

|
.Chapter 3:
The Pelvis
From R. C. Schafer, DC, PhD, FICC's best-selling book:
“Motion Palpation”
Second Edition ~ The Motion Palpation Institute & ACAPress
The following materials are provided as a service to our profession. There is no charge for individuals to copy and file these materials. However, they cannot be sold or used in any group or commercial venture without written permission from ACAPress.
All of Dr. Schafer's books are now available on CDs, with all proceeds being donated
to chiropractic research. Please review the complete list of available books.Basic Considerations Applied Anatomical Considerations Biomechanical Considerations Gillet's Comments on the Sacroiliac Articulations Diagnostic Considerations Pelvic Fixations Sacroiliac Motion Palpation Differentiating Sacroiliac from Lumbar Fixations Pubic Fixations Myofascial Pain Syndromes Significant Neurologic and Orthopedic Tests Gillet's Comments on Common Fixations Found in Lumbago and Sciatica Closing Remarks on Diagnostic Considerations Therapeutic Approach Muscular Fixations Ligamentous Fixations Total vs Partial Sacroiliac Fixations Summary of Sacroiliac Pathodynamics from an Adjuster's Viewpoint Adjusting Pelvic Articular Fixations Gillet's Method of Correcting Lumbosacral Kyphosis or Hyperlordosis Correcting Pubic Fixations Gillet's Comments on Cases of Low-Back Pain Bibliography
Chapter 6: The Pelvis
This chapter draws attention to the effects of fixations occurring within the pelvis (viz, the sacroiliac and pubic joints). Basic biomechanical, diag- nostic, and adjustive considerations are described, along with some important points that will be helpful during differential diagnosis.
BASIC CONSIDERATIONSIlli reported that sacroiliac fixation of any degree inhibits the compensatory torsion capacity of the spinal segments. When the mobile spine is flexed forward, there is always a degree of related lumbar torsion. If the sacroiliac joint is locked, however, normal torsion is restricted and axial torsion of the cord and nerve roots is produced. If this occurs, far-reaching neurologic and biomechanical manifestations can manifest.
From a purely biomechanical viewpoint, the greater the degree of sacroiliac fixation, the greater degree of stress placed upon the primary load- transferral points; ie, the lumbosacral and hip joints. If this stress cannot be spread to other adaptable links in the kinematic chain, local symptoms will arise.
Any degree of sacroiliac fixation or hypermobility disturbing reciprocal motion bilaterally can be associated with:
The direction of excessive rotary forces to the lumbar spine, leading to disc protrusion and potential rupture.
An adaptive lumbar scoliosis away from the side of pain, leading to compensatory biomechanical changes in the thoracic and cervical regions.
Compensatory overstress at the acetabulum, leading to hip pain and arthritis.
Rotational overstress at the knee to widen the base of support, leading to chronic sprain. Such effects may extend as far distal as the ankle and foot.
Applied Anatomical Considerations
The mechanical link between the axial skeleton and the lower extremities is the pelvic basin. Each half of the pelvic girdle consists of the ilium, ischium, and pubic bones that are three separate bones during early life that, through custom, retain their separate identity in adulthood even though they become completely fused and function as one bone. Although the hip joint is classically considered part of the lower extremity from an anatomical viewpoint, it is so closely linked functionally to the innominates, sacrum, and lumbar spine that it must be considered in any discussion of the pelvis.
The anterior superior iliac spine (ASIS), anterior inferior iliac spine (AIIS), posterior superior iliac spine (PSIS), posterior inferior iliac spine (PIIS), and symphysis pubis are the common landmarks of the pelvis (Fig. 6.1).
The summit of the iliac crest is typically listed as being on a level with the L4 spinous process and the PSIS on a level with the S2 spinous (near the midline of the lower third of the sacroiliac articulation. This textbook ideal, however, varies greatly from observations seen in clinical practice.
In our previous descriptions of the articular surfaces in the spine, we were dealing primarily with fairly flat or ovoid surfaces that met congruently unless pathologic changes or congenital deformities existed. Spinal mechanisms of motion, thus, were not especially difficult to comprehend. Unfortunately, this is not true for the complex sacroiliac joints.
From an architectual design viewpoint, the pelvis consists of several interlocking triangles, resembling an inverted pyramid from the front, back, and sides. The dorsal surface of the sacrum is convex, and its anterior surface is concave. To meet with the ilia, which are forced to flare laterally (P-A) because of the angle of the upper and lower sacral facets, the S1–3 segments are wider anteriorly than posteriorly (Fig. 6.2). It is within this area, from S1 to approximately between S2 and S3 that the sacroiliac joint extends.
The concave sacral articulations with the ilia are congruently boot-shaped, and numerous bumps and depressions of the articulating surfaces help to offer stability and limit motion. The ridges and furrows of the sacrum, however, are not always ideally reciprocal with those of the ilium nor are the bilateral planes of articulation commonly symmetrical. The ilia resemble an inverted triangle when viewed laterally.
The Sacroiliac Joint Complex.The Ilia. The ilia are the broad superior portions of the innominate. They are fused with the pubic bones that articulate anteriorly with the symphysis pubis and posteriorly with the sacrum. The flared wings (upper aspect) of the ilia forms the major pelvis (false pelvis), which supports the contents of the lower abdominal quadrants. The lower half of the pelvis forms the minor pelvis (true pelvis), which is surrounded by the pubes, lower ilia, ischia, sacrum, and coccyx (considered inconsequential). Cups within the inferior aspects of the ilia form the superior aspects of the acetabula.
The Iliac Facets. Anterolateral to the PSIS and PIIS of the ilia are the complex facets that articulate with the sacrum. These facets resemble rough, concave, bony ears that face backward or forward, depending upon the area being considered. Some authorities refer to these facets as being boot shaped, with the toes of the boots pointing backward. Regardless of the descriptive similes used, the iliac facets are slightly wider than their mates on the sacrum.
The "foot" of the articulation allows a slight sliding motion anterior-inferiorly or posterior-superiorly and a distinct rotating action about the pit. The leg of the boot articulates at the level of the S1 tubercle. The foot of the boot articulates between the S2 and S3 segments. This design has a distinct influence on traumatic iliosacral motion. The upper pit also serves to offer osseous relief to the relatively weak superoanterior sacroiliac ligaments. Another important role of this design is to prevent sacral displacement during loaded movements. Superior and posterior to the articular surface is a larger area of rough bone that serves for the attachment of strong sacroiliac ligaments.
The articular surfaces of both the sacrum and ilium are fairly smooth during childhood and do not exhibit their rough ridges and furrows until after puberty. Like fingerprints, their exact design is unique to the individual. In the child, stability is essentially ligamentous.
According to Boorsma, the boot-shaped design of the sacral facets is typically deep, oblique, and mobile, and it is especially related to a hyperlordotic spine. When associated with a flattened lumbar spine, the sacroiliac articulation is generally more bean shaped, vertical, shallow, and less mobile.
The most important point to remember about the sacroiliac joints is this boot-shaped design (when viewed from the side), in which two distinct articulations are found: one above the ankle of the boot, which articulates with the S1 segment, and one at the foot of the boot that articulates between the S2 and S3 segments. An oversimplified comparison of these two areas of articulation (at the superior and inferior aspects of the joint) would be a link in a bicycle chain. The upper joint is more influenced by body weight descending via the lumbosacral articulation, and the lower joint is more influenced by forces ascending from the lower extremity via the head of the femoral-ilial articulation. When mobile, these two articulations act reciprocally, when one rotates in one direction, the other rotates in the reverse direction. However, if either the superior sacroiliac articulation or the inferior sacroiliac articulation becomes partially fixed, the other can only pivot in an arc around the abnormal axis of the fixated articulation.
The Sacroiliac Joints. The sacroiliac joints are uniquely both diarthrotic and amphiarthotic. Gehweiler is one of several authorities who states that the sacral facet is covered by hyaline cartilage and that the iliac facet is covered by fibrocartilage. Others, however, report a variety of different findings. The inferior two-thirds of each joint is a true synovial articulation; the superior third is a fibrocartilaginous amphiarthrosis supported by the short but strong sacroiliac ligaments. Thus, a true polysynovitis can involve only the caudad aspect of the joint. Synovial membrane blankets the whole joint cavity except at its posterior aspect where it is replaced by large ligaments that attach to the articular cartilage. See Figure 6.3
The slight but important rotating, sliding, gliding, and pivoting action of the sacroiliac facets serve as the singular link point where the axial skeleton is attached to the pelvis; thus the necessity of this joint being bilaterally strong and slightly mobile to adapt for biomechanical impairments deficiencies above and and below.
By puberty, in adaptation to walking and the imposed stress of daily living, the articulating bony surfaces develop a variety of acquired incongruities and small projections where dynamic stress would be concentrated if not for the smoothing effect of articular cartilage. Of all articulations, the sacroiliac joint contains a large array of reciprocal bony hills and valleys. This joint surface roughness, more prominent in males, is generally considered the result of its segmental heritage; ie, the fused lateral tips of the transverse processes and the intertransverse spaces.
During aging degeneration, calcium infiltration of the joint appears within the fibrocartilage of the ilium long before changes occur in the hyaline coated sacral facet. This is attributed to the fact that the sacral cartilage is three times thicker than the iliac cartilage.
Grieve reports that more than 30% of the population possess accessory sacroiliac joints formed between the PSIS area and either S2 or S1. These accessory articulations, which are lined with fibrous cartilage or sometimes synovial membrane, are common sites of early osteoarthritic changes.
Sacroiliac Innervation and Referred Pain Patterns. The posterior aspect of the sacroiliac joint is innervated by posterior rami of the L5–2 spinal nerves. Inflammation at the posterior aspect of the joint usually refers pain to the buttocks and back of the thigh, following dermatomal distribution. The anterior aspect of the joint is innervated by both posterior branches from the L3--S2 roots and the superior gluteal nerve (L5–2). Irritation of the joint anteriorly commonly refers pain to the groin and anterior thigh. If the sciatic nerves pierces the piriformis rather than exiting the pelvis over or under the muscle (a common occurrence), sacroiliac distortion or inflammation may involve any of the numerous sciatic fibers.
The Sacrococcygeal Joints
The joint between the last sacral segment and the first segment of the coccyx is atypical. It is usually considered a symphysis, united by a rudimentary IVD and tough ligamentous bands around its circumference. Slight motion posteriorly is normal during defecation, gait, and more so during parturition.
Ligamentous Changes During Pregnancy
During pregnancy, all pelvic ligaments normally loosen. This is attributed to natural hormonal changes that occur at this time. Although this is beneficial for enhancing a less painful delivery, two adverse clinical effects of this hypermobility can occur. Many clinicians have found that:(1) the hypermobile joints may not fully return to their normal positioning following delivery;
(2) as it takes several months for the relaxed ligaments to shorten to their prepartum state, sacroiliac and sacrococcygeal instability will predispose the mother to chronic sacroiliac irritation that frequently leads to a state of fixation if not properly monitored. The constant lifting of the child by the mother, often from awkward positions, plus other forms of loading, is certainly a contributing factor. This adds to the list of factors of why chiropractic postnatal care of both mother and child is important as a preventive procedure. [See Clinical Comment 6.1]DR. FAYE'S CLINICAL COMMENT #6.1
The postpartum symphysis pubis often remains hypermobile as described by Sandoz in the Annals of the Swiss Chiropractors' Association. A special roentgenographic view taken with the patient standing on a 4-inch block under one foot and the other limb hanging will show a rise of the pubis superiorly on the side of groin pain or severe episodic sacroiliac pain. In chronic cases, a traction spur commonly forms at the sacroiliac joint inferiorly. During the past year, our practice has revealed three cases; thus, this condition is not rare.
The Symphysis Pubis
Pubic innervation is achieved from branches of the L1–4 fibers, thus referred pain can be diffuse or unpredictably specific. The forward portions of the hyaline coated pubes join at the fibrocartilaginous pad (anuclear disc) of the pubic symphysis. Slight but important movement takes place at this joint by the yielding of the interpubic fibrocartilage. For this reason, the plasticity, flexibility, and elasticity properties of the fibrocartilaginous pad are important in the maintenance of normal pelvic biomechanics. Excessive pubic movement is normally restrained by the superior and inferior pubic ligaments. Clinically, what is more important is the fact that iliac motion imposes reciprocal compression, tensile, and torsional forces on the joint. Although fixation is often found, complete fusion is rare even in old age. [See Clinical Comment 6.2]
DR. FAYE'S CLINICAL COMMENT #6.2Hypermobile or hypomobile symphysis pubis joints will not only produce pain locally, they can also cause severe stress at the sacroiliac joints. In athletes that complain of recurring groin strains, it is necessary to obtain roentgenographs of the symphysis pubis to see if it is stable during the special procedure described in Clinical Comment #6.1. Alternately pulling one knee toward the chest and holding this position for about 30 seconds while sitting will help to mobilize a fixated symphysis pubis.
Biomechanical Considerations
The three-joint complex of a vertebral motion unit has been previously described. This complex consists of the disc anteriorly and the apophyseal facets posteriorly. A similar three-joint complex is seen in the pelvis. This complex consists of the symphysis pubis anteriorly and the sacroiliac facets posteriorly. Thus, the pelvis viewed as a unit has six degrees of freedom just as a vertebral motion unit. See Figure 6.4
Lumbosacral Motion. The transitional junction between L5 and S1 is a unique "universal joint." If the sacrum rotates anteroinferiorly on one side within the ilia, for example, L5 tends to rotate in the opposite direction because of the restraint of the iliolumbar ligament. A mechanical accommodation of the lumbar spine is produced above; viz, a posterior rotation on the side of the unilateral sacral anteroinferiority. It also tends to assume an anteroflexed position, thus producing the three-dimensional movements of the lumbar spine. Owing to the biomechanical intricacy of the lumbosacral junction, anomalies such as asymmetrical facets have a strong influence on predictable movements in this area. Such asymmetry is far more common than generally suspected.
Classes of Intrapelvic Motion. Gillet classifies intrapelvic mobilities into three categories:(1) the P-A and A-P rotations of the ilia relative to the sacrum, and to each other at the pubis,
(2) the various movements of the sacrum itself in relation to the ilia, and
(3) the sitting-standing changes that affect the relationship of the ilia to the sacrum and to each other.Another mobility important to consider is the motion of the sacrum at the lumbosacral joint where it moves passively with the ilia; eg, as seen in lateral flexion of the pelvis during gait. Weisl, Gonstad, and others report of an inferior or superior gliding motion along the caudal aspect of the sacroiliac facet.
Sacroiliac Motion
It was the strong conviction of the medical community for many years that
there was no normal sacroiliac or pubic motion in the absence of disease or
pregnancy and that the sacrum and innominates moved as a whole. This opinion
was disputed by empirical evidence submitted by chiropractic and osteopathic
physicians since the turn of the century and in recent years the allopathic
assumption has been proved a fallacy through cineroentgenographic studies and
reports submitted by objective scientists. Only since the 1970s has sacral
motion been recognized in allopathic literature (an embarrassment never
mentioned).
According to Illi, a human being is the only vertebrate with a movable
sacroiliac articulation. At birth, the joint is only slightly movable. Sacroiliac function is the effect of bipedism. However, because sacroiliac and
pubic articulations are readily subject to fixation, normal movement is not
always exhibited in the adult within modern society where physical activity is
minimal. Nevertheless, several autopsy studies report freely movable joints in
individuals over the age of 80.
Faye mentions that since the sacroiliac joints form their shape as a child
matures as a biped, it is absolutely necessary that all children be examined
periodically to assure normal sacroiliac function. He states that "Sacroiliac
dysfunction in the young leads to abnormal gait and muscle development."
For the sake of study, specific sacroiliac motions will be described. In
vivo, however, these motions are always coupled when the articulations are
mobile. There is no one normal movement of the sacrum upon the ilia. Not
recognizing this point can lead to many analytical errors.
Slight but smooth sacroiliac motion occurs upward, downward, forward, and
backward, and axial rotation occurs about a transverse axis to allow pelvic
tilting. Because the sacrum does not have distinct articular planes but moves
(floats) within the pelvic ring, its motion is multidirectional for 1-3 mm
rather than in restricted specifically defined paths. This multidirectional
movement of the sacrum is likely the result of
(1) the wider iliac facet,
(2) the longer sacral facet, and
(3) the thick articular cartilage of the sacrum. As described previously, this diverse motion is especially passive in the nonweight-bearing positions and influenced above by lumbar forces and/or laterally and below by iliac-ischial forces.
Sacroiliac motion is a consequence of trunk or hip motion and must be able to accommodate both of these movements at the same time. For this reason, it is clinically important to be able to restore restricted sacroiliac function in all directions.
Axis of Rotation. Where the exact axes of rotation for the sacroiliac joints are has not been definitively determined. Farabeuf and DeJarnette place them posterior to the center of the whole joint's surface, posterior to the ankle of the boot (Fig. 6.5). Bonnaire and Cassidy place them anteriorly within the joints, near the heel of the boot. Weisl locates an axis for sacral rotation below the foot of the boot and a plane of transition that moves horizontally through the foot of the boot (Fig. 6.6). Shrader's model indicates that they are likely to be in a common plane that extends from the torsional center of the symphysis pubis through the center of each femoral head. Illi's studies arrived at a combination of Farabeuf's, Bonnaire's, and Weisl's findings. Gillet's findings will be described with various topics within this chapter.
Sacral Changes from Recumbent to Standing Positions. The sacrum approaches its nearest state of static equilibrium in the slightly flexed prone position where inferior and superior forces are removed. This is probably why sacral (eg, Logan Basic) and para-anal (eg, Watkins') reflex techniques achieve their greatest effect in this position. Several studies have shown that there is distinct sacral position alterations when changing position from the recumbent, to the sitting, to the standing postures. Gillet describes these changes in detail.
During forward flexion of the trunk in either the standing or sitting position, the sacral base pivots farther anteriorly and inferiorly, and the apex of the sacrum moves posteriorly and superiorly. Simultaneously, the PSISs of the ilia move posteriorly, inferiorly, and obliquely medial so that the space between the spines is reduced. The ischia concurrently move obliquely anteriorly, superiorly, and fan laterally. During backward bending of the trunk, these pelvic actions are reversed. Note the reciprocal action between the A-P and P-A motions of the sacrum and the ilia and the reciprocity between the inward and outward flaring of the superior aspect of the ilia above and the ischia below.
Standing P-A/A-P Sacroiliac Motion. During erect weight bearing, the base of the sacrum tends to rotate (pivot) anterior and inferior about the lateral S2 tubercles. When a standing subject lifts the right knee to a maximum, for example, as in taking a high step, the right ilium tends to follow the femur in its motion, rotating in the P-A/A-P plane with the approximate center of movement being at the head of the femur. Simultaneously, the right pubic bone moves upward in relation to its partner. This is palpable. The iliac portion of the sacroiliac articulation glides backward and downward relative to its contact with the sacrum. After this, the sacrum arcs posteriorly and inferiorly with the left ilium; ie, it is passively carried along by the active ilium. If both the pubic and sacroiliac articulations reach their limits of mobility and the knee is lifted still further, the pubic joint begins to serve as the center of rotation and, at the posterior aspect of the pelvis, the ilium start to pull the sacrum downward in its course, forcing it to compress against the opposite ilium. Because this latter movement does not follow the plane of the sacroiliac facets, a degree of joint separation must occur. If the knee lifting test is carried still further, the normal limit of the other articulation (the left in this example) will be reached, and then the whole pelvis becomes involved.
In the standing position described, motions of the sacrum relative to the ilia are sometimes difficult to detect because of coupled acetabular changes. Thus, it may be necessary to seat the patient to restrict these movements. Sitting fixes the pelvic base (the ischia), alters its shape, and allows a completely different type of motion than that seen in the standing position.
Sitting P-A/A-P Sacroiliac Rotational Motion. The sacrum readily flexes in the sitting position, turning between the two ilia. To produce this movement, the stabilizing arm of the examiner grasps the opposite shoulder of the patient across the chest and rotates the patient to a maximum while the examiner's palpating fingers follow the sacral spinous processes in their course. The lumbar region also rotates and flexes to follow the line of the thoracic vertebrae that move laterally in a wide arc. The placement of the sacrum can roughly be judged by the direction of the buttocks line.
Rotation and flexion of the sacrum in the sitting position carries the ilia along with it to a degree. Sacroiliac motion in the sitting position can be palpated by placing the thumb on the iliac crest or on the PSIS and following it forward and downward as the thorax is rotated in that direction. Note that most authorities agree that any degree of sacral rotation has a related translatory component.
Sacroiliac Motion During Lateral Flexion. During lateral bending, movement of the sacrum takes place with a maximum of tilting and a minimum of rotation. To palpate this movement, the shoulders of the patient must be put into a complete lateral bending posture, concentrating the movement in the area being palpated. Again, the ilia make an effort to follow this movement into lateral flexion.
Sacroiliac Motion During Walking. Axial or lateral rotation of the pelvis about a fixed femoral head is produced by actions of the muscles of the thigh, loin, and the abdominal obliques. This is exhibited in walking. Illi has shown that sacroiliac motion provides reciprocal action of the ilia and a gyroscopic motion of the sacrum during gait (Fig. 6.7). These motions tend to dampen the axially directed forces of heel strike. Illi reports that as the heel strikes, the ilium rotates posteriorly and inferiorly, the sacral base reciprocally rotates anteriorly and inferiorly, and the ipsilateral transverse of L5 is pulled backward. This vertebral action of the functional lumbar scoliosis diminishes cephally. During midstance, the pelvis moves over the femoral head in a neutral position. As the contralateral extremity is abducted forward, the sacrum is pulled backward and upward on that side. This reciprocal motion between the sacrum and ilium describes a horizontal figure 8 between the ilia when viewed during gait. One side of the sacral base arcs downward, forward, and rotates toward the ipsilateral side, while the other side swings upward, backward, and the sacral apex rotates toward the contralateral side. The path of this arc appears to be the product of (1) sacral translation and torque having various components, depending on the planes of the bilateral facets, (2) the force vectors, and (3) the bilateral integrity of the involved restraining ligaments.
Sacral Motion During Breathing. The majority of references to this mecha- nism have been published by DeJarnette, Goodheart, and a number of osteopaths researching cranial manipulation and reflexes. They have found that there is slight sacral P-A and A-P motion during respiration and Valsalva maneuvers. The base of the sacrum tends to pivot posteriorly during inspiration (or increased intra-abdominal pressure) and anteriorly during expiration of 1–7 mm. The rate is about 14 excursions per minute. This mechanism, synchronized with a reciprocal cranial action, appears to produce a "pump-like action" on cerebrospinal fluid circulation, made possible by the continuous dural sheath that descends from the cranial vault through the spinal canal to insert near S2. This helps to explain why sacral and upper cervical dysfunctions are so frequently associated.
Pelvic Changes During Sitting
During sitting, where weight is borne essentially by the ischial prominences, the body attempts to broaden its base of support by slightly separating
the ischia, which in turn slightly close the iliac crests superiorly. As the
sacroiliac joint space opens inferiorly, the apex of the sacrum juts backward
to remain in contact. That is, because of the oblique slant of the sacral
facets, the sacral base nods anteriorly and the apex moves posteriorly. The
axis of this motion is commonly a horizontal plane located at or near the S2
level. Articulation for this motion takes place at both the pubic and sacroiliac joints.
In arising, however, the ischia are passively brought together to permit
body weight to lie directly over the heads of the femurs. The iliac crests
then open laterally (flare). This closes the inferior sacral angle and opens
the joint space that holds the base of the sacrum. In adaptation, the sacral
base moves slightly backward and the apex nods forward. In considering A-P and
P-A nodding of the sacrum, keep in mind that the position of the ilia are not
rigid and that the slant of the articulations force the ilia to adapt themselves to sacral flexion by lateral flexion of their own. Thus, we rotate each
hip backward and forward each time we walk. Each time we sit and arise, we
cause our ilia to flare outward and inward. Each time we bend or turn in a
seated position, we cause the sacrum to turn within the interiliac space.
Anterior and Posterior Pelvic Tilt
In the neutral standing position, the ASISs normally lie in the same vertical plane as that of the symphysis pubis. The motions of the pelvis as a
whole are
(1) forward and backward tilt around the transverse interfemoral axis,
(2) lateral tilt (associated with lumbar scoliosis), and
(3) rotation in the horizontal plane. None of these motions are produced by intrinsic pelvic muscles; rather, they are produced by the muscles of the trunk and/or hip that attach to the pelvis or sacrum. These motions primarily occur at and affect the lumbosacral junction and the heads of the femurs. They involve the sacroiliacs to a much lesser degree.
Forward and backward pelvic tilts describe an arc that normally follows the arcuate (bow-shaped) ridge and groove of the sacroiliac facets.
Forward tilt is related to lumbar hyperlordosis and hip flexion. The anterior thigh muscles are also a strong component in this motion, thus the frequent involvement of these muscles in pelvic distortions.
Backward tilt is associated with lumbar flattening and hip extension. The major actions come from the posterior pull of the hamstrings and the anterior pull of the rectus abdominis, with help from the obliques.
If an individual shifts most body weight to one leg, passive lateral
pelvic tilt occurs. The pelvis on the unsupported side is restricted actively
by the gluteus medius and minimus and passively by the iliotibial band. When
body weight is distributed bilaterally, lateral tilting of the pelvis is associated with lumboscoliosis, sacroiliac distortion, and a unilateral short leg,
and likely a combination of these factors. [See Clinical Comment 6.3]
DR. FAYE'S CLINICAL COMMENT #6.3
In all low-back pain cases, it is essential to test for hamstring, quadriceps, and psoas length. Shortening of any of these muscles should be treated with PNF or spray-and-stretch techniques as a pre- or post-manipulative procedure. Stretching exercises at home should be prescribed as tolerated during active management as well as a preventive procedure.
| Editorial Comment |
Dr. Leonard Faye reminds us in Chapter 6 of Schafer's text “Motion Palpation” that:
"In all low-back pain cases, it is essential to test for hamstring, quadriceps, and psoas length."
The picture on the left is the best picture I have found that displays the Modified Thomas Test. This test is is a very effective way to assess the length of 2 different muscles.
When the patient holds their knee to their chest, the following 2 things should become immediately apparent:1. If the psoas is of normal length, then the dependent thigh should be free to hang down 45° below the plane of the table. In this picture, the patient’s right psoas is significantly shortened.
2. If the quadriceps are of normal length, the angle of the knee (between thigh and leg) should approximate 90°If the psoas is shortened, it pulls the thigh into (some degree of) flexion, so the thigh cannot fully extend. This shortens your gait. Recalling that the origin of the psoas includes the lower thoracic vertebra, the lumbar segments I-IV, and the neighboring intervertebral discs, you can see why shortness would destabilize the lumbar and pelvic joints. Also… if the psoas is in contraction, the gluts may become inhibited by reciprocal inhibition.
If the quadriceps are shortened, it draws the leg into extension. Because portions of the quads originate on the pelvis, a shortened quads also distorts normal pelvic motion.
The picture on the left is the best picture I have found that displays the Straight Leg Raise (SLR) (although I fail to see the need for bondage). If the hamstrings are normal length, the leg should passively flex to at least 90°, without lifting sacrum off the table. Knowing that the hams originate on the ischial tuberosity, shortness of the hams can also distort pelvic mechanics.
Post-isometric Relaxation (PIR) is an effective and well-tolerated method for returning shortened muscles back to normal resting length.
The Soviet Block countries first adopted using PIR on their Olympic athletes in the 70s. They found that after 6-12 treatments, athletes continued to maintain their improvements, even after 12 months. This is quite remarkable, considering that they continued to train at Olympic levels (numerous hours per day, day after day) for a whole year.
PIR of the Psoas
PIR of the psoas is quite straighforward. The doctor faces the patient, stabilizing the bent knee (and flexed hip) to the patient’s chest. Then place the free hand on the dependent knee and gently push down, until you reach the “barrier” (passive end-range).
Then ask the patient to try to raise that knee towards their chest…at about 50% of their strength level. They will contract the psoas for 30 seconds…and half way through the contraction, ask them to take a deep breath and hold it, while maintaining the contraction. When they release their breath, “follow” the knee down with a gentle over-pressure. Hold for 30 seconds.
The picture on the left is close to approximating the proper setup. If you stand further back, you can use both your arms straight to hold them. Also, note that the patient should be closer to the end of the table, to facilitate unobstructed extension at the hip.
The key to PIR is to remember that this is a very gentle “taffy pull”. Slow and progressive, a light over-pressure, held for 30 seconds, helps to disengage the retained actin-myosin bonds that are associated with muscle shortening. Because these stretches can also be uncomfortable, the doctor must have the courage to continue the stretch, while also being sensitive to the patient’s tolerance level.
PIR of the Quadriceps
PIR of the quads is also is straighforward. When the patient is prone, you should be able to passively flex the knee until the heel can touch the buttocks.
The positioning in this picture is terrible, with the the doctor facing the patient’s feet (not to mention the questionable hand on their rump). If you reverse your position, and stand facing their head, you can use a straight-arm stabilization at the ankle during the contraction phase.
To set up, first, bring the heel towards the buttocks until you meet resistance. Then, ask the patient to try to straighten their leg, at 50% of their maximum ability, for 30 seconds. As with the psoas (and all PIR work), after 15 seconds, ask them to take a deep breath and hold it, while still contracting the quads. At 30 seconds, when they exhale, push the heel forwards gently, with mild over-pressure. Slow is smart, as the quad stretch can be uncomfortable.
Note that you can gain extra leverage in the flexible patient by also gently lifting their thigh off the table (with your other hand), while still maintaining full-flexion at the knee.
PIR of the Hamstrings
As shown in the SLR photo above, bring the straightened leg as high as possible (without lifting sacrum off the table) and then place their ankle (or mid-calf) on your shoulder. Ask them try to lower the leg as 50% maximum for 30 seconds…with the deep breath at half way through the contraction. When they blow out, inch forwards, which will bring the hip into further flexion. As with the quads, slow is smart, as this stretch can be uncomfortable.
Remember to keep the patient’s knee “locked” in full extension (as shown in the SLR photo above), otherwise the clever patient will bend at the knee to reduce their discomfort.
PIR involves 2 distinct phases:
(1) the contraction phase, and
(2) the stretch phase.
Sub-maximal contraction of a muscle for (at least) 30 seconds will inhibit the fast-twitch response of muscle, blocking their ability to resist you during the stretching phase of PIR.
Because of this phenomena, it has been suggested that PIR can provide a 30% “better stretch” than stretching without first exhausting the muscle.
I have found that patients hold their pelvic adjustments longer and better if you first address any shortening found in these 3 muscles.
Thank to Dr. RC Schafer, Dr. Leonard Faye, Dr. Craig Liebenson and all the instructors of the Rehabilitation Diplomate Program, developed by Craig and LACC (now SCUHS), for their combined wisdom!
| End of Editorial Comment |
Lateral Pelvic Inclination
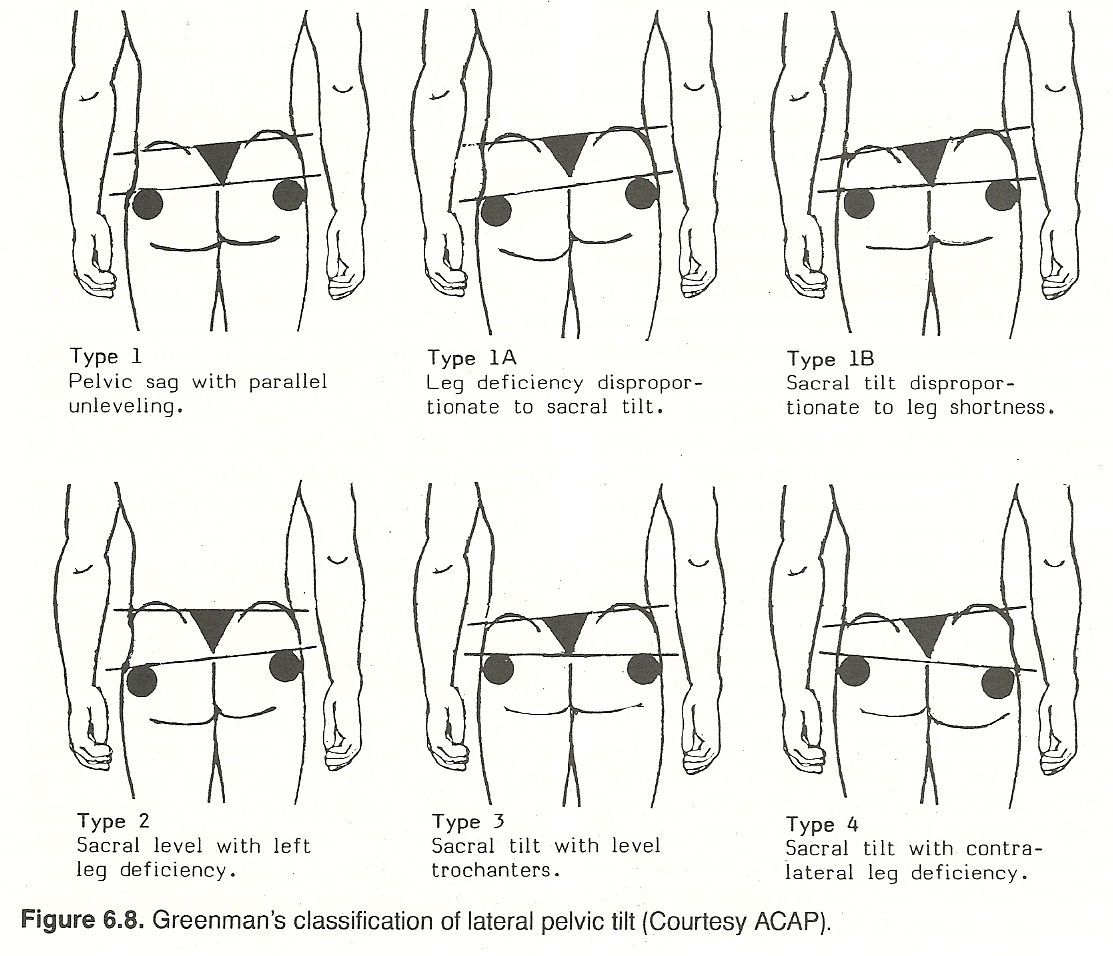
After studying 200 patients with a presenting complaint of low back pain,
Greenman found that 64% exhibited lateral pelvic tilt (sacral base unilaterally inferior). A pelvic sag, as viewed from the anterior or posterior, can be
the effect of several factors. The most common causes are unilateral lower
extremity deficiency, muscle shortening or weakness, sacroiliac dysfunction,
and hip or lower extremity alignment problems. Muscle fixation from lack of
stretch is the second most common cause, second only to the common unilateral
leg-length deficiency. See Figure 6.8.
From a biomechanical viewpoint, lateral pelvic inclination directs the
lumbar curvature and that pelvic inclination is essentially determined by
posture of the hips. Thus, the muscles of the hips are important factors in
controlling pelvic inclination and the lumbar curve. During standing, the
thighs are fixed points from which the hip muscles act. For example, shortening of the pelvic extensors (eg, glutei, hamstrings) reduces the dimension of
the lumbar curve from front to back and rotates the pelvis posteriorly. Shortening of the pelvic flexors (eg, iliopsoas, rectus femoris) increases the
lumbar lordosis and tips the pelvic basin forward. Weakness of the antagonists
would have the same effect. Thus, rehabilitation should be directed to relax
and stretch muscles shortened by spasm or contracture and strengthen counterparts weakened by inactivity or constitutional factors. In mild moderate cases, this need not be a dual activity as a muscle relaxes as its antagonist
contracts against resistance.
In bilateral muscle checking during posture analysis, applied kinesiologists believe that most patients presenting with postural defects have muscle
weakness rather than primary spasm. It is their contention that it is this
weakness that causes the contralateral muscles to contract into an apparent
spasm. Thus, the weakness is said to be primary and the spasm to be secondary.
The spasm is thought to be the result of the prime-mover/antagonist reciprocal
relationship. For example, an elevated iliac crest on the right may be due to
weakness on the right of the psoas, gluteals, and tensor fascia lata or weakness on the left of the adductors, quadratus lumborum, rectus or transverse
abdominis, or the sacrospinalis. Likewise, an elevated shoulder on the right
may be due to weakness on the right of the latissimus dorsi, lower trapezius,
anterior serratus, pectoralis major and minor, subscapularis, teres minor,
infraspinatus, and levator scapulae or weakness on the left of the upper
trapezius. These viewpoints, originated by Goodheart, have not been accepted
by several authorities. Nevertheless, they do help to broaden our perspective.
Gillet's Comments on the Sacroiliac Articulations
There are four possible movements in the pelvic articulations (sacroiliac,
sacrococcygeal, and pubic). The primary considerations are
(1) movements of the sacrum in relation to the ilia in which the sacrum is active and the ilia try to follow the movement,
(2) movements of the ilia relative to the sacrum,
(3) and movements of the ilia relative to each other (at the pubic joint) in which the sacrum is passive and the ilia are active.
Pelvic Movements: General Considerations
In all movements of the trunk, upper body motion forces are transmitted
from the structures to the lower ones in a decreasing degree since the motion
must end upon a solid nonmoving structure, usually the floor or the seat of a
chair. In all movements in which the trunk is almost passive, as in walking
and running, the structures that move the most are the lower extremities, and
this motion is transmitted to the upper structures in diminishing degrees. In
these movements, therefore, the ilia move the most and the sacrum serves as a
connecting link between the ilia and the spine. Farfan has shown a counterrotation occurs by the swinging arms and pelvic swing that counterrotates to
produce a kinetic energy of forward propulsion.
Another factor tends to complicate this study; ie, the functioning of each
articulation is often different in weight bearing. Gillet has done little work
on this subject but "a priori" feels that this would only show some articulations capable of physiologic locking according to the weight borne. In the
study of fixations, therefore, it is necessary to keep this in mind and to
analyze the spine without weight bearing, as far as this is possible.
The best known movement in the pelvis is the forward-backward rotation of
an ilium. No definitive attempt has been made, as far as we know, to determine
the exact pivot around which this motion takes place. In Belgium, the study
group has tried to do so by palpation of a great number of cases. They are
certain that this motion takes places around a point at or near the head of
the femur. This means that the movement occurring at the pubis is a gliding
motion of one articular surface upward and backwards. On the other hand, the
contact of the ilia with the sacrum moves down and backward in its superior
aspect and down and forward in its inferior aspect.
Standing Relationships
Normally, with the patient standing, and in spite of the amount of weight
bearing that this movement applies to the opposite articulation, the sacrum
remains vertical. This means that, at least in its first part, the sacrum does
not participate in this movement. Illi shows this in his motion x-ray films of
the patient walking. If the articular surfaces at the sacroiliac and pubic
joints are completely free, not only will the sacrum remain vertical during
walking, it will remain so when the knee is pulled up flexed to an easy maximum height. In fact, it can be given as a rule that if on doing this movement
the sacrum tilts to one side, there must be at least a partial fixation be-
tween the sacrum and the ilia.
The first part of iliac rotation posteriorly takes place with the moving
ilium gliding down and backward on the surface of the sacrum. Soon, however,
the end of the range of motion is reached. If the knee is lifted higher, the
moving ilium carries the sacrum down with it. At this time, therefore, the
motion takes place between the sacrum and the opposite ilium: the sacrum
moving down and the ilium remaining in its place relative to the limb bearing
the weight of the body. It is important to understand this movement for we
will see it again when all the possibilities of partial fixations have been
described. [See Clinical Comment 6.4]
DR. FAYE'S CLINICAL COMMENT #6.4
It has been my experience that the loss of this second motion of the sacrum against the motionless weight-bearing ilia can produce excruciating sacroiliac pain, the sciatica of the sacroiliac syndrome, and be significant in acute lumbosacral facet syndrome. The specific adjustment for this disorder will be described later in this chapter.
The second type of movement possible between the ilia and the sacrum and
at the pubic joint is one that has practically never been described outside
the literature of dynamic chiropractic. During standing, the weight of the
body is transmitted to the lower extremity and then to the floor via the heads
of the femurs. To do so, the pelvis changes its shape: the crests of the ilia
separate laterally and the ischia come closer together. This movement takes
place around the pubis (which opens and closes at its superior and inferior
aspects) and the sacrum.
Keep in mind that the shape of the sacrum resembles an inverted wedge when
viewed from the anterior or posterior and also resembles a wedge when viewed
from above because of the obliquity of the sacroiliac articulations. The movement of the ilia just described must necessarily produce a related movement of
the sacrum for it to maintain contact with the iliac facets. This movement is
an anterior-posterior flexion, in which the sacral base moves posteriorly and
its apex anteriorly during standing, and vice versa when during sitting. This,
once more, necessitates free mobility at the sacroiliac and pubic facets. It
also brings into function two sets of muscles: the quadratus lumborum and coccygeus, for it is principally these muscles that produce the motion described.
Forward Flexion Considerations
Another movement, which has been described by Grice, is that which occurs
when the patient bends forward. It is widely known that most of this motion
takes place in the hip joints and that the lumbar region participates by forward flexion. There is, however, a movement between the sacrum and ilia in
which the sacrum glides deeply forward between the ilia. This motion can
readily be felt in the standing patient by placing your thumb on some portion
of the sacral apex and the tip of your forefinger on one of the PSISs. When
the subject flexes forward, this space opens up, usually about 1 cm at least
if the articulation is free. One articulation may function normally and the
other not because of fixation. We then see, on the side of fixation, that the
PSIS holds back and the two PSISs are then misaligned.
Lateral Flexion and Rotation Considerations
We will now describe two movements that have given the Belgium group a
great deal of difficulty in their studies: that of pelvic rotation and lateral
flexion in the sitting posture. These two movements are important because we
do much of our examining in this position. In these two movements, as stated
previously, the sacral part of the pelvis is active and the ilia are passive;
ie, they take up the space between the moving sacrum and the immobilized
ischia.
Lateral Flexion. Here we must take the lumbar vertebrae into consideration to make the whole motion clearer. In lateral bending, we know that the lumbar region is forced into flexion-rotation. The intervertebral space is flattened on the concave side and opened on the convex side of the lumbar curve. This is pure lateral flexion, a movement that takes place in spite of what the physiologists say. It takes place normally if the sidebending is made in the sitting posture with the lumbar region in forward flexion; ie, in slight kyphosis. If the normal lordosis is retained, there is a certain amount of rotation that takes place also. The maximum of rotation occurs if the lateral flexion is done with the subject standing.
To reveal these movements in the sitting position, it is necessary to concentrate the motion in the region to be studied. This is done by pushing the shoulder of the patient down as far as possible on the concave side of the curve. This is especially important in the study of the motion of the sacrum. In this movement, the relative motion of the sacrum and the two ilia is complex. The two ilia assume a slanting position toward the convexity of the lumbar curve, with the related side of the pubis gliding upward and laterally. This forces the ilium on that side to shift laterally, with the iliac crest and ischium moving sideward from 5 to l9 mm, respectively. The ilium on the concave side of the lumbar curve just flexes; ie, the ischium serves as a pivot, and the crest moves slightly laterally toward the convex side. This forces the sacrum (and the lumbars) to sway laterally to the same side. The sacrum remains nearly vertical, with only a slight amount of flexion. The base of the sacrum moves a little more laterally than the apex. The difference in movement between the flexing ilia and the swaying sacrum produces a composite motion between the two in which there are two lateral motions: the ilium moving downward on the sacrum on the concave side and upward on the sacrum on the opposite side. Some investigators believe that this movement is not a "natural" one. In fact, it is probably rarely done in everyday life. But as a test for mobility, it is extremely useful.
Rotation. During pelvic rotation, there is another complex movement. To make the description clear, let us suppose we are rotating the patient's torso anteriorly on the right. It will be readily apparent that the patient's right shoulder will move both anteriorly and to the left relative to the patient's midline. The patient's left shoulder will rotate posteriorly and toward the median line of the patient. This forces the T12 area of the spine to sway to the right from 5 to 10 cm, depending on the general suppleness of the patient's spine. The reason for this is that rotation in the thoracic region does not take place in the spine itself but around a pivot point that Gillet believes is located at the sternum.
This lateral sway of the lower thoracic vertebrae forces the lumbar region
into a mixture of rotation and flexion toward the side of rotation. This movement gave Gillet's group another problem to solve because several authorities
teach that the center of rotation in the lumbars is at the tip of the spinous
processes. If this were true, we would find all the tips of the lumbar vertebrae in perfect alignment during rotation and the T12 spinous process in line
with the sacrum. This is evidently not the case in the typical human spine. In
our hypothetical subject, we find (if no fixations exist) that the lumbar spinous processes in rotation produce a straight slanting line that extends from
T12 to the tip of the sacrum. In fact, variations of the line can be used to
indicate the vertebrae in fixation. This has been described by Gillet in the
Annals of the Swiss Chiropractors' Association.
(1) Pull the knee toward the chest, being sure that the femur rather than the tibia is the lever arm.
Sacral Rotation. The sacrum turns within the iliac cavity almost around a
vertical axis, but the base moves more than the apex. This gives the impression of lateral flexion of the sacrum, made in order to follow the line of the
lumbars. At the same time, the ilia rotate on a horizontal axis: moving forward on the far side and backward on the near side. This movement causes a
torsion-like movement at the pubis; and, if fixation exists in this articulation, the sacrum will then turn on a more vertical axis and to a greater
degree (hypermobility).
Pure sacral movement without subsequent movement of the lumbars or of the
ilia normally does not occur. The sacrum can move in spite of certain fixations of the lumbars or of the ilia to each other at the pubis.
Sitting. In the sitting position, the weight of the body is distributed to
the ischia. The body therefore does its best to widen its base by separating
these processes. As they separate, the iliac crests come closer together, thus
producing a medial flexion of both ilia. This movement also takes place around
the pubis, and due to the diagonal slant of the sacral articulations, the
sacral base is pushed forward and the apex is drawn backward, thus producing a
forward flexion of the sacrum. The sacrum is passive, and movement in this
bone usually takes place around an horizontal axis that is near the S2
tubercle.
The Hamstrings. Shortened hamstrings are common, and they may be found
either bilaterally or unilaterally. Taut hamstrings prevent pelvic rotation at
the hip anteriorly by fixing the ischium and destroying normal lumbosacropelvic rhythm; thus, any motion achieved is forced upon the lumbar segments,
often with compensatory stretching of the posterior longitudinal ligaments. If
movement is sharply forced, avulsion may occur that leads to further degenerative changes. [See Clinical Comment 6.6]
DR. FAYE'S CLINICAL COMMENT #6.6.
Failure of the hamstrings to elongate normally produces stress on the posterior elements of the lumbar
spine because the extensors muscles are at the end of their eccentric contraction and the lumbar spine is
hanging on its ligaments. Repeated stress from this scenario causes hypermobility of the zygapophyseal
joints and increased intradiscal pressure. Anular tears and the pathogenesis of disc degeneration develop
from the faulty biomechanics of the hamstrings. This is just one etiologic factor but an often overloooked
point in treatment programs. PNF or spray-and-stretch of the hamstrings, quadriceps, and psoas muscles
should be a priority consideration with all patients except those that are in the acute stage and cannot
withstand the stretches. Chiropractors should declare war on shortened back and thigh muscles.
The effects of shortened iliopsoas or piriformis muscles upon the hip and
lumbar spine will de described later in this chapter.
In a certain number of purely muscular fixations, the contracted or hypertonic muscle will have a tendency to degenerate and become fibrosed. For all
practical purposes, it becomes a "ligament" and, as most muscles are accompanied by a ligament, it is often difficult to determine which structure is
responsible for the fixation. Fortunately, the type and direction of a corrective thrust is practically the same, and even the amount of change to be
expected from a fibrosed muscle or a shortened ligament is the same. Both of
these types of fixations can therefore be considered "ligamentous." From the
point of view of correction, this fixation is the most common, although it is
not the most irritative.
Forward Tilt. An anterior tilt of the ilium is primarily the product of
(1) weak abdominals, hamstrings, or both,
Some authorities believe that the resulting distortion is
"the most common postural fault of muscular origin." Strengthening the inferior pull of the hamstrings posteriorly and the rectus abdominis superiorly
offers an in-line force couple to correct anterior pelvic tilt. The erector
spinae, quadratus lumborum, and iliopsoas usually need stretching.
(1) hypertonic abdominals,
In either cases of forward or backward pelvic tilt, biomechanical correction should incorporate
(1) mobilization of fixated facets,
The Posterior Sacroiliac Ligaments. White/Panjabi state that the interosseous sacroiliac ligaments supporting the thin joint capsule posteriorly and
inferiorly are the strongest of the body. These ligaments, considered the
major bond between the sacrum and ilia, are so thick that they fill the
roughened space between the sacral and iliac tuberosities behind the sacroiliac joint. There is an upper portion that spans between S1-S2 and the
anterior medial iliac crest. Immediately below is the lower part of the ligament that arises from S3 and inserts into the iliac crest. The strength of
these ligaments helps prevent displacement of the sacrum even during forceful
jumping.
In this movement, the sacrum assumes a flexion-rotation to the right
around a pivot point that is located slightly inferior to the tip of the coccyx. The right ilium follows this movement, the crest moves to the right and
anteriorly, the ischium moves very little, and there is probably a torsion at
the pubic joint. The left ilium moves in the opposite direction but to a
lesser degree.
At this point it may be necessary to excuse the length of this description
but it must be considered a necessity to build, once and for all, our
chiropractic theories and practices on facts pure science, if you will and
not do like some of our predecessors: slap on any old theory that might support their findings.
Total (articular) fixation in the pelvis is rare. Total fixations due to
the presence of several degenerated taut ligaments are, in contrast, preva-
lent. [See Clinical Comment 6.5]
Here the pelvic motion takes place to a greater degree at the pubic joint and
to a lesser degree around the head of the femur.
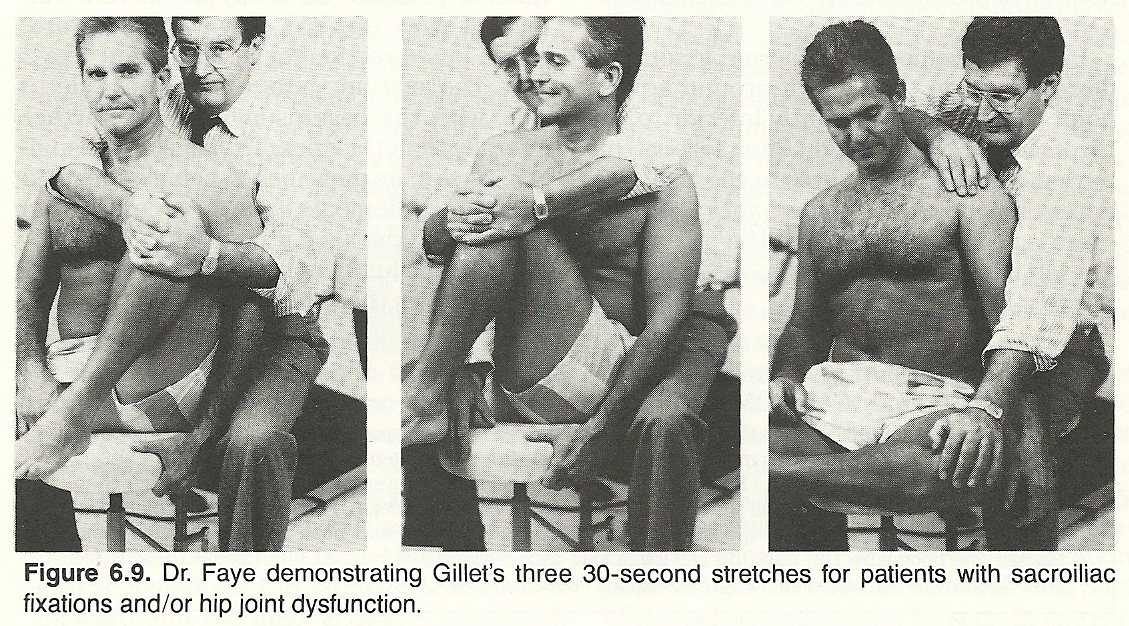
DR. FAYE'S CLINICAL COMMENT #6.5
It is for this reason Gillet taught three 30-second-hold stretches to his patients with sacroiliac fixations. I also use the same regimen for my patients with hip dysfunction. The procedure with a patient sitting on a hard chair is as follows:
(2) Pull the knee toward the opposite shoulder.
(3) Place the lateral malleolus of the ipsilateral ankle on the opposite knee in a "figure 4" fashion and push the knee laterally and toward the floor with the hand on the same side as the externally rotated hip. Repeat these three stretches on the opposite side all for 30 seconds each.
See Figure 6.9.
Considerations with the Patient Supine
One last short description: the movement that takes place when the subject
is in the supine position and lifts one extended leg without bending the knee.
Sacral Motion
As mentioned elsewhere in this chapter, there is no one movement of the
sacrum in relation to the ilia. The sacrum appears to "float" in the pelvic
ring; it does not have a specific "groove" that directs its movements. Indeed,
pressure on a supple sacrum can make it move upward, downward, forward, etc,
in any direction for at least from 1 to 2 mm. The sacrum shifts easily from
side to side, with the base usually moving farther laterally than the apex.
The sacrum is usually passive in its movements, being influenced either by the
lumbars if the force comes from above or by the ilia if it comes from below.
When the lumbars bend sideward, the sacrum follows their movement in
flexion and rotation, and the ilia rotate in a reciprocal opposite direction.
With the patient sitting, and especially if flexion forces are concentrated in
the lumbar region by pushing the shoulder of the patient downward and inward
toward the opposite side, flexion of the sacrum takes place toward the side of
convexity. The ilia will then also flex laterally in the same direction, with
a shearing motion taking place at the pubis. This produces a paradoxical
change of position of the coccyx toward the convexity of the lumbar curve.
Sacroiliac Reciprocity
The ilia move relative to the sacrum and to each other. We have described
that the ilia may flex laterally in relation to the sacrum upon lateral flexion of the latter. There is another iliac flexion that occurs when changing
from the sitting to the standing position, and vice versa. In this movement,
the ilia, instead of flexing to the same side, flex together but in opposite
directions. Allow us to review some important points for emphasis.
Standing. On standing, the pelvis transmits its weight to the head of the
femurs. In order to do so efficiently, the ischia move toward each other. A
separation of the iliac crests therefore occurs. The sacrum then flexes, base
posterior to maintain contact with the iliac articular surfaces. Normally,
when the standing patient stoops forward, this same opening and closing takes
place but now the sacrum is forced inferiorly as if to be drawn down and
wedged deeper into the pelvis.
Iliac A-P and P-A Rotation
Iliac mobility has been the subject of numerous controversies. This is
understandable because in Gillet's studies he found that it can also be influenced by a great many partial fixations of a muscular or ligamentous nature.
Total motion of the different bones of the pelvis takes place in two
parts. With the patient standing and lifting the flexed knee, the ilium on the
side of the knee will follow the movement until its sacral articulation has
reached the end of its range of motion. It will then continue to rotate backward and downward at its sacral aspect, but now it will pull the sacrum down
with it. As the opposite ilium is weight bearing, it will not move, and as a
consequence, the sacrum will glide downward in relation to it, thus producing
an anterior rotation of this ilium. Paradoxically, this movement does not seem
to follow intimately the surfaces of the sacroiliac articulations. They probably gap open to a certain degree. In this movement, the two arms of the
pubic articulation glide one over the other in the anterior-superior direction.
Apart from these multiple movements of the different part of the pelvis
relative to each other, it is evident that there also exist the three fundamental movements of the whole pelvis. For all practical purposes, they can
be considered as movements of the sacrum in relation to the L5. From the fixation point of view, L5 must be considered as part of the pelvis, and it must
be seen in its relationships of lateral flexion and, principally, rotation
between the crests of the ilia.
Why Investigators Differ in Their Conclusions
One of the reasons for the disagreement among investigators who have
studied the function of the pelvic bones in various positions (eg, standing,
sitting, bending forward, etc) is that, unfortunately, the pelvis functions
differently in each of those positions. Another cause for data discrepancies
is that some authors did not clearly define the different positions they
described. They often mention a change of position of an ilium or a sacrum in
relation to what they considered to be the ideal position in space. For many
authors, an ilium was "superior" or "inferior" if it moved "up" or "down."
Little or no mention was made of whether this movement was a sliding motion, a
rotation, or if the sacrum followed the movement or not.
Some authors studied the movement of the sacral articulations relative to
the iliac articulations and described them as moving in relation to the ilia,
when, in fact, it is the opposite that usually happens, especially in walking.
It can be argued that this does not matter much for practical purposes. Unfortunately, when one wants to do fundamental research, it does matter. How often
have we seen would-be men of science argue for hours and not be able to agree
for the simple reason that they had not defined correctly the words they used.
Another mistake often made in spinal research is to consider that the only
"normal" position of a spine is upright, standing, and facing forward the
anatomical position used in textbooks. That is not true. All possible positions of the human body are "normal," at least if the joints are supple.
Humans sit today more than they stand, ride more than they walk, and
recline for about a third of their lives. Why then the emphasis of the
necessity to expose x-ray films of the spine in the standing position? There
may be great changes between the standing and sitting postures, and these
changes can have important clinical meaning. This is also true for the changes
occurring in the recumbent posture.
Gillet's group was therefore forced to take into consideration all the
studies published on the subject, invent many different ways of checking their
accuracy, and push their studies still further to be sure that they had not
missed something. This has taken us years of work; in fact, they were terribly
confused most of the time because they could not put all our findings into a
coherent whole. Today, they hope they have succeeded in solving this problem.
A certain type of chiropractor likes to draw conclusions from anatomical
data. He likes to decide what motion is possible in a joint by looking at the
plane lines of the articulations and at the characteristics of the muscles and
ligaments of the joint. This may sometimes lead the investigator astray as we
have previously shown for the occiput-atlas-axis articulations. Some still
maintain that normal occipitoatlantal rotation is not possible, despite the
fact that it can easily be proved by stress films and motion palpation.
DIAGNOSTIC CONSIDERATIONS
Pelvic Fixations
Total Sacroiliac Fixations
We know today that there are relatively few total fixations of the articular type at the sacroiliacs. By far, most of them seem to be ligamentous. This
region is complicated further by the fact that the superior or inferior portions of the sacroiliac ligaments can become tightened quite separately one
from the other. The pubic articulation can also appear to be in total fixation, which is also due, it would seem, to shortened ligaments.
Sacroiliac Muscular Fixations
The primary muscles that Gillet has found to influence the lumbopelvic
region are the lower portions of the quadratus lumborum, the fibers extending
from the L5 transverses to the crest of the ilia and the two coccygeous
muscles coursing from the inferior part of the sacrum and the superior aspect
of the coccyx to the corresponding part of the ilium. Two other important
muscle groups to consider here are the hamstrings and the lumbar extensors.
The Lumbar Extensors. Shortening of the lumbar extensors has the opposite
effect as that of hamstring shortening. This is a common cause and/or effect
of hyperlordosis. If the hamstrings are normal and the perivertebral muscles
are tight, it will be found that pelvic motion is free but lumbar flexion is
restricted. If movement is forced, overstress is placed on the hips, sacroiliac joints, and posterior soft tissues of the lumbar region. This leads to
chronic strain, sprain, avulsion, spurring, and degenerative arthritis.
Correction of Anterior or Posterior Pelvic Tilt
(2) hypertonicity of the lumboextensors or hip flexors,
(3) contractures of the rectus femoris, or a combination of these factors.
Backward Tilt. Conversely, posterior tilt of the ilium is typically the
result of
(2) shortened hamstrings, or
(3) weakened lumboflexors or hip extensors, or a combination of these factors.
(2) strengthening of weak musculature,
(3) stretching of contractures, and
(4) relaxation of hypertonicity.
The Sacroiliac Ligaments
The Anterior Sacroiliac Ligaments. The primary ligament straps anteriorly
are the thinner anterior sacroiliac ligaments at the superolateral aspect of
the sacrum and the stronger sacrospinous ligaments that extends from the
inferolateral aspect of the sacrum and coccyx to the spine of the ischium. The
superolateral ligaments appear to be little more than extensions from the
anterior capsule.
Sacroiliac Ligamentous Fixations
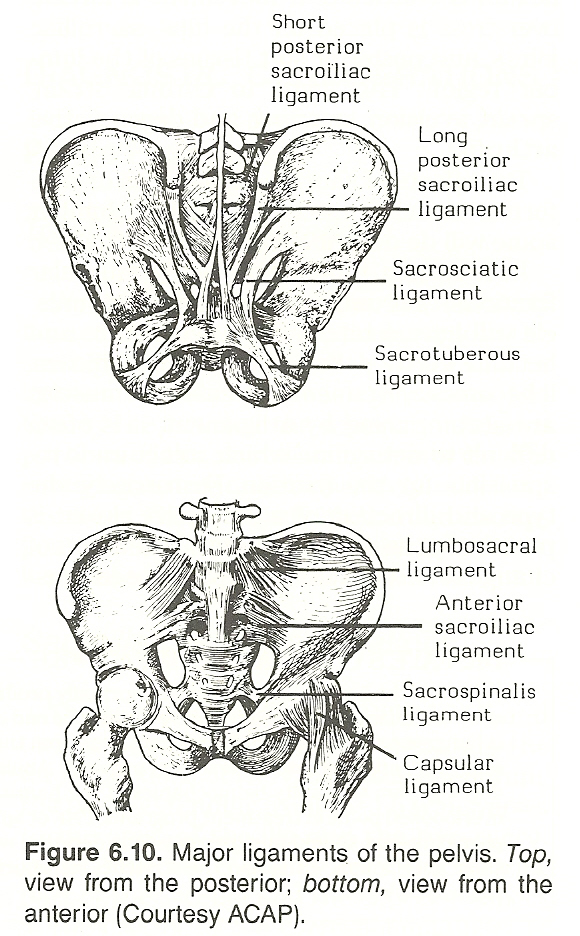
According to Gillet, no other area of the axial skeleton is prone to fixation from ligamentous shortening more than the sacroiliac articulations. In
fact, he feels that it is almost impossible to find a state of clinical imbalance that does not reflect this state. This is probably because few occupations require pelvic motion throughout the maximum range of possible motion.
However, generalized bilateral ligamentous shortening in itself is not
necessarily a cause of clinical concern even if a state of mobility is considered ideal. Gillet believes that the clinical state of the sacroiliac ligaments is determined by the habitual positions the articulations are required
to maintain in the patient's lifestyle. See Figure 6.10.
The iliolumbar, sacroiliac, and sacrotuberous ligaments are common sites
of ligamentous shortening that affect pelvic dynamics, and they appear to
become involved in that order according to Grieve. Gillet, however, reports
many cases of iliolumbar and sacrotuberous fixation without involvement of the
sacroiliac ligaments.
The Iliolumbar Ligaments. The iliolumbar ligaments connect the transverse processes of L5 to the crests of the ilia and sacral base. As an iliolumbar ligament becomes shortened, the iliac crest tends to be pulled medially while the ischium is forced outward. In response to the load above, the sacral base is pushed forward and the sacral apex is pulled backward. Thus, the patient's pelvis will exhibit the normal state of the sitting pelvis in the standing position. This same condition may be the result of a fibrotic or reflexly contracted quadratus lumborum.
Aside from the articular facets, the iliolumbar ligaments are often the most important structures limiting axial rotation of L5 on the sacrum and preventing forward gliding of L5 on the sacrum. Because of its deep position below the iliac crests and the strong strapping by the iliolumbar ligaments and spinal extensors, L5 is only as movable as the sacral base will allow. Thus when lipping or spurs at the inferior aspect of the centrum of L5 are seen (signs of overstress), a history of instability can be presumed.
In Gillet's studies of fixation, as mentioned in the previous chapter, he found that the 5th lumbar acts as part of the pelvis and there the most common ligament at fault is the iliolumbar.
The Sacroiliac Ligaments. When the posterior ligaments shorten, they tend to push the sacral base forward so that the PSISs appear more prominent and closer together. When the anterior ligaments shorten, the sacral base has a tendency to bulge posteriorly, with an unusual mass palpable medial to the PSISs that have flared further apart.
The Sacrotuberous Ligaments. The sacrotuberous ligaments have a strong tendency to shorten. When tight, the sacrum displaces deeper between the two ilia like a driven wedge. With the patient in the lateral recumbent position, deep gluteal palpation will reveal the taut cords. Grieve reports that ipsilateral calf and heel numbness is often associated, thus suggesting sciatic nerve involvement.
Shortening of the sacrotuberous ligaments can also be palpated through the relaxed gluteal muscles when the patient is prone. They will be felt as short, taut, tough cords. The pull of the ligament is usually not total, reports Gillet. In the knee lifting test, the sacrum is capable of moving downward towards the ischium somewhat but it does not move back into its normal location. Furthermore, this motion takes place in one articulation only, the one opposite the side of the lifted knee instead of moving harmoniously in each articulation. This is another example of the hypermobility that usually accompanies partial fixations (ligamentous or muscular).
Shortening of the Sacroiliac Capsular Ligaments. Shortening of the capsular ligaments should give us an "articular" fixation, but here again the amount of fixation is not total for there is still a certain amount of torsion possible in the fixed articulation.
This characteristic of capsule ligament shortening is especially found in extraspinal articulations; eg, in the feet where there are many fixations between the calcaneus, the metatarsals, and the tarsals. These same fixations can also be found in the superior articulation of the fibula with the tibia, in the metacarpals, and in the lateral and medial articulations of the clavicle. Remember that these fixations have noxious effects either in themselves or through the reflex fixations they produce in the spine.
Gillet and associates have found few spinal fixations that can be explain-
ed by shortening of capsular ligaments. On the other hand, practically all
other spinal ligaments seem to be involved in fixations. In fact, ligament
shortening should be a characteristic of all articular fixation, for it is a
normal function of ligaments to take up the slack and adapt themselves to the
amount of motion produced in an articulation.
Sacroiliac Motion Palpation
It has just been explained that covering the sacroiliac articulations are
a host of ligaments which, if normal in tension and elasticity, control
sacroiliac motion and assure that the articular surfaces remain within normal
limits. Unfortunately, most people use a majority of specific and specialized
movements rather than maintaining a healthy mobility in all possible ranges of
motions. This causes one or several of these ligaments to shorten and tighten,
which in turn causes the involved ligament to serve as a new, but abnormal,
center of rotation that may restrict mobility in one or several directions.
The pubic joint, for example, may tighten and effectively hinder A-P and P-A
rotation of the ilia. In the sitting position, however, the sacrum will still
be able to move between the ilia; in fact, hypermobility of both sacroiliac
joints in the sitting position will occur, and at the same time, a total fixation of the ilia will be found in the standing knee lift test described
earlier in this chapter.
Some of Gillet's postulates described previously in this chapter will be
summarized in this section for emphasis.
The Standing Flexed-Knee-Raising Test
The sacroiliac and the lumbosacral joints should be palpated in the standing and/or sitting positions. Several sacroiliac tests are suggested below,
and each should be conducted bilaterally. The thumbs are usually used for
palpation because deep pressure is necessary to hold firm contact during the
tests.
Standing General Sacroiliac Motion. To screen iliac flexion and extension on the sacrum in the standing position, the examiner's thumbs are placed on the patient's PSISs and the patient is asked to raise the right knee up and down, bending the knee as if taking a high step. The right PSIS will be felt to arc posteriorly and inferiorly. After about 20° of leg raise, the patient's left sacroiliac PSIS also drops backward and downward. This is normal sacroiliac motion. Any motion other than this indicates a problem in this joint. Repeat the test by having the patient raise the left flexed knee up and down (Fig. 6.11). If the joint is fixated, the pelvis tends to move as a whole and the ipsilateral thumb will tend to remain level or possibly raise rather than drop. These signs of thumb movement can be seen as well as felt.
Standing Superior Joint Motion. Place one thumb on the sacral base of the patient and your other thumb on the right PSIS. Ask the patient to raise the right flexed knee as if taking a high step, and note the separation of the thumbs. The sacral base will normally be seen and felt to arc ¼–½ inch anteriorly and inferiorly. Or, conversely, the PSIS will move backward and downward. Repeat the test with the patient raising the left flexed knee. During these tests, the tissues over the sacroiliac joint should relax. If the superior sacroiliac joint or the symphysis pubis is locked, the sacrum and ilium will move as a unit, the thumbs will not separate appreciably, and the sacral tissues (ligaments and spinal muscle attachments) will remain taut. This, states Gillet, is probably the most common pelvic fixation found. Invariably, there is a degree of forward tilting of the pelvis and associated lum- bar hyperlordosis.
Standing Inferior Joint Motion. Place a thumb on the patient's sacral apex and your other thumb on the ischial protuberance. Ask the patient to raise the knee on the side first being tested. A ¼–½-inch excursion should be felt as the ischium moves anterosuperior and slightly lateral on the sacrum. If the inferior sacroiliac joint is locked, the ischium and sacral apex move as a unit (Fig. 6.12). Fixation of this motion is most often associated with a contralateral sacral base fixation. The direct cause is usually failure of the muscles acting on the sacral apex to stretch. Piriformis contracture is a common cause, but the iliopsoas or deep glutei may be the cause or a contributing factor.
Anterior Sacral Fixation. In some patients, the anterior sacroiliac ligaments will have shortened but not the posterior ligaments. These anterior ligaments can be divided into superior and inferior straps. If one is short, A-P rotation in the knee lifting test will still take place, but the center of sacroiliac rotation will have changed. Instead of taking place at the head of the femur, it will be found at the offending ligament. A related hypermobility will exist at the pubic articulation. This A-P mobility or immobility can be palpated by placing one thumb on a PSIS and the other thumb on the corresponding part of the sacrum. When the patient lifts the knee, the ipsilateral ilium will normally arc backward and downward. If the contacts are taken on the inferior part of the ilium and sacrum, the former will be felt to move forward and upward. During fixation, both of these movements will be sluggish, quickly reaching their limits and pulling the sacrum into a visible distortion.
Posterior Sacral Fixation. Fixation at the posterior ligaments is more difficult to palpate because the palpating thumbs are over the actual center of rotation, thus unable to register perceptible movement. However, if the patient is turned around and the ASISs are contacted, the knee lifting test will show abnormal mobility. It appears that these forms of sacroiliac fixations also insult the movement of the sacrum itself between the ilia, as tested in the sitting patient, making the motion sluggish or even nonexistent. Bilateral shortening of these ligaments also alters the in- and out-flaring of the ilia when the patient is either standing or sitting.
Gillet's Standing Straight-Leg-Raising Test
With the patient standing, it is also helpful to have the patient lift the
leg with the knee extended. This will produce a decided change in the movement
found in partial fixations, for, as previously explained, the normal movement
of the ilium on the side of the flexed knee is a rotation around a point that
is about the head of the femur. When the knee is not flexed, the pull of the
posterior muscles will change the center of rotation to a point at or near the
pubic articulation (contrary to that seen in the supine position). This will
make no practical difference if these articulations are completely free, but
it may cause a partial sacroiliac fixation to appear as a total fixation. To
make this clear, it will be necessary to describe all possible points of fixa-
tion in this area.
Differential Analysis
It seems that the different sacroiliac ligaments can shorten individually.
Four of these points can be found on each side, two anterior (one superior and
one inferior) and two posterior (one superior and one inferior). Any combination of fixation at these four points on each side can be seen; any two or
three points being simultaneously in fixation would be considered a "total"
fixation. See Figures 6.13 and 6.14. For this reason, a detailed differentiating
form of analysis in this region should be used.
Let us take as an example a sacroiliac fixation at the anterior-inferior
portion of the sacroiliac articulation. It is evident that when the patient's
knee is raised (patient standing), the ilium rotates around this fixed point
rather than around an axis at the head of the femur. There will be motion, but
the motion will be around an abnormal axis. Furthermore, the posterior part of
the ilium opposite the fixed point will appear to move, although the amount of
motion will be smaller than normal. In some cases, especially if the palpator
is in a hurry, this half movement may be mistaken for total motion.
There are other ways of revealing such a fixation for confirmation. One
will be described later when the patient is in the sitting position. In the
standing position, which is our present topic, the following two tests can be
made:
1. When lifting the leg straight, the pubis is blocked physiologically, forcing the facet of the ilium to glide downward on its sacral counterpart. Thus, any fixation in the joint will effectively stop this gliding and the fixation will be more evident.
2. It is also possible to have the patient lift the opposite knee, while you maintain your palpation contacts on the ilium and the part of the sacrum on the side of the weight-bearing limb.
To fully grasp the purpose of this, it is necessary to review the normal
movement of these articulations. When the unfixated subject lifts a knee, the
first part of sacroiliac motion occurs in a gliding manner, in the articulation that does not bear body weight. If, however, the knee is forced a little
higher, the first articulation to come to the end of its range of motion is
the opposite joint, the weight bearing one that is forced to move. That is,
the active ilium continues its motion by pulling the sacrum with it, forcing
the sacrum to move on the opposite ilium.
This motion can be felt and seen when the palpating thumbs are put in contact with the sacrum and ilium on the weight-bearing side. It is thus
necessary, in this test, to have the patient raise the knees one after the
other, putting your thumbs alternatively over the right, left, superior, and
inferior portions of the articulations. There must be palpable-visible movement at all points when each knee is raised to be sure that these articulations are completeIy free of fixation.
When an articulation is completely free, it must be remembered that the
sacrum will remain vertical. If it tips laterally, it is a sign that there is
a partial fixation somewhere. If the point of partial fixation is at the
posterior aspect of the joint, all rotation occurs around that point. No
motion will be felt when either the patient's right or left knee is lifted, or
even when the limb is lifted straight. This may give the impression of a total
fixation, but it is not; for if contact points far removed from the area of
fixation are used (ie, the ischia, the iliac crests, or the ASISs of the
ilia), a definite motion will be felt.
Readers of Gillet's early notes may be surprised that he does not mention
here the test in which the standing patient flexes laterally. The lateral
flexion test can be used, but the amount of mobility in a normal pelvis is
relatively small in this movement and it is difficult to evaluate correctly.
Gillet's Standing Straight-Leg-Extension Test. It is also sometimes helpful to have the patient lift the leg backward. Theoretically, this movement should produce the opposite movement to those described above. In practice, however, this test is not used frequently because, in the standing position, the sacrum comes to rest near one end of its range of motion the ischia are close together, the crests are separated, and the sacral base has moved backward to fill the space between the crests. Posterior movement is therefore normally restricted. This is not true in the sitting position, where the sacrum "floats" at or near the center of its range of motion. This permits the palpator to evaluate motion in the different parts of the pelvis quite easily when the patient is in the sitting position.
Evaluating Horizontal Parallel Sway. Faye attributes the following test for horizontal parallel sway to Grice: The patient stands with legs parallel and is asked to bend sidewards and run the palm of his or her ipsilateral hand down the lateral aspect of the thigh. During the maneuver, the examiner should feel the patient's PSIS glide parallel to the floor in the opposite direction of the patient's lateral flexion. Hip or sacroiliac fixation, however, will cause the PSIS to raise on one side of the pelvis and rotate around one hip joint. Possible quadratus lumborum or psoas imbalance is given as a primary cause.
Gillet's Comments on Palpation in the Sitting Position
Several alternative contacts taken from Gillet's writings will be described in this section. The important thing is to understand what you are palpating and why, then you may select the contacts of your preference.
According to the principle of palpating the major fixations first, it is
helpful to use the back of your hand to generally perceive sacroiliac fixation. As during a spinal screen, your fingers are placed vertically to cover
the whole surface of the sacrum. Your forearm may be reinforced by your thigh,
which can be used to push your palpating hand forward against the patient's
sacrum. This is especially helpful with the patient whose spine has not been
corrected to any great degree because its resistance may fatigue your palpating arm.
The sensation of sacroiliac fixation is evident after it has been felt on
several patients. It can be described as the difference in sensation that is
felt when the hand is pushed against the knee cap (fixation) or the muscles of
the thigh (no fixation, or at least, no total fixation). A total fixation will
be perceived as a resistance to movement at all points of the articulation.
Partial, though important, fixations can be felt if the contact is moved to
the superior or inferior parts of the sacrum, or also to the right and left
articulations. It has been noticed that some students neglect to palpate the
inferior parts of this joint.
Sacral Lateral Flexion During Sitting. Many palpators prefer changing the contact from the back of the hand to the thumb to find the principal area of fixation. In fact, it is even possible to perceive lateral flexion and rotation of the sacrum between the ilia by placing the thumb in the sacroiliac groove at the four points of contact. To judge medial and lateral glide of the upper sacroiliac joint, Gillet palpates just medial to the PSIS and asks the patient to open and close the legs. The ilium should glide medially and laterally over the lateral border of the sacrum.
Lateral flexion and rotation can be felt in still another way, by placing
the lateral aspect of the forefinger vertically against the tips of the sacral
spinouses. The patient is flexed to one side and then to the other with your
free hand on the patient's shoulders. The sacral spinouses should be felt to
glide towards the convexity of the lumbar curve. This movement is normally a
wide and free one. In fact, an abnormal amount of motion may be felt in some
cases. This occurs when there is a total fixation of the pubis.
For palpators who have difficulty in palpating the movement of the whole
sacrum in this way, it is possible to feel the mobility of the superior part
of the joint by contacting the first sacral tubercle with the thumb and then
the mobility of the inferior part of the joint by palpating the end of the
coccyx with the tip of your second finger. The back of the hand is anchored on
the palpating stool, with the tips of the fingers pressed up against the tip
of the coccyx (through the patient's underclothes). On lateral flexion of the
patient, the coccyx will be felt to glide right and left over your finger.
Care must be taken to concentrate the lateral flexion of the patient's lower
back by pushing down and centrally against the patient's shoulder on the side
of lateral flexion.
In lateral bending of the spine, there is also a tilting of the ilia
toward the convexity. This distorts the pelvis into a sort of leaning capital
M in which the two upright lines represent the ilia and the two others (forming the internal V) represent the sacrum. In this movement, the pubis is
forced into lateral gliding. If there is any fixation in this articulation,
the sacral motion will occur, but the ilia will not tip. This movement (or the
lack of it) can easily be felt by placing the palpating thumb on the iliac
crest on the side opposite to the lumbar flexion. Upon forced flexion, this
crest flares laterally.
Contact may also be taken on the ischium of the same side. The palpating
hand is placed as in palpation of the coccyx, with the back of the hand on
the palpation stool and two fingers on either side of the ischium. Upon forced
lateral flexion of the patient, the patient's ischium should normally be felt
to glide laterally.
Sacral Rotation During Sitting. Normal rotation (or its absence) can be felt: (1) on the sacrum by evaluating the lateral movement of the upper sacral tubercles, (2) in the ilium, by contact on the iliac crest and feeling its forward rotation. The ASIS can also be palpated (from the back or the front) and felt to move downwards. Torsion-rotation of the different parts of the pelvis in the sitting position normally takes place around one ischium. The sacrum flexes to the anterior side of rotation, the anterior ilium rotates forward, and the posterior ilium rotates backward but to a lesser degree almost as if all the movement takes place around it.
General Effects of Partial Fixations. Apart from fixations resulting from shortening of the various sacroiliac ligaments, there also exists a certain number of partial fixations in this area that are due to hypertonicity of the sacroiliac muscles mentioned elsewhere in this chapter (especially the coccygeous and the lower portion of the quadratus lumborum). The coccygeous muscles will pull the ischia together, and their hypertonicity will block these two bones in the position that they normally have when the subject is standing. The patient will then prefer to stand rather than sit and will not feel comfortable when sitting for any length of time.
Both coccygeous muscles are not necessarily hypertonic at the same time. When only one is "spastic," the related ilium is functionally as it is in the standing position. When the patient stands, the pelvis seems to be normal because the other ilium takes the same position naturally. When the patient sits, however, one ilium, the mobile one, changes to the sitting position (crest in, ischium out), while the other remains as in the standing position. In this case, the patient's lumbar region will be scoliotic in the sitting position but be straight when standing.
The opposite is true when the lower part of the quadratus lumborum is taut and fails to relax. This pulls the crests of the ilia together and, naturally, pushes the ischia outward. As with the case described above, but in the opposite direction, the patient will feel more comfortable in the sitting posture. In fact, while standing, the patient will rapidly tire and feel pain. Here the lumbar scoliosis will appear in the standing position, and the lumbars will straighten when the patient sits. This point should be quite important to those who radiograph the patient in the standing posture only.
L5 Motion During Sitting. Fixations due to any part of the quadratus muscle or iliolumbar ligament will have also a partial effect on the A-P and P-A rotation of the ilia on the sacrum as seen with the knee lifting test. The knee-raising test will show a characteristic sign of the ilium rotating posteriorly, pulling L5 into rotation with it. With the patient sitting, it is also possible to feel the normal movement between L5 and the ilium on either side by placing the palpating thumb in the space between these two structures and rotating the patient's thorax with your free hand. Normally, the thumb can be pushed relatively easily into this area. The tissues should feel fairly relaxed. If this ligament is shortened, the tissues in the area will feel hard and taut and this will not change when rotating the patient's thorax.
At the other end of the sacrum, we have previously described how the ischia will separate upon lateral flexion and how the coccyx-iliac space will open on one side and close on the other.
Sacral Apex Motion During Sitting. To test forward flexion freedom of the sacral apex with the patient sitting, place a thumb on one PSIS and the other thumb on the sacral apex. Keep in mind that the PSISs are normally about ¼ inch closer together in the sitting position than the standing position due to ischial spread. Note the separation of the thumbs as the patient flexes forward enough to flatten the lumbar curve. This separation will normally be about a half inch if the dynamics are normal. The tissues over the sacrum will be felt to tighten. If either the spinal extensors (multifidi, sacrospinalis) or pelvic extensors (hamstrings, gluteus maximus) fail to elongate during flexion, the sacroiliac joint will be inhibited from above or below, or both, and the lumbars will remain somewhat lordotic. Thus, this type of fixation can be secondary to failure of the lower thoracic and lumbar muscles to stretch. Gluteal lengthening can be further evaluated by flexing the thigh of the supine patient diagonally towards the opposite shoulder. To test motion during spinal extension, take the same contacts described above and have the patient arch the back. The distance between your thumbs should reduce and the tissues overlying the sacrum should relax.
Sacroiliac End-Play Motion During Sitting. The degree of translatory motion (end play) at the end of voluntary motion reflects ligamentous elastcity: The test, originally suggested by Mennell, is made at the end of extension by firm thumb pressure on the sacral apex while the other thumb is on the PSIS. This palpation should elicit further tissue relaxation.
Summary Review of Highlights
Lateral Flexion of the Pelvis During Sitting. Place both thumbs on the patient's PSISs so that your fingers firmly grip the crests of the ilia bilaterally. As the patient curves his trunk laterally, the lumbar spine should arc smoothly. The sacrum will normally tilt towards the side of the concavity,\but the PSISs should remain almost level even though there is some bilaterally reciprocal iliac rotation. The tissues overlying the sacrum on the side of lateral flexion should relax while those on the side of the convexity should tighten. At the end of voluntary motion, added thumb pressure on the sacrum in the direction of its movement should reveal further tissue relaxation. This will not occur if the ligaments have stiffened. If one PSIS raises during lateral flexion, it suggests elongation failure of the lumbar extensors (multifidi, erector spinae) or lateral stabilizers (iliopsoas, quadratus lumborum). If there is bilateral sacroiliac fixation, there will usually be associated lumbar fixations.
In the standing position, lateral sacral flexion is difficult to differentiate from pelvic lateral rotation about the weight-bearing head of the femur.
Position-Change Iliac Alterations. Place your thumbs on the PSISs of a sitting patient. Note the distance between the contacts, and then have the patient stand. Observe the distance between your thumbs. On standing, the PSISs normally open laterally (like a book) so that the inter-PSIS distance increases. If a firm contact can be held on the ischial spines, a reverse reaction will be revealed; ie, the ischia tend to close medially when arising to the standing position. If fixation is present, these iliac and ischial motions will not be felt.
Sitting Iliac Horizontal Rotation. With the patient sitting, place your thumbs on the patient's PSISs and ask the patient to fan his knees open and close several times. As the knees are abducted laterally, the PSISs normally move medially so that they are closer together. Frequently, one PSIS will be felt to move less than the other, indicating a fixation at the inhibited base of the sacrum.
Sitting and Standing Pelvic Changes. Keep in mind the various pelvic changes that occur between the sitting and standing postures that vary with different occupations. These changes are essentially controlled by the sacroiliac-ligament complex. If the superior ligaments are tightened, the crests will be pulled together and actually fix the pelvis in the shape characteristic for the sitting position. Such a patient will feel more comfortable when seated, and spinographs taken in the sitting posture appear quite normal. On standing, however, the crests of such a pelvis would be incapable of separating and the ischia will not approximate. The opposite may also occur; ie, the inferior sacroiliac ligaments may shorten and pull the ischia toward each other, locking the pelvis in the standing position and making sitting uncomfortable if not painful. There are many such states of fixation; eg, one ilium may be blocked or one fixed in a position of flexion on one side and one in a position of extension on the other. Careful analysis is necessary in dif- ferentiation.
It is interesting to see that in Gillet's explanation of his findings in
sacroiliac fixation many concepts of sacroiliac dynamics taught by Hugh Logan
and his son from the 1920s through the 1950s in Basic Technique (and generally
ignored by the profession as a whole) are confirmed. Gillet received his ini-
tial training at Palmer.
Static Palpation
Theoretically, if your thumbs are placed on the patient's PSISs and one
thumb is more posterior and inferior or anterior and superior than the other
when the patient is either standing or sitting, it would indicate a fixed unilateral pelvic rotation. Likewise, if the thumbs are placed on the patient's
PSISs and one thumb is more superior and anterior or inferior and posterior
than the other when the patient is prone, it would indicate unilateral pelvic
rotation. However, because osseous asymmetry is so common, these static signs
are frequently misleading. Dynamic tests, such as those described in motion
palpation, correlated with other signs and the patient's symptoms are much
more reliable during analysis.
Palpating the Lumbosacral Junction
Gillet frequently adds words of caution about palpating the lumbosacral area. He states that the posterior articulations of L5 are probably those in
which errors of palpation can most easily arise. This is because of the wide
range of motion of the sacrum. For instance, if there is movement in the lumbosacral articulation during lateral flexion toward the left, the sacral apex
tilts to the right and the spinous process of L5 glides a little less laterally to the right than the process of the first sacral segment. However, if L5
is fixed to S1 and the sacrum is freely movable, L5 and the sacrum must move
as a whole.
The 5th lumbar vertebra has a great range of movement under the skin but
no appreciable movement relative to the sacrum. Special care must be taken to
feel the scissor-like movement between the spinous process of L5 and the 1st
sacral process and not be misled by the general movement of the sacrum and L5
felt under the skin.
There are other combinations of fixations of the 5th lumbar and the
sacrum. As soon as you are capable of palpating the dynamics in this area, you
will be able to appreciate the different combinations of fixations of this
highly important articular complex.
In the palpation technique described above, Gillet takes into consideration the local movement between two contiguous bones. Palpation of the general
movements of the spine also shows resistance to movement, sometimes of several
spinal segments. In addition, as described in a previous chapter, palpation of
the perivertebral region will usually indicate fixations in the lower thoracic
costovertebral and costocostal complex.
At this point in his teaching, Gillet reviews two points of caution in the
hope of preventing his students from committing serious errors in palpating
the lumbosacral area. The first error is the gliding of the skin over the spinous process, which may give the impression of movement between the spinous
process of L5 and the 1st sacral tubercle even if there is a complete fixation. Therefore, you must concentrate sufficiently to avoid this error.
Secondly, in rotation and lateral flexion, lateral bending of the whole spine
may give the impression of local movement. Constantly keep in mind that the
local movement between two spinous processes is a scissor-like movement. This
mistake, states Gillet, is commonly made in the following areas of the spine:
from C7 to T2, T10 to T12, and L5 to S1.
Differentiating Sacroiliac from Lumbar Fixations
To differentiate sacroiliac from lumbar fixations, Faye offers the following comments for consideration.
With the patient sitting and their hands placed behind their head, rotate
the patient's trunk first to the right and then to the left. Special care
should be taken not to lift the patient's pelvis. Motion restriction of the
patient's left lumbar facets or left sacroiliac joint will reduce rotation to
the left (positive theta Y). Motion restriction of the patient's right lumbar
facets or right sacroiliac joint will inhibit rotation of the patient's trunk
to the right (negative theta Y).
To discern between a lumbosacral or sacroiliac lesion, the patient is
allowed to relax against the doctor (patient's hands are still behind their
head). In this position, the lumbosacral joint is relatively stress free.
Next, twist the patient's trunk into posterior rotation on the right until the
patient's left ischial tuberosity lifts slightly (buttocks remaining on palpation stool). In this position, there is a marked posterior torsion strain on
the right sacroiliac joint. If pain arises in the right sacroiliac that can be
relieved by pushing the left ilium posteriorly, then the pain can be assumed
to arise from the right sacroiliac joint. Reverse the doctor-patient positions
to differentiate fixations on the left. This is Mennell's modified Kemp's test
for the lumbosacral area.
Here are some helpful clues: The patient suffering from sacroiliac dysfunction gets up in the morning with stiffness that improves with activity.
The patient suffering with facet inflammation and/or an IVD lesion arises
improved, but the condition worsens as the day goes on. Fixation produces a
sharp pain on certain movements that is relieved when the site is not
stressed. Other points characteristic of a sacroiliac lesion are:
There is usually unilateral pain in the sacroiliac joint.
The patient may describe an onset involving a lifting or twisting maneuver upon which a "catch" in the back is felt.
The patient has difficulty rising from bed, and the disability is worse in the morning, improving with activity.
The patient has difficulty getting into or rising from a chair because the joints fail to accommodate the normal pelvic changes that occur from changing from a sitting to standing posture.
The associated pain may refer to the
(a) ipsilateral buttock,
(b) ipsilateral posterior thigh (usually no further than the knee),
(c) ipsilateral groin, and/or
(d) ipsilateral anterior thigh (rare). See Figure 6.15.The pain is usually an "achy" type, but it may be sharp on certain movements.
There is usually no severe pain on coughing or sneezing.
There is usually no abnormal neurologic signs, but there may be some current or recent history of paresthesia in the ipsilateral buttock and thigh.
The most common sites of pelvic fixation are found within the sacroiliac joints themselves or the hip joints.
A corrective adjustment frequently results in dramatic relief immediately.
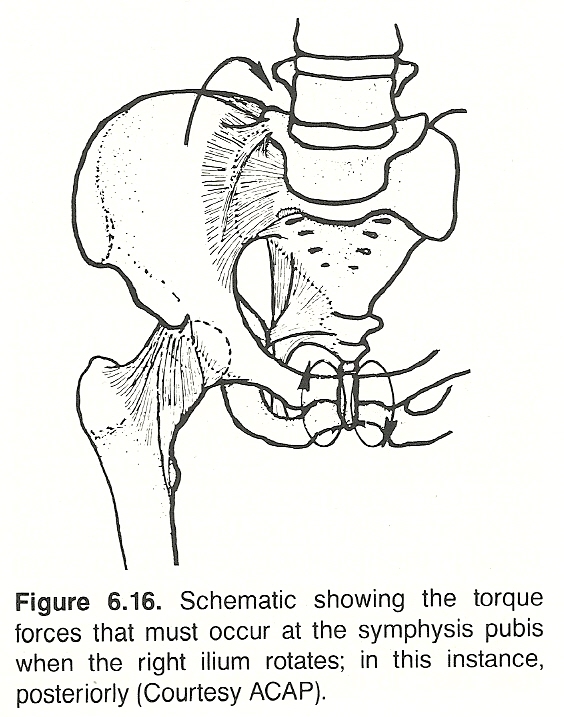 |
(1) normal A-P and P-A iliac rotation does not take place when the pubis is fixated, and
(2) a fixation-mobilizing adjustment results in a rapid improvement in mobility. Neither of these characteristics are typical of ligamentous fixation.
See Figure 6.16.
Myofascial Pain Syndromes
Muscles can undergo changes that of themselves are primary components of a
subluxation complex. If this abnormal state is not treated specifically, it
can severely hinder recovery.
Apart from obvious trauma, states Faye, the examiner must discern if there
are any areas of myodysneuria that serve as a trigger point and/or if there is
a shortening of the overall length of a group of muscles. The iliopsoas, hamstrings, quadriceps, and tensor fascia lata muscles often have areas of
myofascitis.
Proprioceptive neuromuscular facilitation (PNF) and postisometric relaxation (PR) are two effective stretching techniques. It has been Faye's experience that shortened muscles respond best to PNF, PR, or Travell's
"spray-and-stretch" technique. A trigger point refers pain outside its neuromere and should respond to two or three treatments utilizing pressure, ultrasound, electrotherapy, etc. PNF is contraindicated for active trigger points.
Significant Neurologic and Orthopedic Tests
Any patient subjected to pelvic pain should be given a thorough physical,
orthopedic, and neurologic examination, plus any other tests directed by
clinical judgment. Evaluating the possibility of hernia; pelvic, genital, and
rectal lesions; and testing light touch and pain perception should be routine.
Anal, adductor, cremasteric, obliquus, patellar, and Achilles reflexes should
be checked, as well as gross and segmental motions of the lumbar spine,
pelvis, and hips. Following are several additional clinical tests that are applicable for syndromes involving the pelvis. Only a few will be necessary
to apply in any particular case, depending on early clinical suspicions.
Goldthwait's Test. The patient is placed supine. Place one hand under the patient's lumbar spine, with each fingerpad pressed firmly against the interspinous spaces. Your other hand is used to slowly conduct an SLR test. If pain occurs or is aggravated before the lumbar processes open (0° 30°), a sacroiliac lesion should be suspected. In general, Goldthwait believed that if pain occurred while the processes were opening at 30°–60°, a lumbosacral lesion was suggested; at 60°–90°, an L1–L4 disc lesion. If pain is brought on before the lumbar spine begins to move, a lesion, either arthritic or a sprain involving the sacroiliac joint, is probably present. If pain does not come on until after the lumbar spine begins to move, the disorder is more likely to have its site in the lumbosacral area or less commonly in the sacroiliac areas. The test should be repeated with the unaffected limb. A positive sign of a lumbosacral lesion is elicited if pain occurs at about the same height as it did with the first limb. If the unaffected limb can be raised higher than the affected limb, it is thought to be significant of sacroiliac involvement of the affected side. These specific points in differentiation, however, are difficult to explain biomechanically.
In reference to Goldthwait's test, Faye mentions that "The examiner, of course, would have already conducted the SLR test and once pain was experienced would have lowered the leg 5° and then dorsiflexed the foot to see if root stress caused the pain. The examiner must also remember that facet, radicular, and trigger-point syndromes can also be present."
Smith-Peterson Test. If it is possible during Goldthwait's test to raise the limb on the unaffected side to a greater level without pain than the involved side, a positive Smith-Peterson's sign is found, which helps to confirm a sacroiliac lesion; ie, pain usually occurs at the same level for either leg when a lumbosacral lesion is present.
Nachlas' Test. The patient is placed in the prone position. Flex the patient's knee to a right angle, then, with pressure against the anterior surface of the ankle, the patient's heel is slowly directed straight toward the patient's ipsilateral buttock. Stabilize the patient's contralateral ilium with your other hand. If a sharp pain is elicited in the patient's ipsilateral buttock or sacral area, a sacroiliac disorder should be suspected. If pain occurs in the patient's lower back or is sciatic-like in nature, a lower lumbar disorder (especially L3 or L4) is suggested. If pain occurs in the patient's upper lumbar area, groin, or anterior thigh, quadriceps shortening (spasticity or contracture) or a femoral nerve lesion should be suspected.
Erichsen's Test. With the patient supine, place your hands on the patient's iliac crests, and localize your thumbs on the lateral aspect of the patient's ASISs (Fig. 6.17). Forcibly compress the pelvis toward the midline. This tends to separate the sacroiliac joints posteriorly. If conducted very carefully, this test can be quite specific. Pain experienced in the sacroiliac joint suggests a joint lesion (postural, traumatic, or infectious).
Iliac Compression Test. The patient is placed on the side with the affected side up. Place yours forearm over the patient's iliac crest and apply pressure downward for about 30 seconds. This tends to compress the sacroiliac and pubic joints. A positive sign of joint inflammation or sprain is seen with an increase in pain; however, absence of pain does not necessarily rule out sacroiliac involvement. This test is usually contraindicated in geriatrics and pediatrics or with any sign of a hip lesion or osseous pelvic pathology.
Hibb's Test. The patient is placed in the prone position. Stand next to the patient on the side of involvement. Stabilize the patient's contralateral uninvolved hip, flex the patient's knee on the involved side toward the buttock, and then slowly adduct the leg, which internally rotates the femur. Pain initiated in the hip joint indicates a hip lesion; pain rising in the sacroiliac joint but not the hip points to a sacroiliac lesion.
Sacroiliac-Lumbosacral Differentiation Test. To differentiate these two common disorders, the patient is placed supine on a firm flat table. A folded towel is placed transversely under the small of the patient's back. The doctor stabilizes the patient's pelvis by cupping the hands over the ASISs and exerting moderate pressure. The patient is instructed to raise both extremities simultaneously with the legs held straight. If the patient senses discomfort or an increase of discomfort in the low back or over the sacrum and gluteal area at about 25°–50° leg raise and before the small of the back wedges against the towel, sacroiliac involvement is suspected. If, on the other hand, discomfort is experienced or augmented only after the legs have been raised beyond 50° and the small of the back wedges firmly against the towel, lumbosacral involvement should be the first suspicion.
Mennell's Tests. The patient is placed prone, and one hand of the examiner is used to stabilize the contralateral pelvis. With your palpating hand, place a thumb over the patient's PSIS and exert pressure, then slide your thumb outward and then inward. The sign is positive if tenderness is increased. When sliding outward, trigger deposits in structures on the gluteal aspect of the PSIS may be noted. If when sliding inward tenderness is increased, it suggests sprain of the superior sacroiliac ligaments. Confirmation is positive when tenderness is increased when you pull the patient's ASIS posterior when standing behind the patient or when you pull the patient's PSIS forward when standing in front of the supine patient. These tests are helpful in determining that sacroiliac tenderness is due to overstressed superior sacroiliac ligaments.
Sacroiliac Stretch Test. The patient is placed supine. Stand facing the patient, cross the patient's arms, place one of your hands on the patient's contralateral ASIS, and place your other hand on the patient's ipsilateral ASIS. Apply oblique (posterolateral) pressure to spread the anterior aspects of the patient's ilia laterally. A positive sign of sacroiliac sprain is a deep-seated pelvic pain that may radiate into the buttock or groin. While the iliac compression test is designed to stretch the posterior sacroiliac ligaments, this test stretches the ligaments on the anterior aspect of the joints.
Gillis' Test. With the patient prone, stand on the side of involvement. Reach over and stabilize the uninvolved sacroiliac joint while the patient's thigh on the involved side is extended at the hip. Pain initiated by this maneuver in the sacroiliac area of the involved side is a positive sign of an acute sacroiliac sprain/subluxation or sacroiliac disease.
Belt Test. The standing male patient, with feet about 12–15 inches apart, flexes forward while you hold the patient's belt at the back. If bending over without support is more painful than with support, it suggests a sacroiliac lesion. Conversely, if bending over with support is more painful than without support, it suggests a lumbosacral or lumbar involvement. A variation of this test is to stand behind the patient and place your hands so that they firmly support the patient's innominates. Some examiners brace a hip against the patient's sacrum while the patient flexes forward to stabilize the pelvis.
Yeoman's Test. The patient is placed prone. With one hand, apply firm pressure over the patient's suspected sacroiliac joint, fixing the patient's anterior pelvis to the table. With your other hand, flex the patient's leg on the affected side to the limit. The patient's thigh is hyperextended by your lifting the patient's knee off the examining table. If pain is increased in the sacroiliac area, it is significant of a ventral sacroiliac or hip lesion because of the stress on the anterior sacroiliac ligaments. Normally, no pain should be felt on this maneuver.
Piedallu's Sign. When a sacral base is locked unilaterally anteroinferior and lateral so that the adjacent ilium is found to be more posteroinferior and medial than normal, the ipsilateral PSIS on the side of inferiority will be low in the standing and sitting positions. If this PSIS becomes higher than the contralateral PSIS during forward flexion, the phenomenon is called a positive Piedallu's sign. Such a sign signifies either ipsilateral sacroiliac locking where the sacrum and ilium move as a whole or muscular contraction that prevents motion of the sacrum on the ilium. Regardless, it shows that sacral dysfunction is probably present.
Laguerre's Test. With the patient supine, the thigh and knee are flexed and the thigh is abducted and rotated outward. This forces the head of the femur against the anterior portion of the coxa capsule. Increased groin pain and spasm are usually positive signs of a lesion of the hip joint, iliopsoas muscle spasm, or a sacroiliac lesion. This test can help to differentiate a hip or sacroiliac disorder from a lumbar disorder.
Gaenslen's Test. In this test, the patient is placed supine with knees and hips acutely flexed by the patient who clasps his knees with both hands and pulls them toward the abdomen. This brings the lumbar spine firmly in contact with the table and fixes both the pelvis and lumbar spine. Standing at right angles to the patient, bring the patient well to the side of the table and slowly hyperextend the patient's opposite thigh by gradually increasing force by pressure of one hand on top of the patient's knee while your other hand is on the patient's flexed knee for support in fixing the lumbar spine and pelvis. Some examiners allow the hyperextended limb to fall from the table edge (Fig. 6.18). The hyperextension of the hip exerts a rotating force on the corresponding half of the pelvis. The pull is made on the ilium through the Y ligament and the muscles attached to the AIISs. The test is positive if the thigh is hyperextended and pain is felt in the sacroiliac area or referred down the thigh, providing that the opposite sacroiliac joint is normal and the sacrum moves as a unit with the side of the pelvis opposite to that being tested. This test should be conducted bilaterally. A positive sign may be elicited in a sacroiliac, hip, or lower lumbar nerve root lesion. If the L4 nerve is involved, pain is usually referred anteriorly to the groin or upper thigh. If this sign is negative, a lumbosacral lesion should be the first suspicion. This test is usually contraindicated in the elderly.
Lewin-Gaenslen Test. The patient is placed in the sidelying position with the underneath lower limb flexed acutely at the hip and knee. Stabilize the uppermost aspect of the patient's hip with one hand. With your other hand, grasp the patient's leg near the knee and extend the patient's thigh on the hip. Initiated or aggravated pain suggests a sacroiliac lesion.
Lewin's Standing Test. With the patient standing with the back toward you, cautiously forces first the right and then the left knee of the patient into complete extension. Then both knees are straightened at the same time. In lumbosacral, lower lumbar, sacroiliac, and gluteal disturbances, these movements will be accompanied by increased pain and the knee will snap back into flexion.
Mazion's Step-Flex Test. A standing patient with low back pain is asked to take a large step forward, hold this position by keeping the toes in place, and then flex the trunk forward. According to Mazion, the initiation or aggravation of the patient's complaint on the contralateral limb (the one behind) exhibits a positive sign of a unilateral subluxated ilium in relation to the sacrum (ie, sacral base anteroinferior).
Neri's Bowing Sign. This sign is positive when a standing patient can flex the trunk further without low-back discomfort when the ipsilateral leg is flexed than when both knees are held in extension. A positive sign suggests hamstring spasm, contractures of the posterior thigh and/or leg muscles, sciatic neuritis, a lumbar IVD lesion, or a sacroiliac subluxation syndrome.
Minor's Sign. Sciatic radiculitis is suggested by the manner in which the patient with this condition rises from a sitting position. Body weight is supported on the uninvolved side by holding on to the chair for firm support in arising or the patient places the hands on the knees or thighs while working into the upright position, balances on the healthy leg, places one hand on the back, and flexes the leg and extends the thigh of the affected limb. The sign is often positive in sacroiliac lesions, lumbosacral strains and sprains, lumbar fractures and disc syndromes, dystrophies, and myotonias.
Piriformis Spasm Test. The patient is placed supine on a firm flat table.
The patient's heels are grasped and firmly inverted and abducted, and the feet
are externally rotated. If one foot resists this effort and the act is
attended by pain in the gluteal area, piriformis spasm should be suspected.
Differentiation of piriformis spasm from other causes can often be elicited by
reproducing the pain on internal rotation of the femur when it is at a lower
level than the original point of pain.
Ely's Test. To support iliopsoas spasm suspicions, the patient is placed
prone with the toes hanging over the edge of the table, legs relaxed. Either
heel is approximated to the opposite buttock. After flexion of the knee, pain
in the hip will make it impossible to carry out the test if there is any irritation of the psoas muscle or its sheath. The buttock will tend to rise on the
involved side. However, a positive Ely's test can also be an indication of
rectus femoris contraction, a lumbar lesion, a contracture of the tensor
fascia lata, or an osseous hip lesion. Few singular orthopedic maneuvers will
isolate a specific lesion.
Buttock Sign. To conduct this test, a lower extremity of a supine patient
is passively flexed at the hip with the knee extended as in an SLR test. If
the flexion of the limb on the trunk is restricted by local or radiating buttock pain (rather than pain in the hip or lower back), it is significant of an
inflammatory pelvic lesion such as ischiorectal abscess, osteomyelitis of or
near the hip joint, coxa bursitis, sacroiliac septic arthritis, or an advanced
pelvic neoplasm.
(1) that which is due to
irritation of the psoas alone, and
General spasm of the hip muscles is tested with the patient supine and the
limb flexed at a right angle, both at the knee and at the hip. A child may be
tested on its parent's lap. Using the asymptomatic limb as a standard for comparison, draw the patient's knee away from the midline (abduction), toward and
past the midline (adduction), and toward the patient's chest (flexion). Rotation is tested by holding the knee still and moving the patient's foot away
from and toward the median line of the patient.
Patrick's F-AB-ER-E Test This test helps to confirm a suspicion of hip
joint pathology. With the patient supine, grasp the patient's ankle and flex
knee. The patient's thigh is flexed (F), abducted (AB), externally rotated
(ER), and extended (E). Pain arising in the hip during the maneuvers, particularly on abduction and external rotation, was attributed by Patrick to be a
sign of hip pathology. [See Clinical Comment 6.7]
DR. FAYE'S CLINICAL COMMENT #6.7
While doing this test, I find it clinically significant to differentiate capsular restriction from muscular fixation. At the end range of the F-AB-ER-E maneuver, I spring the joint by pressing on the knee. A
springy end feel warrants a stretching technique. The loss of springiness demands a hip joint manipulation
that produces an audible movement and muscle stretching.
(1) sacrotuberous ligament fixation,
It should be remembered that, contrary to what is found in muscular hyper-
tonicity, ligaments can he "pulled" into shape; ie, a slow forcing of the
articulation in fixation can often be sufficient to stretch the shortened
ligament. A dynamic thrust is not always indicated.
(1) Lie supine on a firm surface, flex the right knee toward
the chest, grasp it with both hands, pull the thigh firmly against the abdomen, hold this position for 30 seconds, and then slowly return the limb to the
extended position. During this maneuver, the other limb should remain in contact with the surface on which the patient is recumbent. The same exercise is
then conducted with the contralateral limb.
This exercise will, unfortunately, not have any important effect on total
sacroiliac fixations. It is also evident that the effect of this exercise will
only be momentary in cases where the pelvic fixations are due to fixations
elsewhere, principally those of the feet.
In acute low-back pain cases, marked relief can often be achieved by the doctor, seated behind the sitting
patient, reaching around the patient and pulling the patient's ipsilateral hip into flexion by using a
knee as a fulcrum. This pull should be held for 30 seconds. The relief obtained is often enough to get a
house-confined patient into the office for roentgenography and further care.
(1) break up adhesions in the articulation by opening it,
Gillet's Comments on Common Fixations Found in Lumbago and Sciatica
The Relationship of Upper Cervical Fixation to Low-Back Pain
Gillet insists that a large percentage of low-back pain cases are not
due primarily to lower back fixations. He states that this cannot be emphasized too strongly because there is a type of practitioner who has a tendency
to read medical books and consider that everything written in them is true.
Such a practitioner will invariably think that the only region to correct is
the lower back. If he does not get rapid results in these cases, he feels that
"chiropractic" has been applied in vain and that the case must be rapidly
referred to an orthopedic surgeon.
Gillet maintains that the first region to correct before any other is the
upper-cervical region, even if the trouble appears to be stemming from the
lumbar spine. HIO practitioners have published statistics of these cases in
which only the occiput-atlas-axis complex was adjusted with rapid and gratifying results. There is no reason to deny these statistics, as paradoxical as
they may seem on the surface. The fact that they have sometimes been published
by chiropractors who are a bit fanatically inclined does not eliminate all
their value.
This type of case is often of an overly stressed, highly emotional patient
who has had a mental conflict just prior to the onset of the low-back pain.
The patient, usually, has had similar pains after other emotional conflicts,
and this would tend to show there is an anatomical substratum in the lower
back, one that is not great enough to cause the pain by itself but which would
constitute some type of localizing cause. The occiput-atlas-axis complex is
usually in articular fixation, and the correct adjustment should be given
according to the rules laid down previously. Nothing more need be done at this
time, for if a good correction is made at the top of the spine (the seat of
primary righting reflexes), decided changes will take place in the remainder
of the spine immediately. More changes will take place within the next 24
hours. In a certain number of cases, nothing more need be done at any time,
for the next day the pain will have disappeared and the complete spine will be
found to be moving normally. In other cases, either the atlas is, to start with,
only in partial fixation or it has been corrected. Then an examination should be
made of the pelvis, and thereafter the lumbar spine, searching for total or at
least important fixations in this area.
The Feet
Another part of the body to be taken into consideration in low-back pain
cases is the feet. Gillet recommends that foot fixations should be corrected
last, when the spine shows no signs of recurrent fixations. However, foot
fixations must be investigated and corrected earlier if the spinal fixations
that have been corrected have a tendency to return.
Closing Remarks on Diagnostic Considerations
After motion palpation of the pelvis, often several fixations, complete
and partial, will have been found. Experience shows that it is best to adjust
the articulation that shows the greatest evidence of fixation and contracture,
then the next one in order of importance. Empiric evidence also shows that it
is not the most powerful thrust that is the most corrective. The least force
necessary to move a vertebra is the best because excessive force may lead to
trauma and a reaction contracture. The force of the thrust should be proportional to the resistance of the joint, and it is always best to act prudently.
This method described for spinal analysis is not complete (it is constantly evolving), but it gives today valuable information concerning the mechanical state of the spine. It eliminates the mistake of adjusting a bent spinous
process, it permits an immediate signal that the correction has been made, it
eliminates the danger of repeated x-ray studies, it may be used easily as a
preventive method of examination and correction, and it gives answers to the
questions of when to adjust and when not to adjust (ie, when a segment is
freely movable, there is no need to force movement).
To master the art of motion palpation is not an easy job; but with time,
concentration and steadiness, it gives valuable information on the functional
state of the spine and the way to better and more stable correction. Based on
this principle, chiropractic becomes more scientific and practitioners are led
to a better understanding of the true phenomena that occur in the spine and
how to achieve better results.
THERAPEUTIC APPROACH
Muscular Fixations
Muscle spasms in the pelvis generally reflect themselves in the trunk,
thigh, or both. Shortening of most major muscles acting on the pelvis has a
restrictive influence upon the mobility of the femur and an effect upon an
individual's stance. When evaluating relative muscle function, note that mild
unilateral hypertonicity is difficult to differentiate from contralateral
hypotonicity. In differentiation, static palpation may reveal more than kinetic tests.
Piriformis Hypertonicity
If a patient has deep gluteal pain, sciatic neuralgia, and walks with
the foot noticeably everted on the side of involvement, involvement of the
piriformis should be suspected. Abnormal piriformis tone tends to pull the
sacrum anteriorly and to externally rotate the thigh.
The sciatic nerve should pass under the piriformis and follow the "wisdom"
of the textbooks. In many cases, however, the nerve takes a different course
and is found on surgery to be stretched over or even pass through the muscle
in 15% –20% of the population (ie, about one of every 5–7 patients). This
common "anomaly" and its consequences are often overlooked.
Thomas' Test. This is another test to determine excessive iliopsoas tension. The supine patient holds one flexed knee against the abdomen with the
hands while the other limb is allowed to fully extend (Fig. 6.19). The
patient's lumbar spine should normally flatten. If the extended limb does not
extend fully (ie, the knee flexes from the table) or if the patient rocks the
chest forward or arches the spine, a fixed flexion contracture of the hip is
indicated, as from a shortened iliopsoas muscle. Michelle uses the degree of
pain elicited on forceful extension of the flexed knee as his criteria of
iliopsoas tension. This test should always be conducted bilaterally.
Piriformis Myofascitis Test. The patient is seated on a table with the
hips and knees flexed. Apply resistance as the patient attempts to separate
the knees. In piriformis myofascitis, pain and weakness will be noted on
resisted abduction and external rotation of the thigh. Inflammation will be
confirmed by rectal examination exhibiting acute tenderness over the lateral
pelvic wall proximal to the ischial spine.
Iliopsoas Hypertonicity
In the normal erect posture, only about 12% of the weight of the abdominal
organs is borne by the suspensory ligaments. The majority of weight is supported by the inclined iliopsoas and held there by the abdominal wall.
Increased tone of the psoas major muscle tends to pull the lumbar spine
into anterior and inferior flexion, and externally rotate and flex the thigh.
The psoas minor, which spans between T12 and L1 to the arcuate line of the
hip bone, assists the psoas major.
In psoas spasm, the thigh is flexed to some degree on the trunk, but this
is usually concealed by forward bending of the trunk. Hypertonicity can be
confirmed by tension and pain during deep palpation of the abdomen below the
umbilicus, lateral to the linea alba, medial to and slightly inferior to the
ASIS. The psoas will feel as a taut longitudinal bundle. It is also palpable
in the upper sulcus of the pubic arch.
Bilateral psoas shortening results in lumbar rigidity, anterior pelvic
tilt, and hip flexion. When associated with acute back pain, the patient tends
to flex the knees and hips to help decrease the degree of pelvic tilt and lordosis. When the hip flexors are short, the lumbar region does not flatten in
the supine position unless the knees and hips are flexed. In psoatic sciatica,
states Faye, the patient walks on their toes on the ipsilateral side of
involvement.
Electromyographic studies conducted by Nachemson showed that the iliopsoas
is just as important a lumbar stabilizer against gravitational forces in
standing as it is a hip flexor during gait. Some authorities feel that the
psoas is the key to postural correction.
Michelle, who asserts that 30% of the population has an iliopsoas imbalance, boldly charges that any and all defects of the spine and hip structures
should be evaluated in terms of iliopsoas dysfunction. His studies present
some evidence that practically all conditions working against the "straight
child" are attributable to the failure of the iliopsoas to elongate during
bipedal maturation. He claims: "When the abnormal force of the nonelongated
iliopsoatic musculature is presented bilaterally, the directional force is
symmetrical, with the formation of an exaggerated dorsal kyphosis."
Psoas Abscess
If the urogenital complex, colon, appendix, pancreas, or lumbar lymph
nodes or nerves are diseased, the sheath of the psoas is likely to be secondarily inflamed and painful. As the psoas muscle also crosses the sacroiliac
joint, inflammation is likely to lead to a protective reflex to fix the joint
from irritating motion.
Baron's Sign in Appendicitis. The patient is placed supine, relaxed, and
instructed to breath deeply. The examiner's 2nd, 3rd, and 4th fingers are
placed on the patient's Poupart's ligament and pressure is made in the direction of the psoas muscle. The patient is then told to elevate the leg of the
same side with the knee extended, forming about a 45° angle at the hip. In
this position, the palpating fingers can readily palpate the now tensed psoas
muscle. Similar palpation should be made bilaterally for comparison. In
suspected cases of chronic appendicitis, Baron found that the right psoas
muscle was frequently hypersensitive to pressure. Even in the healthy individual, a tensed psoas may be tender, but when the appendix is involved, the
tenderness is more marked on the right side. It is also important to realize
that because the psoas is covered by peritoneum it can be painful in the presence of sacrospinal and gluteal myalgias; in lumbar, lumbosacral, and
iliosacral arthrosis; and sometimes in sciatica.
General Hip Hypertonicity
Two forms of spasm are common in the hip joint:
(2) that in which all the muscles moving
the joint are more or less contracted. The normal range of hip flexion is
120°. In isolated psoas spasm, motions of the hip (rotation, adduction, abduction, and flexion) are not impeded.
Physical Tests for Hip Pathology
Hip Abduction Stress Test. The patient is placed in the lateral recumbent
position with the underneath lower limb flexed acutely at the hip and knee.
With the upper limb held straight and extended at the knee, the patient is
instructed to attempt to abduct the upper limb while you apply resistance.
Pain initiated in the area of the uppermost sacroiliac joint or the hip joint
suggests an inflammatory process of the respective joint.
Trendelenburg's Hip Test. If the hip and its muscles are normal, the iliac
crest and sacral dimple will be slightly low on the weight-bearing side and
high on the leg-elevated side when one leg is lifted. To test this, have the
patient with a suspected hip involvement stand on one foot (on the side of
involvement), and raise the other foot and leg in hip and knee flexion. If
there is hip joint involvement and muscle weakness, the iliac crest and sacral
dimple will be markedly high on the standing side and low on the side the leg
is elevated. A positive sign suggests that the gluteus medius and minimus
muscles on the supported side are weak. The gait will exhibit a characteristic
lurch to counteract the imbalance caused by the descended hip. The sign is
is not specific, however, It is also commonly positive in a developing
Legg-Calve-Perthes disease, poliomyelitis, muscular dystrophy, coxa vara,
Otto's pelvis, epiphyseal separation, pathology of the superior gluteal nerve,
coxa ankylosis, hip dislocation, fracture, or chronic subluxation of L4, L5,
or the sacrum.
Ligamentous Fixations
Gillet reports that there are three common ligamentous fixations that
occur in the pelvis:
(2) posterior sacroiliac ligament fixation, and
(3) anterior sacroiliac ligament fixations.
These fixations are extremely common and tend to recur unless proper exercises
are conducted frequently.
Sacrotuberous Ligament Fixation
To elongate a shortened sacrotuberous ligament, Gillet recommends a strong
thrust on the apex of the sacrum that is directed cephalad. He states that
this type of maneuver is usually effective, rarely needs to be made more than
once, and that the postadjustive change should exhibit at least a 50% improvement. In contrast, Faye has found that knee-chest stretching exercises are the
most effective.
Posterior Sacroiliac Ligament Fixation
Shortening of the ligaments binding the posterior surface of the sacrum to
the iliac crest is found far more often than sacrotuberous shortening. Tight
posterior sacroiliac ligaments tend to pull the iliac crests posteromedially,
closing the distance between the PSISs (which would indicate movement of the
sacral base anteriorly). Thus, the adjustive thrust should be directed to
separate the joint to allow the sacrum to move posteriorly. A short, stiff
adjustment is recommended by Gillet on the fixated aspect of the sacrum (base
or apex) or on the superior or inferior aspect of the ilium, depending on
where the major fixation is found. The points of contact will vary according
to the particular planes of motion determined to be restricted. Preadjustive
thrusts will help determine whether the major site of fixation is on either
the superior or inferior aspect of the sacroiliac complex.
Anterior Sacroiliac Ligament Fixation
Shortening of the anterior sacroiliac ligaments tends to pull the iliac
crests anterolaterally, increasing the distance between the PSISs, and push
the sacral base posteriorly. The adjustment should be designed to move the
sacral base forward, relative to the ilia, allowing the two ilia to glide
backward. This type of fixation can often be felt by the resistance of the
inferior or superior aspect of the sacrum during preadjustive thrusts.
Supportive and Rehabilitative Exercise
To assist in the elongation process of shortened soft tissues, instruct
the patient to:
(2) After this, both knees are flexed toward the chest in a similar manner.
(3) Each knee is then pulled diagonally toward the opposite shoulder and held there for 30 seconds.
(4) Last but not least, the sitting patient places the lateral side of the ipsilateral ankle on the opposite knee in a figure 4 manner and pushes down on the
medial side of the knee to the point of firm resistance and holds the knee
there for 30 seconds. This exercise should be conducted once each morning and
evening to assure that corrected fixations will not return. If the patient
can effectively conduct this exercise initially, states Gillet, it is likely
that a diagnosis of pelvic ligamentous fixation is in error.
Faye teaches the same technique with the patient in the sitting position.
Little modification is required, and the stretching exercise conducted in
either position will be equally effective. [See Clinical Comment 6.8]
DR. FAYE'S CLINICAL COMMENT #6.8
In bilateral articular fixation of the sacrum or total fixation of the
pubis, all contact points will show no movement, whether the right or left
knee is raised. In unilateral total articular fixation, all points will show a
diminished amount of motion, because only one articulation is functioning. It
will then be necessary to change contacts to the sacrum and each ilium separately to determine the articulation responsible.
Total vs Partial Sacroiliac Fixations
Total Sacroiliac Fixations
It is well to repeat here that in total articular fixation of both sacroiliac articulations, all the tests devised by Gillet will be positive. Even if
the pubis is free, it is evident that a total lack of movement in the sacroiliac articulations will not permit motion in the pubic joint. The contrary is
also true. In pubic fixation, the normal sitting-standing changes in the
pelvis will not be found, the knee-lift test will show no motion, but the
sacrum will still be able to rotate between the ilia (in fact, to a degree of
hypermobility.
Partial Sacroiliac Fixations
Partial fixations of a sacroiliac joint show up differently. The pubic
test will show movement, and the knee raising test will show movement if the
palpatory contact is taken on both ilia but will indicate fixation if the contacts are taken individually; ie, one thumb on the sacrum and the other on the
ilium. Obviously, if the two contacts are made on the articulation in fixation, no movement of the ilium will be felt.
The technique of pelvic palpation is mandated by the great number of
potential partial fixations. This makes it necessary to use multiple contacts
to correctly analyze the type of fixations being palpated (Figs. 6.20 and
6.21). In the first knee-lifting palpation, it is often necessary to use some
eight different points, two on the superior posterior iliac spines, two on the
crests, two near the inferior end of the sacroiliac articulations, and two underneath on the ischia. These last contact points are somewhat difficult to
maintain and especially to follow if movement is normal.
Considerations in the Lateral-Recumbent "Roll" Adjustment
The most popular adjustment in this region is the side-position "lumbar
roll." It is known that this adjustment, as it is usually given, does not
restrict its force to one articulation, much less to one part of an articulation. It is also evident that the same adjustment position can often be used
for many different types of pelvic fixations. Fortunately also, and contrary
to the observations made in other regions of the spine, a poorly delivered
adjustment in this area will have far less adverse effect, either locally or
in the remainder of the spine, not forgetting the highly sensitive upper-cervical region. This should, however, not be interpreted that no harm can be
produced by a traumatizing "cracking" adjustment on the pelvis. We always
desire to use the minimal amount of force necessary to correct the fixation,
no more.
Gillet asks us to remember that an adjustment in any region may be used to
do one of three things:
(2) force it to glide in the plane lines of its articular surfaces (in any
direction that is restricted) but with a preference for the direction that
will "replace" the "subluxated" bone, and/or
(3) move the two bones in fixation in such a way that separates the two ends of the muscle to "break down"
the hypertonicity or apply a force at right angles to the shortened muscle or
ligament to elongate it. In fact, these adjustive effects may explain the dif-
ferent types of adjustments that have been invented by chiropractors since the
turn of the century.
Summary of Sacroiliac Pathodynamics from an Adjuster's Viewpoint
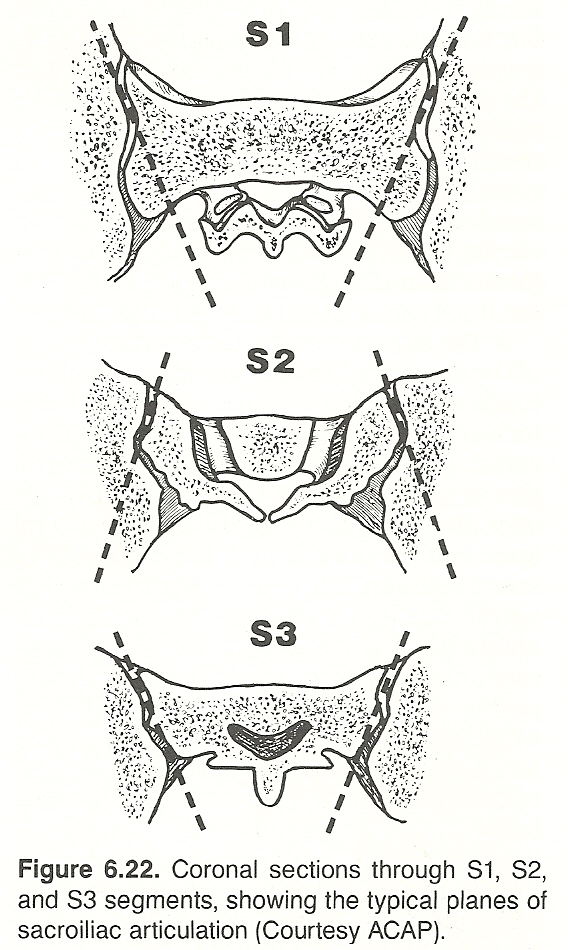 |
Articulation Motion Left superior Iliac rotation posteroinferiorly Left superior Iliac rotation anterosuperiorly Left inferior Iliac rotation posteroinferiorly Left inferior Ischial rotation anteroinferiorly Right superior Iliac rotation posteroinferiorly Right superior Iliac rotation anterosuperiorly Right inferior Iliac rotation posteroinferiorly Right inferior Iliac rotation anteroinferiorly
Some points in communication should be kept in mind when sacroiliac motion is described:
Normal iliac and sacral actions are reciprocally opposite. That is, one might say that the PSIS of the ilium normally rotates backward and downward relative to the sacrum during the knee-raising test. One might also say, and be just as correct, that the sacral base unilaterally rotates forward and downward relative to the ilium. Conversely, if a free ilium rotates upward and forward on the sacrum, the sacrum can be said to have rotated backward and downward on the ilium. Always keep in mind that these terms of rotatory motion are relative. You need no longer be confused when the points of reference (ilium or sacrum) are interchanged.
Inasmuch as iliac and sacral action are reciprocally opposite, it rarely matters whether the adjustive contact is taken on the ilium or the sacrum. For example, a thrust delivered anterosuperiorly on an ilium's PSIS will have the same biomechanical effect as a thrust delivered anteroinferiorly on the sacral apex of that side or anterosuperiorly against the contralateral ischium. Thus, you frequently have the option of taking an iliac, sacral, or ischial contact, depending on how the joint motion is restricted. One exception to this is the obvious fact that it is difficult to move the sacral base backward; much easier to move the ilium forward.
Iliac and ischial actions are reciprocally opposite because they are just different aspect of the same bone, the innominate. When the ilium moves backward and downward on the sacrum, the ischium on the same side must move forward and upward, and vice versa. It has been explained previously that as the iliac crests rotate backward, as in sitting, the sacral base nods forward and the ischia flare laterally. Conversely, when the iliac crests rotate forward, as in standing, the sacral base slides backward and the interischial space decreases.
The options in chiropractic technic are usually not based on mechanical principles, but on their ease of administration. For example, rotating the iliac crest forward has the same mechanical effect as moving the sacral base backward. However, the former is much easier to apply than the latter. Conversely, moving a sacral base or ischium forward has the same mechanical effect as moving the iliac crest backward, but the former is much easier to apply that the latter.
The superior and inferior articulations of the sacroiliac joint on each side resemble a toggle switch. That is, as the sacral base nods forward the sacral apex juts backward. Conversely, as the sacral base slides backward, the sacral apex arcs forward. This toggle effect between the sacral base and sacral apex can be utilized in a large number of sacral technics. It is much easier to move the sacral base posteriorly by a thrust directed anteroinferiorly against the sacral apex than attempt to directly move the sacral base posteriorly. The pressure required anteriorly would undoubtedly injure the pelvic organs and be highly painful to the patient because of the intervening plexus. This toggle effect between the superior and inferior sacral articulations is afforded by the interarticular proturberance on the sacrum that serves as a fulcrum. It is not applicable, however, if the both the superior and inferior aspects of the joint are fixated.
Once these basic principles are understood, chiropractic sacroiliac technics will no longer be a confusing subject. You will immediately see that they
are either logical for the situation at hand or in error.
Adjusting Pelvic Articular Fixations
It is Gillet's opinion that total sacroiliac fixations are second in importance only to total occipitoatlantal fixations. The lesion may be bilateral
or unilateral. If unilateral, the contralateral joint will usually be hypermobile in compensation and be the site of pain and tenderness.
Patient Laterally Recumbent
Gillet recommends the standard side-posture "roll" for releasing
sacroiliac fixations, but special care must be made to deliver the thrust in
the proper plane against the site of fixation. The adjustment may be made with
the patient in the lateral recumbent position by placing the patient so that
the fixated side is upward and taking contact on the the involved iliac crest
or ischium, depending upon what intra-articular motion is to be achieved. This
is the common application. An alternative method is applied by placing the
patient so that the fixated side is downward and taking contact on the contralateral aspect of the sacrum; base or apex, depending upon what intraarticular motion is desired.
In either position, there is no need in most cases to produce heavy
pressure on the patient's flexed knee just enough to stabilize the patient
during the adjustment. It will sometimes be found, however, that a firm
pressure on the flexed knee will be beneficial in opening the superior aspect
of the joint. Each adjustment must be adapted to the needs of the situation
and patient at hand.
The following technics are described by Faye:
Fixation at the Upper Aspect of the Sacroiliac Joint: Involved Side Upward. Place the patient in the lateral recumbent position with the involved ilium facing upward. The patient's uppermost knee is flexed to the maximum. Assure that the patient's lumbars and shoulders are in the neutral position, and apply the contact of the active hand on the PSIS of the involved joint. Support the patient's uppermost shoulder with your stabilizing hand (Fig. 6.23). Open the posterior aspect of the sacroiliac joints by applying downward pressure against the patient's flexed knee with your knee, and with your active hand, deliver an impulse with a body drop directed to mobilize the area of fixation.
Fixation at the Upper Aspect of the Sacroiliac Joint: Involved Side Downward. Place the patient in the lateral recumbent position with the involved ilium against the adjusting table. Assure that the patient's lumbars and shoulders remain in the neutral position. Flex and depress the patient's uppermost knee to stretch the posterior aspect of the sacroiliac joints. Support the patient's uppermost shoulder with your stabilizing hand (Fig. 6.24). Apply contact on the upper quadrant of the sacrum just medial to the PSIS that is closest to the table, and deliver an impulse with body drop directed against the fixation.
Fixation at the Lower Aspect of the Sacroiliac Joint: Involved Side Upward. Place the patient in the lateral recumbent position with the involved ilium facing upward. The patient's uppermost knee is flexed to the maximum (Fig. 6.25). Support the patient's uppermost shoulder with your stabilizing hand. Assuring that the patient's lumbars and shoulders are in the neutral position, apply an ischial contact, depress the patient's knee to open the sacroiliacs posteriorly, and deliver an impulse with body drop to rotate the involved ilium.
Fixation at the Lower Aspect of the Sacroiliac Joint: Involved Side Downward. Place the patient in the lateral recumbent position with the involved ilium against the adjusting table. Assure that the patient's lumbars and shoulders remain in the neutral position. Flex and depress the patient's uppermost knee to stretch the posterior aspect of the sacroiliac joints. Support the patient's uppermost shoulder with your stabilizing hand. Apply contact on the lower quadrant of the sacrum (on the side closest to the table), and deliver an impulse with body drop directed against the fixation (Fig. 6.26).
Patient Prone
If posterior intra-articular adhesions are suspected, the joint may be
opened by "springing" the joint open in either the side position or with the
patient prone. In adjusting a unilateral fixation, the contacts made on the
ilium or ischium are bilateral; ie, one serving as the contact hand and the
other as the stabilizing hand. The thrust should be firm, rapid, and short,
with the abdominal piece of the adjusting table relieved of firm tension.
Lateral flexion mobility of a sacroiliac joint may still be restricted
after A-P and P-A mobility has been restored.
Using Muscle Tension as an Aid During an Adjustment
Schafer advocates using muscle tension as an aid to sacroiliac adjustments
whenever possible. For example, when rotating an iliac crest anteriorly on the
sacral base with the patient in the side position, he does not flex the
patient's uppermost knee. Rather, he flexes the patient's underneath knee and
moves the extended upper limb backward to produce tension on the quadriceps
and hamstring relaxation, which passively helps to rotate the iliac crest
anteriorly. He only flexes the patient's uppermost limb when an ischial contact is taken so that tension on the hamstrings will assist in rotating the
innominate posteriorly. This, states Schafer, is the approach frequently used
in pioneer chiropractic. The more commonly applied flexed uppermost limb positioning taught today is of osteopathic heritage.
The same principles of using muscle tension as a passive aid can be used
when the adjustment is applied with the patient prone. For example, when a
contact is taken on an iliac crest, the patient's extended lower limb can be
raised at the knee with the stabilizing hand to produce tension on the quadriceps and relax the hamstrings. Unfortunately, the advantage of a contralateral
stabilizing hand will be lost. To prevent the contralateral side of pelvis
from raising during the adjustment, a 2-inch-wide leather strap across the
patient's pelvis just below your contact can be used. An alternative is to
have a clinical assistant apply the stabilizing counterpressure.
Patient Supine
The following techniques are taught by Faye:
To perform general posterior rotation of an ilium on the sacrum with the patient supine, flex the patient's knee and hip on the side of involvement. The patient's foot should rest flat and comfortably against the tabletop. Stand on the side of involvement, apply a palm contact over the near ASIS, support the patient's contralateral hip with your stabilizing hand, lean against the patient's flexed knee to bring it toward the medial line and open the sacroiliac joint posteriorly, and then deliver a stiff-arm body drop upon the ASIS. This will rotate the ilium posteriorly (extend) on the sacrum. In stubborn fixations, it may be helpful to place your stabilizing hand under the patient's ischium and lift upward as your active hand applies the thrust against the iliac crest.
To perform general anterior rotation of an ilium on the sacrum with the patient supine, stand on the side of involvement, and shift the patient's body near to the edge of the table where you are standing. Flex the patient's knee and hip on the side of involvement, raise the patient's leg, extending the knee, bring the limb laterally past the side of the tabletop, and allow the limb to lower by its own weight below the level of the tabletop. This will place a stretching force on the anterior muscles of the thigh attached to the ilium that will tend to rotate the ilium anteriorly.
The above technique, not advised for the elderly patient or a patient
afflicted with osteoporosis or coxa pathology, should be applied as a slow
stretching maneuver. If the limb is allowed to drop suddenly in other than a
supple youth, it is easy to produce a groin strain or an anterior dislocation
of the head of the femur. It is also contraindicated in the supple child whose
acetabulae are shallow.
Gillet's Method of Correcting Lumbosacral Kyphosis or Hyperlordosis
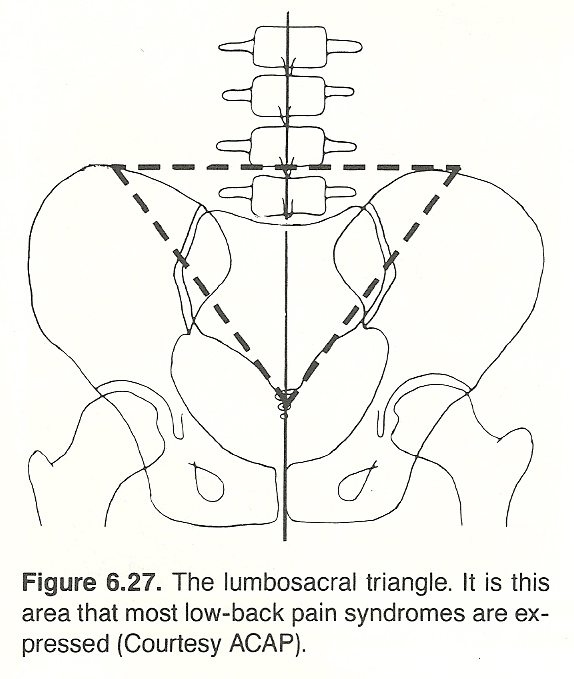 |
Measuring the Amount of Correction Obtained. An effective way to measure the amount of correction obtained, states Gillet, is to place a ruler (about 10 inches long) under the back of the supine patient while he is in full forward flexion. The mid point of the ruler should be centered as nearly as possible over the mid point of the patient's lordosis. A mark is then made on the patient's skin over the two ends of the ruler. After the adjustment, the patient is again put into full forward flexion (sitting), and the distance between the two points described above is remeasured. If the involved spinouses now separate more than before the adjustment, the two points on the skin will be farther apart. In muscle fixations, the change may be as large as a centimeter. In ligament fixations, however, it will rarely exceed 8 millimeters because the involved ligament(s) cannot "relax" like a muscle. It is normal, therefore, to expect a slower change in a ligamentous fixation than in a muscle-induced hyperlordosis.
DR. FAYE'S CLINICAL COMMENT #6.9
In countries where people frequently squat on their heels flat footed, much less degenerated disc disease exists. This squatting posture produces interspinous separation of the lumbar spine. Patients with lumbosacral hyperlordosis should be asked to practice this posture until they can remain comfortable for at least 3 minutes. If they cannot achieve this posture easily, instruct them to hold on to the edge of a desk or a sink until balance is easily achieved. The worse they are at this exercise initially, the more they need it.
Correcting Pubic Fixations
Pubic fixations are of the ligamentous type. The supine exercise previously described for sacroiliac fixations is usually quite effective in correcting
and maintaining pubic fixations. If the pubic fixation is strongly fixed, the
following adjustment should be considered: Place the patient supine and select
the ASIS that has rotated the most anteroinferiorly. Flex the patient's hip
and bring the corresponding knee toward the patient's chest, adding some body
weight of your own if necessary. Stabilizing the patient's contralateral ilium
with your nonactive hand. This is a slow stretching maneuver. A heavy sharp
thrust should never be applied.
Gillet's Comments on Cases of Low-Back Pain
In this concluding section, we will describe the routine of palpation and
correction used by Gillet in all cases of low-back pain of neuromusculoskeletal origin.
In Gillet's practice, for all cases, he searches for total fixations of
the first two cervical vertebrae and corrects them first. In a large number of
cases, nothing else is required if the results are complete and rapid. This
does not mean that the patient's "lumbago" or "sciatica" was simulated or that
it was some type of psychologic "revenge." The upper-cervical fixation did
exist, and it was probably brought on by an emotionally induced contraction of
the muscles at the base of the skull. Any lower lumbar fixation found would
therefore be a localizing factor and the cervical fixation would be the precipitating focus of the patient's pain.
True, these cases would probably get well eventually if these fixations
were corrected in inverse order, or even if they were adjusted during the same
visit. It has been Gillet's experience, however, proved time and again, that
the best, the most rapid, and the most lasting results are attained when the
fixations are corrected in the order suggested (upper cervical, pelvis, and
lower lumbars), with at least several hours between the two corrections to
give time to the body to adapt itself to the corrections made.
Gillet employs the following two palpations:
(1) palpation for total occipitoatlantal fixation (A-P and P-A movement with the palpation contact placed just below the rim of the occiput, on the two sides of the posterior arch;
(2) palpation for total pelvic fixation (A-P and P-A movement, using the back of the hand). Once fixations within these two structure have been corrected, the lumbar vertebra are examined, first for total fixations and then especially for partial fixations.
A question has often been asked about the difficulty of producing the
necessary movements of the spine in palpating for fixations in patients that
are in considerable pain. This is not an insurmountable difficulty. It is easy
to produce small movements that are revealing: motion that is not enough to
exacerbate the patient's pain but enough to reveal any fixations present.
In the lumbar region, three different types of fixation are often found.
In fact, as muscular hypertonicity can be severe in this region, it is not
difficult to see the type of fixation likely present just by recognizing the
characteristic shape of the spinal distortion.
Low-Back Pain on the Convex Side of Lumbar Scoliosis. The most common "distortion" is one of lateral flexion-rotation. This constitutes the basis for the typical "antalgic" posture, which is caused principally by a contraction of the quadratus lumborum that pulls the lumbar vertebrae towards the iliac crest and rotates them posteriorly on the same side. In this type of distortion, the patient's local pain or sciatica will be on the side of lumbar laterality and posteriority. The mechanism of subluxation, states Gillet, will be due to a rotation of L5 on the sacrum, or L4 on L5, in which the pre- and post-zygopophyses have separated, leaving a space between the articular surfaces and forcing the lower facet into the IVF to produce a classic "pressure on nerve." In this type of fixation, it is the lumbar rotation toward the concave side that should take priority consideration because the articulation on that side is still able to function partially. On rotation to the convex side, the movement will immediately be stopped by the hypertonic muscle.
The most efficient adjustment, if the patient can relax enough to permit it, is a "roll" with the patient lying on the concave side. The contact is applied on the iliac crest to exert a rapid traction on the quadratus lumborum. If this is not possible, the muscle may be relaxed by applying a rapid thrust directly on it when the patient is prone and the abdominal piece is free.
Low-Back Pain on the Concave Side of Lumbar Scoliosis. Another type of "sciatica" described by Gillet is one in which the pain is on the concave side of the lumbar scoliosis. Here the mechanism is different. Instead of being separated by muscle hypertonicity, the articulations are pulled together. The offending muscle is invariably the intertransverse. It pulls the vertebrae into lateral flexion and flattens the disc on one side. The patient's pain is on the concave side of the curve, and there is little or no vertebral rotation. Inducing movement (lateral flexion) towards the concave side will be easier in spite of the fact that it is the side of pain. On the contralateral side, however, there will be restriction because of the taut intertransverse muscle (this is typical of all muscle fixations). In this type of fixation, as it is difficult to invent an adjustment that will pull the two ends of the muscle apart, the best thrust is one at right angles to the point of fixation when the patient is prone.
IVD Lesions. The reader may have noticed that little emphasis has been placed on IVD lesions. Gillet's believes that the role of this factor, or its very existence in many cases, has been vastly overplayed. There are probably two types of discal hernias seen clinically:(1) the true rupture, which can be described as an anular "tumor" invading into the spinal canal;
(2) and the false one, which is a posterolateral "bulging" of the disc as the result of abnormal pressure exerted on it by severe muscle contraction. With the second type, anything that will lessen the chronic muscular contraction will relieve the "hernia."Thus, reflex techniques, modalities, or even the anesthesia administered before an operation will have the necessary relaxing effect of the muscles responsible for a "false" hernia.
A great amount of information has been described in this chapter. It is suggested that you review it frequently. We are sure that with each reading you will discover a new idea, a new viewpoint, that will contribute to your clinical proficiency. [See Clinical Comment 6.10]
DR. FAYE'S CLINICAL COMMENT #6.10
As stated in the chapter concerning the thoracic spine for all low-back pain cases determined amenable to manipulation, be sure to include restoring motion to the hip joints and the thoracolumbar junction if these areas are fixated. Both of these sites of fixation can produce hypermobile L4-L5 or L5-S1 function that can readily lead to lower lumbar disc bulging. Upper lumbar and lower thoracic fixations can also produce tension on the spinal cord that results in less angulation of the L5 or S1 nerve roots as they exit from the spine. This more obtuse angulation allows the roots to press against an otherwise tolerable disc protrusion. Such cases will be much more sensitive to Lindner's test, the Soto-Hall test, or a Valsalva maneuver. Thoracolumbar adjustments relieve the root tension, and antalgic postures improve quickly.