

Cervical Radiculopathy: A Systematic Review
on Treatment by Spinal Manipulation and
Measurement with the Neck Disability IndexThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Canadian Chiropractic Assoc. 2012 (Mar); 56 (1): 18–28 ~ FULL TEXT
OPEN ACCESS Robert J. Rodine, BSc, DC, Howard Vernon, DC, PhD, FCCS(C)
Graduate Student, Graduate Education and Research Programs,
Canadian Memorial Chiropractic College,
Toronto, Ontario.
Cervical radiculopathy (CR), while less common than conditions with neck pain alone, can be a significant cause of neck pain and disability; thus the determination of adequate treatment options for patients is essential. Currently, inadequate scientific literature restricts specific conservative management recommendations for CR. Despite a paucity of evidence for high-velocity low-amplitude (HVLA) spinal manipulation in the treatment for CR, this strategy has been frequently labeled as contraindicated. Scientific support for appropriate outcome measures for CR is equally deficient. While more scientific data is needed to draw firm conclusions, the present review suggests that spinal manipulation may be cautiously considered as a therapeutic option for patients suffering from CR. With respect to outcome measures, the Neck Disability Index appears well-suited for spinal manipulative treatment of CR.
From the FULL TEXT Article
Introduction
Cervical radiculopathy (CR) can be a significant cause of neck pain and disability. The reported annual incidence of CR is 83.2/100,000 persons [1], while the reported prevalence is 3.5/1000 persons. [2] Gender preference varies. [2, 3] Individuals are most commonly affected in the 5th and 6th decades of life. [1, 4] Physical exertion or trauma at onset is rare, involving less than 15%. [1] Causal relationship to an automobile accident ranges from 3–23%. [1, 4]
Patients presenting with CR most frequently complain of neck pain, paresthesia and radicular pain. [1] While sensory symptoms typically present along a dermatome, pain is often myotomal. [5] When present, dermatomal pain patterns are more frequent at the C4 level (60%) as compared to the C7 (34.2% of cases) and C6 levels (35% of cases). [3] Scapular pain is found in 51.6% of cases. [3] Physical examination typically reveals painful cervical spine range of motion (ROM) and decreased deep tendon reflexes. [1] Upper limb weakness involves only 15% of cases. [1] Decreased sensation is found in 1/3 of cases; however, muscle atrophy presents in less than 2% of cases. [1] Level of involvement is most typically the C7 (39.3%–46.3%) and C6 (17.6%–42.6%) nerve roots. [1, 3] Bilateral involvement is reported in 5–36% of cases. [1, 4]
The intervertebral disc has be found to be causative in only 22% of cases, while 68% of cases appear to arise from a combination of discogenic and spondylotic causes. [1] With respect to therapy, the Task Force on Neck Pain and Its Associated Disorders (TFNPAD) extensively reviewed the literature to make best-evidence recommendations on the management of neck pain disorders. The review found insufficient evidence to draw firm conclusions or make appropriate treatment recommendations for CR, or identify contraindicated therapies. [6]
This begs the question as to the role of spinal manipulative therapy (SMT) for CR patients’. In fact, Saal et al, stated that “forceful joint manipulation was not used” in their protocol for CR, [7] while Haas et al stated that intervertebral disc herniation and CR are contraindications to manipulation. [8] Unfortunately, statements such as these are unsupported by both basic science evidence which justifies a plausible risk, and epidemiological evidence suggesting hazard or ineffectiveness.
Recently, the first systematic review of manipulative therapy for radiculopathy (including CR) was published. Leininger et al. concluded that evidence for manipulative therapy in CR is minimal, low in quality and presents a high risk of bias. [9] Despite this, 93% of surveyed chiropractors stated they would use SMT despite a suspected or confirmed cervical disc herniation. [10] Therefore, a more detailed review of the existing studies may prove clinically valuable.
A secondary issue concerns the most appropriate outcome measure for determining the effectiveness of SMT for CR? Given that the Neck Disability Index (NDI) is the most commonly used outcome measure of self-rated disability due to non-specific mechanical neck pain, [11] use in a specific cause of neck pain (such as CR) should be evaluated.
The purpose of this paper is to systematically search and descriptively present the evidence as it applies to general chiropractic practice. Therefore, the primary objective of this paper is to review the use of high-velocity low-amplitude (HVLA) SMT for CR, reflecting on chiropractic treatment practices. A secondary objective is to review the use of the NDI, designed for use in neck pain patients, in the management of patients with neck and arm pain.
Methods
Objective 1:
Search Strategy A literature search sought English language manuscripts published before February 28, 2011.

Table 1 The databases of MEDLINE, Alt-Healthwatch, AMED and CINAHL were searched, using the terms found in Table 1. The Index to Chiropractic Literature (ICL) was searched using the terms “cervical radiculopathy” and “manipulation” within “all fields” and limited to the peer reviewed literature.
Relevant manuscripts were hand-searched and content experts were contacted for feedback.
Inclusion Criteria All published, peer-reviewed interventional studies involving more than ten subjects receiving cervical manipulation (defined as an HVLA procedure), delivered by a licensed healthcare professional, for the treatment of CR (confirmed via special imaging and/or clinical examination or described as neck and arm pain/paresthesia) were eligible for inclusion. Studies which presented mixed groups of patients with/without arm pain were not eligible for inclusion.
Manuscripts were excluded if the designs reported data via case-by-case format; identified a mechanical cause of neck and arm pain; involved low-velocity low-amplitude (LVLA) procedures such as mobilizations, flexion-distraction procedures and intermittent cervical traction as the principal method of manipulation (LVLA procedures ancillary to HVLA-SMT were acceptable); thoracic manipulation was principally used; a traumatic mechanism of injury (such as a motor vehicle accident) was identified; or if treatment fell outside the general scope of chiropractic practice (such as manual therapy performed under anesthesia or in combination with injection therapy). This selection process was conducted by one reviewer only (RR).
Quality Reviewing and Data Analysis Formal quality review and data pooling were not conducted. Retrieved manuscripts underwent qualitative analysis only.
Objective 2:
Search Strategy The database PubMed was searched to May 2010 with the key words “neck disability index” and “arm pain.” Retrieved manuscripts were hand-searched for additional citations.
Inclusion Criteria Only articles investigating the psychometric properties of the NDI in the assessment of patients with neck and arm pain were included. This selection process was conducted by one reviewer only (HV).
Quality Reviewing and Data Analysis Data were tabulated on sample characteristics and reliability or validity statistics.
Results
Objective 1:
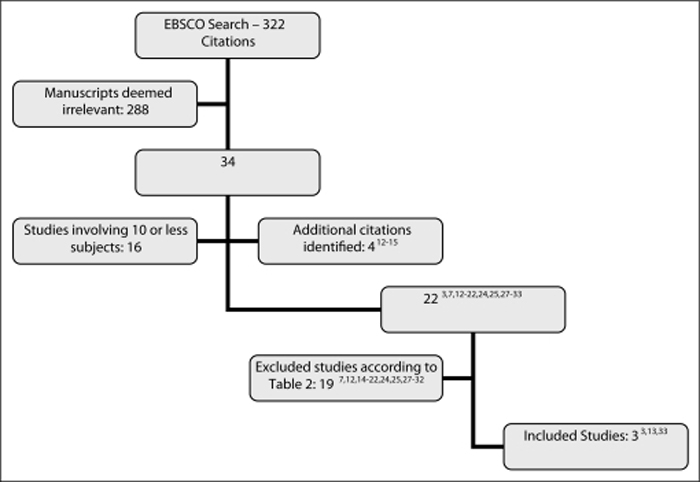
Figure 1
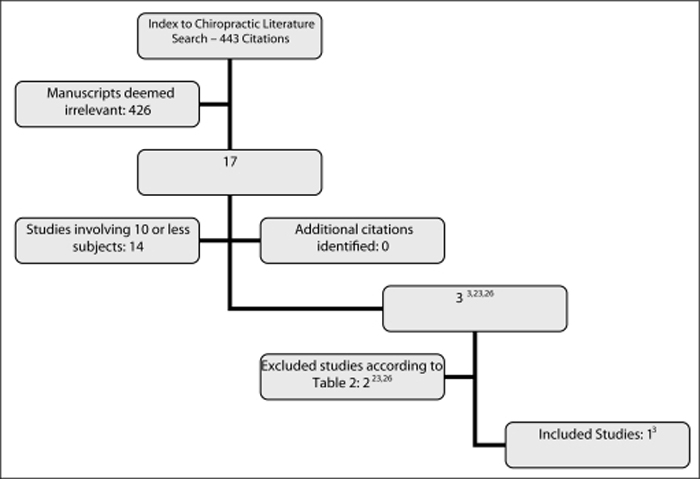
Figure 2

Table 2 The process of literature consolidation and search results is depicted in Figures 1 and 2. Hand searching revealed an additional four citations. [12–15] Contacting content experts provided no further results.
Some inclusions of Leininger et al. [9] were excluded from this paper. As Shin et al. was published as a “letter to the editor” and avoided peer-review, the study was excluded. [12] Moretti et al. was excluded due to “the treatment of benign cervicobrachialgia of mechanical origin.” [13] Walker et al. was excluded given the mixed population of neck pain sufferers, with or without unilateral upper limb symptoms. [13]Table 2 presents the final exclusions, as they are relevant to readers in this field. [7, 14–32] Three manuscripts met the objective criteria. [3, 13, 33]
Study Descriptions Howe et al. [13] used cervical SMT for the treatment of pain/stiffness in the neck with or without shoulder, arm or hand pain/paresthesia, attributed to a lesion of the cervical spine. [13]
Blinded, goniometric ROM measurement of cervical rotation and lateral flexion was assessed before subjects were randomized to either the control or treatment group. Blinded measurement was repeated for the treatment group post-manipulation and subsequent to randomization for the control group, as well as at 1 and 3 weeks following initial consult. [13]
Twenty-six subjects were randomized to each group, a treatment and a control group. Baseline characteristics were comparable, except that more subjects in the treatment group had experienced pain for longer than 4 weeks (6 subjects versus 0). [13]
Arm and hand pain/paresthesia was experienced by 9 controls and 12 members of the treatment group. While a specific cause of CR via clinical testing or special imaging was not identified, arm and hand pain/paresthesia was deemed to be caused by a “cervical lesion” and data was presented separately in this presentation group. [13]
In the treatment group, unspecified manipulation was delivered to 17 subjects once, 4 subjects twice and 2 subjects three times. One subject received both cervical and lumbar manipulation. A subset of subjects received an analgesic injection prior to SMT due to high pain levels (n = 2/26). [13]
In all treated subjects, rotational ROM improved immediately following manipulation by an average of 5°. When results were stratified for patients with arm and hand symptoms, 6/12 members of the treatment group showed ROM improvement immediately following manipulation versus 1/9 of the control group. At 1 week, this number rose to 9/12 in the treatment group versus 4/7 in the control, and 9/11 versus 4/5 at 3 weeks. No statistical significance was found between the stratified groups at any time point.
Symptoms of stiffness and paresthesia were also reported as improved for the treatment group, though supporting outcome data was absent. [13]
BenEliyahu [33] conducted a more detailed clinical case-series. Subjects were required to have neck or back pain with referral into the associated extremity, extremity pain reproduced via stretch testing (ie. shoulder depression test), restricted ROM, neurological deficit and a clinically correlated disc herniation via magnetic resonance imaging (MRI). The overall study included 27 subjects, 11 of which presented with symptomatic cervical disc herniations. [33]
During the acute phase of care, subjects were treated with mechanical traction, interferential current/ultrasound and cold therapy. Cervical rotary SMT was introduced during the subacute phase, along with isometric exercises and stretching. Specific rehabilitation combined with distraction manipulation was introduced during the chronic phase. Subjects were treated 4–5 times per week for the first 2 weeks then 3 times per week with a decreasing frequency as symptoms resolved. Outcome measures included the Visual Analogue Scale (VAS), clinical findings and changes visualized with MRI. A “good clinical outcome” was sought, consisting of a VAS of 2 or less, resolution of extremity pain/paresthesia and improved clinical findings. Repeat MRI was performed upon achieving a good clinical outcome or if subjects had been under care for one year. [33]
Unfortunately, not all data was stratified for cervical and lumbar categories, complicating analysis. For all subjects, the mean duration of care was 9 months. Mean pre-treatment VAS was 6.9/10 and 1.9 post-treatment. Twenty-two subjects achieved a good clinical outcome, 17 of which demonstrated a reduced herniation via repeat MRI. This sub-group experienced an 80% reduction in VAS scores. The remaining 5 subjects demonstrated a marginal or poor clinical outcome, 2 of which demonstrated a worsening of herniation size. In one instance the worsened herniation did not correlate to clinical findings, while the other referred to an adjacent level. This final patient achieved good clinical outcome following 4 months of continued chiropractic care. [33]
Return-to-work data was organized into cervical and lumbar cases, demonstrating a 1 year return to former occupation rate in 82% of cervical cases and 75% of lumbar cases. Details regarding levels of involvement and applied SMT were not reported. No adverse events were reported during care. [33]
Murphy et al’s [3] prospective cohort pragmatically studied 32 confirmed cases of CR. Imaging revealed correlated lateral stenosis in 15 subjects, disc herniation in 10 and a combination in 7subjects. The C6 segment was involved in 23 subjects, C7 in 21, C5 in 7, C4 in 2 and C8 in 1 subject. The mean age of subjects was 47.2 years (24–68; SD 9.2) with a mean duration of symptoms of 46.9 weeks (0.5–260; SD 79.9). The mean baseline Bournemouth Disability Questionnaire (BDQ) score was 37.7 points (11–62; SD 14.8) and a mean Numerical Pain Rating Scale (NPRS) score of 6.4 points (2–10; SD 2.4). A mean of 11.7 treatment sessions (4–24; SD 5.2) were delivered with long-term follow-up averaging 8.2 months (3–23; SD 4.7). [3]
Dysfunctional segments, not mutually exclusive of the level of radiculopathy, received SMT with a thrust-vector directed at symptom centralization. Neural mobilization and muscle energy techniques (MET: low-velocity movements aided by breathing techniques and patient eye movements), end-range loading and over-the-door traction were also employed. Treatment decisions were made as indicated, session to session. The plan of management consisted of 2–3 treatments per week for 3 weeks. Unless subjects were fully recovered at this time point, they were seen 1–2 times weekly. Once fully recovered, subjects were seen every 2–3 weeks for at least 3 months. [3]
Outcome data was available for 31 subjects, 27 of which provided long-term follow-up. The mean self-rated improvement was 75.4% (0–100; SD 24.5), the mean BDQ score was improved by 53% (–240–100%; SD 63) and the mean change in NPRS was 62% (–20–100; SD 34.5) at final re-examination. Compared to baseline, long-term follow-up demonstrated a mean self-rated improvement of 88.2% (40–100; SD 14.9), the mean BDQ score was improved by 78% (5.3–100%; SD 32) and the mean change in NPRS was improved by 72% (66.7–100; SD 43). [3]
All 31 subjects received a manual procedure to the level of radiculopathy, with 18 of these cases being an HVLA procedure and the remaining 13 being MET. No differences were found when comparing HVLA to MET. Adjunctive over-the-door traction was used by 10 subjects. [3]
While no major complications were reported, increased pain not persisting beyond 2 days was experienced by 3 subjects who received HVLA manipulation, 6 subjects who received MET techniques and 7 subjects who received over-the-door traction. [3]
Objective 2:

Table 3 The electronic search identified 91 citations, yielding 5 eligible studies. [28, 34–37] One additional study was identified through hand-searching methods. [38]
The relevant data from these 6 studies are presented in Table 3 and reviewed in the discussion.
Discussion
Strengths & Limitations of the Presented Research
Howe et al’s randomization of a treatment and a control group offered the highest quality design, though only a sample subset presented with arm and hand symptoms. [13] BenEliyahu utilized a lower quality retrospective design and consisted of a small sample size not adequately stratified for cervical case evaluation. [33] Murphy et al. was strengthened by prospective data, though pragmatic application complicated the evaluation of treatment specifics. [3]
Manipulative procedures, examination techniques and outcome measures were highly variable between studies. [3, 13, 33]
Murphy et al. was the only study to adequately describe the indications for SMT, consisting of dysfunctional motion segments identified on palpation in the sitting or prone position, responding with abnormal resistance compared to asymptomatic levels and the presence of clinical symptoms. [3] While Howe et al defines a manipulable lesion to be palpatory evidence of reduced segmental motion and/or palpatory atlas asymmetry, motion parameters, symptom response and positioning details were omitted. [13] BenEliyahu identified only a loss of cervical ROM. [33]
The manipulative procedure was adequately described in all studies. BenEliyahu described using rotational “high-velocity short-lever manipulation.” [33] Howe et al. described moving joints to a comfortable endpoint and delivered a “quick thrust of moderate force” intending to move the joint(s) “as far as comfortably possible.” [13] Murphy et al. moved the spinal joints until “a barrier of resistance” was felt, and delivered a “short and quick thrust.” [3] Only Murphy et al. and BenEliyahu commented that an audible release was usually perceived. [3, 33]
BenEliyahu suggested therapy be modified for stages of healing, utilizing traction and pain-relieving modalities during the acute phase while rotational manipulation was “judiciously added” during the subacute phase. [33] While Murphy et al. did not address this formally, pragmatic treatment showed that only 18 of the 35 patients received HVLA procedures. [3] The remainder of the patients received LVLA techniques and over-the-door traction. [3] Howe et al. did not amend their manipulative protocol; they added an analgesic injection where pain interfered with thrust delivery. [13] While injection therapy is technically part of our exclusion criteria, less than 10% of the subjects in this trial received an ancillary injection, therefore this was not felt to interfere with outcomes. [13]
Unfortunately, the mechanism of injury/onset was not adequately described within these studies. As traumatic onset is less common in CR and presents an alternate pathophysiology, this detail is relevant, [1] though affect on prognosis or treatment has not been commented on in systematic reviews. [39–41]
Conclusions on clinical course from these studies are difficult to draw. Howe et al. detailed a short timeline for outcome measure assessment, following subjects for only 3 weeks and excluded management details. [13] BenEliyahu did not specifically report CR outcomes, aside from the return to work rate at 1 year follow-up. [33] Murphy et al. however provided excellent insight into the clinical course of manipulative therapy as 89% of the patients described their improvement as excellent or good after a mean of 11.7 (4–24; SD 5.2) treatment sessions at a frequency of 2–3 times per week. [3] Long-term follow-up was available for 27/31 subjects, indicating that over 90% maintained clinically significant improvement. [3]
Comparisons of HVLA-SMT versus the natural course of CR are also difficult to draw. Due to high levels of pain and disability, a true no-treatment comparison is difficult to evaluate and control. Therefore, the clinical course of various conservative therapies remains.
For consideration, CR sufferers randomized to hard collar immobilization did not demonstrate statistically different pain scores from baseline at either 4 or 12 month follow-up. [18] Meanwhile, a population based study found that while 90% of CR sufferers reported mild or no symptoms at 4–5 years follow-up, recurrence was observed at 31.7%. [1]
Based on the reported details of the three included studies, it is felt that Murphy et al. provides the best insight into the clinical-course of CR treated with HVLA-SMT. [3]
While limited, non-randomized and without reference to a true control group, this trial may still assist the general practitioner in reasonably designing a trial of therapy. [33]
Reporting of Adverse Events
As previously alluded, concern has been reported regarding the safety of HVLA procedures for confirmed or suspected CR. [8, 10] In fact, published case reports have indicated cervical disc herniation and CR as adverse events related to SMT. [42–44]
While the included studies reported no major adverse events, safety conclusions of HVLA procedures for CR cannot be drawn from this data. [3, 13, 33] While Murphy et al. found a mild transient increase in pain in 16.7% of the subjects receiving HVLA procedures, [3] this is considerably lower than other estimates of similar events experienced in 44–62% of patients receiving SMT for non-specific neck pain. [45–52] Additionally, the TFNPAD did not find SMT to be contraindicated in CR patients. [6] Further research exploring this area is needed to determine proposed mechanisms as well as incidence.
NDI Appropriateness
Only one study reported on the test-re-test reliability of the NDI in neck and arm pain patients. [38] The value obtained, 0.68 (0.30,0.90) is somewhat lower than previously reported for neck pain-only patients. [11] Several studies provided data on the responsiveness of the NDI in neck and arm pain patients. Two studies reported minimum clinically important differences of 7.5 and 7 NDI points, respectively. [28, 38] These values are only slightly higher than those previously reported. [1] One study reported that 20% improvement is a reasonable criterion of clinical success [36] while Carreon et al. provided an estimate of Substantial Clinical Benefit of 9.5 NDI points (19%). [35] Several studies have reported on factors which predicted outcome as measured by the NDI. [11] While varied, these factors generally appear to indicate that low initial pain and distress levels and low impact on neck/arm function predict greater improvement in NDI scores at both 28 days and at 1–3 years.
Taken together, these data support the use of the NDI in studies of SMT for CR.
Review Limitations
First, the existing interventional evidence-base for CR is small and principally composed of low quality study designs. This foundation is further compressed when isolated to a distinct therapy.
Secondly, the inclusion process lacked quality assessment. As this review targets a clinical rather than an academic audience, the limitation is justified. Additionally, in the absence of data pooling, this factor has minimal impact.
Thirdly, the inclusion/exclusion process for each objective lacked consensus. Given the small evidence-base and clearly defined criteria, consensus is unlikely to have altered results.
Lastly, study designs required a threshold of 10 subjects for inclusion. Of the included studies, BenEliyahu presented the smallest sample size, pooling data for 11 CR subjects. [33] During our literature consolidation, no studies were identified that included less than 10 subjects while reporting pooled data. Therefore, it is not felt that this criterion generates bias.
Conclusions
As CR evidence for LVLA and exercise therapy continues to grow, [7, 16–23, 25, 27–32] minimal research concerning HVLA procedures remains. Despite this, existing literature does provide support for the cautious application of HVLA procedures in cases of confirmed or suspected CR.
Currently, randomized trials in the field of CR are lacking. Additionally, the lack of HVLA-related research for CR, particularly comparing HVLA to LVLA procedures, offers a unique and timely opportunity for chiropractic science. In designing such trials, as well as for clinical use, the NDI is well-suited as an outcome measure.
Acknowledgments
Special thanks to the Canadian Memorial Chiropractic College for their continued support of chiropractic research.
References:
Radhakrishnan K, Litchy W, O’Fallon W, et al.
Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990.
Brain: A Journal Of Neurology. 1994;117(Pt 2):325–335Salemi G, Savettiere G, Meneghini F, et al.
Prevalence of cervical spondylotic radiculopathy: a door-to-door survey in a Sicilian municipality.
Acta Neurol Scan. 1996;93(2–3):184–88Murphy D, Hurwitz E, Gregory A, et al.
A Nonsurgical Approach to the Management of Patients With Cervical Radiculopathy:
A Prospective Observational Cohort Study
J Manipulative Physiol Ther. 2006 (May); 29 (4): 279–287Kelsey JL, Githens PB, Walter SD, et al.
An epidemiological study of acute prolapsed cervical intervertebral disc.
J Bone Joint Surg. 1984;66-A(6):907–914Slipman CW, Plastaras CT, Palmitier RA, et al.
Symptom provocation of fluroscopically guided cervical nerve root stimulation. Are dynatomal maps identical to dermatomal maps?
Spine (Phila Pa 1976) 1998;23(20):2235–42Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions: Results of the Bone and Joint Decade
2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123–152Saal J, Saal J, Yurth E.
Nonoperative management of herniated cervical intervertebral disc with radiculopathy.
Spine. 1996;21(16):1877–1883Haas M, Groupp E, Panzer D, Partna L, Lumsden S, Aickin M
Efficacy of Cervical Endplay Assessment
as an Indicator for Spinal Manipulation
Spine (Phila Pa 1976) 2003 (Jun 1); 28 (11): 1091–1096Leininger B, Bronfot G, Evans R, et al.
Spinal manipulation or mobilization for radiculopathy: a systematic review.
Phys Med Rehabil Clin N Am. 2011;22:105–125Croft A.
Appropriateness of cervical spine manipulation: a survey of practitioners.
Chiropractic Technique. 1996;8(4):178–81.Vernon H.
The Neck Disability Index: State-of-the-Art, 1991-2008
J Manipulative Physiol Ther 2008 (Sep); 31 (7): 491–502Shin BC, Kim SD, Lee MS.
Comparison between the effects of Chuna manipulation therapy and cervical traction treatment on pain in patients with herniated cervical disc: a randomized clinical pilot trial.
Am J Chin Med. 2006;34:923–5Howe DH, Newcombe RG, Wade MT.
Manipulation of the cervical spine—a pilot-study.
J R Coll Gen Pract. 1983;33:574–9Moretti B, Vetro A, Garofalo R, et al.
Manipulative therapy in the treatment of benign cervicobrachialgia of mechanical origin.
Chir Organi Mov. 2004;89:81–6Walker MJ, Boyles RE, Young BA, et al.
The effectiveness of manual physical therapy and exercise for mechanical neck pain: a randomized clinical trial.
Spine (Phila Pa 1976) 2008;33:2371–8Honet JC, Puri K.
Cervical radiculitis: treatment and results in 82 patients.
Arch Phys Med Rehabil. 1976;57(1):12–6Rosomoff HL, Fishbain D, Rosomoff RS.
Chronic cervical pain: radiculopathy or brachialgia. Noninterventional treatment.
Spine. 1992;17(10 Suppl):S362–6Persson L, Carlsson C, Carlsson J.
Long-lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar: A prospective, randomized study.
J Manipulative Physiol Ther. 1997;20(7):504Sampath P, Bendebba M, Davis J, et al.
Outcome in patients with cervical radiculopathy: prospective, multicentre study with independent clinical review.
Spine. 1999;24(6):591–597Heckmann J, Lang C, Zöbelein I, et al.
Herniated cervical intervertebral discs with radiculopathy: an outcome study of conservatively or surgically treated patients.
Journal of Spinal Disorders. 1999;12(5):396–401Moeti P, Marchetti G.
Clinical outcome from mechanical intermittent cervical traction for the treatment of cervical radiculopathy: a case series.
J Orthop Sports Physical Therapy. 2001;31(4):207–213Allison GT, Nagy BM, Hall T.
A randomized clinical trial of manual therapy for cervico-brachial pain syndrome-a pilot study.
Man Ther. 2002;7:95–102Schliesser JS, Kruse R, Fallon F.
Cervical radiculopathy treated with chiropractic flexion distraction manipulation: a retrospective study in a private practice setting.
J Manipulative Physiol Ther. 2003;26(9):e19Dougherty P, Bajwa S, Burke J, et al.
Spinal manipulation postepidural injection for lumbar and cervical radiculopathy: a retrospective case series.
J Manipulative Physiol Ther. 2004;27(7):449–56Joghataei MT, Arab AM, Khaksar H.
The effect of cervical traction combined with conventional therapy on grip strength on patients with cervical radiculopathy.
Clin Rehabil. 2004;18(8):879–87Dishman JD, Burke J, Dougherty P, et al.
Spinal manipulation postepidural injection for lumbar and cervical radiculopathy: a retrospective case series.
J Manipulative Physiol Ther. 2004;27(7):449–456Cleland J, Whitman J, Fritz J, et al.
Manual physical therapy, cervical traction, and strengthening exercises in patients with cervical radiculopathy: a case series.
J Orthop Sports Phys Ther. 2005;35(12):802–811Cleland JA, Fritz JM, Whitman JM, Heath R.
Predictors of short-term outcome in people with a clinical diagnosis of cervical radiculopathy.
Phys Ther. 2007;87(12):1619–32Christensen KD, Buswell K.
Chiropractic Outcomes Managing Radiculopathy in a Hospital Setting:
A Retrospective Review of 162 Patients
Journal of Chiropractic Medicine 2008 (Sep); 7 (3): 115—125Young IA, Michener LA, Cleland JA, et al.
Manual therapy, exercise and traction for patients with cervical radiculopathy: a randomized clinical trial.
Phys Ther. 2009;89(7):632–42Kuijper B, Tans JT, Beelen A, et al.
Cervical collar or physiotherapy versus wait and see policy for recent onset cervical radiculopathy: randomized trial.
BMJ. 2009;339:b3883Ragonese J.
A randomized trial comparing manual physical therapy to therapeutic exercises, to a combination of therapies, for the treatment of cervical radiculopathy.
Orthopaedic Practice. 2009;21(3):71–76.BenEliyahu DJ
Magnetic Resonance Imaging and Clinical Follow-up: Study of 27 Patients
Receiving Chiropractic Care for Cervical and Lumbar Disc Herniations
J Manipulative Physiol Ther 1996 (Nov); 19 (9): 597—606Mehta S, MacDermid JC, Carlesso LC, et al.
Concurrent validation of the DASH and the QuickDASH in comparison to the Neck-Specific Scales in patients with neck pain.
Spine. 2010 Epub ahead of printCarreon LY, Glassman SD, Campbell MJ, et al.
Neck Disability Index, short form-36 physical component summary and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion.
Spine J. 2010;10:469–74Peolsson A.
Investigation of clinically important benefit of anterior cervical decompression and fusion.
Eur Spine J. 2007;16:507–14Peolsson A, Vavruch L, Oberg B.
Predictive factors for arm pain, neck pain and neck specific disability and health after anterior cervical decompression and fusion.
Acta Neurochir (Wien) 2006;148:167–73Cleland JA, Fritz JM, Whitman JM, et al.
The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy.
Spine. 2006;31:598–602Carroll, LJ, Holm, LW, Hogg-Johnson, S et al.
Course and Prognostic Factors for Neck Pain in Whiplash-associated Disorders (WAD):
Results of the Bone and Joint Decade 2000-2010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S83–92Carroll, LJ, Hogg-Johnson, S, van der Velde, G et al.
Course and Prognostic Factors for Neck Pain in the General Population:
Results of the Bone and Joint Decade 2000–2010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S75–82Hogg-Johnson, S, van der Velde, G, Carroll, LJ et al.
The Burden and Determinants of Neck Pain in the General Population:
Results of the Bone and Joint Decade 2000–2010 Task Force
on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S39–51Tome F, Barriga A, Espejo L.
Multiple disc herniation after chiropractic manipulation.
Rev Med Univ Navarra. 2004;48(3):39–4Destee A, Lesoin F, Di Paola F, et al.
Intradural herniated cervical disc associated with chiropractic spinal manipulation.
J Neurol Neurosurg Psychiatry. 1989;52(9):1113Rydell N, Räf L.
Spinal manipulation – treatment associated with a high risk of complications.
Lakartidningen. 1999;96(34):3536–40Malone DG, Baldwin NG, Tomecek FJ, et al.
Complications of cervical spine manipulation therapy: 5-year retrospective study in a single-group practice.
Neurosurg Focus. 2002;13(6):ecp1Rubinstein SM, Leboeuf-Yde C, Knol DL, de Koekkoek TE,
Pfeifle CE, van Tulder MW.
The Benefits Outweigh the Risks for Patients Undergoing Chiropractic
Care for Neck Pain A Prospective, Multicenter, Cohort Study
J Manipulative Physiol Ther 2007 (Jul); 30 (6): 408–418Rubinstein SM, et al.
Benign adverse events following chiropractic care for neck pain are associated with worse short-term outcomes but not worse outcomes at three months.
Spine. 2008;33(25):E950–E956Rubinstein SM, et al.
Predictors of adverse events following chiropractic care for patients with neck pain.
J Manipulative Physiol Ther. 2008;31:94–103Senstad O, et al.
Predictors of side effects to spinal manipulative therapy.
J Manipulative Physiol Ther. 1996;9:441–6Senstad O, et al.
Frequency and characteristics of side effects of spinal manipulative therapy.
Spine. 1997;22(4):435–441Leboeuf-Yde C, et al.
Side effects of chiropractic treatment: a prospective study.
J Manipulative Physiol Ther. 1997;20:511–516Cagnie B, Vinck E, Beernaert A, et al.
How Common Are Side Effects of Spinal Manipulation And Can These Side Effects Be Predicted?
Manual Therapy 2004 (Aug); 9 (3): 151–156
Return to RADICULOPATHY
Return to CHRONIC NECK PAIN
Since 3–31–2012


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |