

|
Bruises Effects of Chronic Pronation Strains Ankle Instability Sprains Subluxations Fractures and Dislocations Roentgenologic Considerations Gait Clues Selected Disorders of the Ankle Injuries of the Foot Postural Foot Alterations Bruises and Wounds The Heel Plantar Strain and Fascitis Anterior Compartment Syndrome Sprains Metatarsalgia Subluxations Stress Fractures and Cysts of the Foot Circulatory Disturbances Injuries of the Toes Gait Clues Restrictions Toe Sprains Selected DisordersChapter 27
Leg, Ankle, and Foot Injuries
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Chiropractic Management of Sports and Recreational Injuries”
Second Edition ~ Wiliams & Wilkins
The following materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated
to chiropractic research. Please review the complete list of available books.
Injuries of the Leg Bruises and Contusions Strains Achilles Tendon Lesions Fractures and Dislocations Circulatory Disturbances Circulatory Tests Miscellaneous Pathologic Signs and Reflexes Injuries of the Ankle
Chapter 27: Leg, Ankle, and Foot Injuries
The most common injuries in this area are bruises, muscle strains, tendon lesions, postural stress, anterior and posterior compression syndromes, and tibia and fibula fractures. Bruises of the lower leg are less frequent than those of the thigh or knee, but the incidence of intrinsic strain, sprain, and stress fractures are much greater.
The lower leg, ankle, and foot work as a functional unit. Total body weight above is transmitted to the leg, ankle hinge, and foot in the upright position, and this force is greatly multiplied in locomotion. Thus the ankle and foot are uniquely affected by trauma and static deformities infrequently seen in other areas of the body.
Injuries of the Leg
A continual program of running and jogging is typical of most sports. The result is often strengthening of the antigravity muscles at the expense of the gravity muscles --producing a dynamic imbalance unless both gravity and antigravity muscles are developed simultaneously. An anatomic or physiologic short leg as little as an eighth of an inch can affect a stride and produce an overstrain in long-distance track events.
Various neurologic, orthopedic, and peripheral vascular signs and tests relative to the leg are listed in Table 27.1.
Table 27.1. Review of Neurologic, Orthopedic, and Peripheral Vascular Manuevers, Reflexes, Signs, or Tests Relative to the Leg
Buerger's test Muscle strength grading
Claudication test Neri's leg sign
Duchenne's sign Patella reflex
Heel walk test Perthe's test
Homan's sign Pratt's test
Hueter's sign Repetitive heel raise test
Light touch/pain tests Strumpell's tibialis sign
Lust's sign Toe walk test
Moskowicz's test Trendelenburg's vein test
Bruises and Contusions
The most common bruise of the lower extremity is that of the shin where disability may be great as the poorly protected tibial periosteum is usually involved. Skin splits in this area can be most difficult to heal. Signs of suppuration indicate referral to guard against periostitis and osteomyelitis.
Management. Treat as any skin-bone bruise with cold packs and antibacterial procedures, and shield the area with padding during competitive activity. When long socks are worn, the incidence of shinbone injuries is reduced. An old but effective protective method in professional football that does not add weight is to place four or five sheets of slick magazine pages around the shin that are secured by a cotton sock which is covered by the conventional sock. A blow to the shin is reduced to about a third of its force as the paper slips laterally on impact.
GASTROCNEMIUS CONTUSION
This is a common and most debilitating injury in contact sports. It is characterized by severe calf tenderness, abnormal muscle firmness of the engorged muscle, and inability to raise the heel during weight bearing.
Management. Treat with cold packs, compression, and elevation for 24 hr. Follow with mild heat and contrast baths. Massage is contraindicated as it might disturb muscle repair. The danger of ossification is less in the calf than in the thigh, but management must incorporate precautions against adhesions.
TRAUMATIC PHLEBITIS
Contusion to the greater saphenous vein may lead to rupture resulting in extensive swelling, ecchymosis, redness and other signs of local phlebitis. Tenderness will be found along the course of the vascular channel. During treatment, referral should be made upon the first signs of thrombosis.
Management. Management is by rest, cold, compression, and elevation for at least 24 hr. Later, progressive ambulation, mild heat, and contrast baths should be utilized. Progressive exercises may begin in 4-6 days. When competitive activity is resumed, the area should be provided extra protection.
NERVE CONTUSIONS
Nerve trauma exhibits palsy, paresthesia, or anesthesia. These signs commonly result from a kick in sports. Trauma behind the knee to the external popliteal nerve features inability to extend the foot. Trauma to the peroneal nerve along the lateral aspect of the lower third of the leg may result in a palsy characterized by inability to flex the foot (foot drop). Peroneal symptoms are sometimes associated with asymptomatic loose tibiofibular ligaments. The excessive mobile fibula head, with demonstrated false motion, often "clicks" during gait and tends to irritate the peroneal nerve as it winds around the fibula neck.
Management. Treat as any nerve contusion with emphasis on ice massage or cold packs, followed later by deep massage, contrast baths, and graduated exercises. Heel lifts are helpful in relieving tension on the injured nerve. A loose tibiofibular head can be aided by a sponge pad placed over the area and secured by an elastic bandage. Any case exhibiting a degree of atrophy or sensation loss over a few days deserves neurologic consultation.
Strains
With the increased interest in jogging, musculoskeletal injury is common but usually minor. During middle age, the most common injury is calf-muscle strain, but knee, ankle, and foot sprain, and shin splints do occur frequently. Occassionally, stress fractures will be associated.
A tear of the musculotendinous junction of the medial belly of the gastrocnemius often occurs in tennis, skiing, squash, and track. At the site of tenderness, a palpable gap in the muscle is usually found. It is identified in a radiographic lateral view as an indentation of the soft-tissue margins.
GENERAL MANAGEMENT
Heat is helpful to relieve muscle spasm, but cold and vapocoolant sprays have shown to be as effective. Mild passive stretch is an excellent method of reducing spasm in the long muscles. For example, standing on an incline (eg, Flex Wedge) relaxes a spasm through passive stretching. Heavy passive stretch destroys the beneficial reflexes.
Fatigue may increase contractures and produce pain. Spasms are treated by
(1) warming the muscle with limbering movements;
(2) stretching the muscle by resistance to the tightened muscle and its antagonist;
(3) active stretching in an attempt to fulfill the possible entire range of motion; and then by
(4) passive stretching to fulfill the possible range of motion. The stretching force must be a careful balance between that of easy performance and that of excessive misuse.
Other methods may prove helpful. Peripheral inhibitory afferent impulses can be generated to partially close the presynaptic gate by acupressure, acupuncture, or transcutaneous nerve stimulation. Isotonic exercises benefit by improving circulation and inducing the stretch reflex when done supine to reduce exteroceptive influences on the central nervous system. An acid-base imbalance from muscle hypoxia oe acidosis may be prevented by supplemental alkalinization.
MUSCLE REHABILITATION
Physiologic elasticity, the ability of a muscle to release tension, is highly important for normal movement. A tired muscle loses some of this ability to relax, thus effecting its elasticity and endurance capacity. A muscle with good endurance readily assumes its maximum length after repeated prolonged contractions, but a tired muscle does not return to its maximum length.
When mechanical elasticity is impaired, muscle tissue does not yield to passive stretch. After injury, this "Contracture Tiegel" is frequently the effect of spasm or prolonged immobilization, or both. For this reason, it is highly necessary in athletics to conduct goniometry in the weight-bearing position. For example, an ankle or knee may record a full range of motion while supine but be severely restricted in the squatting or kneeling position due to residual muscle shortening without actual fibrous contracture.
In most sports, a player should not be allowed to return to competition until the injured muscle becomes as strong as its uninjured contralateral mate. Strength-building exercises should be given just below the fatigue level, keeping in mind that injured muscles fatigue rapidly.
SHIN SPLINTS
This syndrome is one of lower leg pain and discomfort after running or walking overstress that is associated with an aseptic inflammation of the injured muscle-?tendon unit. An excessive overstride during running is a typical cause of such irritation. It is a common complaint during early season practice sessions or when the running surface is changed. Keep in mind that the anterior shin muscles warm slowly and cool rapidly because they are squeezed tightly between bone and skin and by fascia. The blood supply of the interosseus membrane is quite limited.
Signs and Symptoms. The term "shin splints" is a catch-all phrase for any discomfort in the anterior leg on exercise. The common cause may be better classified as tibialis anterior or posterior syndrome, tendoperiostosis, or stress fracture. Differentiation is made by mode of onset, site of tenderness, and late roentgenography. A poorly responding case of shin splints with pain even on rest suggests a compartment syndrome. Tenderness is most common over the posterior tibialis muscle, but it is frequently found at the attachment of the anterior tibial muscle to the lateral border of the tibia. The pain is usually throbbing, deep-seated, relieved with rest, but increased at night.
Roentgenographic Considerations. Cortical thickening of the medial tibia or a minimal periosteal reaction is the roentgenographic counterpart of shin splints, the result of muscle/fascial attachments of the anterior mid or lower leg being torn or stretched. In uncomplicated cases, no evidence may be visible except for slight cortical thickening. The possibility of a stress fracture must always be eliminated.
Management. Once the actual cause has been found, which may be as high as the lower back or as low as the foot, treat as a severe strain with accompanying subluxations. After the acute stage, emphasis is on structural alignment, deep heat, analgesic pack, passive massage, heel pad, and good strapping support. The taping should continue for a month after full activity is resumed. Modalities offer unencouraging benefit. An anatomic short leg is often involved that requires a permanent heel lift slightly under actual need.
Some misguided high school coaches recommend that shin splints be "run out". This invariably leads to the development of scar tissue or new bone formation. However, Dayton of Yale feels that most cases will show a history of running "duck footed" with the feet everted and externally rotated, thus stressing the plantar flexors. If this is the case, tenderness and slight swelling will appear at the posteromedial crest where the tibial attachments of the soleus and flexor digitorum longus are located. Dayton feels that strapping the foot in slight inversion and initiating a program of graduated trotting "pigeon toed" is the best regimen to alter the predisposing habit.
Quite frequently, a weak longitudinal arch is involved. A 2 x 2-inch pad of 1/4-inch gauze can be secured on the plantar surface of the foot to cover the arch and the anterior third of the heel. Heavy patients may require a double pad. Good support requires taping high up the lateral and medial leg which is applied with considerable force. Nonyielding tape should never be used. However, the more modern and simpler method is to place a 2 x 6-inch piece of 1/2-inch-thick foam rubber over the shin and secure it with an elastic bandage.
Strapping Procedure. Christensen describes shin splint taping as follows: Place an anchor strip of 1|-inch tape around the ball of the foot. Start the second strip at the point of the anchor strip closest to the great toe. Continue up at a sharp angle, cross the center of the longitudinal arch, encircle the heel, and then descend along the side of the foot to the starting point. The second strip starts by the small toe. Bring the tape across the longitudinal arch, around the heel, and down the side of the foot to the starting point. Overlap each strip three times. Anchor around the ball of the foot, and place anchors over the cross of the strapping for added support if necessary.
TIBIALIS ANTERIOR SYNDROME
The anterior tibial syndrome is a disabling form of muscle stiffness where intramuscular tension (engorgement) is exaggerated by the unyielding surrounding tissues to a degree that local infarction may occur leading to local massive necrosis or Volkmann's contracture.
Background. Alternately raised muscle fiber tension so alters the muscle's internal frictional resistance that rapid movements are impossible and muscle tearing develops if the whole muscle doesn't go into spasm. The engorged muscle becomes trapped within its fascial compartment and tends to strip from its bony attachments. Circulation of the anterior tibial artery becomes impaired. Most authorities do not attribute any part of the disorder with a local accumulation of lactic acid. On rare occasions, prolonged heavy training or overuse may produce muscle hypertrophy of the lower fibers of the tibialis anterior which causes blocking of the upper extensor retinaculum of the ankle. This "spaceoccupying" lesion effect produces local symptoms. A blow to the lower leg will have the same result.
Signs and Symptoms. The syndrome features gradually increasing anterolateral leg pain increased on activity, swelling, and restricted motion. Keep in mind, however, that all muscles swell after exercise, and this is particularly true of unconditioned muscles. During the acute stage, and unlike other shin splints, rest offers little relief. Flat feet, tight calves producing plantar flexion, and imbalance between the anterior and posterior muscle groups are commonly associated. That is, the anterior leg muscles are often weaker than the posterior group and this produces a dynamic imbalance which requires special consideration in rehabilitation.
Management. Prevention through properly graduated conditioning and interval training is the best therapy. Of the various possible therapies, massage, elevation, and deep heat are the most effective, but no regimen has proved ideal. If conservative measures are unsuccessful, surgical decompression should be considered.
POSTERIOR TIBIAL COMPARTMENT SYNDROME
The cause is similar to that of the anterior tibial compartment syndrome or a crushing injury. Pain, entrapped swelling, and numbness are often severe. The engorged muscle becomes trapped within its fascial compartment and tends to strip from its bony attachments. Signs of tendinitis behind the medial malleolus, deep calf myositis, tenderness in the posteromedial angle of the tibia, pain on use, and foot pronation are commonly associated. A difficult complication is widespread tendoperiostitis which terminates in severe scars and adhesions. Surgical decompression is often required.
PERIOSTITIS
Tibial Periostitis. Anterior tibial periostitis is a frequent complication which results from traumatic microelevation of the periosteum by fascial overstress. Severe pain localized at the medial tibial border occurs during activity. A small tender area may be palpable. Conservative measures rarely are helpful other than referral for local anesthesia and steriods.
Fibula Periostitis. Fibula periostitis is a frequent complication of blows to the lateral leg, especially at the lower third of the bone. There is persistent soreness aggravated by activity, shaft tenderness, and shaft thickening demonstrated by roentgenography. Crepitus may or not be present. Management should include 1-2 weeks of rest followed by graduated active exercise.
POPLITEUS TENDON RUPTURE
A player makes a jump, lands, feels a "pop" in the calf, a sudden sharp pain develops, and incapacity overtakes the player. This is the typical picture of popliteus tendon rupture which is often confused with meniscal injury, phlebitis, and Achilles rupture or tendinitis. It occurs most often in the middleaged athlete (eg, basketball, tennis).
Management. Ice, compression, elevation, and rest are the treatment of choice during the early stage, followed by appropriate physiotherapeutic measures. A careful check should be made for associated lower spine, pelvic, hip, or lower extremity subluxations or fixations.
PLANTARIS RUPTURE (TENNIS LEG)
Although termed "tennis leg" because of its association with overhead forehand overstress, the disorder is also frequent to football "button-hook" pass receivers and to basketball players during rebound play. It is sometimes confused with soleus or gastrocnemius strain in that its function is to assist these two muscles. In actual plantaris strain, which is rare, there is pain with an explosive onset, tenderness, and an area of indurated tissues located deep at midcalf and lateral to this site when the palm palpates from the popliteal space to the heel. The pain is increased by dorsiflexing the foot against resistance. Bleeding and a deep thrombophlebitis is often associated. Signs of ecchymosis on each side of the Achilles tendon often appear in a few days. Quite frequently, an Achilles sprain and separation of calf fascia are associated.
Management. General strain therapy should include initial cold packs and compression for at least 36 hr. An analgesic pack of menthyl salicylate (buttered and covered under the strapping), deep heat, heel pads, cane support while walking, progressive passive stretching, and whirlpool or shower hydrotherapy at 108*F are helpful. There is always a danger of tendinitis ossificans. Full activity is rarely assumed before 3-4 weeks. When competitive activity is resumed, it should be preceded by deep massage and stretching exercises for 3-5 months after injury. Recurrent symptoms can often be traced to a degree of myositis ossificans.
GASTROCNEMIUS STRAIN
Strain of the gastrocnemius is the most common strain of the leg in sports and often misdiagnosed as a ruptured plantaris tendon. The onset of symptoms is usually immediate calf cramping, generalized calf spasm, and extreme tenderness at the site of strain. Strain nearer the Achilles tendon is often attributed to running on the balls of the feet. Occasionally, strain occurs at the gastrocnemius heads and is confused with knee injury after a snapping overextension. If this is the case, tenderness will be found deep in the popliteal fossa when the flexed knee is palpated.
Repetitive Heel Raise Test. The standing patient is asked to raise the heels (ie, toe stand) repetitively several times. If this induces ankle pain, insta- bility, a posterior compartment syndrome, or a subluxation complex should be suspected. If this exercise is unable to be performed because of weakness and pain is ankle absent, a gastrocneiumius weakness or neurologic deficit should be suspected.
