

Chiropractic Management of a Patient With
Breast Cancer Metastases to the Brain
and Spine: A Case ReportThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Can Chiropr Assoc 2015 (Sep); 59 (3): 269–278 ~ FULL TEXT
OPEN ACCESS Ismat Kanga, BSc, DC, FCCS(C) 1 and Igor Steiman, MSc, DC, FCCS(C) 2
1 Private Practice,
Mumbai, India.
2 Professor, Division of Undergraduate Studies,
Canadian Memorial Chiropractic College,
Toronto, OntarioCancers of the breast, kidney, lungs, prostate and thyroid metastasize to the musculoskeletal system in the majority of patients with malignancy. This report chronicles the case of a 65-year-old female with a known history of breast cancer who presented to a chiropractic clinic. Once metastasis was ruled out as the cause of her complaint, the patient was treated with manual therapies and exercises. As the patient's treatments progressed and her pain improved, she presented with a new complaint of 'pressure' in her head. Advanced imaging revealed metastasis to the brain and subsequently to the spine. The aim of this case is to heighten awareness of the presentation of metastasis to the brain and the spine in a chiropractic patient, and to demonstrate the benefit of chiropractic care in the management of such patients.
KEYWORDS: brain metastases; breast cancer; chiropractic; chiropractic care; spinal metastases
From the FULL TEXT Article:
Introduction
Tumours of the breast, lung, kidney, prostate and thyroid metastasize to the skeletal system in approximately 70% of cancer patients. [1] With newer developments in cancer treatments, incidence of metastases to the spine and other organs such as lungs, liver and brain is increasing along with survival. [2] Patients with a history of cancer often present to chiropractic clinics with neuromusculoskeletal symptoms. A survey of patients with early stage breast cancer found that 28.1% of patients seek alternative medicine along with their standard therapy, including acupuncture, chiropractic and massage therapy. [3] Twelve to twenty percent of patients present with back pain or headaches, often as the initial presentation of symptomatic spinal metastasis. [2, 4]
This case report describes the chiropractic management of a patient with a known history of breast cancer, which metastasized. The patient presented to the clinic with pain in the neck and low back, and with a history of breast cancer with metastasis to the lungs. As the patient’s cancer progressed she then developed metastasis to the liver, brain and spine. This case report highlights metastases to the spine, and describes their clinical presentation and concurrent chiropractic management; and metastasis to the central nervous system, which may manifest as headaches, a symptom commonly presented at chiropractic practices.
Case
A 65-year-old female was referred by her family physician to a chiropractic clinic for acute low back pain (LBP), but presented to the chiropractor with a chief complaint of neck and mid-back pain. The pain in her cervicothoracic (C/T) region started insidiously two days prior, when she noticed a sharp pain in her neck and numbness and tingling in both hands. The patient also complained of LBP that she had experienced for the last 25 years; the recent acute episode, caused by coughing and pulling a suitcase, which had triggered the referral had resolved within days since the referral was initiated.
She rated the intensity of her neck pain as 9 out of 10 (0 representing no pain at all and 10 representing the worst pain ever felt). The patient scored 44% on the Oswestry Disability Index, indicating severe disability, and 18 out of 50 on the Neck Disability Index, indicating moderate disability. Movement and recumbency were aggravating factors for her C/T pain, but no relieving factors were identified. Advil and swimming attenuated her LBP. Inquiry about current red flags revealed that she experienced no night sweats, fever or chills, headaches, dizziness, dysphagia, or significant change in weight. However, she did experience unrelenting C/T pain that woke her up at night, and had a previous history of cancer.

Table 1 Her family history was significant for multiple myeloma and Parkinson’s disease in her mother, lung cancer in her father and pancreatic cancer in an aunt. Her medical history was significant for osteoporosis since 2008, irritable bowel syndrome, benign paroxysmal positional vertigo, and breast cancer, for which she had received and was again receiving chemotherapy. The timeline related to her past medical history is outlined in Table 1.
Examination revealed a frail woman in moderate distress. Active, passive and resisted ranges of motion of the cervical spine were moderately restricted and painful in flexion, lateral flexion and rotation. Extension of the cervical spine was markedly limited due to elicitation of severe C/T pain. Cervical Kemp’s (compression, extension and rotation), Jackson’s (cervical rotation plus compression), Spurling’s (cervical lateral flexion and compression) and thoracic outlet tests created some local pain but did not elicit upper extremity symptoms. Valsalva maneuver caused some increased pain in her cervicothoracic region. Spinous percussion was unremarkable. The Soto-Hall test (passive head and neck flexion with stabilization of the sternum of the supine patient) exacerbated her neck pain.
Palpation revealed tenderness in the rhomboid, trapezius and C/T paraspinal musculature, bilaterally. Joint mobility restrictions were also found on palpation at C4–C5, C7-T1 and T3–T4 levels. Sensory examination revealed intact light touch in the upper extremities. Motor testing revealed generalized weakness graded 4/5 that could be attributed to previous and ongoing chemotherapy. [5] Deep tendon reflexes (biceps, brachioradialis and triceps) were 1+ bilaterally, and Hoffman’s sign was absent.
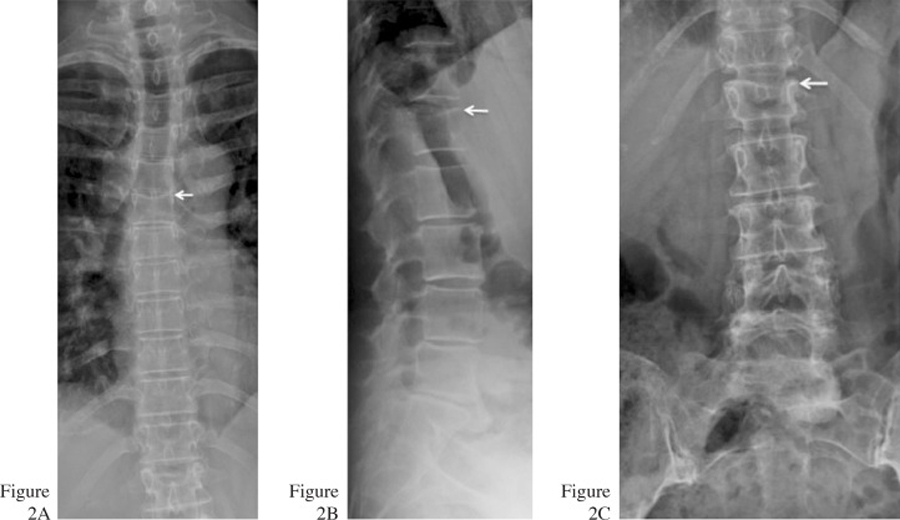
In patients with a history of cancer and new onset of pain, a diagnosis of metastasis should be considered until ruled out. In order to rule out more serious pathologies such metastasis to the spine and compression fracture, the patient was referred for full spine radiographs. The radiographs revealed moderate disc space narrowing from C5 – C7 and L4 – S1, mild disc space narrowing from L2 – L4 and minimal facet joint sclerosis at C2 – C3 (Figures 1A and 1B). There were old endplate compression fractures noted at T6 and L1 (Figures 2A–C). The patient was also sent for a bone scan by her family doctor, which showed no metastasis to the spine.
Figure 1. Lateral (A) and lower AP (B) cervical radiographs reveal
moderate disc space narrowing at C5–C6 and C6–C7 with
uncovertebral arthrosis. Mild facet arthrosis visualized from C2 – C4.
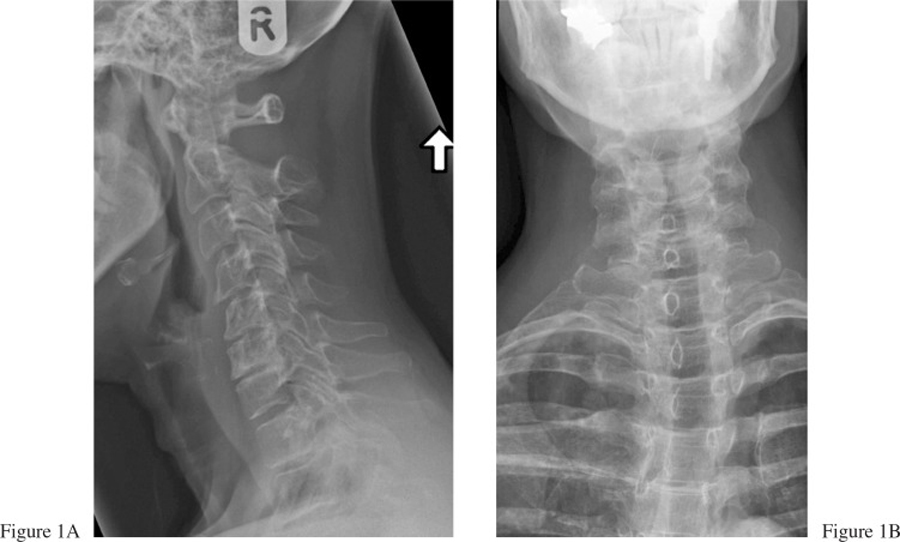
Figure 2. AP thoracic (A) radiograph reveals the old compression fracture
at T6. Lateral (B) and AP (C) lumbar radiographs demonstrate the old
compression fracture at L1 (arrows). Mild (L2–L3), moderate (L4–L5)
and marked (L5-S1) disc degeneration is evident.
The patient was diagnosed with and treated for cervicothoracic and lumbopelvic strains. Since clinical examination could not reproduce the paresthesias in the hands, this symptom was considered to possibly arise from chemotherapy or an undetected thoracic outlet syndrome. Chemotherapy-induced peripheral neuropathy is present in up to 40% of patients receiving chemotherapy, commonly presenting as paresthesia and dysesthesia in the fingers and toes.5
The patient was treated nine times over the span of a month. Her treatments included soft tissue therapy, mobilization, cryotherapy, heat and rehabilitative exercises. Rehabilitative exercises included neck range of motion, stretches and isometric exercises; low back and hip stretches, “bird dog” and plank exercises were prescribed for her low back (hold 10 seconds, repeat five times). As there was no metastasis to the spine, confirmed with radiographs and the bone scan, the patient was also offered spinal manipulation for her neck pain and mobilization for her lumbar spine. In providing informed consent for treatment, the patient stated that she might consider spinal manipulation in the future, if the soft tissue therapy and mobilization were ineffective. Acknowledging the patient’s preference and apprehension in receiving spinal manipulation, the practitioner employed a patient-centred approach and abstained from manipulation. Within a few treatments the patient’s C/T pain resolved, while her LBP persisted. (At the third visit, the patient reported that since resuming chemotherapy in November 2011, she had constant paresthesiae in toes 1 – 4 bilaterally. The symptom was reproduced then with Tinel’s test at the tarsal tunnel, bilaterally.)
On a scheduled visit for her LBP (for which she was considering receiving spinal manipulation, having had this option recommended by her family physician over taking prednisone) a month after her initial visit, the patient presented with a complaint of significant “pressure” in her head. She had also been experiencing difficulty balancing, and was observed to have an abnormal gait. During treatment she had difficulty maintaining a prone position, feeling increased pressure in her head with forward flexion. A letter documenting the unusual increase in severity of her headache, abnormal gait and difficulty tolerating the prone position was sent to her family physician, who noted she also had difficulty with reading, and had developed urinary urgency.
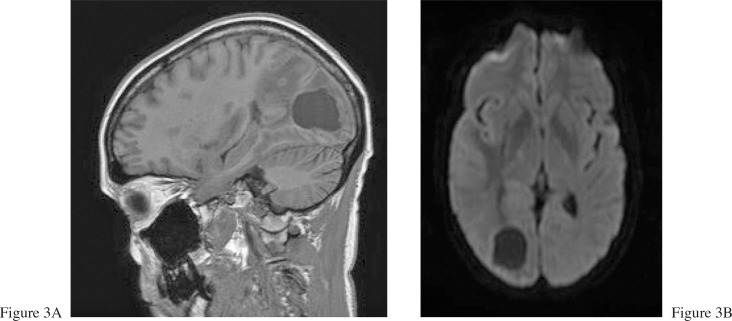
The patient was subsequently referred for magnetic resonance imaging (MRI) that revealed that the Stage 4 breast cancer had further metastasized to her lungs, liver and brain (Figures 3A and 3B). The patient commenced a course of whole brain radiotherapy and decided to temporarily refrain from chiropractic treatment.
Figure 3. Sagittal (A) and axial (B) T1-weighted images following
intravenous injection with gadolinium demonstrate a large intra-axial
mass located in the right occipital lobe.
A few weeks later the patient experienced a significant increase in her LBP. She was referred for radiographs by her family physician, which revealed new pathologic compression fracture of the T9 vertebral body and old osteoporotic compression fractures at T6 and L1 (Figures 4 and 5). The patient was referred to an orthopedic surgeon and underwent kyphoplasties at the levels of T9 and L1, after which she experienced significant reduction in the intensity of her back pain.
Figure 4. AP thoracic radiograph reveals a new compression fracture at T9 (arrow).
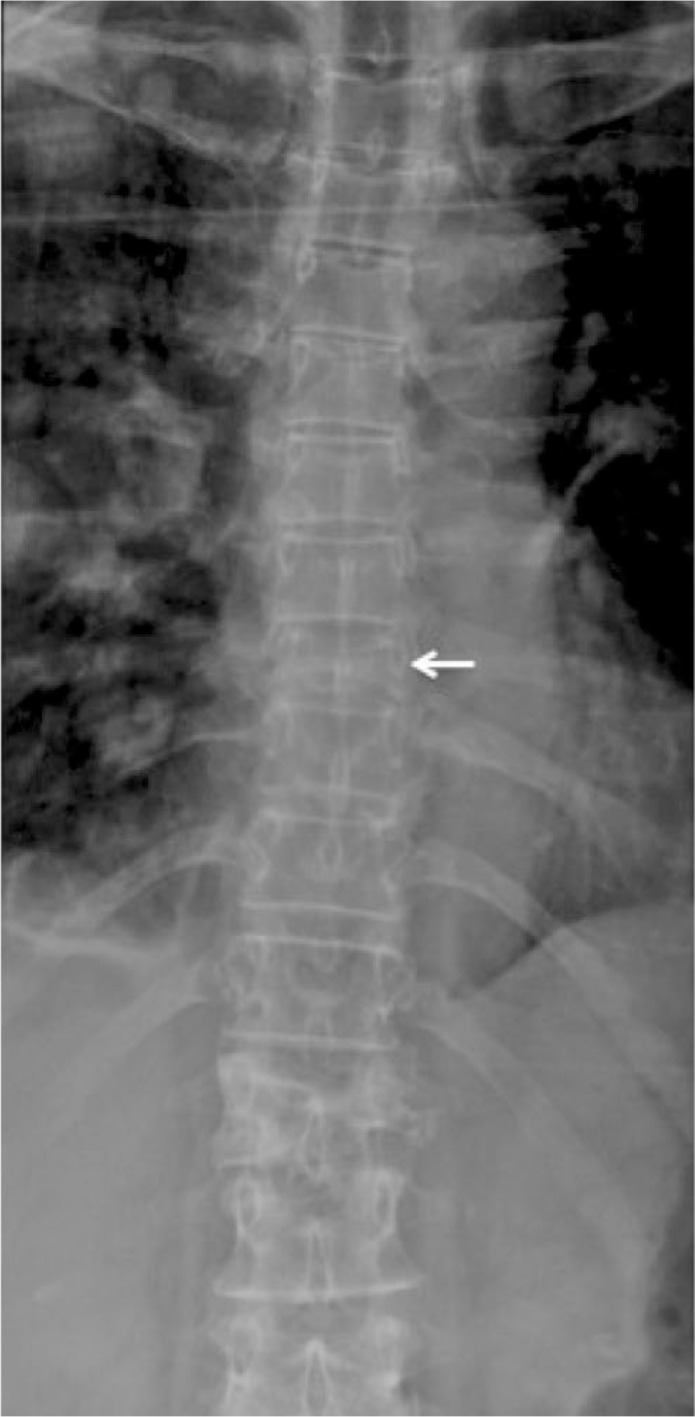
Figure 5. Axial computed tomography (CT) reveals a burst component to the
compression fracture with projection into the spinal canal.

In June 2012, chest x-rays revealed progressive meta-static disease. The patient became anorexic. Follow-up of the patient a few months later revealed she had moved to a hospice for palliative care.
Discussion
Breast cancer is the most common malignancy afflicting women in North America and is one of the leading causes of cancer-related death in women. [6, 7] Risk factors for breast cancer include a positive family history, older age, younger age at menarche and older age at menopause. [6, 7] The incidence increases until the age of 50 and in individuals with a family history of breast cancer (particularly in first-degree relatives). [6] Childbearing increases the risk of cancer soon after birth, but the risk then diminishes such that childbirth confers protection. [7] Other risk factors are oral contraceptive use and hormonal therapy for menopause. [7]
The patient in our case presented to the chiropractic clinic with a new onset of neck pain, chronic LBP and a known history of breast cancer. Therefore, the priority for our patient was ruling out metastasis to the spine. The patient was sent for radiographs and a bone scan, which ruled out skeletal metastasis. A few weeks into her treatment plan, the patient’s neck pain had subsided, but she still had complained of chronic LBP.
On a routine subsequent visit, she complained of a ”pressure” in her head. She also had trouble balancing and found her gait altered. She was sent for a brain MRI that revealed metastasis to the brain, which occurs in 10–16% of patients with stage IV breast cancer, arising within the parenchyma or the leptomeninges. [8] The latency between diagnosis of breast cancer and metastasis to the central nervous system (CNS) is two to three years. In the majority of cases, metastasis to the CNS occurs after spread to the liver, lung and bones, generally in the late stage of breast cancer. [8]
The most common presenting symptom of a parenchymal metastasis, headache (which our patient developed), occurs in up to 48% of patients. Headaches associated with intracranial masses may be described as a dull ache, pressure or throbbing. [9] The headaches do not occur daily, vary from moderate to severe intensity, and are frequently accompanied by nausea, papilledema, blurred vision and neurological deficits.9,10 Only a small percentage of patients present with more ominous headache characteristics such as morning or nocturnal incidence, worsening pain with Valsalva maneuver, and change in presentation of pre-existing headaches. [9, 10] Patients also frequently present with altered mental status, cognitive disturbances, motor deficits, seizures, ataxia, nausea and vomiting. [8, 11] Magnetic resonance imaging with gadolinium is the most sensitive test to diagnose metastasis to the CNS. [8]
Metastasis to the CNS generally occurs in the late stage of breast cancer. The prognosis for patients with CNS metastasis is poor, with the mean survival time varying from two to 16 months. The one-year survival rate of these patients is 20%. [8, 11] Treatments for patients with CNS metastasis include corticosteroids to decrease cerebral edema, whole brain radiotherapy, surgery and chemotherapy. [8]
The patient in our case developed spinal metastasis after metastasis to the CNS. Tumours metastasize to the spine via the arterial system, Batson’s venous plexus, or cerebrospinal fluid, or by direct extension from a paraspinal tumour. [12] Bone is a preferred site for metastasis as it is highly vascularized and rich in growth factors. [13] Spinal metastasis most commonly occurs in patients aged 40 – 65 years. Though the lumbar spine is the most commonly involved region of the spine, metastasis is most symptomatic when it occurs in the thoracic spine. [12] Metastasis to the spine can cause significant morbidity, pain, restricted motion, pathological fractures, compression of the spinal cord and hypercalcemia. [14]
Bone pain is one of the earliest symptoms, occurring in 90% of patients with spinal metastasis.4,12 It is poorly localized, insidious in onset and progressive in nature. [4, 14] The pain is characterized as a deep boring pain that awakens the patient at night or in the early morning, and which may improve with activity during the day. The pain can be caused as a result of release of inflammatory mediators, stretching the periosteum of the vertebral body, reactive muscle spasm and microfractures. [4, 14-16] In contrast to patients with typical mechanical pain, cancer related pain is not aggravated by activity and may occur at rest. [4] Patients may also present with paraspinal muscle spasms and altered biomechanics. [14, 17]
Metastasis results in a reduction in load-bearing capabilities by causing pathological trabecular microfractures and loss of structural integrity. [14] The most common fractures in these patients are vertebral compression fractures and rib fractures. [14] Neurological compression most commonly occurs in the thoracic spine and arises as a result of cord compression from the tumour, retropulsion from pathological vertebral body fracture fragments, or intradural metastasis. [4]
When patients present to a chiropractor, a thorough history and physical examination help discern whether the symptoms are of pathological or mechanical origin. [12] During the patient’s history, practitioners should aim to rule out ”red flags” that often suggest a more serious underlying pathology. Patients who present with constant progressive pain, past medical history of malignancy, unexplained weight loss, or nocturnal symptoms should raise suspicion of malignancy. [18] During the physical examination, practitioners should look for midline tenderness at affected levels during spinous percussion and palpation, and neurological deficits including numbness, weakness and pathological reflexes. [12]
Diagnostic imaging is required to confirm the diagnosis of skeletal metastasis. On plain radiographs, metastatic lesions are classified as osteolytic, osteoblastic or combined osteolytic and osteoblastic.4 At least 50% destruction of bone is required before the lesion is visible on a plain radiograph, which makes it hard to detect metastasis radiographically early in the course of the disease. [4] Destruction of the pedicle, displacement of paraspinal shadows, and compression fracture are common radiographic findings. [12]
Bone scans, capable of detecting lesions with 3% – 5% of bone loss, are more sensitive in detecting metastases, up to 18 months before radiographs. [2, 15, 17] They are also advantageous as they are able to scan the entire body at the same time in search of metastases throughout the axial and appendicular skeleton. Bone scans are not specific in differentiating lesions from compression fractures, infections or degenerative changes, requiring supplementation with other imaging.
Magnetic resonance imaging is the most sensitive and specific imaging modality in detecting metastasis and is considered the gold standard. [2, 15] Magnetic resonance imaging is important to differentiate osteoporotic compression fractures from pathological fractures; both commonly occur in cancer patients, [15] in whom skeletal metastasis can cause significant morbidity and mortality. [14] The prognosis for patients with skeletal metastasis is poor, with only 20% of patients surviving five years after diagnosis. [13]
Patients with cancer may present with tumour-related pain and with various musculoskeletal dysfunctions. [15] Cancer patients may receive radiation therapy, which can cause fibrosis of normal tissue, resulting in restricted and painful ranges of motion. [19] Patients may also present with pain related to joint dysfunction due to long periods of immobilization in the hospital and during recovery. Furthermore, pathologic compression fractures result in severe pain causing patients to alter the way they sleep; e.g., patients with a kyphotic deformity may sleep upright for many weeks until the pain subsides, as lying supine may aggravate their pain. [15] Unfortunately, pathology does not exempt patients from quotidian musculoskeletal dysfunction.
Medical treatment of patients with cancer has traditionally been focused on treating the disease and its immediate sequelae. The treatment options available for spinal metastases include chemotherapy, bisphosphonates, radiation therapy, surgery and kyphoplasty. [14, 15] Treatment for these patients is palliative and aimed at reducing disability. [2] Recently, there has been acknowledgment of the need to improve patients’ quality of life; e.g., multi-disciplinary treatments, including complementary and alternative therapies, to aid in pain management. [19]
This patient was treated with chiropractic care including myofascial massage (soft tissue therapy), mobilization, education and exercises. She responded well to chiropractic care and obtained unique relief from chiropractic treatment that she was unable to achieve from analgesic medication. She did not receive spinal manipulation as part of her treatment plan, though it was not considered absolutely contraindicated in our case. Cervical manipulation was considered in the plan of management because of the anticipation of more effective treatment of joint dysfunction. [20]
Manipulation of pathologically-affected motion segments is absolutely contraindicated, as there is potential for fractures due to compromised bone quality and, possibly, consequent spinal cord compromise. However, malignancy per se should be considered a relative contra-indication to manipulation or other manual therapies in cancer patients, and practitioners should formulate treatment plans tailored to each patient’s unique presentation and needs. [19] In patients with malignancy who do not have compromised bone quality, spinal manipulation could be considered in the treatment plan, as it can offer symptomatic relief and improved function for the patient. [19] Patients with compromised bone strength may be treated with low force techniques and achieve good clinical outcomes. However, practitioners should remain vigilant for signs and symptoms of metastasis, since rates of metastasis are increasing as newer and more effective cancer treatments are increasing survival. [2]
Aside from the improvement in symptomatology, function and quality of life obtained from the chiropractic therapy, this patient’s case reveals less obvious advantages she derived from her chiropractic management. It is unusual for a patient to present with a significant problem, especially actual or suspected malignancy, without concomitant confusion, fear, anxiety, depression or anger. [21] Patient-centred health care based on the biopsychosocial model of illness requires providers to address the psychological and emotional facets of a patient’s presentation as much as the physical ones, yet few primary care practitioners find the time to do so adequately. Although chiropractors have traditionally succeeded at establishing good rapport with their patients, [22] they may feel unqualified to address complex concomitants of patients’ somatic presentations, even when scheduling could be accommodative. At best, patients whose needs have at least been identified may be referred for concurrent care by another appropriate health care provider, though in financially overburdened health care systems, the referral may not be effected for weeks or months.
