

|
Direct Vascular Injuries Laryngeal, Cricothyroid, and Tracheal Injuries Hypopharyngeal and Esophageal Injuries The Cervical Spine Roentgenologic Considerations of the Neck Clinical Compression Tests Soft-Tissue Injuries of the Posterior Neck Cervical Contusions, Strains, and Sprains Nerve Stress Vertebral Artery Deflection Disc Disorders Spinal Cord Injury Bone and Joint Injuries and Disorders Cervical Spondylosis Reversal of the Normal Cervical Curve Cervical Rib Fractures and Dislocations of the Atlas Fractures and Dislocations of the Axis Severe C3-C7 Injuries Cervical Subluxation Syndromes Functional Anatomy Relative to Cervical Subluxations Occipital and Cervical SubluxationsChapter 21:
Neck and Cervical Spine Injuries
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Chiropractic Management of Sports and Recreational Injuries”
Second Edition ~ Wiliams & Wilkins
The following materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated
to chiropractic research. Please review the complete list of available books.
Emergency Care Initial Assessment Emergency Management Soft-Tissue Injuries of the Anterior Neck
Chapter 21: Neck and Cervical Spine Injuries
In general, trauma anteriorly to the neck implies soft-tissue damage and possible airway obstruction; trauma posteriorly suggests cervical spine and cord damage; and lateral trauma indicates possible vascular and musculature damage. Due to relative head weight to neck strength and other anatomic differences, neck injury is more critical in the very young.
The anterior and lateral aspects of the neck contain a wide variety of vital structures, yet have no bony protection. Partial protection is provided by the cervical muscles, the mandible, and the shoulder girdle. Williams/Sperryn report that back and neck injuries form 10%–20% of sports injuries. The peak incidence occurs in the third decade, with 90% of the accidents occurring in males. Body build does not appear to be a major factor. High-speed sports such as seen with vehicle accidents, football backs and ends, gymnastics, diving, skiing, surfing, and horseback riding have the highest injury rate.
Emergency Care
Initial Assessment
Stabilize the neck before assessment of severity. The patient should never be asked to sit or stand until major disability has been ruled out. The first point in analysis is knowing the mechanism of injury. Without moving the patient, check vital signs and palpate for swelling, deep tenderness, deformity, and throat cartilage stability. When logical, another person should apply gentle bilateral traction on the cervical area via the skull during palpation.
Are there bleeding, spasm, pain, motion restrictions, sensory changes, signs of shock? Limb weakness or dysesthesia indicates nerve root compression. Injuries of the upper airway or ailmentary canal feature ventilation abnormalities, stridor, bubbling wound, subcutaneous emphysema, hoarseness and dysphagia, bloody sputum, nosebleed, bloody vomitus, or unexplained wound tenderness. Injuries to the cervical nerves are suggested by deviation of the tongue, drooping mouth corner, sensory deficits, and Horner's syndrome. Cervical fractures are commonly associated with severe pain, spasm, and joint stiffness.
Vascular injuries feature vigorous bleeding, absent superficial artery pulsations, an enlarging or pulsatile hematoma, and stroke signs. If there is any suggestion of injury to the cartoid artery, palpation should be avoided. Such an injury should be suspected if there is a diagonal erythematous contusion on the side of the neck. Palpation may encourage complete carotid occlusion.
If there are no severe complaints or recognizable signs of major disability, ask the patient to conduct mild active movements if able to do so without discomfort. If slight straight axial compression on top of the head produces unilateral or bilateral radiating root pain, deep injury must be suspected and precautions taken immediately. After the neck has been evaluated, check possible injury to other parts of the body.
For a review of neurologic, orthopedic, and peripheral vascular tests, see Table 21.1.
Disorder Procedures/Signs
Cervical
syndromes Active rotary compression test
Bakody's test
Barre-Leiou's test
Biceps reflex
Bikele's test
Brachioradialis reflex
Bradburne's sign
Brudzinski's test
Cervical distraction test
Ciliospinal reflex
Deltoid reflex
George's tests
Head retraction reflex
Infraspinatus reflex
Inverted radial reflex
Kernig's test
Lhermitte's test
Light touch/pain tests
Muscle strength grading
O'Donoghue's maneuver
Passive cervical compression tests
Pectoral reflex
Percussion test
Radial reflex
Range of motion tests
Ruggeri's reflex
Rust's sign
Scapulohumeral reflex
Shoulder depression test
Soto-Hall's test
Spurling's tests
Swallowing test
Triceps reflex
Ulnar reflex
Valsalva's maneuver
Vertebrobasilar maneuvers
Wrist reflex
Disorder Procedures/Signs
Thoracic outlet
and related
syndromes Adson's test
Allen's test
Costoclavicular maneuver
Eden's test
Traction test
Wright's test
After attending to all life-threatening possibilities, a more thorough examination may proceed, but required transportation should never be delayed for this purpose. Seek gross abnormalities, then check for details. When the patient swallows, note the action of the cricoid cartilage area. Check the trachea for midline alignment. Evaluate abnormal contours, curvatures, and restricted movements. Venous thrombosis, masses, and exudates may produce visible and palpable edema in the neck. Palpate the neck with the patient supine so that the muscles are relaxed and the head may be passively controlled.
Laryngeal Injuries. The larynx may be crushed between a blunt object and the anterior cervical spine, leading to cartilaginous fracture, subluxation, and/or dislocation. The most common fracture of the thyroid cartilage is that of a vertical anterior split between the thyroid notch and the cricothyroid membrane producing avulsion of the anterior vocal cord attachments and hematoma. Laryngeal injury usually produces a louder stridor than tracheal injury, but stridor may be absent if the obstruction is severe enough to completely obstruct the airway. Besides stridor, other signs and symptoms of laryngeal fracture are loss of cartilaginous landmarks from edema, dyspnea, dysphonia from paresis or hematoma, pain increased by neck motion, dysphagia, subcutaneous emphysema (sometimes from scalp to clavicle), and local tenderness. Otolaryngeal consultation should be quickly sought. Less severe bruises are the result of a fist, elbow, baseball, racket, or stick. Hoarseness and point tenderness are exhibited, but edema and airway obstruction are absent. An overnight ice collar is usually sufficient.
Due to its mobility and structure, the cervical spine is the most frequent site of severe spinal nerve injury and subluxations. In sports, a wide variety of cervical contusions, 1–3 Grade strains and sprains, subluxations, disc syndromes, dislocations, and fractures will be seen. Much cervical spine injury can be attributed to the relatively small vertebral bodies, the wide range of movement in many planes, and the more laterally placed intervertebral articulations which requires nerve roots to leave the spinal canal in an anterolateral direction. Fortunately, there is greater space within the cervical canal than below.
(1) mild (eg, contusions, strains);
Active Cervical Rotary Compression Test. With the patient sitting, observe while the patient voluntarily laterally flexes his head toward the side being examined. With the neck flexed, the patient is then instructed to rotate his chin towards the same side, which narrows the intervertebral foramina diameters. Pain or reduplication of other symptoms probably indicates a physiologic narrowing of one or more intervertebral foramina.
(1) With the patient seated and the head placed in the neutral position, the carotid and subclavian arteries are palpated for abnormal pulsations and auscultated for bruits. If pulse abnormalities or bruits are found, the test is positive for carotid, vertebral, or basilar artery obstruction (stenosis or compression), and the second maneuver should not be conducted.
Mankopf's Procedure. This is the only objective test for pain, and it is not restricted to musculoskeletal complaints of the cervical spine. The patient is placed in a relaxed position and the pulse is taken. The examiner then precipitates the pain (eg, by probing, applying heat or electrostimulation, etc). The pulse rate is then re-evaluated. In situations of true pain, the pulse rate will increase a minimum of 10%.