Management. Treat as any severe strain, but be forewarned that rehabilitation is difficult. Heat enhances relaxation but increases swelling and pain. Cold reduces swelling but increases cramping. Thus, structural normalization, rest, muscle techniques, acupressure, and a most gradual program of locomotion are the best therapy.
SOLEUS STRAIN
Strain of the soleus independent of the gastrocnemius is rare, but it does occur in sports. It is characterized by a palpably tight and tender soleus but relaxed and nontender gastrocnemius. It is usually a mid-season disability.
Management. As with gastrocnemius strain, management is often frustrating. Rest, structural correction, muscle techniques, acupressure, and a slowly graduated program of dorsiflexion and stretching exercises are the best therapy. It often takes 2 weeks before full competitive strength returns.
PLANTAR FLEXION RESTRICTIONS
Limitation of the gastrocnemius or soleus muscle restricting ankle dorsiflexion can be differentiated by the ankle dorsiflexion test. Have the patient sit on the examining table with the knees flexed and relaxed. Grasp the foot and flex the knee to slacken the gastrocnemius, then dorsiflex the ankle. If this can be achieved, the gastrocnemius is the cause of the restriction. If the soleus is at fault, it will not be affected by knee flexion; ie, it will be the same in either knee flexion or extension.
FASCIAL TEARS
While fascia tears can occur most anywhere, they are most often seen in the leg following blunt trauma near the tibial crests. Bleeding is more persistent than in typical contusions. After swelling reduces, palpation will reveal the muscle herniating through the fascial defect.
Management. Symptoms are usually present only during activity where the muscle swells and causes impingement at the hole. This can simply be prevented by an overlaid sponge pad secured by an elastic bandage. While the method may be crude, it is often the choice of the patient over that of surgery which requires a second donor-site incision.
Achilles Tendon Lesions
The tendon of Achilles inserts into the calcaneus and is formed by the common tendon of the gastrocnemius and soleus muscles. It can be readily palpated in the lower third of the calf. Signs of tenderness, swelling, tenosynovitis, or crepitation should ne noted. Rupture or tear results in lack of push-off during gait.
Skiers and runners have a high incidence of Achilles tendon injury. In runners, Achilles tendon pain is frequently associated with plantar fascitis, leg or ankle tendinitis, paritendinitis, tendon rupture, or local inflammation. Also frequently associated but overlooked are stress fractures of the 2nd metatarsal and fibula. Other sites of related fatigue fractures include the calcaneus, tarsal navicular, tibia, and femur.
RUPTURES
Due to the great tensile strength of the normal Achilles tendon, femoral or calcaneus fractures invariably occur before the tendon ruptures. However, this may not be true when excessive force is applied to a previously injured or diseased tendon. The cause is usually traced to overuse, direct violence during stretch, or a poorly placed injection.
Incidence. The incidence of intrinsic stress injuries is high in middleand long-distance runners. Complete rupture is exceedingly rare in players under the age of 40 years. Both complete and partial ruptures are most often seen in middle-aged athletes.
Signs and Symptoms. Rupture may be present even if the player can extend the foot against resistance. A gap or area of extreme tenderness in the Achilles is greater evidence. The site of tear is invariably about 2 inches above its attachment at the heel. Care must be taken to differentiate rupture from partial tear:(1) Rupture is characterized by sharp pain, often accompanied by perception of an abrupt "thud" at the site. The sharp pain soon subsides, but ankle weakness produces a flat-footed gait. Plantar flexion is usually but not always impossible, and passive dorsiflexion is restricted. The onset is always sudden, a tendon deficit is usually palpable, and Thompson's test is positive. The calf muscles retract to a higher position than normal.
(2) Partial tear, less common than rupture, is characterized by acute pain during activity which persists until stress can be avoided. When activity is resumed, severe pain returns. A tender swelling is inevitably noted when the site is palpated. The onset of symptoms is usually sudden. The soleus and gastrocnemius test weak during weight bearing. Thompson's test may be positive or negative. Tenderness is often more severe than that in complete rupture.Roentgenographic Considerations. The lateral x-ray view of the normal ankle shows a lucent triangle of fatty tissue bounded below by the calcaneus, posteriorly by the smooth margins of the Achilles, and anteriorly by the posterior tibial muscles. Upon tendon rupture, the smooth margin of the tendon becomes altered at the site of rupture as edema and hemorrhage occur within the tendon and the fatty triangle. Signs of fluid filling the triangle appear.
Thompson's Test. To detect a rupture of the Achilles tendon, place the patient in the prone position or have him kneel on a chair with his feet extended over the edge. Squeeze the middle third of the calf. If the Achilles tendon is ruptured, especially the soleus portion, the squeeze will not cause the normal plantar flexion response.
Simmond's Test. With the patient prone, the knee is flexed to a 90* angle and the foot is plantar flexed and then relaxed. The examiner grasps the upper calf strongly and squeezes the muscles against the tibia and fibula. A slight loss in plantar flexion is seen when the Achilles tendon is ruptured.
Achilles Tap Test. With the patient prone, flex the knee to a right angle and tap, with a reflex hammer, the Achilles tendon about 1 inch above its insertion into the calcaneus. If pain is induced or the normal plantar flexion reflex of the foot is absent, a rupture of the Achilles tendon should be suspected.
Management. Surgery presents the risk of complications but usually leads to a quicker return to activity (within 3-4 months) than conservative measures. An extensive postoperative rehabilitation program is necessary after casting. Also, tendinitis with healing and repair might precede an episode of complete rupture requiring prolonged casting or surgical repair. In cases of only a few torn fibers, complete immobilization is contraindicated.
OSSIFICATION
In partial tendon tears, ossification may be found in the patellar tendon during roentgenography following hemorrhage. If joint dislocation has occurred, signs of ossification may be found in the soft tissues. After blunt trauma, the soft tissues may show evidence of heterotopic bone formation. Such ossification involves not only the muscle tissue but also occurs within the fascial planes. The typical picture is one of trauma, muscle pain and soreness, and hemorrhage into the soft tissues, with poorly defined ossification developing in 2-5 weeks.
FOCAL STRESS DEGENERATION
A common site of central-tendon degeneration is at the midpoint between the musculotendinous junction and insertion of the Achilles tendon: the site of poorest blood supply in the tendon. Ischemia appears to be the triggering mechanism. Low-heeled shoes, heel-strike running events, training on hard surfaces, and severe training schedules are causative factors.
Signs and Symptoms. During the early stages, pain is only felt during early warmup and disappears with activity. Later, pain becomes persistent and increases in severity. The onset is gradual. Swelling is characteristic, and tenderness is severe. Somewhere in the range of motion, a painful point in the arc is manifested. Thompson's test is negative.
Management. Of the conservative measures, rest, ultrasound, and heel padding offer temporary relief, but activity causes relapse. Injections are dangerous. Surgical procedures appear to be the best alternative, and most players are able to return to competitive activity in several weeks.
TENDINITIS
Achilles tendinitis is a frequent finding in basketball. The onset of Achillodynia in tendinitis is insidious, and there is severe swelling, tenderness, crepitus, and disability. Thompson's test is negative. The cause can sometimes be traced to tape applied too tightly over the tendon.
Taping Procedures. Proper strapping can be described in three steps:
(1) Two anchors of 3-inch-wide tape are applied; one encirles the instep at the center of the longitudinal arch, the other encircles the leg above the malleoli.
(2) Three or fours strips are applied from the arch anchor, over the heel, and to the calf anchor.
(3) The tape is anchored by a continuous figure-8 and heel lock, also of 3-inch-wide tape.Management. Conservative management is extremely long and frequently disappointing, thus surgical decompression is considered the treatment of choice if relief does not occur within 5 days. Some relief is obtained by rest and heel lifts. Postoperative disability rarely exceeds 6 weeks.
PERITENDINITIS
In acute peritendinitis, the onset is rapid, there is swelling, little tenderness, crepitus may or may not be present, and Thompson's test is negative. Chronic peritendinitis presents a gradual onset, swelling may or may not be present, a thickened nontender paratendon is palpable, and Thompson's test is negative.
Management. Conservative management is usually successful unless there are associated fibrosis and strictures of the paratendon. Postoperative disability is about a month.
TENOSYNOVITIS
Tenosynovitis of the Achilles' tendon often produces pain in the tendon area which is increased by use and sometimes associated with palpable crepitus. Other symptoms include pain on motion, tenderness, and a distinct limp. Treat as any inflammatory tendon reaction with emphasis on hydrotherapy and ultrasound.
DRY SHEATH
This disorder of unknown cause is the result of diminished lubricating fluid within the sheath of the Achilles tendon. Adhesions form binding the tendon to its sheath. Symptoms include a burning pain during and after strenuous activity, inability to raise the heel from the ground during weight bearing, tenderness, mild swelling, and restricted ankle motion. Crepitus is often present.
Taping Procedure. Proper strapping begins in partial extension with a vertical strip from the heel up the calf to just below the knee. The second strap is applied on the medial heel, crosses the tendon, and is attached to the lateral calf just below the knee. The third strip is secured on the lateral heel, crosses the Achilles, and is attached to the medial calf just below the knee. These strips are secured by semicircular horizontal strips of overlapping 2-inch tape from the ankle to the upper calf. Bilateral heel lifts should be provided to accommodate for the fixed partial extension.
Management. During the acute stage, immobilization may be necessary. Contrast or whirpool baths (108*-110*F) at least twice daily, analgesic packs, strapping, and vitamin-mineral supplementation are helpful. Bilateral heel pads should be provided to reduce the strain on the tendons. Rehabilitation to full activity usually requires about 2 weeks.
Fractures and Dislocations
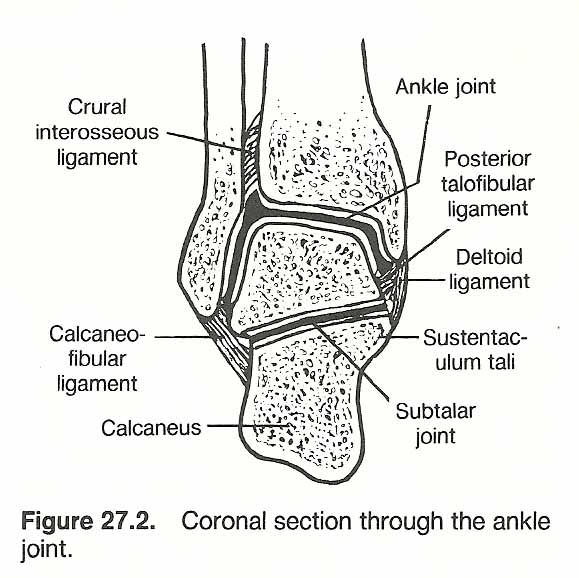
Displacement of lower tibia or fibula fracture is usually posteromedial due to the strong action of the gastrocnemius and soleus. Care must be taken not to mistake an incomplete fracture of the distal-medial tibia (Pott's fracture) for a severely inversion-sprained ankle. See Fidure 27.2
Hueter's Fracture Sign. Being relatively dense, bone readily trasmitts sound waves. Thus, if a fracture of a long bone is suspected (eg, the tibia), the examiner can use a stethoscope to auscultate 2-3 inches proximal to the suspected site while the skin over the bone is tapped with a percussion hammer or a supported index finger 2-3 inches distal to the suspected site. If the percussion sounds are not transmitted in the involved bone, but are in the contralateral limb, a fracture line inhibiting the flow of the vibration is indicated. A variant of this test is to use a 512-c tuning fork rather than percussion. In addition, either procedure can be used effectively to judge the state of healing of a fractured long bone when roentgenography is not available or ill-advised.
 |
LOWER TIBIA FRACTURES
Inasmuch as the tibial epiphysis does not ossify until the early twenties, eiphyseeal fractures are not uncommon in adolescent contact sports. Fatigue stress fractures are characterized by a dull gnawing pain following a run which increases in severity with time and weight bearing.
LOWER FIBULA FRACTURES
Most fibula injuries occur at its distal portion. Minor fractures are often missed as the symptomatic picture often resembles a bruise or mild sprain. As the fibula does not carry direct body weight, a player may continue activity long after fracture has occurred and complicate the original injury. Uncomplicated fractures rarely require more than support followed by progressive exercise unless the medial ligaments of the ankle or tibiofibular supports are ruptured.
STRESS FRACTURES
With repeated, forceful contractions of leg muscles, lower leg stress fractures are sometimes seen as the result of tibia or fibula "wobble". These are commonly related to track and field injuries and can occur whenever a force exceeds the bone's structural strength. Humans are not the only ones affected by this disorder; greyhounds and racing horses also show frequent stress fractures within the limbs.
Signs and Symptoms. Progressive pain during physical activity is the typical symptom. An early sign is that of a linear periosteal reaction which rarely exceeds 1 cm and may present a local bony tenderness. However, bony tenderness is not common. In time, resorption of the fracture margin produces a lucent linear defect on roentgenography. Soft-tissue views and bone scanning are frequently necessary to determine a stress fracture.
Note: The clinical term stress fracture is a misnomer that is common in use. The term fatigue fracture is more accurate biomechanically as all frac=- tures are the result of overstress.
Fatigue fractures of the legs are most always horizontal but occasionally are seen as longitudinal. The first roentgenographic signs are(1) a minute radiolucent tunneling of the cortex as a result of osteoclastic resorption, followed by cortical resorption in a fracture line of one cortex, and
(2) a localized haze on the bone surface representing callus or periosteal new bone development. Within the endosteal bony surface, a line of condensation may be seen. Later, an abundant callus may be confused with a neoplasm.Management. Most stress fractures do not require splinting or casting unless extensive or if the patient is unreliable in providing the necessary rest of the part.
Circulatory Disturbances
INTERMITTENT CLAUDICATION
Intermittent claudication and cramps from insufficient circulation through the arteries of the legs may give rise to a sudden "giving way" of one or both legs during running or walking. Power returns after a short rest. In patients at rest, the frequent recurrence of painful cramps may be the only manifestation of the disorder. In other cases, there are various forms of paresthesia such as numbness, prickling, and "hot feet" at night. True claudication, however, is rare in sports. Obliteration of the dorsalis pedis (or larger arteries) by arteriosclerosis is sometimes found in the older patient, but there is reason to believe that local anemia due to vasomotor disturbance or other causes may produce similar cramps such as those seen in athletes after a hard run and in pregnancy. Rarely is Buerger's or Raynauld's disease found.
VARICOSE VEINS
Varicose veins, with their eczema and ulcers, are the most common lesions of the lower leg. The soft, twisted, purplish eminences are easily recognized. Hardness in such a vein usually means thrombosis. Chronic ulcers of the lower leg, especially those in front, are usually due to varicose veins and the resulting malnutrition of the tissues. They leave a brown scar after healing.
Saphenous Tests. Palpate the greater saphenous vein close to the groin where it joins the femoral vein. Have the patient cough, and a transmitted pulse will be felt if the major valve at this junction is incompetent. Then place your fingers over the largest mass of varicosities on the leg and tap the upper greater saphenous with the fingers of the other hand. Incompetent valves will be indicated if again an impulse is transmitted downward.
EDEMA
Lymphatic obstruction, venous disease, or acute arterial occlusion may result in ankle edema. Venous disease is the most common cause of pitting on pressure. Trauma or local disease is the usual cause for unilateral swelling. Unilateral edema may be due to thrombosis of a vein, pressure of tumors in the pelvis, or to inflammation. Bilateral edema of the legs is most often due to uncompensated heart lesions (primary or secondary from lung disease), lymphatic disorders, nephritis, cirrhotic liver, anemia, neuritis, varicose veins, obesity, flatfoot, and other causes of deficient local circulation. In some cases, no cause can be found (angioneurotic, essential, hereditary types). Diagnosis depends on the history and the examination of the rest of the body. Edema is usually greatest in the front of the leg and in the back of the thigh. Tenderness in the lower legs frequently accompanies edema from any cause. It may also be due to neuritis, trichiniasis, or any local inflammation.
Circulatory Tests
Low back pain is one of the most common complaints to be heard in a chiropractic office. Because of this, Whiele points out the importance of recognizing associated problems of neurovascular stenosis in the large arteries of the leg due to L4-L5 irritation and differentiating them from other factors that can produce circulatory insufficiency. For example, thrombosis of the femoral artery can produce the same symptomatic picture as sciatic neuritis. Thus, diagnostic procedures might include, when indicated, plethysmography, unilateral/vertical and bilateral/horizontal blood pressure comparisons, Doppler ultrasound readings, and reactive hyperemia tests in addition to the clinical tests are described below.
Homan's Sign. The patient is placed supine with the knees extended in a relaxed position. The examiner, facing the patient from the involved side, raises the involved leg, sharply dorsiflexes the ankle with one hand and firmly squeezes the calf with the other hand. If this induces a deep-seated pain in the calf, a strong indication of thrombophlebitis is present. Buerger's Test. The patient is placed supine with the knees extended in a relaxed position, and the examiner lifts a leg with the knee extended so that the lower limb is flexed on the hip to about a 45* angle. The patient is then instructed to move the ankle up and down (dorsiflex and plantar flex the foot) for a minimum of 2 minutes. The limb is then lowered, the patient is asked to sit up, the legs are allowed to hang down loosely over the edge of the table, and the color of the exercised foot is noted. Positive signs of arterial insufficiency are found if
(1) the skin of the foot blanches and the superficial veins collapse when the leg is in the raised position and/or
(2) it takes more than 1 minute for the veins of the foot to fill and for the foot to turn a reddish cyanotic color when the limb is lowered.Claudication Test. If claudication is suspected, the patient is instructed to walk on a treadmill at a rate of 120 steps/min. If cramping, and sometimes a skin color change, occurs, the approximate level of the local lesion can be identified. The time span between the beginning of the test and the occurrence of symptoms is used to record the "claudication time," which is usually recorded in seconds.
Perthe's Tourniquet Test. This is an excellent test to use in differentia- ting the extent of superficial and deep lower limb varicosities. An elastic bandage is applied to the upper thigh of a standing patient sufficient to compress the long sephenous vein, and the patient is instructed to walk briskly around the room for approximately 2 minutes. The varicosities are then examined. This exercise with the thigh under pressure should cause the blood in the superficial (long saphenous) system to empty into the deep system via the communicating veins. Thus:1. If the varicosities increase in their distention (become more prominent) and possibly become painful, it is an indication that the deep veins are ob- structed and the valves of the communicating veins are incompetent.
2. If the superficial varicosities remain unchanged, the valves of both the long saphenous and communicating veins are incompetent.
3. If the superficial varicosities disappear, the valves of the long saphenous and the communicating veins are normal.Pratt's Tourniquet Test. This variation of Perthe's test is used to evaluate the integrity of specific communicating veins. The patient is placed in the supine position with the knees extended position. The limb is raised to about 45* to empty the veins, and an elastic bandage is applied to the upper thigh sufficient to compress the long saphenous vein. A second elastic bandage is wrapped about the limb from the foot to the tourniquet on the thigh. The patient is then instructed to stand, and the examiner carefully observes the varicosities of the leg as the lower bandage is slowly unwrapped from above downward. The tourniquet on the thigh is left in place. As the lower bandage is untwined, the site of an incompetetnt communicating vein will be indicated by the appearance of a prominently bulging varicosity (blowout). When the first blowout is found, the spot is marked, and the upper bandage is extended to that point. Another bandage is then applied from that site downward, and the test is repeated again and again until all blowouts have been marked. Caution should be taken in this test because severe pain and swelling may arise in the calf if the deep veins are obstructed.
Moskowicz's Tourniquet Test. The patient is placed supine with the knees extended in a relaxed position. The straight limb is then elevated by the examiner to about 45*, an elastic bandage is wrapped around the limb in an over- lapping fashion from the ankle to the mid-thigh, and the elevated limb is supported in this position for 5 minutes. At the end of this time, the examiner quickly untwirls the bandage from above downward and notes how rapidly the skin blushes when the obstruction to the collateral circulation has been removed. If the normal blush is absent or lags far behind the unbandaged area, something (eg, an arteriovenous fistula) interfering with the collateral circulation is indicated.
Miscellaneous Pathologic Signs and Reflexes
Strumpell's Tibialis Sign. This test is often used to confirm a pathologic reflex suggesting spastic paralysis in the lower extremity. The patient is placed supine with the knees extended in a relaxed position. The examiner, standing to face the involved limb, lifts the patient's leg, flexes the knee, places his caudad hand against the distal posterior thigh, and grasps the patient's shin with his cephalad hand. The thigh is then flexed on the hip while simultaneously flexing the leg against the examiner's hand held near the popliteal space. If the foot briskly dorsiflexes (and sometimes adducts) on this maneuver, it is a positive sign of an upper motor neuron lesion.
Piotrowski's Sign. Percussion of the tibialis anticus muscle produces sharp dorsiflexion and supination of the foot. When this reflex is excessive, it signifies organic CNS disease.
Oppenheim's Spastic Sign. This reflex is met with in spastic conditions of the legs. With the patient prone, the sign is elicited by striking or goading the midline surface of the leg posteriorly from the upper posterior portion of the tibia downward, which causes contraction of the tibialis anticus, extensor hallucis longus, extensor digitorum communis, and, in some instances, also the peroneal muscle. It has Babinski implications.
Neri's Leg Sign. In organic hemiplegia, while the patient is in the supine position and the affected straight leg is lifted, the sign consists of spontaneous flexion of the knee.
 |
PERONEI STRAIN AND INFLAMMATION
The peronei tendons pass behind the lateral malleolus. They are best palpated during active eversion and plantar flexion. The peronei are the primary foot everters and help in plantar flexion. An aseptic tendon inflammation is often involved. If stenosis of the tunnel in which the tendons run occurs, the peroneal tubercle will feel tender and thick. Tenderness here also suggests bursitis or fracture of the styloid process in severe sprain.
When an associated peroneal tenosynovitis or tendovaginitis is associated with strain, it is characterized by acute tenderness, pain, motion restriction, swelling of the sheath, a probable squeaking crepitus on joint movement, and possible ecchymosis.
Management. Treatment is similar to that for an acute strain, with cold packs, rest, strapping for 8-12 days, and graduated active exercises. Tendovaginitis is stubborn to manage and often requires referral for tendovaginotomy.
PERONEOEXTENSOR SPASM
Peroneoextensor spasm produces a spastic flat foot characterized by pain at the lower lateral leg and ankle, especially after cross-country runs. There is little or no area tenderness, but dorsiflexion and inversion are restricted. Spasm in eversion may become quite marked and may indicate an eversion subluxation.
Management. Management consists of muscle techniques, passive peroneal stretching, ultrasound, and progressive mobilization.
POSTERIOR TIBIAL TENDON STRAIN
While tendons of the peronei run behind the lateral malleolus, the tendon of the posterior tibial muscle passes behind the medial malleolus. The clinical picture is similar to that of peronei strain and inflammation: tenderness, sheath swelling, crepitus, possible ecchymosis.
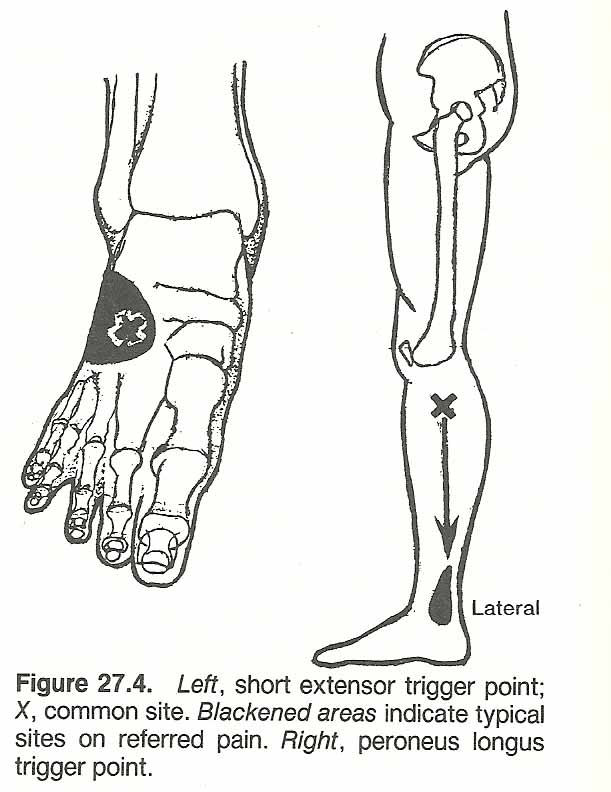
TRIGGER POINT ANKLE PAIN
Pain referred chiefly to the front of the ankle and big toe is frequently caused by a trigger point located in the upper anterolateral aspect of the leg in the tibialis anticus muscle. Firm sustained pressure at this trigger point sets off an aggravating ache. At other times, a trigger area just lateral to this located in the extensor digitorum longus muscle will refer pain more laterally in the ankle and to the dorsum of the foot in the area of the 4th metatarsal bone.
Management. If the area of pain is sprayed with a vapocoolant, the pain will be relieved only momentarily, but spraying over the trigger area may abolish the pain, the restricted motion, and deep tenderness in the reference zone for many hours if not permanently.
Ankle Instability
Ankle instability results when inversion or eversion sprains stretch or rupture supporting ligaments. Always test and compare bilaterally. Screen tests for active range of motion can be made by toe walking to test plantar flexion and toe motion, heel walking to test dorsiflexion, lateral-sole walking to test inversion, and walking on the medial borders of the feet to test eversion. In testing passive subtalar inversion and eversion, stabilize the distal end of the tibia with one hand and firmly grip the heel with the active hand. Alternately invert and evert the heel. Pain during this maneuver suggests subtalar arthritis that is possibly from an old fracture.
DRAW SIGN
Tenderness along the course of the anterior talofibular ligament points to sprain damage. Tears in this ligament allow the talus to slide forward (subluxate) on the tibia. To test for instability and subluxation of the tibia and talus, place one hand on the anterior aspect of the sitting patient's lower tibia and grip the heel within your other palm. When the calcaneus and talus are pulled anteriorly and the tibia is simultaneously pushed posteriorly, the anterior talofibular ligament should allow no forward movement of the talus on the tibia. The test is positive if the talus slides anteriorly from under cover of the ankle mortise. Sometimes the abnormal bone movement can be heard as well as felt during the maneuver.
LATERAL OR MEDIAL INSTABILITY
Gross lateral instability results when both the anterior talofibular and calcaneofibular ligaments are torn. To test lateral instability, stabilize the patient's leg and invert the heel back and forth, noting if the talus rocks loosely in the ankle mortise. Medial instability results in a tear or stretch of the deltoid ligament. To test medial instability, stabilize the patient's leg and evert the heel back and forth, noting any gapping at the ankle mortise.
TALAR SLIDE TEST
This test evaluates ankle joint play (translation) in the horizontal plane. With the patient in either the prone or supine position, the doctor stands to the side and faces the ankle to be tested. The examiner's cephalad hand grasps the patient's lower leg just above the malleoli and the caudad hand grasps the heel just below the malleoli. A pull is made with the upper hand on the lower leg while the lower hand pushes the heel horizontally. Then a push is made with the upper hand while the lower hand pushes the heel. Excessive lateral or medial motion with pain indicates ligamentous instability.
Sprains
As knee sprain, ankle sprain produces a wide variety of damage depending upon which ligaments are stretched and the degree of tear. Isolated tears are rare, and many severe ruptures are associated with lower leg fracture.
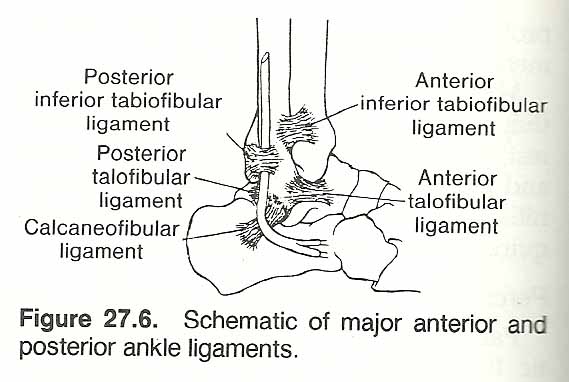 |
The most common form of tarsotibial sprain is created by twisting the leg in varus; ie, inversion and internal rotation, especially when the foot is plantar flexed with the heel off the ground. This injures the talofibular bundle of the lateral ligament. Tears are usually at attachments, with or without avulsion, rather than at the middle of the ligament. Isolated tenderness may be most acute over the anterior talofibular ligament or less often over the calcaneofibular ligament if stress occurs when the ankle is at a right angle. During inversion stress, we see a class-one lever amplifying the external force (five or six times) far above the resistance limit supplied by the bones and ligaments. See Figure 27.6
Lateral sprain often produces an indirect lesser tenderness in the deltoid ligament area from impaction. After eversion sprain, this area will exhibit primary tenderness with secondary tenderness from impaction on the lateral aspect. Hyperextension sprain exhibits lateral, medial, and sometimes posterior tenderness and swelling.
Incidence. According to several studies, capsular ankle sprain appears the most common injury within sports --especially basketball, occurring under the backboard while attempting to recover a rebounding ball. As the result of consistent quick stops and turns, tears of the capsule and the ligaments covering the back of the talonavicular joint are invariably involved. Nearly all participants in hang-gliding and parachuting present some degree of ankle injury as the result of poor landings. With the exception of contusions, ankle sprains and muscle tears near the ankle and knee are the most common injuries in lacrosse. Over-long shoe spikes and studs in football and other field sports render the ankle unstable and contribute to ankle sprain.
Signs and Symptoms of Inversion Sprain. The symptoms and local manifestations are mild to severe pain and swelling beneath the affected tendons and ligaments, tenderness, posible ecchymosis, hypermobile inversion, and spastic functional impairment. The lateral malleolus, talus, and cuboid will palpate as prominent. The talus is usually subluxated from the ankle mortise. In mild cases, only the lateral sulcus is filled with effusion. To support your diagnosis, check for draw sign, judge lateral and medial instability, and use Thompson's test. Acute traumatic arthritis of the ankle following severe sprain is produced by rupture or stretching of the ligaments of the joint by direct or indirect violence.
Signs and Symptoms of Eversion Sprain. Low fibula bone damage is more the rule than isolated medial ligament tears because of the strength of the deltoid. If the inferior tibiofibular ligament tears, the fibula and tibia will separate at the ankle mortise. This widening produces instability leading to degenerative changes. Local manifestations include pain, tenderness, swelling, possible ecchymosis, eversion hypermobility, and inversion motion restrictions.
Management. Poorly treated initial injuries invariably lead to chronic states. Good management requires time and patience. Structural alignment, cold water immersion, elevation, and pressure strapping should be applied as soon as possible after injury to prevent swelling. Strapping should be made with slight eversion in lateral sprain or inversion in medial strain. After strapping over a protective underwrap, walking is encouraged, as functional use facilitates recovery. Keep in mind that the greater the support, the greater the atrophy. Pain relief is enhanced by placing a 2 x 2-inch gauze pad that is about a 1/4-inch thick within the longitudinal arch prior to taping. Double pads are necessary for heavy patients. During the acute hyperemic stage, positive galvanism, mild ultrasound, rest and possibly elevation are also indicated. An application of hyaluronidase is helpful to reduce tissue swelling and edema if used with iontophoresis. Swelling should subside in 36 hr.
After 48 hr, passive congestion may be managed by contrast baths, light massage, gentle passive manipulation, sinusoidal stimulation, heel lifts, and ultrasound. During the stage of consolidation, local moderate heat, moderate active exercise, bracing, moderate range of motion manipulation, and ultrasound are beneficial. In the stage of fibroblastic activity, deep heat, deep massage, vigorous active exercise, toe walking, inversion and eversion walking, negative galvanism, ultrasound, and active joint manipulation speed recovery and inhibit postinjury effects. Active rehabilitative exercises should not begin until walking gait is normal and painless. In preventive strapping, the anterior talofibular ligament which runs from the distal fibula to the talus is the most important ligament to protect for lateral stability. Especially protect the anterior limb of the deltoid after medial sprain. During rehabilitation, a lateral heel wedge is helpful in lateral instability; medial heel wedge, in medial instability. Vitamin C and manganese glycerophosphate are helpful during care.
Vapocoolant Technique in Grade I Ankle Sprains. Place the patient supine with pillows under the knee and ankle. Spray the painful ankle area, and gently assist and resist the patient in ankle flexion-extension. As the pain shifts position, spray the affected area. Once relief has been obtained in flexionextension, add inversion, eversion, and toe flexion-extension, spraying painful sites as necessary between movements. Have the patient attempt to walk, and spray the painful area if necessary. If possible, have the patient stand on his toes and bend forward with his heels on the floor. Once relief is obtained, correct any subluxations isolated, strap the ankle, and instruct the patient in home exercises for 1-2 min each half hour during the waking hours. Begin resistance, stretching, and weight-bearing exercises as soon as logical. These should include toe standing, soleus muscle stretching, and eversion standing.
Simplified Taping Procedure. When swelling has subsided or disappeared, and the ankle shows no ligamentous tear, tape can be applied in a basketweave ankle lock, and weight-bearing can be resumed. During application, the tape begins from the inside and runs under the foot to the outside to hold the heel slightly everted when lateral instability is present. Competitive activity should be avoided for 2-3 weeks for Grade III sprains. Taping during activity should continue for several weeks.
The Gibney Taping Method. This is one of the more time-consuming, but stable, methods. It also allows for swelling without constriction. The foot and leg are shaved and the foot is held at a right angle to the leg while the dressing is being applied. A strip of 1|or 2-inch-wide adhesive plaster is placed against the outer aspect of the leg, passed downward over the outer malleolus, under the heel, making firm upward pressure against the arch by traction as the remainder of the strip is applied to the inner aspect of the leg. A second strip is placed at a right angle to the first, beginning on the outer aspect of the foot over the cuboid bone, passing on the medial side of the foot over the internal cuneiform bone. Successive strips are placed alternately about the leg and foot until the ankle is encased. Semicircular strips of tape are used about the anterior foot and leg to retain the dressing.
Recommended Activity Taping Method. There are about 30 good methods described in literature for taping an ankle. The one recommended by Christensen is described in six steps:(1) After underwrap is in place, apply an anchor of tape about 3 inches above the malleolus and another around the arch and instep.
(2) A stirrup is next placed from the calf anchor on the inside of the leg, bringing it just back of the malleolus, under the heel, and up the outside of the leg to the calf anchor. The foot should be slightly everted. Next, a horizontal strip is run from the inside foot anchor around the heel and under the malleolus to attach to the foot anchor on the outside.
(3) Three stirrups and three horizontal strips are placed to overlap the preceding strip by one-half.
(4) Horizontal strips are continued up the leg to further support the strapping after the basketweave is completed.
(5) A figure-8 is applied starting over the lateral malleolus. Bring the tape across the instep, under the arch, up across the instep, and around the leg to the starting point.
(6) A heel lock is applied to finish the strapping. Starting on the lateral malleolus, bring the tape across the instep, under the foot, and around the heel on the inside of the foot. Continue around and over the instep, down under the foot and heel, and finish on the lateral aspect of the ankle where the strip was started.
Subluxations
LATERAL TALUS SUBLUXATION
Characteristics associated with this subluxation are inversion ankle sprain, excessive pronation, pain anterior to lateral malleolus, and anterior talofibular ligament tenderness.
Adjustment. The patient is placed supine. Sit at the foot of the table, facing the patient. Place the third finger of your medial contact hand over the anterolateral margin of the talus with your thumb on the plantar surface. Your lateral stabilizing hand supports the heel. Apply traction with your stabilizing hand to separate the calcaneus from the talus while simultaneously making a lateral to medial torque adjustment towards yourself. Follow correction by evaluating the integrity of the muscles involved in excessive pronation: tibialis posterior and anterior, peroneus longus, flexors digitorum longus and hallucis longus, abductor hallucis, soleus, gastrocnemius, and intrinsic foot muscles.
Alternative Adjustment Procedure. The doctor-patient position is the same as above. Internally rotate the patient's leg, and make a double-thumb contact on the lateroanterior aspect of the talus. Your lateral hand grips the calcaneus, while your medial hand grasps the anterior surface of the tarsals. Apply pressure with your double-thumb contact, slightly invert the foot, apply traction, and simultaneously make a short, sharp pull towards yourself.
MEDIAL-INFERIOR TALUS SUBLUXATION
This subluxation is often found in association with eversion ankle sprain exhibiting tenderness at the deltoid ligament.
Adjustment. This is essentially the opposite of the adjustment for a lateral talus. The patient is placed supine. Sit at the foot of the table, facing the patient. Place the third finger of your lateral contact hand over the anteromedial aspect of the talus with your thumb on the plantar surface. Your stabilizing hand supports the heel. Apply traction with your stabilizing hand to separate the calcaneus from the talus while simultaneously making a medial to lateral torque adjustment towards yourself. Follow correction by evaluating the integrity of the tibialis anterior and posterior.
ANTERIOR TALUS SUBLUXATION
Indications include pain and tenderness at the anterior aspect of the ankle, inversion sprain that occurs with plantar flexion, exostosis of the dorsal talonavicular articulation, and excessive pronation.
Adjustment. The patient is placed supine. Sit at the foot of the table, and face the patient. Interlock fingers across the anterior ankle with thumbs placed on the plantar surface and your elbows moderately flexed. The third fingers should make specific contact over the anterior aspect of the talus. Apply traction to separate the calcaneus and talus while simultaneously snapping your wrists and elbows inferiorly in a scooping fashion to move the talus from the anterior to the posterior. Evaluate the integrity of the tibialis anterior and extensor digitorum longus.
Fractures and Dislocations
The patterns of ankle injuries can be classified according to direction of primary and secondary forces such as external rotation, abduction, adduction, and vertical compression.
EXTERNAL ROTATION INJURIES
The most common mechanism involved in ankle injury is that of external rotation plus abduction. The classic fracture of this type is an oblique fibular line directed from the anterior-inferior to the posterior-superior aspect which is frequently comminuted along the posterior cortex. Foot pronation is the usual mechanism, associated with a deltoid tear. The interosseous ligaments are usually spared if the foot is in supination rather than pronation. An oblique transverse fracture of the medial malleolus at or beneath the tibial articular surface may occur, with fragments displaced inferiorly by the pull of the deltoid ligament and tearing of the anterior tibiofibular ligament. A small posterior malleolar fracture may result from the rotating fibula.
ABDUCTION AND ADDUCTION INJURIES
An abduction fibula fracture is typically oblique, short, often with comminution of the lateral cortex. As external rotation injuries, abduction injuries produce transverse malleolar fractures or deltoid tears. This fibula fracture usually occurs below or within the syndesmosis. It may occur above the syndesmosis if it ruptures. When external rotation is a secondary force added to abduction, the fracture is usually higher on the fibula and/or more oblique. In abduction injuries, the lateral fibular cortex may be comminuted, small dorsal tibial and fibular avulsions may be noted, and diastasis is more common because the syndesmosis is ruptured. A horizontal fracture of the medial malleolus or torn deltoid, a high fibula fracture, and a complete rupture of the syndesmosis (called a Dupruytren fracture-dislocation) is an unstable injury resulting from abduction and lateral rotation.
Adduction ankle injuries frequently result in distal fibular horizontal fractures at or below the articular surface. Frequently associated is a vertical fracture of the medial malleolus projecting above the articular surface which is often related with a fracture of the lateral aspect of the talar dome. Diastasis is not associated with adduction injuries, but post-traumatic arthritis may result from comminution of the articular surface. Fractures to the posterior margin are not common.
VERTICAL COMPRESSION INJURIES
Vertical compression injuries are subdivided by Dalinka into posterior marginal fractures, anterior marginal fractures, and supramalleolar fractures.
Posterior Marginal Fractures. These types of fractures may occur
(1) with significant vertical compression of the articular margin or
(2) without vertical compression. External rotation injuries, with or without an abduction factor, may produce small posterior marginal fractures. Vertical compression with external rotation force is more likely to produce large fragments. When the posterior articular fragment is large, the incidence of posttraumatic arthritis and chronic instability is high. Posterior marginal fractures seldom occur as isolated injuries, thus the proximal fibula must also receive careful evaluation. Rips of the anterior tibiofibular ligament are frequently associated.Anterior Marginal Fractures. This type of fracture, frequently isolated, may be comminuted. It usually occurs in the dorsiflexed foot.
Supramalleolar Fractures. This fracture, invariably associated with fracture of the fibula, is of the distal 4 cm of the tibia above the ankle (Malgaine fracture). It is typically open, severely comminuted, and related to high-impact forces in the direction of axial compression.
Roentgenologic Considerations
Lateral, A-P, and oblique x-ray views are standard for evaluation of a possible ankle fracture, and sometimes tomography or stress views during inversion and eversion are required.
SEVERE ANKLE INJURIES IN CHILDREN
The area of greatest weakness in children during ankle trauma is at the growth plate. Epiphyseal separations are more common than fractures as the ligaments attach to the epiphysis. The Salter/Harris classification is widely applied to ankle injuries in childhood:
Type I: Fracture occurs through the zone of provisional calcification where the entire epiphysis may be separated or the growth plate widened. Although views may appear normal, the periosteum may be either intact or torn on one surface. Swelling and tenderness are frequent. The mechanism is usually one of inversion or abduction force. This type of injury is uncommon to the tibia, but common to the fibula. Because the germinal layer is intact, prognosis is excellent. Diagnosis is confirmed in 2 weeks after injury by noting periosteal new bone formation.
Type II: Epiphyseal separation plus a small metaphyseal fragment (ThurstonHolland sign) is seen. Plantar flexion and eversion result in fracture produced by lateral displacement. The periosteum is intact on the side of the metaphyseal fragment, and ischemia of the foot may be noted if the fracture is severely displaced. With this tibial injury, a green-stick fibula fracture is frequently associated. Prognosis is excellent as the germinal layer remains with the epiphysis and the separation is through the zone of provisional calcification.
Type III: An intra-articular epiphyseal fracture is seen at the lateral aspect of the tibial epiphysis. The mechanism is one of lateral rotation or shearing injury (Tillaux fracture). The lateral part of the tibial epiphysis is attached to the fibular metaphysis by the anterior tibiofibular ligament, and it is the pull of this ligament which avulses the lateral or anterolateral part of the tibial epiphysis. The medial part of the tibial epiphysis fuses at 13-14 years. There is usually little or no displacement. In spite of damage to the growth plate, prognosis is good if growth has ceased.
Type IV: This is a rare fracture across the epiphysis and the growth plate with a small metaphyseal fragment. Premature growth cessation in the fracture area may result.
Type V: This is a rare compression injury of the growth plate, usually medially, that does not exhibit abnormality in the ossified epiphysis. Premature growth cessation in the fracture area results.
SEVERE ANKLE INJURIES IN ADULTS
Ankle fractures are frequently associated with severe ligament injury. One report states that rupture of one or more syndesmotic ligaments occurs in more than 90% of malleolar fractures. Ligamentous injury is always indicated in displaced malleolar fractures. One of the more common fracture sites occurs when the talus is displaced in the ankle mortise, shifting the talus and fibula laterally. When this happens, a slight widening of the distal interosseous space between the tibia and fibula (indicating interosseous membrane rupture) will be noted.
Fractures of the calcaneus are the most frequent. They usually result from falls where the victim lands stiff legged on his heels. Fracture of the calcaneus may be obvious with a widely separated fracture line and grossly disturbed positioning of fragments or it may be quite discrete with little obvious change visible. Frequently, normal structure is disturbed consequent to crushing of the spongy bone and deformity of outline. The survey should include the posterior halves of both heels. In later views, the fracture line is seldom seen. These injuries are frequently accompanied by compression fractures in the lumbar or lower thoracic regions from force traveling up the legs to the spine. Thus, it is always a good rule to x-ray the thoracolumbar region when crushing fractures of the heel are found.
For the purpose of accurate diagnosis, the utilization of Boehler's angle is recommended. For the normal calcaneus, Boehler's angle results from a line drawn first from the posterosuperior margin of the talocalcaneal joint through the posterosuperior margin of the calcaneus, making an angle of approximately 35*-40* with a second line drawn from the posterosuperior margin of the talocalcaneal joint to the superior articular margin of the calcaneocuboid joint. Less than 28* is considered definitely abnormal and poor position from a functional standpoint.
Fracture of the talus and cuboid are next in frequency to those of the calcaneus. Bilateral films are helpful to rule out a trigonum, the posterior extension of the talus occasionally occurring as a separate bone. Another anatomic variation which sometimes leads to interpretative error is the presence of a separate ossification center at the base of the fifth metatarsal which is usually bilateral.
Fractures also commonly occur in the posterior or midportion of the talus. This area may be the site of avascular necrosis, viewed as a lucent crescent under the articular margin of the talus. In advanced cases, the superior portion of the talus may show collapse of its articular margins. This is best observed on the A-P view as the overlapping malleoli cloud the picture in the lateral position. Care must be taken to not confuse a sharp or rough-edged fracture fragment at the posterior talus with a rounded-edged accessory ossicle (os trigonum). Fractures secondary to impact of the talus are oblique and frequently comminuted, while those secondary to ligamentous avulsion are horizontal. The obliquity of the fracture line is determined by the direction of force. It should be kept in mind that as little as 1 mm of lateral displacement reduces the area of tibial-talar contact by 42%.
Gait Clues
During the stance phase, note heel strike, foot flat, midstance, and toe push-off of each extremity. When the foot slaps down sharply after heel strike, weak dorsiflexors should be suspect. On the other hand, fused ankles will prevent a midstance flat foot. Failure to hyperextend the foot during push-off is a sign of arthrosis. A flat-footed calcaneal gait during push-off is symptomatic of weak gastrocnemius, soleus, and flexor hallucis longis muscles.
During the swing phase, note acceleration, midswing, and deceleration of each extremity. If the hip is flexed excessively to bend the knee and thus prevent the toe from scrapping the floor as in a steppage gait, weak ankle dorsiflexors are the usual cause. The foot will have trouble clearing the floor if the ankle dorsiflexors are weak or the knee is unable to flex properly.
Selected Disorders of the Ankle
The pulse of the posterior tibial artery is often difficult to locate, even when the ankle is relaxed. This artery lies between the tendons of the flexor digitorum longus and the flexor hallucis longus muscles. If the pulse is noted, it should be compared bilaterally. The tibial nerve follows the course of the posterior tibial artery and is located just behind and lateral to the artery. A ligament binds the neurovascular bundle to the tibia creating the tarsal tunnel which has the same implications as the carpal tunnel in the wrist.
TARSAL TUNNEL SYNDROME
This is a nerve compression syndrome of the neurovascular bundle under the medial malleolus. The disorder is characterized by burning sensations of the toes and plantar surface. Pain is often referred along the posterior tibial nerve as high as the buttocks. Deep palpation posterior to the medial malleolus initiates or aggravates pain in the sensory distribution of the nerve. When the neurovascular bundle is percussed, a positive Tinnel's sign is elicited with radiating pain. In the chronic stage, claw toes develop which restrict extension.
Tinel's Foot Sign. With the patient prone, flex the knee to a right angle and tap, with a reflex hammer, the tibial nerve as it passes just behind the medial malleolus. If paresthesiae arise that radiate to the foot, a tarsal tunnel syndrome is suggested.
Ankle Tourniquet Test. The patient is placed supine in a relaxed position, a sphygmomanometer cuff is wraped around the ankle of the affected side, and the cuff is inflated to just above the systolic level and maintained for 90 seconds. An exacerbation of pain in the ankle or foot is indicative of tarsal tunnel syndrome.
Management. The cause of the compression must be found. This may be traced to the effects of chronic subluxation, scar and adhesion formation, tenosynovitis, venous engorgement, valgus deformity of the foot, etc. Recurrent trauma is usually involved. If symptoms fail to respond to conservative care, referral for exploratory surgery is indicated.
SPURS
Two common post-traumatic abnormalities are talonavicular spurs and narrowing of the subtalar joint. These are most common from chronic stress to the talonavicular ligament in sports requiring constant speed, jumping, and rapid changes in direction such as seen in basketball, tennis, soccer, and field hockey.
Bowler's Spurs. Degenerative changes or fracture may result in spur formation of the posterior talus that may irritate the posterior margin of the tibia's inferior articular surface. Once formed, the spur becomes constantly irritated by forced ankle flexion. Conservative care is often frustrating when activity is continued. Deep heat and graduated exercises bring the best results, but referral for surgery to remove spurs or loose bodies may be required. Progression into osteoarthrosis is a common complication.
Football Ankle. This disorder consists of a traumatic osteitis that is sometimes confused with chronic sprain. There is general ankle pain, minimal swelling, and soreness which is aggravated by kicking the ball. Roentgenography shows new bone formation on the margins of the inferior articular surface of the tibia, but the joint surfaces are not involved as in osteoarthrosis. Conservative care incorporating rest and graduated active exercises will usually suffice. If not, the spurs must be removed surgically.