

|
Chapter 8
Compendium of Clinical Geriatrics
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Basic Chiropractic Procedural Manual”
The following materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated
to support chiropractic research. Please review the complete list of available books.Clinical Approach Common Neurologic Aspects of Aging Disorders Chronic Respiratory Disorders in the Elderly Common Cardiac Disorders Common Peripheral Vascular Disorders Common Hematologic Disorders Common Digestive and Gastroenterologic Disorders Common Urologic Disorders Common Dermatologic Disorders Common Endocrinologic Disorders Common Gynecologic Disorders Common Ophthalmic Disorders in Geriatrics Common Otohinolaryngologic Disorders Common Orthopedic Disorders Sexual Aspects of Aging Common Complaints and Symptoms in Later Years Common Drugs and Their Reactive Effects Professional Obligations
Chapter 8: A Compendium of Clinical Geriatrics
The objective of this chapter is to focus attention on disorders witnessed in practice by those dealing with the geriatric patient. Following neurologic disorders, heart, vascular, and blood disorders are discussed. Digestive and gastroenterologic disturbances are then followed by disorders of the urinary system, skin, endocrines, and reproductive system. Next, eye, ear, and throat conditions are followed by orthopedic and respiratory considerations. The chapter concludes with information about the sexual aspects of aging, common complaints and symptoms, and other pertinent considerations.
The topics described in this chapter are not to be considered a complete reference for all geriatric conditions seen in practice. They have been chosen as those most likely to be encountered or because they present a unique situation necessary for differentiation and/or case management.
While some described disease states may not be commonly considered within the scope of chiropractic general practice, their diagnosis is. Thus, this general knowledge will help clarify when referral should be considered, thus serving the best interests of the patient and possibly avoiding a potential accusation of professional negligence.
It is the editor's opinion that most errors in diagnosis or judgment do not occur from a lack of clinical knowledge. They occur as the result of a hurried history and examination. A clinician must be self-disciplined to give full attention to the patient at hand, without distracting concern for those patients waiting in the reception room.
CLINICAL APPROACHIn past years, it was a frequent fault of young practitioners of all disciplines to contribute age an important etiologic factor. It is emphasized that age alone is an inadequate factor in the cause of severe illness in the elderly. Careful examination, treatment of the whole individual, and prolonged follow-up is necessary for optimal results.
Most pathologists readily admit that disease is a process, not a state, but rarely is the process defined other than to say that disease of any tissue or organ is the result of disturbed function --normal physiology gone wrong.
According to most authorities, health is that condition when cells are stimulated (irritated) by nerve impulses that results in specialized cellular function to be increased or decreased so to adapt to environmental needs. While there are no new functions in disease, disease is that state where specialized functions are increased or decreased because some abnormal factor (mechanical, chemical, or psychic) is affecting the nervous system. Thus, disease is the result of abnormal or subnormal function or of normal function out of time with need. While health is the result of the organism maintaining a constant composition of the internal environment, disease results when abnormal function changes the internal environment and threatens cellular integrity.
Abnormal function is the result of perpetuated environmental, mechanical, or psychic irritation of the nervous system interfering with normal control of function for adaptation. As pain, muscle contraction, and visceral dysfunction are symptomatic of many diseases, most disease states are the result of excessive neural impulses rather than a reduction of impulses. In chronic states, for example, anoxia causes the nerve to lose its ability to transmit impulses properly. This results in analgesia, muscle flaccidity, and autonomic dysfunction.
Several pairs of nerves do not pass through movable spinal foramina and direct intervertebral pressure is not common except in severe trauma or advanced degenerative states. However, slight fixation of a vertebra producing neurologic insult can cause abnormal (mechanical, congestive, and/or metabolic) sensory irritation, motor spillover, and/or axoplasmic flow impediment. Thus, microscopic rather than macroscopic subluxation effects are more commonly witnessed clinically.
Symptoms indicate abnormal function; ie, normal function that has been increased or decreased out of time with individual needs. This function points to the organ or structure involved as well as the nerves or final common paths that would normally cause the same function when irritated by impulses initiated by normal controls.
Experience shows that manipulation, diet, counsel, physiotherapy, drugs, and surgery can relieve harmful irritation on the nervous system when used on the right patient at the right time and in the proper combination. As there are multiple causes in any disorder, no profession offers a panacea for any or all disease. The objective of any rational approach is to adjust the individual to better adapt to the environment or adjust the environment to the individual's needs if possible.
COMMON NEUROLOGIC ASPECTS OF AGING DISORDERSNormal Variations
The examining physician must hold a flexible attitude to broaden his criteria of normalcy while evaluating a senior citizen so not to confuse a disorder with a manifestation of the aging process. Aging cannot be measured by years alone; however, without a better yardstick, the following neurologic conditions are based on clinical observation of patients 65 years or over. In such observations, physical signs often offer a differentiation between organic illness and disorders within the normal limits of a particular age group.
Aging is characterized by a steady loss of neurons in the general nervous system that begins in early adulthood (about age 25). Mental disorders result such as absentmindedness, insomnia, and rigid mental attitudes. Neuron loss affecting both brain and spinal cord results in the common signs described below.Eyes. Aging eyes are characterized by arcus senilis, pupil irregularity and inequality, fading iris color (more in blue than brown), and an irregular pupillary outline. In the elderly, pupils tend to become smaller and respond less to light or dark accommodation.
Reflexes. While upper-extremity reflexes appear normal in the aged, lower extremity reflexes are characterized by reduced ankle reflexes and reduced position sense in the toes. Tendon jerks (especially the ankle reflex) may vary plus or minus in comparison to the younger person without other signs of lower motor neuron disease. However, reflex absence or reflexly induced clonus is abnormal at any age. It is debatable whether diminished ankle vibratory sensitivity is significant without further supporting tests.
Muscles. There is a general decrease in muscle bulk in the latter years, especially noted in the small muscles of the hands; and loss of muscle tone in spinal, neck, and facial areas is typical. See Figure 8.1. Muscle strength, however, usually remains intact. It is not abnormal during old age that fine finger movements become less adept. Older people generally show a definite resistance to passive movement of the limbs.Cervical spondylosis is commonly seen, and it may accentuate upper-extremity muscle degeneration. Peripheral vascular occlusion affecting the vasa vasorum may be evident. Loss of neurons from the anterior horn cell pool often give rise to clinically recognizable neurologic signs in 50%--80% of patients over age 70.
Infections
Three infections are of primary concern in geriatric neurologic disorders: zoster infection, meningitis, and syphilis.Zoster Infection. In aging, normal resistance to the herpes zoster virus is lowered. While cervical, thoracic, and lumbar types occur frequently, infection of the facial and cranial types predominate.
Geniculate zoster is characterized by vesicular formation on the exterior ear, soft palate, internal cheek, or along the jaw, with loss of taste on the affected side. Severe pain is noted, beginning in the ear and progressing to the throat and down the neck. The classic complication is severe peripheral ipsilateral facial palsy with denervation.
Ophthalmic zoster features severe pain, redness and swelling of the forehead and cheek around one eye, marked eyelid edema, and neuropathic keratitis. Later stages feature a vesicular rash that becomes purulent in the area supplied by the trigeminal nerve, along with increasing pain, fever, leukocytosis, and sometimes ipsilateral oculomotor paralysis.
Meningitis. Pyogenic meningitis is one of the most silent neurologic abnormalities witnessed in geriatrics and is often misdiagnosed. It's characterized by headache, disorientation to time and place, insomnia, fatigue, demotivation, and slight pyrexia. Although rarely a patient complaint, palpation of the cervical muscles will reveal spasm affecting flexion but not rotation. In later stages, characteristic signs are vomiting with dehydration, increased mental confusion, disorientation, dementia, stupor or coma, and leukocytosis. Meningitis is more common in the elderly than meningism.
Syphilis. Geriatric characteristics of syphilis include dementia paralytica, decreased pupil reflex and extensor plantar reflexes, tremors particularly of the tongue and extremities, slurred speech, depression, and progressive delusionary dementia.
Trauma
With increased forgetfulness and decreased proprioception, the elderly tend to trip and fall more often. Frequently misdiagnosed subdural hematoma is characterized by a history of head injury followed by varying degrees of dizziness, and hemiparesis or hemiparesthesia with Jacksonian convulsions. Headache is not always present. Personality signs may include confusion, forgetfulness, loss of judgment, and other personality changes, which may be attributed in error to senile dementia. Often a differential diagnosis cannot be made without electroencephalography, cerebrospinal fluid examination, and/or carotid angiography.
Extradural hematoma is less common and characterized in the elderly by convulsions, hemiplegia, coma, and rapid progress downward. Parietal fracture is often associated. Following severe head injury, intracerebral hematoma not part of cerebrovascular disease may be witnessed. Signs include papilledema, bradycardia, progressing stupor, and hemiplegia.
Neoplasms and Brain Tumors
No age group is exempt from benign new growths; however, primary and secondary malignancies tend to have a slower growth rate in the elderly. Convulsions without a history of cerebral infarction are more likely the effect of cerebral tumor than of uremia, hypertension, or cerebrovascular disease. In the later stages, papilledema, headache, vomiting, and blurred vision manifest. Peripheral musculature degeneration is accompanied by loss of supinator and ankle reflexes, with sensory loss following in the hands and feet.
While brain tumor is infrequently witnessed in the geriatric population, the physician must be on guard against its occurrence as well as chronic subdural hematoma, which may closely simulate cerebral tumor in signs and symptoms. The characteristic syndromes of brain tumor are the result of the tumor growing and consuming space such as with symptoms of papilledema, headache, stupor, vomiting, and especially a progressive neurologic deficit. An expanding mass may be suspected with progressive sensory loss, ataxia, poor coordination, paralysis, visual impairment, neural deafness, aphasia, and convulsions.
Tumors within the central nervous system arise as meningeal, supratentorial, or infratentorial in origin. Signs may appear slowly or abruptly. Abrupt and dramatic occurrence is more suggestive of metastatic lesions.
Meningeal signs. Severe headache is the rule. Pain is diffuse and unremitting in both sarcoma or carcinoma. Because of nuchal rigidity, headache develops before any other neurologic sign.
Supratentorial signs. In the early stages, specific signs are sensory disturbances, paresis, apraxia, convulsions, and seizures. General signs include fatigue, general weakness, and emotional and behavioral changes. In the late stages, vomiting, headache, and mental dullness often develop.
Infratentorial signs. Early signs offer local syndromes of cranial nerve dysfunction, imbalance, intracranial pressure effects, and limb ataxia. In late stages, focal or lateral paresis or sensory signs may develop.
Cranial x-ray films may show a significant shift of a calcified pineal gland from its normal midline position as well as pressure demineralization of the dorsum sellae. Meningiomas, oligodendrogliomas, and other slow-growing tumors may contain x-ray opaque patches of calcification.
Stroke and Vascular Diseases
A stroke may be defined as an abruptly developing neurologic abnormality secondary to an occlusive or hemorrhagic vascular accident of brain vessels. Stroke is the second leading cause of death in persons over 75 years. On suspicion of a cerebrovascular attack after initial observation and history, the examining physician must determine whether the "accident" is in the anterior (carotid) or posterior (vertebrobasilar) arterial circulation.
Features of Anterior Arterial Stroke. The characteristic syndrome includes contralateral weakness or numbness, transient ipsilateral monocular blindness with homonymous visual field defects, ipsilateral throbbing headache, mental confusion, dysphasia, and apraxia with dominant hemisphere involvement.
Features of Posterior Arterial Stroke. The syndrome of vertebrobasilar artery disease includes dysarthria and dysphagia; unilateral or bilateral motor or sensory deficits, often associated with cranial nerve involvement; visual field defects; vertigo; tinnitus; deafness; and generalized imbalance with unilateral limb paralysis. These signs tend to be bilateral or generalized.
Within the aged, most neurologic syndromes are manifestations of vascular disease. Such disorders range from a minor syncope to a complicated stroke. By far, occlusive cerebrovascular disease is the most common etiology. Ten commonly witnessed clinical conditions are listed below along with their major characteristics.
Minor stroke. Mild stroke is a neurologic deficit due to cerebrovascular disease that lasts more than 1 day followed by almost complete recovery within a few weeks. The effects are probably from ischemic necrosis with minimal infarction. Minor strokes often prelude major strokes within 1 or 2 years in 50% of patients. In short stenotic lesions of the internal carotid artery, a fairly high-pitched pansystolic murmur over the artery on the opposite side of the neurologic deficit can be heard in 50% of the patients. In subclavian artery occlusion, the ipsilateral arm supplied by a reversed flow in the vertebral artery leads to hindbrain arterial insufficiency when the arm is used strenuously.
Major stroke. Severe stroke is characterized by considerable neurologic deficits developing several weeks after the attack. Signs include mental disturbances such as poor comprehension, memory loss, demotivation, lack of perseverance, apathy, and slowed mental faculties. The immediate principles of treatment include maintenance of free airways, preservation of systemic circulation, adequate hydration and nutrition, and prevention of secondary respiratory and urinary infection, urine retention, and pressure sores.
Transient ischemia attacks (TIAs). The underlying cause of cerebral TIAs appears to be occlusive cerebrovascular disease with either intracranial or extracranial arterial atherosclerosis. They are often complicated by atheromatous ulceration of the intima. Attacks last from minutes to hours followed by complete recovery within 24 hours and feature transient attacks of hemiparesis, hemianesthesia, hemianopia, aphasia, and/or loss of vision in one eye if the disorder occurs in the territory of the carotid artery.
Signs of vertigo, dysphagia, dysarthria, blurred vision and diplopia, and vomiting suggest hindbrain ischemia in the territory of the vertebral artery. See Figure 8.2. Transient attacks can be the result of microemboli (platelet, cholesterol, fibrin) carried to the cerebral arteries; systemic hypotension; or atheromatous occlusion of the major arteries of the neck with diminished blood flow associated with local stenosis. Hindbrain ischemia is more common when hypotension is the cause. The carotid variety is more frequently associated with a distal embolism from local atheroma and hypertension.
If the hemoglobin percentage is below normal, strenuous exertion can produce signs of cerebral ischemia. In cervical spondylosis combined with degenerative arterial disease, cervical postures requiring extension and full rotation of the head can interfere with vertebral artery blood flow. Because of its vasoconstrictive effects, heavy smoking may cause ischemic attacks. Hypotensive acting drugs may be iatrogenic etiologies.
In hindbrain ischemia, falling attacks are part of the syndrome. Patients may suddenly lose all postural tone and fall heavily to their knees or face without losing consciousness. Patient anxiety, thus, increases. The accident is often misinterpreted as a "misstep" by the patient.Vertigo. Dizziness, unsteadiness, and loss of equilibrium may result on arising from a recumbent to a sitting posture or from a sitting to a standing posture, The cause is usually physiologic, resulting in diminished cerebral blood flow. Such syncope may result in injury.
Syncopal attacks. These attacks may or may not be associated with occlusive vascular disease. The cause can often be traced to failure of baroreceptor mechanisms in the neck or to changes in systemic arterial circulation. In the elderly, attacks are frequently called micturition syncope when an elderly patient arises quickly from bed to enter the bathroom and suffers an attack of syncope.
Cough syncope. This disorder is characterized by a sudden loss of consciousness, often prolonged, from a heart block producing a Stokes-Adams attack in emphysematous and bronchitic patients. The pulse is usually 40 per minute or below, and electrocardiography usually shows evidence of complete atrioventricular dissociation.
Hypertensive encephalopathy. This disorder features focal or generalized fits, headache, blurred vision, hemiparesis, and a diastolic pressure over 140. Along with these signs, diagnosis can be made from fundi observation where retinal hemorrhages and exudates with papilledema exist.
Cranial arteritis. If left undiagnosed and untreated, this geriatric disorder can result in half the affected elderly patients becoming permanently blind. The disorder is characterized by severe persistent headaches, often temporal and unilateral, with dim or loss of visual acuity, Associated pain in the shoulders and hips is reported if the arteritis is widespread. The condition is often called giant-cell arteritis or temporal arteritis because of the local manifestation, and the most damaging retinal involvement is frequently overlooked.
The temporal arteries are normally tender and sometimes lose their pulsation. They frequently protrude during an attack as thickened cords under hot red overlying skin. Fundi examination shows retinal hemorrhage or some degree of optic atrophy or thrombosis of the retinal artery in 50% of the patients. Abnormalities may be bilateral. Other signs may include a mild fever, leukocytosis, occasional eosinophilia, and a raised erythrocyte sedimentation rate.Apoplexy. This is a less common type of stroke in the elderly and associated with hypertension, probably the effect of rupture of one or more microaneurysms in the smaller branches of the middle cerebral artery. Hemorrhage into the lateral ventricle or subarachnoid space results in complaints of headache and vomiting. Rapid unconsciousness occurs, progressing to deep coma. Flaccid muscles are noted in the face and limbs on the hemiplegic side. The eyes turn first toward the affected limbs conjugately and then away from the affected limbs.
While uncommon in the elderly, primary intracerebral hematoma may occur if the bleeding is confined. In such a case, it is almost impossible to differentiate the condition from cerebral infarction.Primary subarachnoid hemorrhage. Although commonly thought of as a young person's disorder, it is not uncommon for a congenital cerebral aneurysm to rupture during the senior years. In the elderly, headache and neck stiffness may not be severe. However, coma is usually sudden and prolonged, and gastrointestinal symptoms such as vomiting and diarrhea may be predominant in a stuporous patient. Recuperation is extremely slow in the elderly. Communicating hydrocephalus may arise because of the occlusion of the arachnoid villi. If this occurs, severe dementia results.
Common Deficiency States
As will be detailed in the next chapter, deficiency states often result from a decrease in appetite, improper food processing, and improper intake combined with poor absorption and slow metabolism, producing conditions unfavorable for normal function of the nervous system.Cyanocobalamin Deficiency. Classical B-12 deficiency results in subacute combined degeneration of the spinal cord. Neurologically, the condition begins as a symmetric neuropathy with characteristic absent reflexes and peripheral sensory loss, particularly of the vibration sense and position proprioception. Ankles become weak, hands and feet become clumsy, tingling in fingers and toes are noted, and it is difficult for the patient to feel the ground beneath the feet. There may be evidence of pernicious anemia, tongue atrophy, megaloblastic bone marrow, and low serum cyanocobalamin. Achlorhydria is almost always complete. Mental signs include forgetfulness, disorientation, increasing dementia, and psychotic states. Primary optic atrophy is commonly associated in elderly cigarette smokers.
Thiamine Deficiency. Classic B-1 deficiency is commonly the result of alcoholism, producing myelopathy, encephalopathy, and neuropathy. The sensory-motor type neuropathy is characterized by peripheral muscle weakness and degeneration, pain in the lower extremities, and paresthesias in the hands. Severe chronic deficiency often accompanied by heart failure and cardiomyopathy (wet beriberi). Some neurologic changes may be permanent such as amnesia, disorientation, areflexia, and muscle tenderness. Basic treatment consists of supplemental B-complex plus vitamin C, increased carbohydrates, and restricted alcohol despite type.
One related encephalopathy shows itself as Korsakoff's psychosis with associated confabulation, amnesia of recent events, and disorientation of person, place, or time. Another type known as Wernicke's encephalopathy is characterized by ataxia, tremor, nystagmus, pupillary abnormalities, ocular nerve paralysis, and stupor sometimes progressing to coma. The onset is often sudden and may be confused with intracranial tumor, virus encephalitis, or meningitis.
Note: Deficiency of other vitamins in the B group can produce acute mental and emotional disorders in the elderly suffering from malnourishment. States of confusion are common, especially in riboflavin and nicotinic acid deficiency. Differential diagnosis is made by finding fissures at the corners of the mouth, pigmentation over pressure areas, and a raw red tongue.
Common Metabolic DisordersHypothyroidism. Coma due to hypothermia can be a neurologic manifestation in the elderly. Other clinical features include deafness from auditory nerve degeneration, peripheral neuropathy, and cerebellar ataxia. With hypothyroidism, cerebellar disturbance resulting in loss of balance, giddiness, unsteadiness, and motor clumsiness may be the syndrome. This is accompanied by obesity, sluggish mentality, deafness, lowered voice tone, and bradycardia with its associated symptoms. Tendon reflexes indicate a slow phase of relaxation. Associated carpal tunnel syndrome points to peripheral neuropathy but is more common in the middle-aged than the geriatric patient. Diagnosis is confirmed biochemically with blood protein-bound iodine below 3 mg/100 ml and the serum cholesterol content about 300 mg/100 ml.
Diabetes Mellitus. In the elderly, diabetes is the most significant disorder producing metabolic neurologic diseases. It may present a neurologic picture of mild peripheral neuropathy with absent tendon reflexes, peripheral sensory loss, impaired peripheral circulation, muscle degeneration, and a flapping-type gait. In diabetic amyotrophy, proximal weakness and wasting of the lower extremities may be evident. A 5-hour glucose tolerance curve is necessary because of the mildness of the diabetes. In geriatrics, hypoglycemia may be the manifestation of either insulin therapy or an islet-cell tumor causing an intrinsic overproduction of insulin. The condition is characterized by sudden fainting attacks, hemiplegia, convulsions, and irrational behavior.
Drug Reactions. As chiropractic patients may also be under medical care, it is well that the doctor of chiropractic can recognize drug reactions in the elderly, particularly reactions from common hypotensives and sedatives. If hypotensives are prescribed, reactions may include convulsive or syncopal attacks.
It is always advisable to inquire about medical therapy before diagnosing systemic disorders. Barbiturates produce some of the most usually encountered neurologic drug reactions in geriatrics, producing cerebellar ataxia, dysarthria, nystagmus, mental incoordination, dizziness on looking upward, manual incoordination, staggering gait, loss of balance, and altered behavior. Barbiturates in combination with alcohol can produce the grossest abnormalities of mental and physical control. Drug reactions will be described further in the final section of this chapter.
Carcinomatous Neuropathy. While less common in senior citizens, bronchial carcinoma is one of the most common causes of peripheral neuropathy. Thus, neuropathy of unknown origin should be checked by a chest film. Such a neuropathy may be either a motor, sensory, or motor-sensory type.
Neurologic Disorders of Unknown EtiologyParkinsonism. This syndrome is characterized by ideas of persecution, depression, aggressive behavior, disorientation, frightening hallucinations, and behavior disorders difficult to control (especially in patients with concomitant generalized cerebral ischemia). Cerebral infarction is often misdiagnosed as arteriosclerotic parkinsonism. While cerebral infarction may exhibit generalized rigidity, difficulty in initiating voluntary movements, and even parkinsonian facies, it is extremely rare for extrapyramidal tremor to develop because of atherosclerosis. Studies offer evidence that parkinsonism is due to a deficiency of dopamine in the extrapyramidal system.
Senile Tremor. True senile tremor does not affect the hands as much as the head and tongue. Here, head nodding is conspicuous and advances with age. Differentiation from parkinsonism is needed. Pseudosenile tremor is an exaggeration of a familial tremor that worsens with age. The hands are affected first, then symptoms progress to the head and finally to the tongue. It is an intention tremor worsened by social stress. Ethanol is a palliative, and undisciplined use may lead to alcoholism.
Myasthenia Gravis. While the classic form of this disease, with its peripheral or ocular weakness that increases as the day progresses, is more common in young patients, elderly patients more often exhibit the bulbar type characterized by loss of voice after speaking for a few minutes. Chewing and swallowing become a chore. Ptosis without diplopia is evident. In the late stages, respiratory muscles become involved.
Trigeminal Neuralgia. Tic douloureux, commonly seen in the elderly, is characterized by sudden lancinating pain paroxysms in the face unilaterally on sensory stimulation such as by eating, talking, washing, or rubbing the face. Severe pain and muscle spasms of the face are characteristic.
Clonic Facial Spasm. The clinical picture of this disorder is an effect of degenerative changes in the facial nerve nucleus, seen unilaterally, and beginning as an eyelid tic. More commonly seen in women than men, the tic spreads to the whole side of the face, increases in severity, and results in the angle of the mouth being drawn upward and the eyelid completely closed.
Motor Neuron Disease. The peripheral form is progressive, bilateral, shows increased tendon reflexes without sensation alteration, and features muscle atrophy affecting the hands, arms, and shoulder girdle with evidence of fasciculation and muscle degeneration. It is more benign than the medullary form, which is usually severe and characterized by tongue atrophy, rapidly progressing dysphagia, dysarthria, and respiratory failure. Prognosis seldom exceeds 1 year for the medullary variety.
Neurologic Disorders from Skeletal Changes
Senior citizens are the most likely age group to present with skeletal abnormalities. See Figure 8.3. Cervical spondylosis, Paget's disease of bone, and osteoporosis are the three main conditions seen clinically.Cervical Spondylosis. While spondylosis is commonly demonstrated by x-ray films of the elderly, neurologic effects may not be evident. Osteophytes may distort the vertebral arteries and affect hindbrain circulation --resulting in cerebral ischemic attacks, particularly during cervical extension and rotation. A murmur may be heard over the artery in the supraclavicular fossa. Also, ischemic myelopathy may be the result of transverse intervertebral bars that interfere with the blood supply to the cervical cord. This situation is characterized by clumsiness, weakness in the lower extremities, urinary sphincter disturbances, spastic lower limb muscles with exaggerated tendon reflexes, clonus and extensor plantar responses, restricted neck movements, paresthesias in the hands, and upper-extremity sensory loss of peripheral and occasionally segmental distribution. The posterior columns may become involved by cord compression.
By increasing cord circulation and reducing cord pressure, upper limb pain diminishes, lower limbs tend to relax, nocturnal flexor spasms decrease, and extensor plantar responses can change to flexor responses. In the elderly, cervical traction is usually contraindicated as it might increase attacks of hindbrain ischemia. Differential diagnosis should consider subacute combined cord degeneration, cord tumor, and atherosclerotic myelomalacia.
Paget's Disease of Bone. This disorder is characterized by symmetrical facial weakness, headache, lower extremity pain, and deafness, and it occasionally results in cord compression. Determination is made by hearing a murmur over affected bones and finding a raised alkaline phosphatase level, typical radiologic findings, and the often concomitant high-output cardiac failure.
Osteoporosis. In geriatrics, this condition is characterized by spinal pain and occasional root pain as the effect on the spinal column produces neurologic symptoms. Serum calcium and phosphorus usually appear normal. Diagnosis is confirmed by roentgenography, which allows differentiation from secondary deposits or myelomatosis, evidence of a primary growth with localized osteoporosis, or osteosclerosis in carcinoma. Myelomatosis is differentiated by serum protein changes and a high sedimentation rate. In cord or cauda equina compression, vertebral collapse is rarely the cause. Overmedication for thyrotoxicosis or of corticosteroids should be considered if the patient has been or is under medical care. Besides regular chiropractic care, concern should be given to maintaining a positive nitrogen balance that is important for calcium retention, to bed rest, and to nonweight-bearing exercises until the patient is ambulatory.
Senile Dementia This vaguely defined disorder is difficult to set apart from the normal aging process and all too often the diagnosis is the result of elimination of more specific disease processes. Rather than a disease process, senile dementia is looked on as an incremental deterioration of the nervous system contributed to by vascular and metabolic deficiencies, progressive sensory insufficiency, and/or social and cultural isolation.Simple Dementia. This disorder is characterized by diminished recent recall and memory, shortened attention span, increased task performance time, and difficulty in orienting to new situations and chores.
Senile Psychoses and Degenerative Dementia. The degenerative dementias are clinically marked from simple dementia by distinct pathologic features. Disorientation, delusions, and hallucinations advance from simple confusion. Aphasia, apraxia, or agnosia may appear, making speech and gestures inappropriate. Hemiparesis and epileptic or spontaneous choreiform movements may precede complete helplessness or coma.
Differentiation should be made from associated or underlying metabolic or toxic psychoses. Subacute spongiform encephalopathies have distinguishable pathologic features. Frontal fossa meningioma, incisural block, or chronic subdural hematoma may be responsible for a deteriorating mental state, as would disorders such as uremia; diabetes mellitus; myxedema; pulmonary, hepatic, or renal insufficiencies and encephalopathies; CNS syphilis; or congestive heart failure. Localized cerebrovascular disease, schizophrenia, and Wernicke and Korsakoff syndromes should be ruled out, and the presence of Alzheimer's disease, arteriosclerosis, parkinsonism dementia, or Pick's lobar atrophy must be considered.
Concluding Remarks
Geriatric neurologic conditions are rarely unique to old age. No neurologic disorder can be relegated exclusively to the aged. The most common cause of neuropathy in the elderly is diabetes mellitus. The second most common cause is nutritional deficiencies associated with alcoholism and chronic illness.The Central Nervous System. Because the CNS is largely encased in bone, except for the optic nerve head, direct examination must be replaced by indirect methods that evaluate sensibility, muscle strength, coordination, gait, and station. This often requires active patient participation. Besides a regular clinical physical examination including orthopedic and neurologic tests, the chiropractic physician should listen over the cranium or blood vessels to detect bruits. Muscles should be palpated to evaluate mass and tone, and the general body surface should be examined for specific local departures from normal bilateral muscular symmetry.
Muscle Weakness. Complaints of weakness are common in senior citizens. They may stem from increased joint stiffness associated with arthritis or from muscle atrophy consequent to motor neuron disorders or disorders of muscle fiber. A simple lack of exercise should not be overlooked.
Complaints may also stem from anemia, diabetes, or pulmonary, cardiac, or systemic conditions. Disabling weakness may he the result of neuropathy, myasthenia gravis, primary myopathy, thyroid disorders, hypokalemia, hypercalcemia, sodium depletion, or hormonal or electrolytic disturbances such as seen in Cushing's disease. The occurrence of myopathy in the senior citizen is typically associated with systemic malignancy or connective tissue disorders.
Muscle weakness may be the result of local motor-nerve impulse conduction (as in an extremity) or to involvement of motor paths descending from the brain. As in stroke, an abrupt unilateral paralysis may result because of involvement of the long tracts of the CNS. Remember that a crossing of motor outflow paths from the cerebral hemisphere to the opposite spinal outflow mechanism is necessary because one side of the body is controlled by the opposite half of the brain. Similarly, sensory flow over afferent nerves eventually meets with sensory long tracts that decussate within the spinal cord in their course to the opposite cerebral cortex.
Peripheral Nervous System. Peripheral sensory impairment generally occurs in the supply of specific spinal roots, nerves, or a nerve plexus. Sensory impairment is characterized by specific patterns in nerve or root involvement. Local nerve involvement or a spinal segment disorder exhibits as muscle atrophy and flaccid paralysis. Absent tendon reflexes may show involvement of the sensory side, the motor side, or both sides of the reflex arc. While nerve or nerve root disturbances result in unilateral signs, spinal segment disturbances frequently cause bilateral signs. Any disturbance with pyramidal tract function (from cerebral cortex through the cord) will be revealed by the presence of an extensor plantar Babinski response.
The Neuropathies. Peripheral neuritis is a frequent complication in a long list of geriatric illnesses. It is extremely important clinically as it is often the earliest and only indication of systemic disease. Mononeuropathy, affliction of a single nerve, may occur temporarily and spatially among several nerves as in polyneuropathy or mononeuritis multiplex, or involve only the distal portion of nerves bilaterally as in symmetrical distal polyneuropathy. The most common mononeuropathies in senior citizens are Bell's palsy, trigeminal neuralgia, and postherpetic neuralgia.
Whether the peripheral neuritis is described as motor, sensory, or mixed, diagnosis requires two or more of the following signs:
Pain
Sensory impairment
Paresthesias
Regional muscle weakness
Projected sensations on percussion of an affected nerve
Atrophic changes in the skin and nails resulting from coincident postganglionic sympathetic axon involvement.
The Myopathies. Geriatric myopathies are usually secondary to generalized systemic disease, occurring far less than the neuropathies. The trunk, shoulder girdle, and throat areas tend to be more involved than the face, distal extremities, or diaphragm. Specific muscles or groups appear to be involved with out regard to motor nerve supply. While distal limb weakness is a feature of generalized neuropathic processes, the proximal distribution of weakness is characteristic in myopathy.
The syndromes of myopathy present with a gradually progressive course of weakness, weight loss, and reduced muscle bulk in a prolonged period. Muscles become painful on exercise. On palpation, the involved muscles are tender and "doughy" to the touch. Myotatic reflexes elicited by muscle stretch may be well preserved until severe muscle atrophy sets in during the late stages. No objective sensory signs are present.
Movement Disorders. Several neurologic conditions associated with aging are characterized by involuntary and abnormal movements of the body. Many of these are likely related to the loss of basal ganglia control. Movement disorders include the slow writhing sinuous movements of athetosis, the coarse rhythmic tremor of parkinsonism, and the brief dancing and jerky movements of chorea in the trunk and extremities (rarely the result of cerebrovascular disease in the elderly). Other movements include the stereotyped activity patterns mimicking natural behavior as seen in habit tics; the uncontrolled gestures preceding movement as seen in action dystonia; and the involuntary asynchronous and arrhythmic forced blinking, wrinkling of the nose, licking movements of the tongue, and pursing of the lips as seen in Meigs' syndrome.
The movement disorder of Parkinson's disease is commonly encountered in geriatrics. Idiopathic parkinsonism exhibits diminishing voluntary movements and progressing rigidity of the muscles of the trunk and extremities. Trunk and neck flexion is severe. The face becomes as expressionless as a frozen mask; speech is muffled with monotonous whispers; and eye motion becomes markedly circumscribed. Rapid, rhythmic tremors occur involuntarily in the head, feet, fingers, and lips that disappear briefly during volitional movement. In the more rare variety of postencephalitic parkinsonism, signs of torsion dystonic posturing, respiratory dysrhythmias, oculogyric crises, and personality and sleep disorders are seen besides the signs of idiopathic parkinsonism.
As well as basal ganglia dysfunctions, disorders of the cerebellum are important considerations in the incidence of geriatric movement ailments. Cerebellar movement disorders in the aged usually manifest as either truncal ataxia with a broad based unsteady gait or as an uncoordinated action tremor in one or more limbs. Eye movements may become jerky, and speech can become slurred as in cerebellar dysarthria. Malignant metastasis can result in a subacute cerebellar syndrome when the posterior fossa is involved or result in parenchymatous degeneration of the cerebral cortex. On the other hand, fulminating cerebellar syndromes in senior citizens are frequently attributed to vertebral basilar arterial ischemia, which is often complicated by sensory and motor dysfunctions of the lower cranial nerve centers.
In evaluating any movement disorder, thyroid conditions should always be considered. Drug intoxication from tranquilizers, hypnotics, and sedatives is not beyond question. These two factors are often overlooked in the working diagnosis.
CHRONIC RESPIRATORY DISORDERS IN THE ELDERLYWhile pulmonary tuberculosis remains the most serious chronic infectious disorder of adult Americans, chronic airway obstruction disorders have replaced tuberculosis as the major concern.
Emphysema
Emphysema is increasing in incidence in the elderly. It results from loss of alveolar walls and manifests as chronic dyspnea or exertion, profound respiratory drive, and increased volume of ventilation per minute. Distribution between ventilation and perfusion is usually well maintained, thus excessive right-to-left shunting is minimized. Hypoxemia and carbon dioxide retention are rarely a factor, but chronic bronchitis may exist. Differentiation is necessary from pulmonary fibrosis and bronchiectasis.
Chronic Bronchitis
This chronic airway obstruction is characterized by chronic cough, excessive nonseasonal expectoration, dyspnea, mucous gland hyperplasia, hypoxemia, and carbon dioxide retention in established cases. Because of air trapping, the residual air volume is increased, but the total lung capacity is not. Respiratory drive is reduced, and there is altered distribution between ventilation and perfusion due to localized airway plugging and shunting through areas of reduced ventilation. See Figure 8.4 for major structures.
Differentiation must be made from neoplasm or pulmonary tuberculosis. Reactive pulmonary hypertension, cor pulmonale, or congestive heart failure may be associated. The hypoxemia may lead to secondary polycythemia. If acute bronchiolitis coexists, marked inflammation, edema, and increased airway plugging will be found.
Other Airway Obstructive Diseases
Pulmonary tuberculosis, chronic bronchial asthma, interstitial fibrosis, and chronic pneumonitis are other conditions of geriatric concern.
Pulmonary tuberculosis is rapidly becoming a disease of the elderly. On examination, lower lobe infiltrates and plural effusion may be manifestations of tuberculosis in the elderly rather than the classic x-ray findings of apical cavitation. Chronic bronchial asthma often coexists with chronic airway obstruction, as do interstitial fibrosis and chronic pneumonitis. Diffuse interstitial fibrosis is usually associated in the senior citizen with collagen disease, fibrosing alveolitis, or desquamative interstitial pneumonitis. Bronchiectasis is an infrequent finding.
COMMON CARDIAC DISORDERSPathology
In general, the cardiovascular conditions most commonly seen in geriatrics are coronary sclerosis, aortic sclerosis, and vascular nephritis. Cardiovascular deaths amount to 72% of deaths of those aged 65 years or over. A review of common pathologic changes helps to visualize what is occurring in many geriatric patients with abnormal cardiovascular signs.
In the elderly, the heart (Fig. 8.5) exhibits a general decrease in muscle cell size, smaller output, and progressively decreasing strength. Diastolic filling resistance increases, recovery of contractile ability is delayed, and there appears to be a decreased efficiency in converting nutrients into mechanical heart energy. At the cellular level, pigment increases at the poles of the nuclei, brown atrophy appears, and muscle cell striation around the nuclei decreases. Mitochondria atrophy occurs, enzymes needed for contraction reduce, and catecholamine mobilization becomes less effective, which impairs the speed and power of contraction under stress. Cardiac filling and emptying become difficult with decreased aortic elasticity and atrial atrophy. See Figure 8.6.
Because of general body atrophy, lowered BMR, and reduced work load, the normal aged heart provides an adequate output under ordinary conditions. However, the ability to compensate under stress is greatly hindered. Acute coronary insufficiency, congestive heart failure, myocardial necrosis, and arrhythmias may be the result of chronic or sudden cardiac stress, decreased venous return on standing, a sudden heart rate increase, anoxia from bleeding, hyperthyroidism, or an excess of parenteral fluids, steroids, or vasopressors. Oxygen uptake values are reduced, and the incidence of ischemic electrocardiographic S-T depressions increases with advancing years.
Diagnosis
Techniques do not vary greatly from those used in younger patients except that special care must be taken not to tire a patient with too prolonged testing during one visit. The history should include personal and familial dates, past and present; habits of diet, exercise, avocations and vocations, physical and mental occupations, and the use of drugs. Physical examination should include all systems. Laboratory tests such as urinalysis, blood profiles, electrocardiogram, and chest films are usually routine, along with special tests and views as indicated. As both cardiospasm and angina pectoris are common in the elderly, special concern must be given to differentiation. For example, dyspnea resulting from pulmonary emphysema is frequently confused with that associated with coronary heart disease because of coincidental electrocardiogram findings. Thrombosis from a leg vein can result in pulmonary embolism and be confused with acute myocardial infarction or hypostatic pneumonia because of similar symptoms and electrocardiographic findings. It is important in geriatric evaluation to realize that acute conditions are often superimposed on chronic disorders.
Prognosis
Benign arrhythmia, premature beats, and short paroxysms of atrial tachycardia tend to increase with age but are seldom important clinically.
However, special attention should be given to the presence of flutter and fibrillation, or ventricular or atrial paroxysmal tachycardias that present in prolonged episodes. Both bundle branch and atrioventricular heart block are usually the result of coronary atherosclerosis. Atrioventricular block with Stokes-Adams attacks of syncope are highly serious, even if convulsions are not present, and signals specialized care.
Rest and a simple diet are important adjuncts in congestive heart failure. In angina pectoris, walking is an excellent exercise; however, physical exertion combined with emotional stress (especially after eating or during exposure to cold and wind) should be avoided. Physical and emotional overstress should be avoided if the patient has angina attacks at rest (angina decubitus).
As no two patients are exactly alike, each must be evaluated for individual treatment or referral. Referral should not automatically imply dismissal. The ideal situation in many cases is combined cardiologist and chiropractic case management.
Prevention
While each case must be considered from an individual standpoint in the light of clinical judgment, general preventive measures should include structural and neurologic considerations, rest and exercise, nutrition and supplementation, and all the other factors necessary to aid the patient in adjusting to the environment or adjusting the environment to the patient's needs.
Rehabilitation
In reference to rehabilitation, Dr. Paul Dudley White stated: "Such rehabilitation has been accomplished by the growing recognition of nature's own curative measures that are achieved in the main through the development of collateral circulation, as well as by active measures ...."
Cardiac Ischemia
Cardiac ischemia as the result of coronary artery disease increases in severity with aging and exists in almost all individuals over the age of 70. While myocardial infarction, acute coronary insufficiency, subendocardial infarction, and the anginal syndrome are specific entities, many clinical pictures do not offer clearly defined categories. However, for the sake of classification, several disorders are described below that are commonly witnessed in geriatrics.Acute Myocardial Infarction. This disorder is frequently misdiagnosed as pneumonia or hypertensive heart disease in the elderly. It is commonly the result of fresh thrombotic occlusions producing large infarcts or less common mural thrombi. Symptoms may or may not include precordial pain, nausea, vertigo, dizziness, or epigastric discomfort. An acute attack may be superimposed on old myocardial infarctions, coronary artery disease, left ventricular hypertrophy, angina, and/or congestive heart failure. A history of definitely abnormal electrocardiograms will be found in over 60% of the cases.
In typical situations, precordial, neck, shoulder, arm, or epigastric pain occurs. Such cases usually have a low incidence of preceding failure, coronary heart disease, cardiac enlargement, or other disorders considered associated with poor collateral circulation.
In atypical (silent) myocardial infarction, the major characteristic is the lack of pain with dyspnea, dizziness, weakness, abdominal distress, or syncope. This variety is more common in patients in their 80s than in their 70s. Preceding failure, coronary heart disease, cardiac enlargement, or other disorders associated with poor collateral circulation are typical. The symptomatic picture can often be traced to functional disorders.
Dyspnea is usually attributable to acute failure of the left ventricle. Vertigo, dizziness, weakness, and mental confusion are the result of decreased cardiac output aggravated by a sluggish carotid sinus reflex and cerebral arterial narrowing affecting cerebral arterial circulation. While syncope is the effect of complete heart block with bradycardia, discomfort in the abdominal area is attributable to right cardiac failure resulting in visceral congestion. Evidence of myocardial infarction may be present without any overt subjective complaints or clinical manifestations.
The subendocardium area of the myocardium is highly susceptible to anoxia and resulting necrosis. Such a disorder occurs with anemia, fever, electrolyte depletion, hemorrhage, dehydration, and sudden hypotension. This condition is seen frequently in patients suffering with severe coronary artery narrowing. During infarction, the inner wall of the left ventricle and the septum may be totally involved.
The Anginal Syndrome. This syndrome is one of transitory coronary insufficiency seen in people with diffuse coronary artery disease. Symptoms vary considerably and overlying chronic disorders of the stomach, esophagus, lungs, and chest wall often confuse accurate diagnosis. While chest pain is typical, silent coronary artery disease is not rare. Hyperthyroidism, anemia, and the tachycardias and arrhythmias may be aggravating factors. Several episodes over several years result in multiple areas of myocardial necrosis and fibrosis, which predispose diffuse myocardial fibrosis, muscle weakness, and congestive heart failure.
Acute Coronary Insufficiency. Acute coronary insufficiency is the anginal syndrome in the extreme. If the initiating stress is greater or the arterial narrowing is more severe, the myocardial damage is greater. The precordial pain is of much longer duration. Associated findings include leukocytosis, elevated sedimentation rate, slight elevation of isoenzymes, low-grade fever, and electrocardiographic evidence of sagging or horizontal S-T depressions and T-wave inversions from several days to several weeks or even longer, with signs of chronic insufficiency progressing to a symmetric T-wave inversion. Recurring severe insufficiency results in local necrotic areas leading to diffuse fibrosis by coalescence. Adjunctive treatment consists of bed or chair rest, a light diet, avoidance of stress, and often oxygen therapy.
Ventricular Aneurysm. Extensive transmural myocardial infarction can lead to ventricular aneurysm; however, rupture is rare. Death usually results from associated conditions rather than the aneurysm itself. Multiple small aneurysms are usually asymptomatic and do not affect longevity. Calcified and nonpulsatile aneurysms have been associated with prolonged survival, probably because they are indicative of patient adaptation capabilities.
Cardiac Rupture. Occasionally, myocardial infarction leads to cardiac rupture and is often associated with the aged. Rupture, usually fatal, is regularly associated with long-standing hypertension; less often with pre-existing left ventricle hypertrophy or coronary artery disease; and even less often with aneurysm, angina, infarction, occlusion, muscle failure, and impulse abnormalities. Preceding coronary artery disease appears to exert a protective effect against rupture because of the consequent increase in collateral circulation and the resulting muscle hypertrophy and fibrosis. While sustained hypertension on strong heart muscle facilitates rupture, protection against rupture is seen in the failing heart with decreasing blood pressure producing lowered intracavity pressure. Aged females with acute myocardial infarction are prime candidates for rupture, especially if the hypertension is of long duration.
Hypertension
Both systolic and diastolic pressure is increased in essential hypertension as the result of arteriolar vasoconstriction that increases peripheral resistance. Both systolic and diastolic pressure may be increased as the result of increased heart output as seen in thiamine deficiency, Paget's disease of bone, hyperthyroidism, and parkinsonism. Conversely, both systolic and diastolic pressure can be decreased as the result of a decreased heart output as seen in acute infarctions, heart failure, inanition, and in those disorders resulting in increased aortic length or circumference. Aortic stenosis or rigidity lowers diastolic and raises systolic pressures, resulting in a wider pulse ratio.
Keep in mind that two antagonistic disorders may be superimposed. Normal blood pressure does not necessarily prove a normal cardiovascular system; eg, when recent thiamine deficiency is superimposed on basic essential hypertension.
Pulmonary Heart DiseaseLeft Heart Failure. Changes secondary to left heart disorders and mitral disease in the elderly can adversely affect pulmonary functions. Typical dysfunctions are the result of chronic bronchitis and bronchiectasis, alveolar dilation, fibrosis and emphysema, loss of elastic tissue, chronic fibroid tuberculosis, residual fibrosis as an effect of old pulmonary infarctions, and severe kyphosis.
Right Heart Failure. Changes secondary to right heart disorders include superimposed infections, embolitoxemias, anoxemias, and other conditions that increase breathing effort. Other changes include acute cor pulmonale, which is brought forth by massive pulmonary embolus or lung infection superimposed on pre-existing atrial fibrillation and/or chronic right heart failure. Frequently diagnosed are thrombi from the veins of the lower extremities leading to pulmonary emboli. Preventive attention must be given in such cases to optimal nutrition, early ambulation, elastic stockings, care of cardiac arrhythmias and congestive heart failure, and other procedures to prevent emboli formation.
Emphysema. Pulmonary emphysema is the most common cause of chronic cor pulmonale and is difficult to diagnose until acute symptoms appear as the result of pulmonary emboli or infection, reaction from respiratory depressants, or spontaneous pneumothorax from rupture of an emphysematous bleb.
Bronchiectasis. Cyanosis and finger clubbing indicate bronchiectasis. Early signs are a lowered liver and diaphragm, distinct breath sounds, and restricted chest movements on breathing. Later signs are the result of right heart failure such as liver enlargement, distended neck veins, peripheral edema, and paroxysmal arrhythmias from coexisting coronary artery disease. The history will usually report chronic cough, dyspnea, asthmatic wheezing, several respiratory infections, heavy smoking, and/or lung resection, collapse, or some restrictive lung disease such as granulomatous, fibrotic, or infiltrative diseases.
Congenital Heart Disease
Because severe congenital heart disease shortens life span, it is rare in geriatrics except those conditions that have become well adapted until stressed by other disorders. It is not uncommon, however, to find signs in the elderly of an atrial septal defect. Before congestive heart failure appears, there will be a history of difficult breathing and several attacks of bronchopneumonia.
High pulse and blood pressure occur and likely with signs of coronary artery disease. Fluoroscopy reveals an enlarged right ventricle and atrium, a normal left atrium, a small left ventricle and aorta, and a hilar dance with a prominent pulmonary artery. Other signs include a fixed splitting of the pulmonic second sound, a low-pitched systolic murmur in the second left interspace (occasionally also at the apex and left fourth interspace), incomplete right bundle-branch block, and atrial fibrillation.
In the elderly, signs of a ventricular septal defect, an isolated pulmonic stenosis, congenital aortic lesions, a patent ductus arteriosus, or coarctation of the aorta may appear when adaptive forces are weakened.
Rheumatic Heart Disease
It is not uncommon in geriatrics to find signs of mitral insufficiency supported by a history of rheumatic fever during the younger years. Because of probable myocardial weakness and emphysema, low intensity systolic murmurs will be found localized at the apex. High blood pressure, atrial fibrillation, and atherosclerosis may be associated and hasten congestive heart failure or thromboembolism or both. However, adaptation to mitral stenosis in the elderly is commonly seen because of the decreased basal cardiac output, decreased work load, and resulting lessened stress against the narrowed mitral orifice.
Aortic and Mitral Murmurs
Aortic systolic murmurs are often the effect of degenerative processes associated with aging. Examples include fibrotic thickening of the valve cusps, aortic dilation, increased stroke output from stress, and hyperthyroidism. The extent of involvement, stenosis, calcification, fibrosis, and adhesions increase in intensity and incidence with age. Symptoms of aortic stenosis in the elderly usually include syncope, dizziness, angina, and left heart failure in association with an aortic systolic murmur. Signs include a narrow pulse pressure, a loud precordial murmur that is transmitted to the neck, a systolic aortic thrill, a faint aortic second sound, and left ventricular hypertrophy. Prognosis is poor once congestive heart failure develops. See Figure 8.7.
Degenerative changes associated with aging can involve the mitral value. The pathologic picture begins as a degeneration of collagen, progressing to lipid infiltration, fibrosis, and ending in calcification. On the other hand, mitral murmurs may be the result of anemia, cardiac dilation associated with heart muscle failure, coronary disease leading to papillary muscle dysfunction, or be due to rheumatic heart disease. Associated conditions affecting mortality in the elderly include high blood pressure, obesity, elevated serum cholesterol, albuminuria, and right bundle-branch block.
Acute and Subacute Bacterial Endocarditis
The acute variety of endocarditis is uncommon in geriatrics. When present, the rapid deterioration and high fever is often confused with diabetic acidosis, bronchopneumonia, cerebral hemorrhage, or coronary thrombosis. In the elderly, the subacute variety is more common and usually secondary to skin, sinus, dental, urinary bladder, and lower intestinal infections. Lowered endocardial resistance is often the result of heart valves being damaged by rheumatic, degenerative, or congenital diseases; especially in patients suffering from diabetes, collagen disorders, or lymphomas. Multiple, nonspecific signs and symptoms make diagnosis difficult. If the aortic valve becomes damaged, the resulting congestive heart failure offers a poor prognosis.
Luetic Heart Disease
As in subacute bacterial endocarditis, leutic heart disease offers an obscured clinical picture. While calcification of the ascending aorta may suggest a leutic condition, aortic aneurysms are more likely from arteriosclerotic and degenerative origins. Aortic insufficiency is more likely of rheumatic origin leading to aortic stenosis. While atrial fibrillation is commonly associated with luetic heart disease, tertiary lues of the CNS is rare.
Effects of Hyperthyroidism
It is not uncommon in the elderly to find chronic heart failure underlined by thyrotoxicosis, even if the hyperthyroidism is mild. Characteristics include atrial fibrillation, persistent tachycardia, dyspnea, palpitation, and reduced perspiration. However, other signs of thyroid overactivity such as tremor, weight loss, emotional disturbances, bulimia, and ocular changes may or may not exist.
Effects of Hypothyroidism
Compared to hyperthyroidism, hypothyroidism is the more common geriatric condition because of the higher incidence of associated coronary artery disease. Myxedema is frequently seen in patients and associated with anemia, arthritis, mental torpor, constipation, weight gain, general weakness, and characteristic neurogenic facial signs.
Cardiac Arrhythmias and Conduction Disturbances
While not completely understood, most of these disturbances are attributed to degenerative changes affecting the common bundle and its branches, the mitral annulus, pars membranacea, central fibrous body and/or base of the aorta. Complete heart block is a common result of a severe lesion to the atrioventricular node and bundles. Muscle loss, collagen increase, and fat infiltration can involve sinoatrial and atrioventricular nodes, as can coronary artery disease or occlusion.
Atrial arrhythmias and conduction disturbances can be due to a right bundle-branch block, residua of rheumatic fever, epicardium and pericardium metastases particularly from pulmonary carcinoma, hypokalemia, angina, and coronary insufficiency. While atrial fibrillation predisposes the patient to emboli infarction, premature ventricular beats may predispose ventricular tachyarrhythmia or indicate toxicity.
Congestive Heart Failure
At least half the elderly, whether ambulatory or incapacitated, show signs of congestive cardiac failure. Predisposing conditions include ischemic heart disease, cardiac hypertension, cor pulmonale, mitral insufficiencies, cardiac hypertension, mitral insufficiencies, cardiac amyloidosis, calcific aortic stenosis, pulmonary embolism, subacute bacterial endocarditis, pericarditis (chronic), thyrotoxicosis or myxedema, bronchitis, pneumonia, congenital heart disease, and especially coronary artery disease.
COMMON PERIPHERAL VASCULAR DISORDERSArterial Disorders
The arterial disorders most commonly witnessed in geriatrics are arterial embolism, arteriosclerosis obliterans, diabetic vascular lesions, and aortic and peripheral aneurysms. See Figure 8.8.
Myocardial infarction and arteriosclerotic heart disease with or without atrial fibrillation are the most common etiologic factors in arterial embolism. Emboli may arise from mural thrombi (from a silent myocardial infarction), from aortic aneurysms, or from atheromatous plaques of the aorta or its major branches. Early diagnosis is important as at least half of peripheral arterial emboli lead to gangrene of the extremities.
Clinical findings will differentiate a dissecting aneurysm, arterial spasm, or arterial thrombosis from arterial embolism. Visceral emboli occur more frequently than generally suspected, and mesenteric, renal, and cerebral emboli are not uncommon. Management must be focused on immediate attention to the ischemia and underlying heart condition.
The most common cause for ischemic lesions in the extremities is arteriosclerosis obliterans. Studies show that the process is more often localized and progressing rather than generally distributed. Involvement of a single segment of the arterial tree is not uncommon. While the progression of aortoiliac occlusion may be slow, involvement of the femoral, popliteal, or tibial arteries may cause dramatic ischemia and gangrene.
Diabetic vascular lesions are the most common cause of death in the elderly diabetic. The vascular process is widespread, involving all arterial, peripheral, and visceral areas. Lesions range in size from large arterial forms to microscopic capillary types. Diabetic neuropathy and local infection are usually associated and tend to cloud the clinical picture.
Any agent that can weaken the arterial wall can cause aneurysm. Arteriosclerosis is the most common cause in aneurysm of the abdominal aorta and the major arteries of the extremities. Approximately 75% of abdominal aorta aneurysms are found in patients in the 70s or 80s. Associated conditions include a history of angina, myocardial infarction, congestive heart failure, occlusive artery disease, and aneurysms of the lower extremities.
Peripheral aneurysms commonly involve the femoral and popliteal arteries and can usually be palpated during examination. Associated conditions include hypertension, coexisting cardiovascular disease, and other aneurysms of the arterial tree --especially of the abdominal or thoracic aorta. Special attention should be given to the lower dorsal and lumbar sympathetics. While rupture is the greatest concern in abdominal aortic aneurysms, thrombosis and consequent gangrene is the greatest hazard in peripheral aneurysms.
Venous Conditions
The venous disorders most commonly witnessed in the senior citizen are venous thrombosis and pulmonary embolism. The incidence of both conditions increases with age.
Venous thrombosis is usually the result of thrombophlebitis of the lower extremities, especially of the veins of the calf as the result of chronic ailments and/or lack of exercise such as in convalescence. Thrombophlebitis of the iliofemoral segment, the inferior vena cava, and the superficial veins of the lower extremities are also common. Any condition leading to stasis and coagulation in the venous system can encourage thrombophlebitis and increase the risk of pulmonary embolism. While most thrombi occur in the venous plexus of the lower extremities, some occur in the pelvis and heart. Danger occurs when a lower thrombus may detach with the embolus migrating to the right heart with possible progression to the lungs.
COMMON HEMATOLOGIC DISORDERSNormal Variations
While geriatric anemia is common, the cause appears to be more commonly attributed to life-style rather than physiologic processes. Many reports indicate a change in the erythrocyte system, the leukocyte system, platelet and blood coagulation, and bone marrow, but other studies show insignificant changes attributable to age alone.
Aging and Hematologic Resources
Certain physiologic alterations during aging have been shown to affect the hematopoietic apparatus, which in turn affects the senior citizen's ability to adapt to environmental stresses and lowers resistance (both bacterial and viral). Characteristic of these alterations are lymph node and thymus atrophy, and decreased testosterone levels resulting in reduced circulating erythropoietin.
Frequently in the elderly, immunologic alterations encourage lymphoproliferative disorders such as lymphosarcoma, macroglobulinemia, chronic lymphocytic leukemia, reticulum cell sarcoma, and multiple myeloma. Several changes in bone marrow occur, but it is difficult to determine whether these are from chronic disorders or senescence. These changes are reflected in decreased hematopoietic cells with alteration of their ratio and increased reticuloendothelial system cells and tissue mast cells --probably the result of hormone imbalance.
Anemia, splenomegaly, or other clinical findings of hematologic disorder must be evaluated in geriatrics from the same viewpoint as held for younger patients, with the possible exception that the malignant or lymphoproliferative disorders have a higher incidence and thus demand greater concern.
Hemorrhagic Diathesis
While congenital hemorrhagic disorders are extremely rare in the senior citizen, several types of the acquired variety are witnessed. Symptomatic thrombocytopenia due to leukemia, aplastic anemia, and allied disorders are frequently observed. A tendency to hemorrhage may be noticed in patients with hepatic or renal insufficiency, marrow cancer, weakened blood vessels, or disorders affecting platelet dysfunction or enhanced fibrinolyses. Metastatic cancer, promyelocyte leukemia, and dysproteinemia are also associated conditions.
Leukemia and the Proliferative Disorders
Acute leukemia is not a rare geriatric condition; rather, it is often insidious on onset. Three acute and four chronic myeloproliferative disorders are seen in the elderly that frequently overlap or shift to one another. The acute disorders are acute granulocytic leukemia and acute myelosclerosis with myeloid metaplasia. The chronic disorders include chronic myeloid leukemia, polycythemia vera, thrombocythemia, and chronic myelosclerosis with myeloid metaplasia. Common features of these disorders are the proliferation of one or more lines of bone marrow elements (of a self-perpetuating character) and the absence of a demonstrable cause of the proliferation.
The incidence of polycythemia and myelosclerosis with myeloid metaplasia increases with age. Patients presenting with myelosclerosis and myeloid metaplasia typically show spleen enlargement, possible liver involvement, bone marrow fibrosis, and leukoerythroblastic anemia. The most common disorders are chronic lymphoid leukemia, Waldenstrom's macroglobulinemia, and myelomatosis. Other disorders classified as proliferative disorders seen in the elderly include lymphosarcoma, giant follicular lymphoma, reticulum cell sarcoma, and Hodgkin's disease.
Chronic lymphoid leukemia also has a high incidence in senior citizens and can take the benign form with few clinical symptoms or take the aggressive form exhibiting an intense clinical picture. The more common benign form is characterized by slow progress, unprominent splenomegaly and lymphadenopathy, decreasing gamma globulins and granulocytes, and a leukocyte count often remaining in a range of 15,000 to 50,000 per cubic millimeter.
Waldenstrom's macroglobulinemia is characterized by lymphocytes secreting an abnormal amount of high-molecular gamma globulin and the proliferation of atypical lymphocytes. It is associated with bleeding tendencies and mild hepatosplenomegaly and lymphadenopathy.
Myelomatosis is also a condition witnessed in patients over 50 years of age. In this disorder, the myeloma cells proliferate at extra- and intra-medullary sites. During the advanced state, rheumatic or neuralgic pain, nephritis like changes in the urine, an increased sedimentation rate, and anemia are characteristic.
Iron-Deficiency Anemia
This disorder more common in the young than in the elderly, yet it is the most common anemia of the elderly. Peptic ulcers, hemorrhoidal bleeding, and diaphragmatic hernia are the main etiologic factors in geriatrics. Clinical features include a microcytic hypochromic anemia associated with a lowered serum iron level and an increased unsaturated iron-binding capacity (UIBC). Gastric carcinomas in men and women and gynecologic cancer in women should always be considered. Achlorhydria may be a precipitating factor.
In late stages, characteristic tissue and epithelial changes occur such as thin, pliable, and brittle fingernails having longitudinal ridging progressing to koilonychia; dry inelastic skin; thin brittle hair; tongue atrophy progressing to Plummer-Vinson syndrome; and other signs attributable to impaired tissue nutrition because of depleted iron-containing enzymes. Treatment is the same as for younger age groups.
Pernicious Anemia
While not as common in the elderly as iron-deficiency anemia pernicious anemia is almost exclusively (in this country) associated with old age. In contrast to iron-deficiency anemia, pernicious anemia is a disorder of the whole hematopoietic apparatus, which includes general cellular metabolism, and results in a pancytopenia with reduction in white cells and platelets as well as anemia.
In contrast, iron-deficiency anemia is hypochromic and microcytic but pernicious anemia is normochromic and macrocytic. This latter condition is truly a nutritional anemia -- the fundamental cause being B-12 deficiency.
Injectable B-12 appears to be more efficient than oral supplementation in stabilizing the patient.
Clinical signs of pernicious anemia besides the hematologic abnormalities include marked tongue atrophy with flattened papillae, yellow pallor of the skin, prematurely gray or white hair, and hepatosplenomegaly. In advanced stages, all levels of the central and peripheral nervous system can be involved, resulting in profound neurologic lesions. The condition is characterized by a loss of vibration sense over the toes, loss of proprioception sense, loss of Achilles or patellar reflexes, paresthesias, and possible dementia. Associated or subsequent gastric carcinoma should be considered. In spontaneous myxedema, a megaloblastic anemia may develop that is indistinguishable from pernicious anemia.
Folic Acid Deficiency
Folic acid deficiency is another common factor in geriatric anemia. Deficiency affects DNA synthesis much the same as B-12 deficiency. Clinically, the epithelial and neurologic pictures are not as widespread or as severe. Here, diet is more important as the body does not store folic acid in quantities as it does for B-12. The condition is commonly associated with alcoholism and often blended with the features of cirrhosis and fatty liver.
While maintenance therapy is usually life-long in pernicious anemia, it need not be so in folic acid deficiency. Return to normal hematopoiesis is more often the rule than the exception. Studies show that folic acid deficiency is almost always associated with vitamin C deficiency, which compounds the condition as ascorbic acid acts as a cofactor aiding in the reduction of folic acid to its active coenzyme form.
Other Nutritional Anemias
Deficiencies of riboflavin, niacin, B-6, and vitamin E have also been attributed to deficiency anemias, but these are rare in the elderly.
Symptomatic Anemias
The so-called symptomatic anemias are those related to an underlying disease and represent a major category in the anemias of the elderly. While all types of cancer represent the foremost disorders involved, renal failure anemia, chronic infection anemia, and uremic anemia are occasionally seen.
COMMON DIGESTIVE AND GASTROENTEROLOGIC DISORDERSThe digestive system of the elderly probably causes more discomfort, distress, and annoyance than any other system in the body. This is as much to following misinformation as it is to specific disorders. On the other hand, a doctor should not be too eager to drastically alter senior citizens' diets. The elderly have had may years of experimentation and have acquired through trial and error a good idea of what they can and cannot easily digest. Biologic adaptation to some unusual diets and eating customs is common. Nevertheless, certain aging processes in the elderly predispose digestive and gastroenterologic disorders.
Progressively with age, secretions of hydrochloric acid and the digestive enzymes of the stomach, pancreas, liver, and intestines diminish. Motility of the gastrointestinal tract becomes modified. Muscular atrophy of the small and large intestines occurs along with a decrease in mucus secretion, which contributes to constipation. Habits and life-style often lead to weakened abdominal muscles, general inactivity, anorexia, and inadequate fluid intake. Habitual frequent use of laxatives may be a problem.
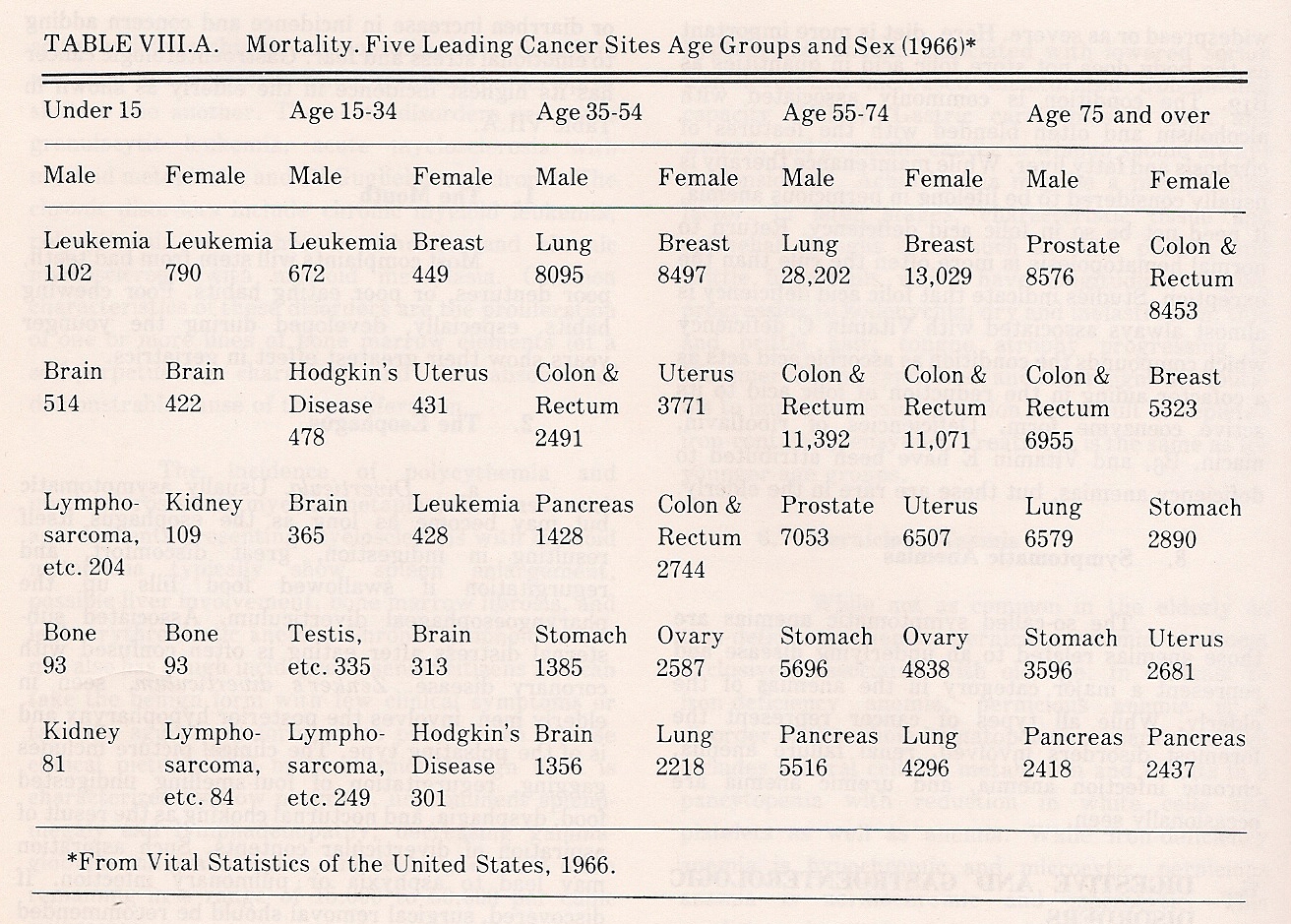
Protein undernutrition may lead to hepatic fatty infiltration, and cirrhosis gives the same picture as found in younger groups. Symptoms of heartburn, gas, dyspepsia, flatulence, constipation, or diarrhea increase in incidence and concern, adding to emotional stress and fear. Gastroenterologic cancer has its highest incidence in the elderly. See Table 8.1
Table 8.1. Mortality in Five Leading Cancer Sites, Age Groups, and Sex
The Mouth
Most geriatric complaints stem from bad teeth, poor dentures, or poor eating habits. Poor chewing habits developed during the younger years show their greatest effect in late life. See Figure 8.9.
The EsophagusEsophageal Diverticula. This disorder is usually asymptomatic, but the mass may become as long as the esophagus itself, resulting in indigestion, great discomfort, and regurgitation if swallowed food fills the pharyngoesophageal diverticulum. Associated substernal distress after eating is often confused with coronary disease. Zenker's diverticulum, discovered in some elderly males, involves the posterior hypopharynx and is of the pulsating type. The clinical picture includes gagging, regurgitation of foul-smelling undigested food, dysphagia, and nocturnal choking as the result of aspiration of diverticular contents. This aspiration may lead to asphyxia or pulmonary infection. If discovered, surgical removal should be recommended for all significant diverticula.
Esophageal Spasm. Simple esophageal spasm is the result of interference with normal nervous control and is usually localized. It may be a signal of an upper thoracic subluxation complex, especially if episodes of upper extremity paresthesia are associated. Dysphagia is the chief symptom. Achalasia produces a spasm of the esophagogastric junction and is characterized by difficulty in swallowing and lower abdominal distress. A corkscrew or curled esophagus can cause a diffuse esophageal spasm in the elderly, but it is not limited to this age group. Typical symptoms include severe substernal (coronary type) pain and rapid irregular nonpropulsive contractions.
Schatzki Ring. This is a thin, diaphragm-like constriction of the lower esophagus just above the cardia. Typical symptoms are intermittent dysphagia, pain on swallowing solid food, and coronary like substernal pain. Various degrees of a hiatus hernia are sometimes associated.
Barrett's Ulcers. These ulcers involve any portion of the columnar-lined segment of esophageal mucosa near the esophagogastric junction.
Reflux Esophagitis. Esophagitis is commonly associated with hiatus hernia, obesity, and the eating of highly spiced foods. Postmeal distress is common, along with long-term heartburn. Frequent regurgitation can result in esophageal "burning" and tissue erosion, progressing to stricture from scar tissue. Bleeding may occur, as may a cryptic iron-deficiency anemia.
Hiatus Hernia. This protrusion occurs from rupture of the upper part of the stomach through the diaphragm at the esophagogastric junction. Strangulation is rare. This hernia is frequently seen after the age of 50. Symptoms include gaseous dyspepsia, postmeal distress, nocturnal discomfort, heartburn, dysphagia, aerophagia with belching, regurgitation and frequent vomiting, and either covert or massive bleeding.
Peptic ulcer and carcinoma of the lower esophagus may exhibit the same symptoms. Esophageal ulcers, stricture, and esophagitis may be superimposed. Associated cholecystitis and diverticulosis are not rare. The pain of hiatus hernia may suggest coronary artery disease. Differentiation from a coronary disorder is made by the fact that distress comes at rest when prone and rarely after exercise, yet both conditions present distress after a heavy meal.
Benign Tumors. Benign tumors are rare in this area except mucosal polyps and leiomyoma. Polyps may protrude into the stomach or mouth. Angiomas, lipomas, and fibromas occasionally produce cryptic bleeding with dysphagia.
Malignant Tumors. Chronic achalasia is associated with esophageal carcinoma that may affect the hypopharynx, the midportion of the aortic arch, or the distal end of the esophagus. Metastatic spread to the mediastinum and lymphatic spread to the stomach and liver are common. The clinical picture presents increased thirst and salivation, chronic hiccups with bleeding, anemia, and progressive suffering.
The Stomach
Stomach disorders may be confused with intestinal disorders because of stomach position. In thin women especially, the stomach may lie quite low in the abdomen. Interference with either the vagus or sympathetics should be suspected in most cases of stomach disorders found in the elderly.
Achlorhydria, ulcers, and tumors are customarily symptomatic. Both hypertrophic and emphysematous gastritis are rare. Polyps are common and usually asymptomatic, but they may be associated with bleeding and predispose carcinoma. Gastric diverticula increase in incidence with age; however, they rarely are distressing.Achlorhydria. Achlorhydria is usually associated with abdominal gas, belching, bloating, and sometimes loose stools.
Peptic Ulcers. Stomach and duodenal peptic ulcers are commonly located in the antrum but may be found in the stomach curvature or fundus. Related bleeding and perforation are rare, but they do occur. Epigastric distress is not necessarily relieved after eating. The ulcer or ulcers may or may not be associated with abnormal gastric acids.
Disorders such as cerebral hemorrhage and thrombosis, and chronic pulmonary disease (especially emphysema) can underlie stress ulcers. In the elderly, drug-induced ulcers prevail (eg, induced by aspirin and cortical steroids) and are associated with bleeding. Stools tests for occult blood should be routine when suspicions arise.
Tumors. Benign tumors are rare. Occasionally, polyps and cysts will be witnessed. Schwannomas, lipomas, fibromas, and bezoars (rare) are unusual. Carcinoma is associated with chronic gastric mucosa atrophy and coincidental with pernicious anemia. Most gastric cancers are infiltrating, ulcerative, or hypertrophic adenocarcinomas, ordinarily involving the pylorus or antrum of the stomach. Metastatic, venous, and lymphatic spread is common and can affect the entire abdomen, pelvis, chest cavity, bones and brain.
The clinical picture includes epigastric pain and tenderness, anorexia, weight loss, anemia, liver enlargement and hardening, hematemesis, and melena, but bleeding is rarely profuse. In late stages, a gastric mass may be felt and rectal examination may reveal pelvic metastases. Sarcomas are more common in younger age groups. Sarcomas are bulky, bleed profusely, are rarely obstructive, and have a slower course of development.
The Duodenum
The most common duodenal lesion is ulceration; however, the clinical picture in the elderly is not as clear cut as in younger age groups. The associated distress is usually irregular and unrelated to food intake. Severe gaseous dyspepsia is the rule.
Duodenitis without ulceration is common in the elderly, and the clinical picture is similar that of peptic ulcer. Polyps may occur; they are usually small and benign yet difficult to differentiate from carcinoma even with special tests.
The Liver, Biliary Tract, and GallbladderHepatitis. Even if hepatitis is uncommon in the elderly, its possibility should be kept in mind. Although painless jaundice is usually associated with a malignant obstruction of the common duct, hepatitis could be the cause with or without jaundice. The characteristic picture is a gradually progressing illness, anorexia, and low-grade fever.
Cancer of the pancreas and hepatobiliary duct is associated with half the cases of jaundice in the elderly. The other half is due to such benign disorders as hepatitis, cirrhosis, cholecystolithiasis, drugs, and hemolytic disorders. Painless jaundice from common-duct obstruction by a stone is common. Pancreas carcinoma often offers hepatic symptoms and is associated with severe epigastric and/or back pain. This fact can easily be overlooked when the history and physical are rushed.
Cardiac disease is often coincidental with hepatitis and clouds the picture. The incidence of viral hepatitis is increasing in the aged. A parasite type, acute granulomatous hepatitis, is rare. It can occur at any age.
Cirrhosis. In the elderly, hepatic cirrhosis is usually the result of chronic hepatitis associated with alcoholism and characterized by an enlarged nodular liver and a chronic jaundice. Fat absorption is poor, and ascites may become marked in the late stages. Bile in the urine is a significant finding.
Biliary Stones. The incidence of gallstones in the elderly increases progressively with age, but the stones are often asymptomatic. Renal calculi, peptic ulcer, or carcinoma of the hepatic flexure will generally offer a similar symptomatic picture. Severe pain with evidence of cholangitis and obstruction may result in a recommendation of possible cholecystostomy. Perforation is suspect if symptoms appear of acute cholecystitis, high fever, reflex shoulder pain, jaundice, moderate leukocytosis, and rigidity and tenderness in the upper-right quadrant. Predisposing cholecystitis may be seen at any stage. It begins as a mild gaseous dyspepsia; progresses to severe distress, distention, epigastric and right quadrant pain; and then to severe colic.
Gallbladder Carcinoma. This disease is especially a geriatric disorder and more common in women as are most gallbladder disorders. Direct extension of the tumor into the liver and common bile duct is common, and distant metastases are seen in the later stages. It is commonly associated with stones, but the relationship is unclear.
The clinical picture presents with early pain in the upper-right quadrant followed by anorexia, nausea, vomiting, weight loss, constipation, and general weakness. Jaundice and common-duct obstruction with cholangitis are frequently related. Sarcomas of the gallbladder, however, are rare.
The PancreasPancreatitis. Pancreatitis can occur at any age. While the etiology is usually unknown, sympathetic and parasympathetic nerve irritation should be suspect, with obesity and excessive alcohol consumption acting as predisposing factors. Two major types are seen. The most severe form, hemorrhagic pancreatitis, is an acute pancreatic necrosis characterized by hemorrhagic infiltration of the pancreas parenchyma and fat necrosis. The other form, interstitial pancreatitis, is an acute pancreatic edema featuring parenchymal edema, pressure necrosis, and inflammation.
Pancreatitis is reported secondary to trauma, vascular accidents, febrile disorders, acute cholecystitis, and the reflux of bile into the pancreas through the common biliary duct. The typical clinical picture is one of gradually rising pain that becomes severe and may last for several hours. The pain is usually located in the upper-left quadrant, often referring to the back at the same level, but it may spread to include the entire lumbar area and lower abdomen. Sometimes the pain is localized in the right iliac area, mimicking a sacroiliac disorder.
Other symptoms include nausea, vomiting, anorexia, bloating, unusual fatigue, generalized abdominal tenderness with abdominal wall rigidity, and left costovertebral angle tenderness. Signs of peritonitis may appear if necrosis is widespread. At times, serum pancreatic enzyme levels will be high, blood glucose levels will be high, and lymphopenia and a low-grade hypochromic normocytic anemia will be present. Chronic relapsing pancreatitis can occur at any age, but it is more common in the elderly. Pancreas calcification and lithiasis are often associated.
Pancreatic Carcinoma. This tumor is usually an adenocarcinoma of the ductal epithelium infiltrating to the duodenum and spreading to distant parts through the veins or lymph ducts. Liver, lungs, and bone are common metastatic sites. The patient presents with general weakness, anorexia, weight loss, and wasting. Epigastric pain radiates to the back, which is relieved by bending forward. The pain often becomes worse at night. Other symptoms include dyspepsia, belching, nausea, heart burn, intermittent diarrhea and constipation, signs of obstructive jaundice, emotional depression, and possibly fever.
In late stages, the liver becomes enlarged and hardened by metastases, an epigastric mass may be palpable, and the gallbladder may be enlarged and palpable. Splenomegaly, ascites, and peripheral edema appear with portal vein obstruction. Deep or superficial venous thrombi, multiple and migratory, are often an early sign. While blood in the stool may be from diabetes, the diabetes may be the result of neoplastic destruction of the islets. A glucose tolerance test is usually essential within a comprehensive diagnostic work-up.
The Small Intestines
See Figure 8.10.Regional Enteritis. While more commonly found in the young, this disorder may be discovered in geriatrics. Lesions are usually localized near the end of the small bowel and are characterized by granulomatous, necrotizing, ulcerating, and cicatrizing lesions. The typical clinical picture presents abdominal cramps, fever, anemia, diarrhea, weight loss, and perianal abscesses. Fistulas, obstruction, and bleeding are serious complications. Obstruction is usually the result of edema and cellular infiltration of the bowel wall; surgery is imperative. Postmeal colic, rheumatoid polyarthritis, erythema nodosum, and pyoderma gangrenosum can be associated.
Hemorrhagic Intestinal Necrosis. This disorder is commonly localized in the small intestine, but it may extend to the stomach and large bowel. It is usually secondary to reduced circulatory flow because of severe heart disease, shock, or a reduced cardiac output causing venous dilatation and mucosal bleeding. Ischemic necrosis is the result of local anoxia and may extend to the liver and spleen.
Meckel's Diverticulum. It is possible for a person to go through childhood and the maturity years yet not have trouble with Meckel's diverticulum until late in life. In such a case, inflammation is common, but bleeding is rare. The common clinical picture presents discomfort near the umbilicus, just left of the vermiform appendix. Fever, leukocytosis, and abdominal distention may be present and confused with appendicitis, ileocecal spasm, or colonic diverticulitis.
Superior Mesenteric Vascular Occlusion. An acute abdominal catastrophe results from sudden closure of the superior mesenteric artery or vein by an embolus or a thrombus. This leads to drastic peritoneal irritation and intestinal obstruction. Usually affecting the ileum or jejunum, the disorder features congestion, inflammation, obstruction, and ischemic necrosis. Severe vomiting, pain, abdominal distention, shock, hemoconcentration, leukocytosis, and bloody diarrhea are characteristic. Early hyperactive bowel sounds disappear with peritonitis, spasm, and fever. Prognosis is poor even with immediate massive bowel resection.
The Malabsorption Syndrome. Not uncommon in the elderly, this sprue-like syndrome is characterized by abdominal and watery stools containing excessive amounts of fat. Pallor, anemia, and subcutaneous hemorrhages may occur.
Abdominal Angina. A calcific plaque at the aortic orifice, or a mural thrombus or atherosclerotic narrowing involving the superior mesenteric artery, can result in arterial insufficiency. Ischemia of the intestinal wall results that leads to pain after eating. This pain is often localized in the upper abdomen while walking and relieved in the prone position. Severe attacks, called intestinal claudication or Pal's crisis, usually begin about a half hour after a heavy meal and last for about 2 hours. Sometimes the pain is restricted to the back.
Abdominal Apoplexy. This vascular accident is the result of a spontaneous rupture of an intra-abdominal vessel. The rupture is usually the result of long-standing local atherosclerosis, polyarteritis nodosa, aortic aneurysm, or aneurysms of the splenic and inferior pancreaticoduodenal arteries. However, the most commonly affected tissues are the gastric and superior mesenteric arteries. An initial slight bleeding episode is usually followed by severe hemorrhage.
Small Intestine Scleroderma. Subcutaneous scleroderma may progress to the small intestines and esophagus. If the small intestine is involved, the bowel has a localized thick wall with distended loops, and symptoms of malabsorption are featured. Dysphagia is the major feature of the esophageal variety.
Malignancies of the Small Intestines. Neoplasms of the small intestines are rare and generally found in males.
Adenocarcinomas usually involve the papilla of Vater and result in obstructive jaundice (fluctuating). The major features are bleeding, epigastric pain, nausea, anorexia, weight loss, and symptoms of intestinal obstruction.
Lymphosarcomas, usually multiple, involve the terminal portion of the small bowel. Features include pain, fever, malabsorption with steatorrhea, and a palpable abdominal mass. Bleeding and obstruction signs are usually minimal.
Carcinoids often metastasize to the liver from the stomach, ovary, or bronchus and are associated with such diverse symptoms as asthma, right-heart disease, hypotension with tachycardia, dyspnea, facial edema and cyanosis, and flushing attacks accompanied by abdominal discomfort. Flushes may occur several times a day and last up to an hour, appearing after ingestion and emotional stress.
Intestinal Obstruction. Both mechanical and paralytic intestinal obstructions occur.
Mechanical obstruction is the result of adhesions, volvulus, diverticulum, hernias, tumors, gallstones, fecaliths, or worms. Features include severe cramping, pain, vomiting from small bowel obstruction, distention, constipation, and prominent borborygmi.
Paralytic (adynamic) obstruction is associated with peritonitis, septicemia, pneumonia, pancreatitis, ureteral calculus, biliary colic, myocardial infarction, retroperitoneal hematoma, hypopotassemia, retrograde pyelography, and mesenteric thrombosis. Features include mild or absent pain, frequent vomiting, distention, and constipation. Borborygmi are absent.
The Large IntestineIntestinal Tuberculosis. TB of the gut may occur in either the ulcerative or hyperplastic form. The typical clinical picture presents progressive weight loss, low-grade fever, anorexia, and an irritable bowel with periodic loose stools. Ulcers in the large colon usually run transverse to the long axis. In the small bowel, they appear irregular in both shape and distribution. Both forms are most often localized in the ileocecal area. The hyperplastic type may appear as an asymptomatic mass and is not uncommonly found in the sigmorectal area. X-ray film analysis might reveal an old lung lesion.
Acute Appendicitis. Because of the mistaken belief that appendicitis is rare in the elderly, a higher mortality and morbidity is seen as the result of delayed diagnosis and treatment. In addition, the clinical picture is slightly different in the elderly. Manifestations are milder, perforation is earlier, pain is milder and often atypical, fever is minimal, and drastic leukocytosis may be absent.
Diverticulosis and Diverticulitis. These disorders are usually confined to patients in the upper age bracket. The diverticula (especially of the large bowel) may become so extensive that a deficiency syndrome results from definite interference with nutrient absorption; thus, it's sprue-like in character. Gradual weight loss and progressive deficiency symptoms are characteristic. If inflammation exists, abdominal cramps from diverticulitis are experienced. The sigmoid is the most common site of inflammation, but it may occur at any point. Fistula and perforation may develop. Asymptomatic diverticula are common in the elderly. Surgery is usually necessary if severe infection or obstruction occurs.
Irritable Bowel Syndrome. This symptom complex occurs in the elderly as well as in the young. While any chemical, mechanical, or psychic irritation may affect the bowel, emotional states especially register effects. Excitement, prolonged tension, fear, deep worry, and other emotional stresses are reflected in loose stools progressing to diarrhea.
Amebiasis. Foreign travelers, especially those from Mexico and the Orient, may present with symptoms of amebiasis characterized by dyspepsia, fatigue, anorexia, periodic diarrhea or dysentery. Rectal mucosal inflammation may exist along with ulcers. Increased international travel has also increased the incidence of other parasitic problems. Treatment is the same as in the young.
Polyposis. Polyps are seen in five varieties: singular, multiple, disseminated, diffuse, and those secondary to inflammatory disease such as ulcerative colitis. The latter may be classified as either carcinomatous, adenomatous, or pseudoadenomatous. Rarely do these polyps cause bleeding or become malignant except the carcinomatous type, which is often familial.
An inherited triad consisting of multiple polyps of the large intestines predisposed to malignancy, Gardner's syndrome, is seen in association with bone and soft-tissue tumors.
Polyposis with ectodermal changes (Cronkhite-Canada syndrome) involves the entire gastrointestinal tract and is characterized by alopecia, nail atrophy, skin pigmentation, and profuse diarrhea.
Villous adenoma, a papillary polypoid lesion usually found in the sigmoid or rectum, has a high malignancy incidence. Features include bleeding and watery diarrhea that may become profuse enough to result in mild dehydration progressing to severe weakness, vascular collapse, and paralysis.
Ischemic Colitis. This disorder is the effect of colonic ischemia and infarction because of circulatory hypotension from septic shock or disease of the inferior mesenteric artery. Intramural gas is usually present, suggesting ischemic necrosis potentially leading to shock and infection. Spontaneous ischemic proctitis is seen whose features include abdominal pain; rectal bleeding; sigmoid nodes, polyps, and ulcers; mucosal edema and ulceration; and progress to rectal stricture is sometimes witnessed.
Chronic Ulcerative Colitis. This condition may manifest itself as acute, progressing, chronic, exacerbating, or fulminating. Features include general depletion, weight loss, diarrhea, pallor, anorexia, low-grade fever, mild-to-severe abdominal distention, and bleeding. In the course of a long-standing condition, rectal strictures, toxic colonic dilatation, and malignant neoplasms may occur.
The Bloater Syndrome. This clinical picture is frequently seen in elderly women of highly emotional temperament. It is characterized by obvious abdominal distention not the result of intra-abdominal disease. Examination reveals marked lordosis and bilateral diaphragm fixation. Lumbar flexion in the side position frequently offers quick relief, but it is not permanent until the emotional problems are relieved.
Note: The etiology of the bloater syndrome can be either psychosomatic or somatopsychic, or a noxious cycle of both. It is unfortunate that contemporary chiropractic research has been so wanting in this area of mind< >body disorders. This was not true in the 1950s, when the work of Herman Schwartz, DC, focused international attention on chiropractic management of many "behavioral" disorders.
Colon and Rectal Cancer. While rectal cancer is more common in men, cancer of the colon is more common in women. Incidence in both sexes increases with age. Ulcerative, stenosing, infiltrative, or proliferative adenocarcinomas are seen that may metastasize by direct extension or by lymphatic or hematogenous dissemination. Features include dull pain, bloody stools, colitis symptoms, anorexia, general weakness, weight loss, borborygmi, obstruction symptoms, anemia, and a palpable mass. Sometimes the only symptom is sciatic or back pain when the tumor infiltrates the sacral plexus. Thus, rectal and abdominal examination is necessary along with spinal and pelvic analyses.
Chronic Constipation. The elderly are generally predisposed to constipation. This is usually the result of lack of physical activity, abdominal weakness, inadequate fluid intake, excessive starch intake, and the habitual use of laxatives and opiates. However, before dietary considerations are made, causes such as partial intestinal obstruction, hypercalcemia, neurologic cord lesions, myxedema, diabetic autonomic neuropathy, intestinal strictures, tumors, and tissue spasms should be eliminated.
Fecal Impactions. Chronic constipation requires careful abdominal and rectal examination to determine suspect masses, fecaliths, obstruction, ascites, distention, or inflammation. Fecaliths may be mistaken for tumors; however, tumors are usually more fixed. Fecal impactions and stercoroma are common in the elderly and usually felt as a hard movable mass in the lower-left quadrant, but one may appear in the ascending colon.
Bleeding of the Digestive Tract
While hematemesis and tarry stools are features of upper-GI bleeding, lower tract bleeding is characterized by bright red blood. However, bright blood from the upper tract will occur if transit time is rapid, and dark blood from the colon will occur if the bowel is sluggish and the bleeding is not severe. Bleeding is usually associated with ischemia, polyps, fibromas, lipomas, lymphomas, diverticula, uremia, cryptic anemia, hiatus hernia, colon carcinoma, and internal piles.
Urinary Tract and Gastrointestinal Symptoms
Urinary tract disorders frequently present with gastrointestinal symptoms as a result of their proximity and common innervation. Urinary calculi, urinary tract infections, uremia, and prostate disorders all present GI signs and symptoms. See Figure 8.11.
Diabetes Mellitus and Its Gastrointestinal Symptoms
Pernicious anemia and gastritis are commonly associated with the diabetic elderly. Most of the gastrointestinal conditions related to diabetes are the result of diabetic autonomic neuropathy. In this gastritis, hydrochloric acid secretion is diminished, colon bacteria migrate into the stomach, and the stomach becomes atonic and dilated, food is retained, and symptoms of pyloric obstruction arise. Other features include a watery nocturnal diarrhea, abdominal distention, and sigmoid volvulus with megacolon. More rarely, difficult swallowing, megaesophagus, and an enlarged gallbladder are associated.
COMMON UROLOGIC DISORDERSPathologic States
Just as urinary disorders are a primary concern in pediatrics, they become an increasing concern in geriatrics. Unfortunately, urinary tract obstruction from benign prostatic hypertrophy or asymptomatic prostatic carcinoma exhibit few symptoms until the condition is well advanced; thus the need for routine urinalysis and digital prostate examination.
Cerebral vascular accidents and myocardial infarction can result in urinary retention requiring catheterization. However, the use of an indwelling catheter has received criticism as it is often associated with the development of chronic urinary tract infection.
Two major complaints are invariably heard in geriatrics: mental confusion and urinary incontinence. Both have many causes of a mechanical, chemical, and psychic nature. In reference to the genitourologic conditions of geriatrics, sexual dysfunction, kidney lesions, bladder lesions, prostate lesions, urethra lesions, and penis and scrotal lesions are the most commonly reported.
Urinary Tract Infection
The incidence of urinary tract infection is much higher in institutionalized populations than those living in a residential environment. Infection may be either acute or chronic. The clinical picture is similar to that of the young.
Aging and Neurogenic Disorders
Bladder disturbances in the elderly are often noted such as diminished capacity, increased residual urine, and uninhibited bladder contractions resulting in urgency and incontinence. Thus, the aging bladder grows progressively inefficient in both filling and emptying. This is generally attributed to arteriosclerotic changes above the level of the midbrain. Atrophy of the frontal cortex especially contributes to impairment of the micturition reflex. Funneling of the bladder outlet is often found in the elderly, especially in women, which may be a reflection of a pelvic diaphragm incompetence associated with cystocele. In elderly men, bladder diverticula are common. In either gender, however, the cause or precipitating factor may be a thoracolumbar subluxation complex.
Neurogenic bladder disorders can be classified into four distinct types:
The atonic neurogenic bladder. Commonly seen with tabes dorsalis, this type of disorder is associated with involvement of the posterior sacral nerve roots resulting in dysfunction of the afferent fibers of the reflex arc. While reflex micturition is lost, voluntary control is possible. The bladder becomes atonic as a result of chronic overdistention because of abolished sensation. It is not uncommon for a chronic sacroiliac syndrome to be involved; less frequently, a lower thoracic or upper lumbar subluxation.
The autonomous neurogenic bladder. Lesions involving the sacral cord or cauda equina result in interruption of both afferent and efferent fibers of the reflex arc. The effect is that sensation is abolished, both reflex micturition and voluntary control are lost, with the bladder emptying by small contractions initiated by local myoneural irritation. The examiner's first suspicion should be a thoracolumbar subluxation etiology, but the editor has occasionally found an upper cervical focus.
The reflex neurogenic bladder. A lesion located between the sacral reflex center and the midbrain results in the destruction of both afferent and efferent fibers, such as in complete cord transection. Along with paraplegia, bladder sensation is destroyed, micturition is reflex, unconscious, and uninhibited.
The uninhibited neurogenic bladder. A lesion of the micturition center in the frontal cortex or to partial destruction of spinal pathways can lead to loss of central inhibition leaving the sacral reflex arc predominate. Partial bladder distention results in uninhibited contractions causing low volume emptying. This type disorder is common in old age and is associated with stroke, frontal lobe tumor, and cerebral arteriosclerosis.
Urinary Incontinence, Retention, and Dysuria
In the elderly, a predisposing factor and a precipitating factor are usually involved in urinary incontinence. As described above, the predisposing factor is usually an uninhibited neurogenic bladder of various consequence. The precipitating factor may be illness requiring bed confinement, urinary infection, stroke, mental confusion, or overstress exhaustion. In these conditions, involvement affecting the sacral reflex arc should be suspected. In women, the genital tract and the trigone of the bladder have the same embryonic origin, thus neurohormonal dysfunction may have some effect on bladder control.
Urinary retention in the elderly may be witnessed with or without incontinence. In women, the most common cause is fecal impaction. In men, the common cause is prostatic hypertrophy. See Figure 8.12. In both sexes, the atonic neurogenic bladder is suspect.
Stress incontinence is often seen in elderly women and is probably the result of an associated pelvic diaphragm weakness. If so, stimulation of the pelvic diaphragm, "bloodless surgery" massage, reflex technics, and prenatal type exercises may be helpful adjuncts. A pessary is sometimes helpful, but surgery might be justified in severe cases. When stress incontinence coexists with an uninhibited neurogenic bladder, treatment directed to the musculature of the pelvic floor is usually inefficient.
Renal Disorders in Latter Life
Chronic renal failure progresses with age. Optimal maintenance includes low protein intake and prevention of renal acidosis. The anemia of chronic renal failure is often noted. Quite frequently, chronic pyelonephritis and nephrosclerosis are coexistent. Less common causes of chronic failure in the elderly include chronic glomerulonephritis, diabetes, malignant hypertension, carcinoma, hyperparathyroidism, carcinoma, myelomatosis, and amyloid disease. In elderly men, uremia resulting from prostatic enlargement leading to bladder outlet obstruction is frequently found.
Kidney Lesions
Any chronic renal obstruction or infection may result in uremia.
Asymptomatic pyelonephritis of long standing may not appear clinically until later life.
Calculus disease is usually not significant unless associated with pain, hematuria, gout, or infection.
Renal carcinoma may metastasize to the chest, to the bones resulting in pathologic fractures, or to intracranial sites resulting in psychoses.
Renal tuberculosis is occasionally witnessed and characterized by hematuria and pyuria in the absence of urine bacteria.
Bladder Lesions
In elderly women, chronic recurring attacks of cystitis, urinary tract infection, bladder neck contracture, neurogenic bladder dysfunction, and marked cystourethrocele are seen. In the elderly male, cystitis is unusual unless associated with pyuria, prostate infection, bladder stones or tumor, or some form of bladder outlet obstruction.
The incidence of bladder calculi is increasing; ie, both sexes in the aged. Neurogenic bladder dysfunction, previously described, is frequent. Occasionally, periurethral inflammation leads to abscess formation. Neoplasms of the bladder are frequently carcinomatous.
Prostate Lesions
Prostatism produced by vesical neck obstruction is the result of prostate carcinoma, contracture of the vesical neck, or nodular hyperplasia. In carcinoma of the prostate, little obstruction occurs until the disease is in an advanced state. In contracture of the vesical neck, characteristics include frequent nocturia, progressing hesitancy, and bleeding if nodular hyperplasia occurs.
Urethral Lesions
Urethral carcinoma is not seen frequently or is urethral structure from gonorrhea. When present, symptoms often mimic those of bladder neck obstruction.
Penile and Scrotal Lesions
Lesions affecting the penis in the elderly are typically the result of tumor or inflammation. Penile carcinoma is only seen in the uncircumcised as it is associated with an unretractable foreskin. In the elderly uncircumcised diabetic, chronic infection and scarring may lead to balanitis xerotica obliterans. Occasionally, sebaceous cysts of the scrotal skin may become infected. Transillumination may reveal a hydrocele of the tunica vaginalis. Spermatocele is usually asymptomatic. Testicular epididymo-orchitis may be associated with coexisting urinary tract infection. Testicular tumors are rare in the elderly, but seminoma is occasionally encountered.
Sexual Dysfunction
Both diabetes and generalized atherosclerosis can produce low levels of sexual activity. Thus, two important tests to include are a 5-hour blood glucose level determination and palpation of pedal pulses.
COMMON DERMATOLOGIC DISORDERSAging Considerations
External Changes. Cumulative effects of environmental exposure insults, acquired dysfunctions and trauma, and hereditary characteristics influence the skin's aging process. At the cellular level, keratin formation is slower during old age, and the epidermis is flattened and shows cells of various size and shape. The skin reveals signs of dryness and thinning with xerosis and atrophy. Sebum, sweating, and other gland secretions are reduced. This is related to changes in the adnexal structures, a lowered androgen level, a decreased number of sweat glands, diminished function of the eccrine glands, and apocrine gland atrophy.
The skin becomes less elastic, scale-like, and less pliable or resilient due to degenerative changes in collagen and elastic fibers and decreased water content. Skin changes are manifested by patches of pigment or freckles, especially in areas exposed to the sun. Nails become brittle and tend to peel. Loss of facial skin elasticity is accompanied by wrinkles, deepened forehead and nasolabial lines, drooping eyelids, and fan-shaped radiating lines around the eyes and mouth. The number of scalp hair follicles reduces, and the hair is finer. Nose and ear hair thicken, and facial hair often increases in women.
Internal Changes. Both senile seborrhea and essential senile pruritus are linked to alterations in the central nervous system. Reticuloendothelial system degeneration may predispose decreased resistance to skin infection, inflammatory dermatoses, and fungus disease. Peripheral vascular dysfunction is associated with impairment of the trauma response, temperature regulation, and infection resistance, which may predispose stasis dermatitis and ulcer, decubitus ulcers, purpura, and senile tibial erosion and nodules.
Environmental Changes. A change of residency can produce nutritional eczema because of dietary changes. Sensitivity may occur from exposure to new contactants. Economic considerations and misguided self-help may complicate or precipitate disorders. Internal cancer may underlie multiform or toxic erythema, pemphigoid, or metastasize to the skin. Prolonged exposure to actinic radiation, ionizing radiation, and carcinogen contact may precipitate or contribute to lowered resistance, dysfunction, and degenerative changes.
Classification of Dermatogeriatric Disorders
In the aged, skin disorders can be classified into four main problem dermatoses:1. Obligatory dermatoses are almost exclusively found only in geriatrics. Examples are seborrheic dermatitis, senile xerosis, pressure nodules, milia, lentigo, essential senile pruritus, seborrheic keratosis and verruca, actinic keratosis and verruca, guttate hyperkeratoses of the leg, angioma, ectasia, and basal cell, prickle cell, or anaplastic epithelioma.
2. Constitutional dermatoses reflect an underlying change. Examples are senile tibial erosion or sclerosis or nodule, capillary arteritis, stasis dermatitis and ulcer, pemphigoid, gluteal hyperemia and erosion, decubitus ulcer, and senile purpura.
3. Inveterate dermatoses are disorders originating in an earlier age period as asymptomatic but manifest during senescence. Examples are psoriasis, lupus erythematosus, neurofibromatosis, radiodermatitis, and ichthyosis.
4. Incidental dermatoses are disorders that can be a problem at any age. Examples include the neurodermatoses, contact dermatitis, urticaria, clavi, perleche, intertrigo, pyoderma, onychomycosis, herpes, pruritus, neurotic excoriations, erythema multiform, dermatitis exfoliativa, and drug reactions.
The Pruritic Dermatoses
Because itching is a common complaint in senior citizens, special care should be given to differential elimination of skin and systemic disorders. Essentially, the pruritic dermatoses can be classified into six major categories:1. The neurodermatoses
2. Senile xerosis
3. Essential senile pruritus with systemic disease
4. Pruritus vulvae and ani
5. Miscellaneous disorders
Of the five above categories, the neurodermatoses may be subdivided into five disorders: (1) autosensitization dermatitis, (2) nummular eczema, (3) lichen simplex chronicus, (4) generalized neurodermatitis, and (5) winter eczema. The miscellaneous disorders commonly include psoriasis, senile seborrhea, contact dermatitis, intertrigo, tinea cruris and corporis, candidiasis, neurotic excoriations, urticaria erythema multiform, dermatitis excoriations, urticaria erythema multiforme, dermatitis exfoliativa, drug reactions, and infestations such as pediculosis and scabies. Infestation should be the first etiology ruled out during differential diagnosis; the second, fungus infection.
The Neurodermatoses
Neurodermatoses often respond to chiropractic case management but they sometimes tax the doctor's complete scope of therapeutic knowledge. Neurodermatoses are usually chronic conditions with acute manifestations. The history frequently includes a familial tendency toward atopic dermatitis and/or allergy (autosensitization, inhalation, and/or food) and emotional hypersensitivity or a "burn-out" syndrome. Diagnosis is almost always by elimination of possible etiologies.Autosensitization Dermatitis. This generalized autogenous eczema is usually diffusely distributed and characterized by the development of pinhead-size vesicles on an erythematous base having a tendency to group and form coin-size patches that may join and involve extensive areas. Drying, crusting, and scaling accompanied by mild thickening are seen in the late stages. Thousands of small vesicular or infrequent bullous lesions may appear and become hemorrhagic because of scratching. The eyelids may exhibit a contact dermatitis with edema, erythema, and scaling. The itching is severely intense, unrelenting, and often unrelated to specific areas of rash.
Many cities exert poor control over the chlorine content of the municipal water supply. Sometimes just having the patient substitute distilled water for drinking and cooking purposes will greatly relieve the condition. Males should use an electric razor to avoid tap water, and showers are restricted to once a week. Daily sponge baths should be made with distilled water (commercially available in most areas) and light use of a mild detergent-free soap such as Basis when necessary.
The incidence of autosensitization dermatitis is on the rise in populations of urban areas. The overt condition is usually secondary to an eczematous or infected local dermatosis and aggravated by rubbing and scratching. Hot showers temporarily relieve the intense itching because of the sedation effect of the hot water, but they remove oils from the skin that leads to dryness and microcracks that contribute to the pruritus. Differentiation should be made from winter or disseminated nummular eczema, generalized neurodermatitis, dermatitis exfoliativa, and drug reactions.
If referral is made beyond the profession, the editor prefers consultation with an allergist or homeopath rather than a dermatologist for autosensitization dermatitis. A dermatologist may restrict therapy to oral and lotion corticosteroids. This may palliate the inflammatory rash, but oral corticosteroids are notorious for eroding the stomach wall and/or possibly producing ischemic necrosis of the hip. Allergization, homeopathy, and chiropractic therapy are aimed at enhancing the immune system of the patient.
Lichen Simplex Chronicus. This localized neurodermatitis is usually found in the nuchal region, extensors of the forearms, and anterior tibial region, but it may be found anywhere on the body. It is characterized by a single (or few) lesions composed of well-defined, dry, and possibly excoriated plaques that show lichenification. If lesions appear on the neck, differentiation should be made from seborrheic dermatitis, psoriasis, and contact dermatitis. If lesions appear on the forearm, differentiate from psoriasis.
Generalized Neurodermatitis. This skin disorder is almost impossible to differentiate from autosensitization in the elderly except by history of a precipitating eczematous eruption in expression of autosensitization.
Nummular Eczema. This skin disorder is commonly seen in the alcoholic or debilitated patient. It is characterized by a few lesions becoming confluent and spreading about the entire forearm or leg with possible scattered lesions in other parts of the body. Differentiation should be made according to area of lesion appearance:
Hand-contact dermatitis, lichen simplex chronicus, fungus infection
Leg stasis dermatitis, lichen simplex chronicus, psoriasis
Eyelids, contact dermatitis
Ears, fungus disease
The disseminated form should be differentiated from winter eczema, drug eruptions, and fungus disease.
Other Pruritic DermatosesWinter Eczema. This disorder is generally found of the exterior surfaces of the extremities and trunk and is brought out by changes in temperature, humidity, and season. If found on the legs, it features an extremely dry skin showing find fissures and cracks that may form a geometric pattern. If found on the surfaces of the extremities and thighs, it features extremely pruritic, guttate, annular, and arciform lesions.
Rubbing and scratching often lead to exudation, eczematization, and autosensitization dermatitis. Differentiation of winter eczema should be made from senile xerosis; contact, stasis, or autosensitization dermatitis; fungus disease; and drug reactions.
Senile Xerosis. This localized or diffuse skin disorder features a dry, scaling, noninflammatory dermatosis of the leg that is worse in winter and aggravated by soaps, wool, and bed linen. Because sebum production is reduced, the skin appears dry and finely scaly. Differentiation should be made from contact dermatitis and generalized neurodermatoses.
Essential Senile Pruritus. Itching may be localized or general. The cause is often suspected to be the result of multiple little strokes involving latent central nervous system damage. Differentiation should be made from the neurodermatoses and systemic diseases.
Pruritus Vulvae and Ani. Chronic moisture from sweating or urinary/fecal incontinence, local irritation, and local functional changes contribute to either of these disorders, as would an irritating sacroiliac or coccygeal subluxation. Differentiation should be made from local skin disease, extension of disseminated dermatoses, and dermatoses of a gynecologic nature.
Senile Seborrhea. This form of seborrhea is usually found on the scalp, facial folds, eyebrows, behind the ears, on the sternum, or in the axillae or groin. Features may include a fine, whitish, gritty scale (without inflammation) diffusely distributed on the scalp; patchy to confluent areas of accumulated oils, sweat, and lint; or an acute erythematous dermatitis characterized by scaling, which may extend below the hairline. Differentiation should be made from psoriasis and contact dermatitis.
Contact Dermatitis. Local or diffuse, this disorder is usually chronic and aggravated by local neurodermatitis. Common contact irritants are wool, chrome, plastic, woods, cosmetics, paints, pesticides, mold, nail polish, dust and dust mites, solvents, and detergents. Differentiation should be made from nummular eczema, fungus infection, and generalized exanthema.
Neurotic Excoriations. In any accessible skin area, neurotic excoriations may be found that appear as punched out or linear erosions presenting either a clean or crusted surface. Such self-induced dermatoses suggest a predisposing psychotic disorder requiring expert counseling or referral to cope with the emotional problem.
Urticaria, Erytherma Multiforme, and Exfoliative Dermatitis. Urticaria in the elderly is often the result of drug sensitivity. Single, multiple, or cumulative factors may also exist such as certain foods, beverages (eg, apple cider), contactants, or inhalants resulting in the acute or allergic form. Bacteria, viruses, and fungal infections are often suspected and just as often eliminated. It is not uncommon in geriatrics to have the disorder precede the development of dermatitis herpetiformis or pemphigoid or to see it associated with lymphoma or cancer.
Erythema multiforme usually appears localized, but it may be generalized and exhibit bullae and extreme mucous membrane involvement such as in Stevens-Johnson syndrome. Drug reactions and allergic manifestations are common causes.
Exfoliative dermatitis is difficult to diagnose accurately. The disorder is seen often as a complication of psoriasis, autosensitization dermatitis, generalized neurodermatitis, lichen planus, and drug or contact sensitivities. Development into lymphoblastoma is not uncommon.
The Bullous DermatosesFour common types of bullous diseases are differentiated in geriatrics. The first three forms described below show subepidermic bulla.
1. Bullous erythema multiform is characterized by acute onset in the presence of a history of infection or medication ingestion.
2. Bullous pemphigoid features a chronic form of erythema multiforme that is less severe. Associated degenerative disease and cancer may be the precipitant.
3. Bullous dermatitis herpetiformis is characterized by intense itching and burning.
4. While all three forms above show subepidermic bulla, mucous membrane involvement, weight loss, and gradual physical deterioration, they can be contrasted to true pemphigus that is insidious in onset and eventually becomes generalized.
Bacterial, Viral, and Mycotic Infections
Syphilis is rare in patients over 60 years of age. Even if a serologic test is positive, one must first suspect an acute disease, autoimmune disorder, dysgammaglobulinemia, or some biologic factor producing a false-positive reaction. Primary syphilis without an obvious syphilitic chancre should be differentiated from psoriasis, seborrheic dermatitis, herpes, lichen planus, contact dermatitis, nonspecific balanitis, monilial infection, epithelioma, erythroplasia, or a localized drug reaction. Secondary syphilis should be differentiated from lymphoblastoma, mycotic infection, psoriasis, pityriasis rosea, and drug reactions.
Herpes zoster may exhibit a dramatic manifestation of bullae, ulceration, and necrosis in association with malnutrition, debilitation, and lymphoma. The eruption often arises after fever.
Candidiasis (moniliasis) is often seen in the intertriginous areas in the groin and submammary regions. It frequently arises as a complication of inflammatory dermatoses, psoriasis, exfoliative dermatitis, or a drug reaction. Predisposing factors often include diabetes, general debility, neoplasia (advanced), peripheral circulation dysfunction, and reactions from steroids or antibiotics. Candida superimposed on a moist and irritated skin produces perleche and balanitis.
Onychomycosis is common in the elderly. Features of this fungus infection are dystrophic thickening of the nail plate, subungual hyperkeratosis, and nail deformity, with accompanying irritation leading to secondary infection and paronychia. Diabetes may be associated. Differentiation should be made from psoriasis, eczema sequelae, bacterial infection, and lichen planus.
Furunculosis may be acute or recurrent with poor hygiene or in systemic disorders such as diabetes. Predisposing conditions in the elderly include multiple infections and abscesses, diabetes, and other debilitating conditions that lower resistance.
Erysipelas usually presents an acute, rapid onset accompanied by systemic symptoms. The disorder often complicates skin trauma, folliculitis, and chronic dermatitis. Fissures between the toes and excoriations complicating chronic dermatitis are the most common portals of entry.
Dermatoses of the Lower Extremities
These disorders are frequently associated with peripheral vascular dysfunction. Drug reactions may be expressed as erythema nodosum. Nummular eczema and hypostasis may predispose atrophy and xerosis accompanied by itching and scratching. Toxic vascular disease may be expressed as nodular vasculitis and periarteritis nodosa. Cellulitis, a potentially dangerous condition, and erysipelas may be the result of bacterial infection with chronic dermatitis or interdigital fissures serving as portals of entry.
Generally, dermatoses of the lower extremities can be classified as either vascular, eczematous, or miscellaneous:Vascular Dermatoses of the Leg. Capillaritis of superficial vessels indicates punctate-to-confluent depositions of blood pigment. Stasis dermatitis features defined, red, shiny exudative lesions progressing to ulceration. Infection and dermatitis from drug reactions leading to autosensitization are frequent complications. Senile tibial erosion is seen as punched-out nummular or linear erosions, and atrophic scars with a spontaneous or traumatic history. Senile tibial sclerosis exhibits deeply pigmented lesions usually on the lower third of the leg that decrease in diameter and present scleroderma-like changes. Associated with stasis and sequelae to long-standing disease, postthrombotic ulcer features exudative ulceration at the lower medial aspect of the leg. The history usually discloses thrombosis with edema, induration, pain, and a family tendency.
Eczematous Dermatoses of the Leg. There are two common types in this category: (1) Nummular eczema is seen as guttate, coin-shaped or confluent plaques, from exudative to crusted, on the anterior and lateral shins. The disorder may be preceded by winter eczema, senile xerosis, or just scratching. Differentiation should be made from stasis dermatitis. (2) Contact dermatitis features defined exudative and erythematous lesions on the leg, often complicating nummular eczema or stasis dermatitis. Autosensitive dermatitis may be precipitated.
Miscellaneous Dermatoses of the Leg. There are three common types in this category. (1) Erysipelas shows a rapidly advancing, defined, bordered lesion. Systemic symptoms are often associated, and diabetes is always suspect if erysipelas recurs. (2) Erythema nodosa is characterized by multiple, tender, warm, red plaques progressing to a violaceous tint that are located bilaterally. Multiple causes often include infection, drugs, and malignancy. (3) Rapidly extending cellulitis sometimes manifests as tender, red, warm plaques that are unilateral and measure 10 or more centimeters in diameter. Elevated temperature and an obvious portal of entry (eg, scratch, puncture, deep burn, chronic dermatitis, interdigital fissures) are usually associated. Swelling, heat, and tenderness may be the only signs of this dangerous potentially extending situation.
Skin Tumors (Benign and Precancerous)
Benign tumors and forms of precancerous lesions are frequently witnessed in geriatrics.Benign Verrucae and Clavi. Warts and callosities are differentiated by paring the keratotic surface to reveal the pinpoint capillary bleeding of the wart or the homogenous substance of the callous. Both verrucae and clavi are found at points of trauma such as on the weight-bearing surfaces of the feet or the fingers.
Benign Senile Sebaceous Adenoma. These facial adenomas are slow-growing, raised, yellowish, shiny, and vary in size from 1 to 5 mm in diameter. In the malignant variety, the cheeks and forehead are common sites of these benign tumors in the elderly. They are characterized by multiple, yellowish, umbilicated, flat papules, which are the result of hyperkeratotic sebaceous glands. Single lesions are frequently confused with basal cell carcinoma.
Precancerous Seborrheic Keratoses. These appear as slow-growing, yellowish, slightly raised lesions located usually on the back, hair margin, neck, and chest. In later stages, they may become verrucous, pigmented, and present a greasy characteristic. Neck lesions are often dome-shaped, shiny, and black. The malignancy potential is slight. Differentiation must be made from nevocarcinoma and pigmented basal cell epithelioma.
Malignant Seborrheic Keratoses. Usually located on the trunk, scalp, and face, these benign uninvasive epithelial tumors appear in the elderly as slightly elevated yellowish plaques covered by a greasy scale and presenting definite borders. They average in size about a centimeter in the early stages, increase in size and thickness, and deepen to a brown-black color with granular surfaces. They may develop to basal cell carcinoma if subjected to constant friction such as from clothing or shaving.
Precancerous Radiodermatitis. As an aftermath of overexposure to ionizing radiation, features include atrophy, obliteration or normal skin markings, cicatrization, and surface telangiectasis and radiokeratoses that may progress to ulceration and epithelioma.
Precancerous Senile Actinic Keratoses. Two forms are commonly seen distributed to areas exposed to the sun such as the face, lips, ears, and back of the hands. The first form appears as a raised, verrucous, well-defined lesion overlaid with a thick, horny, adherent layer that appears dense gray or black. The second form appears as a flat, dry, undefined, adherent hyperkeratosis that often has progressed from a rough place on the skin that tends to bleed slightly with irritation. Anaplastic epithelioma may supervene. In both the raised and the flat forms, differentiation must be made from seborrheic keratoses and verrucae.
Precancerous Leukoplakia. These usually mouth lesions are distributed to the gums, inner lip areas, dorsal surface of the tongue, cheek membranes, but sometimes the vulva. They resemble actinic keratoses of the skin. Lesions appear from dull white to silvery and are raised and verrucous, while the cancerous variety is usually smooth and patchy. The precipitating factor is usually some chronic irritation such as a chronic focal infection in the mouth, poor fitting dentures, or pipe smoking. Differentiation must be made from lichen planus.
Malignant Skin TumorsPrickle Cell Epithelioma. This is a fast-growing, well-defined, raised growth with surface erosion in areas of chronic stasis, ulcer, and crusting. A surrounding palpable inflammatory reaction is associated. While this type metastasis is frequent. The cancer often occurs in actinic keratoses, radiodermatitis, leukoplakia, and chronic ulcers. Verrucous, papillomatous, and fungating forms can occur anywhere on the body. A crateriform ulcer may be seen on the face with a wide, grayish, rolled border.
Basal Cell Epithelioma. This lesion progresses from one showing a discrete, nodular, waxy, well-defined border often with telangiectasia to one showing ulceration and crust. Rarely metastatic, these cancers are slow-growing and locally malignant.
Pigmented basal cell epithelioma appears shiny brown-to-black and should be differentiated from seborrheic keratoses and carcinoma.
Morphia-like basal cell epithelioma appears as raised-bordered plaques, white to ivory in color.
Superficial epitheliomatosis appears as erythematous, scaly, defined, and plaque-like lesions from 1 to 10 cm in diameter, usually appearing on the back and trunk.
Differentiation must be made from psoriasis. This usually takes referral for biopsy.
Melanotic Freckles. Such freckles usually appear first on the face and extremities and then progress to circumscribed macular pigmented lentigo, deepening pigment, papules within the lesion, and peripheral enlargement. The course is relatively benign, but biopsy is mandatory for differential diagnosis.
Anaplastic Epithelioma. These highly malignant tumors can be found anywhere on the body; however, primary types associated with Bowen's and Paget's diseases are commonly found on the back and trunk. The lesions begin as papules that rapidly progress to a nummular with a grayish crust or scale and peripheral activity and ulceration. Secondary types are usually associated with precancerous conditions or basal cell and prickle cell epithelioma. Biopsy is necessary for differential diagnosis.
Miscellaneous Skin ConditionsFreckles and Lentigines. Childhood ephelides that have disappeared often reappear in later life because of an inability of the melanocytes to produce an even distribution. Such cosmetic flaws are harmless. Lentigines, on the other hand, may become malignant. These are commonly found on the trunk, thighs, and genitals, and do not fade when protected from sunlight.
Senile Ectasia. These lesions are asymptomatic tufts of dilated capillaries that bleed on irritation. They appear as bright red or purplish papular angioma or varix in the skin. Varying in size from 1 to 5 mm in diameter, they are usually found on the upper chest and trunk.
Venous Lakes. These are bluish-black to gray papular lesions distributed in exposed areas such as the face, neck, ears, and hands. They may be singular or multiple. These apparently cosmetic defects must be differentiated from basal cell carcinoma or melanoma.
Vascular Changes. Various arteriosclerotic changes can occur during the aging process that may be accountable with asymptomatic conditions such as the loss of hair; cool skin; nails that are brittle, thickened, and dystrophic; petechial changes; and pregnancy changes.
Stasis Eczema. In aging, increasing incompetence of the valves of the saphenous veins often is witnessed. The result is increased lower extremity venous pressure, swelling, bluish-red skin changes from passive congestion, and local nutritional dysfunction. Skin necrosis and ulceration frequently follow trauma and are associated with pruritus.
Localized Dermatitis of Vidal. This lichen chronicus simplex is a commonly seen eczematous process perpetuated by pruritus. A vicious cycle is seen of itching, scratching, and lichenification. Skin furrows are prominent, and rectangular papules are found that are first pink, progress to thickened brownish lesions, and then to white scaly furrows.
Fungus Infections. In the elderly, fungus infections are a more complex problem because of the predisposing physiologic changes resulting from reduced peripheral circulation. Moniliasis in the elderly is often seen as a complication of antibiotic therapy or a complication of intertriginous eczema.
Perleche. This commissural dermatitis is characterized by the downward folding and maceration of the corners of the mouth. In the elderly, it is often associated with poorly fitting dentures, resulting in saliva constantly keeping the area moist and receptive to maceration and secondary mycotic and bacteria infection. Constant burning is perceived, and fissures develop later.
Acrochordons. Soft, pedunculated, skin colored, cutaneous tags are often seen in the elderly. They are usually benign unless chronically irritated.
Keratoacanthoma. These solitary lesions seen in exposed areas of elderly skin are characterized by a dome-shaped tumor whose central crater is filled with fibrous keratinous debris. These rapidly growing lesions should be differentiated from low-grade squamous cell carcinoma.
Visceral Diseases and Their Cutaneous ManifestationsCutaneous Visceral Manifestations. Herpes zoster may suggest viral infection, chemical poisoning, neoplasm, or a secondary condition to trauma or a drug reaction. Gastric adenocarcinoma may be reflected to the skin by the development of acanthosis nigricans lesions with their characteristic blackish, papillary or verrucous hypertrophy in the axillae, on the neck, face, genitalia, groins, submammary areas, and/or inner thighs. These pigmented areas are covered with discrete vegetating masses, nodules, and papillomatous tumors. Nail changes and alopecia are often related.
Poorly Controlled Diabetes. Recurrent furunculosis and folliculitis are seen in the elderly because of pruritus and scratching. The buttocks and posterior thigh areas are common sites. Also in diabetes in the elderly, necrobiosis lipoidica diabeticorum may be rarely witnessed. Sometimes called dermatitis atrophicans lipoides diabetica, the lesion is characterized by an oval or a round well-defined papule that is firm and initially red turning to yellow-centered plaques that are irregular and sclerodermic with a violet periphery. Common sites are the ears and upper and lower extremities.
Vitamin Deficiencies and Their Cutaneous Manifestations
Although described fully in another chapter, brief mention follows on cutaneous manifestations of common conditions recognized in geriatric nutritional deficiency.Avitaminosis A. Improper intake or assimilation of vitamin A leads to lesions characterized by keratotic papules associated with pilosebaceous follicles relatively uniform at onset and associated with skin that is dry and rough. As the disorder progresses, hyperkeratotic papules appear and spread rapidly, and skin color darkens and often shows fine scaling. Lesions usually first appear on the arms and thighs, then spread to the extensor surfaces of the extremities, abdomen, shoulders, back and buttocks. The flexure areas are rarely involved.
Riboflavin Deficiency. Cheilosis, dyssebacia, magenta tongue, and perleche are characteristic findings of vitamin B-2 deficiency. Chronic manifestations include lip irregularity and wrinkling, magenta tongue, oily skin, desquamation in the ears and canthi and especially on the midface and nasolabial folds. Acute manifestations may be observed as lip edema, cheilosis, and loss of normal lip wrinkling, all progressing to chronic signs.
Pellagra. The classic picture of is dermatitis, dementia, and diarrhea is rarely seen. Subnormal deficiency of niacin deficiency (niacinamide B-complex) is indicated by a characteristic bright red and swollen tongue, mucous membrane atrophy, painful fissures, ulcers (especially commissural), and redness and edema followed by dark pigmentation in areas exposed to the sun.
COMMON ENDOCRINOLOGIC DISORDERSWhile complete endocrine deficiency does not permit survival, insufficiency in the elderly of pituitary, thyroid, parathyroid, insular, and adrenal hormone secretions may be adapted to for several years. However, recognize that the clinical picture of incomplete deficiency does not produce the classic syndromes of overt deficiency.
Thyroid DisordersHyperthyroidism. Characteristics involve the sensation of subjective warmth, a warm moist skin, increased perspiration, and weight loss but with increased appetite. Circulatory signs include tachycardia, auricular fibrillation, high pulse pressure, and increased cardiac excitement and output with possible precordial pain. Muscular and nervous characteristics suggest myasthenia, muscular atrophy, creatinuria, or cerebration with possible psychosis from intoxication or reflect increased pulse amplitude, tremor, palpitation, diarrhea, vomiting, nausea, abdominal pain, nervousness, and irritability. The fluid signs are those of polyuria, increased blood volume and iodine, decreased sugar tolerance and cholesteremia, and hyperexcretion of calcium, phosphorus, sodium, and potassium.
Hypothyroidism. In contrast to the features of hyperthyroidism, those of hypofunction include the sensation of subjective chilliness, a dry cold skin, decreased perspiration, weight gain without polyphagia, and inflammatory eye lesions. Skin, hair, and nails are coarse and slow growing. Circulatory signs include bradycardia, decreased pulse pressure, reduced cardiac tone and output, and possibly precordial pain. Muscular and nervous characteristics suggest myxedematous muscle infiltration, and hearing and memory loss or reflect in macroglossia, hoarseness, general muscle weakness, decreased pulse amplitude, edema of the heart muscle, sleep and emotional irregularities, constipation, fatigue, and cerebration. The signs are those of edema, increased proteinemia, urine albumin, sugar tolerance, cholesteremia, decreased blood volume and iodine, and decreased excretion of calcium and phosphorus. Hypothyroidism is highly significant in geriatrics.
Parathyroid DisordersHyperparathyroidism. Characteristics of hyperparathyroidism include anorexia, nausea, constipation, polydipsia, bone pain, bone rarefaction and decalcification, muscle weakness, hypotonia, and polyuria. Serum calcium and protein are increased, serum inorganic phosphorus is decreased, and calcium excretion increases. Commonly associated are spontaneous fractures, nephrocalcinosis and kidney damage from calcium salts, giant cell bone tumors, epuloides, multiple bone cysts, and vertebra collapse.
Hypoparathyroidism. Features of hypoparathyroidism include positive Chvostek's, Trousseau's, and Erb's signs. Circumoral paresthesia, dyspnea with possible cyanosis, and tonic spontaneous muscle contractions progressing to chronic generalized tonic convulsions are typical. Neuromuscular irritability, photophobia, and bone density are increased. Serum shows low calcium and high phosphorus levels, and calcium excretion is decreased or absent. Cataracts, papilledema, mental retardation, and calcification of the basal ganglia may be associated.
Osteoporosis
Secondary osteoporosis may be the result of active endocrine disease, severe malnutrition, connective tissue disease, multiple myeloma, diffuse metastatic carcinoma, paralysis or immobilization. In the elderly, primary osteoporosis is a common finding and probably linked to lack of exercise and inadequate intake of calcium and vitamins. The basic endocrine mechanism is one of continued gluconeogenetic corticosteroid activity combined with hypoestrogenemia resulting in a failure of the adrenal cortex and ovary to balance.
Because the disorder involves bone trabeculae principally, vertebral compression fracture and collapse, Colles' fracture of the wrist, and fractures of the neck of the femur (Fig. 8.13) are frequently related. While menopausal back pain may be an early sign associated with hypoestrogenism, postmenopausal osteoporosis may not become evident until years later.
Pituitary Disorders
The pituitary gland appears to have little relationship to the aging process. Small differences are noted in secretions of the young or old. Posterior lobe disease resulting in hypofunction of the supraoptic-hypophyseal system and consequent diabetes insipidus is rare in the elderly.
Anterior lobe dysfunctions resulting in reduced or excessive levels of all or one of the anterior pituitary hormones may be the clinical problem. Such dysfunctions are witnessed in forms of Cushing's syndrome, local infections and tumors, and Simmonds' disease. The characteristics are similar to those found in the young.
Diabetes Mellitus
Most cases of diabetes mellitus are thought to be predisposed by a genetic defect precipitated by an acquired environmental condition such as nervous strain or insult, infection, obesity, hyperthyroid metabolism, or tumor. The classic picture is one of itching, polyuria, weakness, weight loss, glycosuria, hyperglycemia, polydipsia and polyphagia, and ketosis and acidosis leading to coma. However, this picture is restricted commonly to the acute form in the young. In the elderly, the disorder is much more chronic, subtle, and the symptoms are much less drastic.
Geriatric diabetic complications primarily include the peripheral vascular disease, coronary artery disease, and diabetic retinopathy, nephropathy, and neuropathy. Sometimes the symptoms of the diabetes are so mild in senior citizens that the disorder is not found until treatment is sought for a complication.
Adrenocortical DeficiencySubclinical Adrenocortical Insufficiency. This disorder is common in the elderly. The characteristic picture of the often misdiagnosed disease includes asthenia, anorexia, hypotension with easy fatigue, low sodium and high potassium serum levels, and tendencies toward Addison's disease.
Clinical Chronic Adrenocortical Deficiency (Addison's Disease). The distinctives include muscular weakness, abnormal pigmentation of the skin and mucous membranes, weight loss with dehydration, hypotension, frequent episodes of hypoglycemia, and various gastrointestinal complaints. Anorexia, nausea, vomiting, diarrhea, dizziness, syncope, asthenia, peripheral vascular collapse, and renal failure with azotemia often occur. Laboratory findings usually suggest low sodium and high serum potassium, low fasting blood sugar, elevated blood nonprotein nitrogen, decreased carbon dioxide combining power, a low leukocyte count with an elevated hematocrit, and a basal metabolism rate of from -15 to -20. X-ray findings often show evidence of a small heart, calcifications in the adrenal areas, and associated renal and/or pulmonary tuberculosis.
Menopause
Cessation of the menses in the average woman usually takes place between ages 40 and 50 with no change in her sexual life. Adequate estrogen and androgenic steroids are provided by the adrenal gland for the remainder of life. If the reduction of ovary secretions is not compensated by the adrenal cortex, the disorder is characterized by back pain, hot flashes, sweats, nervousness, excitability, fatigue, apathy, tearful depressions, insomnia, vertigo, allergic dermatitis, palpitation and precordial discomfort, headaches, paresthesias, myalgias, polyuria and incontinence. Pruritus vulvae, vaginal atresia, dyspareunia, osteoporosis, and atherosclerosis may also be associated.
Atrophy and changes in fat, pigment, vascular tissues, calcium levels, and stroma are characteristic of the changing physiology in the female aging process. They are usually attributed to progressive diminution of gonadal endocrine stimulation to the organs of reproduction. While no endocrine disorder is exclusively a geriatric condition, changes in the internal and external organs of reproduction become apparent in the elderly as a result of the pituitary-gonad-uterus mechanism diminishing in function.
The Male Climacteric
In contrast to menopause, the aging process does not involve cessation of either spermatozoa formation or male hormone secretion. In rare cases in elderly men, testosterone insufficiency is characterized by chronic fatigue, muscular weakness, loss of libido and potential, vasomotor paroxysms, emotional depression, and other signs of decreased androgenic tissue metabolism.
Pseudosenility
Early senility is often confused with a true dysfunction of testosterone, estrogen, aldosterone, or hypothyroidism, either alone or in combination. Signs and symptoms are of increasing fatigability with poor endurance, weight loss, menopausal or climacteric vasomotor symptoms, apprehension, irritability, insomnia, depression, muscle and skin atrophy, protruding subcutaneous veins, and the senile posture.
COMMON GYNECOLOGIC DISORDERSAfter the menopause, tissue atrophy is progressive. Tissues become pallid, shrunken, and less moist. Uterine size decreases, and the cervix narrows and often stenoses. The myometrium becomes fibrous, related blood vessels sclerose, and the endometrium thins and atrophies. The stroma and the ovaries become compact.
Note: The editor has found that similar symptoms may arise in the adolescent female along with PMS and dysmenorrhea. Here, adjunctive soft-tissue "bloodless surgery" (deep stretching of pelvic adhesions and manually relocating misplaced [traumatic, postural] organs) are beneficial in relaxing stretched fascia, vessels, and nerves. In abdominopelvic prolapse, a full girdle should be worn until abdominal exercises become effective.
Relaxation of the pelvic floor in the elderly and its consequent disorders are aggravated by the diminishing muscle tone associated with the aging process. The incidence of neoplastic, endocrine, metabolic and excretory system disorder increases, Most of these disorders are chronic, insidious, and progress slowly. Rarely, advanced acute bacterial, monilial, or trichomonal infections of the vulva are associated that require referral.
Relaxation of the Pelvic Floor
In the elderly, physiologic changes and atrophy are seen to progressively aggravate predisposing weakness in the levator musculature and enveloping fascial layers. While child-bearing injuries may be contributing factors, congenital or acquired weakness is also associated with relaxation in the virgin or nulligravid. When relaxation of the pelvic floor occurs, a mild sense of pelvic weight or bearing-down may progress to acute integumental hernia if precipitated by abdominal overstrain. Cystocele, rectocele, enterocele, stress incontinence, and uterine prolapse are all associated with relaxation or overstress of the pelvic floor.Cystocele. This is a defect in the pubocervical and pubovesical fascia, usually following obstetric injury. The relaxation of the anterior vaginal wall, often coexistent with urethrocele, is characterized by subjective pelvic weight, dysuria, and a mass protruding from the vagina. Recurring urinary tract infections are frequently associated.
Rectocele. Weakening or laceration of the rectovaginal fascia, levator muscles, and perineal tissues, which usually follows obstetric injury. This disorder is characterized by subjective pelvic weight, defecation faults, and protrusion of the anal pouch and rectum through the vaginal opening. Cystocele is usually coexistent. When advanced, surgery should be recommended.
Enterocele. This disorder is a true hernia of a peritoneal sac through the pelvic outlet via the vagina. The herniation may include omentum or bowel; predisposing entrapment, strangulation, or incarceration. The symptomatic picture is often that of rectocele; and rectocele and uterine prolapse are frequently associated. Skillful rectal examination aides differentiation.
Stress Incontinence. Weakness in the supporting structures of the vesical neck may lead to partial incontinence as the result of sudden intra-abdominal pressure as from coughing, sneezing, overstrain, laughing, running, or horseback riding. Obstetric trauma is usually predisposing. Comprehensive eclectic chiropractic therapy is highly effective in the young.
Uterine Prolapse. Obstetric trauma or acquired weakness may lead to descending of the uterus below its normal level in the pelvis. The loss of muscle tone associated with the aging process aggravates the condition. Subjective pelvic pressure may progress to increased pressure, protrusion of the cervix through the vaginal orifice, and end in procidentia. Coexistent cystocele and rectocele are common.
Postmenopausal Bleeding
Progressive ovarian quiescence and associated secondary endocrine readjustments are said by the medical establishment to be normal physiologic processes in the elderly female. This may not be true under chiropractic care. However, bleeding occurring a year after menopause is suspect of an organic problem.
Pathologic disorders in the elderly associated with postmenopausal bleeding and most commonly witnessed are as follows:
Benign. Examples include senile vaginitis and endometritis, systemic disease, urethral caruncle, cervical erosion and polyps, endometrial hyperplasia and polyps, and reactions from estrogen therapy.
Malignant. Examples include ovarian granulosa, thecal cell tumor, and vulvar, cervical, and endometrial carcinoma.
Disorders of the Vulvar Skin
Vulvar atrophy predisposes an assortment of disorders such as leukoplakia with fissures or ulcers, vulvar carcinoma, lichen sclerosis et atrophicus characterized by subepidermal edema without fibrosis, senile vaginitis associated with vascular insufficiency possibly resulting in punctate hemorrhages and epithelial discharge, and basal cell vaginal dermis.
Pruritus vulvae may be associated with either local or systemic disorders. Local conditions include senile vaginitis and leukoplakia, which can often be corrected with a douche containing a small amount of Scope (or similar mouthwash) and vinegar. Other disorders principally include lichen sclerosis et atrophicus, kraurosis, polyps, and neoplasms. Commonly associated systemic conditions include diabetes, vitamin deficiencies, leukemia, and drug reactions.
Occasionally in the elderly vulva, basal cell carcinoma, melanoma intraepithelial carcinoma, Paget's disease (a counterpart of Paget's disease of the breast), and Bartholin gland carcinoma will be found. However, true invasive carcinoma of the vulva is a common geriatric finding. A flat, infiltrative or ulcerative, growth arising in the anterior half of the vulva is characteristic. Signs may include vulvar irritation, pruritus, a palpable mass, ulceration, bloody discharge, and pain in the late stage. Metastasis is via the regional lymph system.
Uterine Cancer
Lesions may be localized or metastasized, primary or secondary, and vary in type from superficial, polypoid, or anaplastic growths. Signs include uterine hypertrophy and postmenopausal bleeding. In the elderly, endometrial carcinoma has a higher incidence than cervical cancer and is commonly associated with carcinoma of the uterine body. When suspected, referral is necessary for confirmation.
Senile Ovary
The senile ovary is one that has become atrophied, convoluted, and sclerosed. Geriatric incidence of germinal inclusion cysts is high, while the dysfunctional types of endometrial ovarian cysts and ovarian tumors are low in frequency. Many symptoms attributed to a senile ovary are medically misdiagnosed and amendable to chiropractic with nutritional therapy.
Other Gynecologic Tumors of the Elderly
Granulosa cell tumors, almost impossible to discover by palpation, are frequent in the elderly. These are very small tumors (estrogen producing) that may show only an external sign of postmenopausal bleeding. Malignancy may follow development.
Even more frequent in the elderly female is ovarian thecoma, characterized by a solid fibrous tumor. It is commonly associated with endometrial carcinoma rather than granulosa cell tumors.
Brenner tumors, common in the elderly, are often associated with cystic endometrial hyperplasia.
Sign Primary Suspicion
Fixed dilated pupil of one eye Involvement of the 3rd cranial nerve
Fixed dilated pupil of one eye with Complete involvement of 3rd cranial
ocular muscle paralysis nerve
Cotton wisp cornea insensitivity Involvement of the 5th cranial nerve
(sphenoidal fissure syndrome)
Stethoscopic bruit heard over closed Arteriovenous aneurysm
eye
Unilateral proptosis Possible orbital growth or meningioma
invading the orbit
Diplopia Involvement of the 6th cranial nerve
or 3rd cranial nerve's midbrain nucleus
Ptosis Myasthenia gravis
Hemianopsia - bitemporal loss Involvement at the chiasm or pituitary
body
Hemianopsia - homonymous Involvement of the optic tract or optic
radiation, vascular crisis, or
unilateral tumor
Hemianopsia - altitudinal Possible calcification of the internal
carotid artery as it enters the cranial
cavity and presses on the optic tract
Disorders of the Transformer. No major disorder of the external ear is
unique with the elderly. While the aged ear drum often appears thicker,
whiter, and more opaque, such changes seem to have no clinical significance.
Infection in the middle ear resembles that of the young; however, the
associated incidence of diabetes, tumors, polyps, and malignancies is much
higher. Middle ear infections are often complications in the elderly suffering
from leukemia or carcinomatosis, predisposing mastoiditis, meningitis, and
brain abscess. Cholesteatomas may be aftermaths of childhood mastoiditis with
effects witnessed as acute brain abscess, mastoiditis, or facial nerve
paralysis.
The Cranial Vault. With age, perinasal and temporal sinuses increase in
size, and sclerosis of the cranial sutures increases. Bilaterally and
symmetrically, the outer parietal tables thin, beginning parasagittally and
extending to the temporal bones. New bone formation along the inner table of
the dura mater is characteristic of hyperostosis frontalis, which is of little
clinical significance yet often mistaken for meningioma. The demineralization
of senile osteoporosis leads to decreased cranial density, especially at the
base of the vault, with decreased density of the dorsum sellae without
thinning or erosion. See Figures 8.15--17. Note: The characteristic findings of barium studies are beyond the scope
of this chapter. Please refer to a standard reference.
Etiology. Calcium loss can be attributed to either increased urinary loss
or decreased intestinal absorption. An example of urinary loss is seen in
chronic idiopathic hypercalciuria, while malabsorption is noted in conditions
such as nontropical sprue or another dysfunction of the absorption mechanism.
In the presence of decreased calcium intake, renal calcium loss often fails to
adapt, resulting in a demand for calcium from the skeletal mass resulting in
demineralization.
Note: A radiographic report of "joint-space narrowing" (viz, the IVD area)
is misleading because no space exists. What appears as reduced joint space is
narrowing from cartilage thinning at one or both interfaces or within the
anulus.
Bursitis. This disorder may occur in any joint. The shoulder area is
usually affected; however, elbow, hip, knee, and heel areas are often
involved. Bursitis is often confused with tendinitis with or without calcium
deposit because of secondary bursa inflammation.
Widespread Fibrositis. The term fibrositis is often a catch-all term used
for a vague diagnosis. There is almost always a better explanation for pain
and tenderness other than muscle sheath inflammation. Frequently, accurate
examination will lead to more distinct disorders such as osteoporosis,
osteomalacia, myxedema, tabes dorsalis, Paget's disease, malignant secondary
deposits, parkinsonism, systemic disease or some psychologic disorder or a
common disorder such as overuse, spasm, neuralgia, or radiculitis. Localized
fibrositis is usually a trigger-point syndrome and common found in the
posterior shoulder girdle (Fig. 8.19). Note: Carpal tunnel syndrome has become the "fad" diagnosis in recent
years. Thus, never take for granted that a previous diagnosis is valid
unless thoroughly substantiated by personal findings.
Hip Pain Syndrome. While osteoarthrosis of the hip is usually asymptomatic
unless the joint is overstressed, idiopathic avascular necrosis of the hip may
give severe unilateral pain of sudden onset. Tenderness will be noted over the
greater trochanter and there will be signs of bursitis and local inflammation.
See Figure 8.22. Hip motion is usually normal. In the elderly, unexplained hip
pain is often suspicious of fracture. In avascular necrosis, first seek a
history of steroid medications.
Several surveys among senior citizens suggest that senescent changes and
emotional conditioning often cloud sexual problems. It has long been held that
aging sex faculties regress and vary in gradual reduction of sexual intensity,
frequency, and urgency, but this theory is highly individualistic.
Anorexia
Since its inception, the chiropractic profession has openly stated its
concern of overmedication and drug utilization. This concern has often been
twisted unfairly by political medicine to imply a total indictment of the
medical profession. In recent years, however, an abundance of insight has
arisen within the medical and scientific communities to support chiropractic's
concern. Heavy use of aspirin may lead to gastric hemorrhage and is associated with
the iron-deficiency anemia of the elderly.
Phenacetin use leads to methemoglobinemia, sulfhemoglobinemia, and
possible renal damage.
The side effects of codeine and dihydrocodeine include dizziness,
sleepiness, and constipation.
Diarrhea may be the effect of mefenamic acid.
Gastric intolerance is often witnessed with most analgesic or
antirheumatic drugs.
The side effects of lignocaine are dizziness, blurred vision,
drowsiness, and hypotension.
Reactions to propranolol are noted in bowel disturbances, indigestion,
fatigue, dizziness, and depression, and it may predispose asthmatic attacks.
Adverse reactions to quinidine are witnessed as febrile abnormalities,
skin eruptions, thrombocytopenic purpura, respiratory embarrassment,
cinchonism, and gastrointestinal disturbances.
Methyldopa, often used in geriatric hypertensive conditions and CNS
disturbances, may react with symptoms of GI disorders, black tongue, drug
fever, drowsiness, rashes, depression, hallucinations, parkinsonism, and
hepatocellular damage signs.
The hydantoins, commonly used anticonvulsants, may lead to symptoms of
gingival hyperplasia, ataxia, nystagmus, blood dyscrasia, fever, lymphoma
syndromes, and enlargement of the liver and/or spleen.
Phenobarbitone and primidone manifest adversely in symptoms such as
nausea, vomiting, skin rashes, and personality changes.
Toxicity from the antiparkinsonism drugs exhibits as urinary retention,
vomiting, blood dyscrasia, impaired visual accommodation, dry mouth, rashes,
tachycardia, circulatory collapse, respiratory paralysis, and fainting
episodes, and such mental symptoms as hallucinations, confusion, and suicidal
tendencies --depending on the type and quantity of the drug used and patient
tolerance.
When hormonal agents are used, common side effects include diabetes
mellitus, fungus infections, pityriasis skin complications, and peptic ulcer.
Androgens may manifest in liver disorders, hypercalcemia, fluid
retention, and virilization acne.
Commonly used alkalizing agents may manifest adverse symptoms of
digestive disturbances, gastrointestinal ulcerations and hemorrhage, alveolar
capillary block syndromes, alopecia, and bone marrow depression.
Folic acid antagonists can precipitate signs of systemic toxicity such
as renal impairment, oral ulceration, diarrhea, bone marrow depression,
abdominal pain, hepatitis, and alopecia.
Fluoridated pyrimidine's side effects include gastrointestinal and
hematologic signs of toxicity.
Vinblastine alkaloids may react as symptoms of gastrointestinal
disorders, neurotoxic effects, liver damage, and hair loss.
Interarterial therapy with cytotoxic drugs may lead to systemic toxicity
characterized by thrombosis, embolism, secondary hemorrhages, septicemia,
peripheral nerve damage, and skin blistering with or without cutaneous edema.
As one of the basic causes of disease is environmental irritation of the
nervous system by mechanical, chemical, thermal, pathogenic, and/or psychic
factors, it is apparent that any measure helping to relieve such irritation,
despite its nature, constitutes indicated therapy. At times, the source of
harmful nerve irritation is obvious, simple, and accessible, making the
therapeutic approach easy. Then again, the irritating factors may be complex,
obscure, manifold, and inaccessible, posing a more complicated therapeutic
problem.
Agate J:
COMMON OTOHINOLARYNGOLOGIC DISORDERS
Aging and Hearing
The aging process tends to impair hearing, first only at the higher
frequencies and then progressing to the speech frequencies. Circulatory
impairment, acoustic trauma, and genetic factors often coexist with aging
changes that complicate the diagnosis.
Hearing loss in the elderly is usually a combined decrease in receptive
capacity due to changes in the organ of Corti and decreased discrimination
capacity from involvement of brain pathways. A sensorineural loss is often
found in impairment of taste and smell senses as well as that of hearing.
Besides frank sensory input degeneration, any involvement of the hearing
apparatus must be considered. See Figure 8.14. Diseases such as Paget's
disease of bone, otosclerosis, and osteogenesis imperfecta may have otic
consequences in the elderly.
Keep in mind that the outer and middle ear, cochlea, 8th cranial nerve,
and central nervous system, respectfully, act similar to a transformer, a
transducer, a connector, and an analyzer. Symptoms of hearing loss, tinnitus,
vertigo, or unsteadiness usually suggest some destructive process within the
transducer, connector, or analyzer mechanisms.
Disorders of the Transducer. Senile degeneration at the base of the
cochlea is the most common cause of presbycusis. Several conditions can affect
cochlea degeneration such as a manifestation of a previously asymptomatic
genetic disorder. Other examples include autosomal dominant progressive
hearing loss, trauma from flagrant environmental noise, or a reaction to
ototoxic drugs.
Disorders of the Connector. In the elderly, involvement of the 8th cranial
nerve is found in such conditions as acoustic neurinoma (with possible
superimposed cochlear degeneration), cochlear artery aneurysms, intracranial
tumors, or metastatic tumors at the base of the skull.
Disorders of the Analyzer. Older individuals generally have diminished
capability in understanding complex language or interpreting sounds
superimposed over a background noise. Thus, elderly hearing loss may not be
strictly cochlear involvement but an associated CNS disorder.
Nasal Disorders
Four common geriatric nasal disorders require mention. These are the virus
infections, epistaxis, rhinitis, and sinus malignancies. Virus infections show
no unusual manifestations except recuperative powers are often diminished
in the elderly because of deterioration. Epistaxis in the elderly can be
severe enough to threaten life. Rhinitis is often seen as a result of chemical
irritation from overuse of nasal sprays and nose drops. Environmental
atmospheric pollutants may precipitate a vasomotor rhinitis associated with
sneezing episodes and rhinorrhea. Sinus malignancies have a higher incidence
in the elderly. Characteristics include maxillary pain, infraorbital nerve
paresthesias, lower jaw edema, bloody nasal discharge, loosening of teeth, or
oroantral fistula.
Throat Disorders
Postnasal discharge in the elderly usually presents subjective complaints
that are difficult to relate to clinical findings. Occasionally, nasopharynx
crusting and inflammation exist that usually respond well to conservative
treatment.
Costen's TMJ syndrome features joint pain, tinnitus, and pressure
sensations in the ears. The pain is usually referred to the jaw, ear, or both.
Acute dysphagia of rapid onset is often symptomatic of epiglottitis, that
can be fatal without tracheostomy because of the loss of a patent airway.
Hoarseness persisting over several days is suspicious of cord paralysis,
malignancy, leukoplakia, tuberculosis, laryngeal nodes, or localized
hyperplasia. Cerebrovascular accidents often present symptoms of dysphagia and
laryngeal paralysis. Vocal cord paralysis is usually related to vagus
involvement (peripheral or central connections) or a tumor.
Nasopharynx malignancy is often first noted by concomitant nasal
obstruction and fluid in the middle ear. Carcinoma of the larynx, pharynx, or
tonsil is often first noted by related dysphagia and odynophagia. Leukoplakia
of the vocal cord is often considered precancerous.
Disorders Affecting Communication
Speech disorders are the result of a breakdown in any one of the various
organs or functions involved in the speech-producing process --from the lungs
to the articulators of the mouth. The nervous system integrates and
coordinates all speech processes. However, with age, there is a tendency for
system breakdowns that progress and increase with advancing years. Central
nervous system disorders especially affect the integrating mechanism and
principally arise from cerebrovascular accidents. Parkinson's disease and
generalized CNS disorders also result in degenerative processes that manifest
in the elderly as senile speech impairments. Aphasia, acalculia, amusia,
agnosia, and dysarthria are symptoms commonly reflecting CNS involvement.
COMMON ORTHOPEDIC DISORDERS
General Roentgenographic Aspects of Aging
The Skeleton. Skeletal atrophic and hypertrophic changes are readily
visible in x-ray films of the elderly. Usually noted is a generalized skeletal
atrophy with proliferation at attachment sites in the form of hypertrophic
osteophytes.
The physiologic effects of aging are often noted in calcification of the
dura mater, petroclinoid ligaments, falx, tentorium, pineal body, choroid,
carotid siphon, intercavernous portions of the carotid artery, and diaphragm
sellae. Calcification found above the level of the sella may indicate an
aneurysm.
The Spine and Pelvis. Exostoses found at the ischial tuberosities and
iliac crests, spinous processes, and external occipital protuberance in the
elderly are attributed to aging changes rather than pathology. Stress at the
insertion of the perispinous ligaments is reflected in spur formation along
the anterolateral aspect of the vertebral bodies, while disc stress is noted
by hypertrophic spondylosis. Osteophyte formation is usually the result of
concavity stress in kyphosis or scoliosis. Senile ankylosis is a term commonly
used to describe extensive calcification of the anterior paraspinal ligaments
to the extent that the disorder imitates ankylosing spondylitis. Bone changes
underlying skin lesions of decubitus ulcers and infection are the result of
osteomyelitis and commonly found at the ischial tuberosities and heels.
The Extremities. Also noted in the elderly skeleton is enlargement of
external bone contours at attachment insertions with coexisting thinning of
cortices, especially in the flat bones of the hands, feet, and femur.
The Chest and Heart. Normal changes noted in the elderly are associated
with decreased bone density. While heart size does not typically increase with
age, it may appear so relatively with progressive kyphosis, increased A-P
diameter of the thoracic cage, and decreased lateral diameter of the cage,
which appear to have no relationship with pulmonary disease. Calcification of
the left coronary artery and calcified infarcts are often seen on film in
advanced lesions, Pulsations from the thoracic aorta may produce in time
osteophytes of the thoracic spine on the right.
The Abdomen. Increased density of thickened aortic walls and frequent
calcium deposits are characteristic of aortic arteriosclerosis. Signs of
aneurysm may be noted. Calcification may be seen of the splenic artery in the
upper left quadrant, of iliac and femoral vessels or aneurysms, of the renal
artery near the kidney hilus, and/or of the abdominal aorta anterior to the
spine in lateral views.
Basic X-Ray Manifestations of Systemic Disease
Periosteal new bone formation is a significant finding, often indicating
manifestation of systemic disease. In the long bones, it is usually a sign of
intrathoracic disease or chronic venous stasis.
Bone changes in diabetics are characterized by neurotrophic changes and
the results of vascular insufficiency and infection. Neurotrophic changes,
usually associated with osteomyelitis and adjacent soft-tissue infection, are
commonly manifested in the feet and toes and noted by progressive tapering of
the distal ends of the phalanges and metatarsals along with bone resorption
(not necessarily irreversible).
Skeletal diseases such as osteoporosis, arthritis, Paget's disease, bone
neoplasms, rheumatic disorders, and fractures and dislocations are described
in subsequent pages.
Osteoporosis (Osteopenia)
Osteoporosis is generally characterized clinically by shortened stature,
kyphosis, and predisposition to skeletal fractures. X-ray manifestations in
the late stages include decreased bone density as the result of
demineralization. The five most common causes are calcium loss, decreased
physical activity, or deficiencies of calcium, protein, or hormones.
Intolerance to milk products may lead to a deficiency in calcium with
associated lactase deficiency. Decreased physical activity, either from
immobilization or apathy to exercise, leads to osteoporosis because muscular
stress on bone insertions is an important stimulus for bone formation and
health.
Osteoporosis is not necessarily a sign of calcium loss or deficient
intake. It may be associated with inadequate protein and/or vitamin
deficiencies. Bone changes from protein deficiency are often noted in
association with characteristic skin atrophy and changes in subcutaneous and
muscle tissues. Vitamin C plays an important role in the formation of bone
matrix.
There may also be a hormonal factor. Demineralization is often seen
associated with hypogonadism and female gonadal dysgenesis, thus a decrease of
estrogens and androgens may be a contributing factor in osteoporosis. In
addition, an imbalance between the sex hormones and adrenal secretions affects
the relationship between bone formation and resorption leading to
demineralization of the skeleton.
Pathology. Normal bone chemistry is maintained by a balance between bone
formation and resorption. Thus, osteoporosis results either from increased
resorption or decreased formation. While decreased bone formation as the
result of decreased osteoblastic activity is rare, increased bone resorption
is stimulated by any factor tending to raise the plasma calcium level. This
level is normally maintained despite variances in intake or loss by release of
bone calcium governed by the parathyroids. In the elderly, slight but chronic
acidosis leads to dissolution of bone calcium to meet the need for an alkaline
buffer.
Clinical Symptoms, Findings, and Signs. In the early stages, the disorder
is usually asymptomatic, even to the point of vertebral collapse. Initial
symptoms are usually confined to back pain in the thoracolumbar area
associated with paravertebral muscle spasm that is increased on percussion,
jarring, flexion, and extension. On vertebral collapse, nerve root involvement
may refer pain to substernal and/or abdominal areas. Vertebral collapse leads
to progressive spinal deformities, a reduced lumbar curve, and an increased
thoracic kyphosis, all which tend to affect respiration and cardiopulmonary
dynamics predisposing pulmonary disease.
Roentgen findings are characterized by prominent demineralization that is
especially noted in dorsal, lumbar, and pelvic cortical thickness. Vertebral
bodies appear shell-like and biconcave, with biconvex IVDs progressing to
herniation and resulting Schmorl's nodes. Vertebral fractures on minor
overstress may be associated such as of the ribs, neck of the femur, and lower
end of the forearm. Fracture healing is slow, and callus formation is minimal.
Roentgen findings alone rarely can be used for the basis of diagnosis because
of the often indistinguishable picture presented with hyperparathyroidism,
osteomalacia, osseous metastases, and multiple myeloma.
Blood chemistry is more supportive of the disorder when normal blood
chemistry is found than when it is abnormal. Serum calcium, phosphorus, and
alkaline levels are usually normal.
Urinary calcium and phosphorus excretion levels are usually normal in
senile osteoporosis. Specialized investigations such as bone densitometry,
tetracycline labeling, histologic studies, radioisotope trace studies, calcium
balance studies, calcium tolerance tests, and acoustical methods are all
helpful in differentiation, but none are absolute in themselves.
Other Causes of Demineralization
A condition offering roentgen findings similar to osteoporosis is
osteomalacia, which is associated with vitamin D deficiency or secondary to
chronic pancreatitis or liver/gallbladder disease. Here, fractures are of the
greenstick variety, and bowing of the extremities is often noted. In
differentiation from senile osteoporosis, serum calcium, serum phosphorus, and
calcium excretion levels are usually low. Serum alkaline phosphatase levels
are typically high.
Multiple myeloma presents a picture of demineralization associated with
punched-out radiolucent skeletal lesions. It is differentiated from
osteoporosis by severe and persistent bone pain, and the possible presence of
hypercalcemia and hypercalciuria. Blood chemistry shows a reversed A/A radio,
hyperglobulinemia, an abnormal electrophoretic plasma pattern, and/or the
presence of Bence-Jones protein.
Neoplastic bone disease also reveals roentgen signs of demineralization.
Even if a primary neoplastic lesion cannot be located, suspicion is enhanced
by hypercalciuria, hypercalcemia, and high serum alkaline phosphatase.
Signs of demineralization are noted in both hyperthyroidism and
hyperparathyroidism. Hyperthyroidism is characterized by hypercalcemia,
hypercalciuria, and data from thyroid functions tests such as the BMR and PBI.
Hyperparathyroidism is differentiated frequently by subperiosteal bone
resorption and the moth-eaten appearance of cortical outlines of the phalanges
or lateral ends of the clavicles, along with an incomplete outline of the
lamina dura. The skull in hyperparathyroidism often shows a stippled
salt-and-pepper appearance. Recurrent kidney stones can be associated. The
laboratory picture includes hypercalcemia, hypophosphatemia, high calcium
excretion, normal-to-high serum alkaline phosphatase, and increased plasma
parathyroid hormone.
Vitamin D intoxication may reveal roentgen demineralization from
self-medication of 150,000 units/day or above, leading to osteoporosis and
osteitis fibrosa cystica. Hypercalcemia and hypercalciuria are usually
present. Complications such as calcification of soft tissues, renal stones,
and supravalvular aortic stenosis are helpful in differentiation.
Chronic alcoholism and liver disease may present roentgen findings such as
demineralization. Fractures associated with the decreased bone density are of
different bones than those commonly associated with senile osteoporosis and
are linked to a history of prolonged alcohol intake. Jaundice will usually be
associated with the demineralization associated with obstructive liver
disease.
Secondary osteoporosis is usually attributed to a drug reaction or a
consequence of another disease. Examples of drug reactions are seen in
osteoporosis resulting from cortisone and heparin use. Osteoporosis is often
seen secondary to endocrine disturbances such as Cushing's syndrome,
hyperthyroidism, hyperparathyroidism, diabetes mellitus, or prolonged
immobilization such as from casts, braces, or prolonged bed confinement.
Paget's Disease
This geriatric condition is characterized by excess bone resorption and
deposition often resulting in sclerosis, abnormal bone destruction processes
and overgrowth resulting in severe deformity and other findings associated
with osteitis deformans. Multiple areas of the skeleton are involved in the
polyostotic form; however, the disease is usually monostotic and limited to a
single bone or area.
While roentgen films are classic, the patient is usually asymptomatic
until the very late stage. Initial symptoms are usually of bone pain at the
site. Skeletal deformities, long-bone fractures, spinal cord or nerve root
compression and resulting paraplegia are frequent complications. Other
complications include cranial nerve compression in skull involvement or high
output heart failure from multiple small arteriovenous fistulae in areas of
the bone involved. Pain and swelling in the humerus or femur can suggest a
complicating osteogenic sarcoma.
Paget's disease is commonly located in the pelvis, femur, tibia, vertebra,
rib, clavicle, humerus, skull or mandible. Early roentgen findings in the
porotic phase reveal lesions of demarcated radiolucent areas (osteoporosis
circumscripta) that usually are found in the skull, tibia, and ilium. Later
findings show large areas of demineralization surrounded by sclerotic changes,
followed by bony overgrowth from successive layering of new bone in the
periosteum, cortex thickening, and a trabecular pattern that is coarse and
dense.
Differentiation must be made from osteoblastic metastatic disease. Bone
in Paget's disease is prone to fracture and bending. Femur curvature, anterior
tibial bending, femur acetabular protrusion, and protrusion of the odontoid
into the base of the skull may be found. Fracture is typically associated with
the femur or tibia. Laboratory findings usually reveal high serum alkaline
phosphatase during the bone deposition stage or if osteogenic sarcoma is
present.
Rheumatoid Arthritis (RA)
An acute onset of RA in the elderly is not uncommon, even in those over
80. In the acute geriatric manifestation, the onset is explosive,
polyarthritis is rapid, and edema in the hands and feet are gross. In chronic
RA in the elderly, geriatric deterioration often offers a cloudy picture.
Cervical subluxation with cord compression offers deceptive conclusions.
Suppurative arthritis, spontaneous fractures, and vertebra collapse are common
complications --especially if the patient has been under steroid medication.
Ulcerative colitis, psoriasis, and regional ileitis may be associated. Acute
thyroiditis or pleuritis may coexist and be predisposing factors.
A history of rheumatic fever, fibrositis, tenosynovitis, rheumatism, or
bursitis is frequent. The onset appears to follow overstress from trauma,
infection, or a severe emotional upset (eg, death in the family, divorce).
Severe involvement leads to tendon sheath swelling; a swollen joint that is
red, warm to the touch, and tender; subcutaneous extensor nodules; and
multiple deformities with severe destructive changes particularly in the
weight-bearing joints. Morning stiffness and a steady burning pain in the
affected joints are classic symptoms.
Roentgen findings are specific but subtle in the early stages. Joint
erosions; subchondral cysts and joint space narrowing, without osteophytes or
sclerosis; and justa-articular osteoporosis are typically seen in radiographs.
RA of the hands and fingers are the most common initial sites, with the knees
and spine secondary. Advanced RA of the cervical spine reveals profound
abnormalities with subluxation and bony erosion. Complete erosion and shearing
of the odontoid process may be seen. Sacroiliac involvement is also common.
Osteoarthritis (OA)
Because uncomplicated OA is noninflammatory, it is better termed
osteoarthrosis or degenerative joint disease. It is characterized by
degeneration of articular cartilages and adjacent tissues. Stress from aging
and daily trauma appears to be a predisposing factor, but this is
controversial as OA rarely involves the ankle and often involves the fingers.
Fingers and weight-bearing joints such as the knees, hips, pelvis, and spine
are the most common sites. The knees and hands have the highest incidence.
Typically, the affected joints are mildly swollen, crepitant on movement, and
tender to compression.
Roentgen findings include articular cartilage thinning, thickening and
sclerosis of underlying subchondral bone, sharpening and lipping at joint
margins, and asymptomatic cysts in adjacent bones. OA is associated with
calcified or ossified loose bodies formed from the metaplasia of detached
cartilage fragments.
Gout and Abnormal Calcification
As with RA and OA, the incidence of gout increases with age and is often
precipitated by emotional overstress. The patient's history usually reveals
brief attacks with intervals of complete remission --sometimes preceded by an
attack of the "flu" or some other acute GI disturbance. The onset of an acute
manifestation usually involves a single joint such as of the toes, knees,
wrists, fingers, or elbows. The affected joint is severely painful and swollen
with acute effusion. The clinical picture can resemble cellulitis. Fever is
common during the acute onset, and the disorder generally appears to be
brought out by acute infection, joint trauma, drug, and especially emotional
reactions. Hyperuricemia is an important laboratory finding.
Roentgen findings in the initial stage are absent. In the later phase,
punched out bone lesions and tophi manifest. Renal colic, hypertension, and
calcification of menisci or hyaline cartilage are often associated.
Tenosynovitis, bursitis, periarthrosis myalgia, and RA may be superimposed on
gout.
Pseudogout, a pyrophosphate arthropathy, is usually asymptomatic and first
noted in roentgen findings. Film analysis shows punctate radiopacities
particularly in menisci, IVDs, articular discs, distal radioulnar joints, the
acetabular or glenoid labrum, and/or the symphysis pubis. It is not uncommon
to see a faint line of hyaline cartilage calcification in the large joints.
While the disorder is usually asymptomatic, it may progress to resemble acute
gouty arthritis or progressive arthropathy.
Extra-articular calcium apatite deposits present a picture of acute pain.
Deposits are commonly found in the rotator cuff of the shoulder or in the hip
near the greater trochanter. They occasionally are seen in the feet and hands.
Agonizing spontaneous pain in the shoulder is often the result of tendon
calcification. Calcification of knee menisci is usually asymptomatic.
Other Pertinent Geriatric Arthropathies
Degenerative Joint Disease in the Hands. Heberden nodes are often the
cause of pain; in the elderly however, they are more unsightly than
symptomatic. Mild pain is associated with the less common proximal
interphalangeal joint degenerative changes. Osteoarthrosis of the
carpometacarpal joint of the thumb and other wrist joints often cause
considerable disability in hand dynamics in the elderly. See Figure 8.18.
Suppurative Arthritis. This disorder commonly involves large joints such
as the knee and hip, but the ankle, shoulder, elbow, or wrist may be involved.
It is often associated with RA patients receiving systemic or local steroids.
Staphylococcal infection is the most common form, and immediate diagnosis is
important as the enzymes rapidly destroy cartilage. Unfortunately, the elderly
do not offer a clear clinical picture as do the young. An unexplained joint
swelling may be the only physical sign.
Bone and Joint Tuberculosis. In the elderly, the condition is usually
benign and deceptive. Unexplained pain or joint swelling may be the only
physical findings. Common sites are the spine or single joint arthropathy.
Pulmonary Osteoarthropathy. Occasionally, osteoarthropathy is witnessed
clinically in the absence of finger clubbing. The cause is unknown, and
involvement is peripheral and especially noted in the hands. X-ray findings
may show fine periosteal reactions in the hands, forearms, and ankle areas.
Coexisting clubbing and osteoarthropathy are highly suspicious of bronchogenic
carcinoma.
Intervertebral Disc Rupture. Herniation is not as rare in the elderly as
is often supposed. As in the young, rupture causes severe symptoms of spinal
and referred pain.
Neuropathic Joints and Neurotrophic Disorders. An unstable, relatively
painless, destroyed joint is classic. Roentgen findings show ectopic bone
especially in the weight-bearing joints, but they are also found in the
shoulders, hands, and other joints. In the elderly, the condition is usually
associated with tabes dorsalis, but it is also related to such a variety of
disorders as diabetes, disseminated sclerosis, brain damage, paraplegia,
syringomyelia, myelitis, peripheral neuropathy, leprosy, and reaction to
steroid medication. When tabes is primary, involvement will usually be of the
knee, foot, ankle, hip, or spine. Diabetes will most commonly affect the foot
(especially tarsal and metatarsal joints) and ankle. While paraplegia will
usually affect the upper thigh, syringomyelia will usually involve the upper
extremity.
Malignant Arthropathies. Pain is usually long standing in metastatic
disease far before x-ray films show evidence. While pain is common in
metastatic disease in all weight-bearing joints, it is often a vague and
aching discomfort rather than a strikingly severe syndrome. Fractures through
metastatic lesions are not unusual, especially in the aged. In the lower
extremities, the femur is the most frequent bone involved. Metastases are
rarely seen below the knee in the elderly.
The clinical picture of metastatic arthropathies often resembles the
appearance of RA or bilateral shoulder-hand syndrome. Such disorders are
related to malignant tumors, especially bronchogenic carcinoma. In women, the
primary site is almost always the breast. In men, primary sites are often
found in the lung, kidney, or prostate. Osteoblastic metastatic lesions found
in men are invariably from the prostate. Long-standing osteomyelitis with
draining sinuses may progress to carcinoma. Physical stiffness with little
swelling may be the only early outer signs.
Primary bone or joint malignant lesions are much less common than those
from metastasis. Chondrosarcoma, Paget's sarcoma, and lymphoma are the most
frequently witnessed primary lesions. Myeloma presents characteristic
radiographic findings of a solitary lesion resembling secondary lytic neoplasm
and extensive demineralization resembling osteoporosis. Small sharply defined
multiple lesions can involve the total skeleton, but they are especially found
in the skull and ribs.
Pertinent Syndromes in Geriatric Orthopedics
Polymyalgia Rheumatica. Patients over 60 may develop symmetrical pain and
stiffness having a tendency to ease during the day and become severe at night,
yet not be associated with distinct rheumatic arthropathy. In the order of
incidence, the common sites are the shoulders, hips, spine, and limbs. Weight
loss and a high sedimentation rate are associated. The syndrome is often (50%)
related to potentially dangerous giant cell arteritis.
Shoulder-Hand Syndrome and Sudeck's Atrophy. Unexpected severe stiffness
and persistent pain throughout the hand may be witnessed following hand/wrist
trauma or Colles' fracture of the wrist. The syndrome is called Sudeck's
atrophy when confined to the wrist area; shoulder-hand syndrome when limited
to the shoulder and elbow or forearm. Both syndromes are frequently
misdiagnosed as capsulitis or carpal tunnel syndrome. The cause is unknown,
yet many believe it is some aberration of the nervous system, possibly
secondary to neuropathy, coronary artery disease, bronchogenic carcinoma, or
pulmonary tuberculosis. Osseous structure is shown in Figure 8.20.
Sudeck's atrophy in the lower extremity is usually confined to the foot
and ankle following trauma; eg, fracture, nerve or ligament injury. Vasospasm
of the terminal arterioles results in degenerative changes, edema, tenderness,
and a glossy cyanotic overlying skin. Burning pain occurs that is prominent,
persistent, aggravated by movement, and often associated with paresthesia.
Roentgen findings show a spotty localized osteoporosis distal to the site of
injury.
Spinal Pain Syndromes. This subject has been described in greater detail
in other chapters; however, it is important to mention here pain from senile
degeneration and resulting loss of spinal mobility. Roentgen findings commonly
reveal atrophy in discs and apophyseal joints. Rare is the absence of
osteoporosis, and osteophyte formation may be extensive. As in the young, pain
may be from unusual postural overstress. Almost all pain originating from
nerve root involvement will be increased on active and passive spinal motion.
Cervical rotation will usually increase neck pain (often referred to the
arm) if root compression exists. Again, carpal tunnel syndrome is a common
misdiagnosis. Rotation may also elicit vertigo, occipital headache, and neck
pain when vertebral artery compression is a factor. Degenerative changes in
the cervical area are the most common cause of spinal cord compression.
Thoracic pain is more common in the elderly than any other age group. Pain
is increased on thoracic rotation. Cutaneous hyperesthesia can usually be
demonstrated in root distribution (nerve tracing).
First sacral and L5 root compression is common in both the elderly and the
young; however, the incidence of upper-lumbar root compression increases with
age. Disc protrusion may cause compression of the cauda equina leading to
lower extremity claudication. While osteoporosis is usually asymptomatic,
sudden vertebral collapse will produce spontaneous pain.
Shoulder Pain Syndrome. While shoulder OA is rare, tendon and rotator cuff
tendon degeneration is common in the elderly. This syndrome is usually
associated with shoulder capsulitis following shoulder trauma, cervical
subluxation, or chest disorders. The condition is characterized by uniform
motion restriction, pain on passive movement in all directions, and the
absence of abnormal roentgenographic findings. Differentiation must be made
from referred pain from the liver, gallbladder, or right diaphragm that may
demonstrate identical shoulder signs. Keep in mind that local tenderness and
spasm may also be referred.
Elbow Pain Syndrome. Following trauma or chronic arthritis, osteoarthrosis
of the elbow may be the cause of elbow pain, swelling, crepitation, and motion
restriction. See Figure 8.21. The ulnar nerve may be damaged; rarely, the
posterior interosseous nerve is affected.
Carpal Tunnel Syndrome. This syndrome is more insidious in the elderly
than in the young. It is characterized by compression of the median nerve in
the carpal tunnel resulting in the classic features of numbness and tingling
of the first three fingers (especially at night), with pain often radiating
into the first three fingers and/or up the forearm. There is the possibility
of thenar wasting and weakness of thumb opposition. The disorder is often
secondary to old trauma, circulatory disturbances, entrapment syndromes, RA,
myxedema, and myelomatosis.
Knee Pain Syndromes. Especially in the elderly, degenerative changes will
be encouraged by obesity, former occupational stress, or almost any of the
arthritides. The affection may be widespread throughout the knee or localized
in the area of the patella or popliteal space. Lateral instability, stiffness,
and severe weight-bearing pain are common. Intermittent episodes of painful
spasms are usually caused by hemarthrosis (with splinting) or loose bodies
(with locking) of the joint. In all knee afflictions in the elderly, it is
important to differentiate such conditions as osteochondritis dissecans,
osteoarthritis, tumors, fractures, and neuropathic joints.
Ligament injuries are less common in the elderly because of reduced
strenuous activity. It naturally follows that semilunar cartilage lesions are
primarily degenerative rather than acute traumatic. Quadriceps muscle
avulsion, osteonecrosis, and flattening of the articular surface of the medial
femoral condyle are three conditions growing in incidence with the elderly.
Quadriceps muscle avulsion, as from a fall, is characterized by loss of
active knee extension and tenderness and swelling at the top of the patella.
Osteonecrosis is characterized by persistent and progressing acute medial knee
pain. Effusion, synovial thickening, and a decreased motion range will be
noted. Roentgen examination may determine a flattening of the articular
surface of the medial femoral condyle. The lesion will be localized at the
weight-bearing surface of the medial femoral condyle and surrounded by a
sclerotic reaction. In later stages, subchondral radiolucency will be seen.
See Figure 8.23.
Ankle Syndromes. Ankles in senior citizens tend to show a general synovial
thickening, especially in the obese. The subtalar joint stiffens with aging;
however, the joint limitation is usually asymptomatic. See Figure 8.24.
Foot Syndromes. In the elderly, years of putting a normally wide forefoot
into narrow shoes result in bunions, bunionettes, hallux valgus deformity,
secondary OA, hammer toes, and dorsal calluses. The senile foot is noted for
its poor blood supply, resulting in significant changes from arteriosclerosis
and diabetic effects. Such conditions readily predispose to local edema,
slough, infection, and even gangrene on slight provocation. See Figures 8.25
and 8.26.
The skin of the foot is especially sensitive, atrophic, delicate, and very
prone to pressure ulcers over and under callosities. Aging changes result in
subcutaneous tissue and fat pad atrophy resulting in weight-bearing bone pain.
While asymptomatic OA in the foot is often noted from x-ray examination,
painful OA is uncommon. Foot pains, particularly in the toes or plantar
fascia, are common complaints and usually attributed to degenerative joint
changes or gout.
Dislocations and Tendon Ruptures
Dislocations in the elderly are much lower in incidence than in the young.
The shoulder is the most common dislocated joint, not the hip. Because of
geriatric demineralization, humerus neck fractures are common. Similarly, hip
dislocations in the elderly are rare; hip fracture is more common.
Tendon ruptures are often suffered by the elderly yet mistakenly
diagnosed. Degenerative changes associated with aging often predispose
spontaneous tendon rupture. This is often seen in the rotator cuff, biceps
brachii, thumb extensors, quadriceps femoris tendons, or the Achilles tendon.
While rupture of major tendons requires surgical care, partial or incomplete
rupture of the minor tendons can often be treated conservatively.
Embolic Considerations
Pulmonary embolism is a major concern in geriatrics following fracture of
a long bone or lower extremity surgery. In addition, fat embolism may result
from trauma. In fat embolism, shock appears to play a role, but the mechanism
is undetermined. Fat embolism may cause sudden death.
Circulatory Deficiency
While not an orthopedic problem, circulatory deficiency is mentioned here
because such disturbances are frequently misdiagnosed. For example, hip pain
resulting from inadequate circulation (intermittent claudication of the hip)
is often misdiagnosed as arthritis of the hip in the elderly.
Geriatric Fractures
Fracture may be the first symptom of a disease process in the elderly.
Metastatic tumor and advanced osteoporosis are classic examples.
The most common upper-extremity fractures occurring in senior citizens are
clavicular, humeral neck, elbow area, wrist, and rib fractures. Of fractures
of the spine and pelvis, vertebral fractures are by far the more common. Most
are either compression fractures with wedging or intercorporeal fractures.
Hip fractures are commonly encountered in the elderly. Of femur neck
fracture or fracture in the region of the trochanter, the latter is more
common. Other fractures of the lower extremities often seen in the aged
include fractures of the femur shaft, supracondylar femoral fractures,
patellar fractures, and fractures of the upper tibia, tibial shaft, ankle,
tarsals, and metatarsals.
SEXUAL ASPECTS OF AGING
Sexuality in the Latter Years
The concept of a male climacteric is still unresolved. Germinal and
endocrine functions of testicular tissue are maintained into advanced years.
Anatomical, physiologic, and endocrine factors are all involved in the aging
process, but there are also psychologic, sociologic, and pathologic factors to
be considered in reduced sexuality of the aged.
Conventional opinion holds that physical changes in men are pre-eminent in
the decline of systemic and sexual capacities. In women, decline is more a
social effect. In men, all forms of sexual activity usually lessen in the 7th
decade of life. The frequency of marital coitus decreases rapidly after 70
years, yet there appears to be a reduction of youthful inhibitions that may
lead to low-incidence sexual psychiatric disorders in males. In women, the sex
drive continues far into the later years. This often leads to increased female
frustrations.
Influences on Function
While diabetes, spinal cord trauma, alcoholism, and other disorders of
nervous system may affect potency, most conditions can be attributed to
psychogenic factors. Social myths and codes often interfere with the ability
to perform. Overexposure with the sexual partner, a part of the retirement
syndrome, may play an important psychologic role. Unfortunately, sexual
interest in the male senior citizen may reduce while the interest of his
postmenopausal partner might increase due to the removal of the fear of
pregnancy.
Impotency
There appears to be little correlation between sexual potency in the
latter years and hormonal insufficiency. While congestive prostatitis often
plays a role in geriatric impotence, psychogenic and sociopsychologic factors
predominate. Medications (especially those given for hypertension) can
also depress potential, libido, or both, and are often overlooked as dampening
influences. This is true at all age levels, but more noticeable in the
elderly.
Sedatives, psychotropic drugs, and other agents affecting the central
nervous system are known to contribute to impotence. Many authorities believe
amphetamines and Tegamet for gastric ulcers, while not altering sex hormone
levels, tend to decrease libido. Vasomotor depressants such as rauwolfia
serpentine have been shown to inhibit estrus and fertility without affecting
testis function because of an affect on the hypothalamus and biochemical
levels.
COMMON COMPLAINTS AND SYMPTOMS IN LATER YEARS
Loss of appetite in the elderly may be associated with psychologic,
functional, or organic causes. It is often the first sign noted in disorders
of a toxic or pyrexial nature and the last thing to recover in convalescence.
It is almost always associated with liver disease, renal failure, uremia, and
gastric carcinoma. Anorexia is a general component of nihilism and depression
and, especially in elderly women, may present itself as anorexia nervosa.
Anorexia may be the first sign of a digitalis over dosage, noted even before
the stages of vomiting and bradycardia. In situations where not so serious
causes manifest, a glass of wine often serves as an appetizer if this is
agreeable with the patient.
Blindness
Diminishing vision in the aged is not necessarily an effect of pathology.
Presbyopia is widespread among senior citizens. Complaints of photophobia
should not be ignored as this sign is often indicative of developing
cataracts. Sudden blindness in one eye may be significant of retinal
detachment, retinal vein thrombosis, or hemorrhage. Bilateral sudden blindness
is occasionally seen as the result of stroke (occipital cortical lesion);
rarely is it hysterical in old age. Retinopathy from giant-cell arteritis
requires prompt treatment to prevent blindness.
Constipation
Constipation in the elderly is occasionally the result of organic,
functional, or psychogenic causes. It just may be from lack of exercise or
liquids. Organic causes are usually attributed to mechanical or paralytic
obstructions, neoplasms, diverticulitis, or inflammatory stenoses. The
functional causes most often witnessed are those affecting the storage,
transportation, or evacuation mechanisms of the colon from either systemic or
neurogenic disorders. The systemic disorders are usually debilitating
infections or endocrine dysfunctions; while the common neurogenic disorders
are irritable colon, inactive colon, or acquired megacolon.
In an inactive colon, the bowel fails to respond to normal stimuli to
prompt evacuation. This may be due to interference with normal nerve reflexes
such as from lumbar subluxation or just lack of stimuli from eating or
exercise. Both acquired megacolon or the congenital variety seen in children
are the result of a disorder of the intrinsic nervous network controlling
colon movements. The acquired variety is often related to psychologic
disorders.
While bowel emptying once every 4 days is not unhealthy, many senior
citizens believe in "regularity" and are convinced of the need for consistency
in stool color, quantity, and content appearance. This phobic concern can lead
to habitual use of laxatives that can cause the "imaginary constipation" to
progress to a chemically initiated irritable colon.
Deafness
Hearing loss is not an inevitable consequence in old age except for that
of high-pitch sounds. Perception or nerve deafness is more common in the
elderly than conduction deafness. When deafness does occur, resulting
frustrations, superimposed egocentricities, and attitude changes are more
often the major concern rather than the loss of hearing.
Dysphagia
Difficulty in swallowing is rarely functional in the elderly. Achalasia is
rare in the elderly, but hiatal hernia is widespread and leads to reflux
esophagitis that increases the dysphagia. Causes for dysphagia may be found at
the upper end of the digestive tract, abnormalities of the tongue root, of the
fauces, and/or of the pharynx. Cancer, pouches, or abscesses are the most
common disorders discovered. Dysphagia is also associated in the elderly with
globus hystericus, the dysphagia of Plummer Vinson syndrome, and iron
deficiency states. When dysarthria and impaired locomotion are associated with
dysphagia, stroke involving the mechanism of deglutition is suspect,
especially pseudobulbar palsy of cerebrovascular origin.
Dysphagia is a common sign in larynx carcinoma, postcricoid carcinoma
(especially in women), and midesophageal carcinoma (especially in men).
Obstructions at the upper or middle esophagus may be neoplastic, but they are
more suspect of benign diverticula or involuntary pain spasms. Painful spasms
associated with dysphagia and angina-like symptoms suggest tension diverticula
or a "corkscrew" esophagus. Lower esophageal swallowing difficulties are often
linked to neoplasms. On the other hand, bronchial carcinoma and atheroma
rarely cause dysphagia.
Dyspnea
In geriatrics, acute or chronic breathlessness can be helpful or
misleading. In the normal aging process, there is a steady decline in lung
function: vital capacity reduces, ventilatory capacity reduces, and residual
volume increases. With these factors in mind, it is not unusual that the
elderly become breathless from exertion; however, acute and chronic
breathlessness may be indicative of serious causes. Chronic dyspnea is noted
in the aged in cases of obesity, anemia, lung disease, and heart disease.
Breathlessness at rest points to chronic cardiopulmonary insufficiency, but it
is more common during middle age than the later years.
Periodic attacks of breathlessness may be one of the first
life-threatening signs witnessed in periodic Cheyne-Stokes respiration, acid
base imbalance, cerebral vascular disease, or a variable cardiac output
resulting from myocardial ischemia. Acute dyspnea in the elderly that is
urgent is associated with left ventricular failure. Acidosis presents
persistent, deep, panting respirations related to a debilitated patient.
Acute dyspnea resulting from pulmonary embolism may occur at any age.
However, in geriatrics, such a sudden onset is commonly attributed to
inhalation of a foreign body, a plug of mucous, or a bolus of food. Acute
dyspnea with a coexisting increased respiratory rate soon followed by a rise
in pulse rate may be the first signs of respiratory tract infection, even in
the absence of fever.
Fainting and Convulsive Attacks
During the later years, fainting spells are often associated with minor
periodic abnormalities of cardiac output affecting peripheral and cerebral
circulation. Vasomotor instability resulting in simple syncope is a condition
more common in youth. Overbreathing, especially seen in elderly women, often
leads to alkalosis and even to tetany without classic demonstrable carpopedal
spasms and Chvostek's sign. In the elderly, sudden fainting attacks are
associated with anemia, hypoglycemic episodes (often associated with
diabetes), or cerebral anoxia from undiagnosed melena.
Acute fainting attacks related to acute low blood pressure are suspect of
cardiovascular causes. Fainting, fits, and falling spells are frequently
indicative of cardiac infarction, especially if a triple rhythm is noted that
was not previously present. Acute collapse, prostration, near panic, and often
sudden diuresis attacks are associated with paroxysmal tachycardia or
paroxysmal fibrillation if a high pulse rate is coexistent. Such signs are
also suspect of Stokes-Adams attacks from cardiac conduction defects.
Acute vertigo, weakness, and possibly convulsions following neck rotation
during extension are frequent symptoms of carotid sinus sensitivity or
spondylosis affecting vertebral artery circulation. Falling attacks that are
spontaneous in which consciousness is not lost is a common complaint of
unknown cause. However, actively pushing the extended sole of the foot against
resistance immediately results in returned tone and power to the lower
extremities.
Major fits in old age are frequently associated with the initial sign of
stroke or serious cardiac infarction. Epileptic-like attacks (focal Jacksonian
type) are usually the result of cerebral ischemia from an atheromatous plague.
Fatigue
Progressive with age, movements become slower and laboriously done. Rapid
or strained movements are of short duration. Paradoxically, while anxiety and
psychosomatic disorders are rare in the elderly, feelings of general fatigue
are more psychogenic than organic. In elderly fatigue, boredom and/or
oversedation are more the rule than the exception. Organic causes are usually
attributed to cachexia, wasting illnesses, anemias, heart disease if
associated with dyspnea, congestive heart failure if associated with decreased
blood pressure, left ventricular failure and ischemic heart disease if
associated with a large failing heart, or severe hypokalemia if associated
with lassitude.
Headache
Headache is a less common complaint during the later years. Nevertheless,
headaches that are severe, periodic, and preoccupying are suspicious of
cranial tumor, especially chronic subdural hematoma. Occipital muscle tension
headaches may be associated with sprains or strains of the neck or cervical
spondylosis. Severe temporal headaches or facial pain in the elderly point to
giant cell arteritis if found with a raised sedimentation rate and disturbed
electrophoretic pattern. Sinus headaches are rare in the elderly.
Hypotension
During the advanced years, a sudden decrease in blood pressure is a sign
of severe circulatory disturbance. This is commonly from gastrointestinal
hemorrhage or a major heart or cardiopulmonary incident. In old age, cardiac
infarction rarely takes the classic form of chest pain. Pulmonary infarction
is first noted by signs of sudden collapse with cyanosis. The major signs of
low blood pressure are limpness, dizziness, and even fainting when arising
from a lying or sitting position. While hypokalemia is often a causative
factor, overuse of antihypertensive drugs should always be a suspicion.
Postural hypotension is noted by the signs of limpness, giddiness,
dizziness, vertigo, and even syncope on arising. These signs are transient
and always related to posture. The disorder appears to be associated with
cerebral vascular disease and especially deficiency in the baroreceptor
reflexes, venous pooling, low serum sodium levels, and an uncompensated
decrease in cardiac output.
Insomnia
Many senior citizens mistakenly believe that age requires additional
sleep. In insomnia, treatment should first look to relieve any pain or
discomfort present. While persistent drowsiness is symptomatic of uremia,
heart failure, and respiratory insufficiency, persistent insomnia may be due
to rheumatic pains, ischemic pains of peripheral vascular disease, nocturnal
micturition, emotional stress, or just lack of adequate exercise to induce
sleep.
Insomnia often has a psychic etiology. Difficulty in falling asleep is
usually attributed to anxiety, while waking early is usually a sign of
depression.
As explained below, the habitual use of drugs to enhance sleep often
presents a clinical problem. However, use of a small alcoholic nightcap is
often an aid to sleep.
Vertigo
Occasional giddiness, dizziness, and vertigo in the elderly appear to be
widespread in the senior population and are often associated with minor
functional alterations. Organic causes of vertigo range from a simple syncopal
tendency, postural hypotension, and wax in the ears to severe progressive
anemia, acute gastrointestinal hemorrhage, carotid sinus syndrome, changes in
cardiac rhythm, episodes of cardiac infarction, minor cerebral vascular
insufficiency including basilar system involvement, middle-ear disease,
acoustic neuroma, acute labyrinthitis, or paroxysmal labyrinthine vertigo
(Meniere's disease). Vertigo and giddiness are often attributed to the overuse
of drugs, especially the salicylates, quinidine, barbiturates, and
antihypertensives.
COMMON DRUGS AND THEIR REACTIVE EFFECTS
Louis Lasagna in "The Diseases Drugs Cause," Perspectives in Biology and
Medicine, published by the University of Chicago Press, states that
antibiotics can trigger unfavorable reactions and thus "produce iatrogenic
complications in one out of five cases." Charles C. Edwards, MD, while HEW
Assistant Secretary for Health, declared that more than half the antibiotics
used in hospitals are not needed, inappropriately chosen, or used in improper
dosages. The result, he said, has been "needless adverse reactions,
unnecessary expense, and, in the long run, a shift in the ecology of hospital
infections toward gram negative infections," which he characterized as "more
dangerous and harder to treat than the gram positive infections that were more
common in the past."
A paper by Henry E. Simmons, MD, MPH, developed while Deputy Assistant
Secretary for Health, HEW, and Paul D. Stolley, MD, of John Hopkins School of
Hygiene and Health, questioned whether the trends and consequences of
antibiotic use in the U.S. constituted medical progress. Presenting data
regarding antibiotic prescriptions in both community practice and the hospital
setting, the authors point to the high frequency in which physicians and
surgeons prescribe antibiotics by telephone without examining the patients,
prescribe antibiotics without having taken a culture, prescribe antibiotics
for viral diseases, and prescribe antibiotics when the efficacy of the alleged
prophylaxis is unproved. According to the conclusion of this paper, the
enormous risks associated with antibiotic use are beginning to outweigh their
benefits.
Dr. Milton Silverman, then a professor of pharmacology at the University
of California, went on record in stating that adverse drug reactions are
needlessly killing tens of thousands of Americans each year, hospitalizing
millions of others, and costing the nation $3.6 billion in medical bills. Even
more outstanding was the 1974 report before a Senate Health Subcommittee by
Robert Talley, a medical physician, and Marc Laventurier, a druggist, both of
the San Joaquin Medical Foundation. Their findings charge that 60,000 to
140,000 Americans are killed each year by the side effects of prescription
drugs.
This is not an indictment against the judicious use of chemotherapy. It
is, simply, an authoritative accounting of facts of its abuse. Patient history
should be careful to include the medical history, especially if signs of skin,
allergic, gastrointestinal, blood, or CNS reactions are manifesting.
Throughout this chapter, there have been many references to disorders
resulting from adverse drug reactions. Because of this, and as authorities
have openly stated that senior citizens are the most overly medicated age
group, it behooves the chiropractic physician to be cognizant of common
toxicities so proper consideration will be made in the diagnosis and prognosis
of those patients also under medical care.
Medical Therapeutic Reactions and Side Effects
Once drugs are absorbed in the body, almost all have multiple actions and
exert some effect on all cells. While safety margins are sought, action
tolerance is often reduced by senescence, disease, or combined factors.
Adverse drug reactions are reported to be at least 50% higher in incidence
in those over age 60 as compared to younger age groups, with toxic effects
noted sooner in the elderly as well as more often. This is attributed to
changes in aging physiology such as a reduction in metabolic turnover, a
slower rate of drug elimination, altered CNS responses, and the variable
effects of aging tissues --as well as direct toxic effects of drugs.
Analgesics and Antirheumatic Drugs
The dependency fault of narcotics and tranquilizers is common knowledge.
Other effects are:
Antibiotics and Influenza Vaccines
Aside from the complications arising from direct drug sensitivity and the
development of resistant bacterial strains, the adverse effects of
antimicrobials can be widespread. Characteristic reactions include hemolytic
anemia, neurologic disturbances, enteritis, encouragement of candidiasis,
steatorrhea, and associated liver and kidney damage. The common side effects
of influenza vaccination are fever and local reactions.
Antiarrhythmics and Hypotensive Drugs
Anticoagulant Drugs
The noxious effects of commonly used anticoagulant drugs are
gastrointestinal upsets, skin reactions (eg, severe hives, various rashes),
cystitis, cyanotic toes, and necrosing cutaneous hemorrhages. Antibiotics,
sulfonamides, salicylates, phenothiazines, alcohol overuse, and other drugs
increase anticoagulant sensitivity. Manipulation, massage, traction, deep
heat, and certain acupuncture techniques are sometimes contraindicated in
patients under anticoagulant therapy.
Anticonvulsants and Antiparkinsonism Drugs
Adverse Digitalis Effects
A much higher incidence of digitalis toxicity is noted in the elderly,
especially in the presence of potassium deficiency, hypothyroidism, renal
insufficiency, anoxic lung disease, and advanced myocardial disorders. While
cardiac arrhythmia is usually the first sign of toxicity, other cardiac,
gastrointestinal, and neurologic manifestations may be witnessed. Anorexia,
blurred vision, amblyopia, scotomata, drowsiness, hallucinations, seizures,
coma, delirium, nervousness, weakness, peripheral neuralgia, trigeminal
neuralgia, paresthesia, recurrent syncope from carotid sinus reflex
sensitivity, various types of cardiac fibrillation and tachycardia,
thrombocytopenic purpura, eosinophilia, and gynecomastia are clinical
manifestations of digitalis reactions.
Cancer Chemotherapy
Serious damage can be inflicted on normal tissues by cytotoxic agents if
not used with utmost discretion.
Side Effects of Diuretics
The adverse effects of diuretics include the precipitation of urinary
retention, urinary incontinence, sodium depletion, hypokalemia, chronic
dilusional hyponatremia, hypochloremic alkalosis, azotemia, hyperuricemia,
hyperglycemia, rashes, vasculitis, yellow vision, intestinal ulcerations,
thrombocytopenia, nausea, diarrhea, drowsiness, confusion, gynecomastia, and
headache --depending on the specific type of diuretic used.
Sedatives and Tranquilizers
Hypersensitivity reactions from sedatives and tranquilizers are seen as
severe rashes, jaundice, and agranulocytosis. Episodes of drowsiness,
hypotension, imbalance, and falling tendencies are not uncommon. Dysphagia,
drooling, parkinsonian rigidity, and mental depression are often associated
with the phenothiazines. Liability to bronchopneumonia, dehydration,
dyskinetic syndromes, and hypothermia are clinical manifestations that are not
rare.
Sedatives suppress paradoxical sleep, and rapid tolerance is developed
resulting in increasing dosages. Withdrawal produces restlessness, nightmares,
emotional disturbances, and reduction in body movements that predispose to bed
sores during confinement.
Tranquilizers, as blocking agents, rarely suppress mental activity as do
sedatives. They affect the autonomics by sympathetic depression and
parasympathetic stimulation. Characteristic is a lowering of blood pressure
with reactions of dizziness, a tendency to fall, and reduced cerebral
circulation that may predispose to cerebral ischemia or infarction.
PROFESSIONAL OBLIGATIONS
The chiropractic profession makes no claim to a panacea, nor does it seek
to encroach on the specialized methods of others. It does claim the exclusive
prerogative to determine the limitations of its own methods and scope of
practice, and it seeks the professional courtesy of cooperation, consultation,
and referral privileges from members of the other healing arts and ancillary
groups.
Chiropractic willingly shoulders its moral, ethical, and legal
responsibilities and therefore is determined to obtain the rights and
privileges that permit a profession to minister adequately and efficiently to
the populace, with dignity, self-respect, and the right to pursue additional
knowledge and contribute to the solution of the problem of disease.
While no single therapy offers a panacea, one may be better suited to a
problem than another, or a combined effort might be advisable. The axioms,
"Primo Non Nocere" (The First Principle Is Do No Harm) and "Salus Aegroti
Supreme Lex" (The Welfare of the Ailing Is the Supreme Law) places an enormous
responsibility on every physician, since he or she must decide what therapy or
therapies are justified for a specific patient. There might be cases in which
the patient's condition may be cared for by the therapeutic competency of one
specific school of healing and other instances where the skill and wisdom of
more disciplines of the healing art are required.
The above quoted principles oblige all physicians to discern according to
their best ability what path of treatment should be followed. It should he
emphasized that the existence of this obligation presents a difficult task
confronting practitioners faithful to the tenets on which their healing
profession rests. Doctors of chiropractic have pledged, as other physicians
have done, complete adherence to those avowed principles.
BIBLIOGRAPHY OF MAJOR REFERENCES
The Practice of Geriatrics.
London, William Heineman, 1963.
Bittner H, et al:
Chiropractic of Today.
ACA Journal of Chiropractic, November
1973.
Brodie BB, Shore PA:
Annals of the New York Academy of Science, 66:631, 1957.
Cotes JE:
Lung Function.
Philadelphia, F. A. Davis, 1965.
Cowdry EV, Steinberg FU (eds):
The Care of the Geriatric Patient.
St. Louis.
C. V. Mosby, 1971.
Exton-Smith AN, Woodford-Williams E (eds):
Proceedings of the Third Meeting of
the European Clinical Section of the International Association of Gerontology.
Basel, Karher, 1962.
Fischer FP:
Senescence of the Eye.
Modern Trends in Ophthalmology. New York,
Hoeber, 1947.
Haldeman S:
Interactions Between the Somatic and Visceral Nervous System.
ACA
Journal of Chiropractic, August 1971.
Hanoka JP:
Chronic Obstructive Lung Disease.
ACA Journal of Chiropractic,
December 1969.
Harring HC:
Arthritis.
ACA Journal of Chiropractic, February 1966.
Martin RJ:
Autonomic Nerve Control and Neurovascular Dynamics.
ACA Journal
of Chiropractic, October 1969.
Mercer W, Dothie RB:
Orthopedic Surgery.
Baltimore, Williams & Wilkins, 1964.
Nelson WA:
Function vs Structure.
ACA Journal of Chiropractic, February 1970.
Nordin BEC:
Osteomalacia, Osteoporosis, and Calcium Deficiency.
Clinical
Orthopedics, 17:235, 1960.
Palmateer DC, Hollen WV:
Urinary Tract Calculi Diagnosis and Treatment.
ACA
Journal of Chiropractic, April 1971.
Palmer ED:
Clinical Gastroenterology.
New York, Hoeber, 1963.
Paprocki CC:
Gastrointestinal Disorders.
ACA Journal of Chiropractic, August
1969.
Rossman I (ed).
Clinical Geriatrics.
Philadelphia, J. B. Lippincott, 1971.
Sataloff J:
Hearing Loss.
Philadelphia, J. B. Lippincott, 1966.
Schafer RC:
Basic Principles of Chiropractic: The Neuroscience Foundation of
Clinical Practice.
Arlington, VA, American Chiropractic Association, 1990.
Schafer RC:
Chiropractic Health Care, ed 3.
Des Moines, Iowa, The Foundation
for Chiropractic Education and Research, 1978.
Schafer RC:
Chiropractic Physical and Spinal Diagnosis.
Oklahoma City,
Associated Chiropractic Academic Press, 1980.
Schafer RC:
Clinical Biomechanics: Musculoskeletal Actions and Reactions, ed
2.
Baltimore, Williams & Wilkins, 1987.
Schafer RC:
Physical Diagnosis: Procedures and Methodology in Chiropractic
Practice.
Arlington, VA, American Chiropractic Association, 1988.
Schafer RC:
Symptomatology and Differential Diagnosis: Conspectus of Clinical
Semeiographies.
Arlington, VA, American Chiropractic Association, 1986.
Shelby RL:
Chiropractic Management of Degenerative Joint Disease of the Spine.
ACA Journal of Chiropractic, December 1970.
Shock NW:
Physiological Aspects of Aging.
Journal of the American Geriatrics
Society, 15:995, 1967.
Sikes AC:
Management of the Rheumatoid Patient.
ACA Journal of Chiropractic,
March 1966.
Skully RL:
The Nervous System and Its Disorders.
ACA Journal of Chiropractic,
February 1972.
Smith AR:
An Anatomic and Physiologic Basis for Chiropractic.
ACA Journal of
Chiropractic, October 1973.
Trueta J:
Studies of the Development and Decay of the Human Frame.
Philadelphia, W. B. Saunders, 1968.
Turek SL:
Orthopaedics: Principles and Their Application.
Philadelphia, J. B.
Lippincott, 1967.