

|
Inequality of Muscle Balance Abnormal Structural Support Stress Factors Resulting in Subluxation Indicative Criteria Classification of Selected Causes of Spinal Pain Vertebral Causes of Spinal Pain Disorders Simulating Spinal Pain Precipitating Factors of Spinal Subluxations Effects of Spinal Subluxations Structural Alterations Events at the Intervertebral Foramen Distal Neurologic Manifestations Spinosomatic, Spinovisceral, and Viscerospinal Syndromes Basic Clinical Considerations Potential and Scope of Reactions The Neurodystrophic ProcessesChapter 18
Basic Spinal Subluxation Considerations
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Chiropractic Management of Sports and Recreational Injuries”
Second Edition ~ Wiliams & Wilkins
The following materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated
to chiropractic research. Please review the complete list of available books.
Spinal Biomechanics The Vertebral Motor Unit Normal and Abnormal Vertebral Movements Motor-Unit Classification of Subluxations Static Intersegmental Subluxations Kinetic Intersegmental Subluxations Mechanics Involved in the Spinal Examination Spinal Motions Motion Barriers Evaluating Joint Motion and Strength Precipitating Factors of Spinal Subluxations
Chapter 18: Basic Spinal Subluxation Considerations
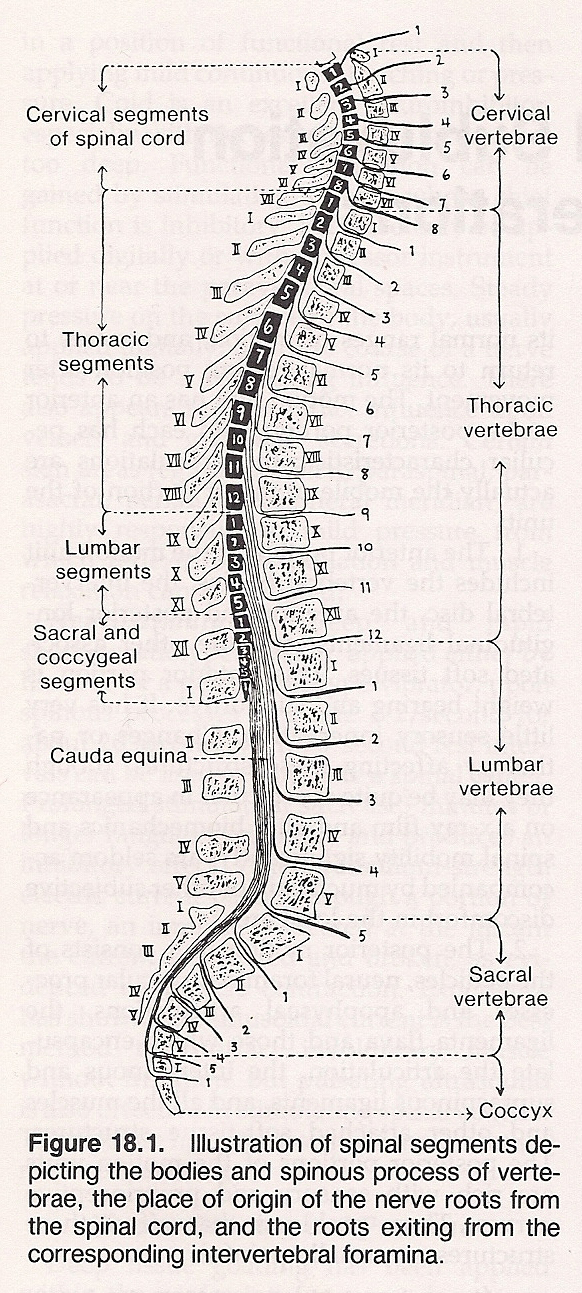
While the erect spinal column is a concern in static postural equilibrium, it is never actually in a static state in life. It is alternately changing from a state of "quiet dynamics" in the static postural attitude to a state of "active dynamics" in movement. These kinetic aspects of normal spinal biomechanics are an important consideration since the totality of spinal function is the sum of its individual component parts. The anterior portion of the motor unit includes the vertebral bodies, the intervertebral disc, the anterior and posterior longitudinal ligaments, and the other associated soft tissues. This anterior portion is weight bearing and supportive. It has very little sensory innervation. Changes or pathology affecting these structures, though they may be quite spectacular in appearance on a x-ray film and alter biomechanics and spinal mobility significantly, are seldom accompanied by much pain or other subjective discomfort in the local area.
The posterior motor unit consists of the pedicles, neural foramina, articular processes and apophyseal articulations, the ligamenta flava and those which encapsulate the articulation, the interspinous and supraspinous ligaments, and all the muscles and other attached soft-tissue structures. The posterior portions of the motor units are rich with sensory and proprioceptive nerves. Thus, problems that affect these structures are usually painful.
Abnormal spinal biomechanics primarily relate to the intervertebral subluxation and other spinal "dysarthrias" which result in structural and functional inadequacies of the spinal column. This state is the condition of a vertebral motor unit which has lost its normal structural and/or functional integrity and is, therefore, unable to move from its normal resting position, unable to move properly through its normal range of motion, or unable to return to its normal resting position after movement. One should avoid the tendency to speak of a subluxated vertebrae when in fact it is solely the articulations that subluxate.
Flexion Subluxation. This is characterized by approximation of the vertebral bodies at the anterior and by separation of the vertebral bodies, facets, and spinous processes at the posterior. When found, it is indicative of irritative microtrauma to the anterior intervertebral foramen (IVF); forced excursion of the nucleous pulposis and bulging of annular fibers; stretching of the posterior longitudinal, interspinal, and supraspinal ligaments; traction shearing stress of the synovia of the facet articulations; and biomechanical impropriety of the motor unit.
Lateral Flexion Subluxation. This is characterized by approximation of the vertebral bodies and facets on the side of flexion and separation of the vertebral bodies and facets on the side of extension. This type of subluxation is suspicious of irritative microtrauma to the intervertebral disc (IVD) on the side of flexion, imbrication of the facets and compressive shearing stress to the synovia on the side of flexion, forced excursion of the nucleous pulposis with bulging of the annular fibers, stretching of the anterior longitudinal ligament at its lateral aspect, and biomechanical impropriety of the vertebral motor unit.
Anterolisthesis Subluxation with Spondylolysis. This is featured by anterior excursion of the vertebral body independent of the posterior division of the motor unit. The posterior division of the unit remains in position with the structure below because of separation of the pars. It is characterized by irritative microtrauma to the posterior aspect of the IVD, forced excursion of the nucleous pulposis with buldging of the annular fibers, forward shearing stress to the annular fibers, stretching of the anterior longitudinal ligament, and biomechanical insult of the vertebral motor unit.
Laterolisthesis Subluxation. This is characterized by lateral, superior, and posterior excursion of the vertebral body on the side of deviation and by separation of the facets on the side of deviation with reverse torsion and approximation on the side opposite deviation. This suggests irritative microtrauma to the IVD on the side opposite deviation, lateral and posterior shearing stress to the annular fibers on the side of deviation, imbrication of facets and anterior shearing of the synovia on the side opposite deviation, and biomechanical insult to the vertebral motor unit.
Increased Interosseous Space Subluxation. This is characterized by superior excursion of the vertebral body and the facets. It results in inflammatory swelling or pathologic enlargement of the IVD, traction shearing stress to the annular fibers of the IVD and the synovia of the facet articulations, stretching of the anterior and posterior longitudinal ligaments, and biomechanical insult to the vertebral motor unit.
Hypomobility and/or Fixation Subluxation. This common subluxation is characterized by fixation of the vertebral motor unit in relation to the supporting structure below and compensatory hypermobility of the vertebral motor unit above the level of fixation. It is associated with irritative excessive function of the hypermobile vertebral motor unit resulting in microtrauma or macrotrauma to the IVD, anterior and posterior longitudinal ligaments, periosteum, etc; muscular irritation, spasticity, muscle trauma, fatigue, etc; neurologic insult within the confines of the neural canal and IVF; vascular insult to the paraspinal and interforaminal blood vessels; and biomechanical impropriety of all vertebral motor units involved.
The direction of vertebral rotation is determined by inspection and dynamic palpation of the transverse processes, with the process being more posterior on the side toward which the vertebrae have rotated. If one or more segments are rotated to one side in the neutral position, lateroflexion will usually be noted to the side opposite the rotation. In spinal flexion, the segment rotated will be side bent to the same side with a loss in its ability to bend forward. Likewise, during spinal extension, the segment is rotated to the same side and is unable to bend backward.
The spinal dysarthric subluxation may be either a cause or an effect, and the immediate causes may be divided into two major categories: the unequal or asymmetrical muscular efforts upon the joint structures and the inequality in the supporting tissues of a particular joint such as the cartilage, intervertebral disc, ligaments, etc. Some form of internal or external stress is necessary to produce a subluxation to a degree sufficient to cause a state of neurodysfunction.
Trauma. Frank trauma may cause inflammation, degeneration, etc, and particularly the muscular splinting reaction that muscles make when their surrounding tissues are injured. This alters the position and motion of the structural tissues that are related. Sustained microtrauma, though of a less acute nature, may cause a slow continual irritation and eventually create degenerative pathologic changes which similarly alter muscular reaction. The obvious trauma of a fall or blow which surprises a joint with the intrinsic muscles unprepared will cause a joint sprain with ligament injury. A sudden slip during a lift is equally damaging to the unprepared or weak joint. Watkins reminds us that the slower trauma of occupational strain is not as easy to visualize. He reminds us of the game of youth in trying to hold an axe at arms length to the side for 1 minute. Within 2 minutes, the shoulder aches but the big "catch" is at the lumbosacral level in following hours and days.
(1) Genetic and developmental abnormalities causing asymmetry of the vertebrae, cartilage, muscular structure, etc.
Stress Factors Resulting in Subluxation
(1) muscle splinting, especially on the side of greatest stimulation according to Fluger's Law or
Fluger's Law states that if a stimulus received by a sensory nerve extends to a motor nerve of the opposite side, contraction occurs only from corresponding muscles; and, if contraction is unequal bilaterally, the stronger contraction always takes place on the side which is stimulated. When affecting one or more vertebrae, this state of decreased mobility of the motor unit encourages nerve dysfunction leading to pathologic processes in the areas supplied by the affected nerve root or neuromere depending upon the degree and chronicity of involvement.
(1) mechanical irritation of the nerve roots, Traumatic: eg, dislocation, fracture, sprain, strain, subluxation.
Infection: eg, brucellosis, Escherichia coli, staphylococcal, tubercular.
Developmental: eg, hypermobility, kyphosis, lordosis, scoliosis, spondylolisthesis, various anomalies.
Degenerative: eg, apophyseal osteoarthritis, cauda equina disorders, degenerative disc lesions, hyperostosis, joint instability, nerve root compression, spinal cord diseases.
Tumor: eg, carcinoma (secondary), myelomatosis.
Inflammatory Arthropathy: eg, ankylosing spondylitis, collagen diseases, fibrositis, focal sepsis, gouty rheumatism, muscular rheumatism, osteochondritis, panniculitis, psoriasis, regional ileitis, Reiter's disease, rheumatoid arthritis, ulcerative colitis.
Metabolic: eg, osteomalacia, osteoporosis.
Systemic: eg, secondary involvement of primary infection and general disease processes such as actinomycosis, alkaptonuria, blood dyscrasias, brucellosis, cancer, gout, influenza, smallpox, typhoid fever.
Idiopathic: eg, Paget's disease, rare bone diseases.
Miscellaneous: eg, psychogenic conversion syndromes; iatrogenic causes such as unskilled or illadvised manipulation, myelography, surgery with subsequent adhesions, and poorly fitted or prolonged use of supports. Cervical Pain: eg, malignant lymphadenopathy, pancoast tumor, subarachnoid hemorrhage, vertebral artery syndrome.
Thoracic Pain: eg, aortic aneurysm, bronchial carcinoma, cardiac enlargement, coronary artery disease, gallbladder disease, herpes zoster, hiatus hernia, lung disease.
Lumbar Pain: eg, aortic obstruction, colon carcinoma, disseminated sclerosis, endometriosis, hip disease, pelvic carcinoma, obstruction of iliac arteries, pancreatic carcinoma, peptic ulcer, rectal carcinoma, renal disease, short leg, spinal cord tumor.
Miscellaneous: eg, visceral diseases causing referred pain to the spine or pressure erosion; central nervous system diseases such as meningitis, poliomyelitis, syringomyelia, tetanus, spinal subarachoid hemorrhage; psycogenic causes; iatrogenic manifestations.
The concept that an "off centered" vertebral or pelvic segment parallels a unique effect upon the neuromuscular bed which may be the cause of, aggravation of, or "triggering" of certain syndromes is a major contribution to the field of functional pathology and clinical biology by the chiropractic profession. This section discusses the basic biomechanics and effects of vertebral subluxations as related to the management of sports-related and recreational injuries.
Spinal Biomechanics
The Vertebral Motor Unit
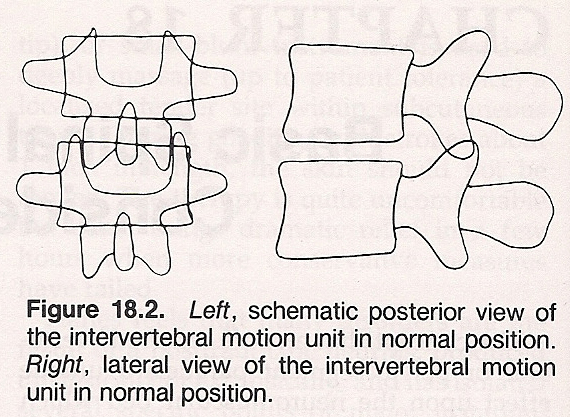
An intervertebral motor unit consists of two vertebrae and their contiguous structures forming a set of articulations at one intervertebral level. Thus, what is called a vertebral "subluxation" in chiropractic is the alteration of the normal dynamics, anatomical or physiological relationships of contiguous articular structures. The components of the spinal column (the vertebral motor units) confer a quality and quantity of motoricity to the relationship of two vertebrae. They are firmly interconnected by the intervertebral disc and restraining ligaments, which are activated by muscles which respond to both sensory and motor stimulation.
The biomechanical efficiency of any one of the 25 vertebral motor units, from atlas to sacrum, can be described as that condition (individually and collectively) in which each gravitationally dependent segment above is free to seek its normal resting position in relation to its supporting structure below, is free to move efficiently through its normal ranges of motion, and is free to return to its normal resting position after movement. The motor unit has an anterior and a posterior portion, and each has peculiar characteristics; the articulations are actually the mobile or motor portion of the unit:
Normal and Abnormal Vertebral Movements
Normal movements of a vertebral segment relative to its supporting structure below may be described by its ability to laterally flex on the coronal plane, rotate on the transverse plane, and anteroflex and retroextend on the sagittal plane. To some extent, all vertebrae are able to function in all three dimensions; however, the magnitude of such movements varies in degree in the lumbar, thoracic, and cervical spinal regions, as well as in the transitional areas.
The degree of derangement of a bony segment within its articular bed may vary from a microtrauma to one that is macroscopic and quite readily discernible. It is always attended to some degree by articular dysfunction, neurological insult, stressed muscles, tendons, and ligaments. Once produced, the lesion becomes a focus of sustained pathological irritation: a barrage of impulses stream into the spinal cord where internuncial neurons receive and relay them to motor pathways. The contraction that provoked the subluxation initially is thereby reinforced, thus perpetuating both the subluxation and the pathological process engendered.
Motor-Unit Classification of Subluxations
There are numerous methods to classify vertebral subluxations. Each has its own rationale and each has had certain validity that has been a contribution to our understanding of this complex phenomenon. The biomechanical element of the vertebral motor unit subluxation is classified by Hildebrandt/Howe in accord with its static or kinetic aspects and in accordance with the number of vertebral motor units involved. Following are the generally accepted characteristics and significance of the classified vertebral motor-unit subluxation-fixations:
Static Intersegmental Subluxations
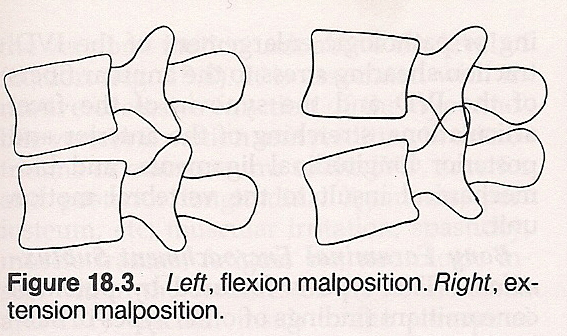
Extension Subluxation. This type of subluxation is featured by separation of the vertebral bodies at the anterior and approximation of the vertebral bodies, facets, and spinous processes at the posterior. Such a subluxation points toward irritative microtrauma at the posterior IVF, forced excusion of the nucleous pulposis and bulging of the annular fibers, stretching of the anterior longitudinal ligament, imbrication of the facet articulations with compressive shearing stress to the synovia of the facet articulations, and biomechanical insult of the vertebral motor unit.
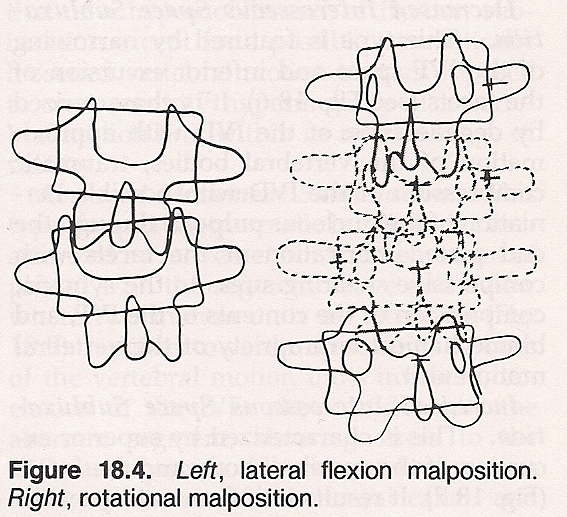
Rotational Subluxation. Such a subluxation is featured by rotatory displacement of the vertebral bodies laterally and posteriorly on the side of rotation with torsion of the facet articulations in the direction opposite to vertebral body rotation. This situation is significant of torsion binding of the annular fibers of the IVD, decreased resiliency of the IVD due to torque compression of the annular fibers, torsion stretching of the anterior and posterior longitudinal ligaments, rotatory imbrication of the facets with reverse shearing stress to the synovia, and biomechanical insult of the vertebral motor unit.
Anterolisthesis Subluxation Without Spondylolysis. This is characterized by an anterior-inferior excursion of the vertebral body at the anterior and by anterior-superior excursion of the vertebral body and facets at the posterior. It points toward irritative microtrauma at the anterior IVD, forward shearing stress to the annular fibers of the IVD, stretching of the anterior and posterior longitudinal ligaments, imbrication of facets with forward shearing stress to the synovia, and biomechanical impropriety of the vertebral motor unit.
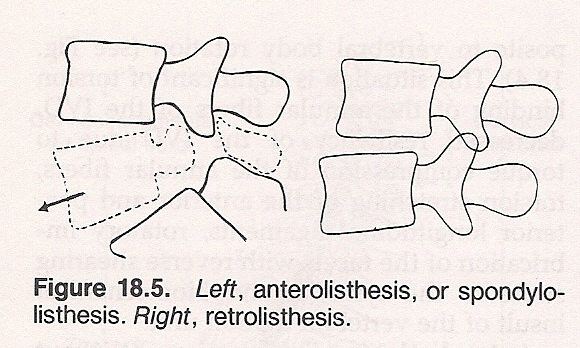
Retrolisthesis Subluxation. Such a subluxation is featured by posterior-inferior excursion of the vertebral body and by posterior-inferior excursion of the facets. This subluxation signifies irritative microtrauma to the posterior IVD, posterior shearing stress of the annular fibers, stretching of the anterior and posterior longitudinal ligaments, imbrication of the facets with posterior shearing stress to the synovia, and biomechanical impropriety of the vertebral motor unit.
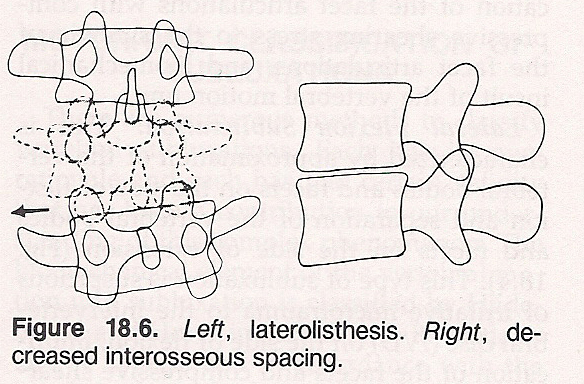
Decreased Interosseous Space Subluxation. This type is featured by narrowing of the IVF space and inferior excursion of the facets. It is characterized by degeneration of the IVD with approximation of the vertebral bodies, traumatic compression of the IVD with possible herniation of the nucleous pulposis through the end plate, imbrication of the facets with compressive shearing stress to the synovia, compression of the contents of the IVF, and biomechanical impropriety of the vertebral motor unit.
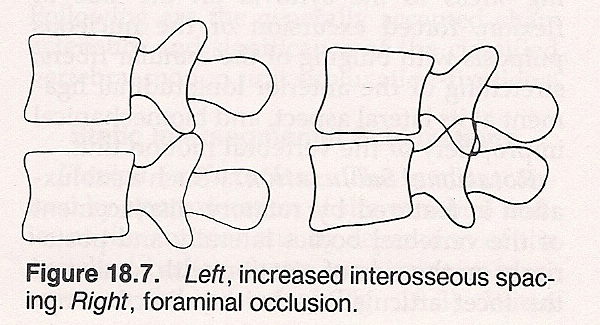
Bony Foraminal Encroachment Subluxation. This type is featured by potential concomittant findings of other types of subluxations with a possible relationship to osteophytic interforaminal spurs in conjunction with other types of subluxations. It features associated microtraumas and macrotraumas to the vertebral motor unit; compression, irritation, and swelling of the foraminal contents; osseous and soft-tissue primary degenerative processes of the vertebral motor-unit structures; and interforaminal neurovascular insult effecting possible disseminated secondary pathophysiologic processes.
Kinetic Intersegmental Subluxations
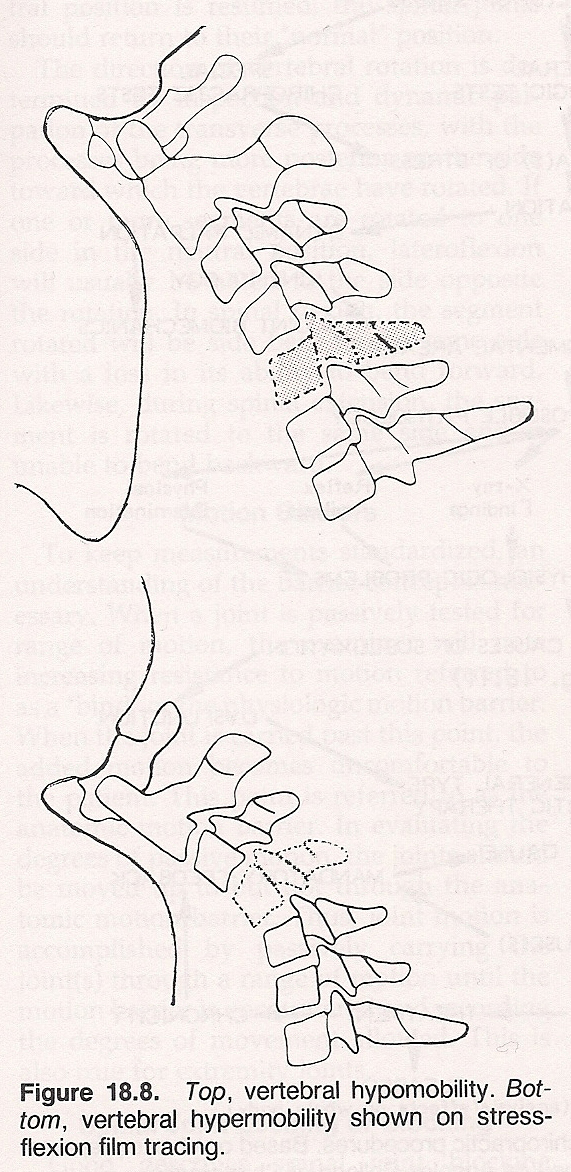
Hypermobility Subluxation. This is featured by a hypermobile vertebral motor unit in relation to a normally functioning or hypomobile motor unit below. It has the same features as that of a hypomobile and/or fixation subluxation except for a possible traumatically loosened vertebral motor unit as opposed to compensatory hypermobility of a vertebral motor unit within its normal range of motion.
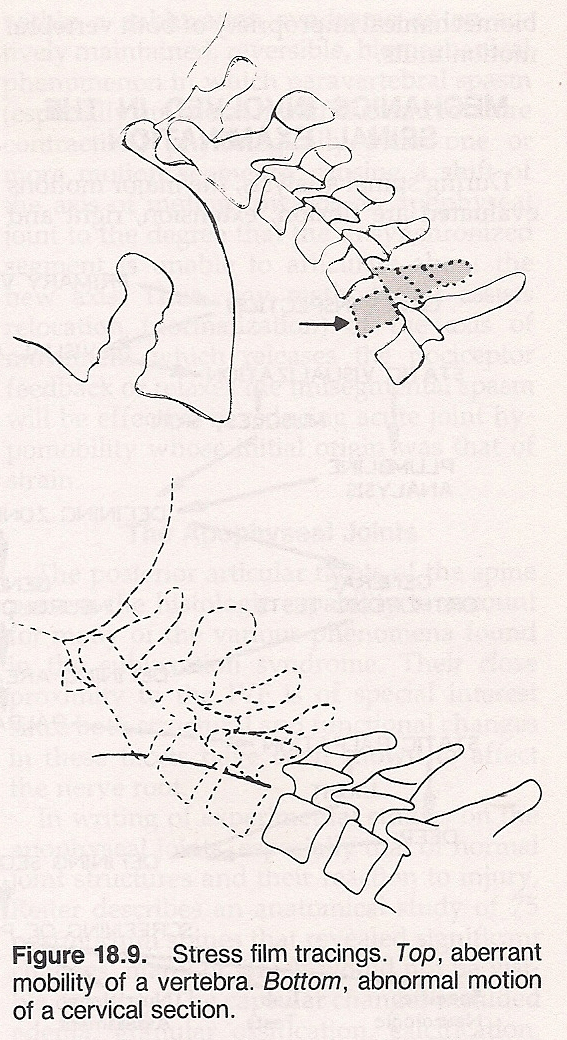
Aberrant Movement Subluxation. This type, frequently traumatic in origin, is characterized by movement of a vertebra "out of phase" with the segment above and below where two motor units are involved. It points toward microtrauma to both of the vertebral motor units involved, occlusion of the IVFs above and below the aberrant segment, shearing stress to the IVDs and synovia of both vertebral motor units, restriction of the neural canal, and biomechanical impropriety of both vertebral motor units.
Mechanics Involved in the Spinal Examination
During spinal analysis, the major motions evaluated are flexion, extension, right and left lateral flexion, and right and left rotation. Motion of a superior segment is described in terms of the segment beneath it. Motion evaluations, however, are just one part of the examination procedures.
A larger scope of chiropractic procedures is roughly charted in Figure 18.10.
Spinal Motions
When the spine is in a neutral standing or sitting position, the anterior surface of a vertebral body will rotate to the side opposite the lateroflexion with the vertebral bodies tending to crawl out from under the load. This pattern of function usually takes place within multiple spinal segments, but dysfunction will occur when ligaments and muscles attached to and affecting the vertebral articulations are shortened or lengthened to effect restricted or excessive motion of one or more segments. The articular facets open during flexion, close during extension, and individual segments rotate and side bend to the same side. When the neutral position is resumed, the spinal joints should return to their "normal" position.
Motion Barriers
To keep measurements standardized, an understanding of the barrier concept is necessary: When a joint is passively tested for range of motion, the examiner will note increasing resistance to motion referred to as a "bind" or the physiologic motion barrier. When the joint is carried past this point, the added motion becomes uncomfortable to the patient. This point is referred to as the anatomic motion barrier. In evaluating the degrees of passive motion, the joints should be moved up to but not through the anatomic motion barrier. Thus, joint motion is accomplished by passively carrying the joint(s) through a range of motion until the motion barrier is encountered and recording the degrees of movement allowed. This is also true for extremity joints.
Spinal Joint Locking or Blocking
Good describes spinal joint blocking within a subluxation syndrome as an actively maintained, reversible, biomechanical phenomenon in which paravertebral spasm (especially unilateral multifidus and rotatore contraction) physiological- ly locks one or more motion segments, causing a shift of the axes of motion towards an apophyseal joint to the degree that the unsynchronized segment is unable to articulate about the new axis. Thus, any method that assists reloca=- tion (normalization) of the axes of movement, which releases the nociceptor feedback, or relaxes the unisegmental spasm will be effective in reducing acute joint hypomobility whose initial origin was that of strain.
The Apophyseal Joints
The posterior articular facets of the spine possess the histological capa- bility to account for many of the various phenomena found in the subluxation syndrome. Their close proximity to the IVF is of special interest since both structural and functional changes in these facets have been shown to affect the nerve root.
In writing of experimental studies on the apophyseal joints, especially that of normal joint structures and their reaction to injury, Reiter describes an anatomical study of 75 postmortum spines that revealed significant changes, many of which would not be visible on x-ray. The capsular changes included edema, granular ossification, calcification, and adhesion between the capsule and the meningeal covering of the nerve root adjacent to it. The intra-articular changes included hypertrophy of the menisci up to four times their normal size, occa=- sional chondrification and ossification of the menisci, detached bodies, ulcera- ted areas of denuded hyaline cartilage, cartilage thinning, fibrillation, and osteophytic marginal proliferation.
Evaluating Joint Motion and Strength
The range of motion for any particular spinal area is usually recorded in degrees by a goniometer with comparable measurement of the opposite side noted. When asymmetry of motion range is observed, the examiner must determine whether the side with the greatest movement is weak or the side with less motion is restricted. Testing the strength of a muscle or group of muscles is made by carrying the joint to the extreme of allowed movement permitted by the antagonist muscles afterwhich the examiner resists an active maximum effort by the patient to contract the muscles being tested. Strength is recorded bilaterally from Grade 5 to Grade 0.
Precipitating Factors of Spinal Subluxations
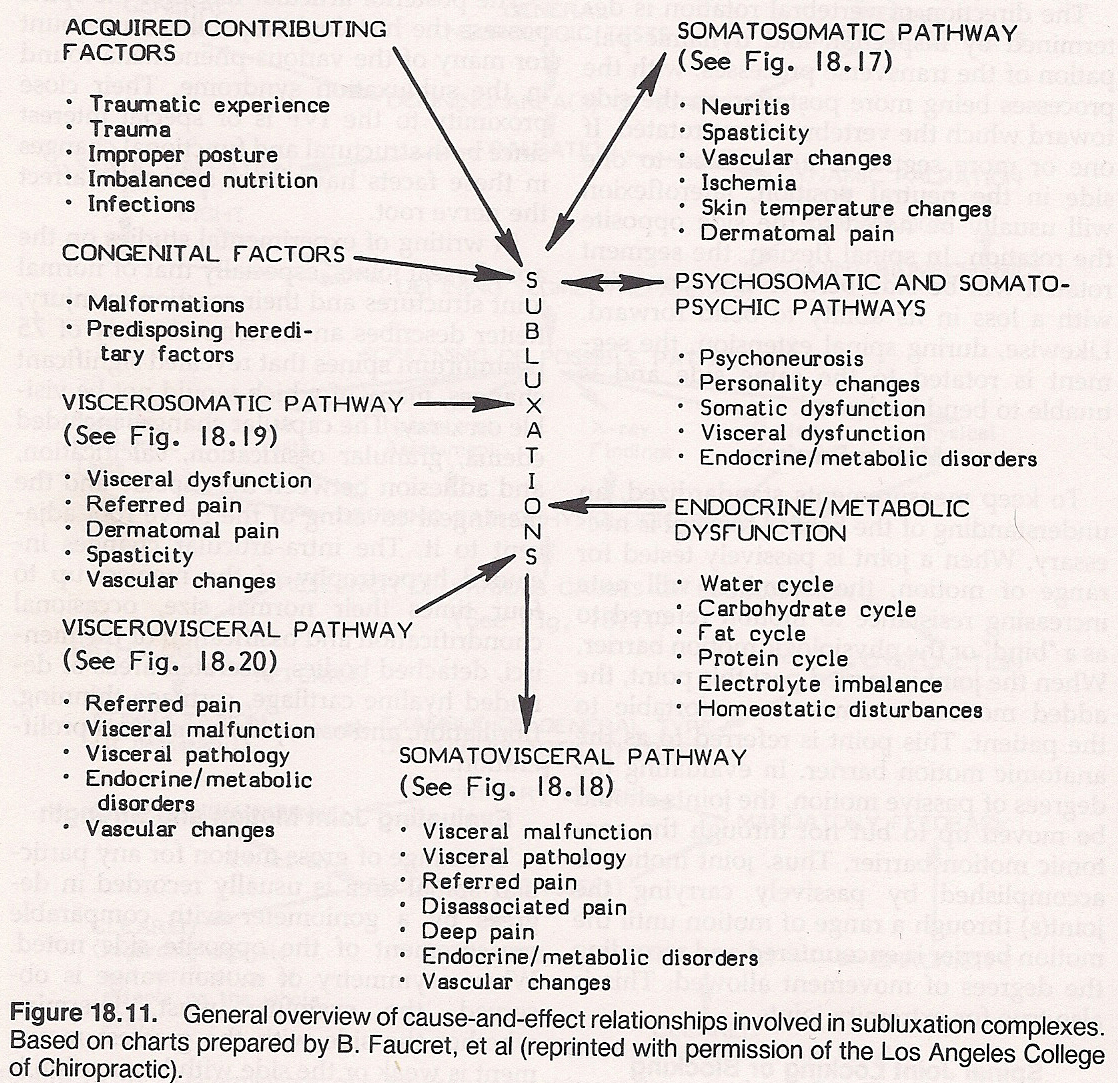
The general cause-and-effect relationships involved in subluxation complexes are shown in Figure 18.11.
Inequality of Muscle Balance
Inequality in muscular balance may be initiated by trauma, postural distortion phenomena, biochemical reactions, psychomotor responses, paralytic affects, somatic and visceral responses.
Postural Distortion Phenomena. Postural compensations for either mechanical activity or structural changes in the skeleton itself are referred to as postural distortion phenomena. These changes, as well as other causes of subluxation, often result in a series or combination of minor mechanical errors which together may be termed scoliosis, kyphosis, lordosis, distortion, or similar terms. Such a distortion phenomenon is dependent upon the ability of the spine to adjust to any interference in the body's vestibular, visual, or proprioceptive adaptation which is incompatible with the normal balance of the musculoskeletal system to gravity. Whether this structural imbalance creates disturbances or appears asymptomatic is dependent upon the neurological irritation developing within the tissues affected. They may not elicit apparent disturbance at a given time; but, rather, at a later date when they overcome the adaptation and resistance of the individual.
Biochemical Reactions. The acute or chronic hypo- or hyper-tonicity of musculature may be due to various biochemical changes within the above-mentioned tissues. This may be brought about by foreign bodies, by either local or general pathologies which may cause anoxia, ischemia, toxicity, etc, or by systemic fatigue-producing activities, nutritional deficiencies or excesses, caustic chemical exposure, ingestion of harmful chemicals, inhalation of noxious gases, microorganism toxins, abnormal glandular activity, excessive heat or cold, or electric shock affecting the chemical environment of cells histologically.
Psychomotor Responses. These responses refer to the reaction of musculature to emotional effects on the nervous system as the body depicts its psychologic stresses. They may be environmentally, socially, or intrinsically initiated.
Paralytic Effects. Primary disease of the neuromuscular system itself (eg, paralytic diseases) affects musculoskeletal tone and strength, thus affecting position and quality of motion.
Somatic and Visceral Responses. These responses refer to the secondary reactions of the muscular system to somatic or visceral sensory irritation which may develop elsewhere in a given neurological segment. Our embryologic nature is such that the various components of a given vertebral segment and its ramifications or neuromere may be influenced by sensory stimuli that arise from any tissue supplied by these components. The somatic or visceral sensory neurons that enter into a given neurological segment and cause somatic or visceral motor response may cause a similar response throughout the various ramifications of that segment. This, of course, depends upon certain states of sensitivity or facilitation, certain convergencies or divergencies within the nervous system, and particularly upon the intensity and duration of the initiating stimulation. Therefore, could well be a visceral sensory irritation in the intestinal tract or other viscus that is causing motor changes not only in the internal organs, but also in the vascularity and the musculature of the body. These changes may result in motor alterations in the tone of muscles, consequently resulting in a spasm or splinting action. If long standing, degenerative changes, atonicities brought about by atrophy, contractures, or other pathologic changes within the musculature may develop which can influence the mechanics of the vertebral segment(s) involved.
Abnormal Structural Support
Mechanical errors in position or motion may also be brought about by structural alterations in the supporting tissues of the joint itself. These in turn may be brought about by:
(2) Various acquired disease processes within the joint such as arthritic degeneration, avascular necrosis, or a neuropathic process that causes the cartilage, bone, ligaments, or musculature to be structurally altered.
(3) The resolution of macro- or micro-traumas, strains, sprains, or of other primary pathology may cause fibrosis, degeneration, or other retrograde changes of a structural nature within the joints themselves.
These same processes not only develop within the vertebral column and its paravertebral tissues but also in the musculoskeletal tissues of the appendicular skeleton. Thus, similar lesions may exist remote from the spine which perpetuate neuropathic responses by their presence. When the cause is within the structures of the vertebral column, the effects are more evident because of the close anatomical proximities and the functional importance of normal motor-unit motion or integrity to the various components of the nervous system.
Depending on the degree of stress produced, any internal or external stress factor involves the nervous system directly or indirectly, resulting in decreased mobility of the vertebra of the involved neuromere. This decreased mobility may be the result of:
(2) from abnormal weight distribution to the superior facets and other structures of the vertebrae involved. , resulting in decreased mobility of the vertebra of the involved neuromere. This decreased mobility may be the result of:
Indicative Criteria
The importance of a subluxation depends on its clinical features and whether the lesion and its neurogenic responses are affecting the health and performance of the individual to a significant degree. Minor mechanical errors in positions and motion occur in all of us as do consequent neurologic irritations from their effects. We are all subject to environmental irritations and respond to them in a manner that creates errors in musculoskeletal symmetry in the body, resulting in errors of position and mechanics of related anatomic structures. These in turn cause or perpetuate neurologic aberrations of motor reflexes. However, these motor responses may be of a temporary nature for the body is capable of correcting minor mechanical faults within its structure. On the otherhand, certain forms of lesions cannot be corrected without proper professional attention. It is not so much the presence of a subluxation that is significant but how it is affecting the total economy of the body and how involved it is in the production of aberrant neurologic responses and the creation of a state of dysfunction. These effects may be determined by a proper diagnosis and spinal analysis.
Classification of Selected Causes of Spinal Pain:
Vertebral Causes of Spinal Pain
Pain can be perceived in the vicinity of the spinal column by a number of factors such as:
(2) mechanical irritation of any of the involved pain-sensitive soft tissues,
(3) edema and vascular distension,
(4) reflex spasm of the paravertebral muscles,
(5) chemical irritation of any of the involved pain-sensitive tissues by the effect of inflammatory exudates,
(6) by referred pain from viscera or distant structures, and
(7) psychic mechanisms.
Typical classes include:
Disorders Simulating Spinal Pain
| CEREBELLAR SYNDROME SIGNS AND PROCEDURES | ||
| Andre-Thomas sign Finger-to-finger test Finger-to-nose test Finger tapping test | Heel-to-knee test Heel-to-toe test Homes' sign Patting test | Pronation-supination test Rebound test Toe-to-finger test |
| CEREBRAL SYNDROME SIGNS AND PROCEDURES | ||
| Adie's sign Baillarger's sign Barany's pointing test Berger's sign Fundi signs | Glabella reflex Grasp reflex Jaw jerk Kleist's sign Macewen's sign | Quinquad's sign Saeneer's sign Setting sun sign |
| CRANIAL NERVE SYNDROME SIGNS AND PROCEDURES | ||
| 1. Olfactory Odor differentiation 2. Optic Consensural reflex Dazzle reflex Field of vision Ophthalmoscopic signs Gunn's sign Pupillary reflex Visual acuity 3. Oculomotor Accommodation reflex Argyll-Robertson's sign Arroyo's sign Ballet's sign Cantelli's sign Consensural reflex Disconjugate gaze Gower's sign Pupillary reflex Red glass test 4. Trochlear Ballet's sign Cantelli's sign Red glass test 5. Trigeminal Bite test Consensural reflex Corneal reflex Oculocardiac reflex Orbicularis reflex Sneeze reflex Snout reflex Zygomatic reflex | 6. Abducens Ballet's sign Cantelli's sign Disconjugate gaze Red glass test 7. Facial Chvostek's sign Consensural reflex Corneal reflex Facial motion tests Glabella reflex Jaw jerk Jaw reflex Taste test (anterior two-thirds) 8. Auditory Nerve Cochlear Division: Auditory reflex Bing's test Gelle's test Gruber's test Otoscopic signs Rinne's test Schwabach's test Weber's lateralization test Vestibular Division: Babinski-Weil's test Barany's test Caloric test Cantelli's sign Cochleopapillary reflex Mittlemeyer's test Past-pointing tests | 9. Glossopharyngeal Carotid sinus reflex Gag reflex Laryngoscopic signs Palatal reflex Swallowing test Taste test (posterior third) 10. Vagus Carotid sinus reflex Erben's reflex Gag reflex Nasal speech sign Oculocardiac reflex Saliva pH test Salivation response Somagyi's reflex 11. Spinal accessory Active cervical rotation test Cervical range of motion test Shoulder elevation test Shoulder posture evaluation 12. Hypoglossal Protruding tongue Speech test Tongue tremor sign |
Distal Neurologic Manifestations
Because of the effects of the subluxation's microtrauma and the consequent pathological changes involved, the neurologic insult may result in:
(1) modification of the basic chronaxie,
(2) alteration of normal impulse amplitude, wave length, force intensity, and/or
(3) extension of the refractory period.
The neurologic manifestations of a subluxation are indicated by the response the nervous system makes to irritation not external to it (ie, discernable in its immediate area), but rather from within the body. Thus, it is an intrinsic source of neurologic irritation. This altered state of the nerve-fiber threshold and the impulse proper leads to dysfunction in the sensory, motor, vasomotor, and spinovisceral responses.
Somatic Responses. Dysfunctions in the somatic-sensory field include varying degrees of discomfort and pain, tension, superficial and deep tenderness, muscular tone, periosteal tenderness, hyperesthesia and hypoesthesia, haptic sensations, acroparesthesia, formications, flushing, numbness, coldness, and postural fatigue. Dysfunctions in the somatic-motor field include painful and especially proximal muscle spasms; abnormal muscular tone such as from hypotonicity to spasm and weakness, atrophy, or degeneration in long-standing cases; sluggish and incoordinated movements; paralyses; fasiculations, tics, and tremors.
Visceral Motor Responses. Visceral motor responses of the nervous system may be evidenced as:
Dysfunction in the vasomotor field include local swellings, angioneurotic edema, flushing, blanching, mucous membrane congestion, urticaria and dermatographia. Minor changes in the circulation of the skin can be measured by various heat sensitive devices, thermography, galvanometers, or infrared photography. Such changes often parallel circulatory changes in the deeper tissues as they too are affected by similar vasomotor responses.
Changes in the ability of the skin to secrete oils or perspiration which can be measured by various electrical means. These secretory errors may also be indicative of similar changes in deeper visceral tissues. Hyperhidrosis or dryness, as well as hyperesthesia or hypesthesia, in a local area near the spine implies altered vasomotor activity in the subsequent spinal segment. Hyperesthesia and hyperhidrosis are usually associated with an increased "red response" to scratching and a decrease in electrical skin resistance.
Dysfunction in the spinovisceral field include visceral musculature abnormalities, glandular and mucous membrane secretory malfunctions, and sphincter spasms of the detrusor muscles and myocardium.
Changes in the quality of tissue from trophic disturbances such as atrophies, degenerations, thinning or discoloration of the skin, or other changes that reflect viscerotrophic abnormalities.
Spinosomatic, Spinovisceral, and Viscerospinal Syndromes
Interosseous derangements within the spine and pelvis provoke neurologic insults that cause, aggravate, precipitate, or prolong a large number of:
(1) spinosomatic and spinovisceral syndromes,
(2) general body ailments that may evolve into specific diseases, and
(3) triggering and exacerbating of subclinical conditions into acute symptom expression.
The concept of referred pain is one mechanism which explains why spinal lesions often cause extraspinal symptoms. Pain originating from fascia and tendons tends to be more localized while that from muscles and ligaments is more diffuse and tends to be referred. As is true with trigger points, it appears that referred pain from most spinal structures does not follow the dermatomal or known segmental patterns of distribution.
Spinosomatic and spinovisceral syndromes often occur as symptom sets of the peripheral sensory, motor, and autonomic beds that arise in consequence to mechanical pathologies and structural derangements of the segments and articular complexes of the spine and pelvis. Examples are:
Extension neuralgias such as cervical migraine and the supraclavicular, subscapular, radial, median, ulnar, intercostal, iliohypogastric, femoral, gluteal, femoral cutaneous, and sciatic neuralgias. An extension or radiating neuralgia presents pain radiating along the peripheral course of the sensory distribution of a spinal or cranial nerve as the result of nerve root irritation at the point of exit from its osseous and musculofascial containments.
Common types of sensory disturbances such as (a) all types of paresthesias, including causalgias, burning perceptions, tingling sensations, numbness with ache, formications, haptic sensations, etc; (b) variations of dysesthesias, including anesthesia, hypesthesia, hyperesthesia; (c) variations of pain syndromes such as burning pain, sharp pain, penetrating pain, deep pain, superficial pain, radiating pain, lanciating pain, throbbing pain, and aching discomforts.
Common types of somatic motor disturbances such as lessening or loss of deep and superficial reflexes, neurogenic atrophies, reaction of degenerations, trigger point formation, fasciculations, incoordinations and clumsiness, spasms, contractures, paraplegias, and disturbed postural and locomotive patterns.
Common spinovisceral or viscerospinal syndromes such as functional strabismus, disturbed occular accommodation, vasomotor migraines, asthmatic symptoms, diaphragmatic spasms or fasciculations, functional arrhythmias, distal coronary spasms, heart blocks, dyschronias of peristalsis, pyloric and biliary spasms, functional constipation, vasomotor congestions of the pelvic organs, peripheral vasomotor reactions, and small vascular and lymphatic points of stasis.
The Perplexing Reflexes
The human body exhibits an astonishingly complex array of neural circuitry. While the study of reflex communication between tissues under "voluntary" control and tissues under "autonomic" control (and their excitatory and inhibitory effect on one another) is still in its infancy, the answers to why so many visceral disorders mimic musculoskeletal disorders and why so many musculoskeletal disorders mimic visceral disorders appear to be on the horizon. Hypotheses are also being presented that help to explain the progressive reaction spread of some disorders that fail to respond to conventional therapies.
These reflexes can be classified into four broad categories; ie, those communicating
(1) from a site on the body wall, cranium, or limb to another site on the body wall, cranium, or a limb (somatosomatic reflex);
(2) from a site on the body wall, cranium, or a limb (cutaneous, subcutaneous, musculoskeletal) to an internal organ or gland (somatovisceral reflex);
(3) from an internal organ or gland to a site on the body wall, cranium, or a limb (viscerosomatic reflex); and
(4) from an internal organ or gland to another internal organ or gland (viscerovisceral reflex). It must also be considered that these reflexes usually have segmental, propriospinal, and/or suprasegmental implications.
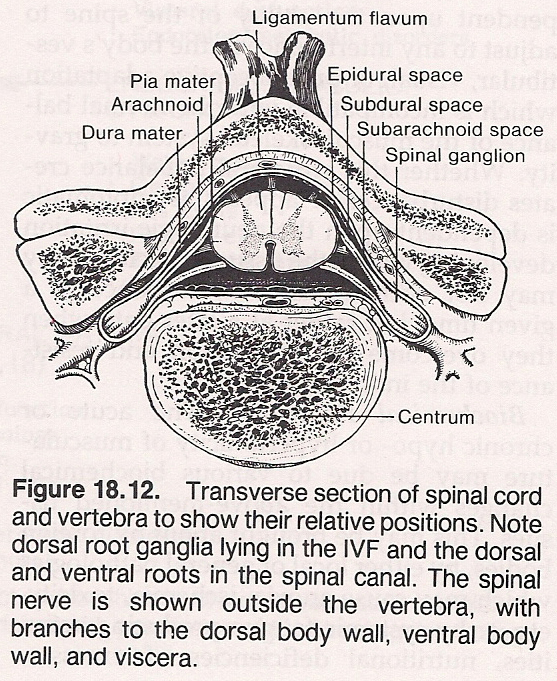
Inasmuch as many reflexes are modulated within the spinal cord, their potentional interrelationship with a subluxation complex, and vice versa, cannot be ignored when we consider that a vertebral lesion can be a focus for neuronal hyperexcitability or hypoexcitability. Thus all structures receiving efferent fibers via the IVF and all afferent fibers entering the IVF are potentially exposed to excessive stimulation or inhibition by some factor producing irritation, pressure, or tension at this vulnerable gateway.
Somatosomatic Reflexes. A somatosomatic reflex develops when a sensory receptor in the skin, subcutaneous tissue, fascia, striated muscle, a tendon, ligament, or a joint is stimulated to trigger a volley of reflex impulses to another anatomical location of this type via efferent sensory, motor, or autonomic fibers. Therapeutically, these reflexes are commonly evoked by manipulation, superficial heat or cold, electrotherapy, meridian therapy, hydrotherapy, traction, compression, vibration/percussion, applied kinesiology, and massage. The projected effects of spinal subluxations on the somatosomatic pathway are shown in Figure 18.17.
Somatovisceral Reflexes. A somatovisceral reflex develops when a sensory receptor in the skin, subcutaneous tissue, fascia, striated muscle, a tendon, a ligament, or a joint is stimulated to trigger a volley of reflex impulses to an internal organ, a gland, or a vessel via efferents of the autonomic nervous system. Therapeutically, these reflexes are commonly evoked by manipulation, superficial heat or cold, electrotherapy, meridian therapy (possibly), hydro- therapy, traction, compression, vibration/percussion, and massage. The projected effects of spinal subluxations on the somatovisceral pathway are shown in Figure 18.18.
Viscerosomatic Reflexes. A viscerosomatic reflex develops when a sensory receptor in an internal organ, a gland, or a vessel is stimulated to trigger a volley of reflex impulses to the skin, subcutaneous tissue, fascia, striated muscle, a tendon, a ligament, or a joint. It essentially operates through motor or sensory efferents (eg, the abdominal spasm overlying peritonitis, angina pectoris). Therapeutically, these reflexes are commonly evoked by biofeedback therapy, spinal manipulation, spondylotherapy, and spinal traction or compres- sion. The projected effects of spinal subluxations on the viscerosomatic pathway are shown in Figure 18.19.
Viscerovisceral Reflexes. A viscerovisceral reflex develops when a sensory receptor in an internal organ, gland, or vessel is stimulated to trigger a volley of reflex impulses to another anatomical location of this type via efferents of the autonomic nervous system. Rarely, however, does this reflex exist alone; ie, it usually has a segmental somatic component. Therapeutically, these reflexes are commonly evoked by spinal manipulation, deep heat, and hypnosis or other forms of psychotherapy. The projected effects of spinal subluxations on the viscerovisceral pathway are shown in Figure 18.20.