|
Today’s Chiropractic; Vol 27, No 5: 3247
Autism, Asthma, Irritable Bowel Syndrome, Strabismus, and Illness Susceptibility: A
Case Study in Chiropractic Management
William C. Amalu, DC, DABCT, DIACT, FIACT
ABSTRACT:
Pathologies of organic
origin are commonly thought to be the exclusive realm of medical treatment and not part of
the mainstay of chiropractic care. The clinical observations of a patient presenting with
autism, asthma, irritable bowel syndrome, strabismus, and illness susceptibility are
reported. Alleviation of symptoms is seen subsequent to corrections of abnormal
biomechanical function of the occipito-atlanto-axial complex. A relationship between
biomechanical faults in the upper cervical spine and the manifestation of abnormal central
neurophysiological processing is suggested as the genesis of this patient’s
symptomatology.
Key words: Autism, Asthma, IBS, Strabismus, Infrared Imaging, Upper Cervical Spine.
INTRODUCTION
Autism
usually manifests itself in the first year of life with onset rarely later than 30 months
of age. The cause of autism is unknown, but evidence points to a neurological basis. The
syndrome is characterized by extreme aloneness (lack of attachment, failure to cuddle, and
avoidance of eye contact); insistence on sameness (resistance to change, ritual morbid
attachment to familiar objects, and repetitive acts); disordered speech and language
(which varies from total muteness to markedly idiosyncratic use of language); and uneven
intellectual performance. The syndrome tends to maintain a consistent symptomatic picture
throughout development.
Medical treatment, for the
most severely impaired children, includes systematic application of behavior therapy; a
technique that can be taught to parents in order to help manage the child in the home and
at school. The benefits of this therapy vary widely, but may be considerable for these
children who try the patience of the most loving parents and devoted teachers. Medications
provide limited benefit and are used mainly in controlling the most severe forms of
aggressive and self-destructive behavior. However, they do not resolve the condition. [13]
Asthma is a lung disease
characterized by: airway obstruction that is reversible (but not completely in some
patients), airway inflammation, and increased airway responsiveness to a variety of
stimuli. The airway obstruction in asthma is due to a combination of factors that include:
smooth muscle spasm of the airways, edema of the airway mucosa, increased mucus secretion,
cellular infiltration of the airway walls, and injury and desquamation of the airway
epithelium. A family history of allergy or asthma can be elicited in most asthmatics.
Research on the
pathophysiology of asthma over the past decade has focused on the inflammatory cells and
their mediators, neurogenic mechanisms, and vascular abnormalities involved. Recent
interest in neurogenic mechanisms has focused on neuropeptides released from sensory
nerves by an axon reflex pathway. These peptides have vascular permeability and mucus
secretagogue activity, bronchoconstrictor activity, and a bronchial vascular dilation
effect. These sensory nerves also act on the pulmonary airways and their microvasculature
contributing to the special kind of airway inflammation that is characteristic of asthma.
The medical treatment of
asthma may be conveniently considered as management of the acute attack and day-to-day
therapy. Drug therapy focuses on the two main aspects of the disease: bronchospasm and
inflammation. Sympathomimetic medications cause bronchial smooth muscle relaxation as
their effects mimic those of the sympathetic nervous system. The inflammatory aspect is
managed with corticosteroids. While systemic corticosteroids are considered exceptionally
effective, they are reserved for more difficult episodes because of their potential for
serious adverse effects. [13]
Irritable bowel syndrome
(IBS) is characterized as a motility disorder involving the entire hollow GI tract,
creating an upper and lower GI symptom complex. The etiology of IBS is unknown. No
anatomic cause can be found. Two major groups or clinical types of IBS are recognized. In
the spastic colon type, most patients have pain over one or more areas of the colon
associated with periodic constipation or diarrhea. The second group of IBS patients
primarily manifest painless diarrhea, usually urgent, precipitous diarrhea that occurs
immediately upon rising or, more typically, during or immediately after a meal.
The pathophysiology of
IBS is based upon motor abnormalities of both the small and large bowel. When the normal
segmentation mechanism of the sigmoid colon becomes hyperreactive, so-called spastic
constipation results. In contrast, diminished motor function is found in the group
associated with diarrheal episodes. Treatment is basically supportive and palliative. If
offending foods can be identified, diet changes are suggested. Medical management with
drugs are used only as a temporary expedient to relieve spastic pain. [13]
Strabismus is
characterized as the deviation of one eye from parallelism with the other. The etiology is
either paralytic or myospasmotic. Paralytic (nonconcomitant) strabismus results from
paralysis of one or more ocular muscles and may be caused by a specific oculomotor nerve
lesion. Nonparalytic (concomitant) strabismus usually results from unequal ocular muscle
tone caused by a supranuclear abnormality within the CNS. A concomitant strabismus may be
convergent (esotropia), divergent (exotropia), or vertical (hyper- or hypotropia).
The focus of medical
treatment is for muscle imbalance. If this alone is responsible, strabismus is treated
early with corrective glasses or contact lenses, medications, orthoptic training (eg. eye
exercises, patching the normal eye, etc.), or surgical restoration of the muscle balance.
Permanent loss of vision can occur if strabismus and its attendant amblyopia are not
treated before the age of 4 to 6 yrs., with intermittent follow-up examinations at least
until age 10. [13]
Considering the above
pathophysiology and treatment approach to this patient’s conditions, it can be
understood that the contribution of chiropractic care in the management of these diseases
is considered to be of no significance to the medical community. However, the body of
literature detailing a possible upper cervical etiology, or at least contribution, is
substantial; and the case made for greater recognition of the involvement of abnormal
upper cervical spine biomechanics is compelling.
CASE REPORT
A 5 year old female was
referred to our clinic with the chief complaint of autism. Her parents advised that the
patient had also been diagnosed with asthma, allergies, irritable bowel syndrome, and left
sided strabismus. The patient’s diagnosis was made through an extensive medical
workup at a specialized autism research institute with the other conditions diagnosed over
time by various medical specialists.
Her mother reported that
she had been very susceptible to illnesses since birth, but had experienced normal
development until a viral upper respiratory illness at 21 months of age. The URI developed
into a complication with asthma necessitating a 5 day regimen of prednisone. The
patient’s mother advised that she was never the same and began to deteriorate from
that point on.
At the time of
consultation, the patient had been experiencing 25 violent temper episodes per day with
each episode lasting up to 20 minutes. The episodes consisted of ear piercing screams,
combatant behavior, and the patient throwing herself onto the floor. She also exhibited 3
episodes each day of self-inflicted violent behavior which included biting her arm,
slapping her head, and repeatedly banging her head against a full length mirror. Her
parents advised that she also expressed at least 1 episode each day of outward violent
behavior which consisted of hitting people, especially her mother to include slapping the
glasses off her face.
The patient’s speech
was limited to only a few words such as mama, dada, milk, and walk. Her fine motor skills
were delayed to the extent that she could only feed herself with her fingers. The
patient’s sleep pattern was considerably disturbed with waking screaming at least
twice at night and once with napping. It was also very difficult to get her back to sleep
once this occurred. The most difficult time was trying to get the patient to sleep in the
evening. Every night consisted of 11 1/2 hours of screaming, comforting, and stories just
to get her to sleep.
The irritable bowel
syndrome was described by her parents as profuse loose bowel movements which would occur 4
times a day with the need to change clothes. They were unable to correlate any food
sensitivities or pattern to the bowel movements. Due to her overall condition she was
unable to be toilet trained. Her parents also noted that she was allergic to dust and
plastics. She had constant eczema behind each ear along with rashes, redness, and sores
which could appear at random anywhere on her body.
Her parents noted that
she had continued to be very susceptible to illnesses. Out of 810 months per year, the
patient would experience a URI or flu lasting at least 3 weeks each time. Of these
illnesses, 50% would include asthma attacks necessitating the use of albuteral or a 5 day
regimen of prednisone. Occasionally, she would have to be taken for in-office nebulizer
treatment.
At the time the patient
was seen in our clinic, she had been undergoing various forms of home behavior therapies
along with attempted eye patching with limited results. Her parent’s noted that most
of her symptoms were getting worse in both intensity and frequency.
Upon examination, the
patient presented in constant motion with running on her toes while loosely flapping her
hands and arms. Her gait included a bilateral toe-in with a marked increase on the right.
She was uncommunicative, uncooperative, and prone to screaming violent outbursts. Vital
signs, ear, nose, and throat examinations were unremarkable with the exception of
bilateral posterior auricular eczema.
Orthopedic examination
revealed significant palpatory hypertonicity of the paraspinal musculature from the
occiput to C3 bilaterally with a marked increase on the right. A combination of screaming,
arched cervical extension, and outward violence suggested tenderness in the same areas.
The patient demonstrated a reduction in passive cervical extension and right lateral
flexion. Her lumbosacral evaluation was unremarkable.
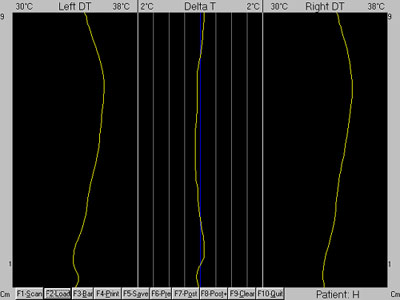
 Figure 1 |
Gross
neurologic examination was also found to be unremarkable. A moderate left
esotropia was noted along with a mild right. A paraspinal digital infrared
imaging analysis was performed in accordance with thermographic protocol. [46] Due to the patient’s violent behavior, she had to be restrained
by both parents and the doctor in order to take the scan. A continuous paraspinal
scan consisting of approximately 300 infrared samples was taken from the
level of S1 to the occiput (Fig. 1).
|
The data was analyzed against established normal values and found to contain
wide thermal asymmetries indicating abnormal autonomic regulation or neuropathophysiology [710] (Figs. 2 and 3).
Figure 2
|
Figure 3
|
Since the cervical spine displayed highly abnormal thermal asymmetries, a
focused scan was performed with approximately 75 infrared samples taken from T1 to the
occiput (Figs. 4 and 5).
Figure
4 |
Figure 5
|
The full
spine scans also displayed an abnormal central hypothermia of the spine, which suggests
long standing nervous system dysfunction (Figs. 2 and 6).
Figure
2 |
Figure 6
|
The above information yielded a high suspicion of abnormal upper cervical arthrokinematics.
Consequently, a precision upper cervical radiographic series was performed for
an accurate analysis of specific segmental biomechanics. [11] Since positioning
chairs and head clamps cannot be used with infants or uncooperative children,
supine table films were taken using an on-patient laser-optic alignment system
to precisely align the patient to the central ray. With this system, maintenance
of precision patient alignment can be facilitated without a head clamp system
due to the laser being aligned to the source of the X-ray beam rather than the
bucky. However, with children who are old enough to sit on their own, weight-bearing
laser-optic alignment is preferred (Figs. 7 and 8).
 Figure
7 |
 Figure 8 |
An analytical radiographic
method consisting of mensuration combined with arthrokinematics was performed. [11]
Biomechanical abnormalities were noted at the atlanto-occipital and atlanto-axial
articulations.
CHIROPRACTIC MANAGEMENT
Correction of the
atlanto-occipital subluxation was chosen as the first to be adjusted from the accumulated
degree of aberrant biomechanics noted at this level. Before treatment was rendered, the
parents were counseled that they may expect exacerbations in symptomatology as part of the
normal response to care due to the global impact of neural reintegration.
To correct the
subluxation, the patient was placed on a specially designed knee-chest table with the
posterior arch of atlas as the contact point. An adjusting force was introduced using a
specialized upper cervical adjusting procedure. [12] The patient was then placed in a
post-adjustment recuperation suite for 15 minutes as per thermographic protocol. [46]
Correction of the subluxation was determined from the post-adjustment cervical infrared
scan noting resolution of the patient’s presenting neuropathophysiology (Figs. 9 and
10).
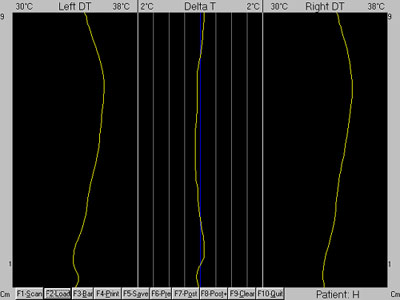
Figure 9 |
Figure 10
|
All subsequent office visits included an
initial cervical infrared scan; and if care was rendered, another scan was performed to
determine if normal neurophysiology was restored. Since the focus of the patient’s
care was in the upper cervical spine, infrared scans were made in this region only during
normal treatment visits with full spine scans performed at 30day re-evaluation intervals.
The patient was adjusted
twice during the first week of care. After the first adjustment, the patient’s mother
noted that she had her first good night sleep since she could remember. By the end of the
week, she reported that the patient’s violent temper episodes had reduced to 15 per
day along with a substantial decreased in intensity. She noted that reasoning with the
patient could stop them now. The patient’s self-inflicted violent behavior was also
decreasing in frequency. Her speech had suddenly improved with an increase in vocabulary
with the ability to expressing feelings (saying hungry, tired, mad). Her sleep pattern
also changed to waking only once at night along with longer napping times. The
patient’s mother reported that she was running less and walking more flat footed.
Performing thermal scans had also become much easier as she was now able to sit on her own
without restraint.
During the second week of
care the patient was adjusted only once. Her mother reported that by the end of the week
the temper episodes had decreased to only 5 per day with a further decrease in intensity.
She also noted that she was able to stop them quickly. The patient’s left strabismus
had improved to the point that her mother noticed it only twice since the week before. She
advised that the right eye showed no signs of strabismus since treatment began. The
patient’s mother was elated to report that she had been increasingly vocal this week
and began speaking in sentences for the first time. She was also able to nap now without
waking and woke only once per night this week with the ability to go back to sleep on her
own. Her toe in gait continued to decrease with more flat-footed walking. Her mother
reported a marked decrease in hyperactivity along with wanting to be touched and hugged
now.
The patient was adjusted
once during the third week of care. By the end of the week, the patient’s violent
temper episodes had decreased to only twice per day with a continued decrease in
intensity. Her mother noted that she continued to speak using more sentences and
vocalizing disappointment, anger, hunger, tiredness, and other feelings. The
patient’s strabismus was now showing up in the left eye only when tired. Her gait was
absent of toe-in by this time. Her mother advised that there was very little running or
hyperactivity now. She had also ceased to display any self or outward violent behavior.
The patient’s mother also noted that her IBS had improved to the point of 12 loose
bowel movements per day with only an occasional need to change clothes. She noted that the
patient was now beginning to recognize bowel and bladder functions on her own. Because she
was doing so well, they decided to go to a friend’s house as a family for the first
time. The patient’s social behavior was excellent; she played with their dog, used
the stairs without falling, and came home and asked to go to bed because she was tired.
No adjustments were
necessary during the fourth week of care. The patient’s mother reported that by the
end of this week all temper episodes, hyperactivity, self and outward violent behavior had
stopped. She was now napping and sleeping through the night perfectly. The patient was
also walking more and more, running less, and showed no signs of toe-in. Her mother
advised that there were no signs of any strabismus by this time. The IBS continued to
improve with only one loose bowel movement per day at the most and only a rare clothing
change. Her mother also noted that the eczema behind her ears had cleared up and that her
allergic skin reactions had stopped.
Before entering our clinic
for care, an appointment had been made at a special autism, occupational therapy, and
speech center to evaluate the patient for specialized therapy. Her parents decided to keep
the appointment due to the difficulty in getting one in the first place and to see what if
anything could further the patient’s development. The patient underwent one hour of
observation and evaluation by two therapists. Upon conferring their findings they both
reported that the patient did not have autism and that there must have been a
misdiagnosis. The patient’s mother was pleasantly amused and elated by this and
proceeded to explain in detail the patient’s behavior four weeks previously. Upon
hearing this, the therapists agreed that the original diagnosis was autism, but that the
patient was not currently exhibiting this disorder. They reported that due to her current
level of behavior that she would not need in-center therapy and that they would give the
parents work for her to do at home. Their report also noted that at her current rate of
improvement she would be able to function in society.
A re-evaluation was also
performed in our center at this time. The examination revealed: no signs of posterior
auricular eczema, normal cervical muscle tone, cervical PROMs WNL, lack of toe-in gait,
and bilateral central positioning of the eyes. A full spine paraspinal infrared scan was
performed at this time noting near total resolution of the patient’s presenting
neuropathophysiology along with a return of normal central spinal heat (Figs. 11, 12, and
13).
Figure
11 |
Figure 12
|
Figure 13
Having the patient in the
office had become a pleasure by now. She would hold my hand while walking down the hall,
position herself with her back to the examining chair while allowing me to lift her up to
sit, and finally holding her own hair out of the way for me to perform an infrared scan.
Weeks six and eight were
punctuated by a mild return of symptoms. The patient’s mother advised that the temper
episodes had returned at approximately once per day along with her left strabismus, but
that both were very mild in intensity. Concomitantly, her infrared scans noted a return of
her presenting neuropathophysiology necessitating an adjustment once during each week. All
of her other conditions continued to improve at a steady rate. Her mother reported that
she was climbing, exploring, and doing things she would never do before. A re-examination
was performed at eight weeks with no remarkable findings.
Figure 14 |
No
adjustments were needed during the ninth through twelfth weeks of care.
The patient’s mother continued to report improvements with no temper
episodes, self or outward violent behavior, or strabismus (Fig. 14). Her
sleeping habits remained undisturbed. The patient’s hyperactivity continued
to decrease along with an increased frequency of a heel-toe gait. Her speech
continued to improve with more and more sentence use. The IBS had almost
completely resolved with no episodes needing a change of clothes. |
The patient continued to
improve over the next 8 months. Adjustments were rendered very infrequently. Her mother
reports that the patient currently exhibits the type of anger in intensity and frequency
that normal children have when not getting their way, etc. The patient may rarely show
some self-violent behavior with slapping her own head if she is over stimulated or very
tired. Any outward violent behavior, if ever seen, is described by her mother as usual
childhood behavior as when mad with a sibling. Her sleep pattern continues to be
undisturbed. She continues to improve in her speech development with increased use of
complex structured sentences. Her gross motor skills have improved to the point of
performing somersaults and playing catch, while her fine motor skills include work with
holding pencils correctly, using keys, and the ability to feed herself (even soup) using
utensils.
Her IBS has almost
completely resolved with possibly one loose bowel movement a week with no clothing
changes. To her mother’s delight she is now toilet training. Her left strabismus is a
rare occurrence, hardly noticeable, and only when she is extremely tired. The
patient’s mother reports that her allergies and eczema never returned. She has also
never had another asthma attack. Over the past eleven months of care, the patient has
experienced only three minor colds lasting at the most five days. Considering the amount
of developmental delay, learning disabilities, and immune dysfunction seen in this
patient, it is amazing how much progress she made in such a short amount of time. However,
even though improvements continue day-by-day, she still has a long way to go.
NEUROBIOLOGICAL MECHANISMS
There are two extensively
studied neurophysiological mechanisms which may explain the profound changes seen in this
patient. The first is CNS facilitation. [1317] This condition arises from an initiating
trauma (birth, falling, etc.) which causes entrapment of intra-articular meniscoids
resulting in segmental hypomobility and finally compensatory hypermobility. Consequently,
hyperexcitation of intra and periarticular mechanoreceptors and nociceptors occurs. Over
time, this bombardment of the central nervous system can cause facilitation. Facilitation
results in an exponential rise in afferent signals to the cord and/or brain. This may
cause a loss of central neural integration due to direct excitation, or a lack of normal
inhibition, of pathways or nuclei at the level of the cord, brainstem, and/or higher brain
centers. The upper cervical spine is uniquely suited to this condition as it possesses
inherently poor biomechanical stability along with the greatest concentration of spinal
mechanoreceptors.
The second mechanism is
cerebral penumbra or brain cell hibernation. [1824] Previous research held that the
neuron had two basic states of existence: function and dysfunction. However, a third state
was uncovered which may explain the rapid and profound changes seen in some cases. When a
certain threshold of ischemia is reached, the neuronal state of hibernation occurs; the
cell remains alive, but ceases to perform its designated purpose. Entire functional areas
of the cerebral cortex or cerebellum may be affected. The mechanism of hyperafferancy, as
mentioned above, plays an initiating role. Hyperafferant activation of the central
regulating center for sympathetic function in the brain may cause differing levels of
cerebral ischemia. A second route via the superior cervical sympathetic ganglia, may also
cause higher center ischemia.
These recent advances in
neurophysiological research correlate well with the pathophysiology currently proposed in
the presented conditions. [13] Normalization of frontal lobe and limbic system
physiology would account for this patient’s drastic personality and behavior changes. [13]
Cerebral penumbra may hold the greatest explanation for the changes seen in autism
with specialized upper cervical chiropractic care.
Since recent research has
elucidated neurogenic mechanisms which cause bronchoconstriction, mucus secretion, and
airway inflammation in asthmatics [13]
, normalization of neural function could correct
the condition. In the treatment of asthma, sympathomimetic drugs are used to mimic the
normal activity of the sympathetic system. [13]
Why not return function to this system
rather than prescribing drugs that mimic it. Normalization of pathological central
sympathetic regulation due to cerebral penumbra, and/or direct pathophysiological spinal
pathway integration to the bronchial tree, may explain our effects.
In the case of strabismus,
supranuclear abnormalities within the CNS or direct occulomotor nerve dysfunction can
cause unequal ocular muscle tone. [13]
Correction of cerebral penumbra and/or facilitated
pathways could explain the return of normal central ocular positioning in this patient.
Motor nerve abnormalities
which cause the bowel motility dysfunction seen in irritable bowel syndrome [13]
, may
arise from either pathologies of central motor regulation due to cerebral penumbra or loss
of direct pathway controls. Normalization of motor nerve function would cause a return of
regular bowel motility.
The role that the
sympathetic nervous system plays in the regulation of immune function is substantial. [13]
Dysregulation of this system can result in sympathetically mediated immune
dysfunction and thus, susceptibility to illnesses. Correction of pathological central
sympathetic regulation resulting from cerebral penumbra and/or facilitation would lead to
a return of normal immune function.
CONCLUSION
The most important factor
in this case was our ability to objectively monitor the adjustment’s affects on the
patient’s neurophysiology. Many different types of tests are used in our profession
such as leg length, cervical challenge, motion and static palpation, and others. However,
these tests lack objectivity, posses inherent errors, and have no literature confirmation
of their ability to monitor neurophysiology. [2528] Digital infrared imaging, however,
has been researched for over 30 years compiling almost 9,000 peer-reviewed and indexed
articles confirming its use as an objective measure of neurophysiology. By using this
technology, our clinic has been able to consistently determine the correct adjustive
procedures that produce reproducible and dramatic positive neurophysiological improvements
in our patients.
If the foundation of our
profession stands on the principle that homeostasis is dependent upon coordinated
neurophysiology, then we must directly and objectively monitor this system as an outcome
measure to our care. But not any way of monitoring this system will suffice. We need to
measure the autonomic nervous system if we are to monitor the global systemic aspect of
the nervous system’s control. Paraspinal digital infrared imaging fulfills this need
by objectively measuring the autonomic changes of all 32 spinal nerves as they exit to
effect deep visceral function. Since testing does not involve patient compliance, such as
movement or a verbal response, paraspinal infrared imaging becomes as objective a test of
neurophysiology as we can get.
To what magnitude the
upper cervical spine is involved in the genesis of organic conditions remains to be seen.
In an atmosphere where much of the public see our profession as useful for neck and back
pain treatment at most, patients with complex disorders are left unaware of the possible
benefits of care. The body of literature detailing a possible upper cervical etiology, or
at least contribution, to organic disorders is substantial. Further research into this
area of the spine, combined with objective monitoring of neurophysiology, may reveal that
chiropractic does indeed offer consistent conservative management of complex visceral
disorders.
ACKNOWLEDGMENTS:
The
authors would like to gratefully acknowledge the Titronics Corporation.
For without their design of the TyTron C-3000 Paraspinal Digital Infrared
Scanner, we would not have been able to monitor this patient’s neurophysiology.
REFERENCES:
1.) Schroeder, S., Krupp, M., Tierney, L.
Current
Medical Diagnosis and Treatment.
Norwalk, CT: Appleton & Lang; 1988.
2.) Berkow, R., Beers, M., et al.
Manual of Diagnosis
and Therapy.
Merk & Co.; 16th ed. 1992.
3.) Andreoli, T., Carpenter, C., Plum, F.
Essentials
of Medicine. 2nd ed.
Philadelphia: W.B. Saunders; 1990.
4.) Thermography Protocols -
International Thermographic Society
1997.
5.) Thermography Protocols -
American Academy of Thermology 1984.
6.) Thermography Protocols -
American Academy of Medical Infrared Imaging 1997.
7.) Uematsu, S., Edwin, D., et al.
Quantification of Thermal Asymmetry. Part 1:
Normal Values and Reproducibility.
J Neurosurg 1988;69:552-555.
8.) Feldman, F., Nickoloff, E.
Normal Thermographic Standards in the Cervical Spine and Upper Extremities.
Skeletal Radiol 1984;12:235-249.
9.) Clark RP.
Human Skin Temperature and its Relevance
in Physiology and Clinical Assessment.
In: Francis E, Ring J, Phillips B, et al,
Recent Advances in Medical Thermology,
New York: Plenum Press, 1984:5-15.
10.) Uematsu S.
Symmetry of Skin Temperature Comparing One Side of
the Body to the Other.
Thermology 1985;1:4-7.
11.) Amalu, W., Tiscareno, L., et al.
Precision
Radiology: Module 1 and 5 -- Applied Upper Cervical Biomechanics Course.
International Upper Cervical Chiropractic Association, 1993.
12.) Amalu, W., Tiscareno, L., et al.
Precision Multivector Adjusting: Module 3 and 7 --
Applied Upper Cervical Biomechanics Course.
International Upper Cervical Chiropractic Association, 1993.
13.) Gardner, E.
Pathways to the Cerebral Cortex for Nerve Impulses from Joints.
Acta Anat 1969;56:203-216.
14.) Wyke, B.
The Neurology of Joints: A Review of General Principles.
Clin Rheum Dis 1981;7:223-239.
15.) Coote, J.
Somatic Sources of Afferent Input as Factors
in Aberrant Autonomic, Sensory, and Motor Function.
In: Korr, I., ed. The Neurobiologic Mechanisms in Manipulative Therapy.
New York: Plenum, 1978:91-127.
16.) Denslow, J., Korr, I., Krems, A.
Quantitative Studies of Chronic Facilitation in Human Motorneuron Pools.
Am J Physiol 1987;150:229-238
17.) Korr, I.
Proprioceptors and the Behavior of Lesioned Segments.
In: Stark, E. ed. Osteopathic Medicine.
Acton, Mass.: Publication Sciences Group, 1975:183-199.
18.) Heiss, W., Hayakawa, T., Waltz, A.,
Cortical Neuronal Function During Ischeamia.
Arch Neurol 1976;33:813-20
19.) Astrup, J., Siesjo, B., Symon, L.
Thresholds in Cerebral Ischemia -- The Ischemic Penumbra.
Stroke 1981;12:723-5
20.) Roski, R., Spetzler, R., Owen, M., et al.
Reversal of Seven Year Old Visual Field Defect
with Extracranial-Intracranial Anastomosis.
Surg Neurol 1978;10:267-8
21.) Mathew, R., Meyer, J., et al.
Cerebral Blood Flow in Depression.
Lancet 1980;1(818):1308
22.) Mathew, R., Weinmann, M., Barr, D.
Personality and Regional Cerebral Blood Flow.
Br J Psychiatry 1984;144:529-32
23.) Jacques, S. Garner, J.
Reversal of Aphasia with Superficial Temporal Artery
to Middle Cerebral Artery Anastomosis.
Surg Neurol
1976;5:143-5
24.) Lee, M., Ausman, J., et al.
Superficial Temporal to Middle Cerebral Artery Anastomosis.
Clinical Outcome in Patients with Ischemia of Infarction
in Internal Carotid Artery Distribution.
Arch Neurol 1979;36:1-4
25.) DeBoer, K., Harmon, R., et al.
Inter- and Intra-examiner Reliability of Leg Length
Differential Measurement: A Preliminary Study.
J Manipulative Physiol Therap 1983;6:61-66
26.) Falltrick, D., Pierson, S.
Precise Measurement of Functional Leg Length Inequality and Changes
Due To Cervical Spine Rotation in Pain-Free Students.
J Manipulative Physiol Therap 1989;12:364-368
27.) Keating, J.
Inter-examiner Reliability of Motion Palpation of the
Lumbar Spine: A Review of Quantitative Literature.
Am J Chiro Med
1989;2:107-110
28.) Nansel, D., Peneff, A., Jansen, R., et al.
Interexaminer Concordance in Detecting Joint-Play Asymmetries
in the Cervical Spines of Otherwise Asymptomatic Subjects.
J Manipulative Physiol Therap 1989;12:428-433

Return to AUTISM
|