Cervical Contusions, Strains, and Sprains
O'Donoghue's Maneuvers. The cervical spine of a seated patient is passively flexed, extended, laterally flexed to both sides, and rotated in both directions against patient resistance. Pain precipitated by such isometric contraction indicates cervical strain. The test is then repeated without patient resistance. Pain precipitated by passive unrestricted motion signifies cervical sprain.
“manipulation of the cervical spine is not to be considered conservative therapy, but rather a most aggressive non-invasive procedure by which the normal mechanical attitudes of the motion segments can be restored if aberrant. In all cases of cervical radiculopathy where there is demonstrable pathomechanics, it is recommended that manipulation be the primary treatment of choice, and that this therapy be prescribed and administered by qualified clinicians who have had extensive training in this science.”
To relieve muscle spasm, heat is helpful, but cold and vapocoolant sprays have shown to be more effective in acute cases. Mild passive stretch is an excellent method of reducing spasm in the long muscles. Heavy passive stretch, however, destroys the beneficial reflexes. For example, place the patient prone on an adjusting table in which the head piece has been slightly lowered. Turn the patient's head toward the side of the spastic muscle. With head weight alone serving as the stretching force, the spasm should relax within 2–3 min. Thumb pressure, placed on a trigger area, is then directed towards the muscle's attachment and held for a few moments until relaxation is complete.
The Barre-Lieou Syndrome. This syndrome frequently occurs from trauma to the cervical spine, and an underlying cervical arthritis and/or IVD lesion (eg, spondylosis) are often present. Although the symptomatology is nonspecific, Kimmel describes the common features to be earache, eye pain, facial vasomotor disturbances headache, temporary blurred vision, tinnitus, and vertigo. Dysphagia, phonation defects, and laryngeal and pharyngeal paresthesiae are often associated. If chronic cervical arthritis is a cause of sympathetic irritation, especially in the midcervical area, corneal hyperesthesia and small persistent ulcers usually appear that are confined to the exposed conjunctiva.
Degenerative Disc Disease. Specific signs of acute disc herniation are: C4–5 disc rupture: shoulder and arm pain and paresthesia, hypesthesia of 5C root distribution, deltoid or biceps weakness.
C5–6 disc rupture: hypesthesia of lateral forearm and thumb, biceps and supinator weakness.
C6–7 disc rupture: hypesthesia of the index and middle fingers, triceps, and grip weakness.
C7–T1 disc rupture (uncommon): ulnar hypesthesia and intrinsic muscle weakness in the hand.
Lhermitte's Test: With the patient sitting, flexing of the patient's neck and hips simultaneously with the knees in full extension may produce sharp pain radiating down the spine and into the upper or lower extremities. When pain is elicited, it is a sign suggesting irritation of the spinal dura matter either by a protruded cervical disc, tumor, fracture, or multiple sclerosis.
(1) conservative treatment fails to produce remission of symptoms;
Direct injury to the cord, the nerve roots, or both may be caused by impact forces or shattered bone fragments. The cord may be crushed, pierced, or cut. This type of injury is generally an open wound.
Indirect injury to the cord may be caused by the disturbance of tissues near the spine by violent forces such as falls, crushes, or blows. This type of injury, which is normally closed with respect to the spinal column and cord, is of a lesser degree than direct injury. It takes the form of concussion, hemorrhage, or edema of the cord. The cord may cease to function below the site at which the force was applied even if the cord itself received no direct injury. Such dysfunction may be temporary or long standing. Injuries to the spinal column in which the cerebrospinal fluid is rapidly depleted may be fatal.
If the cervical cord is injured, there is loss of sensation and flaccid paralysis. The lower limbs exhibit a spastic paralysis. If the space in which the spinal fluid flows between the spinal cord and the surrounding vertebral column is either compressed or enlarged, severe headache occurs. Posttrauma penile erection strongly suggests either cervical or thoracic cord injury.
Emergency Care. Immediate and obvious symptoms of spinal cord injury parallel those of a fracture of the spinal column. In the emergency-care situation, the patient with spinal cord injury must be treated as if the spinal column were fractured, even when there is no external evidence. Shock must be prevented or reduced. If the player is conscious, ask the location of pain. Ask if the player can move arms and legs. Pinch the skin and check for pain perception. Clothing should be loosened, and everything removed from the pockets. Shoes and moist socks should be removed. Knee and ankle reflexes can be tested, but do not move the head and neck. The patient should be protected from temperature extremes, but heavy covers should not press against paralyzed parts.
Emergency Management
Establishment of an adequate airway takes priority over all other concerns with the exception of spurting hemorrhage. After injury to the anterior neck, tenderness and crepitus in the thyroid area associated with hoarseness or signs of respiratory distress signal the need for probable emergency intubation. The airway in the neck region may be obstructed by blood, mucus, edema, and broken parts of the trachea and larynx. Clearing the mouth (not the pharynx) with the fingers, together with postural drainage in the semiprone position, may be successful, but care must be taken not to force debris further down the airway with probbing fingers. If not successful, an emergency surgical airway must be performed promptly by the most experienced person available.
Whenever spinal injury is suspected, a backboard should be used before transporting the patient. Gentle constant hand traction should be applied to the chin and occiput while transfer is being made to a board. The head should be laterally fixed with sandbags or rolled cloth, and the rest of the body with straps. A cervical collar should not be used as it interferes with examination and tracheostomy. See that the neck is never flexed.
Hemorrhage from a neck wound, unless treated at onset, is rapidly fatal. Dressings applied to the neck must be tied over the head or downward under the opposite armpit, but never around the neck. Avoid pressure on the trachea, carotids, and deep veins.
After severe neck injury, return to play should not be allowed until after roentgenography indicates proper healing, the neck is stable and painless during passive and active motion, and the neck has been strengthened by progressive therapeutic exercises.
Soft-Tissue Injuries of the Anterior Neck
Direct Vascular Injuries
With the exception of spinal cord damage, injuries of the major blood vessels comprise the highest mortality and morbidity of all neck trauma. The most serious consequences are those of airway obstruction from blood, air embolism, spurting hemorrhage, cerebral infarct, and neurologic deficits consequent to cerebral hypoxia. Seek signs of bleeding, discoloration, swelling, lack of superficial pulses, or auscultated bruits. Pressure will control almost any hemorrhage.
Laryngeal, Cricothyroid, and Tracheal injuries
Obstruction within the upper airway is the second most common cause of death resulting from head and neck trauma. Thus, the priority concern in any anterior neck injury is impairment of the airway. In this regard, the cricoid and thyroid cartilages are quite vulnerable to direct trauma of the neck. Any injured person tends to hyperventilate. Thus, ventilation is not difficult to assess. A minor airway obstruction may soon become suddenly life threatening or be delayed for several hours after injury.
Cricothyroid and Hyoid Injuries. Displaced fractures of the cricoid, especially, must be quickly openly reduced as the cricoid encircles the airway. Subglottic stenosis is a common result of associated lacerations and mucosal tears not being carefully reapproximated. Hyoid injuries are rare, extremely painful, and rarely affect the integrity of the airway.
Tracheal and Thyroid Injuries. Tracheal injuries are fortunately rare, usually resulting from a clothesline-type injury or a "chop" to the base of the neck just below the "Adam's apple". Possible airway obstruction requires quick and careful evaluation. Tracheal rupture causes air to leak into neck tissues (balloon neck) and connective tissues of the shoulder girdle. Fracture is also characterized by emphysema and breathing difficulties. A similar blow above the sternum may cause a thyroid hematoma, characterized by severe hoarseness. After any neck or thorax injury, the trachea should be checked for its midline position. Indirect whiplash injury to the cervical spine is also a possibility with any blow to the anterior neck.
Emergency Care. The first-aid priority is to assure an adequate airway. The problem becomes complex when endotracheal intubation is necessary (requiring extension of the neck) and possible cervical spine and/or cord damage may be present, making extension of the neck contraindicated. This requires "blind" endotracheal intubation, cricothyreotomy, or tracheotomy by an experienced person. Also, if the larynx has separated from the trachea or separated between two tracheal rings, attempts at endotracheal intubation may be fatal. This situation requires inserting the tube below the separation if possible.
Thyroid Cartilage Mobilization. Chronic pain or ache may occasionally arise from a fixated thyroid cartilage. This is usually from previous trauma resulting in immobilization and stasis. For correction, place the patient on a table in the supine position without a pillow. Stand to the side of the patient, and grasp the upper and lower margins of the thyroid cartilage with the fingers of your caudad hand while your cephalad hand supports the patient's chin. Gently manipulate in a clockwise and counterclockwise motion with the fingers using the thumb as a pivet. The action should come from your elbow rather than your wrist or fingers. Several movements should show increased cartilaginous mobility after 1–3 sessions.
Hypopharyngeal and Esophageal Injuries
The esophagus is normally collapsed and shielded by surrounding structures. However, because it has extremely delicate walls, it can be easily injured by internal (eg, foreign body ingestion, exploration) or external penetrating wounds. Simple tears of the oropharynx or nasopharynx respond well to saline irrigation, restricting solid food, and taking precautions against infection. More severe injuries require surgical repair and antibiotics.
The Cervical Spine
Cervical spine injuries can be classified as being:
(2) moderate (eg, subluxations, sprain, occult fractures, nerve contusions, neuropraxias);
(3) severe (eg, axonotmesis, dislocation, fracture without neurologic deficit); and
(4) dangerous (eg, fracture and/or dislocation, spinal cord injury).
Roentgenologic Considerations of the Neck
A well-founded appreciation of normal variations, epiphyseal architecture, development defects, and congenital anomalies is a distinct aid in evaluating injuries of the cervical area. After the age of 8 years, the neck, with few exceptions, attains an adult form where growth plates present few diagnostic problems. On the lateral view, the anterior and posterior soft tissues, the atlanto-occipital articulation area, vertebral bodies, disc spaces, facet joints, and spinous processes should all be carefully evaluated. It is easy to miss lower cervical fractures inasmuch as they are often obscured on lateral views by the subject's shoulders if proper precautions are not taken.
If routine cervical views are normal, then oblique, open-mouth odontoid, flexion, and extension views with most extreme care should be taken to verify symptoms. Flexion and extension views will indicate the extent of ligament rupture and bony displacement, but the danger of causing further damage is great. A complete radiographic study of the cervical spine can usually be accomplished with the views of the Davis or the modified-Davis series. Such a series is recommended when there is a history of trauma to the cervical spine and adjacent tissues or a history of chronic complaint and symptoms of possible pathology. Subtle fractures are often elicited only on laminagrams or tomograms.
SOFT TISSUES
In a conscious player that has been injured, any neck spasm should be considered the expression of a cervical fracture or dislocation until proved otherwise. Dislocation or severe subluxation of C1 at the occipital junction may be seen, especially on the lateral view, and be associated with widening of the prespinal soft-tissue space following hemorrhage. The soft-tissue shadows anterior to the upper cervical vertebrae are normally narrowest in the upper cervical area and seldom wider than a C6 vertebral body's A–P dimensions in the lower cervical area. The retropharyngeal space should not exceed 7 mm, and the retrotracheal space should not exceed 22 mm. Signs of free air, edema, or hemorrhage may be seen in the prespinal and anterior area of the neck. After trauma, an increase in soft-tissue width is presumptive evidence of hemorrhage or edema from fracture.
With close inspection, one may sometimes note a lucent line tracking along the anterior margin of the cervical vertebrae, representing fatty tissue between the esophagus and anterior longitudinal ligament. This strip may be displaced anteriorly in spinal trauma and present the only evidence of injury.
The space available for the spinal cord (diameter of spinal canal) is the narrowest distance between the posterior edge of a vertebral body and the anterior edge of the posterior vertebral arch. This measurement should not exceed 14 mm from C1 to C7 in adults or children. The width of the odontoid is approximately equal to the width of the spinal cord at the C1 level, and thus is a guide to the space available for the cord. If the space is less than the width of the odontoid, the cord is likely compromised.
Up to 3 mm of displacement of the atlas on the axis infers that the transverse ligament is intact, while ligament rupture is implied if displacement is from 3–5 mm. When displacement exceeds 5 mm, it may be assumed that the ligament has ruptured and the accessory ligaments are stretched and partially deficient. Atlantoaxial instability is commonly caused by odontoid fracture, rheumatoid arthritis, and odontoid anomalies.
An acute rupture is often indicated by collapse of the disc space. Keep in mind that severe neurologic damage may be present without roentgenographic evidence (eg, brachial plexus injury), thus indicating a possible need for myelography after acute injury to elicit evidence of an avulsed nerve-root sleeve, intramedullary hemorrhage, bone fragments, or edema.
OSSEOUS TISSUES
Bony spurs are common in the cervical spines of male wrestlers, although adjacent intervertebral disc spaces are usually normal. Check for possible vertebral compression fractures by evaluating the anterior aspects of the vertebral bodies for collapse and comparing their margins. Posterior vertebral margins are compared for signs of subluxation or dislocation; ie, a continuous line passing through each posterior vertebral margin should be smooth and unbroken.
Carefully evaluate the relationships of the apophyseal joints and spinous processes for possible injury. The joints may show possible slippage. On an oblique view, the facets will be shingle-like and the end-on images of the lamina will appear as a chain of ovals. Whether or not a subluxation appears, a fracture may be located in the neural arch or facet joint. Fractures of a spinous process frequently occur without displacement.
Intervertebral joint dislocation, unilateral or bilateral, may result from severe flexion trauma. Lamina fracture may or may not be associated. Facet locking is particularly common in unilateral dislocations, and it is usually associated with severe root and/or cord involvement.
Clinical Compression Tests
There are several syndromes to consider under the classification of neurovascular compression syndromes (also termed thoracic outlet or inlet syndromes), each of which may produce the symptom complex or radiating pain over the shoulders and down the arms, atrophic disturbance, paresthesias, and vasomotor disturbances. These syndromes do not necessarily give the cause of the problem. In some cases, poor posture, anomalies, muscle contractures, or other factors may be responsible. In addition, subluxation syndromes may initiate these and other disturbances of the shoulder girdle and must be further evaluated. Always x-ray before performing a cervical compression test, especially when the patient has been involved in trauma, to rule out possible arteriosclerosis, disc compression, fracture, avulsion, gross subluxation, dislocation, or bone disease.
Passive Cervical Compression Tests. With the patient sitting, stand behind the patient. The patient's head is laterally flexed and rotated slightly towards the side being examined. Place interlocked fingers on the patient's scalp and gently press caudally. If an intervertebral foramen is physiologically narrowed, this maneuver will further insult the foramen by compressing the disc and narrowing the foramen, thus causing pain and reduplication of other symptoms. In the second test, the patient's neck is extended by the examiner who then places interlocked hands on the patient's scalp and gently presses caudally. If an intervertebral foramen is physiologically narrowed, this maneuver mechanically compromises the foraminal diameters bilaterally and causes pain and reduplication of other symptoms.
Shoulder Depression Test. With the patient sitting, stand behind the subject. The patient's head is laterally flexed away from the side being examined. This is done by the doctor stabilizing the patient's shoulder with one hand and applying pressure alongside the patient's head with the palm of the other hand; thus stretching the dural root sleeves and nerve roots or aggravating radicular pain if the nerve roots are adhered to the foramina. Extravasations, edema, encroachments, and conversion of fibrinogen into fibrin may result in interfascicular, foraminal, and articular adhesions and inflammations that will restrict fascicular glide and the ingress and egress of the foraminal contents. Thus, pain and reduplication of other symptoms during the test probably indicate adhesions between the nerve roots and the capsular structures within the intervertebral foramen.
Spurling's Tests. With the patient in the seated position and the examiner standing behind, the patient's head is rotated and laterally flexed to one side. With the patient actively holding the head and neck in this position, the ex- aminer places a palm on the patient's scalp and vertically strikes it with the other fist. The patient's head is then rotated and laterally flexed to the oppo=- site side, and the test is repeated. If these tests can be tolerated by the patient without undue discomfort, the procedure is repeated with hyperextension added. In radiculitis, sensitive spondylosis, IVD syndromes, and other inflamma- tory or space-occupying conditions in or near the IVF or posterior facets, pain will be increased by the induced compression.
Cervical Distraction Test. With the patient sitting, stand to the side of the patient, place one hand under the patient's chin and the other hand under the base of the occiput. Slowly and gradually lift the patient's head to remove its weight from the cervical spine. Such a maneuver widens the intervertebral foramen, decreases the pressure on the joint capsules around the facet joints, and stretches the paravertebral musculature. If the maneuver decreases pain and relieves other symptoms, it is a probable indication of narrowing of one or more intervertebral foramen, cervical facet syndrome, or spastic paravertebral muscles.
Adson's Test. With the patient sitting, palpate the radial pulse and advise the patient to bend the head obliquely backward to the opposite side being examined, take a deep breath, and tighten the neck and chest muscles on the side tested. The maneuver decreases the interscalene space (anterior and middle scalene muscles) and increases any existing compression of the subclavian artery and lower components (C8 and T1) of the brachial plexus against the 1st rib. Marked weakening or loss of the pulse or increased paresthesias indicate a positive sign of pressure on the neurovascular bundle, particularly of the subclavian artery as it passes between or through the scaleni musculature, thus indicating a probable cervical rib or scalenus anticus syndrome.
Eden's Test. With the patient sitting, palpate radial pulse and instruct the patient to pull shoulders backward and throw the chest out in a "military posture" and to hold deep inspiration as the pulse is examined. The test is positive if weakening or loss of pulse occurs, indicating pressure on the neurovascular bundle as it passes between the clavicle and the 1st rib, thus a costoclavicular syndrome.
Wright's Test. With the patient sitting, the radial pulse is palpated from the posterior in the downward position and as the arm is passively moved through an 180* arc. If the pulse diminishes or disappears in this arc or if neurologic symptoms develop, it is suspect of pressure on the axillary artery and vein under the pectoralis minor tendon and coracoid process or compression in the retroclavicular spaces between the clavicle and 1st rib, thus a hyperabduction syndrome.
Vertebrobasilar Artery Maneuvers.
NOTE: This 2nd portion of George's Test (hyperextension and rotation) is no longer recommended. It is included in this section for its historical significance only.
(2) If palpatory and auscultory signs are negative in the neutral position, the patient is asked to slowly rotate and hyperextend the neck first in one direction and then the other to place a motion-induced compression on the vertebral arteries. Positive signs include dizziness, faintness, nausea, nystag- mus, vertigo, and/or visual blurring.
Other Pertinent Tests
George's Tests. With the patient seated, blood pressure and the radial pulse rate are taken bilaterally and recorded. Stenosis or occlusion of the subclavian artery is suggested when a difference of 10 mm Hg between the two systolic blood pressures and a feeble or absent pulse is found on the involved side. Even if these signs are absent, a subclavian deficit may be exhibited by finding auscultated bruits in the supraclavicular fossa.
Traction Test. With the patient seated and the arm held in the anatomical position, the radial pulse is determined while traction is firmly applied to the patient's wrist. If a decreased pulse is found on one side but not the other, a cervical rib should be suspected on the side of the decreased pulse.
Swallowing Test. The seated patient is asked to drink some water. If a pharyngeal lesion is ruled out (eg, tonsillitis), painfully difficult swallowing may suggest a space-occupying lesion at the anterior aspect of the cervical spine (eg, abscess, tumor, osteophytes, etc).
Brudzinski's Test. With the patient in the relaxed supine position, the examiner's slowly flexes the patient's neck toward the chest. If a spinal cord inflammatory process (eg, meningitis) is present, the neck will become painfully rigid and the patient will automatically flex the knees to lessen the traction forces being placed on the cord. Meningeal irritation is rarely seen in sports; however, this does not eliminate the possibility of a professional or amateur athlete becoming involved with such a disorder. Also see Kernig's and Soto-Hall's tests.
Valsalva's Maneuver. The seated patient is asked to bear down firmly (abdominal push), as if straining at the stool. This act increases intrathecal pressure, which tends to elicit localized pain in the presence of a space-occupying lesion (eg, IVD protrusion, cord tumor, bony encroachment, etc) or of an acute inflammatory disorder of the cord (eg, arachnoiditis). Coughing will produce the same effect under like circumstances.
Bikele's Test. The seated patient is asked to raise the arm laterally to a horizontal and slightly backward position, flex the elbow, and laterally flex the neck to the opposite side. If active extension of the elbow, which stretches the brachial plexus, produces resistance and increased cervicothoracic radicular pain, the test is said to be positive for a nerve root or spinal cord inflammatory process (eg, brachial neuritis, meningitis).
Bakody's Test. The seated patient is asked to raise the arm laterally to a horizontal position, flex the elbow, and then place the open palm upon the top of the head. This maneuver should relieve traction on the ipsilateral lower cervical roots and offer relief of nerve root irritation in cases of an IVF syndrome.
Soft-Tissue Injuries of the Posterior Neck
Contusions in the neck are similar to those of other areas. They often occur to the cervical muscles or spinous processes. Painful bruising and tender swelling will be found without difficulty, especially if the neck is flexed. Phillips points out the necessity of normally lax ligaments at the atlanto-axial joints to allow for normal articular glidding, thus making tonic muscle action the only means by which head stability is obtained.
Strains (1–3 Grades) or indirect muscle injuries are common, frequently involving the erectors. Flexion and extension cervical sprains are also common in sports (1–3 Grades), and usually involve the anterior or posterior longitudinal ligaments, but the capsular ligaments may be involved. In the neck especially, strain and sprain may coexist. Severity varies considerably from mild to dangerous. Anterior injuries are more common to the head and chest as they project further anteriorly, but a blunt blow from the front to the head or chest may result in an indirect extension or flexion injury of the cervical spine. Many cervical strains heal spontaneously but may leave a degree of fibrous thickening or trigger points within the injured muscle tissue. Residual joint restriction following acute care is more common in traditional medical care than under mobilizing chiropractic supervision.
Cervical sprain and disc rupture are associated with severe pain and muscle spasm and are more common in adults because of the reduced elasticity of supporting tissues. Pain is often referred when the brachial plexus is involved. Cervical stiffness, muscle spasm, spinous process tenderness, and restricted motion are common. When pain is present, it is often poorly localized and referred to the occiput, shoulder, between the scapulae, arm or forearm (lower cervical lesion), and may be accompanied by paresthesias. Radicular symptoms are rarely present unless a herniation is present.
Diagnosis and treatment are similar to that of any muscle strain-sprain, but concern must be given to induced subluxations during the initial overstress. Palpation will reveal tenderness and spasm of specific muscles. In acute scalene strain, tenderness and swelling will usually be found. When the longissimus capitis or the trapezius are strained, they stand out like stiff bands.
Rust's Sign. A seated patient is asked to lie back to a recumbent (supine) position. A positive sign is seen when the patient automatically places the palm of one hand behind his neck to support the cervical spine. This sign is thought to be indicative of a lesion leading to weakness in the cervical flexors.
Extension Injuries. When the head is violently thrown backwards (eg, whiplash), the damage may vary from minor to severe tearing of the anterior and posterior ligaments. Severe cord damage can occur which is usually attributed to momentary pressure from the ligamentum flavum and lamina posteriorly, even without roentgenographic evidence. A facial injury usually suggests an accompanying extension injury of the cervical spine as the head is forced backward. Management of minor injuries requires reduction of subluxations, traction, physiotherapeutic remedial aid, a supporting collar for 10–12 weeks, and graduated therapeutic exercises.
Flexion Injuries. Slight anterior subluxation is usually not serious, but neurologic symptoms may appear locally or down the arm. Disc degeneration may follow, leading to spondylosis. An occipital injury usually suggests an accompanying flexion injury of the cervical spine as the skull is forced forward. Management is similar to that of extension injuries except required support is often shorter (6–8 weeks).
Torticollis, Spasms, and Similar Disorders. Wry-neck spasm (tonic, rarely clonic) of the sternocleidomastoideus and trapezius may be due to irritation of the spinal accessory nerve by swollen glands, abscess, acute upper respiratory infections, scar, or tumor, but it more often occurs from traumatic cervical subluxations or idiopathically in "rheumatic" or "nervous" individuals. The muscles are rigid and tender, the head tilts toward the spastic sternocleidomastoideus, and the chin is rotated to the contralateral side. Common trigger points involved in "stiff neck" are in the trapezius (usually a few inches lateral to C7) or the levator scapulae and splenius cervicus lateral to C4–C6 cervical processes. These points are often not found unless the muscle is relaxed during palpation.
Wry neck may also be the result of subdiaphragmatic irritation being mediated reflexly into the trapezius and cervical muscles. Subclinical visceral irritation is often the factor involved.
Dislocations of upper cervical vertebrae cause a distortion of the neck much like that of torticollis. A fracture-dislocation of a cervical vertebra will produce neck rigidity and a fast pulse, but fever is absent. Local and remote trigger points are frequently involved. In suspicious cases, the neck should always be x-rayed before it is examined. Neck rigidity may also be the result of a sterile meningitis from blood in the cerebrospinal fluid. Thus, if a 3
patient has slight fever, rapid pulse, and rigid neck muscles, subarachnoid hemorrhage is suspected. Lateralizing signs are often indefinite.
Management. The correction of any spinal subluxation-fixation complex should never be attempted by the unskilled. In this context, Carrick wisely warns that
Isotonic exercises are useful in improving circulation and inducing the stretch reflex, especially in the cervical extensors. These exercises should be done supine to reduce exteroceptive influences on the central nervous system.
Peripheral inhibitory afferent impulses can be generated to partially close the presynaptic gate by acupressure, acu-aids, acupuncture, or transcutaneous nerve stimulation. Most authorities feel deep sustained manual pressure on trigger points is the best method, but a few others prefer brutal short-duration pressure (1–2 sec). Deep pressure is contraindicated in any patient receiving anti-inflammatory drugs (eg, cortisone) as subcutaneous hemorrhage may result. The effects of cervical traction are often dramatic but sometimes short lived if a herniated disc is involved. In chronic cases, relaxation training with biofeeback is helpful.
During rehabilitation, a cervical pillow is recommended to provide proper postural support while sleeping. Grade 2 injuries should invariably be provided with an immobilization collar to provide support assistance and protection during the early stages of healing. This support should remain until pain-free motion is obtained. Any activity that induces discomfort should be avoided.
Nerve Stress
"HOT SHOTS" AND BRACHIAL PLEXUS TRACTION
After lateroflexion injuries of the neck, a sharp burning pain may radiate along the course of one or more cervical nerves, the result of nerve contusion due to stretching. Scalenus anticus syndrome may be exhibited. This is often referred to as a "hot shot" or "pinched nerve" by players and sports writers. Recurring injury is common, especially in football from "spearing". The syndrome is also seen in wrestling, squash (sidewall collision), and collisions in basketball.
Immediate pain may radiate to the back of the head, behind the ear, around the neck, or down towards the clavicle, shoulder, arm or hand. There are frequent arm paresthesias, severe arm weakness if not lack of active motion, often decreased biceps and triceps reflexes, forearm numbness, and cervical movement restriction. These signs and symptoms may disappear and reappear with greater severity. Roentgenography may show spur formation on cervical vertebrae.
If the symptoms appear on the opposite side of the forceful bending, undoubtedly a nerve has been "pinched" within the powerful muscles dorsal to the sternocleidomastoid. If this be the case, symptoms usually subside in a few minutes with only slight residual tenderness and paresthesia which disappear within a few hours. On the other hand, if symptoms appear on the same side as the direction of the forceful bending, deep skeletal injury such as fracture, dislocation, severe rotary subluxation, or nerve compression may be involved.
Prevention of aggravation requires correction of associated subluxations, strengthening cervical muscles, wearing a plastic roll within a stockinet as a cervical collar or applying a Thomas-type collar, and avoiding dangerous techniques of play.
A similar but more severe nerve injury common in sports is injury to the brachial plexus or its roots which is usually caused by a fall on the shoulder, a blow to the side of the neck, forceful arm traction, or a combination of these mechanisms. The injury is essentially caused by acute shoulder depression which stretches the brachial plexus, especially in the supraclavicular area. The effect may be root tear near the vertebral foramen, spinal cord damage, duralcuff leaks of cerebrospinal fluid, and/or vertebral fracture or dislocation. But such severe manifestations are rarely seen in well-conditioned athletes where the picture is usually limited to pain radiating into the arm and/or hand.
THE STINGER SYNDROME
Albright describes the "stinger" syndrome as an apparently mild athletic brachial plexus injury that reflects a transient radiculopathy at the time of impact. Football "spearing" and head butting are common causes. The injury usually occurs when the neck is forcibly hyperextended and laterally flexed, and symptoms can usually be precipitated in this position during examination.
The condition is initially felt as a painfully severe electrical shock-like dysesthesia that extends from the shoulder to the fingertips. This feeling passes within a few moments and is replaced by sensations of numbness and upper extremity weakness that may last from a few seconds to several minutes.
The most common site of injury is at the C5 or C6 root level; and because of this, the most persistent sign will be weakness of the proximal shoulder muscles. An initial attack rarely leaves residual neurologic symptoms. Repetitive injuries of this nature, however, tend to have an accumulative effect that may lead to axonotmesis and chronic muscle weakness, which may take up to 6 months for full recovery.
The most common lesion associated with the stinger syndrome is cervical sprain with traumatic compression neuritis. Infrequently, an acute cervical disc rupture or a spontaneously reduced hyperextension dislocation may be associated. These later disorders are far more serious and usually require hospitalization until the severity of the injury can be properly assessed.
TRIGGER POINTS
The cervical and suprascapular areas of the trapezius frequently refer pain and deep tenderness to the lateral neck (especially the submastoid area), temple area, and angle of the jaw. The sternal division of the sternocleidomastoideus refers pain chiefly to the eyebrow, cheek, tongue, chin, pharynx, throat, and sternum. The clavicular division refers pain mainly to the forehead (bilaterally), back of and/or deep within the ear, and rarely to the teeth. Vapocoolant sprays to isolated sites often produce rapid spasm reduction of affected areas.
Vertebral Artery Deflection
The vertebral artery is a captive vessel from C6 upward. Extremes of rotation and flexion occur at the upper cervical region, but the four normal curves in the vertebral artery help to compensate for neck movements. Deflection may be caused by any stretching or elongation of the artery during neck injury. In later years, it is commonly associated with bony spurs from covertebral joints or grossly hyperplastic posterior vertebral articulations from arthrosis.
In discussing this situation, Smith explains that extension of the cervical spine allows the tip of the superior articular process of the posterior joint to glide forward and upward. If sufficiently hyperplastic, the motion may cause encroachment on the vertebral artery and/or the intervertebral foramen. Deflection of the artery and any resulting symptoms are exaggerated by rotation and/or extension of the neck. As a result of pressure against the artery, there may be temporary lessening in the volume of blood flow. Atheromatous changes may occur later within the vascular wall. Symptoms (the Barre-Lieou syndrome) include headache, vertigo, nausea, vomiting, nystagmus, and suboccipital tenderness, which may be exaggerated by cervical extension. Sometimes symptoms are aggravated by dorsal extension and relieved by forward flexion with cervical traction.
The vertebral nerve has its origin in the middle cervical sympathetic ganglion, and it offers vasomotor control over the vertebral artery. The Barre-Lieou syndrome is thought to be the result of vertebral nerve irritation that causes a circulatory impairment in the area of the cranial nuclei, especially those of the trigeminal and auditory nerves.
EDITOR'S NOTE: The following test involves some level of risk to the patient, because rotation exerts a small amount of traction to the Vertebral Artery. Before using tests of this nature, you would benefit from reading the whole introducory section at the top of our Stroke and Chiropractic Page, and focusing on the section titled the 5 D's and the 3 N's
Barre-Leiou's Test. The seated patient is asked to slowly but firmly rotate the head first to one side and then to the other. Crawford reports that transient mechanical occlusion of the vertebral artery may be precipitated by simply turning the head, and this phenomenon is attributed to the compressive action of the longus colli and scalene muscles on the vertebral artery, just prior to its course through the IVF of C6. A positive sign in Barre-Leiou's test is exhibited if dizziness, faintness, nausea, nystagmus, vertigo, and/or visual blurring result, indicative of buckling of the vertebral artery.
Roentgenologic Considerations. When the vertebral bodies of the mid-cervical region are involved, the process of vertebral artery deflection may be visualized either by oblique or A–P projections. Smith feels stereoscopic studies are especially valuable. The mid-cervical region shows a predilection for this process. An aneurysm-like condition occurs not uncommonly within the cancellous lateral mass of C2. The tortuosity is visualized in both A–P and lateral views. Since the erosion develops slowly, there is a radiolucency surrounded by a white curvilinear line in the osseous structures adjacent to the vertebral artery. The significance of the erosions is the implication of vessel wall changes, but these erosions may be mistaken for the results of tumor pressure or other destructive processes involving bone.
Cervical Disc Herniation
Degenerative Disc Disease. The cervical spine is readily subject to degenerative disc disease because of its great mobility, regional biomechanical stress, and because it serves as a common site for various bony congenital defects. Bone changes are more common posteriorly in the upper cervicals and anteriorly in the lower cervicals. Cervical degenerative changes can be demonstrated in about half the people at 40 years of age and 70% of those at 65 years, many of which may be asymptomatic.
Management. Adjustive treatment consists of specific manipulation performed with manual traction at the involved motor units to free impinged synovial fringes and reduce intra-articular subluxations and disc displacement, but this should never be performed with the neck in extension. Therapy includes immobilization of the neck with a cervical collar, sleeping with the head between sand bags or in traction, heat (diathermy, infrared, moist hot packs), massage, ultrasound to cervical paraspinal muscles, and periodic bed rest with cervical traction (10–20 lb). Supplementation with 140 mg of manganese glycerophosphate six times daily has proven helpful. Refer for radical treatment if one of the following occurs:
(2) attacks reappear after a short period;
(3) severe nerve-root compression with paralysis is indicated by muscle wasting and/or a sensory deficit has developed.
Spinal Cord Injury
While only about 6% of spinal cord injuries occurring within sports result in permanent paralysis, even this number is unacceptable inasmuch as many are preventable. Most injuries are caused by extreme flexion where subluxation, fracture and dislocation may be associated. Hemorrhage may occur at the site with the same reaction as brain injury (liquefaction, softening, disintegration). Congenital fusions and stenosis may predispose a child to spinal cord trauma during a sporting activity.
There are direct and indirect classes of injuries:
On-Field Evaluation. Schneider warns that the initial examination of a player on the field with cord damage can be quite deceiving. Rarely is a deformity palpable in a muscular athlete. If cord damage has occurred, the player may complain of little or no pain even if paralysis or sensory loss are present. See Table 21.2.
Bradburne's Sign (Thorburn's position). During the acute stage of cervical cord contusion, compression, or shock (with or without vertebral fracture), a sign of spinal cord damage in the area of C5 and C6 is exhibited by bilateral abduction of the arms and flexion and external rotation of the forearms.
Table 21.2. Quickly Determined On-the-Field Cord Signs
Injury
Level Paralysis Loss of Pain to Pin Prick
C3–C4 Trunk, extremities, Below clavicle, upper extremities
diaphragm
C4–C5 Arms, lower extremities, Numbness to the level of the outer
trunk, only abdominal border of the upper extremity between
breathing the shoulder and elbow
C5–C6 Fingers, impaired Thumb and index finger
arm extension
C6–C7 Impaired grasp, weak Middle finger, radial half of ring
elbow flexion and finger
extension, loss of
finger spread
 |
A pathologic loss of the normal anterior curve of the cervical spine, characterized by a straightening of the spine, results in mechanical alteration of normal physiologic and structural integrity. The condition occurs more frequently after the age of 40, and the sexes appear equally affected. The cause is usually the result of trauma-producing whiplash injury, herniated disc, subluxation, dislocation, fracture, or ligamentous injury. Torticolis, arthritis, malignancy, tuberculosis, osteomyelitis, and other pathologies may be involved.
Symptoms and signs include headaches (occipital, occipital-frontal, supraorbital), vertigo, rigidity due to cervical muscle spasm, limited extension and flexion, tenderness elicited on lateral C4–C6 nerve roots, neuritis involving branches of the brachial plexus due to nerve-root pressure, hyperesthesia of one or more fingers, and loss or lessening of the biceps reflex on the same or contralateral side. In rare cases, the triceps reflex may be involved. One or more symptoms are frequently aggravated with an abnormal position of the head such as during reading, sleeping, or driving.
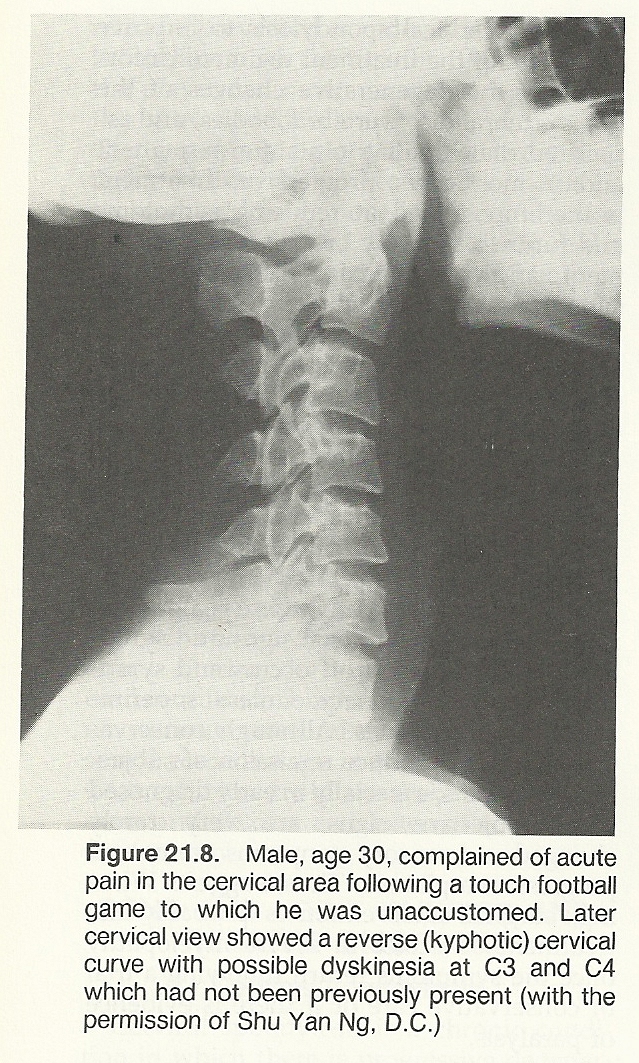
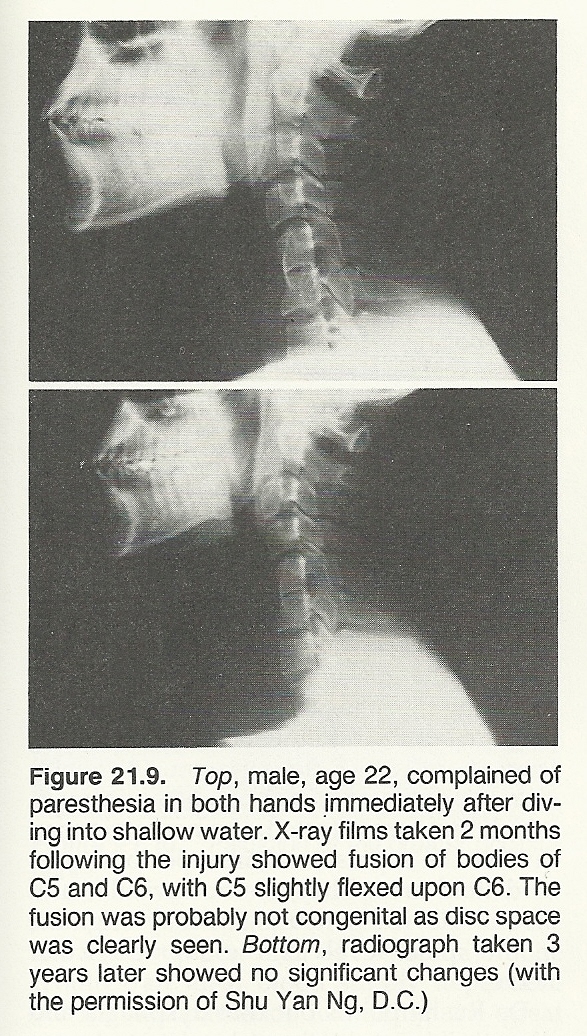
Roentgenographic Considerations. Rehberger reports the typical radiographic findings to include loss of cervical curve with straightening of the cervical spine (78% cases), anterior and posterior subluxation on flexion and extension views, narrowing of intervertebral disc spaces at C4–C6 (46% cases), discopathy at the affected vertebral level as the injury progresses, and osteoarthritic changes which are often accompanied by foraminal spurring.
Case Management and Prognosis. Specific correction of offending vertebral subluxation(s) should be accomplished. Adjuctive care includes massage, intermittent traction, and methods to reduce muscle spasm such as ultrasound, diathermy, hydrocolator packs, reflex spinal techniques, and a rolled towel placed under the neck in the supine position to increase the cervical curve. The individual should be instructed to sleep without a pillow. Cervical muscle reeducation is quite helpful. Rehberger feels that the prognosis is excellent if the condition is treated early and the case is not complicated by fracture or dislocation, but guarded if the trauma is severe. In cases of minimal cervical discopathy, symptomatic relief can be expected. Prognosis is poor in advanced degenerative osteoarthritis.
Cervical Rib
Anomalous development of extra ribs in the region of the cervical vertebrae may be a single unilateral rib, be bilateral, or be multiple bilaterally. The condition is usually seen at C7, and the cause is a variation in the position of the limb buds. It may vary from a small nubbin to a fully developed rib. A small rudimentary rib may give rise to more symptoms than a well-developed rib because of a fibrous band attached between the cervical rib and sternum or 1st thoracic rib. Incidence is more frequent in females in the ratio of 3 to 1.
A cervical rib arising from C7 and ending free or attached to the T1 rib appears in the neck as an angular fullness which may pulsate owing to the presence of the subclavian artery above it. It rarely produces symptoms, often encountered when percussing the apex of the lung. The bone can be felt behind the artery by careful palpation in the supraclavicular fossa and demonstrated by roentgenography. Pain or wasting in the arm and occasionally thrombosis may occur.
Differentiation. Symptoms usually occur at age 12 or later, after the ribs have ossified. Two groups of symptoms are seen, those of scalenus anticus syndrome and those due to cervical-rib pressure. The symptoms of cervical rib and scalenus syndrome are similar, and the scalenus anticus muscle is the primary factor in the production of neurocirculatory compression whether a cervical rib is present or not. When symptoms are presented, they are usually from compression of the lower cord of the brachial plexus and subclavian vessels such as numbness and pain in the ulnar nerve distribution. Pain is worse at night because of pressure from the recumbent position. Pain of varying intensity, tiredness and weakness of the extremity, finger cramps, numbness, tingling, coldness of the hand, areas of hyperesthesia, muscle degeneration in the hand, a lump at the base of the neck, tremor, and discoloration of the fingers are characteristic. Work and exercise accentuate symptoms, while rest and elevation of the extremity relieve symptoms.
Adson's and other like signs will be positive. The 4th and 5th decades mark the highest incidence, probably because of regressive muscular changes. Trauma is a common factor in sports. Aneurysms of the subclavian artery are rare. Differential diagnosis must exclude infectious neuritis, arthritis of the shoulder joint, cervical arthritis, subachromial bursitis, deformities, and cardiac disease. Compression of nerve tissue results in numbness, pain, paralysis, and loss of function. Compression of vascular structures results in moderate pain, edema, swelling, and obstruction of circulation resulting in clotting within the vessels with possible consequent infarction in the tissues supplied. These unilateral phenomena are limited to the cervicobrachial distribution.
The etiologic theories of the cervicobrachial syndrome are compression of the nerve trunks, trauma to nerve trunks, injuries to the sympathetic and vasomotor nerves, trauma to the scalenus anterior muscle, embryologic defects, postural or functional defects, narrowing of the upper thoracic cap as a result of adjacent infections or anatomic defects, acute infection producing myositis, intermittent trauma to the subclavian artery, or a cervical rib.
Case Management. It has been Claypool's experience that some palliative relief can be obtained in some cases by correction of posture, gentle manipulation of the upper dorsal and lower cervical spine, cervical traction and other relaxing physiotherapy. Those cases which don't respond to conservative treatment require surgery, and those cases treated conservatively usually show a recurrence of symptoms periodically.
Cervical Fractures
Fractures of the cervical spine are usually the result of blows, falls, or vehicular accidents. Most cervical fractures are characterized by neck pain that tends to radiate into the trapezius and upper extremities. The neck is rigid because of a protective spasm. Localized tenderness, upper extremity motor and sensory disturbances, and easy fatigue of involved musculature is common. Referred pain may radiate to the scalp, and upper extremity pain and paresthesiae may be present. In many cases, however, the patient will be asymptomatic except for mild symptoms.
Fractures and Dislocations of the Atlas
Atlanto-occipital dislocations, often bilateral, are usually quickly incompatible with life. Any severe subluxation in the upper cervical area can lead to quadriplegia or death, often with little warning and few symptoms to differentiate it initially from a mild strain. Thus, it is always better to be extra cautious (and be accused of being overly concerned in mild injuries) to insure against a possible disaster. Signs and symptoms vary from subtle to severe pain and gross motor involvement. Tenderness may be acute over the posterior atlas, aggravated by mild rotation and extension.
Classes. There are three major types of severe injury, all of which are serious:
(1) The atlas may displace on the axis and fracture the odontoid process. The patient usually survives if extreme care is taken in transportation to the hospital.
(2) A vertical blow may split the atlas and force the lateral masses outward, disrupting the ring. Severity depends upon fragment displacement relative to the cord and vital tissues.
(3) If the odontoid is displaced posteriorly, the situation is usually fatal because of injury to the cord. The spontaneous fusion of C1 to the occiput is always a potential complication.Roentgenographic Considerations. In C1–C2 dislocations, C1 often displaces anteriorly relative to C2. This will alter a line connecting the cortices of the anterior parts of the spinous processes from C1 to C7, unless the process of C2 is fused with the occiput or congenitally short. If this is suspected, flexionextension views or a C1–C2 tomogram should be considered.
The atlas may be fractured on the posterior arch, ring, or anterior arch. Of all atlantoid fractures, most literature states that those of the posterior arch are the most common yet easily overlooked as the displacement is usually mild. The common site is at the narrowest portion just posterior to each lateral mass. The typical mechanism is hyperextension with compression of the posterior atlantal arches between the occiput and axis pedicles. Retropharygeal swelling is usually absent, and oblique views are often necessary for demonstration. Ring fractures are frequently produced by blows on top of the head where forces are dispersed laterally, fracturing the arches of the atlas and spreading them sidewards. Overhang of the atlantal lateral masses and widening of the paraodontoid space will be associated. Most authorities state that fractures of the anterior arch are rare, mininimally displaced, usually comminuted, and frequently require tomography to be detected. However, Iversen/Clawson feel that fractures to the anterior arch are quite common and found either in the midline or just lateral to the midline.
Fractures and Dislocations of the Axis
Odontoid fractures are often produced by severe forces directed to the head, and the direction of force usually determines the direction of displacement.
Suboccipital tenderness may be present. A severe extension force may fracture the odontoid at its base, with possible odontoid posterior displacement. The danger of cord pressure is great. Open-mouth views, flexion-extension x-ray views, or tomography may be necessary for accurate determination.
Roentgenographic Considerations. The atlantal-dens interval should be 3mm or less in adults even during cervical flexion. The interval is slightly more (eg, as much as 4 mm during flexion) in children under the age of 8 years. Many years ago but still applicable, Anderson/D'Alonzo classified fractures of the axis into three types:
Type I: Avulsion of the upper part of the odontoid (rare).
Type II: Fracture through the base of the odontoid at or below the level of the superior articular facets of the axis. This is the most common type of axial fracture, and the cruciate ligaments on the posterior aspect of the odontoid may remain intact. Occasionally the odontoid will not be displaced but slightly angulated as a result of a toggle effect on flexion-extension films. This type fracture is quite unstable and leads to nonunion.
Type III: Fracture of the body of the axis. Displacement may not occur. A small bone chip separated from the anterior-inferior rim of the axis at the point of rupture of the anterior longitudinal ligament may be a clue. About 36% of these fractures occur through the cancellous bone of the body of the axis, are stable, and heal without difficulty.
Care must be taken not to confuse odontoid nonunion with os odontoideum. In os odontoideum, the process is about 50% smaller than normal, round, and separated from the hypoplastic odontoid by a wide gap. The remnant hypoplastic odontoid appears as a hill, forming upward from the slope of the superior articular facets. The fracture line in nonunion is narrow and at or below the level of the superior articular facets, and the process is normal in size and shape.
Hangman's Fracture. This injury by distraction and extension causes fracture of the C2 when the chin is fixed and the forehead is struck. The classic damage is a bilateral fracture through the posterior aspect of the lateral masses and into the intervertebral notch. The posterior elements dislocate in relation to C3 while the anterior elements dislocate in relation to the atlas and skull. Survival is not common; when it occurs (no spinal cord involvement), only minor complaints of local pain, stiffness, and tenderness over the spinous process may be expressed.
Severe C3–C7 Injuries
 |
Cervical fractures and dislocations are not common in sports. They are usually the result of a football pile-up, trampoline, gymnastic, vehicular, or diving accident. Bruises on the face, occiput, and shoulders may offer clues as to the mechanism of injury. Seek signs of vertebral tenderness, limitation in movement, muscle spasm, and neurologic deficits. As in upper-cervical damage, careful emergency management is necessary to avoid paralysis and death. Severe fracture and/or dislocation of any cervical vertebra require orthopedic referral for reduction, bone traction, and casting. Keep in mind that overdiagnosing instability of C2–3 is a common pitfall.
Compression or flexion damage is sometimes seen, but extension injuries (eg, whiplash) are more common. Spinous process fractures usually occur at the C6 or C7 level after acute flexion or a blow to the flexed neck producing ligamentous avulsion. There is immediate "hot" pain in the area of the spinous process which is increased by flexion. Any injury to C6–C7 is difficult to view on film because of overlapping structures.
Compression Fractures. Vertebral body crush fractures are rare, and less common in the cervical spine than elsewhere. Compression fractures of articular processes occur in extension (eg, rear-end whiplash) injuries to the neck. They are not common in sports with the exception of those occurring in divers and are not demonstrable on A–P or lateral films until deformity is severe. Oblique views will often demonstrate them, but they are best seen on "pillar views". The pillar view is taken with the trunk A–P and the head turned 45* to the side, exposure factors are the same as those for the AP exposure. These views, taken bilaterally, will show the articular pillar in profile. Fractures are frequently quite apparent when present.
Flexion Injuries. During forceful cervical flexion, a unilateral facet dislocation and/or fracture may occur with the contralateral side remaining intact, or bilateral dislocation or fracture-dislocation may occur. Unilateral dislocation is more common in the lower cervical area.
Hyperextension "Whiplash" Syndrome. Forceful extension produces tearing of the anterior longitudinal ligament which may coexist with an avulsion fracture at the anterior vertebral bodies. Pedicle fracture or severe posterior subluxation may also occur. Tenderness will usually be shown along the lateral musculature. Upper extremity pain or numbness and restricted cervical motion at one interspace during flexion-extension may be exhibited. Symptoms may be prolonged without demonstrable evidence.
Cailliet points out that it is difficult to visualize a sprain causing rupture of the ligaments of a joint without causing some derangement of the opposing joint surfaces, which by definition is a degree of luxation or subluxation. If a "whiplash" injury is considered a severe sprain, a subluxation injury must be assumed.
Cervical Spinal Percussion Test. The head of a seated patient is moderately flexed while the examiner percusses each of the cervical spinous processes and adjacent superficial soft tissues with a rubber-tipped reflex hammer. Evidence of point tenderness suggests a fractured or acutely subluxated vertebra or localized sprain or strain, while symptoms of radicular pain suggest radiculitis or an IVD lesion.