In this case, the patient, often accompanied by her husband, typically brought lists of questions about her condition, therapy, alternatives, progress, etc. to her chiropractic appointments, requiring scheduling of lengthier treatment sessions to address her needs more comprehensively. She often volunteered that she valued the psychological relief she felt from knowing she had this resource available to her and the reassurance she derived from knowing that everything possible was being done to assess, treat and monitor her entire health status by each of the providers of her health care team. She also related the profound relief she felt from the opportunity afforded to her by the regular chiropractic treatment schedule to vent the intense emotions affecting her to an empathic practitioner.
The nature of administration of many complementary therapies requires the patient to attend more frequently than, for example, for medical management. Therein lies the inherent potential benefit of quicker detection of new or worsening symptoms or signs. This was another benefit the patient in this case derived from her chiropractic management, as the detection of new symptoms and signs, which may have remained unexplored for a significant time if she were only attending for medical follow-ups, prompted the chiropractic referral to the family physician, which led rapidly to detection of further metastasis. Although this did not ultimately effect cure in this case, avoiding delay in effective treatment based on definitive diagnosis is critical for cure when it can be attained. [23] Thus, the patient’s confidence and trust in her chiropractic management, which included ongoing collaboration with her medical physician, was justified.
Summary
Patients may often present to chiropractic clinics with a known history of cancer, with musculoskeletal pain as the first manifestation of undiagnosed cancer, and with benign musculoskeletal dysfunction. Practitioners should complete a thorough history and physical examination in order to rule out serious underlying pathology prior to initiating treatment. Practitioners should be cognizant that in patients presenting with cancer, metastasis to the CNS may occur earlier than to the skeletal system. Patients with headaches and a known history of cancer should be evaluated for the presence of intracranial space occupying lesions. In any patient with new onset of spinal pain and a known history of cancer, a diagnosis of metastasis should be considered until ruled out.
Once malignancy has been diagnosed, chiropractors can still have a role to play in the interdisciplinary management of patients, offering effective treatments for relief of dysfunction and symptoms. [19] Patients with malignancy can still be treated with chiropractic care including spinal manipulation, mobilization, soft tissue treatments, education and rehabilitative exercises. The patient in our case underwent a thorough history and physical examination with appropriate diagnostic imaging, and received patient-centred treatment and chiropractic care.
Cancer patients, like the one described in this case report, often respond well to chiropractic care, achieving outcomes that are unattainable by medication or other therapies, or that reduce the patient’s requirement for analgesic or narcotic medication. For cancer patients who are often on multiple pharmaceutical regimens for years, reduction of the need for any medication is in itself a desirable outcome. As illustrated by this case, patients can also benefit from chiropractic treatment, with its typical requirement for attending in person for the physical administration of treatment more frequently than attending the family physician or medical specialists, by being assessed more frequently and having any new developments in status recognized and managed appropriately, including communicating with other involved members of the health care team. Patient-centred treatment provided by any health care practitioner must involve establishment of good rapport with the patient in order to discover and address all facets of their illness.
References
Choi D, Crockard A, Bunger C, Harms J, Kawahara N, Mazel C, et al.
Review of metastatic spine tumour classification and indications for surgery:
the consensus statement of the Global Spine Tumour Study Group.
Eur Spine J. 2010;19(2):215–222White AP, Kwon BK, Lindskog DM, Friedlaender GE, Grauer JN.
Metastatic disease of the spine.
J Am Acad Orthop Surg. 2006;14(11):587–598Burstein HJ, Gelber S, Guadagnoli E, Weeks JC.
Use of alternative medicine by women with early-stage breast cancer.
N Engl J Med. 1999;340(22):1733–1739Hage WD, Aboulafia AJ, Aboulafia DM.
Incidence, location, and diagnostic evaluation of metastatic bone disease.
Orthop Clin North Am. 2000;31(4):515–528Wolf S, Barton D, Kottschade L, Grothey A, Loprinzi C.
Chemotherapy-induced peripheral neuropathy: prevention and treatment strategies.
Eur J Cancer. 2008;44(11):1507–1515Tirona MT, Sehgal R, Ballester O.
Prevention of breast cancer (part I): epidemiology, risk factors, and risk assessment tools.
Cancer Invest. 2010;28(7):743–750Key TJ, Verkasalo PK, Banks E.
Epidemiology of breast cancer.
Lancet Oncol. 2001;2(3):133–140Lin NU, Bellon JR, Winer EP.
CNS metastases in breast cancer.
J Clin Oncol. 2004;22(17):3608–3617Kirby S, Purdy RA.
Headache and brain tumors.
Curr Neurol Neurosci Rep. 2007;7(2):110–116Goffaux P, Fortin D.
Brain tumor headaches: from bedside to bench.
Neurosurgery. 2010;67(2):459–466Cheng X, Hung M.
Breast cancer brain metastases.
Cancer Metastasis Rev. 2007;26(3–4):635–643Perrin RG, Laxton AW.
Metastatic spine disease: epidemiology, pathophysiology, and evaluation of patients.
Neurosurg Clin N Am. 2004;15(4):365–373Roodman GD.
Mechanisms of bone metastasis.
N Engl J Med. 2004;350(16):1655–1664Coleman RE.
Metastatic bone disease: clinical features, pathophysiology and treatment strategies.
Cancer Treat Rev. 2001;27(3):165–176Bilsky MH, Lis E, Raizer J, Lee H, Boland P.
The diagnosis and treatment of metastatic spinal tumor.
Oncologist. 1999;4(6):459–469Mercadante S.
Malignant bone pain: pathophysiology and treatment.
Pain. 1997;69(1–2):1–18Verbeeck A.
Bone metastases from breast cancer: guidelines for diagnosis.
J Manipulative Physiol Ther. 2004;27(3):211–215van Tulder M, Becker A, Bekkering T, Breen A, Carter T, Gil del Real MT.
European Guidelines for the Management of Acute Nonspecific Low Back Pain in Primary Care
European Spine Journal 2006 (Mar); 15 Suppl 2: S169–191Schneider J, Gilford S.
The Chiropractor's Role in Pain Management for Oncology Patients
J Manipulative Physiol Ther 2001 (Jan); 24 (1): 52–57Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions: Results of the Bone and Joint Decade
2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123–152DiMatteo MR, Lepper HS, Croghan TW.
Depression is a risk factor for noncompliance with medical treatment:
meta-analysis of the effects of anxiety and depression on patient adherence.
Arch Intern Med. 2000;160(14):2101–2107Coulter ID, Hurwitz EL, Adams AH, et al.
Patients Using Chiropractors in North America:
Who Are They, and Why Are They in Chiropractic Care?
Spine (Phila Pa 1976) 2002 (Feb 1); 27 (3): 291–298Caputo L, Cusimano M, Steiman I.
A study on the frequency of delayed diagnosis of neurological conditions by primary contact health care providers.
J Chiropr Educ. 1997;10(4):81–81
Return to CHIROPRACTIC AND CANCER
Since 11-03-2015


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |