

Factors in Patient Responsiveness to Directional Preference-Matched
Treatment of Neck Pain With or Without Upper Extremity RadiationThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Patient Cent Res Rev. 2017 (Apr 25); 4 (2): 60–68 ~ FULL TEXT
OPEN ACCESS Benjamin Holmes, DC, Ruta Brazauskas, PhD, Laura D. Cassidy, PhD, Rachel A. Wiegand, DC
Institute for Health and Equity,
Medical College of Wisconsin,
Milwaukee, WI.PURPOSE: Patient-related predictive factors in responsiveness to directional preference therapy for neck pain with or without upper extremity radiation (NP/R) have not been reported. A directional preference is any neck movement that, when performed repeatedly to end range, results in centralization and/or alleviation of NP/R. It was hypothesized that patient compliance with a prescribed, directional preference-matched home exercise program would improve positive responsiveness to NP/R treatment.
METHODS: Patient-related factors thought to affect responsiveness to care were collected retrospectively from charts and de-identified for patients with NP/R who underwent chiropractic treatment at a multispecialty spine clinic from January 2014 through June 2015. Responsiveness was measured by calculating the percentage change in Neck Bournemouth Questionnaire (NBQ) scores over treatment time. Multiple linear regression was used to identify factors associated with positive responsiveness.
RESULTS: Mean percentage change in patient NBQ score from initial intake to discharge was 50% (standard deviation: 32%). Of 104 patients meeting study inclusion criteria, 86 (83%) reported experiencing improvement after the first treatment session. Bivariate analysis of patient characteristics by compliance with directional preference-matched exercise indicated that compliant patients (n=95, 91%) demonstrated significantly greater responsiveness to care than did noncompliant patients, at 55% versus 25% change in NBQ score, respectively (P=0.0041). Four factors were statistically significant predictors of patient responsiveness to directional preference therapy for NP/R: patient compliance with directional preference-matched exercise (P=0.0023), patient age (P=0.0029), condition chronicity (P<0.0001), and whether the patient reported improvement of symptoms following initial treatment session (P=0.0003).
CONCLUSIONS: The results of this study suggest that patient compliance with directional preference exercise is associated with patient responsiveness to conservative treatment of NP/R, as are age, chronicity and report of immediate symptom improvement.
KEYWORDS: Bournemouth questionnaire; directional preference; neck pain
From the FULL TEXT Article:
Background
Neck pain is common among adults, with global annual incidence rates reported between 10.4% and 21.3%. [1] It is the fourth leading cause of disability globally. [2] Neck pain can be accompanied by upper extremity radiation of pain, paresthesia, numbness or weakness, sometimes attributable to cervical radiculopathy. The annual age-adjusted cervical radiculopathy incidence rate in one large epidemiological survey in Minnesota was 83 per 100,000 persons. [3]
Several conservative treatment options are available for neck pain, including “wait and see,” [4] spinal mobilization or manipulation, home exercises, physical therapy modalities, medications and epidural steroid injection. Evidence of the efficacy of conservative management is tenuous. Some evidence suggests that exercise may be beneficial for neck pain. [5] Studies supporting conservative management of neck pain with upper extremity radiation are even sparser, and randomized controlled trials are needed to examine the clinical effectiveness of conservative treatments. [6]
One conservative treatment approach is called directional preference therapy. Variations of directional preference therapy have been studied and performed under different monikers, namely the McKenzie approach [7] and mechanical diagnosis and therapy (MDT). [4, 8] Directional preference involves manual therapy, exercise therapy or both, which are predicated on the discovery of a “directional preference” during the physical examination. A directional preference is any specific neck movement that, when performed repeatedly to end range, results in centralization and/or alleviation of neck pain with or without upper extremity radiation (NP/R) as well as improved mechanical presentation (eg, improved active global range of motion). [9] Once the preference has been ascertained, the directional preference practitioner may utilize, if necessary, the specific direction when performing manual therapy to the spine and match the direction in prescribing home exercises.
Eight clinical trials have assessed directional preference therapy in treating NP/R, [7, 10–16] but the trials lack definitive evidence of treatment efficacy. One systematic review assessed directional preference therapy for neck pain and concluded that directional preference therapy may not be significantly more effective than a “wait and see” approach for neck pain; however, skillset adequacy of the directional preference therapists in the included studies was questioned. [4] Several studies have evaluated and supported directional preference therapy for lumbar spine pathology. [17–23]
This study evaluated characteristics of NP/R patients and responsiveness to directional preference therapy. Recognizing both the theoretical value of directional preference-matched home exercise performance and the capability of self-management in patient-centered care to improve health outcomes, the investigators conducting this study hypothesized that patient compliance with a prescribed, directional preferencematched home exercise program would improve responsiveness to conservative treatment of NP/R.
METHODS
The local institutional review board determined that this study, designed primarily as a quality assessment and improvement project, did not constitute human subject research.
A retrospective chart review was conducted for all patients who presented with axial NP/R and who demonstrated limited and/or painful active cervical range of motion, showed a directional preference on evaluation and underwent directional preference treatment by a single chiropractor at a spine clinic within a large health system from January 2014 through June 2015 (N = 245). Patients whose symptoms and signs did not satisfy the above diagnostic criteria, who were younger than 18 years, who suspended care prematurely or for whom outcome data were incomplete were excluded from the study. Data were de-identified prior to statistical analysis.
Aside from the chiropractor, this study’s clinic team comprised an orthopedic spine surgeon, three orthopedic physician assistants and four pain proceduralists. Occasionally throughout the course of individual patient care, other treatment modalities were utilized as prescribed/performed by team physicians, assistants and proceduralists, including the prescription of anti-inflammatory, muscle relaxant, analgesic and anti-epileptic medication and epidural steroid injection. Treating members of the clinic team along with individual patients made the decision to utilize these modalities on a case-by-case basis. Anti-inflammatory, muscle relaxant and analgesic medications were prescribed in the presence of either neck pain alone or neck pain with upper extremity radiation. Anti-epileptic medication and epidural steroid injections were recommended only in cases of neck pain with upper extremity radiation.
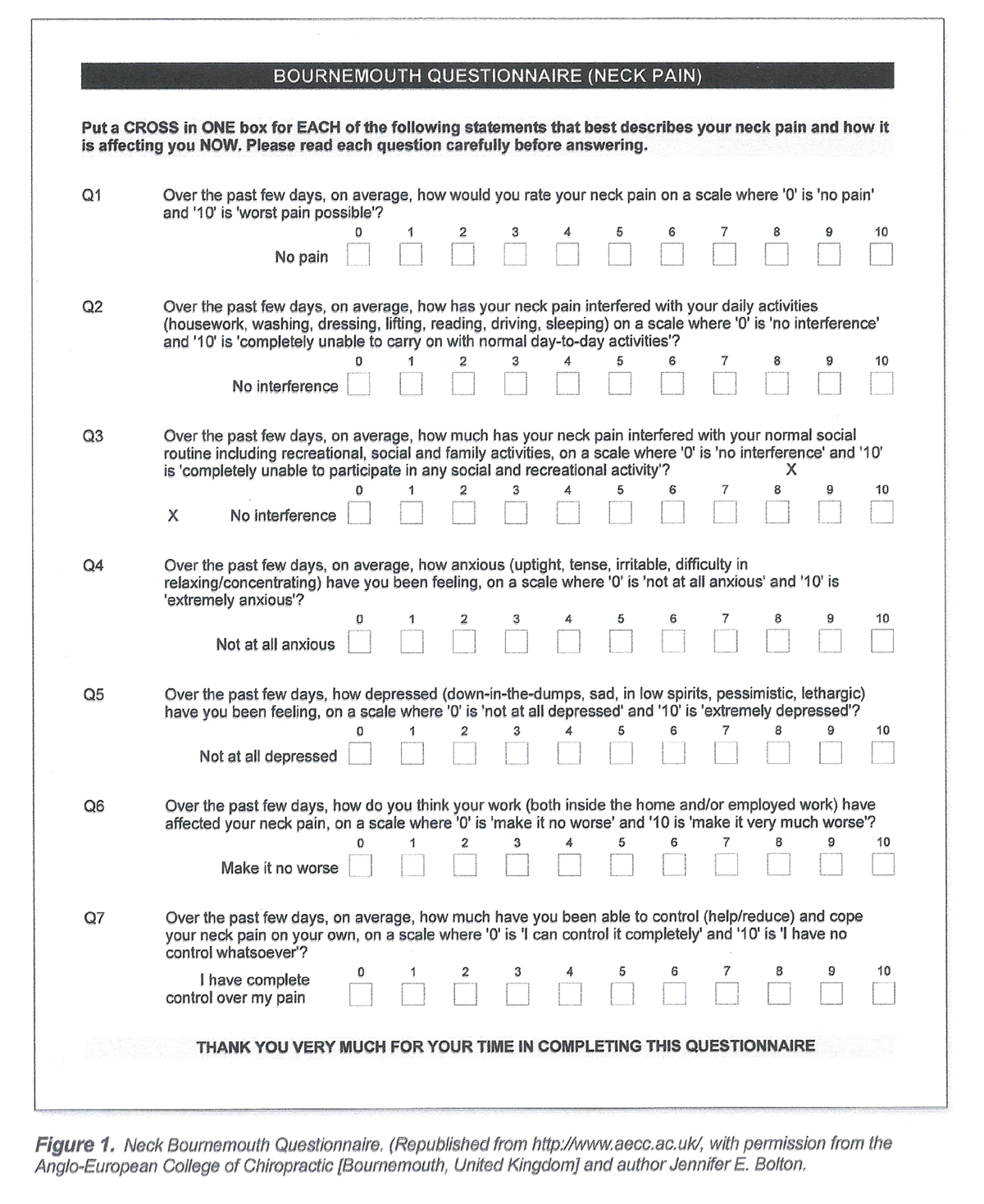
Figure 1 Responsiveness to directional preference therapy was measured by changes in scores reported by the patient on the Neck Bournemouth Questionnaire (NBQ) pre- and post-treatment span. The NBQ is a reliable, responsive and efficient outcomes measurement tool (Figure 1) to assess the effects of patients’ neck conditions on seven aspects of their lives: pain, activities of daily living, social activities, anxiety, depression, work and fear-avoidance beliefs, and locus of control. [24–27]
This study assessed patient compliance with prescribed directional preference-matched home exercises as a predictive factor of positive response to directional preference therapy. Other patient characteristics analyzed as factors in responsiveness were: age, body mass index, comorbidities of anxiety or depression, diagnosis, sex, whether the patient reported improvement immediately following the first treatment session, payor, treatment dosage, number of treatments throughout course of care, smoking status, condition chronicity, and prescription medication usage (including epidural steroid injection).
On initial presentation to the chiropractor, the patient complaining of neck pain with or without upper extremity pain, numbness, paresthesia or weakness underwent directional preference assessment. The directional preference assessment process is well-described in the literature [9, 28] (and a synopsis is provided in this paper’s introduction). Following the ascertainment of a directional preference in the patient with NP/R, exercise and manual therapies matched to the preferred direction were performed. NBQ scores were assessed at intake and every 2–4 weeks thereafter until the patient’s condition was determined fixed and stable, and the patient was released from care.
Occasionally, NP/R symptoms returned after the patient was released and care was reinitiated, creating a subsequent course of treatment. After the NBQ scores were collected, the percentage change was calculated, meaning the difference between a patient’s NBQ score at intake and at the conclusion of the treatment course, divided by the score at intake, and multiplied by 100, with positive percentages indicating improvement and negative percentages indicating decline. [29]
Statistical Analysis
Patient characteristics were summarized with descriptive statistics. Patient-related factors were compared between exercise-compliant and exercisenoncompliant groups using Wilcoxon rank-sum test for continuous variables and χ2 test for categorical variables.
Multiple linear regression analysis was used to model patient responsiveness to directional preference therapy in relation to: age; body mass index; comorbidities of anxiety and/or depression (as determined by presence of anxiety and/or depression diagnoses in the patient’s electronic medical record); NP/R primary diagnosis variation (neck pain without upper extremity radiation or neck pain with upper extremity radiation); sex; reported improvement after first treatment session (yes or no); payor (commercial or noncommercial insurance, the latter of which includes self-pay, personal injury, workers’ compensation, Medicaid and Medicare); reported compliance with the home exercise program as prescribed; treatment dosage (number of treatments per days of treatment span); total number of treatments throughout the course of care; smoking status; chronicity of symptoms (acute/ subacute or chronic/acute-on-chronic); and the use of prescription substances (anti-inflammatories, muscle relaxants, analgesics, anti-epileptics and/or epidural steroids). A backward elimination model selection procedure was used to identify statistically significant covariates to include in the model. Significance was defined as P<0.05 throughout. SAS OnDemand for Academics software (SAS Institute, Cary, NC) was used to perform statistical analysis.
RESULTS

Table 1 A total of 104 patients, undergoing a total of 119 treatment courses, met the inclusion criteria and were included in the analysis. The largest number of treatment courses per patient was four (which occurred in 1 patient); 8 of the 104 patients underwent two treatment courses and 2 patients underwent three courses. The average number of treatment sessions per course of care was 6.8 (Table 1). For analysis purposes, only a patient’s first treatment course of NP/R was considered.
Also shown in Table 1, the mean age of study population was 47 years (standard deviation: 12.0), and 68% of patients were female. The mean change in NBQ score with respect to initial reported score was 50% ± 32%; 86 patients (83%) reported experiencing improvement after the first treatment session, and 95 patients (91%) reported being compliant with the prescribed home exercise program. A majority of patients (n = 65, 62.5%) suffered from chronic or acute-on-chronic pain as opposed to acute/subacute pain. Chronic pain was defined as neck and/or upper extremity pain that had been persistent for greater than 3 months, acute pain defined as less than 7 days, subacute pain defined as lasting between 7 days and 3 months, and acute-on-chronic pain defined as a flare-up of acute or subacute pain in the presence of underlying chronic pain.

Table 2

Table 3

Table 4 Table 2 shows the results of the bivariate analysis of patient characteristics by compliance with prescribed directional preference-matched home exercise. Exercise-compliant patients (“exercisers”) demonstrated significantly improved responsiveness to care compared with noncompliant patients (“nonexercisers”), with a 55% and 25% change in NBQ score, respectively (P = 0.0041). Only 25% of exercisers experienced depression compared with 78% of nonexercisers (P = 0.0010). Payor classification varied significantly between the two groups as well — 91% of exercisers were commercially insured, whereas 44% of nonexercisers were noncommercially insured (P = 0.0024). No statistically significant difference between exercisers’ and nonexercisers’ chronicity of symptoms was found.
Results of multiple linear regression are summarized in Table 3. Compliance with a prescribed directional preference-matched home exercise program was positively associated with responsiveness to directional preference therapy (P = 0.0023), and condition chronicity was negatively associated (P<0.0001). Patient age ≥ 55 years and noted improvement of symptoms following the initial treatment session also were both positively associated with responsiveness to therapy (P = 0.0029 and P = 0.0003, respectively).
Patient responsiveness to directional preference therapy based on combinations of patient characteristics within the best-fit linear regression was estimated (Table 4). Analysis was repeated to include all treatment episodes. Results of this secondary analysis (data not shown) were very similar to the presented analysis, which involved only the first treatment episode.
DISCUSSION
The general agreement among health scientists is that patient engagement and participation in health care, such as via home exercise performance, are beneficial; however, clinical trials and reviews specifically evaluating directional preference therapy for NP/R are sparse and insufficiently informative. While the results of this study are consistent with previous studies that support the use of directional preference therapy in treating NP/R, [7, 10–16 our results also explicate specific patient-related factors in responsiveness to directional preference therapy outside the practitioner-related factors studied prior. For instance, these findings suggest a possible mechanism behind limited responsiveness of neck pain patients to directional preference therapy reported in the systematic review by Takasaki and May, [4] as 61 of the 100 patients from two of the five trials studied by the authors had suffered from neck pain for more than 3 months. Our finding that chronicity of symptoms is a predictive factor in patient responsiveness to care may provide an explanation of limited responsiveness to directional preference therapy in those two trials.
This study has limitations. Several data points are patient-reported, such as NBQ scores, chronicity, improvement following initial treatment session, compliance with directional preference home exercises and smoking status. These data are subjective reports and potentially carry social desirability bias (for example, the underreporting of smoking and overreporting of exercise compliance). Also, some of these reports relate to the patient’s experience with pain. Because pain and its effects are a subjective experience, some level of subjectivity is inescapable. Nevertheless, by comparing percentage change of NBQ scores — which are intrapersonal ratios and therefore control for personalization [30] of the pain experience — instead of raw NBQ scores, data volatility is maximally neutralized and interpersonal comparability maximally facilitated. Small patient numbers limited some comparisons, particularly regarding nonexercisers.
Because the study population was predominantly Caucasian and commercially insured — a make-up that accurately reflects the overall patient population at our clinic — findings are not generalizable. However, they will inform processes to assess and improve quality at our institution (and perhaps those that are similar) as well as motivate and guide further research of directional preference therapy for NP/R. These findings may inform further assessment of larger samples in more demographically diverse settings. Dissemination of these results may motivate patients to comply with directional preference home exercises and also encourage regional clinicians to enlist patient involvement when treating NP/R. Local directional preference practitioners also can use these findings to inform themselves and patients of likelihood of responsiveness to care at the early outset of treatment, which could be financially, emotionally and therapeutically beneficial to the patient.
CONCLUSIONS
Patient compliance with directional preference exercise is associated with patient responsiveness to directional preference therapy in conservative care treatments of neck pain. Patients 55 years of age or older, those with acute/subacute chronicity and those who report symptom improvement following the first treatment session showed significant improvement. Implementation of these findings could improve care of patients with neck pain, with or without upper extremity radiation, at a local level.
Patient-Friendly Recap
Patients experiencing persistent neck pain with or without arm symptoms have several treatments at their disposal. Often, a conservative course of “directional preference” therapy is chosen.
Directional preference refers to neck movements that, when performed repeatedly, result in centralization or alleviation of pain. Patients using directional preference therapy may be assigned home exercises as part of their treatment plan.
The authors found that compliance with these exercises, along with patient factors such as age ≥ 55 and noted improvement after initial treatment session, contributed significantly to success of therapy.
References:
Hoy DG, Protani M, De R, Buchbinder R.
The epidemiology of neck pain.
Best Pract Res Clin Rheumatol. 2010;24:783-92.Cohen S.
Epidemiology, diagnosis, and treatment of neck pain.
Mayo Clin Proc. 2015;90:284-99.Radhakrishnan K, Litchy WJ, O’Fallon WM, Kurland LT.
Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990.
Brain. 1994;117:325-35.Takasaki H, May S.
Mechanical diagnosis and therapy has similar effects on pain and disability as ‘wait and see’ and
other approaches in people with neck pain: a systematic review.
J Physiother. 2014;60:78-84.Gross A, Kay TM, Paquin JP, et al.
Exercises for mechanical neck disorders.
Cochrane Database Syst Rev. 2015;1:CD004250.Gebremariam L, Koes BW, Peul WC, Huisstede BM.
Evaluation of treatment effectiveness for the herniated cervical disc.
Spine. 2012;37:E109-18.May S, Gardiner E, Young S, Klaber-Moffett J.
Predictor variables for a positive long-term functional outcome in patients with acute and chronic neck
and back pain treated with a McKenzie approach: a secondary analysis.
J Man Manip Ther. 2008;16:155-60.Donelson R.
Mechanical diagnosis and therapy for radiculopathy.
Phys Med Rehabil Clin N Am. 2011;22:75-89.McKenzie R, May S.
The Cervical & Thoracic Spine: Mechanical Diagnosis & Therapy, Second Edition.
Waikanae, New Zealand: Spinal Publications New Zealand Ltd, 2006, p. 86.Rasmussen C, Rechter L, Schmidt I, Hansen VK, Therkelsen K.
The association of the involvement of financial compensation with the outcome of cervicobrachial pain
that is treated conservatively.
Rheumatology (Oxford). 2001;40:552-4.Moffett JK, Jackson DA, Gardiner ED, et al.
Randomized trial of two physiotherapy interventions for primary care neck and back pain patients:
‘McKenzie’ vs brief physiotherapy pain management.
Rheumatology (Oxford). 2006;45:1514-21.Kjellman G, Oberg B.
A randomised clinical trial comparing general exercise, McKenzie treatment and a control group
in patients with neck pain.
J Rehabil Med. 2002;34:183-90.Guzy G, Fra?czuk B, Kr?kowska A.
A clinical trial comparing the McKenzie method and a complex rehabilitation program in patients
with cervical derangement syndrome.
J Orthop Trauma Surg Rel Res. 2011;2:32-8.Kongsted A, Qerama E, Kasch H, et al.
Neck collar, “act-as-usual” or active mobilization for whiplash injury? A randomized parallel trial.
Spine (Phila Pa 1976). 2007;32:618-26.Rosenfeld M, Seferiadis A, Carlsson J, Gunnarsson R.
Active intervention in patients with whiplash-associated disorders improves long-term prognosis:
a randomized controlled clinical trial.
Spine. 2003;28:2491-8.Singh P, Gupta K.
Comparative study of a structured progressive exercise program and McKenzie protocol in individuals with
mechanical cervical spine pain.
Physiother Occup Ther J. 2012;5:11-7.Balkovec C, McGill S.
Extent of nucleus pulposus migration in the annulus of porcine intervertebral discs exposed to cyclic flexion
only versus cyclic flexion and extension.
Clin Biomech (Bristol, Avon). 2012;27:766-70.Takasaki H, May S, Fazey PJ, Hall T.
Nucleus pulposus deformation following application of mechanical diagnosis and therapy:
a single case report with magnetic resonance imaging.
J Man Manip Ther. 2010;18:153-8.Beattie PF, Arnot CF, Donley JW, Noda H, Bailey L.
The immediate reduction in low back pain intensity following lumbar joint mobilization and
prone press-ups is associated with increased diffusion of water in the L5-S1 intervertebral disc.
J Orthop Sports Phys Ther. 2010;40:256-64.Zou J, Yang H, Miyazaki M, et al.
Dynamic bulging of intervertebral discs in the degenerative lumbar spine.
Spine (Phila Pa 1976). 2009;34:2545-50.Tsantrizos A, Ito K, Aebi M, Steffen T.
Internal strains in healthy and degenerated lumbar intervertebral discs.
Spine (Phila Pa 1976). 2005;30:2129-37.Clare HA, Adams R, Maher CG.
Reliability of McKenzie classification of patients with cervical or lumbar pain.
J Manipulative Physiol Ther. 2005;28:122-7.Hefford C.
McKenzie classification of mechanical spinal pain: profile of syndromes and directions of preference.
Man Ther. 2008;13:75-81.Bolton JE, Humphreys BK.
The Bournemouth Questionnaire: a short-form comprehensive outcome measure.
II. Psychometric properties in neck pain patients.
J Manipulative Physiol Ther. 2002;25:141-8.Irgens P, Lothe LR, Kvammen OC, Field J, Newell D.
The psychometric profile of chiropractic patients in Norway and England: using and comparing the
generic versions of the STarT Back 5-item screening tool and the Bournemouth Questionnaire.
Chiropr Man Therap. 2013;21:41.Peterson C, Bolton J, Humphreys BK.
Predictors of Outcome in Neck Pain Patients Undergoing Chiropractic Care:
Comparison of Acute and Chronic Patients
Chiropractic & Manual Therapies 2012 (Aug 24); 20 (1): 27Gay RE, Madson TJ, Cieslak KR.
Comparison of the Neck Disability Index and the Neck Bournemouth Questionnaire in a sample of patients
with chronic uncomplicated neck pain.
J Manipulative Physiol Ther. 2007;30:259-62.Spanos G, Zounis M, Natsika M, May S.
The application of mechanical diagnosis and therapy and changes on MRI findings in a patient
with cervical radiculopathy.
Man Ther. 2013;18:606-10.Hurst H, Bolton J.
Assessing the clinical significance of change scores recorded on subjective outcome measures.
J Manipulative Physiol Ther. 2004;27:26-35.Toombs SK (ed).
Handbook of Phenomenology and Medicine.
Dordrecht, The Netherlands: Kluwer Academic Publishers, 2001, p. 379.
Return to McKENZIE METHOD
Return to CHRONIC NECK PAIN
Since 9–16–2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |