

|
Chapter 6:
Radiologic Manifestations of Spinal Subluxations
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Basic Chiropractic Procedural Manual”
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated |
Spinal Subluxations
Definition and Significance
Radiologic Manifestations
Terminology of Radiologic Manifestations of Subluxations
Static Intersegmental Subluxations
Kinetic Intersegmental Subluxations
Sectional Subluxations
Paravertebral Subluxations
Classification of Radiologic Manifestations
Static Intersegmental Subluxations
Kinetic Intersegmental Subluxations
Sectional Subluxations
Extraspinal Subluxations
Case Presentations
Case Illustrating Classifications A-I and C-3
Case Illustrating Classifications A-I and R-2
Case Illustrating Classifications A-2, A-3, A-8, C-1, and C-2
Case Illustrating Classifications A-2, A-6, A-9, and C-1
Case Illustrating Classification A-3
Case Illustrating Classifications A-3, C-3, C-4, and D-1
Case Illustrating Classification A-3
Case Illustrating Classification A-4
Case Illustrating Classifications A-4 and C-2
Case Illustrating Classification A-5 (Spondylolisthesis)
Case Illustrating Classifications A-5, A-6, A-8 and A-9
Case Illustrating Classification A-7
Case Illustrating Classifications A-1, A-3, A-4, A-7, and A-8
Case Illustrating Classification A-8
Case Illustrating Classifications A-1, A-3, A-4, A-8, and A-9
Case Illustrating Classifications B-1, C-2, C-4, A-8, and A-9
Case Illustrating Classifications C-1, A-1, A-3, and A-8
Case Illustrating Classification C-1 and A-1
Case Illustrating Classifications C-2 and A-3
Case Illustrating Classifications C-4 and B-1
Through the years, there have been several concepts within the chiropractic profession about what actually constitutes a subluxation. Each has had its rationale (anatomical, neurologic, or kinematic), and each has had certain validity contributing to our understanding of this complex phenomenon.
Note: In years past, what is referred to above as a motion unit was called
a motor unit. The term motion unit was incorporated into chiropractic
terminology in the late 1970s to avoid confusion with the neurologic term
motor unit, meaning a single motor neuron and the muscle fibers its
branches innervate.
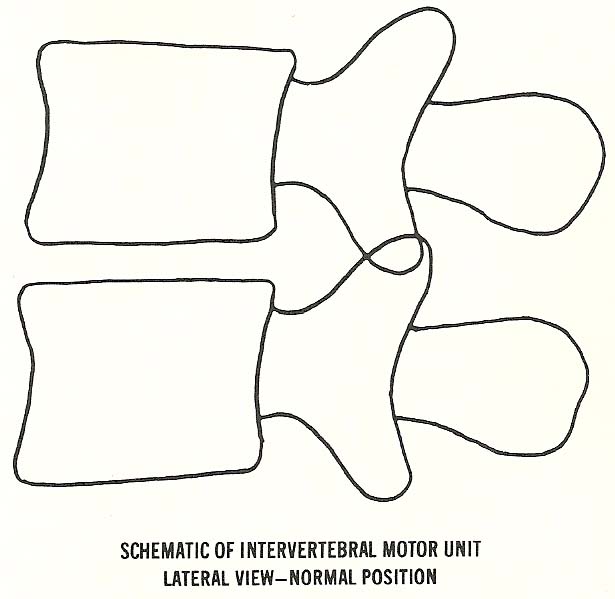
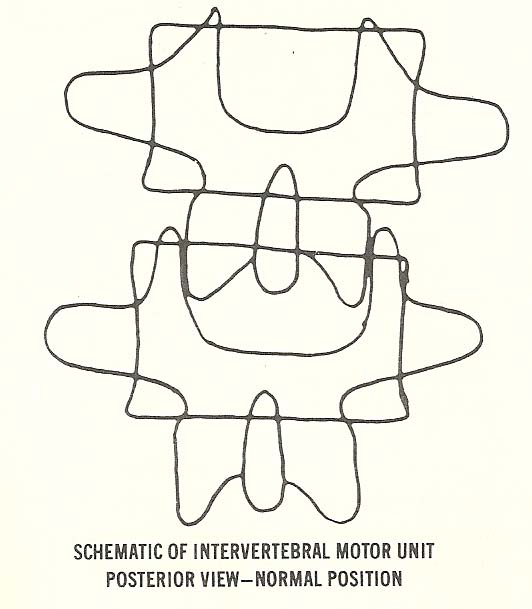
The method used for classifying roentgenographic manifestations of
subluxation is based on the concept of the intervertebral motion unit. An
intervertebral motion unit consists of two vertebrae and their contiguous
structures (disc interface and two posterior apophyses) forming a set of three
articulations at one intervertebral level. It is best illustrated by using a
lateral view (Figs. 6.1 and 6.2).
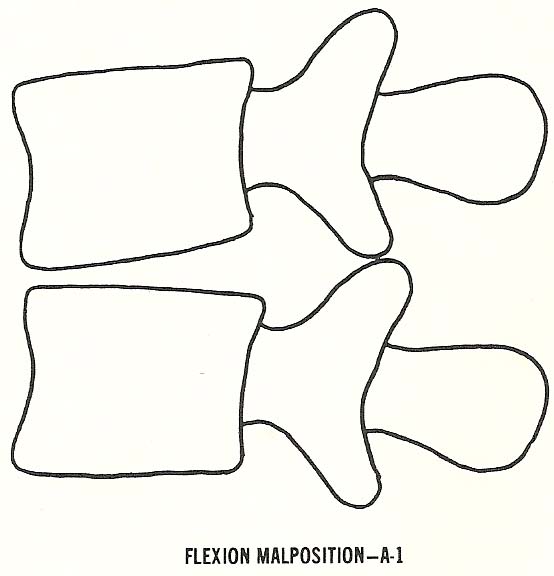
A-1. Flexion malposition.
Kinetic Intersegmental Subluxations
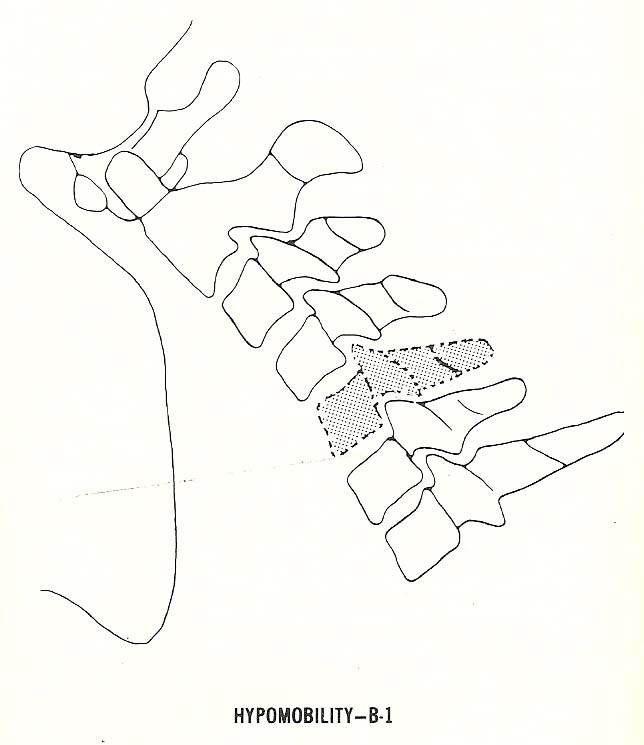
B-1. Hypomobility (fixation subluxation).
Sectional Subluxations
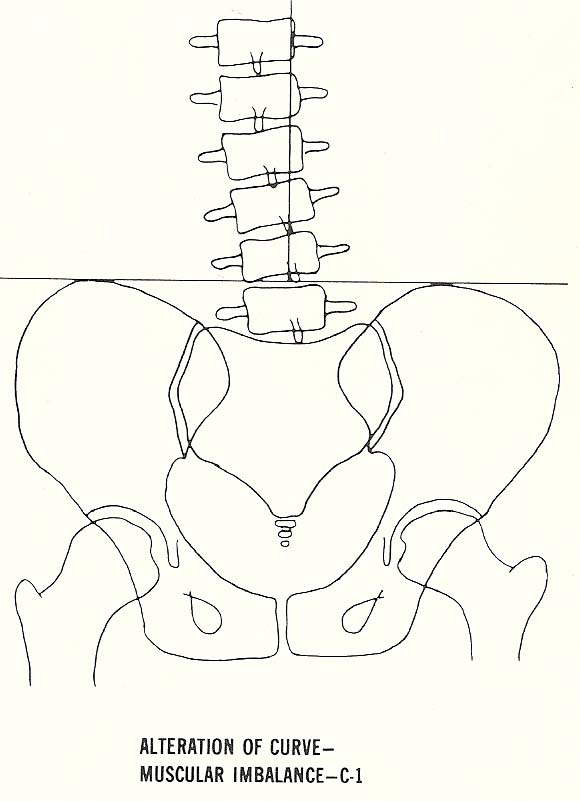
C-1. Scoliosis and/or alteration of curves secondary to musculature imbalance.
Paravertebral Subluxations
D-1. Costovertebral and costotransverse disrelationships.
Flexion Malposition. In flexion subluxation, there is wedging of the disc
space anteriorly as the vertebral bodies somewhat approximate one another
anteriorly (Fig. 6.3).
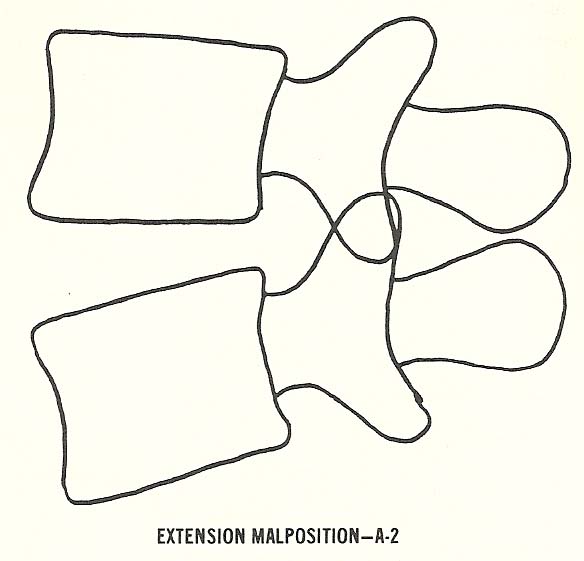
Extension Malposition. In this type of subluxation, which is one of the
most commonly encountered (especially in the low back), the vertebral bodies
approximate posteriorly and thus the disc narrows posteriorly (Fig. 6.4).
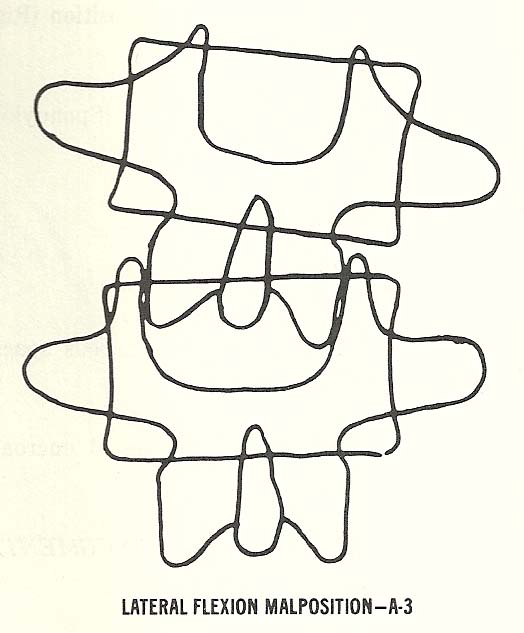
Lateral Flexion Malposition. This subluxation is characterized by lateral
wedging of the disc interspace produced by approximation of the vertebral bodies on the side toward which the vertebra above laterally flexes (Figs. 6.5 and 6.6).
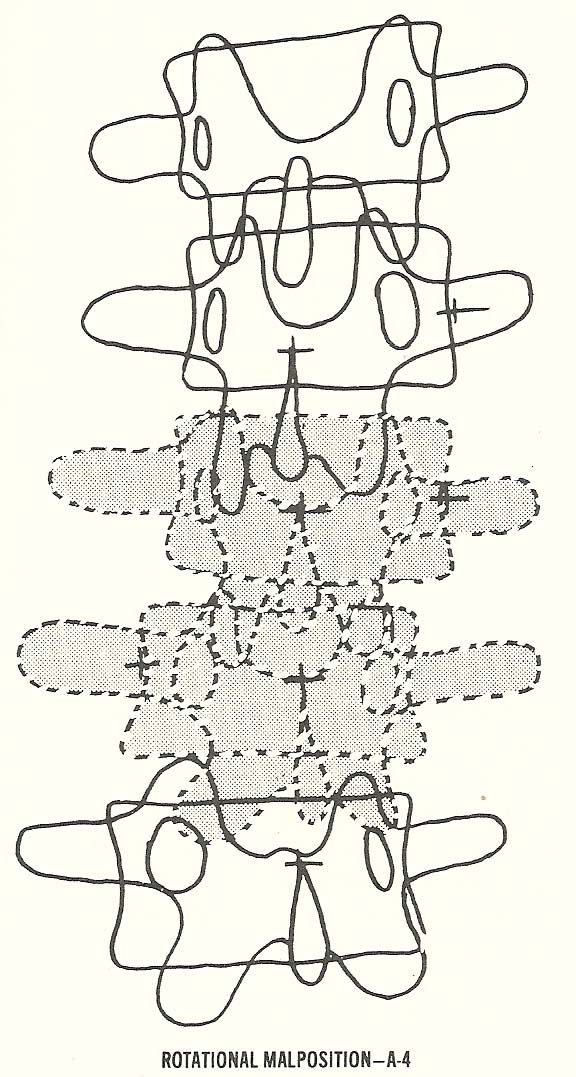
Rotational Malposition. Intervertebral rotation, even in subluxation, is
extremely limited at any single intervertebral level except in the upper
cervical spine. Thus, there are usually several segments involved in a
rotational disrelationship (Fig. 6.7).
Chapter 6: Radiologic Manifestations of Spinal Subluxations
This chapter describes the radiologic signs that may be expected when spinal subluxations are demonstrable by radiography.
SPINAL SUBLUXATIONS
Articular disorders of the spine are not always demonstrable by roentgenography, and to depict them radiographically often requires techniques other than those routinely used in spinal radiography (spinography). The
radiologic manifestations of spinal subluxation described in this chapter are
an attempt to provide a uniform classification of manifestations that may be
found when there is radiologic evidence of the presence of subluxation.
Admittedly, there are other classifications and concepts. Those chosen were
selected because they were believed to be defensible, widely acceptable, and
relatively easy to understand.
A motion unit has an anterior and posterior portion, and each has peculiar
and special characteristics. The articulations are the mobile portions of the
unit. This is mentioned because of the tendency to speak of a "subluxated
vertebra" when in fact it is the articulations that subluxate.
The anterior portion of the motion unit includes the vertebral bodies, the
interposed disc, the anterior and posterior longitudinal ligaments (which are
not truly visible on a radiograph), and, of course, the muscles and other soft
tissues not radiographically visible. The function of the anterior portion of
the motion unit is essentially weight bearing and supportive. It has little
sensory innervation. Changes or pathology affecting these structures, while
they may be quite spectacular in appearance on a radiograph and alter spinal
biomechanics significantly, are seldom accompanied by severe subjective
discomfort in the local area.
The posterior aspect of a motion unit consists of the pedicles, neural
foramina, articular processes and apophyseal articulations, the ligamenta
flava, apophyseal capsules, the laminae, spinous processes, the inter- and
supra-spinous ligaments, and all the muscles and other attached soft-tissue
structures. Many of the posterior elements of a motion unit are richly endowed
with sensory and proprioceptive innervation. Therefore, problems, pathologies,
stresses, and distortions affecting these structures are typically painful.
The following sections explain and illustrate the consensus statement
regarding subluxation from the historic Houston Conference of Chiropractic
that was held in November of 1972.
Definition and Significance
A subluxation is the alteration of the normal dynamics and anatomical or
physiologic relationships of contiguous articular structures. In evaluating
this complex phenomenon, we find that it has or may have biomechanical,
pathophysiologic, clinical, radiologic, and other manifestations. Subluxations
are of clinical significance as they are affected by or evoke abnormal
physiologic responses in neuromusculoskeletal structures and/or other body
systems.
Radiologic Manifestations
In considering the possible radiologic manifestations of subluxations, it
should be emphasized that clinical judgment is necessary to determine the
advisability of exposing a patient to the potential hazards of ionizing
radiation. An important purpose of exposure, in addition to the evaluation of
subluxations, is the determination of other pathologies.
Radiographic procedures necessary to determine possible fractures,
malignancies, etc, may not be the specific views needed to evaluate the
possible radiologic manifestations of subluxation. When subluxation can be
evaluated by other clinical means, it may be prudent to avoid radiation
exposure.
Terminology of Radiologic Manifestations of Subluxations
Static Intersegmental Subluxations
A-2. Extension malposition.
A-3. Lateral flexion malposition (right or left).
A-4. Rotational malposition (right or left).
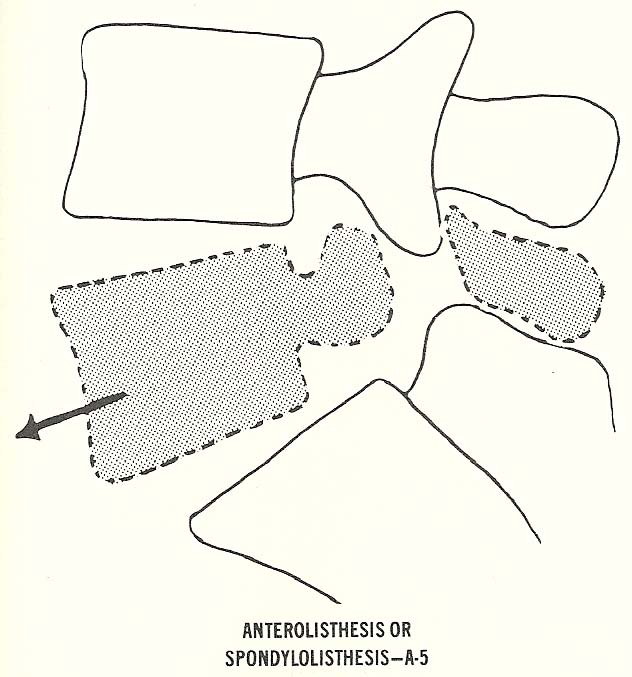
A-5. Anterolisthesis (spondylolisthesis).
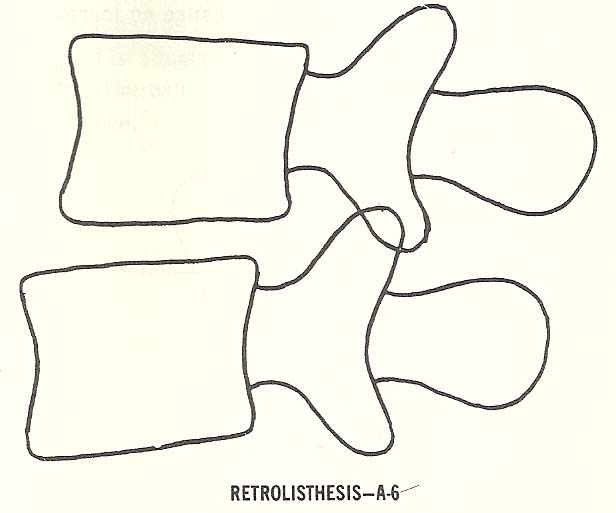
A-6. Retrolisthesis.
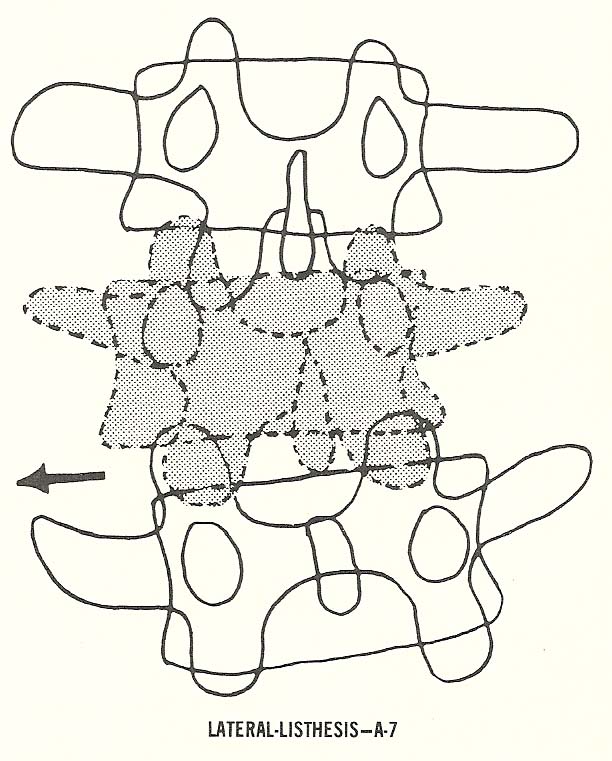
A-7. Laterolisthesis.
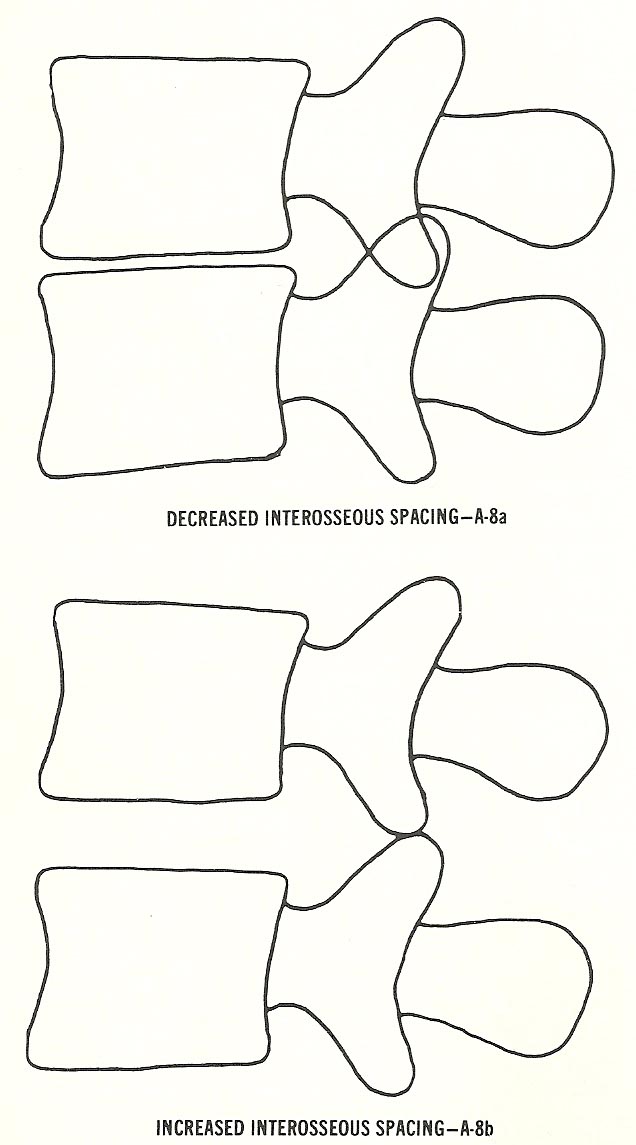
A-8. Altered interosseous spacing (decreased or increased).
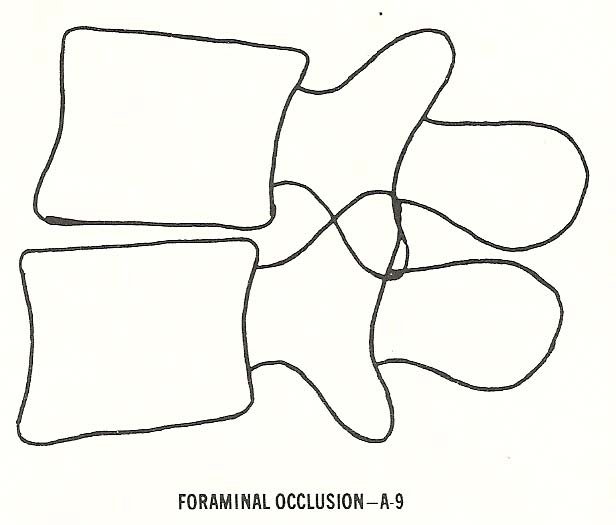
A-9. Osseous foraminal encroachments.
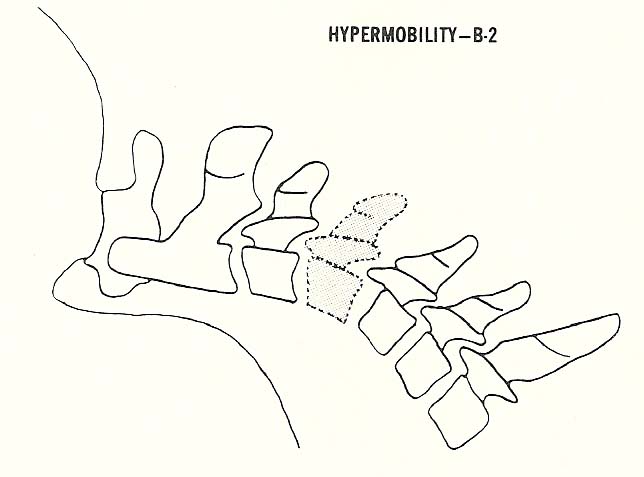
B-2. Hypermobility (loosened vertebral motion unit.
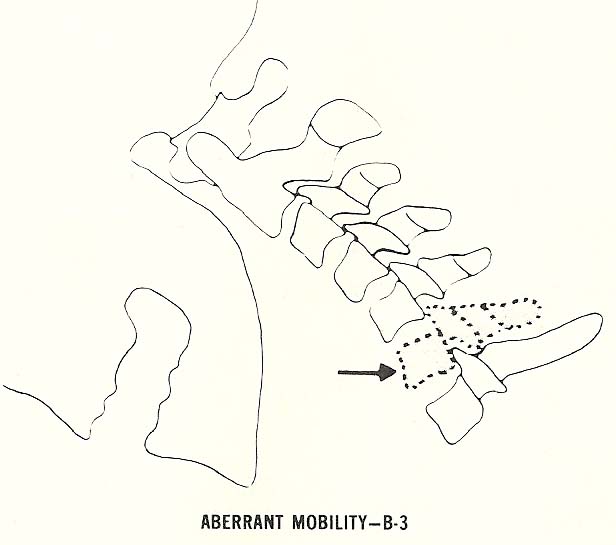
B-3. Aberrant motion.
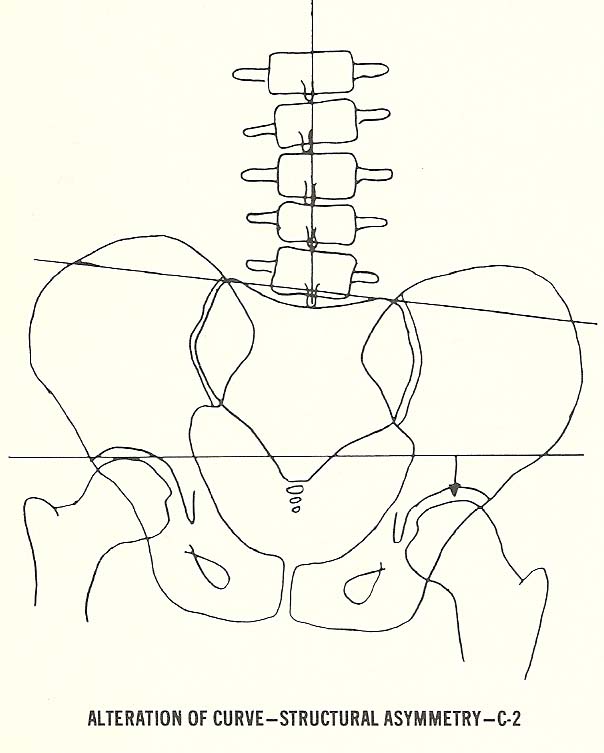
C-2. Scoliosis and/or alteration of curves secondary to structural
asymmetries.
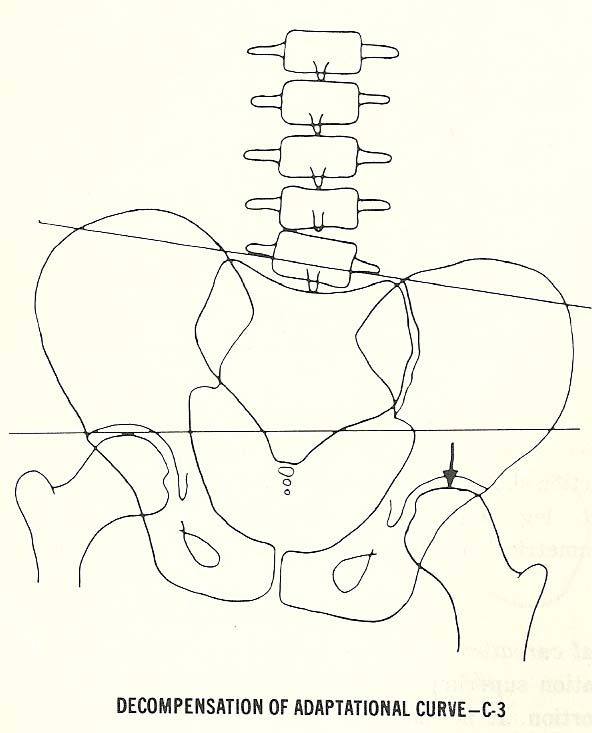
C-3. Decompensation of adaptational curvatures.
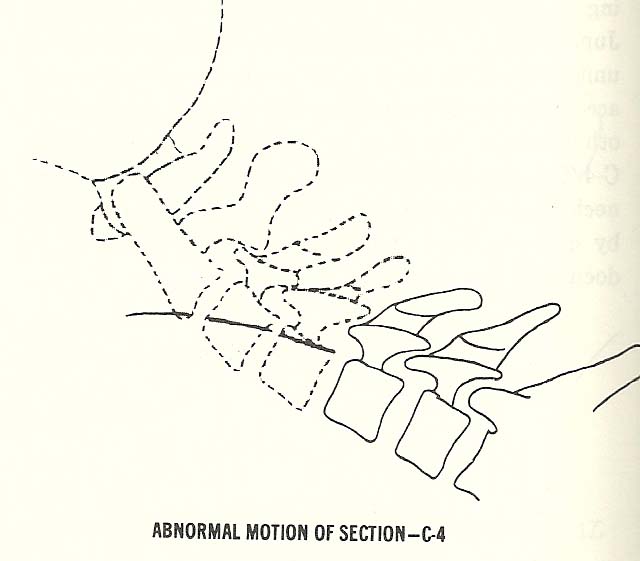
C-4. Abnormalities of motion.
D-2. Sacroiliac subluxations.
Note: The code names (eg, A-1, B-2, C-3, or D-2) listed above are rarely used in professional communications. A descriptive title is used such as "flexion malposition of C5," rather than "A-1 C5." ![]()
![]()
![]()
![]()
![]()
Classification of Radiologic Manifestations
Static Intersegmental Subluxations
Because of this, the spinous processes separate (open)
and the inferior articular processes of the vertebra above glide upward upon
the superior articular processes of the vertebra below. This elongates the
intervertebral foramen (IVFs) so they appear larger in their vertical
dimension.
The
posterior articulations show radiographic imbrication as the inferior
articular processes of the vertebra above glide downward relative to the
superior articular processes of the vertebra below. As the motion unit
extends, the IVFs of the unit appear to become smaller in their vertical
dimension.
This also causes the facet articulation on the side of disc
narrowing to imbricate while the contralateral articulation shows separation
(opening) of the articular processes as the inferior articular process of the
upper vertebra glides upward on the apposing process of the lower segment.
dimension.
The preponderance of the body of a
rotated vertebra relative to its spinous process on the side toward which the
vertebra has rotated posteriorly is well known to all doctors of chiropractic.
A line drawing taken from an actual radiograph will show reverse rotation
between the vertebrae that can be portrayed by a dotted line with the top
three and the lower two vertebrae rotated in corresponding relationship to one
another.
The next three types of subluxation are those in which the suffix
"listhesis" is used. This suffix means "slippage," and the displacement is
usually a gross distortion.
|
Anterolisthesis or Spondylolisthesis. This malposition is typically
produced by interruption of the isthmus (usually congenital) of a displaced
vertebra at its pars interarticularis. |
|
|
|
Retrolisthesis. Posterior malpositioning of the upper segment of two
vertebrae set (motion unit) is known as retrolisthesis. |
|
|
|
Laterolisthesis. The lateral slipping characteristic of this type
subluxation is typically accompanied by considerable segmental rotation. |
|
|
|
Altered Interosseous Spacing. This form is probably the most common of all
subluxations in elderly people. It mainly occurs when IVD degeneration has
caused narrowing of disc space, which approximates the vertebral bodies and
jams the posterior facets (Fig. 6.11). |
|
|
|
The last type of static subluxation, foraminal occlusion, may be a
consequence of one or more of those malpositions previously described (Fig.
6.13). |
|
|
Kinetic Intersegmental Subluxations
|
Segmental hypomobility, also called a "fixation subluxation" by many clinicians, may affect one or several motor units. |
|
|
|
Hypermobility, called loosening of the vertebral motor unit by Earl Rich
and Junghanns, may also be found at one or several levels. It is often found
as a compensatory mechanism accompanying hypomobility (fixation) at one or
more other levels in the kinematic chain. |
|
|
|
Aberrant motion exists when one or several vertebrae move in a way that is
not in coordination with neighboring segments during some movement of the spine. |
|
|
Sectional Subluxations
Sectional subluxations are another group to be considered. They comprise
disrelationships of a group of vertebrae.
|
Scoliosis and/or Alteration of Curves Secondary to Muscular Imbalance. Such disrelationships are quite common. |
|
|
|
Scoliosis and/or Alteration of Curves Secondary to Structural Asymmetries.
This is a frequently found scoliosis usually due to a short leg with pelvic
unleveling (Fig. 6.18). |
|
|
| Decompensation of Adaptational Curvatures. This is usually a relatively acute situation superimposed over a chronic deformity or distortion (Fig. 6.19). |
|
|
|
Abnormalities of Motion. These disorders can be found in spinal regions or at individual motor units (Fig. 6.20). |
|
|
Extraspinal Subluxations
Following are some case presentations depicting the various
classifications of subluxations described above. Also included are some facts
of historical significance, pertinent physical findings, diagnostic
conclusions, and a short description of the patient's response to chiropractic
management. The reader should keep in mind that these are not comprehensive
reports. They will, however, underscore some relevant points.
The final classification of subluxations consists of articulations in
which extraspinal structures articulate with the spine. The common
disrelationships occurring at these articulations (costotransverse or
costovertebral) are poorly shown radiographically, but the dysfunction
incidental to the disrelationship may well cause spinal distortions suggestive
of the subluxation. Marginal sclerosis of the articular surfaces is
presumptive evidence of the existence of a subluxation.
CASE PRESENTATIONS
Classification of Radiologic Manifestations
Case Illustrating Classifications
A-I (Flexion malposition) and C-3 (Decompensation of adaptational curvatures).
|
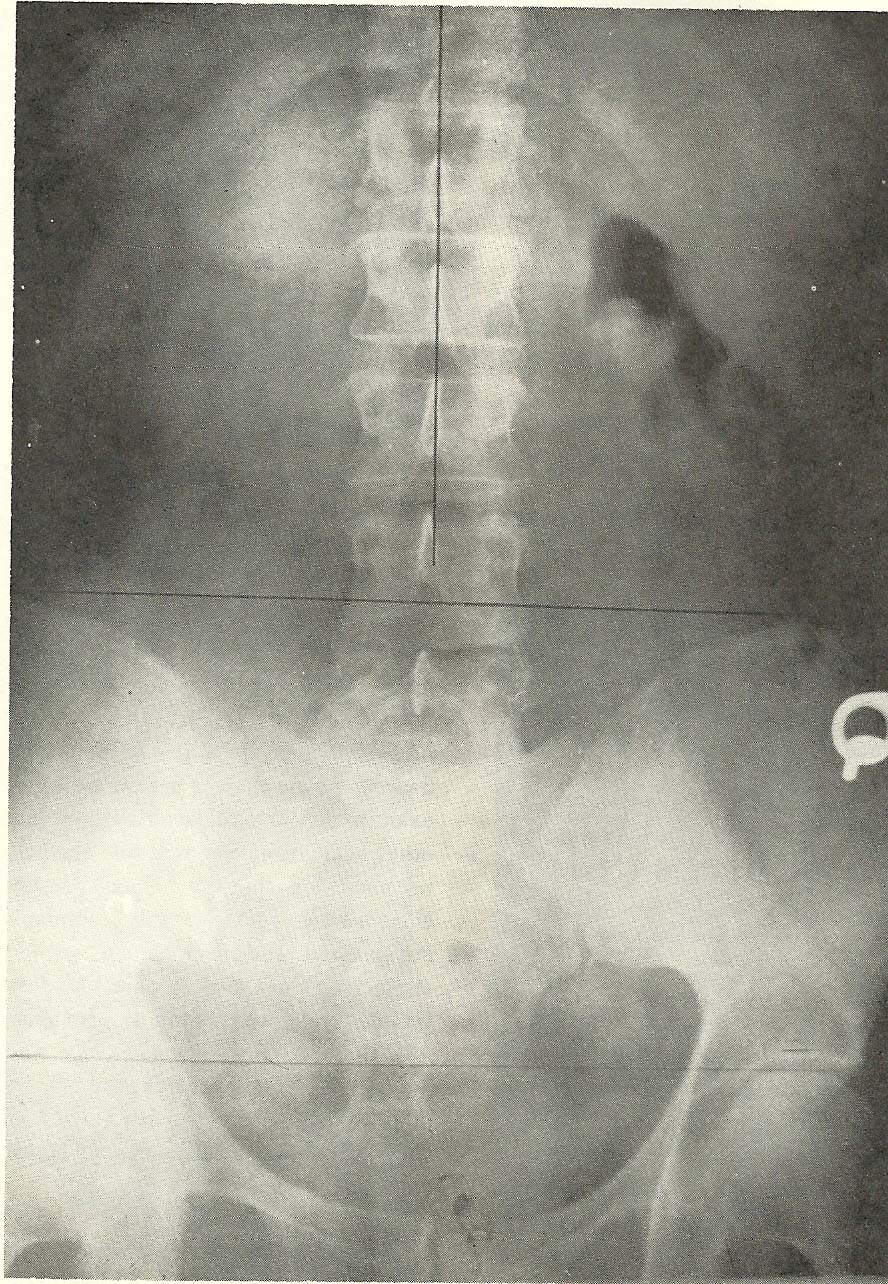
Note that there is a mild right-inferior pelvic tilt due to deficiency of
the right lower extremity in the film shown in Figure 6.21. Yet, there is no
distinct evidence of a lumbar scoliosis to the right as would normally be
expected. This interesting finding was observed as one of the roentgenographic
findings in the following case presentation. |
|
|
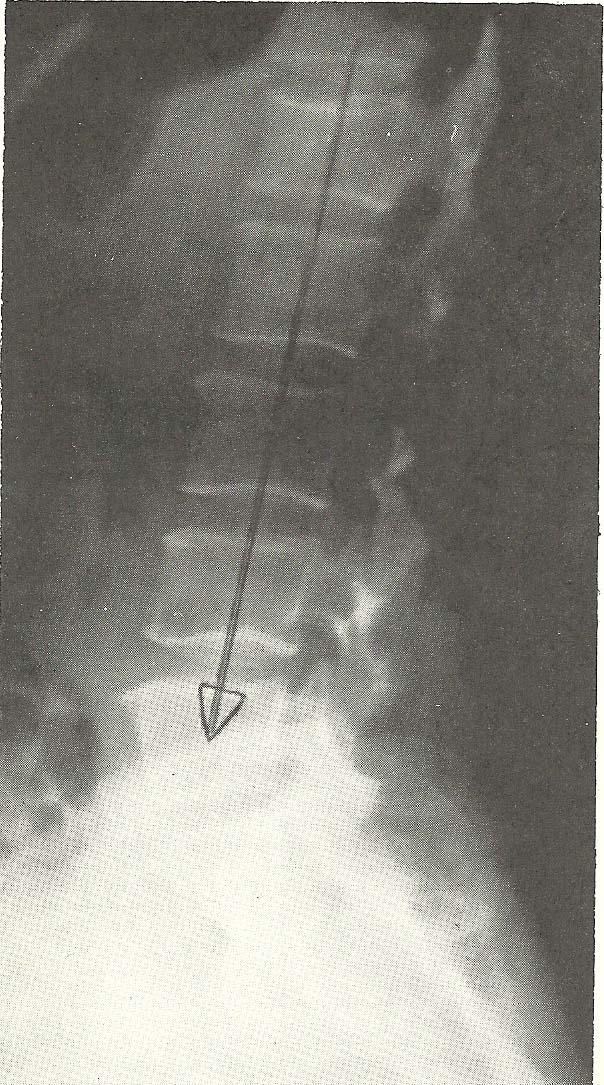
The lateral lumbar view (Fig. 6.22) shows a marked flexion subluxation of
L4 over L5 (A-1). In addition, we see loss of interosseous spacing at L5 and
S1. No other evidence of osseous or soft-tissue abnormality is noted on this
film. |
|

|
Case Illustrating Classifications
A-I (Flexion malposition) and B-2 (Scoliosis and/or alteration of curves secondary to structural asymmetries)
In this case, films of a 48-year-old female show a patient who has
sustained a torsion-flexion injury to the cervical spine when the automobile
she was driving was struck at the left front. She was taken in a conscious
state to the emergency room of the nearest hospital where she was given only a
brief examination and released without roentgen study or other evaluations.
She was told she lacked injuries and had no need for therapy. On presenting
herself to chiropractic service, she complained of marked stiffness of the
neck, blurred vision, vertigo, neck pain, and severe pain at both temples. She
reported no previous neck injury. |
|

|
In the forward-flexed position film (Fig. 6.24), hypermobility (B-2) of C4 is seen as a definite segmental subluxation of the hypermobile type. |
|
|
In the cervical extension position, restriction of the total range of mobility is seen (Fig. 6.25). |
|

|
The right posterior oblique film in flexion (Fig. 6.26) discloses unilateral hyperflexion of C4 over C5 and C5 over C6, with widening of the IVFs. |
|

|
The general alignment on the A-P
film is good (Fig. 6.27). |
|
|
Case Illustrating Classifications A-2, A-3, A-8, C-1, and C-2
One of the most common subluxations found in the lower back is that of
hyperextension of the vertebral motion unit. This usually accompanies, or is
caused by, a posterior shift of weight bearing and is frequently found
associated with an increased lumbosacral angle. It is characterized on film by
an approximation of the spinous processes, extension or imbrication of the
facet articulations, and posterior wedging of the interbody disc space. |
|
|
The oblique projection (Fig. 6.29) shows the downward displacement of the
L4 articular process relative to the opposing superior articular process of
L5. he contralateral oblique film demonstrates facet disrelationship on this
side that even more marked than that seen on the other side (Fig. 6.30). |
|
|
The right anterior
oblique film (Fig. 6.30) shows similar but less marked jamming of the facet
on the left. Reactive scoliosis is also obvious. |
|
|
In the A-P projection (Fig. 6.31), we see a rather severe right
inclination of the vertebrae above L5, which produces a right rotoscoliosis
extending into the thoracic spine and including the vertebrae above those
visualized in this film. |
|
|
Extension subluxation (A-2) at L4-L5 (not shown).
Severe right lateroflexion subluxation at L4-L5 (A-3) in this case, at
least partially due to asymmetrical structural development.
Scoliosis cephalic to L4 from the L4-L5 facet asymmetry. Muscular
imbalance is also a factor in this scoliosis (C-1).
Narrow interosseous spacing at L5-S1 (A-8). Discopathy is the cause of the narrowed spacing at L5-S1, and there is resultant facet arthrosis.
As explained previously, the presenting complaint in this case was
low-back pain with sciatic neuralgia radiating down the left leg to the ankle.
The patient came to the doctor of chiropractic after having spent 2 weeks in
the hospital where hot packs, bed rest, and traction provided little relief.
He was taking Robaxin (methocarbanol), which gave little comfort, and said
that his MD had told him he was suffering from a "disintegrated disc."
Examination showed him to be in severe pain, with an obvious antalgic
posture. He was guarding his movements very cautiously. The pain was so severe
that a full physical examination could not be made. All low-back motions were
severely restricted, and sitting aggravated the pain. The patient was wearing
a back support provided by the orthopedic surgeon. Orthopedic tests brought
out the following signs:
Lasegue SLR: positive on right at 80°, left at 10°.
Goldthwait: positive on the left.
Well-leg raising: positive on the right.
Lewin supine: pain on left.
Gaenslen: positive on the left.
Kernig: positive on the left.
Leg rocking: positive on the left.
Ely's test: positive bilaterally.
The diagnosis was Grade 4 disc syndrome, and especially careful
chiropractic manipulation was started. A sitting disc adjustment afforded
marked relief almost immediately. He was then sent home to bed. The following
day the patient called and was in too much pain to come for treatment.
Two weeks from the date of first visit, he presented himself in worse pain
than at the time of the initial visit. He had been in the hospital for a week,
having been released the day before this visit. The orthopedic surgeon had
recommended disc surgery, and he was scheduled for a myelogram the next day.
A chiropractic adjustment again gave marked temporary relief. He was advised
to return home to bed and to have another treatment the next day. The DC's
reasoning concluded, since each adjustment helped temporarily, further
treatment might be worthwhile. However, the patient did not appear for
treatment the next day. A telephone call reported that he had returned to the
hospital. Disc surgery subsequently showed posterolateral herniation on the
left at L4.
Case Illustrating Classifications A-2, A-2, A-6, A-9, and C-1
A 57-year-old female presented herself to a DC's office with the primary
complaint of low-back pain, which began approximately 6 days previously when
she was bent over to dust furniture. She had a history of low-back pain
approximately 10 years before this incident. The patient had a chronic
complaint of stiff neck, suboccipital headache, tinnitus, and frequent
paresthesias in both upper limbs, especially along the lateral aspect.
Physical examination showed:
(1) Blood pressure, 128/78.
(2) Pulse rate, 84.
(3) Auscultation of the heart and lungs revealed no abnormality,
(4) Abdominal palpation revealed no masses but some tenderness over the descending colon.
(5) Examination of the eyes, ears, nose and throat was unremarkable.
(6) On neurologic evaluation, the left patellar reflex was reduced. Other reflexes were normal. A mild hypesthesia was present along the lateral aspect of the right forearm and distally to the thumb. Passive elevation of the legs resulted in pain in the area of L4 and L5. Lasegue's SLR test was negative but restricted in range due to tight hamstring muscles.
(7) Because of a history of high serum cholesterol, blood was taken for this determination. Laboratory reports showed a cholesterol level of 257 mg%.
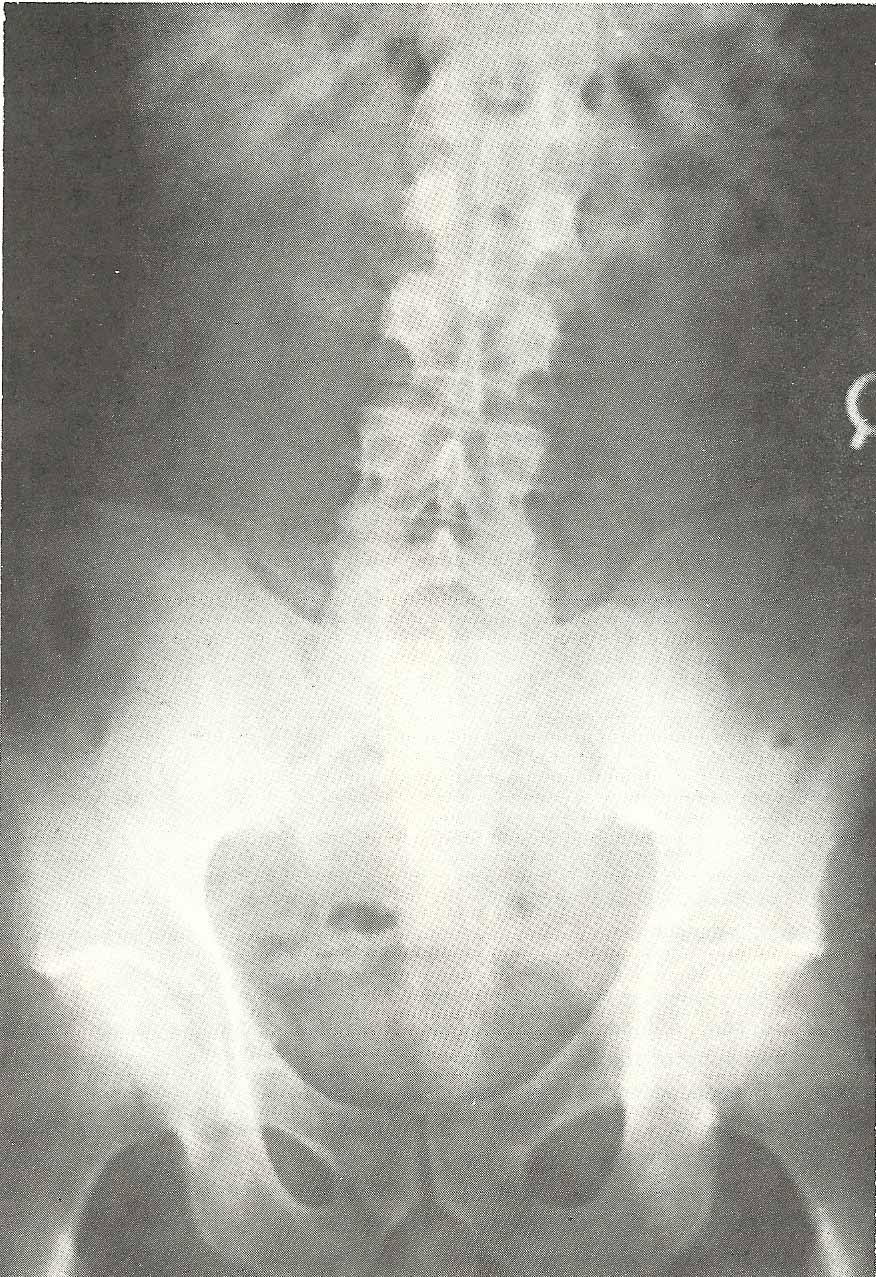
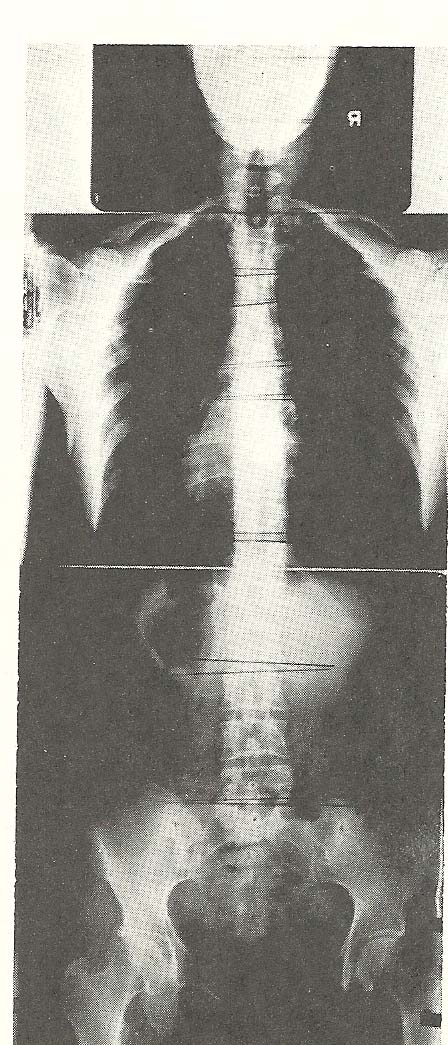
In the A-P film of the lumbar spine and pelvis (Fig. 6.32), a level pelvis
and sacrum is seen. |
|
|
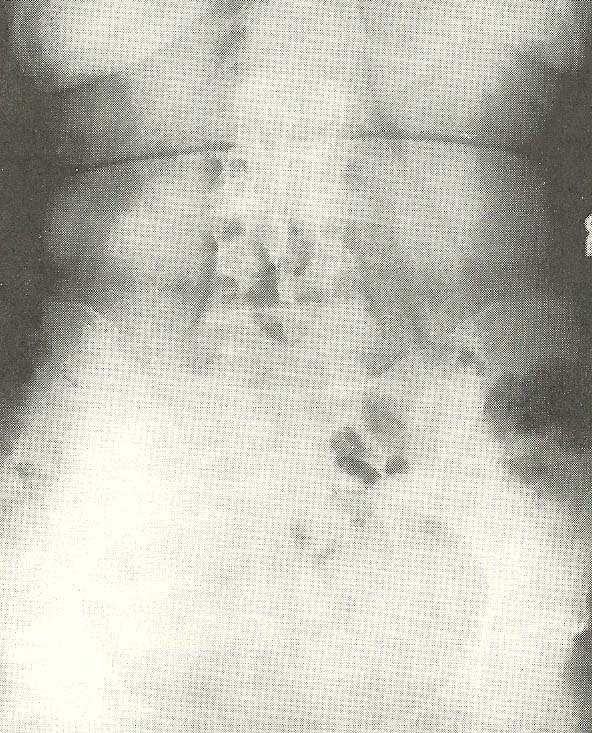
The next film, a lateral lumbar view (Fig. 6.33), disclosed an extremely
marked hyperextension of the lumbar spine in general, with specific segmental
hyperextension occurring especially at L4 on L5, L3 on L4, and L2 on L3. |
|
|
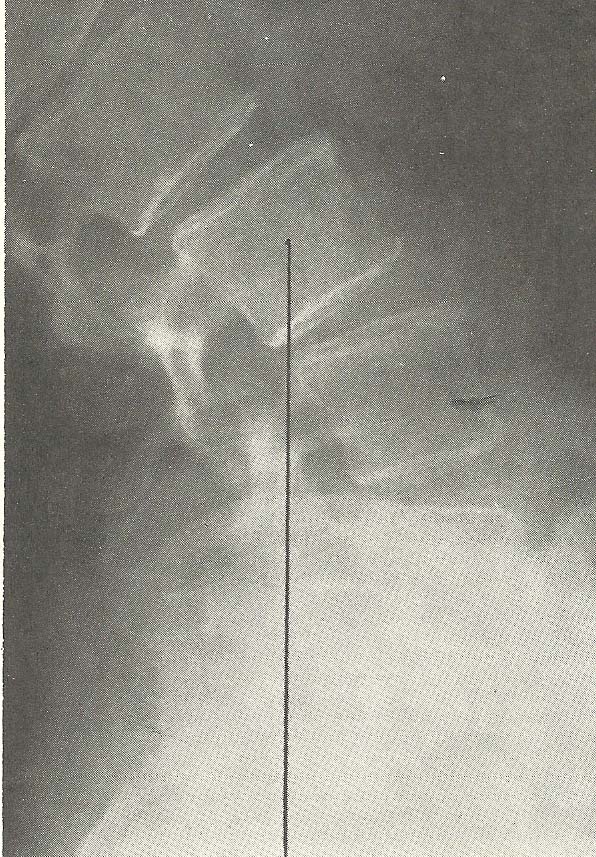
The cervical films reveal several deviations from normal spinal alignment,
the most obvious of which is the retrolisthesis of the C5 segment (A-6). |
|
|
The cervical films reveal several deviations from normal spinal alignment,
the most obvious of which is the retrolisthesis of the C5 segment (A-6). |
|

|
Case Illustrating Classifications A-3
The radiograph shown in Figure 6.36 reveals an easily demonstrable left
lateral flexion subluxation of C3 upon C4 (A-3) and C4 on C5. |
|

|
Case Illustrating Classifications A-3, C-3, C-4, and D-1
The lateral lumbar view shown in Figure 6.37 is that of a 57-year-old
female. There is a loss of the normal lumbar lordosis. |
|
|
The anteroposterior full-spine films (Fig. 6.38) exhibit several
lateral flexion-type subluxations (C-3) and a rotational type at the level of
L5 (C-4). |
|
|
Case Illustrating Classifications A-3
A 53-year-old male presented himself to a chiropractic office with a
complaint of very acute lumbar pain with radiation into the right gluteal area
and posterior thigh. His pain started at his place of employment when he had
reached to the left in a slightly flexed position to pick up an object of less
than five pounds. He felt a sharp stabbing pain in the lower back and was
unable to straighten. He was taken to the plant infirmary where diathermy
treatments were applied, but these did not alleviate the symptoms. On
presenting himself for chiropractic care, he had great difficulty walking.
|
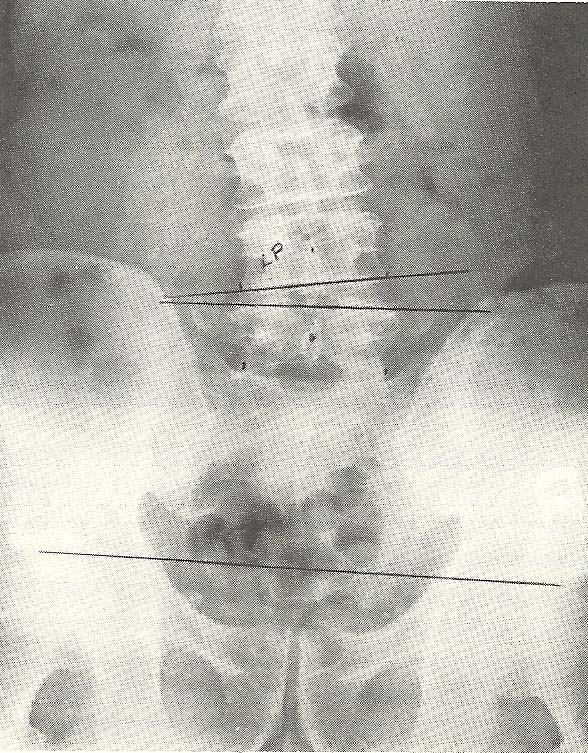
The A-P lumbopelvic film (Fig. 6.39) demonstrates an acute rotary and left
lateral subluxation of L4 (A-3), and there is a slight left posterior body
rotation of this segment relative to L5. |
|
|
The second film (Fig. 6.40), which was taken several days later, shows
complete reduction of the L4 subluxation. |
|
|
Case Illustrating Classifications A-4
This 53-year-old housewife presented herself with a complaint of neck
stiffness when awakening in the morning that was associated with stiffness and
discomfort in the right shoulder area. She said her problems brought on
headaches and a decreased ability to move her neck comfortably. She reported
episodes of this problem occurred frequently for a duration of more than 30
years. The length of her current problem was approximately 3 weeks.
In the past, she had obtained considerable relief from her symptoms
through chiropractic manipulative therapy, but her usual doctor of
chiropractic had retired. She said that medication prescribed by several
medical doctors had been of no help. The MDs who had examined her had told her
she had arthritis in her neck, and one told her "nine tenths of her body" was
so affected. She reported that she had been in three automobile accidents:
1940, 1943, and 1965. Exercise seemed to aggravate her symptoms. Her only
other presenting complaint was occasional low backache.
Her history revealed chronic eye strain and visual impairment. Chronic
postnasal drainage, supposedly associated with sinusitis, an appendectomy at
age 17, and partial hysterectomy at age 40 were revealed. She smokes 1-1/2
packs of cigarettes daily and drinks alcoholic beverages occasionally. No
liver or gallbladder symptoms were expressed.
Physical examination showed normal vital signs and an abdominal scar from
a hysterectomy but little else of significance. Orthopedic and neurologic
evaluations showed no abnormalities except a slight decrease in rotatory
cervical movements and some spasticity of the neck muscles. No orthopedic
tests were positive. The neurologic examination was normal except for slight
exaggeration of deep tendon reflexes in both arms and legs. A CBC showed
normal values. The erythrocyte sedimentation rate and RA latex determinations
were negative. Urinalysis revealed no abnormal findings.
Routine x-ray examination of the cervical spine showed a relative
hypolordosis and a slight right convexity of the neck, with the head tilted
slightly to the left in normal posture. No significant degenerative or other
pathologic changes were noted. In fact, for her age and history, the lack of
obvious degenerative changes was remarkable.
The lateral cervical film (Fig. 6.41) shows evidence of rotational
disrelationships of the midcervical vertebrae (A-4). The axis and atlas show
relatively little rotation, but the articular processes of C2 are superimposed
over one another. To the contrary, C3 shows its articular processes to be
quite distinctly not superimposed. C4 is similarly rotated but less markedly
so. C5 and C6 show increasingly less rotation as evidenced by articular
superimposition. C7 is also neutral in rotation; its articular processes are
superimposed in the lateral view.
The A-P open-mouth film (Fig. 6.42) confirms the vertebral rotation. The
left head tilt causes rotation of the axis with its spinous process right of
central. This is the normal position for C2 with the head tilted left and no
significant facial rotation.
The lower cervical A-P film (Fig. 6.43) shows increasing deviations of
spinous processes to the right of central cephalad from C3 to C7 and the C3
vertebra shows the greatest deviation. The facets, as revealed by oblique
films (not shown), appear to be adequately aligned, and the neutral foramina
were patent.
To summarize the x-ray findings, we saw no demonstrable degenerative
disease. Rotational subluxations (A-4) are apparent in the midcervical region.
Treatment by chiropractic manipulative therapy brought prompt relief of
symptoms. She experienced a mild return of symptoms after 5 days, and returned
for further treatment a week following her initial visit. Weekly visits for 2
weeks more and another after a 2-week interval found her to be comfortable,
with no return of symptoms. She returned a month later with a mild recurrence
of symptoms, which were quickly alleviated. Two months have elapsed without
her return for further treatment. A telephone check showed her to be
asymptomatic.
Classification of Radiologic Manifestations
Case Illustrating Classifications A-4 and C-2
A 62-year-old Caucasian male presented himself to a chiropractic office
with the primary complaint of "gnawing" pain in the left hip. This condition
had existed for about 6 months, and the history further revealed a weight loss of
approximately 30 lbs since the previous October. At that time, he had
experienced upper abdominal pain and, after hospitalization, had been
diagnosed as having diabetes mellitus. He was placed on oral medication. The
weight loss had occurred in the interim from October to June. He had received
periodic "blood tests" that apparently were related to blood sugar
evaluations.
Physical examination revealed:
(1) normal blood pressure and pulse rate,
(2) slight systolic murmur over the mitral area,
(3) normal and equal deep tendon reflexes,
(4) abdominal palpation found hepatic and splenic enlargement,
(5) bilateral pitting edema of the lower extremities was elicited, and
(6) prostatic examination revealed mild hypertrophy.
The orthopedic evaluation revealed:
(1) bilateral leg lowering, positive left;
(2) Patrick's test, positive left;
(3) Lasegue's SLR test for the right leg caused pain on the left side;
(4) deep tenderness to pressure was found at the level of L3 bilaterally; and
(5) the lumbar range of motion was normal, although there was some pain in the left hip on left side bending.
The A-P film of the lumbar spine and pelvis (Fig. 6.44) demonstrates a
mild scoliosis due to structural asymmetry (a right lower-extremity deficiency
a definite right rotary subluxation
of L3 relative to L4 (A-4). Evaluation of the abdominal soft-tissues revealed
an inferior displacement of both the splenic and hepatic flexures of the
colon. The inferior border of the liver can be seen below the level of the
iliac crest, and the inferior border of the spleen is seen at the level of the
iliac crest. Although these films were taken in the upright position, the
probability of splenomegaly and hepatomegaly existed.
The oblique spot film of the left hip reveals a very mild degree of
degenerative joint disease (Fig. 6.45). The lateral lumbar film (Fig. 6.46)
shows mild proliferative change but with good maintenance of lumbar disc
spaces. There is a slight degree of lumbar hyperextension and osteoporosis.
The patient was instructed to return to his family physician for further
laboratory evaluation, only to be told that his weight loss was due to the
diabetes. During the interim, he received chiropractic care for his original
complaint of hip pain. Within 2 weeks, a marked improvement in the symptom
pattern was experienced, and he began to walk without favoring the left side.
During the course of treatment, trigger-point therapy was given and the
patient developed hematomas at the trigger-point sites. It was at this time
that the DC insisted on drawing blood, even at his expense, to do a CBC. The
report showed 386,000 WBCs. A diagnosis of probable myelocytic leukemia
(chronic) was made, and the patient was again referred to the family physician
--this time with full lab reports preceded by a phone call. The patient was
treated for the leukemia by chemotherapy, and the DC continued to treat the
hip disorder. The chiropractic diagnosis was one of L3 nerve root radiculitis,
with extension to the left hip.
Following 3 months of chiropractic therapy, the second A-P film was taken.
By use of a heel-lift, the pelvic tilt was somewhat corrected and the rotation
of L3 over L4 was reduced. The patient was released completely asymptomatic
relative to his primary complaint. He has not had a recurrence of this pain.
Classification of Radiologic Manifestations
Case Illustrating Classification A-5 (Spondylolisthesis)
Another classification of subluxation is spondylolisthesis. In this case,
we have a 46-year-old male who not only exhibits a classic spondylolisthesis
but also manifests many problems encountered in the average chiropractic
practice. These problems include a history of trauma involving litigation that
eventually resulted in a permanent disability award under Social Security,
which qualified him for Medicare coverage.
The patient stated that, while walking across a temporary ramp at a
building under construction, he caught his heel on a nail and fell with a
twisting motion. This resulted in immediate pain in the lower back and left
buttock area. His lower back continued to hurt and steadily became worse, with
the pain extending the full length of the left leg. He said he had never had
symptoms of back trouble before this accident.
The patient was taken to a chiropractic office and was ambulatory with
assistance. He had difficulty supporting his weight and undressing for the
examination. He was unable to perform any mobilization test for the lower
back. All passive tests for the low back were positive. There was severe
trigger-point tenderness bilaterally from the lumbosacral joint, symptoms of
left sciatic neuralgia, rigidity in the lower lumbar muscles, and the deep
reflexes of the lower extremities were sluggish.
The lateral radiograph (Fig. 6.47) reveals a distinct anterior
displacement of L5 in relation to another peculiarity of this case, a
transitional lumbosacral segment. This transitional segment is immovable
because of synostosis with the sacrum on the left. Therefore, the segment
above (L5) becomes the lowest freely movable vertebra in the spine (Fig.
6.48).
This anterolisthesis subluxation (A-5) can be graded by several methods,
one of which is a percentage evaluation of anterior body displacement. We
value this as a 20% spondylolisthesis (Grade 1).
In typical cases, the predisposing factor toward spondylolisthesis is a
defect where there is no osseous connection at the pars interarticulari. It
may be bilateral or unilateral. A pars defect, a spondylolysis, is best
visualized only on carefully positioned oblique views. Here, the spondylolysis
is well demonstrated in both right and left views (Figs. 6.49 and 6.50).
Chiropractic treatment was started in an attempt to improve biomechanical
function of the lower spine. This was accomplished to a great extent within 3
months. However, the spondylolisthesis and spondylolysis are irreversible and
will result in continued instability. Periodic treatments as clinically
indicated may be required, depending on the patient's activities.
Classification of Radiologic Manifestations
Case Illustrating Classifications A-5, A-6, A-8 and A-9
This case again shows coexistence of several classifications of
subluxations and serious alteration of mechanical functioning of the neck.
This 65-year-old female gave an extensive history of many illnesses and
consulting many doctors of various specialties over several years. Her history
revealed many complaints, both old and recent. She had experienced radical
mastectomy of the left breast 21 years before her first consultation at a
chiropractic clinic. Her chief complaint on the first visit was continuous
neck pain of 4--5 weeks duration. She also complained of chronic occipital
headaches, eye pain, pain radiating into the left shoulder, paresthesias of
the neck and left arm, and pain sometimes extending to the left elbow.
Questioning revealed a history of "arthritis" affecting her neck and low
back, gastritis and intestinal disturbances with discomfort after meals,
nervousness, and pain on micturition on occasion for which she consults a
urologist and periodically has urethral dilatation. These conditions were of
several years duration and for which she takes prescribed medication. She had
a L5 laminectomy 5 years ago, a hysterectomy at age 49, a cholecystectomy at
age 30, surgery for an ectopic pregnancy when in her 20s, and an appendectomy
while in her 20s. She suffered bronchopneumonia on one occasion in youth. A
year before her visit to the chiropractic clinic, she had experienced viral
pneumonia.
Physical examination showed her to be obese at 160 pounds for her height
of 5 feet 2 inches. Her vital signs were essentially normal, with blood
pressure of 130/78 left brachial; 136/80 right brachial. The significant
abnormal findings were:
(1) Obvious postural distortion, especially in the neck, which carried toward the anterior. There was pain on the extremes of neck motion, with slight diminution in range of motion.
(2) The cervical compression test was positive bilaterally, worse on the left.
(3) Moderate lymphedema of the left arm.
(4) Absence of the left breast.
(5) Several scars over the abdomen and lower back consistent with the surgical history.
(6) Tenderness over the stomach and flexures of the colon. Other abnormal findings were apparent.
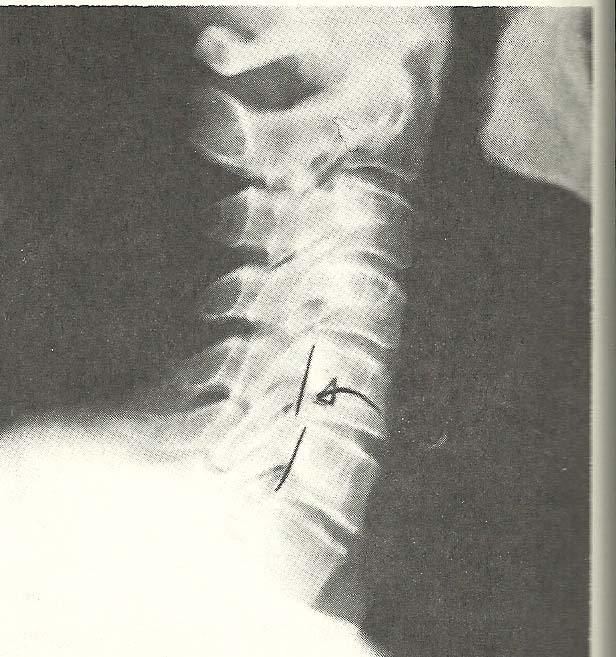
Cervical spine films revealed several abnormalities. Significant
generalized osteoporosis was evident by the relative radiolucency of osseous
structures and lack of trabeculations within the visualized bone. Spondylotic
hypertrophy and spurring of vertebral body margins were not severe but present
throughout the neck. Sclerosis of the articular facet surfaces is evidence of
degenerative joint disease. The disc narrowing at C4-C5, C5-C6, and C6-C7 is
noted. Several subluxations are apparent on the neutral lateral film alone
(Fig. 6.51). C2 shows slight anterior displacement upon C3, with C4 (A-5)
showing more anterior disrelationship relative to C5. C5 shows posterior
displacement upon C6 (A-6). The anterior carriage of the head alters the
cervical lordosis.
The lateral film taken during flexion of the neck fails to reveal
significant overall reduction in flexion, but a little flexion is seen at the
atlanto-occipital motion unit (Fig. 6.52). The anterior disrelationship of C2
upon C3 and C4 on C5 is not significantly altered during flexion, but the
posterior disrelationship of C5 upon C6 is improved.
General extension of the neck is adequate with all motion units extending
to the greatest degree allowed by structure (Fig. 6.53). In hyperextension,
there is no apparent alteration of the anterolistheses at C2-C3 and C4-C5, but
the retrolisthesis at C5-C6 is exaggerated as compared to the position in the
neutral lateral film.
The open-mouth A-P film is essentially unremarkable, but the A-P of the
lower cervical region (Fig. 6.54) shows considerable proliferative change of
the posterior facets at C4-C5 on the right and less hypertrophy at other
levels.
The oblique films (Fig. 6.55) show encroachment of the neural foramina at
C3-C4, C4-C5, C5-C6, and C6-C7 on the left with similar changes on the right
due to the uncovertebral arthrosis and uncinate hypertrophy (A-9).
X-ray examinations of the thoracic spine and the low back were also
conducted. They showed severe osteoporosis and moderately severe spinal
degenerative disease. The L5 laminectomy was demonstrable. These films and the
chest studies (which were essentially normal except for the left mastectomy)
are not shown here.
In summary of the cervical spine x-ray findings, we note generalized
osteoporosis and spinal degenerative disease of moderate severity. The
subluxations observed were:
(1) Anterolisthesis at C2-C3 and C4-C5 (A-5). Note that these are not the usual spondylolistheses seen in the lumbosacral area that show defects in the pars interarticulari. These anterolistheses are allowed by the disc and articular degenerative changes. They do not change significantly in flexion or extension of the neck.
(2) Retrolisthesis at C5-C6 (A-6), which is somewhat unstable and shows moderate hypermobility and abnormal motion on neck flexion and extension.
(3) Foraminal alteration or encroachment (A-9) at nearly every level in the neck bilaterally due to degenerative change and malposition of the vertebrae.
(4) Decreased interosseous spacing (A-8) from disc degeneration.
(5) Aberrant motion (B-3) with various motion abnormalities seen on stress study.
Blood chemistries and serology did not reveal significant deviations from
normal. Hematology showed a slightly low hemoglobin (11.5 grams), but
otherwise was essentially normal. Urinalysis did not show significant
abnormality.
This patient was treated with conservative chiropractic care and
encouraged to continue with the medical specialists who were attending her
when she consulted the chiropractic clinic. She showed slow improvement in the
neck and shoulder pain, and the headaches diminished in severity and
frequency after only a few treatments. She continued under chiropractic care
for almost 2 years, receiving frequent treatments for approximately the first
2 months of care, at which time she was advised that her problems would
probably show little further improvement. She felt that she received benefit
from the treatments and continued to present herself once or twice a month
after that. Subsequent x-ray films of the spine were made after 14 months.
They showed essentially no change. At her last visit, somewhat more than 2
years after the initial chiropractic examination, she was only slightly
improved, having many complaints and experiencing only temporary relief
following treatment.
Classification of Radiologic Manifestations
Case Illustrating Classification A-7
We see here an unusual complex of anomalies accompanied by a
laterolisthesis type of subluxation (A-7) and a gross postural alteration.
This 55-year old pharmacist complained of severe, nearly constant, pain
affecting the lower back. He had suffered from varying degrees of low-back
pain for most of his life. The problem became progressively worse with
advancing age.
The gross trapezoidal shape of the lower two lumbar segments shown in
Figure 6.56 shows the result of anomalous segmentation. A hemivertebra may
take varying forms. In this case, there are two half vertebrae forming the
right portion of the upper trapezoidal segment and two half vertebrae forming
the left portion of the lower segment. These are completely fused, resulting
in a grossly unlevel superior surface of the lowest mobile vertebra. This
causes a severe disrelationship combining rotational and lateral displacement
(a laterolisthesis subluxation).
These gross abnormalities are expected to cause eventual degeneration
despite proper maintenance care. In review, we can arrive at a diagnosis of
double hemivertebra of the lower lumbar segments with a laterolisthetic
subluxation (A-7).
Classification of Radiologic Manifestations
Case Illustrating Classifications A-1, A-3, A-4, A-7, and A-8
A 65-year-old male laborer presented himself for chiropractic care. He
reported a primary complaint of acute low-back pain centering between L2 and
S1 and was unable to work because of the pain. His history revealed very
little low-back pain before this incident despite his heavy work. The pain
was precipitated by a fall on ice.
Physical examination was relatively unrevealing except for the following
orthopedic tests:
(1) Hyperextension of the lumbar spine produced increased pain.
(2) Lasegue's SLR and Goldthwait's tests were positive bilaterally.
(3) The lumbar ranges of motions were markedly restricted in all directions.
(4) The normal lumbar lordosis was flattened.
X-ray films of the lumbar spine were taken that revealed left lateral
flexion of L5, which was best noted in the AP film (Fig. 6.57) by the
approximation of the left transverse process of L5 to the left sacral ala
(A-3). Severe rotational disrelationship of L4 to L5 (A-4) with slight right
lateral flexion of L4 on L5 has produced a left laterolisthesis (A-7) of L4.
L3 showed less rotation than L4, and L2 was in a position of reverse rotation
(A-4) to the right so that an unusual left lower lumbar rotoscoliosis was
formed with a slight right rotoscoliosis in the thoracolumbar area.
The lateral film showed decreased interosseous spacing (A-8) throughout
the lumbar spine, with the least amount of disc narrowing noted at L4-L5. Loss
of normal lumbar lordosis is also exhibited (Fig. 6.58). These changes have
produced multiple flexion disrelationships (A-1), particularly in the upper
lumbar area. Both A-P and lateral films showed marginal proliferative changes
that were evidence of chronic disc degeneration. Moderate generalized
osteoporosis is also present. By correlating these findings, a working
diagnosis was made of lumbosacral strain with myofascitis superimposed on
moderate spinal degenerative disease.
The subluxations noted are of several types, including:
(1) laterolisthesis of L4 on L5 (A-7);
(2) decreased spacing throughout (A-8);
(3) flexion malposition of the upper lumbar vertebra (A 1);
(4) left lateroflexion of L5 on the sacrum (A-3); and
(5) reverse rotation of L3 on L4 and of L2 on L3 (A-4).
Conservative chiropractic therapy was started. The patient was seen six
times over a period of 4 weeks, with complete relief of symptoms. He could
return to work after 10 days of treatment and was subsequently discharged with
the advice that he should return for care as symptoms warranted. With the
degree of degenerative changes present, he will likely have recurrent low-back
problems.
Classification of Radiologic Manifestations
Case Illustrating Classification A-8
A 58-year-old housewife presented with a primary complaint of heavy aching
pain between the shoulder blades, with a tendency toward sharp cutting pains
to the front of the chest on awkward movement or coughing. She further
complained of difficulty in breathing at times. These symptoms had occurred
periodically over the past 5 years and were becoming more frequent and severe.
Physical examination did not show significant alteration of normal
cardiovascular or pulmonary function. A detailed spinal examination revealed
rigidity and tenderness of the thoracic paraspinal muscles, especially on the
right in the lower thoracic area. Muscle testing against resistance
demonstrated weakness of both divisions of the pectoralis muscles bilaterally.
The lateral film shows marked narrowing of the intervertebral disc spaces
throughout the thoracic spine (A-8). Note reactive hypertrophic and sclerotic
changes along the vertebral body margins, indicating a chronic condition (Fig.
6.59). This film definitely exhibits decreased interosseous spacing at
multiple intervertebral levels. These subluxations, associated with
thoracocostal myofascitis, and the other findings led to a working diagnosis
of moderately severe thoracic degenerative disease.
Conservative chiropractic management was begun and, after six treatments
over a period of 2 weeks, considerable symptomatic relief was obtained. After
that, weekly adjustments were advised that resulted in continued improvement.
She was relatively symptom free after 4 more weeks. The patient's diagnosis
suggests that she will have periodic recurrence of symptoms requiring further
treatment.
Classification of Radiologic Manifestations
Case Illustrating Classifications A-1, A-3, A-4, A-8, and A-9
The x-ray views presented next are those of a 69-year-old female (Figs.
6.60--6.62). There is foraminal narrowing at four levels on the right and two
on the left due to proliferative changes (A-9). Flexion subluxation exists at
C4 (A-1), and marked interspace narrowing is found at C5, C6, and C7 (A-8). A
loss of normal cervical lordosis is evident. Rotary subluxation is present at
C2 and C3 (A-4). Also note the generalized osteoporosis.
This lady complained of objective vertigo, tinnitus, and suboccipital pain
and pressure. She had consulted her family physician 2 weeks previously, at
which time she received an ECG, chest x-ray, and several blood tests. She was
informed that nothing serious was wrong and her symptoms were related to a
"weak chest."
Chiropractic examination revealed the following pertinent information:
(1) blood pressure, 190/110;
(2) pulse, 108;
(3) height, 5 feet 5 inches;
(4) weight, 123 lbs;
(5) cicatrix formation of the left tympanic membrane due to an old rupture;
(6) postnasal drip with hyperemia of the posterior pharynx;
(7) on auscultation, slight accentuation of the aortic sound; and
(8) the ranges of cervical motions showed restricted flexion and extension as well as in right lateral flexion; and
(9) a cervical compression test was positive bilaterally.
A working diagnosis of hypertension, possibly of neurogenic origin, was
made. The patient was placed on a program of conservative chiropractic care,
and after a month her blood pressure had stabilized in a range between 140/80
and 150/80. At the same time, her vertigo, tinnitus, and suboccipital pain
were eliminated, and the ranges of cervical motions were increased. She was
placed on supportive treatment at this time.
Classification of Radiologic Manifestations
Case Illustrating Classifications B-1, C-2, C-4, A-8, and A-9
The films of this case (Figs. 6.61--6.67) show alteration of the cervical
lordosis in the neutral lateral film and lessened ability to flex the neck,
coupled with slight hypermobility during neck extension (C-4).
As the cervical curve is naturally convex toward the anterior, alteration
of this pattern usually means pathology or significant injury to the skeletal
and/or supportive structures. Note in the neutral lateral film that there is
flexion of the C3 and C4 motion units.
With neck flexion, near total fixation or hypomobility from C3 through C6
motion units (B-1) is demonstrated. The atlantoaxial and atlanto-occipital
motion units show considerably diminished ability to flex (B-1).
Extension of the neck is accomplished, even to the point of hypermobility.
All motion units extend as far as structure allows so that the posterior
arches and spinouses approximate. By comparing the three lateral films (Figs.
6.63--6.65), we have an excellent example of abnormal mobility of a spinal
section or region (C-5). Intervertebral hypomobility is present at several
levels.
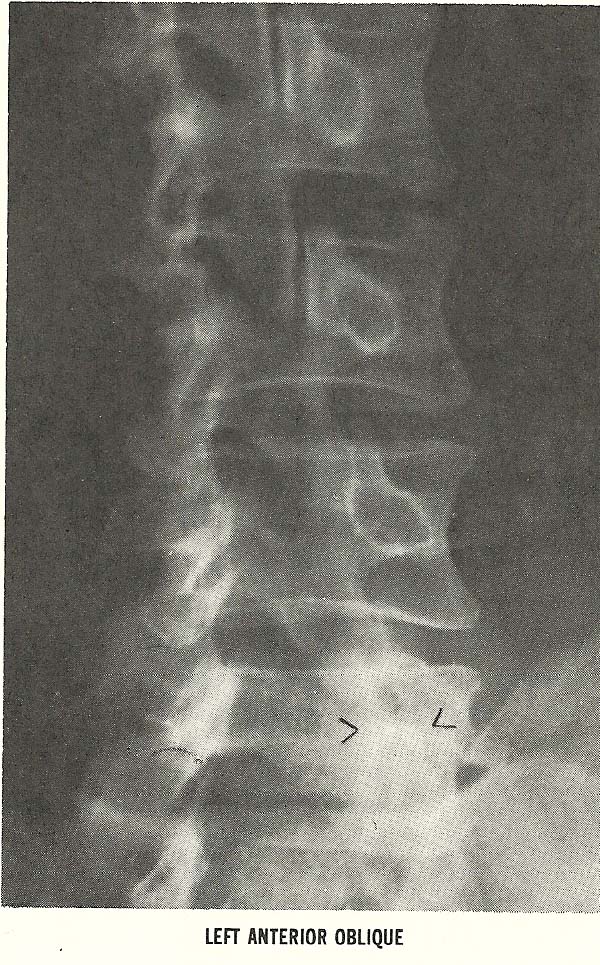
This case also exhibits manifestations of other radiologically evident
subluxations. The decreased disc height at C4-C5, C5-C6, and C6-C7, due to the
evident discopathy and spondylosis, is classified as decreased interosseous
spacing (A-8). The rather marked intrusion and compromise of the neural
foramina at C4-C5, C5-C6, and C6-C7, seen on the left anterior oblique film
(Fig. 6.66), and similar alteration of the foramina at the same levels
are shown on the right anterior oblique film (Fig. 6.67), also meet the
criteria of subluxation under the classification of foraminal encroachment
(A-9).
The patient is a strong 66-year-old male who has continued to work as
manager of a solid-waste disposal plant though he had passed the age of
retirement. He was suffering from pain in the neck, which radiated to the
right shoulder. The duration of the complaint, at the time the x-ray films
were made, was 3 weeks. He had this complaint on several previous occasions
and each time had experienced an excellent remission of symptoms following
chiropractic treatment. He had not had similar pain for about 3 years prior to
the time he presented himself for chiropractic care for the current episode.
Views of the right shoulder, one of which is shown in Figure 6.68, were
essentially normal. Physical examination was largely unrevealing, except that
orthopedic testing showed grossly restricted ability to laterally bend the
neck to either side, and foraminal compression tests were positive
bilaterally.
The moderately severe degenerative disease the x-ray examination reveals
in this man's neck are chronic. The relatively short duration of the present
symptom complex suggests that his current pain is more related to neuralgia
from functional disturbance in his neck than to a chronic neuropathy. The
foraminal encroachment of sufficient magnitude and severity to suggest neural
canal stenosis.
Chiropractic adjustment and reflex techniques brought marked relief in
three treatments over a 1-week span. Two treatments the following week were
able to bring a near total remission of the pain. He continued with weekly
treatments for 2 more weeks, stating that he felt markedly better. Following
the 4th week of care, he was discharged from active treatment and advised to
return periodically as symptoms dictated. He has continued with monthly
visits, at his request, since he feels much better under such a regimen.
Classification of Radiologic Manifestations
Case Illustrating Classifications C-1, A-1, A-3, and A-8
Frequently several subluxations of different classifications are
demonstrable in spinal films of a specific patient. This case illustrates such
a situation. Alteration in the lumbar lordosis and an antalgic lateral list of
the lumbar vertebrae (both of which represent subluxations classified as C-1:
alteration of the spinal curve secondary to muscular imbalance) are noted.
Concurrently, flexion subluxation (A-1) is noted at L4 L5 and at L5-S1,
narrowing of the disc interspaces (A-8) being evident at both these levels.
Right lateral flexion of L4 upon L5 (A-3) can be suspected from the A-P
film (Fig. 6.69). Wedging of the disc interspace at L4-L5, narrow on the
right, is seen; and although the L5-S1 interspace is only poorly depicted on
the standard A-P film, it may be narrow on the left.
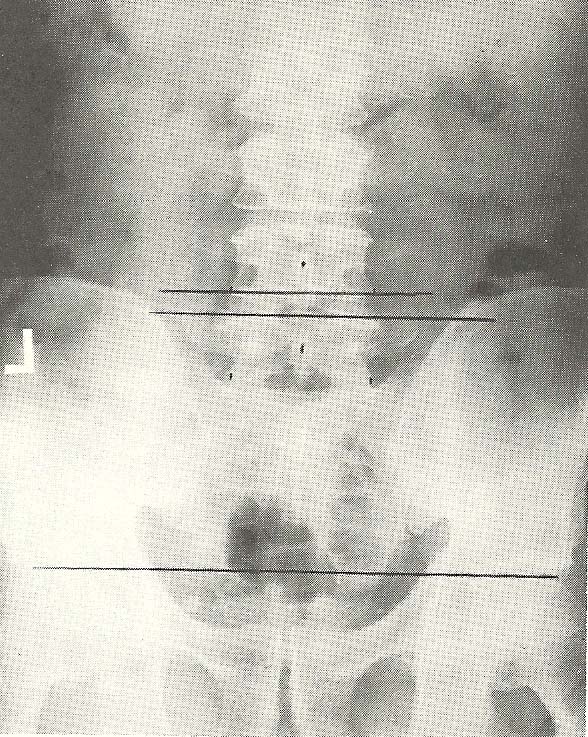
By use of the spot A-P film (Fig. 6.70), making the central ray
approximately parallel to the sacral base, the L5-S1 disc is better seen and
its wedging toward the left is more apparent. This projection gives an
excellent view of the lumbosacral junction and the extent of degenerative
spondylosis. The standard A-P and the lateral film (Fig. 6.71) showed the
obvious marginal spurring of the vertebral bodies at the two lowest motion
units.
Oblique projections gave an enhanced ability to visualize facet
articulations and are especially valuable in determining subluxations. The
left anterior oblique view is taken with the patient prone, then turned 45°
with the left side near the film (Fig. 6.72). This case shows the
approximation of L4 and L5 vertebral bodies and the extent of the spondylotic
changes along the vertebral body margins from L3-L4 caudally and depicts the
facet articulations. Note that the right L4-L5 facets show imbrication or
downward displacement of the L4 articular process relative to those of L5, the
discrepancy at the superior of the articulation being evident. Note also the
sclerosis of articular surfaces at this facet, which is evidence of
degenerative arthrotic changes. At L5-S1, there is also slight imbrication and
definite arthrosis.
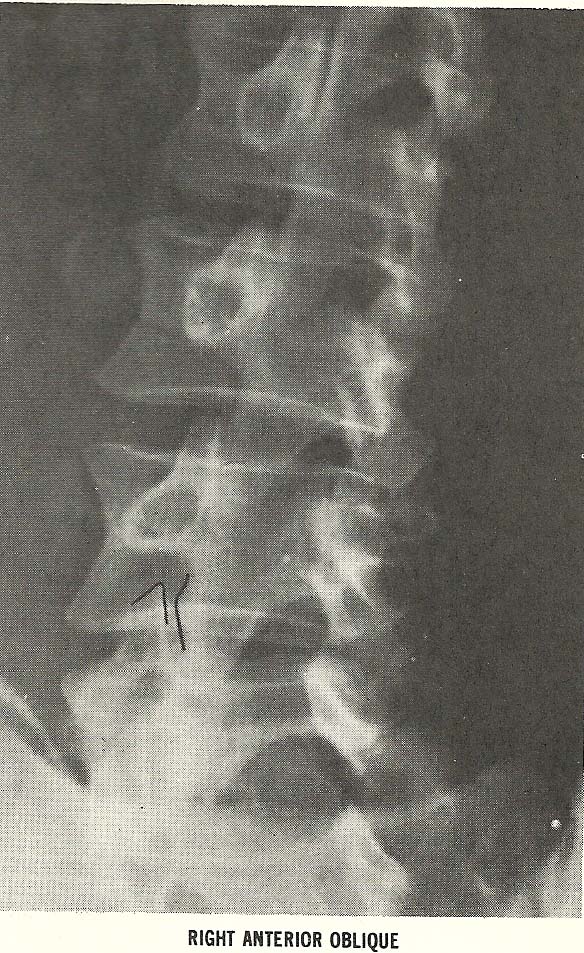
The opposite oblique film, the RAO, shows the left articular structure
(Fig. 6.73). In this film, the L4-L5 articular processes do not show
imbrication, but arthrosis is obvious. The presence of imbrication on the
right facet is seen on the other film. The lack of it on the left of this
motion unit verifies that there is right lateral flexion of L4 relative to L5.
At L5-S1, the obliquity of the facet articulation makes the facet joints less
easy to visualize. The marginal sclerosis of the articular processes shows a
degenerative reaction to chronic stress. Observe that the superior articular
process of S1 approximates the inferior surface of L5's pedicle on the left,
which is evidence of imbrication and verifies left lateral flexion of the
L5-S1 motion unit. Again, the spondylotic changes of the vertebral body
margins are easily seen.
To summarize the roentgenographic findings, there are:
(1) Degenerative spondylosis, facet arthrosis, and disc narrowing.
(2) Alteration of the lumbar lordosis and listing or deviation of the lumbar vertebrae to the right, presumably due to asymmetrical muscular spasticity, and antalgic mechanisms.
Several classifications of subluxation are evident:
(1) Decreased interosseous spacing (A-8).
(2) Flexion subluxation at L4-L5 and L5-S1 (A-1), which is incidental to the flattened lordosis and disc narrowing.
(3) Lateral flexion subluxations at L4-L5 and L5-S1, opposite inclination (A-3).
(4) Alteration of spinal curves due to muscular imbalance is also considered a subluxation of the spinal region or section (C-1).
This patient has a chronic low-back problem and has had recurrent episodes
of low-back pain for approximately 10 years. These usually result from
prolonged or strenuous work. He is a retired lithographer whose work often
required heavy lifting. His most recent complaints were of 2 weeks duration,
with pain predominantly perceived at the lumbosacral junction No radiation of
pain to buttocks or legs were reported. This disorder had been present since
the patient shoveled snow, and it remained relatively constant and of moderate
severity. Some relief was obtained while recumbent. He was in obvious discom-
fort both while sitting and standing. He had consulted with his family MD but
had not received satisfactory relief from the medication prescribed.
The physical examination findings were essentially within normal limits
for a 66-year-old male. Orthopedic tests revealed some restrictions in all
ranges of motion in the low back with no other significant positive findings.
There were no abnormal neurologic responses. Imbalance of the low-back
musculature was noted, especially weakness of the left psoas and quadratus
lumborum muscles and bilateral spasticity of the erector spinae muscles.
Conservative chiropractic treatment provided some relief after the first
treatment, and the patient was relatively asymptomatic after 10 days and three
treatments. Because of the history of recurrent problems and of moderately
severe spinal degenerative disease, the patient was advised that periodic
treatment would be helpful in discouraging recurrence of his pain, and that
exercises to strengthen the lower back and abdominal muscles, along with use
of a lumbosacral support during strenuous activity, might be of value.
Classification of Radiologic Manifestations
Case Illustrating Classification C-1 and A-1
Acute subluxations are frequently caused by or at least associated with
muscle spasm and imbalance following either major or minor trauma. The
following case is an illustration of this and demonstrates a rapid return to
normal after treatment alleviated the abnormal spasticity.
This patient first presented himself for chiropractic care after a minor
auto accident, following which he experienced transient neck pain. The initial
lateral cervical radiograph shows a normal to slight hyperlordotic cervical
curve, with hyperextension subluxations at C3 and C4, and little else (Fig.
6.74).
The second lateral cervical film --also a neutral lateral, at least as
nearly as his pain would allow, was taken 7 months after the first, the
exposure was made 3 days after a severe auto accident when his neck was
extremely painful (Fig. 6.75). Note the reversal of the lordosis (C-1) and the
definite flexion disrelationship at C3-C4 (A-1).
The third neutral lateral was taken 5 weeks after the second. In it, a
return to normal vertebral alignment is seen (Fig. 6.76). Chiropractic
manipulative therapy gave thorough relief within a few days after the first
accident.
The second, more serious accident, obviously caused more problems --both
to the patient and to the management of his case. After the second accident,
physical examination showed marked restriction of neck mobility and severe
pain even when the neck was not moved. Relief occurred following especially
careful chiropractic manipulation, and the patient was relatively asymptomatic
by the 4th week following the accident. Improvement had been steady from the
first treatment until that time. The diagnosis in this case was acute cervical
sprain.
Classification of Radiologic Manifestations
Case Illustrating Classifications C-2 and A-3
A 50-year-old male entered chiropractic care with a complaint of sharp
pain centering around the right hip and radiating down to the middle of the
anterior aspect of the right thigh. His history revealed malaria and scarlet
fever.
During the examination, it was determined that lateral flexion of the
lumbar spine to the left was markedly restricted. Flexion and extension were
adequate. Mild hypertension was encountered, though other vital signs were
unremarkable. Palpation of the abdomen revealed an enlarged liver
(approximately 3 cm). Since this man had recently received a CBC and liver
profile, these tests were not repeated. Orthopedic testing of the lower spine
was negative. However, trigger points were found in the gluteus medius and the
tensor fascia lata on the right.
Roentgen evaluation of the right hip disclosed no pathology. During
upright evaluation of the lumbar spine and pelvis, however, a scoliosis of the
lumbar spine was noted. The convexity was directed to the left side. This
scoliosis was secondary to a structural asymmetry in the form of a 13-mm
deficiency of the left lower extremity (C-2). Compensatory right lateroflexion
subluxations were evident at L3 and L2 (A-3). The illusion of right posterior
rotation of the lumbar spine is due to left anterior pelvic rotation over the
femurs (Fig. 6.77).
The lateral lumbar film shows mild degenerative change at the L3 disc,
with other lumbar discs of normal vertical height. A small amount of calcific
deposition is present in the abdominal aorta (Fig. 6.78).
A diagnosis of a short-leg syndrome, with nerve irritation at the L2-L3
and L3-L4 levels, was made. The extension neuralgia to the thigh was
responsible for the patient's symptoms. With conservative chiropractic
management, which included lift therapy, the patient's symptoms were
completely relieved within a month. During this time, he received nine
treatments, which resulted in partial correction of the leg deficiency. He has
not had a recurrence of symptoms at this time.
Classification of Radiologic Manifestations
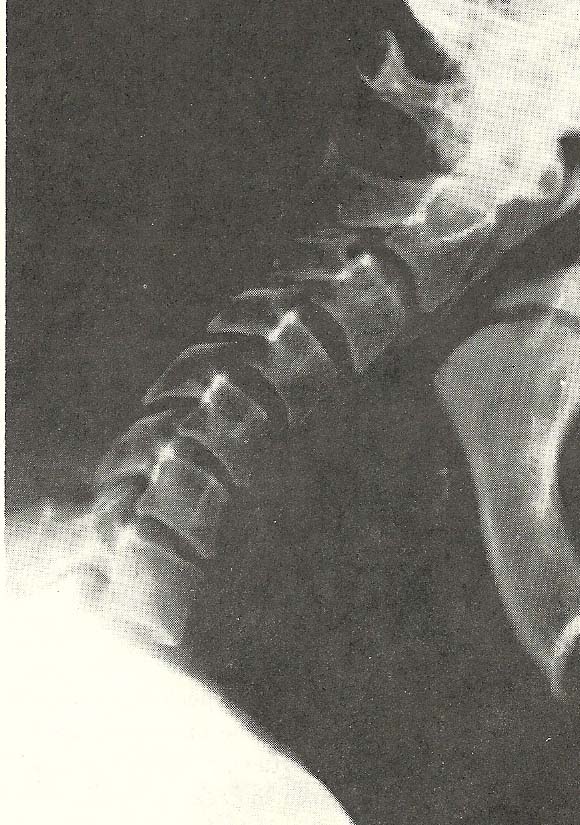
Case Illustrating Classifications C-4 and B-1
Another instance of altered vertebral mobility is shown in this case. The
altered cervical curve (hyperlordosis) shown in the neutral lateral film is
obviously associated with minor anomalies of the vertebral arches and
articular processes at C2--C4 (Fig. 6.79). There is also obvious arthrosis of
the facets throughout the neck, especially at C2-C3, and disc wedging to the
posterior is evident at C3-C4.
Flexion of the neck (Fig. 6.80) is grossly abnormal, the motion occurring
mainly as anterior bending of the neck as a unit --the lordosis remaining
essentially unchanged compared to the neutral film (Fig. 6.79). This
illustrates extreme hypomobility of nearly every cervical motion unit (B-1)
and abnormal motion of the cervical spine as a whole (C-4).
Extension of the neck is fairly well accomplished overall. At individual
motion units, however, one can see signs of restriction or hypomobility,
especially at C6 and C7 (B-1) where a comparison with the neutral film shows
little intervertebral extension (Fig. 6.81).
This 70-year-old male had a long history of neck pain and stiffness
associated with frequent headaches and bilateral shoulder pain. Orthopedic
tests showed diminished ranges of motion in all directions in the neck.
Cervical compression tests were negative.
Manipulation and adjustments of the neck were painful to him unless very
gentle techniques were used. Muscle stretching and postural correction gave
him some measure of increased comfort. After several weeks of various
manipulative approaches and changing intervals between treatment, it was found
that a treatment every 2 weeks helped him to experience less neck discomfort
and headache. He has remained on this schedule for several years.