

|
Chapter 5:
Neuroconceptual Models of Chiropractic
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Basic Principles of Chiropractic Neuroscience”
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated |
Introduction: Explanation of Conceptual Models Classic Concepts of the Chiropractic Subluxation The Stimulus Response Phenomenon Variables Between Stimulus and Perception Variables Between Perception and Response Disease and the Stimulus Response Phenomena Neuroinsult and the Origin of Disease Stimuli and Pseudostimuli Functional Alterations Causes of Disease: Traditional and Current Concepts The Irritation Resistance Concept Habitual Responses Reactions at the Vertebral Motion Unit The Intrinsic Factor (Subluxation) Definitions of Subluxation Irritation—Subluxation—Disease Patterns of Sensation and Selection Causes of Subluxation The Intrinsic Factor Has Two Major Categories Muscular Responsibilities Supporting-Tissue Responsibilities Basic Effects of Spinal Subluxation Immediate Local Effects of Subluxation Mechanical Effects of Subluxation Neurologic Effects of Subluxation The Effects of Bipedism Implied Etiology Implied Diagnosis The Diagnostic Recognition Hierarchy Implied Therapeutics Spinal Subluxation's Clinical Significance Facilitation and the Subluxation: Segmental Rheostats Segmental Facilitation and Subluxation Skin Resistance Findings Conceptual Models Autonomic Imbalance Reflex and Referral Models The "Garden Hose" Theory The Melzak/Wall Gate-Control Theory Trophic Influences of Nerves Interruption of the Neurotrophic Flow Conditioning Influences of Nerves Morphogenetic Influences Role of Nerve in Regeneration Regulation of Gene Expression Bibliography
Chapter 5: Neuroconceptual Models of Chiropractic
Conceptual models are collections of ideas, principles, facts, philosophy, and experiences setting our attitudes and directing our behavior. Ideas and principles include hypotheses and theories (whether right or wrong) that generate new attitudes and behavior, the spirit of invention, and the accessibility to important facts.
The structural spinal fault, the associated nerve involvement, and the ensuing functional alterations comprise classic chiropractic subluxation concepts. In contrast, limited concepts of spinal biomechanical faults, modes of possible nerve involvement, and etiologic rationales of functional changes promote narrow viewpoints, disciplines, and therapeutic approaches, as well as foster empiricism and dogma. Awareness of the varied concepts of structural lesions, neuroinsults, and the causes of abnormal functional changes promotes wider perspective for intuitive practices, multifaceted observations, and fewer practices with reliance on empiricism that is dictated by dogmatic frameworks.
A true stimulus initiates sensory signals at a receptor that produces impulse generation and subsequent afferent conduction. A false stimulus, on the other hand, does not affect a receptor but initiates impulses somewhere proximal to the receptor, along the course of the afferent fiber. This is allowed by an action potential being reached anywhere on the surface of a neuron that results in impulses being generated and transmitted. Impulses thus generated are transmitted in dual directions:
(1) toward the CNS (orthodromic) and
The antidromic impulses, in the sense of going against "normal traffic," interfere with conduction of true sensory information that is being generated at the receptor. In such a situation, the depolarization of antidromic impulse meets the depolarization of the true impulse and cancels both transmissions. Unimpeded antidromic impulses reaching the receptor terminals do not produce resultant changes or effects, simply because they are receptor organs and not effector organs.
Reactions at the Vertebral Motion Unit. A major site of a secondary internal source of sensory stimulation due to and producing physical and functional changes is the vertebral motion unit and its closely associated neurologic components.
The vertebral motion unit, with physical changes produced as explained, is the intrinsic factor recognized in chiropractic as a spinal subluxation. A subluxation, more specifically, is an intrinsic factor of abnormal biomechanical relationships between adjacent anatomical structures that is eliciting and/or contributing to neurologic responses which may clinically manifest as signs, symptoms, functional changes and morphologic alterations of a disease state.
“A vertebra is said to be displaced or luxated when the joint surfaces are entirely separated. Sub-luxation is a partial or incomplete separation; one in which the articulating surfaces remain in partial contact. This latter condition is the one so often referred to and known by chiropractors as subluxations.”
“A subluxation is the condition of a vertebra that has lost its proper juxtaposition with the one above or the one below, or both; to an extent less than a luxation; which impinges nerves and interferes with the transmission of mental impulses.”
“The disrelation of a vertebral segment in association with the contiguous vertebra, or vertebrae, is not visualized as a partial dislocation, as the term implies, but, rather, as a disturbance of normal function of a vertebral segment, which would be better expressed by the term 'Fixation'. Thus, the vertebra in question is within its normal range of motion with its facets continuing to articulate with those of the vertebrae above and below. Such a fixation does not alter the size of the associated intervertebral foramina materially, yet the disrelation, or disturbed function, does have profound significance for the neuromere and nerve trunk.”
“Subluxation: D. D. Palmer insisted that the word subluxation be applied to the intervertebral disrelationships amounting to less than a locked dislocation. He maintained at the same time that there is a functional response within the nervous system resulting from this structural disrelationship.”
“Subluxation: A subluxation is the alteration of the normal dynamics, anatomical or physiologic relationships of contiguous articular structures.”
“Next to the word 'chiropractic,' the term 'subluxation' or 'spinal subluxation' is perhaps the most important and most frequently used word used by chiropractors. The definition of 'subluxation' varies, depending on whether it is viewed from a chiropractic or medical point of view.”
The Intrinsic Factor Has Physical Properties: Two Major Categories Muscle activity provides, along with ligamentous elasticity, postural tone. The ligamentous spine is unstable and unable to maintain erect postural attitudes. Changes in postural attitude (eg, a shift in center of gravity) must be counterbalanced by active muscular efforts perceived and directed by the nervous system. This ongoing muscular activity may result in observable motion or a state of hypertonicity (viz, a muscular resistance to effects of other forces). Muscle activity generates and directs spinal actions of movement. Muscular efforts do the work that produces movement. Under the direction of the nervous system, the work done provides accurate, adequate, and prompt activities of spinal movement. Muscular efforts also provide for asymmetrical static or motion positions during or following an activity. Within a normal range of motion, a state of active equilibrium is provided by excitation and inhibition of muscular efforts within myotatic units of function. Muscular efforts are also required in maintaining asymmetrical postural positions for as long as is necessary. Muscle activity returns parts to symmetrical perfection when desired or after activity is performed. Muscular efforts provide precise and prompt return of symmetry to re-establish spinal stability, regain maximum spinal support, protect the nervous system, and prepare for the next activity. In this context, Steindler reports: "In the ability of the spine to revert to symmetry at will from all asymmetrical positions with promptness and precision lies the characteristic earmark of the normal spine. The inability to do so makes the spine abnormal. The normal spine can, at any point within its range of motion, establish an active equilibrium, can maintain this position at will as long as necessary, and can return to the position of perfect symmetry again, whenever it is desired."
Acute frank trauma. Trauma may result in damaged muscle tissues releasing excitatory substances to pain receptors and initiate an inflammatory reaction. Muscle inflammatory changes in myositis, myofibrositis, and fibromyositis, along with pain, exhibit muscular guarding, edema, circulatory changes, metabolic changes, toxic metabolic end-products, fatigue, scar-tissue formation, and calcium infiltration. During the early stage, there is nociceptive domination of sensory and motor impulse direction over proprioceptive signals and reactions. Microtrauma. Trauma of less magnitude and longer duration may produce the same alterations of spinal muscular efforts as does acute trauma. The process is slower with aches instead of pain and tonicity changes in muscles instead of active guarding, and the overt manifestations may remain subclinical over a long period. Postural compensations. Postural adaptations to minor mechanical faults of support, minor dyskinesia in the ranges of motions, and minor instability of asymmetry of position may produce spinal muscular efforts of self-correction. Proprioceptive sensory awareness to minor structural faults of sectional or segmental deviation prompts spinal muscle activity in an attempt to remove the fault. If successful, the spinal muscle efforts cease with no more proprioceptive irritation. If the effort is unsuccessful, the proprioceptive demands continue and adaptive (compensatory) changes in the spine follow with continued muscular efforts. Biochemical changes. Biochemical alterations can alter muscular efforts of the spine that are required for normal spinal functions. Ischemia of spinal musculature due to functional constriction or actual obstruction of vessels results in varying degrees of circulatory deficiencies in delivery and removal. Psychologic Stressors. Vertebral efforts can be altered by states of psychologic and emotional stress. This is illustrated in the classical posture of profound anxiety. The "worry muscle," the trapezius, is innervated by the spinal accessory nerve (cranial XI). The hypersympathetic activity aroused by stress or fear produces generally increased spinal muscular tone and stiffness and especially targets the trapezius muscle. Prolonged anxiety coupled by hypersympathicotonia (sympathetic dominance) and excessive motor activity could well be an initiating factor altering spinal muscular efforts and the etiology of subluxations.
Primary neuromuscular disease. Primary diseases of the neuromuscular system, either active or inactive with remnants of altered function and structure, can affect spinal muscle efforts. Muscular imbalances at the vertebral motion units, deviations in tone or strength, and proprioceptive embarrassments following disease processes may ultimately alter vertebral position and the quality of motion, and initiate the pathologic reflexes and referrals common to spinal subluxation.
Secondary motor reactions. Secondary motor reactions of the vertebral motion unit musculature to sensory stimulation or irritation of either somatic or visceral origin arising anywhere and having afferent neurons enter the CNS at or near the corresponding cord level may alter spinal muscle efforts. Stimulation of somatic or visceral sensory neurons that enter a given neurologic segment and elicit somatomotor or visceromotor responses may cause responses throughout the various ramifications of that segment as defined in dermatomes, myotomes, sclerotomes, and rudimentary visceral innervations.
The spinal ligaments. Spinal ligament responsibilities are recognized to include allowance for adequate motion, support for static postural attitudes, protection of the spinal cord by restricting motions within well-defined limits, and protection of the spinal cord from trauma of high loads applied at fast speeds. The elastic nature of ligaments provides spinal support and stability with a minimum expenditure of muscle energy. The ligaments readily resist tensile forces and absorb large amounts of energy that are suddenly applied to the spine. Assisted by muscular efforts, they provide a degree of tone and contribute to spinal preload forces. However, when taken beyond normal elastic limits, tone may be lost with resulting lengthening and laxity; and if damaged, scaring and shortening results.
The intervertebral discs. The IVDs have responsibilities of absorbing shock, dispersing forces, providing a fulcrum of balance, bearing weight, adhering vertebral bodies together functionally, limiting ranges of motions, separating vertebral bodies, maintaining height of the IVFs, and contributing to the normal A-P spinal curves. Degenerative changes and aging reduce the passive role of the IVDs in many of these responsibilities.
The apophyseal joints. Restricting the ranges of motions within normal limits, sharing compressive loads of weight bearing, and adding to torsional stiffness are the responsibilities of the posterior facets. By their shape, size, plane of articulation, density, and other joint properties, the facets play important roles in spinal function. Trauma, degenerative joint disease, tropism, and edema adversely affect normal support properties.
The vertebral bodies. The vertebrae centra, along with the IVDs, give structural height, help form the A-P spinal curves, and share the compressive loads of weight bearing. Malformations, compression fractures, and degenerative changes with aging may compromise the responsibilities of the vertebral bodies in spinal functions.
Subluxations following structural alterations of these supporting tissues may be augmented by musculature efforts the vertebral column or be clinically reduced by successful accommodations of response. As the supporting tissues allow subluxations to occur, evidence of segmental malposition, altered kinetics, and neuroinsult may become apparent.
The effects of subluxation may be divided into three major categories: immediate local effects, mechanical effects, and neurologic effects.
An individual's postural attitude is continually unstable; ie, constantly changing; going through adaptations, compensations, alterations, and long-range and short-term reactions. The local, discrete somatic component of the vertebral subluxation is a reflexly organized and sustained biomechanical response to stress, irritation, and excessive demands placed upon the axial structure by the environment and by the total activities, responses, and adaptations of the individual. The differences in our environments, our elected and demanded activities, our patterns of responses, and our special adaptive mechanisms result in individual evidence of stress.
The musculoskeletal component of vertebral subluxation elicits a complex response organized by the CNS that is basically the same for all and extends, to some degree, to all tissues (somatic and visceral) directly related to the corresponding part of the nervous system. The singular stimulus of the somatic component's presence excites sensory elements of proprioception, muscular activity, ligamentous tension, tissue damage, and excessive forces. Culmination of this sensory information is received via the CNS with a complex group of responses organized and directed (requested) through the CNS.
The organization of the responses to vertebral subluxation by the CNS involves sensory, motor, and autonomic responses that interfere with the organization of normal responses to the impact of life situations and environmental factors. The result is that ordinary life situations become stressful and taxing, demand costly reserved bioresources, and reduce protective responses. The triad of nervous system responses is designed to redirect sensory attention, specifically designate motor responses, and focus functional changes.
Because the vertebral subluxation receives this attention from the CNS, other situations and environmental changes encountered during daily activities are either given less attention than would normally be required or they are given excessive attention of alarm by an excessively alert CNS. Either way, additional stimuli, may evoke (elicit) abnormal responses (excessive or inadequate), both of which adversely affect the body's bioresources and protective responses. Initiating factors arise most frequently in the musculoskeletal system because of man's incomplete adaptation to the vertical stance and as part of each individual's postural adaptation to gravitational factors. The segmented vertebral column provides many vulnerable sites for focused stress as it provides the means for postural adaptations. Ideal dispersion of gravitational stresses would occur with total spinal adaptations. However, segmental adaptations are the rule rather than the exception. Segmental adaptations focus stress over the level of tolerance and resistance.
Whatever the mode of initiation of subluxation, its presence sensitizes every disease process to the influence of gravity. The primary subluxation and the secondary subluxation both, by their presence and affect on the nervous system triad, are focal points of stress. Continual or additional gravitational demands magnify the complex responses associated with each subluxation, accelerating the abnormal processes involved.
Local or segmental neurologic and neurovascular disturbances contributing to chronic and acute diseases appear to be a significant part of this general process. The subluxation syndrome includes less stimulus of deep pressure to elicit discomfort, less stimulus required to produce muscular responses, and the recognition of vasoconstriction in tissues innervated by the affected segment.
The rate and degree to which disease develops through the subluxation complex will be determined by the total demands upon the individual and the other determining factors of physical configuration (eg, age, attitude, nutrition, exercise, habits, etc) that influence the total "adequacy to cope." The subluxation inevitably impairs human (resistance) adequacy to some extent, while the importance of the subluxation to the individual is determined by the total adequacy to the total environment and to the life situations encountered and created. The subluxation increases the importance of every stress and defect; ie, every stress and defect render the subluxation more critical. Since the neurologically directed response to local stress, irritation, or excessive demand is basically the same for all subluxations, the potential clinical manifestations will be determined by the segment level (and its associated tissues) involved rather than by the nature of how the subluxation was produced. However, the nature of how the subluxation was produced will help to decide the procedures necessary for its reduction, removal, and prevention of its return. The same process, acting through different levels of subluxation, produces a variety of syndromes. The location and nature of the subluxation determine the target organs and therefore the potential pathology effected.
The location of the subluxation, arising in adaptation to the erect posture, is significantly influenced by habitual postural attitude along with the additional factors of age, physical configuration, etc, with suggested relationships between grouped factors and the incidence of various disease processes. Knowledge of the patterns of postural distortions and subluxations associated with increased incidence of various diseases allows for prediction of possible liabilities. Conversely, various diseases that become clinically evident may strongly suggest levels and patterns of distortion and subluxations. On the basis of the etiologic significance of the subluxation complex just outlined, the finding of a subluxation marks a segment in which or through which the probability of disease is relatively high. The potential probability of adverse effects varies with the subclinical changes, its chronicity, the effects of remissions and exacerbations, and the obvious manifestations (which may be only the effects of exacerbation).
At best, the subluxation is only a vulnerable segment, demanding compensations from the entire organism. Where resources and reserves are adequate for directed accommodations and compensations of response, the subluxation remains only vulnerable.
At worst, the presence of subluxation indicates compensation has already been overtaxed and spent resources and reserves are not available for additional responses of accommodation and compensation or resources and reserves are no longer available to support or maintain the responses of long-standing accommodation and compensation.
Recognition of a vertebral subluxation can reveal early invasion of physiologic reserves and predisposition to disease. With potential probability and subclinical presence of disease, preventive measures can be identified and therapy (subluxation reduction, postural correction) can be initiated before the clinically proven presence of disease.
Spinal subluxations appear to be the silent insidious problems, which leading medical thinkers have concluded need to be sought in apparently healthy people and which are some of the earliest clues to chronic disease. Postural distortions of compensation may be the more silent insidious problem that produce, allow the presence of, or perpetuate the presence of spinal subluxations.
Postural distortions then become an even earlier clue to chronic disease, preceding spinal subluxations. The earliest clue may exist before postural distortions are evident in patterns of excessive, prolonged gravitational stresses even before these stresses produce postural compensations with subsequent spinal subluxation.
1. Recognition of habitual, excessive gravitational stress in an individual's daily activities.
Along with the relief of pain and discomfort, therapeutic attention must obviously be given to all the controllable factors in and around each patient that influence total fitness and resources. This therapeutic approach directs itself to all diagnostic implications (hierarchy of recognition), whereas subsequent implications are directed to the spinal subluxation.
Because of the neuropathology associated with the subluxation increases the vulnerability of the individual to all factors, decisive, critical importance should be directed to the reduction of vertebral subluxations (no matter what level of recognition or stage of involvement).
Since existing subluxations impair the resources of the ill patient for further resistance and recovery, despite their apparent etiologic relation to the illness, no therapy can be complete without the maximum liberation of those resources (plus the provision for additional resources).
Treatment of the vertebral subluxation offers a specific approach to the local neurologic disturbance that is associated with many chronic diseases. Diagnostic implications of subluxation and diseases lead automatically to therapeutic implications in the reduction of subluxation and disease.
The direct participation of the subluxation in basic responses to disturbing influences, its accessibility, and its responsiveness to appropriate chiropractic adjustments render it a direct and strategic factor through which to modify the response (the disease process) and to augment the patient's capacity for response, resistance, recovery, and adaptation.
Since the spinal subluxation both reflects and influences the adequacy of the individual's resources and reserves, responses to the demands of life, vulnerability, and predisposition, early detection and treatment to reduce subluxation offer a direct and systematic approach to the prevention of chronic disease.
The origins of subluxation, the processes with which they are associated, and their implications to health have yet to be fully explored or understood. This is the major challenge before us now. Subluxated segments of the spinal column occur in all individuals, including apparently healthy persons, and the presence of spinal subluxations is universally apparent in all individuals. The variability among individuals is in the number, degree, duration, level, grouping, and peculiarity of the subluxations as well as the individual's ability to accommodate and compensate in respect to their resources and reserves.
Subluxated segments are abnormal in their activity and in their response to various stimuli. Biomechanically, the vertebral subluxation is an alteration in the normal kinetics of the vertebral motion unit as well as a level of focused stresses of abnormal tension, torque, shearing, compression, and other forces affecting the unit's ability to provide required support as a segment in the column. Subluxated segments affect some neurons mediating sensory, motor, and autonomic function by altering their state of excitability. This results in abnormal responses to impulses reaching them from many sources. A vertebral subluxation decreases the function of spinal column to provide protection of the neurologic elements, allowing neural insult at the level of the subluxation. The nature of the resulting neurologic insult can categorically be identified by the effects on various activities under the control of the specialized elements affected. Subluxated segments are susceptible to sustained and exaggerated activity under conditions of daily life. In the state of maximum rest of the body, with no activities occurring and a minimum of sensory stimuli present in the environment, the vertebral subluxation continues to be a source of intrinsic stimuli and generated responding efforts (including efforts to self-correct). The complex responses even in this state are spending resources and taxing reserves of the individual when normal energy consumption should be minimal and body parts should be recuperating and repairing. Subluxated segments alter the normal influence of the neurons on the tissues they innervate and, in turn, the activity of those tissues is altered. The stimulus-response phenomenon mediated by the nervous system depends on the integrity of that system and all its parts. The normal mediating influence can not occur with any degree of diminished integrity of the system or any of its parts.
Subluxated segments are evidence of postural weight-bearing adaptations and compensations. The resulting muscular efforts due to adaptation and compensation are above and beyond the efforts required for normal activities and responses of motion units. Supportive tissues of the motion unit change in response to postural adaptations and compensations. The resulting unequal muscular efforts and changes in the supportive tissue allow or actively produce vertebral subluxation.
Subluxated segments result in the inability to provide adequate support and normal motion in the axial skeleton and inadequately protect the delicate elements of the nervous system from insult. The recruitment of muscular efforts for compensations alters the availability of muscular efforts required for normal motion patterns. Changes in supportive tissues in compensatory responses alter the reliability of support for stability, and the normally allowed ranges of the various motions and the unit's stability are shifted one way or the other. With either excessive motion or stability, the potential of function necessary for protection of the mediating nervous system is compromised.
Subluxated segments displace weight-bearing forces, producing points of focused stress. The requirements for weight-bearing transfer forces from one segmental level to the next and direct the roles of muscular efforts and supportive tissues.
Subluxated segments have altered kinetic patterns that affect the normal range of motion in spinal activity. The normal vertebral segment is allowed activity patterns with normal ranges of axial rotation, lateral bending, flexion, and extension to participate in gross spinal column mobility. When the segment is already in a state of axial rotation, lateral bending, flexion, or extension before activation of the spine, the additional demands may be out of normal ranges resulting in excessive stress damage and/or referral of participation to other elements or segments. Subluxated segments induce spinal accommodations and compensation responses, eventually producing subluxated segments at other levels. In the preactive state of the spine, the vertebrae in a state of rotation, bending, flexion, or extension (subluxated) alter their support base to the vertebrae above and alter their transfer of forces to the vertebrae below. In response, the vertebrae above accommodate or compensate to or for the altered support base. Also in response, the vertebrae below accommodate or compensate to or for the altered transfer of forces from above. Continued or progressive responses above and below produce muscular reactions and changes in supporting tissues of other segments of the spinal column, resulting in subluxation of those segments with all the clinical significant potentials as the originally involved vertebra. Subluxated segments misdirect and tax the individual's bioresources, resulting in diminished reserves. Neurologically, the subluxation can adversely misdirect the effects of the utilization of bioresources for abnormal muscular activity of self correction or accommodation. Statically, the subluxation requires use of reserves to supply additional responses for altered base support and to transfer forces to other supportive tissues. Stressfully, the subluxation places more demand intrinsically for compensation by the system.
1. Facilitated segments of the spinal cord occur in most individuals, including apparently healthy persons.
Summary. Under conditions of normal daily life, there may be steady streams of impulses flowing out of facilitated subluxated segments through sympathetic pathways to structures that they innervate. These impulses and the reactions to them may be beyond or conflict with the demands of homeostatic mechanisms.
Under circumstances in which sympathetic activity normally occurs, the "drive" through facilitated segments is initiated earlier, reaches higher intensities sooner, and is sustained longer than in unfacilitated segments. With conditions of chronic environmental and emotional stress, the potentially dangerous influences will be preferentially focused upon and channeled through the facilitated segments.
1. The greater the invasion of physiologic reserves, the higher the probability that the subluxation will become the decisive factor that limits the adequacy of or misdirecting the use of available resources.
It is important to recognize that the early and progressive manifestations of subluxation may change with time. Prolonged activity may fatigue, resulting in changes from hyperhidrosis to hypohidrosis and vasospasm to vasomotor atonia. Somatosensory → somatomotor reflexes. The simple reflex arc shows a somatosensory stimulation synapsing in the cord to a somatic motor neuron, with consequent somatic muscle reflex actions. This is illustrated by the simple stretch reflex.
Somatosensory → somatosensory referrals. Somatosensory neurons may diverge to other somatic afferent fibers on route, causing their facilitation or stimulation and a resultant interpretation of sensory awareness in a somesthetic area some distance from the original stimuli; therefore, a somatosensory to somatosensory referral of sensation. Viscerosensory → visceromotor reflexes. Afferent visceral sensory neurons arise from internal organs and tissues or from the visceral components of skin, muscles, tendons, ligaments, or other somatic structures that contain viscerosensory receptors . The visceromotor activity that occurs reflexly is dependent upon the nature of viscerosensory stimulation. One simple example might be the presence of a bolus of food in the esophagus exciting stretch receptors of viscerosensory neurons producing visceromotor reflexes of peristalsis, secretion and sphincter contractions. Viscerosensory → viscerosensory referral. There may occur within the cord a referral of viscerosensory stimuli to afferent fibers from other visceral sources that, in turn, elicit visceromotor responses other than those produced reflexly. This is similar to somatosensory to somatosensory referral.
Viscerosensory → somatosensory referral. This is commonly accepted as the mechanism of referred pain, with the afferent viscerosensory fibers diverging to internuncial or first-order somatosensory neurons, causing their stimulation and the perception of pain in a somatic area or structure. Viscerosensory → somatomotor reflexes. Somatic muscular spasm is in response to viscerosensory afferents in appendicitis with abdominal cramps. This may involve viscerosensory to somatosensory referral that, in turn, sets up the somatosensory to somatomotor reflex.
Somatosensory → visceromotor reflexes. Ussher states: "In general, afferent impulses from the skin, the dorsal musculature, or the articulations of the vertebral column are relayed through the cord and emerge as impulses to the viscera." An example might be subluxation of the T6 vertebra that produces somatosensory irritation, resulting in spastic closure of the cardiac sphincter by visceromotor reflexes producing achalasia. Somatosensory → viscerosensory referrals. The distribution of, as well as the character of, referred visceral pain may not only have its origin in an internal viscus, it also may arise from the stimulation of somatosensory, proprioceptive, and pain-conducting fibers in ligaments, musculature, fascia, or other somatic sources.
Korr reports that injection of the C7—T1 interspinous ligament with hypertonic saline solution produced a perfect facsimile of an angina attack, not only pain distributed substernally, pain and radiation to the ulnar surface of the arm, but also hyperalgesia areas, muscular rigidity, and a sense of compression of the chest. Injection of the first lumbar interspinous ligament produced pain of renal colic.
Korr states: "Because of the sustained facilitation of sensory, motor, and autonomic pathways, the lesioned segment acts as a neurological lens, focusing and exaggerating the effects of impulses from many sources upon the tissues innervated from that segment; through the segment the individual is subject to the exaggerated impact of life situations and environmental factors."
In view of the basic tenets of D. D. Palmer's chiropractic philosophy and the concepts presented thus far, it is strongly suggested that a system of healing based on that philosophy, incorporating these concepts, must be as liberal as its therapeutic applications. Further suggested are methods and procedures necessary for the removal and/or correction of mechanical, chemical, and psychic irritations (environmental and constitutional factors of disease) as related to the nervous system as well as removal of the subluxations, which maintain or amplify the neurologic aberrations thus initiated.
Causey/Schoepfle state: "The maintenance of the normal structure and function of peripheral nerve fibers depends on an adequate blood supply to nerve trunks. The importance of the blood supply is illustrated by the observations that for the first 6—8 hours after section of a nerve, the metabolic activities associated with the recovery from fatigue induced by stimulation are more dependent on the blood supply to the fiber than on its connection with the cell body."
Theory. Impulses in large mechanoreceptive fibers and those in small nociceptive fibers converge on specialized nerve cells (T-cells) in the posterior horn of the spinal gray matter. Somatosensory information is processed here and relayed to the brain through ascending tracts.
When the activity in T-cells reaches a high level, it is interpreted as a sign of potential tissue damage and reacted to as if it were painful or threatening (a demand for awareness and action). If this were all, any intense somatosensory stimulation would be painful, but this theory assumes the existence of a "sensory gate."
1. Atrophy of denervation is due to disconnection between neuron and organ rather than the arrest of impulse traffic as seen in cutting the glossopharyngeal nerve on one side. The taste buds (sensory organs and receptors) on the same side of the tongue soon began to dedifferentiate back into nonspecific epithelium, eventually disappearing completely. On reinnervation, redifferentiation was triggered, and complete normal gustatory apparatus was restored. The fact that sensory receptors do not rely on impulse arrival (antidromic impulses) suggests that the degeneration and dedifferentiation were secondary to interruption of neurotrophic flow and that the subsequent regeneration and differentiation was also under the influence of neurotrophic substances.
Boyd WA:
by Gary C. Johnson, DC
This chapter offers a review of the highlights of preceding chapters that concern subluxation syndromes and forms a foundation of thought for following chapters.
INTRODUCTION: EXPLANATION OF CONCEPTUAL MODELS
Scientific facts and our philosophical hierarchy of importance (priority) provide selective (choice) groupings of knowledge and thoughts, comfortably placed in support of our experiences. How we perceive what we do, why we do it, why the results, and how the results occur set attitudes and practice activities and change our minds and activities as new concepts are developed and tested.
CLASSIC CONCEPTS OF THE CHIROPRACTIC SUBLUXATION
To illustrate the variations of concepts on structural spinal faults, the term subluxation can be defined in the areas of static juxtapositions of vertebrae (eg, lateral flexion subluxation, rotation subluxation, anterolisthesis subluxation, etc). Another category is spinal "dyskinesia" with all its potential faults (eg, fixation, altered range of motion, hypermobility, etc). The focal points of structural stress in different postural attitudes can be considered as subluxations or they may produce structural compensations that manifest as subluxations.
The multiple concepts of possible nerve involvement include the subluxation as an intrinsic source of irritation (excitation), a source of impulse generation, a source of interference in impulse conduction, a source of segmental neuronal pool facilitation, and a source of impedance of axoplasmic flow. In the following sections of this chapter, facts and ideas will be presented to support the development of the many conceptual models possible for the "chiropractic subluxation."
The Stimulus Response Phenomenon
Life has classically been described as a stimulus response phenomenon. External and internal changes of the environment act as stimulants that evoke reactions in response to the change. The reactions of the response are meant to keep the organism in harmony with itself and its dynamic external and internal environmental elements. Within certain parameters of the rate and magnitude of responses afforded by the organism, the harmony and equilibrium are usually expected and insured. However, a major class of variables in higher forms of life is also present and can play a major role in the stimulus response phenomenon and the quality of life.
The changes occurring with the stimulus should excite some tissues that, in turn, should excite some afferent neuronal elements. The afferent neurons should transport this information to the CNS for awareness, recognition, and the selection of priority of importance.
The CNS should process the stimulus-generated information and initiate and direct a selected afferent patterned response. The afferent neurons, in turn, should transport the demand information to proper reactive target tissues. To complete the process, the reactive tissue should be acceptable and responsive to the demand and be capable of performance as directed. This response should be timely, accurate, and be of exact duration in harmony to the stimulus.
The "shoulds" in the above scenario suggest the many variables and possible alterations of the elements and mechanisms involved to produce such a stimulus response phenomenon and to the extent that, if the response is appropriate and accurate, it is an astonishing phenomenon in itself!
A given stimulus (ie, an environmental energy change within the parameters of enough magnitude to excite and not too great as to injure the organism) should excite (stimulate) receptor cells of lower threshold to the specific type of energy change. After the stimulus depolarizes the receptor membrane, the generated action potential (impulse) should initiate conduction of the impulse via afferent fibers to the CNS. On arrival, the afferent firings should produce patterns of impulses through multiple synapses and resulting pathways at different rates within the spinal cord and brain.
The final destination of these sensory patterns of impulses in the brain greatly determines the conscious or unconscious perception of the stimulus. This perception of the stimulus should be accurate concerning the stimulus (ie, touch should be perceived as such and not as pressure or pain). The message received at the cortex is a pattern of impulses dispersed in time and space and not just that of a single fiber of a special sensory modality.
Classically, this phenomenon of stimulus sensory perception was simplified by the doctrine of specific nerve energies by M. Muller (1801—1858). This explanation theorized that there were specific receptors of lowered threshold to one particular modality of sensation. In turn, the special receptor activates a neuron having a "private line" to a specific point in the sensory cortex. Excitation of this specific point by a specific fiber in the spatial organization of the cortex identified the type of stimulus perceived more than the character of the actual stimulus.
We are now confronted by more difficult concepts of neurophysiology, moving from the simplistic to the more involved variables present in the stimulus perception phenomenon.
Variables Between Stimulus and Perception
The most obvious variables between peripheral activation and central perception deal with the state of the receptors, the state of the peripheral afferent nerves and their fibers, the state of the cord level sensory neuronal pools, the state of the cord sensory tracts, and the state of the cerebral sensory cortex.
The response of the receptor and the following perception, within limits, depend upon the strength of the stimulus, the rate of stimulus application, and the duration of stimulation. Multiple factors of adaptation, phasic receptors, tonic receptors, recruitment, habituation, sensitization, ionic concentrations, inflammation, degeneration, undifferentiation, and fatigue can alter receptor function and the physiologic role between stimulus and perception.
The role of peripheral afferent nerves and fibers in transmission of messages to the CNS is variable in performing responsibility by biochemical changes, direct stimuli, mechanical deformation, degeneration, regeneration, inflammation, ischemia, and ionic concentrations. Interference with patterned afferent impulse conduction can obviously alter the perception of the stimulus, even to the degree that with no stimulus present at receptor site, midfiber stimulation produces perception of the receptor site plus antidromic depolarization inhibition of the involved receptors to true stimulation.
Perception is influenced by attention with over 90% of stimuli suggested to be ignored as unimportant. The selection of priority perception through a learned process depends on the perception of experiences. Some experiences develop greater attention to certain stimuli; others may block attention. The state of sensory perception also can be altered by fatigue, chemical imbalances, disease processes or their remnants, drugs, and advanced aging processes.
Variables Between Perception and Response
The transfers of information from afferent sensory input through the sensory cortex or lower centers and levels of perception of the stimuli affect the motor cortex or lower centers as patterns of impulses that excite efferent elements of response. Again, memory patterns of learned responses selectively direct the nature of the reaction.
Accuracy, precision, and appropriateness of the response depend on the level(s) of perception, the selection of perception, and continued attention as priority awareness of higher brain levels, as well as the state of the descending tracts, motor neuron pools, anterior spinal nerve roots, peripheral efferent nerves, and the target (reactive tissues).
Altered states of the neuromotor system result in inaccurate, inappropriate, crude, diminished, or exaggerated responses. Timeliness, synchronization, duration, magnitude, and coordination of responses are also variables.
The responses in the simple, primitive concept are reflexes. Many of these simple responses are cord-level controlled. Sensory stimuli enter the cord, diverge, ascend to the brain, or initiate cord-level motor response as reflexes. The descending motor impulses have the major responsibility to either facilitate or inhibit cord-level reflexes.
By facilitation and inhibition reactions, reflexes of multiple-unit reactions become body system activities. This is illustrated by pyramidal tract lesions producing hypotonicity by loss of facilitation and by extrapyramidal tract lesions followed by hypertonicities with loss of inhibition, and spontaneous, aimless, unintentional movements.
Patterns of responses are classically identified as innate reflexes, habitual responses (preferred group of reflexes), special learned responses (practiced reflexes with special directions of responses), and pathologic responses (loss or altered physiologic reflexes and actions).
The variables involved in reflexes and responses are characterized by the state of facilitation or inhibition of the higher centers of the CNS such as motor loss after stroke and the altered state of cord-level neuronal pools with internuncial facilitation and inhibition. The state of the peripheral efferent motor neurons is altered by stages of degeneration or regeneration, mechanical deformation, inflammation, ischemia, and changing ionic concentration.
The state of the neuromuscular junctions depends on the production and release of neurotransmitter substances, ionic ratios, frequencies of repetitive nerve stimulation and stages of fatigue. Finally, the state of the reactive gland or muscle target tissue can be changed as witnessed in ischemic conditions, myositis, and degenerative states.
DISEASE AND THE STIMULUS RESPONSE PHENOMENON
Neuroinsult and the Origin of Disease
Life can be explained as a stimulus-response phenomenon within a homeostatic range of interactions. However, from the preceding explanation of the variables between stimulus and response, it can be concluded that homeostasis is not automatic or guaranteed, or the result of simple phenomena.
"Disease in its beginning is abnormal function. Abnormal function is function out of time and phase with environmental need. Disease, whether of the heart, kidney or brain, is disturbed function, not merely disordered structure," stated William Boyd, the father of modern pathology. The functions related to in this quotation are groups of responses related to the descriptions previously made. Some diseases can be explained by abnormal responses (functions) to stimuli; others can be attributed to normal responses to abnormal stimuli or sensory perceptions (processing).
Stimuli may be too great for an appropriate response (shock), for adequate psychologic adaptation (sudden loss of a loved one with neurotic anxiety and depression), for physiologic response (frost bite), or they may become irritants above the resistance at a given time (resistance fluctuates with many variables).
As it mediates between stimulus and response, the nervous system, with all the variables identified, may not perceive and process sensory signals adequately or correctly. The responses may be directed inaccurately and/or be malcoordinated. The control of various functions in response to changes may not be appropriate. "Many pathological processes, the cause of which had been regarded as foreign to nervous influences, have been found to be in reality entirely dependent on the latter for their origin," wrote Speransky.
Because a given stimulus can be altered by the sensory system (eg, amplified, diminished, diverged, inhibited, facilitated, perceived, or ignored), and a designated response can be altered by the motor system (eg, exaggerated, weakened, synchronized, unsynchronized, prolonged, or shortened) the nervous influences on life processes, functions, structural integrity, biophysics, and energy utilization of the body may seriously compromise the health and welfare of the individual.
Any situation, phenomenon, or condition that interferes with the mediating functions and responsibilities of the nervous system could be initiating or sustaining causes of disease and the associated clinical signs and symptoms of altered functions.
Stimuli and Pseudostimuli
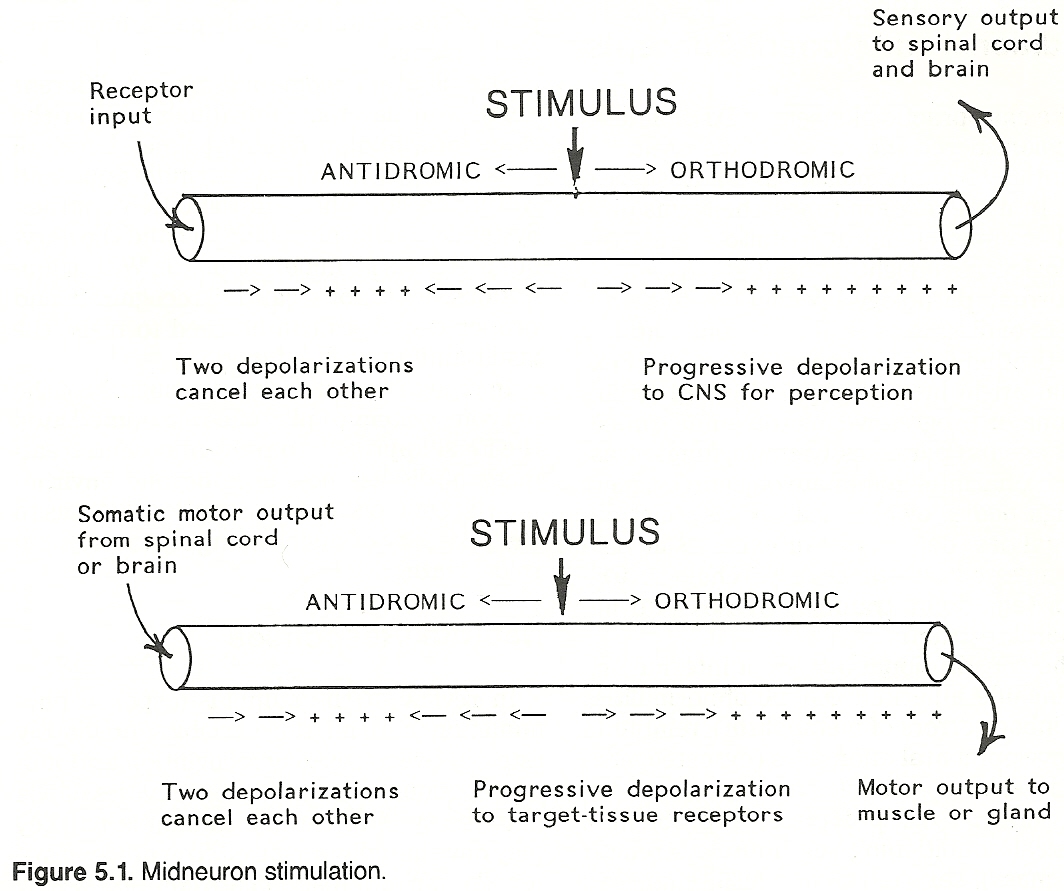
(2) back (distally) toward the receptor (antidromic).
The false orthodromic impulse is transmitted in the normal direction (centrally) to the CNS. On reaching its destination in the sensory cortex or other interpretive centers, false signals are perceived as any other information and recognized as true or real data. The CNS cannot differentiate between actual stimulus-receptor impulses and pseudostimulus (nonreceptor) impulses. Therefore, the false information is processed as true information and passed on to the motor centers to evoke responses to possible nonexisting stimuli of any modality, both somatic or autonomic.
Even if the false sensory information is too weak to produce a response, the impulses thus generated may produce a state of facilitation in the pattern of sensory neuron pathways at the spinal cord and/or higher levels. This inevitably produces lowered thresholds to other subsequent real or false sensory impulses, which results in exaggerated or prolonged responses.
Functional Alterations
In the same manner that false sensory information can be generated midneuronally, so also can response-directed motor efferent impulses be generated and transmitted. Again, these false demand impulses are conducted in opposite directions, orthodromic and antidromic. However, in the case of efferent neurons, the antidromic direction is toward the CNS and the orthodromic is the normal course (directed peripherally) toward reactive target tissue for muscle or glandular action.
The antidromic false impulses (moving against traffic) can either interfere with normal efferent impulses by predepolarization or terminate at the next synapse with no effect. It is presently thought that antidromic impulses cannot jump synaptic clefts or continue to the next higher motor neuron.
False orthodromic efferent impulses travel the same course and produce the same responses as would true motor impulses. The potential tragedy is the exaggeration of responses to no true stimuli and the misdirected responses from the CNS. The normal neurologic influences of inhibition, facilitation, coordination, and timeliness on function may be absent.
The resulting unchecked reactions may produce the syndromes of signs and symptoms of many disease stages. This state could represent the abnormal function referenced by Boyd as the beginning of disease. Abnormally low function could be false inhibitory reactions. Conversely, excessive activity could be the result of false excitatory reactions going unchecked.
Causes of Disease: Traditional and Current Concepts
The chiropractic pioneers of D. D. Palmer's time considered the causes of disease to be essentially trauma, poison, and autosuggestion. In more modern times, the terms physical trauma, chemical irritation, and psychologic stress might be used.
Current pathology broadly classifies the causes of disease as either environmental or constitutional. Environmental factors of external origin include physical injury (frank trauma or progressive microtrauma), infectious agents (parasites, bacteria, fungi, viruses, etc), harmful inanimate objects (eg, inert foreign bodies or chemical toxins), diet abnormalities (deficiencies or excesses in various ingested substances), psychologic irritants (emotional trauma, stresses, and behavioral restraints).
The constitutional factors of internal origin include inherited genetic abnormalities (eg, inborn errors of metabolism), remnants of developmental anomalies (eg, osteogenesis imperfecta), changes from previous disease states (eg, postmeasles problems), physical conditioning (eg, muscle strength and mass), sex (eg, menopausal changes), and age (eg, senile osteoporosis).
In the concept of environmental and constitution factors of disease, the ideal approach to prevention and treatment would be to remove or control the sources of irritation in the patient's environment while simultaneously building resistance through an improved constitutional health status.
The Irritation Resistance Concept
An individual's health status can be viewed as the overall state of function regarding the presence of irritation and the level of resistance. Stimuli become irritants with increased magnitude, duration, quantity, and concurrent combinations. Irritants are stimuli endangering or detrimental to the individual. Resistance is the recruitment of functions (responses) designed to lessen the irritant to a stimulus or to remove the threatening source completely or develop functions of adaptation that reduce the impact of the irritant on body parts, functions, and systems.
Stimuli also become irritants at different degrees in different individuals and in the same individual at different times. Levels of resistance also vary between individuals and within the same individual at different times. Systemic equilibrium is the key, and the nervous system is its major mediator. Within limitations, irritations can be recognized and proper responses can be used to resist the insult and normalize functions.
In recognition of the responsibilities of the nervous system to play the role of mediator, the ideal approach to prevention and treatment of disease now goes beyond environmental controls and constitutional status to the necessity of maintaining sustained neurologic integrity.
Habitual Responses
In review of the stimulus-response phenomenon and all the variables previously listed between sensory recognition and motor reactions, the mediating activities of the nervous system are not as simple as they may have initially appeared.
The processes of recognition and reaction are complicated by the nervous system, which, in reacting to irritations, may establish certain neurologic patterns of response. These patterns may become habitual or self-perpetuating to the extent of producing physiologic and/or structural alterations.
The alterations thus produced, in tandem with the initial neurologic patterns of response, become intrinsic sources of neurologic irritation, generating additional patterns of response with more functional and/or structural alterations. This condition may persist or progress long after the original stimulation (irritation) has ceased. Via positive feedback reflexes and recruitment, the condition may even worsen after removal of the causative factors.
First-stage resultant functional and/or structural alterations can become constitutional stimuli (irritants) demanding awareness and reaction by way of sensory and motor activities. This internal (intrinsic) source of sensory stimulation (irritation), in turn directing motor responses, may be the etiologic factor in the production of signs, symptoms, functional changes, and morphologic alterations associated with various disease entities.
As disease processes progress, the positive feedback circuit continues with the development of more intrinsic sources of sensory stimulation. Thus, more motor responses with chronic syndromes result.
The motion unit can show evidence of physical changes subsequent to the original stimulus-response reactions and become a mechanical source of neuropathologic reflexes and referrals. The primary source may diminish or vanish, leaving the secondary vertebral source actively propagating functions out of time and phase with environmental need. The motion unit also can show evidence of physical changes in normal ranges of daily activity and become a primary internal source of reflexes and referrals with similar adverse effects.
INTRINSIC FACTOR (SUBLUXATION)
The abnormal biomechanical relationships of the motion unit in subluxation may anatomically exist as a static malposition of related structures (counterrotation, etc) or as an alteration of the biokinetic range of motion of the motor unit (hypomobility, etc).
The intrinsic factor may be neurogenic in origin, participating as a habitual response to a distant source of irritation. The subluxation also may originate as a simple biomechanical fault, self-irritating and self-perpetuating. In either case, the effects are similar in potential harm and in need of corrective attention.
Definitions of Subluxation
Following are some selected references that define the term subluxation.
Textbook of the Science, Art and Philosophy of Chiropractic.
Portland, OR, Portland Printing House, 1910.
“A vertebra racked from its normal position ever so little, is rotated around its axis, thereby displacing all its parts proportionately. The relationship existing between bones and nerves are so nicely adjusted that any one of the 200 bones, more especially those of the vertebral column, cannot be displaced ever so little without impinging upon adjacent nerves.”
“A subluxation does not restrain or liberate vital energy. Vital energy is expressed in functional activity. A subluxation may impinge against nerves, the transmitting channel may increase or decrease the momentum of impulses, not energy.”
“A sub-luxation consists of two or more bones, whose articular surfaces have lost in part their natural connection --or in which the articulating surfaces remain in partial contact those which partly preserve their connection.”
![]()
Chiropractic Textbook.
Davenport, IA, published by author, 1927.
![]()
The Neurodynamics of the Vertebral Subluxation, ed 3.
Place of publication not shown, published by author, 1981.
![]()
![]()
Basic Chiropractic Procedural Manual, ed 4.
Arlington, VA, American Chiropractic Association, 1984.
![]()
Biomechanical aspects of subluxation.
In Goldstein M (ed): The Research Status of Spinal Manipulative Therapy. vBethesda, MD, NINCDS Monograph No. 15, US Dept of HEW, 1975.
“The major difference between the medical and chiropractic viewpoint is that chiropractic includes 'neurophysiological disturbances' in the definition of 'subluxation.' This implies that 'subluxation' has a living character which includes both biomechanical and neurophysiological abnormalities. Therefore, any conclusion regarding subluxation that is based solely on the study of cadavers is not acceptable.”
![]()
Irritation-Subluxation-Disease
As a simplistic overview of this section, the following tour of events is offered.
Environmental or constitutional irritation received, transmitted, and mediated by the nervous system produces patterns of habitual responses. This patterned activity can alter function and structure.
A primary site of alteration is the vertebral motion unit, demonstrating abnormal position, faulty kinetics and segmental neurologic changes. The altered motion unit is a spinal subluxation and an intrinsic factor of irritation and reaction, producing a second generation of habitual responses.
The subluxation complex is a site of both stimulation and response. Later responses may continue from the intrinsic factor after the original environmental or constitutional irritations cease. In addition to persisting, these secondary patterns of responses may produce an additional set of functional and structural alterations. With prolonged time and continued cyclic positive feedback-dominating activity, signs, symptoms, malfunction, and morphologic changes of disease states may become apparent. When left unattended for a long duration, these adverse processes may recruit more abnormal responses and become packaged into the manifested syndromes of chronic disease states.
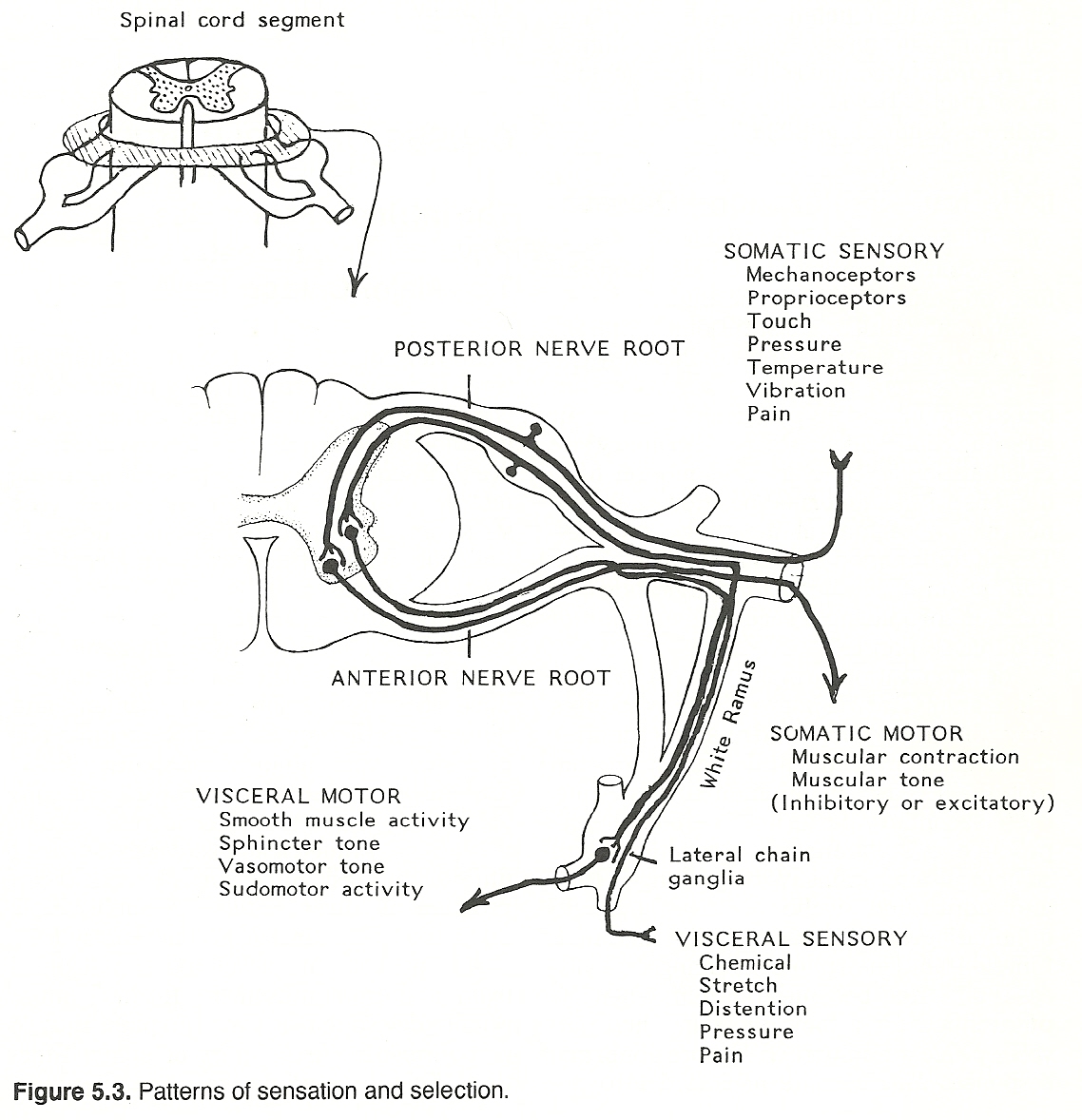
Patterns of Sensation and Selection
Because the triad of the nervous system (sensory, motor, and autonomic) is segmentally organized, the subluxated segment will exhibit clinical evidence of the signs and symptoms of subluxation; eg, segmental tenderness; spontaneous pain; altered activity of segmentally innervated muscles; and vasomotor, sudomotor, and visceral changes of segmental sympathetic innervation.
CAUSES OF SUBLUXATION
In view of the variables of phenomena from stimulus to response as mediated by the nervous system, the initial causes of subluxation are often difficult to identify. However, subsequent to all the possible initiating factors producing the intrinsic factor (the structural/functional deviation of the vertebral motion unit), there are two major classifications of causes.
The first category is an active one of muscular effort. Abnormal muscular responses, usually directed by the nervous system, produce and sustain abnormal positions and motions of the vertebral motion unit. The presence of these abnormal responses generates sensory irritation and motor deviations of the nervous system. Referral, reflexes, and unequal, asymmetrical, excessive, deficient, untimely, aphasic muscular efforts thus can produce all three criteria of subluxation: malposition, dyskinesia, and neuroinsult.
An appreciation of subluxations caused from abnormal muscular efforts is more readily developed in view of spinal muscle responsibilities in support of spinal functions. Spinal functions are commonly identified to include motion, support, and protection. Allowing and generating motion, within certain parameters, of gross movement, sectional movement and segmental activity are obvious spinal functions of design.
Spinal motion is directed by muscular efforts, ligamentous restrictions, osseous architectural forms, and intervertebral disc plasticity. Structural support of form (postural attitude) is a spinal function afforded by muscular efforts, ligamentous restrictions, osseous density, and the intervertebral disc. The protection of the delicate elements of the nervous system is provided as a spinal function of muscular guarding, ligamentous absorption of forces, osseous armature, confinement by the associated IVD, and cushioning by the meninges and CSF.
Muscular Responsibilities
Muscular efforts in support of spinal column function include the following:
These muscular efforts to maintain posture also provide spinal preload forces to segments of much larger magnitude than the physiologic loads of motion that occur during normal activity. Preload forces provide support through stiffness and motion through flexibility. Postural tone and preload, as products of muscular activity, provide for a degree of inactive symmetry. This symmetry of posture provides for added spinal structural support and, in tandem, more protection of the neurologic elements.
Postural tone is also important in providing preparedness of the muscular state for active movement. The strength of contraction is affected by previous activity. Muscular efforts provide direct sensory information generated by contraction and indirectly provide sensory information from resulting changes in muscle fiber tone and length. Combined, this information provides a status report on spinal functions and a data supply for further reactions.
Muscular efforts in support of the spinal functions just outlined may be altered by the following:
All the above changes occur at various degrees posttrauma and alter the ability to perform normal contraction functions. Proprioceptive block and dominant-pain-directed guarding results in the inability to maintain static equilibrium of the postural tone (segmentally, sectionally, or totally) of the spinal system. Muscular reactions also result in the inability of segments and spinal sections to perform in normal ranges of motion (axial rotation, lateral bending, flexion, extension).
The inability of the spine and its parts to return to perfect symmetry also is presented with altered muscular efforts and activities. The malpositions of spinal elements, the altered spinal kinetics of segments and sections, and the neuroinsult to sensory awareness and motor attempts at correction of the muscular reactions to trauma combine to produce such intrinsic factors as "segmental subluxations," "sectional towers," and "spinal distortions."
Prolonged stresses of faulty postural attitudes, habitual activities, and altered spinal biomechanics can manifest as inflammation, edema, circulatory changes, metabolic activity, fatigue, scar formation, and calcium infiltration of muscular tissue. As with acute trauma, altered spinal muscle efforts produced by prolonged microtrauma can produce such intrinsic spinal factors as malposition, dyskinesia, and neuroinsult collectively identified as the "segmental subluxations," "sectional towers," and "spinal distortions," described above.
These on-going muscular efforts along with efforts to perform normal daily activities fragment the spinal system, reducing the activity of some levels or segments while recruiting more activity in other levels or segments. The minor mechanical faults, dyskinesias, and instabilities initiating unequal muscular efforts may progress through these continued efforts to become intrinsic factors of malposition, altered kinetics, and neurologic irritants of segmental spinal subluxations.
Segmental dyskinesia may be amplified by the starting position of the vertebral motion unit. When at rest, the motion unit exhibits a minor fault in resting position, rotation, flexion, extension, and lateral bending, and it is then called on to perform a motion. The predisposed attitude may limit final performance or shift the responsibility to perform to another level. For example, the L5 vertebrae may be rotated 5 degrees to the left at rest.
Axial rotation of the lumbar spine is necessary in a movement and L5 may not be able to contribute without damage to restricting elements or without placing the responsibility at higher levels of the lumbar spine. The abnormal muscular efforts involved in diverting the responsibilities of motion to higher levels may cause the altered position, deranged kinetics, and neuroinsults commonly associated with spinal subluxations.
Segmental biokinetics may be altered by spinal preload. The presence of forces of weight-bearing and the tonic muscular action associated with normal resting and active posture is spinal preload. The weight-bearing forces on a spinal segment are more than the weight of the body above that segment because of spinal ligament and muscular activity or tone.
Preload is responsible along with other elements (eg, strapping ligaments) for segmental stiffness. The spinal stability provided by preload may alter the kinetic range of motion of the vertebral motion unit by an excessive or a diminished amount of preload. The following altered range of motion may result in unequal muscular efforts to induce motion in a stiff segment, or it may add stability to an excessively relaxed segment. These muscular efforts may cause spinal subluxations that exhibit segmental juxtaposition, neuroinsults, and the obvious kinetic faults.
Segmental ranges of motion may be altered by osseous architectural asymmetries of facet tropism or wedged-shaped vertebral bodies, for example. Attempts to perform spinal motions with such structural deviations present may lead to unequal spinal muscular efforts to produce and maintain vertebral subluxation at the level of the abnormal bone position or remote from it.
Habitual motion patterns of the spine or sections of the spine may alter segmental ranges of motion in several ways. Motion patterns may lead to changes in ligamentous resistance sectionally and segmentally, allowing for altered muscular efforts and the various ranges of motions.
Unilateral motion patterns may produce muscular hypertrophy of required muscles and atrophy of unused muscles. Unequal use and subsequent unequal strength of spinal muscles may reduce the responsibilities of those muscles in maintaining position and performing other activities of a segment and thus lead to subluxation.
The transfer of normal spinal forces and added loads to other areas of the spine may result in abnormal ranges of motions as suggested in the event of spinal preload. Segmental forces of shear, compression, tension, and torsion change in different postural attitudes at all levels of the spine.
Different combinations of these loads at various levels produce proprioceptive sensory information, which elicit spinal muscular activity in an attempt to reduce focal points of stress, disperse the forces over larger areas, and redirect the potentially more harmful forces to vectors that produce loads to which the spinal elements are more resistant.
The ensuing muscular efforts to normalize segmental loads may produce the triad of a subluxation in the process. Segmental position, kinetics, and neural neutrality could therefore be easily compromised.
Muscular efforts are also influenced by mechanoreceptor signals from all segments of the spine. Motion and the resultant changes in segmental positioning are constantly producing sensory data. This information is used to analyze angle, velocity, direction, and amplitude of joint displacement by awareness to the amount of or changes in tension.
Dyskinesia of a spinal section or segment produces patterns of mechanoreceptive information and subsequent patterns of spinal muscle reactions. Assuming these patterns of muscular responses are present in a given area and additional activity is required that involves that area, the potential of unequal, asymmetrical, and inappropriate muscular efforts could produce vertebral position changes, kinetic changes, and unnecessary neurologic reflexes or referrals common to the subluxation syndrome. Sensitization, accommodation, denervation, degeneration, or a degree of regeneration of mechanoreceptors also may alter sensory information, motor responses, segmental motion, and produce subluxations.
Spinal motions accompanied by pain perception may lose mechanoreceptive input centrally because of the dominance of pain signals. Muscular efforts, in turn, are primarily concerned with guarding of painful motion. Thus, segmental subluxations may follow the loss of appropriate muscular activity.
Postural compensations to minor spinal instabilities caused by fatigue, incomplete responses to changes in forces and loads, proprioceptive lesions, prolonged static stress, habitual stress patterns of motion, and altered ligamentous tension may incorporate profound muscular efforts of adaptation. The minor instabilities, with time and active muscular responses, may produce major spinal instabilities of subluxation.
In summary, spinal muscle efforts involved in postural compensations to minor biomechanical faults may result in the inability to maintain static equilibrium of postural tone, inability to perform in the normal ranges of motions, and the inability to return to resting symmetry. These deficiencies of function may allow for segmental malposition, aberrant motion, and neuropathologic reflexes and referrals. Segmental deviations become the intrinsic factors of subluxations.
Spinal subluxations become intrinsic sources of irritation with special patterns of responses. The presence of subluxation may precipitate major postural compensations, distortions, and health liabilities.
Heat, oxygen, carbon dioxide, glucose, lipids, buffers, phagocytes, calcium, potassium, and sodium concentrations and their availability to muscle tissue can have profound effects on contractility and relaxation. Abnormal concentrations may change peak tension, periods of contraction and relaxation, the rate of tension change in contraction and relaxation, and the period of latency.
The most obvious changes in spinal muscle activity would be expected in myotatic units where muscle members are interdependent mechanically. Changes in length or tension of a particular muscle should affect its synergists and antagonists. Biochemical changes in a particular muscle could alter its functional relationship within the myotatic unit and thus alter spinal efforts enough to produce segmental subluxations. On a larger scale, myotatic units of spinal sections could be altered as well as gross spinal distortions from myotatic units of the trunk muscles.
These visceral or somatic motor responses may affect motion unit musculature via somatic reflexes and referrals, resulting in altered muscular tone or activity. The motion unit also may be affected by visceral reflexes and referrals, producing vasomotor responses that can alter muscular activity by ischemia or hyperemia. Vertebral position, motion, and neurointegrity could be consequently reduced to the state commonly associated with a subluxation syndrome.
Supporting-Tissue Responsibilities
The second major category of causes of segmental subluxations is inequality of supporting tissue of the vertebral motion unit. In recognition of the significance of this cause of subluxation, the following review of supportive tissue responsibilities in assisting normal spinal functions of motion, stability, and protection of the neurologic elements is provided.
The four most important supporting tissues of the spinal motion units are the paraspinal ligaments, the intervertebral discs, the posterior facets, and the vertebral bodies.
The "chicken or egg" argument can lead to academic debate on the sequence of events that lead to the presence of the intrinsic factor (subluxation). It is a clinical exercise because indifference to the initiating role of muscular efforts, supporting tissues, or neuropathologic reflexes and referrals promotes multiple recognition of simultaneous factors in the genesis of subluxation and multiple approaches to eradication or reduction of these somatic faults through manipulation and adjunctive therapy.
An interesting idea that is parallel to the supporting functions of vertebrae described in this chapter is suggested in the following report by Drum in An Introduction to the Study of Postural and Spinal Mechanics:
"Mechanical stress is converted to an electrical stimulus by piezoelectric elements within the bone; this stimulus affects pH and ion population, the alignment and probably the aggregation pattern of extracellular macromolecules and also cell behavior; through these cellular and extracellular influences the electrical stimulus produces change in the osseous architecture appropriate to resist the deforming force and shut off the initiating signal.
Astronauts, subjected to the weightlessness of space, rapidly become osteoporotic because they lose a major portion of three of the four mechanical stimuli to bone. This should make it clear that stress is essential for the maintenance of a strong skeletal architecture; that the ideal approach to combat disease is not the search for a stress-free environment, but rather a strengthening of the body's inherent defense mechanisms so they can adequately cope with a level of stress commensurate with an exciting productive life."
The various processes, outlined above, are not limited to the vertebral column or its paravertebral tissues. Similar conditions may exist in other musculoskeletal tissues producing similar intrinsic factors (subluxations) and self-perpetuate neuropathic responses. However, in respect to the vertebral column, the effects may be more evident and crucial because of the close anatomical relationships and the functional importance of normal mechanical integrity to the closely associated delicate elements of the nervous system.
Stoddard states that the effects of mechanical irritation to especially vulnerable neurologic areas are:
BASIC EFFECTS OF SPINAL SUBLUXATION
Immediate Local Effects of Subluxation
Immediate local responses of any tissue to irritation, degeneration, or changes resulting from disease processes may occur within and around the vertebral motion unit tissues. Inflammatory reactions of redness, swelling, heat, and pain may follow precipitating injury, degeneration, or proliferative reactions and processes of repair, healing, and regeneration. Local effects also may include edema, circulatory and pH changes that adversely affect joints, muscles, and nerve roots.
Mechanical Effects of Subluxation
Mechanical effects are alterations in biokinetic ranges of motions, balance, or position of local segments, or include the effects upon the musculoskeletal system elsewhere, due to compensatory distortions and alterations as the proprioceptive-directed mechanisms attempt to correct their mechanics to the segmental presence of structural imbalance.
Neurologic Effects of Subluxation
Neurologic effects of subluxation are manifested in alterations of the neurologic triad: sensory, motor, and autonomic. Some neurologic effects are a result of direct physical pressure (compression) and stretching (tension) of the nerve. Other effects may follow circulatory changes supplying the cord and nerve roots, meningeal irritations, impedance of CSF flow, direct proprioceptive insult, and propagation of facilitated segments.
THE EFFECTS OF BIPEDISM
Postural deviation demands and elicits complex responses of interrelated parts (postural components) organized by the CNS. The stimulus-response of proprioceptive mechanisms is mediated from mechanoreceptors to spinal muscles. These complex responses are initiated by insult or excessive demand placed on any tissue or organ. Through spinal reflexes and/or referrals, the initial stimulus alters input and reaction of the proprioceptive mechanisms.
The responses are essentially the same for all tissues, depending on which part of the nervous system is involved. Each level will show responses in proprioception, sensory, motor and autonomic changes directed by the level of the insult. The more levels involved, the more complex the syndrome of alterations.
Involvement of somatic musculoskeletal components, especially of the axial structure, has a high incidence in man. They manifest as disturbances intensified by gravitational stresses and as initiating factors in the syndromes of complex responses. Vertebral subluxations are the musculoskeletal components of the spine initiating sensory, motor, and autonomic alterations. Their presence and significance are magnified and prolonged by focused gravitational stresses.
Once the responses are organized and initiated by the CNS, the total postural response to gravitational factors is altered, producing new compensations, new stresses, and new more-complex responses. The presence of a vertebral subluxation, with its sustained responses, alters its ability to participate in normal postural responses, shifting responsibility to other components that react with new compensations, stresses, and responses.
The recruitment of overtaxed musculoskeletal components that are reflexly organized and sustained by stress, foci irritations, and excessive demands become sustaining or exacerbating factors in the complex responses of postural accommodation (even if secondarily induced). Such inability for vertebral subluxation self-correction results in sustained responses, exaggerated responses, and the recruitment of other responses that perpetuate patterns of postural reaction (distortions of structure).
Pain, tenderness, muscular rigidity, and motor, sensory, and autonomic disturbances are interrelated components of this syndrome of response. The gross evidence of spinal structure distortion leads to obvious evidence of vertebral subluxations with identifiable characteristics of sensitivity changes, reaction alterations, and autonomic visceral changes segmentally patterned. It is not coincidence to find a somatic component and to find visceral components as they are interrelated by design, development, and function. They individually represent the different sides of the same coin.
Musculoskeletal stress is an extremely frequent initiating factor to complex responses of the nervous system associated with and contributory to many different chronic and acute functional disorders to which humanity is peculiarly susceptible. Erect posture is an active defiance toward gravitational forces. Compliance to gravitational forces becomes a matter of choice. The correct choice is often not made because of lack of sensory information, priority options, socioeconomic demands, or unawareness of consequences.
The concept of cause (an initiating etiologic idea) finds soundness as it directly guides successful diagnostic implications and therapeutic applications. The inability to identify the responses and the lack of suggested therapeutic direction strongly suggest that the etiologic concept is deficient or incorrect in rationale.
Implied Etiology
The presence of the subluxation may vary in the degree of the associated complex responses. Subclinical responses may stay within physiologic limits and not be of assistance in locating the subluxation. The degree of subluxation malposition, altered kinetics, and neurologic insult are also factors in directing the magnitude of responses and clinical significance.
The subclinical "dormant" subluxation may be elevated in clinical importance by additional stresses produced by new or continued demands upon the individual. Along with the degree of subluxation and its responses is the variable factor of the number of subluxations in the system as well as the levels or groupings of subluxation patterns.
Environmental stress may increase and lower resistance through the subluxation or resistance may be lowered through subluxation so environmental stresses that would not ordinarily be taxing become overwhelming, producing pathologic responses and syndromes. The duration of the subluxation complex also may be a determining factor as to its clinical significance relative to the amount and degree of degenerative changes, the amount and degree of accommodations and compensations, and the amount of tissue changes that have occurred progressively over time.
Implied Diagnosis
The Diagnostic Recognition Hierarchy
Five points should be noted:
2. Recognition of postural compensations in response to gravitational stresses.
3. Recognition of the presence of spinal subluxations in postural compensations.
4. Recognition of the depletion of physiologic reserves by subluxations.
5. Recognition of disease processes as a result of loss of or misdirection of reserves and resources.
Implied Therapeutics
SPINAL SUBLUXATION'S CLINICAL SIGNIFICANCE
The presence of the subluxation also alters the segments' role of responsibility in providing protection for the neurologic elements of that level. Decreased protection allows for neural insult from external stimuli and also from internal stimuli (of which the subluxation is an intrinsic source because of aberrant position and motion).
Because they are abnormal in their activity, subluxated segments can no longer play normal roles in desired or demanded activities; ie, otherwise normal responses become exaggerated or diminished. Because of the persistent neuroinsult involved, the segment is also unable to receive stimuli adequately, because a normal excitation is unable to generate or direct a normal corresponding response.
The subluxation may allow insult to the sensory elements (neurons) in many variable patterns depending on the nature of the insult, the spatial location of the insult, the area or numbers of sensory neurons involved, and the modalities of sensation transmitted by the involved neurons. The classic patterns of effects of sensory insult are hyperesthesia, paresthesia, hypesthesia, anesthesia, discomfort, and pain (especially pain with no evidence of tissue damage).
The subluxation may also allow insult to the motor elements (efferent neurons) in the same variable patterns as above. The classic involvement of motor neurons is hypertonicity, hypotonicity, atony, and spastic or flaccid paralysis.
In addition, the subluxation may allow insult to the autonomic afferent and/or efferent neurons in variable patterns depending on the same variables as above with either sympathetic or parasympathetic motor and sensory activities. The classic patterns of effects of autonomic insult are increased or decreased glandular secretion, motility, and sensitivity, constriction or dilation of innervated organs, and vasotonic disorders.
Further complexities of neural insult are possible with the involvement of a nearly infinite combination of elements involved. Clinical manifestations become most evident when a predominant involvement is present.
The obvious continual stress and demand associated with subluxation in this state are greatly amplified by restlessness and by added irritating stimuli from the environment. Added to this state of restlessness are the activities of daily life at home, work, play, and even during leisure periods. The stresses at rest are magnified many times with sustained and exaggerated activity. Activities for which one is unaccustomed are even greater sources of stress and usually demand new accommodations and compensations. Habitual activities become more stressful with extended duration, increased loads or demands, coupled activities, and unpleasant environmental changes.
A given vertebra, for example, in the preactive state of the spine is in axial rotation to the limits of its normal range of that level. A subsequent active state of the spine for a given movement normally requires axial rotation of the involved segment.
During the effort to participate in the spinal activity, the segments that produce excessive stress in abnormal range of axial rotation may damage elements of restraint designed to maintain the range of motion or may transfer its response to another level with that level now responsible for its own normal participation as well at that of one of its fellows. The final product will be faulty spinal motion because of faulted biomechanical function.
In the active state of the spine performing a daily activity, the subluxation producing excessive stress, damaging restraining elements, and/or transferring activity to other elements. The result is altered muscular activity and changes in supporting tissues of other segments of the spine, which then become subluxated. These subsequently subluxated vertebrae possess all the potential of the initial subluxation. The vicious cycle involved in subluxations is, in itself, of extreme clinical significance that is often overlooked in studies of axial skeleton disorders.
Pathologically, the subluxation results in damage to overstressed tissues that require repair resources. Physically, the subluxation transfers responsibility of responses to other tissues, increasing their consumption of bioresources. Collectively, the subluxation is a potential ecological disaster!
Facilitation and the Subluxation: Segmental Rheostats of Lowered Thresholds
The various definitions of facilitation all support the effect produced in nerve tissue by the passage of an impulse. The resistance of the nerve is diminished so that a second application of the stimulus evokes the reaction more easily. The law of facilitation specifically addressed, according to Dorland's Medical Dictionary, is "when an impulse has passed once through a certain set of neurons to the exclusion of others, it will tend to take the same course on a future occasion, and each time it transverses this path, the resistance in this path will be smaller."
Sensory impulses traveling via afferent neurons to a spinal cord segmental sensory neuronal pool causes facilitation of that pool, and sensory stimulation terminating in a segmental motor neuronal pool of the spinal cord causes facilitation of that pool. Descending motor impulses over efferents from higher motor centers of the brain to a segmental motor neuronal pool cause facilitation of that pool.
Sensory origins include both somatic afferents and visceral autonomic afferents, and descending efferents may originate in somatic brain centers or autonomic visceral centers. Motor neuronal pools facilitated by sensory afferents or descending efferents are both somatomotor and visceromotor pools.
When a segmental neuronal pool is in a state of facilitation, afferent impulses have a greater than normal effect on the neuronal pool; thus, they produce increased sensitivity. Efferent impulses are more easily generated; thus, they produce increased motor activity. This increased sensitivity and motor activity include the autonomic pools and functions.
Musculoskeletal stresses of subluxation initiate or are associated with an unbalanced stream of impulses entering the CNS. This, in effect, upsets the delicate balance of that part of the nervous system with which it is most intimately connected.
The debate rages on (chicken or egg). The theoretical possibility of segmental facilitation producing spinal subluxation is just as popular as that of spinal subluxation producing segmental facilitation. Even without settlement, the presence of subluxation as an intrinsic source of sensory irritation and the state of facilitation altering muscular activity of a vertebral motion unit warrants further thought.
Segmental Facilitation and Subluxation
Subluxated segments meeting the criteria of malposition and altered biokinetics have lowered motor reflex thresholds. The more clinically evident the subluxation, the lower the threshold.
Research has shown that lesioned segments, as determined by clinical criteria, were distinguishable by physiologic criteria of motor activity. Segmental motor reflex thresholds were determined by measuring the amount of pressure applied to the spinous process of each segment that just evoked contraction of the paravertebral muscles at that segmental level.
Muscle contractions were detected and evaluated by EMG recordings. Denslow found that lesioned segments invariably required weaker stimuli to produce reactions than did normal segments.
A later study demonstrated that diffuse and remote stimuli, including those from higher centers, and stimuli that occur in normal daily life, preferentially excited the pathways of paravertebral muscles of the facilitated segments. Other segments remained quiescent. Under conditions in which there was generalized muscular contraction, the activity in the facilitated segments was relatively exaggerated.
The easier opening of the motor pathways, the motor facilitation, had its origin in a sustained afferent bombardment by impulses from some segmentally located source, according to Denslow, Korr, and Krems. It is suggested, therefore, that lowered segmental motor reflex thresholds, in a state of segmental facilitation, would result in exaggerated activity of those innervated postural muscles when only postural tone is required. The resultant activity, out of phase with need, could perpetuate existing subluxations or generate new subluxations.
Since postural spinal muscles function in myotatic units (together or in opposition) and are mechanically interdependent, any change in the activity of one muscle has direct effects on its synergists and antagonists. When facilitated, excitatory motor efferents elicit exaggerated muscle contractions of that muscle directly innervated as well as its synergists, and the facilitation will increase inhibition of the antagonists. This exaggerated reaction and increased antagonistic inhibition further alters the ability to stabilize posture by imbalanced postural tone and postural activity.
This also may suggest that kinesiologic testing of a myotatic unit innervated by a subluxated segment would establish a weak (inhibited) muscle component and a strong (exaggerated) muscle component. Which muscle is inhibited and which is exaggerated may be dependent on the source originating the facilitory state. From a clinical viewpoint, the weak component has the same significance as the strong component.
Subluxated segments also exhibit a state of hyperirritability to sensory stimuli. Sensory components were measured and evaluated through cutaneous pain thresholds in various dermatomes and through mapping areas of cutaneous and deep hyperesthesia. Evidence gathered by Korr for hyperirritability of sensory pathways found the presence of persistent areas of lowered pain thresholds and of tenderness.
When using pressure on the spinous processes to elicit paravertebral contractions, it was also suggested that the involved segment with a demonstrated lowered segmental motor reflex threshold also would be hyperirritable to a pressure stimulus applied to the spinous process. Denslow found that the product of a lowered motor threshold plus a lowered threshold to sensory stimuli further exaggerates the motor activity associated with the abnormal segment.
Also suggested through hyperirritability and hypersensitivity in subluxated segments is the facilitated reception of all modalities of sensation with innervation through the sensory components of a given segment. In addition to cutaneous pain, lowered thresholds to sensations of somatic temperature, vibration, touch, proprioception, pressure, muscle stretch, and visceral pressure, distention, and pain also may be altered in the facilitated segment.
Skin Resistance Findings
Studies, limited to the sympathetic division because of segmental distribution, were evaluated through measurement of the activities of the sweat glands and blood vessels of the skin. These cutaneous visceral structures served as physiologic indicators of activity of sympathetic outflow to the corresponding areas or segments. Sweat gland activity was measured by electrical resistance of the skin (ERS). Skin resistance is lowered by increased sweat secretion and elevated in its absence.
Also used were thermal readings of the skin. Cool skin with higher vascular tone suggests increased sympathetic motor innervation, as does increased sweat. Segments of sympathetic hyperirritability showed low ERS recordings and comparatively cool skin. There was also segmental lowering of the red (hyperemic) response to mechanical stroking of the skin.
Findings of a low ERS, low skin temperature, and feeble red response suggest increased irritability of both sensory and motor sympathetic pathways in affected spinal segments. Other studies have suggested relationships among a diagnosed pathologic organ or structure and areas of low ERS, especially where there also was a pain component present. After exploring large numbers of apparently healthy persons, it was found that in a growing number of such individuals the signs and symptoms of visceral disease appeared months and years after the demonstration of prominent areas of low electrical resistance in dermatomes related to the involved viscera.
Some of these symptom-free subjects who later developed visceral disease had pre-existing ERS patterns resembling those found on patients with similar diseases. In other subjects, it was shown that new and prominent areas of low ERS could be induced experimentally by acute stresses and myofascial irritations, and accidentally as a result of trauma.
Some interesting conceptual models of subluxated segments and the facilitated state are offered below:
2. These segments are abnormal in motor activity and in response to various stimuli.
3. In these segments, at least some neurons mediating sensory, motor, and autonomic functions are in a state of hyperexcitability with easier, exaggerated, and prolonged responses to impulses reaching them from many sources.
4. These segments are susceptible to sustained and exaggerated activity occurring in normal daily life.
5. The influence normally exerted by these neurons on the tissues that they innervate may thereby be exaggerated.
6. The antagonists of those muscular components that are in a state of facilitation are correspondingly inhibited, and the synergists are excited.
7. The state of facilitation effected by a subluxated segment refers to the tissues innervated by that segment; thus, the individual as a whole, through imbalance of homeostatic controls, is sensitized to all the influences operating within and without.
8. Facilitation of the sensory pathways in a subluxated segment means there is easier access to the nervous system through which environmental changes (especially stressful, noxious, or painful stimuli) have exaggerated impact on the individual.
9. Facilitation of motor pathways leads to sustained muscular tensions, exaggerated responses, postural asymmetries, and limited and painful motion. Positive feedback occurs because the muscles have rich sensory innervation, and under these conditions, the related muscles, tendons, ligaments, joint capsules, and articular surfaces become sources of intense and unbalanced afferent streams of impulses that perpetuate the state of facilitation.
10. Local sympathetic hyperactivity secondary to segmental facilitation subluxation that is reflected in the skin may be associated with sympathetic hyperactivity in the viscera. The cutaneous manifestations are associated with disturbances elsewhere in the segment, and this local sympathetic activity is an important factor in the production of disease processes. Hyperhidrosis and lowered ERS in dermatomes related to pathologic viscera have been demonstrated.
Autonomic Imbalance
Many serious clinical entities may be associated with local autonomic imbalance in the direction of sympathicotonia. Symptomatic relief, lasting improvement, and even "cures" have been achieved through surgical, pharmacologic, and other blocks of the sympathetic pathways to the involved organs.
A number of visceral and other chronic diseases appear to begin as ischemic states of the involved tissues due to local neurogenic vasospasm. This vasospasm seems to be of sympathetic origin and is also associated with vasospasm, pallor, and hypothermia in related segments of the skin.
Vasomotor responses in the skin and viscera are quite parallel; ie, stimuli that elicit vasoconstriction in one, commonly do so in the other. This is exemplified in diffuse sympathetic activation under intense environmental or emotional stress, with blood being shunted from the viscera and skin to skeletal muscles. The ensuing visceral ischemia of the gut produces abdominal "butterflies," and the patient's ischemic skin gives an "as white as a ghost" appearance.
Normal sympathetic activity is intermittent and comparatively brief in response to emergency situations. When sympathicotonia is sustained, reduction in visceral blood flow, inhibition of secretion and smooth muscle activity, and spasm of sphincters will eventually result in some damage and dysfunction of the affected organs and thus the entire body's economy.
Whether overt disease processes develop depends on the total resources and resistance of the individual and demands of daily life. The greater the demands made by the total environment or the individual in relation to available resources, the more likely the following may be realized.
2. With altered bioresources, the certainty that associated tissues will be impaired and damaged by exaggerated demands is greater.
3. The greater the sum of altered resources and tissues, the greater probability that disease will start in or through the facilitated segment and/or in the mechanisms that carry the burden of compensation for the altered functions and structures.
It appears that segmental sympathetic hyperactivity originates as a part of a highly organized reflex response that is organized at the spinal cord level. It is initiated by certain forms of sustained irritation arising in one or more tissues innervated from or by the corresponding segment; manifesting sustained and exaggerated impulse traffic in the sensory, motor, and autonomic pathways that originate in this segment.
This state of facilitation may be maintained by impulses reaching this segment from any source. Factors evoking these segmental responses arise with high frequency in the weight-bearing or axial portion of the musculoskeletal system. One culprit may be the sustained impulses from proprioceptive insult caused by minor biomechanical faults.
Most visceral structures and functions are under both sympathetic and parasympathetic influences at least by a tonic level of activity. By either increasing or decreasing the influence of one system, the result will be an alteration of the influence of the other through antagonistic actions. Hypersympathicotonia thus could result, in effect, from either increased sympathetic activity or inhibited parasympathetic activity. Hyperparasympathicotonia, conversely, could result, in effect, from constant parasympathetic activity or inhibited sympathetic activity.
The centers controlling the sympathetic system can determine to a great degree whether they discharge selectively or totally. Under basal conditions, selective tonic and reflex activities occur; but under stress or in anger, the system can and does discharge as a whole.
Autonomic fibers are not essential to the functioning of all visceral tissues. However, overaction of this innervation has major physiologic consequences and underaction also impairs normal function, at least until the tissues recover from their dependency on this innervation.
Low vasomotor tone produces orthostatic hypotension. Overactivity of vasomotor nerves can result in hypertension. In Raynaud's disease, there is a spasmodic contraction chiefly of the blood vessels supplying the digits.
A general conceptual model is that the parasympathetic system has a conserving, protective function and tends to promote emptying of the hollow organs. The sympathoadrenal system functions in emergency situations, during stress, fear, anger, and rage, or when suffering with pain. Both systems tend to preserve an essential homeostatic balance of body functions, correct imbalances, and support behavioral activities.
Hypersympathicotonia may be involved in the following changes: pupillary dilation and protrusion of the eyeball in exophthalmos, constriction of gland cells with immediate increased secretion, vasoconstriction of glands with later decreased production and secretion, cardiac acceleration of pacemakers and increased strength of contraction with dilation of coronary arteries, dilated bronchi with decreased secretion and mild constriction of blood vessels of the lungs, decreased peristalsis and tone of lumen in the GI system with increased tone of sphincters plus inhibited secretion and vasoconstriction, vasoconstriction of renal vessels with decreased output, increased output of both epinephrine and norepinephrine from the adrenal medulla, increased adrenal cortical secretion, vasoconstriction of cutaneous vessels and vasodilation of blood vessels of skeletal muscles, piloerection and increased secretion of eccrine sweat glands, (but not the approcrine glands, which are humorally influenced), inhibited gallbladder contraction, increased glycogenolysis and increased liberation of glucose by the liver, reduction in blood clotting time, and contraction of the spleen to discharge red blood cells.
Reflex and Referral Models
In the following conceptual models, reflexes are defined as sensory activity producing motor responses. Referrals are defined as sensory activity referred by divergence of synapses to excite other sensory activities. In other words, reflexes are sensory to motor patterns and referrals are sensory to sensory patterns. Both should originate at sensory receptors, but they may originate anywhere along the course of an afferent fiber.
The various reflexes and referrals of initial stimuli that exist within and between individual components of the sensory, motor, and autonomic systems may exhibit the neurologic effects of subluxation. The ramifications and complexities of various reflexes and referrals and the countless number of signs, symptoms, and pathologic changes arising from these neurologic activities are even more challenging when considering not one but the interactions of many of these mechanisms that occur simultaneously in various degrees, overlappings, and combinations.
For ease in presentation of "the big eight" reflexes and referrals, each will be identified singularly:
Somatosensory neurons are those afferent fibers that carry sensory information to the cord from all somatic structures innervated by that cord segment; particularly, dermal sensations, muscle stimuli, and musculoskeletal-related proprioceptive sensations of motor activity, vibration, and position. Somatomotor neurons are those efferent fibers that innervate skeletal muscles at a given cord level and control tonus or contraction of the related somatic elements.
The sympathetic visceromotor response may occur throughout a specific neuromere. Therefore, a viscerosensory stimulus may elicit a vasomotor response of constriction or a smooth-muscle contraction in a specific organ. It also may cause a vasoconstriction of blood vessels of the somatic structures, musculature, skin, ligaments, etc, depending on the divergence of collaterals of the visceromotor neurons affected.
Once initiated, this referral may cause additional areas to become involved through somatosensory to somatosensory referrals so that referral of conscious pain may occur in other areas than that of the segment involved (cord, medulla, or thalamus level). A classic example is the angina of ischemic heart muscle with viscerosensory impulses of the heart being perceived as somatic sensitivity of the left shoulder and arm.
This reflex also explains the red response of stroking the skin and various systems of reflexology. Somatic stimulation of a vertebra (manipulation, percussion, etc) also may alter visceral motor responses. Subluxation is a somatic lesion and through somatosensory irritation of its presence may reflexly alter segmental visceral functions.
Another example needs mention because somatic-tissue irritations may directly induce the inflammatory reflexes of vasculature.
Somatomotor or visceromotor effects through reflexes and somatosensory or viscerosensory referrals may be initiated by either a visceral or somatic stimulus. But the synaptic area (neuronal pools) subserving these processes, both in the spinal cord and/or brain centers, may, because of repetitious activity or previous stimulation (activation), have lowered thresholds (eg, be in a facilitated state).
Even if the initiating cause of this process is removed, the minimal threshold for eliciting a neurologic response is reduced so that what was previously subthreshold stimuli may now elicit or maintain the signs, symptoms, and pathophysiologic processes involved. In such a situation, previously irrelevant stimuli evoked by daily environmental or constitutional stress may now maintain (sustain) or exacerbate (amplify) these processes through facilitated reflexes and referrals.
The "Garden Hose" Theory
Historically, this concept suggests that pressure on a nerve, produced by subluxation, decreases its ability to transmit impulses. This author has not found scientific evidence to support such a phenomenon in all neurologic tissue. The research findings of Suh indicate that spinal nerve roots are far more susceptible to compression block than peripheral nerves. Large rapidly conducting fibers are more susceptible to compression block than small slowly conducting fibers. Inhibition of trophic nerve flow is also suggested by the "garden hose" theory.
In peripheral nerves, some fibers are blocked by pressure as low as 30 mm Hg. Reduction of compound action potential to at least half required at least 100 mm Hg. A pressure of 150 mm Hg was required to produce a complete block of the sciatic nerve within 3 minutes. In contrast, with pressure applied to spinal nerve roots, slight impairment could be observed with 10 mm Hg and was reduced to half size by only 20 mm Hg.
Denny-Brown and Brenner report that "Sensory fibers are more resistant to pressure than motor fibers." Suh states that "Fibrotic and thickened ligaments may, in the extremes of motion, press on spinal nerves where they exit from the IVFs. Protruding discs may encroach on spinal nerves.
Thinning discs and other disorders may result in narrowing of the foramina and pressure on spinal nerves. The compression of spinal nerves presumably results in aberrant neuronal activity which alters the operating characteristics of reflex mechanisms within the cord."
Most biologists would agree with Crelin that the vertebral column of man is marvelously engineered to protect the delicate spinal nerves. Through a wide dynamic range and while supporting large loads, the spinal column normally performs well, IVFs normally remain spacious, and nerves normally need not endure sustained compression effects. Nevertheless, the literature provides ample evidence that the spinal nerves can be compressed during certain pathologic conditions, including disc protrusion or thinning, fibrosis or thickening of spinal ligaments, osteoarthritis, neoplasms, hemorrhage or swelling, etc.
Between the extremes of normal functioning and those of gross pathology such as are associated with medically diagnosed nerve compression syndromes, there must exist various degrees of abnormality in which forces transmitted to spinal nerves can exceed the normal level. Under such conditions, subtle impairment of nerve function may occur that are not easily diagnosed as a nerve compression syndrome. Such impairments might, however, respond to manipulation provided by chiropractic treatments and be recognized as significant phenomena of the subluxation syndrome.
With compression block, two factors have been implicated: (1) anoxia, with resulting effects on the microvasculature of the nerve, and (2) mechanical deformation or rupture of nerve fibers. Both could be involved, especially in chronic nerve compression. Recent studies of nerves subjected to chronic constriction indicate that the most peripheral fibers undergo the earliest degeneration.
According to Moldaver: "It can be accepted as a generalization that, during the development of a compression block, the different modalities are lost in the following order: proprioception, touch, temperature, and pain sensibility."
The Melzak/Wall Gate-Control Theory
In view of the law of specific nerve energies, impulses conveyed to the CNS by nociceptive afferent fibers would be interpreted as painful, and those conveyed by contact-sensitive fibers would be interpreted as noninjurious mechanical stimulation. But Melzak/Wall point out that the signals often seem confused or inhibited. Neuralgia and causalgia are examples of excruciating pain being produced by gentle touch or vibration. Pain generated by tissue damage may diminish or disappear in emotional excitement or in the presence of "counterirritants."
Both large and small fiber inputs (both nociceptive and nonnociceptive inputs) can be blocked by the activity of inhibitory interneurons in the substantia gelatinosa area of the dorsal gray matter. These inhibitory neurons act directly on the sensory endings of the afferent neurons to reduce their effectiveness and inhibit transmission to the T-cells. These inhibitory neurons, partly because of descending influences from the brain, are always active, tending to hold the sensory gate partly closed (centrifugal influences).
The large, mechanoreceptive fibers activate the inhibitory cells, tending to close the gate. The small, nociceptive fibers, on the other hand, retard the substantia gelatinosa inhibitory cells, and by this "inhibition of inhibition" open the sensory gate.
In the subluxation-free segment, large mechanoreceptive fibers carry continual impulses to the cord and maintain the gate in the closed position. With the addition of a subluxation that has a compression factor on the spinal nerve root and that compression selectively blocking large mechanoreceptive fibers, the symptoms of pain may appear as a result of an opening effect of the sensory gate. Conversely, removal of compression-causing subluxation may allow return of the large mechanoreceptive fiber impulses, closing the gate and relieving the symptoms of pain.
Trophic Influences of Nerves
The trophic influence of nerves on the organs and tissues they innervate has long been recognized as a mysterious innate phenomenon in chiropractic philosophy and practice.
We are now approaching an understanding of how nerves exert long-term influences that cannot be ascribed to impulse conduction. Research suggests that there are certain proteins (not yet identified), and possibly other highly specific substances of large complex molecular structure, that are synthesized in peripheral nerve cells (somas) and that these neuronal components (trophic substances) are transported through the length of the fiber (neuronal peristalsis) and cross the junctional barriers into tissue cells.
Interruption of the Neurotrophic Flow
Korr reports that "The atrophy of denervation (interrupted neurotrophic flow) and the atrophy of disuse (interruption of motor nerve impulses) in the structural, functional, and biochemical aspects of muscle are quite different in nature and in course, though the former does naturally include aspects and components of the latter. What seems involved is not so much interruption of impulses (and therefore contractile activity), but disconnection between nerve cells and muscle cells."
Confirmation of this concept can be approached several ways:
2. Atrophy of disuse (diminished impulse traffic) in a muscle can be avoided or corrected by synthetic electrical stimulation of that muscle. However, the atrophy of denervation is not reversed or avoided by synthetic electrical stimulation and continues its course of degeneration and dedifferentiation.
3. A hair-size string tied around a fiber may act as a node of Ranvier, not interfering with impulse conduction (may even facilitate impulse conduction) but, rather, interrupting neurotrophic flow. Impulses (orthodromic) continue to arrive at the end organ. Dedifferentiation and degenerative changes occur in the end organ with interrupted neurotrophic flow. The atrophy of disuse, a result of interruption of impulses, has been found much less severe, much more readily reversed, and different in many ways than the atrophy occurring following axonal interruption.
Conditioning Influences of Nerves
Nerves exert a conditioning effect on the functional properties of some tissues and on responses to other influences; ie, denervation of skin augments its susceptibility to the action of carcinogenic agents. Denervation also affects responses of various organs to certain hormones.
Morphogenetic Influences
If the nerve supply to one kidney is interrupted in a puppy before the 10th or 11th day of life, the development of the kidney is also interrupted at that point. This is also suggested in muscle differentiation and growth.
Role of Nerve in Regeneration
Nerves are capable of regenerating entire limbs after amputation. If the nerve is removed from the amputated stump, regeneration does not take place. Resection of the sensory fibers in the stump allowed for regeneration. Healing and regeneration are influenced by nerve supply in wounds and repair of defects in skin, bone, and other tissues, in all mammalian species, including man.
Regulation of Gene Expression
Skeletal muscle is commonly classified into two categories: red and white. Red fiber is slowly contracting and relaxing with twitches of long duration, and sent into sustained tetanic contraction with low-frequency stimulation; ie, tonic, postural muscle. White fiber is phasic, rapidly contracting muscle, with brief twitches, and requires high-frequency stimulation to produce tetanus. Red muscle is largely aerobic (oxidation metabolism), while white muscle is capable of a high degree of anaerobic glycolytic metabolism.
When the nerves to red and white muscle cells are switched (by cross-reinnervation) and time is allowed for neural regeneration, an important generalization emerges: A remarkable degree of cross-transformation takes place, which includes structure, chemical composition, metabolic pathways, and enzyme activity. The nerve, in effect, instructs the muscle (muscle is pluripotential) by determining which genes of the muscle cells will be repressed and which will be expressed.
Over time, any factor altering the metabolism and protein synthesis of a neuron or impedes axonal transport could interfere with the neurotrophic influences on the innervated structures or cause an adverse or detrimental effect, thereby contributing to disease processes. The most likely factor is the vertebral subluxation, with compressive forces and mechanical stresses occurring where the nerves pass, the accompanying chemical changes in these tissues, and the associated aberrant sensory input and motor activity.
BIBLIOGRAPHY:
A Textbook of Pathology.
Philadelphia, Lea & Febiger, 1961.
Denslow JS:
Evidence of the osteopathic lesion: Data on what is known, what is not known, and what is controversial.
In Goldstein M (ed): The Research Status of Spinal Manipulative Therapy.
Bethesda, MD, NINCDS Monograph No. 15, US Dept. of HEW, 1975.
Homewood AE:
The Neurodynamics of the Vertebral Subluxation, ed 3.
Place of publication not shown, published by author, 1981.
Janse J:
History of the development of chiropractic concepts: Chiropractic terminology.
In Goldstein M (ed): The Research Status of Spinal Manipulative Therapy.
Bethesda, MD, NINCDS Monograph No. 15, US Dept of HEW, 1975.
Janse J:
A concept: the neurological element as it relates to clinical chiropractic.
The Chirogram, December 1975.
Janse J:
The integrative purpose and function of the nervous system: a review of classical literature.
Journal of Manipulative and Physiological Therapeutics, 1(3), September 1978.
Korr IM:
Discussion: papers of Sidney Ochs and David E. Pleasure.
In Goldstein M (ed): The Research Status of Spinal Manipulative Therapy.
Bethesda, MD, NINCDS Monograph No. 15, US Dept of HEW, 1975.
Korr IM (ed):
The Neurobiologic Mechanisms in Manipulative Therapy.
New York, Plenum Press, 1978.
Korr IM:
The spinal cord as organizer of disease processes: Some preliminary perspectives.
Journal of the American Osteopathic Association, September 1976.
Melzack R, et al:
Neurophysiological foundations of pain.
In Sternbach RA (ed): The Psychology of Pain.
New York, Raven Press, 1978, pp 1-26.
Melzack R, Wall PD:
On the nature of cutaneous sensory mechanisms.
Brain, 85:331-356, 1962.
Palmer DD:
Textbook of the Science, Art and Philosophy of Chiropractic.
Portland, OR, Portland Printing House, 1910.
Schafer RC (ed):
Basic Chiropractic Procedural Manual, ed 4.
Arlington, VA, American Chiropractic Association, 1984.
Speransky AD:
A Basis for the Theory of Medicine; translated by C.P. Dutt.
New York, International Publishers, 1943.
Steindler A:
Kinesiology of the Human Body Under Normal and Pathological Conditions.
Springfield, IL, Charles C. Thomas, 1955.
Stephenson RW:
Chiropractic Textbook.
Davenport, IA, published by author, 1927.
Suh CH:
Biomechanical aspects of subluxation.
In Goldstein M (ed): The Research Status of Spinal Manipulative Therapy.
Bethesda, MD, NINCDS Monograph No. 15, US Dept of HEW, 1975.
Suh CH: Computer-aided spinal biomechanics.
In Haldeman S (ed): Modern Developments in the Principles and Practice of Chiropractic.
New York, Appleton-Century-Crofts, 1980.
Wall PD: Gate control theory of pain mechanisms: a re-examination and restatement.
Brain, 101:1-18, 1978