randomized, controlled 10-week trial.
J Man Manip Ther 2005; 13: 163–176Niekerk S, Louw Q, Vaughan C, Grimmer-Somers K, Schreve K.
Photographic measurement of upper-body sitting posture of high school students: a reliability and validity study.
BMC Musculoskelet Disord 2008; 9: 113Talavera-Carbajal MR, Estañol-Vidal B, López-Lomelí MM, et al.
Monitoring dermatomal somatosensory evoked potentials at the ERB point, the cervical spinal cord
and the cerebral cortex in the diagnosis of cervical radiculopathy.
Rev Neurol 2003; 36: 917–924Liguori R, Taher G, Trojaborg W.
Somatosensory evoked potentials from cervical and lumbosacral dermatomes.
Acta Neurologica Scandinavica 1991; 84: 161–166Yip CHT, Chiu TTW, Poon ATK.
The Relationship Between Head Posture and Severity and Disability of Patients With Neck Pain
Manual Therapy 2008 (May); 13 (2): 148—154Falla D, Jull GA, Russell T, Vicenzino B, Hodges P.
Effect of neck exercise on sitting posture in patients with chronic neck pain.
Phys Ther 2007; 87: 408–417Robertson V, Ward A, Low J, Reed A.
Electrotherapy explained, principles and practice, 4th edn.
Berlin: Butterworth-Heinemann, 2006Kendall FP, McCreary EK, Provance PG, et al.
Muscles: testing and function, with posture and pain, 5th edn.
Baltimore, MD: Lippincott Williams & Wilkins, 2005Strand LI, Moe-Nilssen R, Ljunggren AE.
Back performance scale for the assessment of mobility-related activities in people with back pain.
Phys Ther 2002; 82: 1213–1223Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D.
The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers.
Br J Sports Med 2010; 44: 376–381Moore MK.
Upper Crossed Syndrome and Its Relationship to Cervicogenic Headache
J Manipulative Physiol Ther 2004 (Jul); 27 (6): 414—420Valli J.
Chiropractic management of A 46-year old type 1 diabetic patient with upper crossed syndrome
and adhesive capsulitis.
J Chiropr Med 2004; 3: 138–144Chiu TT, Ku WY, Lee MH, et al.
A Study on the Prevalence of and Risk Factors for Neck Pain Among
University Academic Staff in Hong Kong
J Occup Rehabil 2002 (Jun); 12 (2): 77–91Willford CH, Kisner C, Glenn TM, Sachs L.
The interaction of wearing multifocal lenses with head posture and pain.
J Orthop Sports Phys Ther 1996; 23: 194–199Hanten WP, Olson SL, Russell JL, Lucio RM, Campbell AH.
Total excursion and resting head posture: normal and patient comparisons.
Arch Phys Med Rehabil 2000; 81: 62–66Moodley M, Brantingham JW.
The relative effectiveness of spinal manipulation and ultrasound in mechanical pain: Pilot study.
J Chiropr Med 2002; 1: 184–188Srbely JZ, Dickey JP.
Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity:
novel applications in myofascial therapy?
Clin Rehabil 2007; 21: 411–417Hiemeyer K, Lutz R, Menninger H.
Dependence of tender points upon posture: a key to the understanding of fibromyalagia syndrome.
J Man Med 1990; 5: 169?74McKenzie R.
Treat your own neck.
Raumati Beach, New Zealand:
Spinal Publications, 2006Humphreys SC, Chase J, Patwardhan A, et al.
Flexion and traction effect on C5-C6 foraminal space.
Arch Phys Med Rehabil 1998; 79: 1105–1109Wainner RS, Gill H.
Diagnosis and non operative management of cervical radiculopathy.
J Orthop Sports Phys Ther 2000; 64: 64–70Schnebel BE, Watkins RG, Dillin W.
The role of spinal flexion and extension in changing nerve root compression in disc herniations.
Spine 1989; 14: 835–837Albert TJ, Smith A, Bresseler E.
An in vivo analysis of the dimensional changes of the neuroforamen after anterior cervical diskectomy and fusion: a radiologic investigation.
J Spinal Disord 1997; 10: 229–233Brian K, David HK, Andrea M, Louis GJ.
Outcomes following anterior cervical discectomy and fusion: The role of interbody disc height, angulation, and spinous process distance.
J Spinal Disord Tech 2005; 18: 304–308
Return to RADICULOPATHY
Return to FORWARD HEAD POSTURE
Since 9-25-2011


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |