Scoliosis Treatment Using a Combination
of Manipulative and Rehabilitative Therapy:
A Retrospective Case SeriesThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: BMC Musculoskeletal Disorders 2004 (Sep 14); 5: 32 ~ FULL TEXT
OPEN ACCESS Mark W Morningstar, Dennis Woggon, and Gary Lawrence
Pettibon Biomechanics Institute
3416-A 57th St Ct. NW;
Gig Harbor, WA 98335, USABackground The combination of spinal manipulation and various physiotherapeutic procedures used to correct the curvatures associated with scoliosis have been largely unsuccessful. Typically, the goals of these procedures are often to relax, strengthen, or stretch musculotendinous and/or ligamentous structures. In this study, we investigate the possible benefits of combining spinal manipulation, positional traction, and neuromuscular reeducation in the treatment of idiopathic scoliosis.
Methods A total of 22 patient files were selected to participate in the protocol. Of these, 19 met the study criterion required for analysis of treatment benefits. Anteroposterior radiographs were taken of each subject prior to treatment intervention and 4–6 weeks following the intervention. A Cobb angle was drawn and analyzed on each radiograph, so pre and post comparisons could be made.
Results After 4–6 weeks of treatment, the treatment group averaged a 17° reduction in their Cobb angle measurements. None of the patients' Cobb angles increased. A total of 3 subjects were dismissed from the study for noncompliance relating to home care instructions, leaving 19 subjects to be evaluated post-intervention.
Conclusions The combined use of spinal manipulation and postural therapy appeared to significantly reduce the severity of the Cobb angle in all 19 subjects. These results warrant further testing of this protocol.
From the Full-Text Article:
Background
In the MEDLINE- indexed literature, chiropractic treatment has shown to be largely ineffective at significantly reducing scoliotic curvatures. Chiropractic treatment for scoliosis typically consists of spinal manipulation, electric stimulation, some form of isotonic, active exercises, and shoe lifts. [1] However, Lantz et al [2] has shown that these procedures, when applied over a one-year duration, were not sufficient to significantly reduce the Cobb angle of a scoliotic curvature.
The treatment in this study focuses on the reduction of scoliosis by manipulative and rehabilitative methods not commonly used by most chiropractors. The major difference in this treatment compared to others is that stimulation of the involuntary postural reflexes is utilized in the clinic setting as well as in home care. Many of the proposed etiologies of idiopathic scoliosis are neurological in origin, including brain asymmetry [3], neural axis deformities [4], and central nervous system processing errors. [5] Additionally, many coexistent neurological alterations are present in scoliosis patients, such as visual deficiency [6] and decreased postural stability. [7, 8] Therefore, the goals of the proposed treatment are not only to reduce the scoliotic curvatures, but also to rehabilitate any underlying postural and neurological weaknesses or imbalances. Previous chiropractic authors have investigated the effectiveness of various physiotherapeutic modalities in the treatment of scoliosis, such as Pilates, [9] stretching and massage, [10] therapeutic exercises, [11] orthotics, [2] and ultrasound or electric stimulation. [1] The purpose of the present study is to investigate any possible benefits from combining manipulative and rehabilitative techniques from a randomized sample collected from various chiropractic facilities. Preliminary evidence [12] suggests that these procedures may be beneficial for reducing the curvatures associated with scoliosis.
Methods
A nonrandomized set of 22 patients participated in the study. The age range of the subject group was 15–65 years of age. The patients were selected from 3 different chiropractic facilities in the United States. Patients were evaluated according to their chief complaint at initial presentation. Patients were excluded from the study if neoplasm, malignancy, fracture, scoliosis secondary to genetic disorders, or previous arthrodesis were identified.
Each patient was examined radiographically for location and severity of scoliosis with standing anteroposterior full spine imaging. All patients removed their shoes for the imaging. Cobb angles were drawn on each radiograph to identify the degree of curvature present. A specific treatment plan was created based upon the results of each patient's radiographic measurements before and after a sample trial of the proposed clinical procedures. Initially, standing lateral cervical, nasium, lateral lumbar, and anteroposterior lumbopelvic views were taken. These views were taken to quantify forward head posture, cervical lordosis, lumbar lordosis, the sacral base angle, and the Cobb angle of the major lateral curvature. We decided to use the radiographic positioning and analysis outlined by Harrison et al, [13–16] due to its previously published reliability. After these images were taken, each patient was fitted with a 4–lb anterior headweight. They were instructed to walk around with the headweight for 10 minutes. After 10 minutes, a follow-up lateral cervical radiograph was taken while wearing the anterior headweight. The purpose of this lateral stress view is to evaluate the potential improvement in cervical lordosis and reduction in forward head posture from using these procedures. [17, 18] The basis for this aspect of the protocol is based upon the inherent properties of a curved column. In the spine, lateral spinal displacements may occur when the normal sagittal spinal curves [19–22] are flattened, reversed, or accentuated. These curves are necessary for the overall strength and flexibility of the curved spinal column, according to the Delmas Index. [23] Therefore, the proposed treatment is intended to restore a normal cervical and lumbar lordosis, and reduce forward head posture before the scoliotic curvatures are addressed.
The specific manipulative and rehabilitative procedures used in this study are designed to both reduce the scoliotic curvature and theoretically retrain the involuntary neuromuscular, reflexive control of posture and balance. However, the specific neurological effects, if any, remain to be investigated. Some of the procedures have been separately introduced or tested. [17, 18, 24–26]
The manipulative procedures included an upper cervical adjustment designed to mobilize the atlantal-occipital joint with the use of a percussive instrument. This technique is shown in Figure 1. This technique is delivered to patients whose lateral cervical radiographs demonstrated atlanto-occipital flexion. If atlanto-occipital extension was present on the initial lateral cervical radiograph, a -Z drop piece was used to mobilize the occiput into flexion. This is also shown in Figure 1. An anterior thoracic adjustment was administered with the patient's thoracic cage rotated opposite to the rotational displacement. A thoracic drop piece was also used to mobilize and correct the smaller upper thoracic curvature. Side posture lumbopelvic adjustments were delivered bilaterally to correct the rotational component of the pelvic misalignment. These side-posture manipulations were performed on a 30°-incline bench to help pre-stress the spine out of its existing scoliotic curvatures.
Figure 1. The picture on the left demonstrates the mechanically assisted manipulation used when a patient's skull is restricted in extension on lateral cervical radiograph. The picture on the right is the procedure used when the skull flexion is restricted.Certain traction procedures are also employed. These procedures are delivered using high-density foam blocks to pre-stress the spine into specific positions so ligament deformation and stress-relaxation can take place. Supine pelvic blocking was performed on each patient for 15 minutes. The position of the blocks was determined by each patient's pelvic rotation on radiograph and posture analysis. One block is placed under the iliac crest of the posterior ilium, and the other block is placed under the femoral head of the opposite, anteriorly-rotated ilium.
Figure 2 illustrates the position of the pelvic blocks. The rehabilitative procedures, demonstrated in Figure 3, included the use of head, shoulder, and hip weighting devices. These devices may be used while simultaneously performing specific balancing exercises. These exercises include the use of a Pettibon Wobble Chair® and a Posturomed®. [17] Tjernstrom et al [27] showed that repeated performance of a postural alteration induces a long-term motor memory for achieving that novel postural position.
Figure 2. This picture shows the placement of the pelvic blocks for an anterior right ilium. The blocks are placed opposite of the pelvic rotation.
Figure 3. The above picture illustrates a sample placement of the Pettibon Bodyweighting System. Here we have an anterior headweight, right shoulderweight, and left-back and right-front hipweights.
The position of the body weighting was also determined radiographically for each patient. Initially, hipweights and shoulderweights were applied according to each patient's posture analysis. Anteroposterior cervicothoracic and lumbopelvic views were taken while wearing the head and body weighting. Since changes in spinal position are not reliably seen by visualization, [28, 29] these stress radiographs were taken to confirm their corrective effects.
The attending physician treated each patient 3 times per week for the first 4–6 weeks. A total of 3 physicians performed the treatment intervention for all patients. However, each patient did not receive identical treatment at all visits. The physicians performed only those manipulative procedures that were deemed necessary based upon a visual posture analysis at the beginning of each treatment session. However, the rehabilitative procedures remained constant throughout the study for all patients.
Specific home care exercise programs were taught to each patient. These exercises were performed on a daily basis. Each patient was instructed to wear the head and body weighting twice daily for 15 minutes each time. Secondly, each patient was given a set of triangular foam blocks to lie on once daily for 20 minutes, immediately prior to going to bed at night. The foam blocks were positioned under the cervicothoracic and thoracolumbar regions simultaneously. The position of these blocks is shown in Figure 4. Patients participating in any weightlifting activities were required to cease those activities until further notice from the attending physician. Patients who failed to perform the home care more than 3 times were dismissed from the study. A total of 3 subjects were eventually dismissed, leaving 19 subjects to perform post-intervention evaluations.
Figure 4. This figure shows a demonstration of the positional traction procedure. The cervical block is placed under the patient's cervicothoracic junction, allowing the head to extend back over the sloped portion of the block. The low back support is placed under the patient's thoracolumbar junction, posterior to the lowest palpable ribs. The blocks are outlined in white.
Results
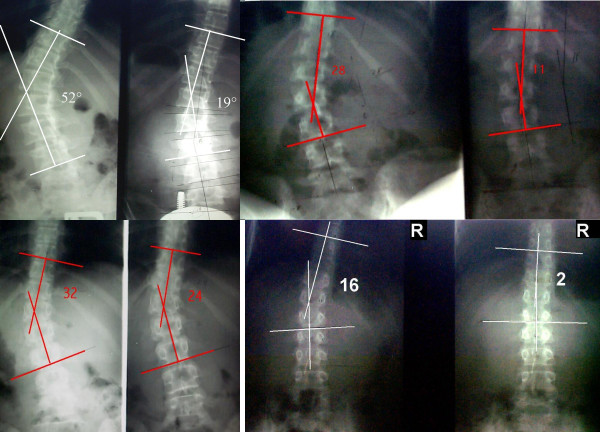
At the conclusion of the trial period, a post-intervention radiographic study was conducted. The same anteroposterior full spine view was taken, and Cobb angles were again measured at the same vertebral levels. The average starting Cobb angle was found to be 28°, while the post-intervention Cobb angles measured an average of 11°, for an overall average reduction of 17°. Every patient made at least a 25% improvement. The largest improvement measured 33°, and the smallest improvement measured 8°. Table 1 shows the results of all 19 patients that followed through with the entire treatment plan. Figure 5 is a sample of the improvements made by a few of the patients.
Table 1: Cobb Angle Measurements after 4–6 Weeks (Degrees)
Figure 5. This figure illustrates some of the pre and post x-rays taken after 4–6 weeks of treatment.
It is important to mention that these patients were initially treated prior to this study. Because of this, the pre and post treatment radiographs had previously been analyzed for sagittal curve and Cobb angle measurements. For purposes of this study, however, all of the radiographs were sent to a single chiropractic physician to analyze each of the patient files. This physician did not participate in the treatment process, nor did this physician have contact with any of the patients. This was performed to separate examiner bias from the treatment results.
While only radiographic procedures were reported for this study, other physiologic parameters were utilized to document patient progress. Unfortunately, since the patient files were extracted from 3 different spine clinics, a consistent functional or symptomatic measure was not used in all 22 cases. A functional rating index, a visual analog scale, and SF-36 were used on the patients here. As a result, these values are not reported to avoid variability in outcome interpretation.
Discussion
Scoliosis has recently been associated with a lower quality of life [30–32], lower scores on the SF-36 health questionnaire [33], and makes patients prone to developing chronic pain more often than the general population [34]. Therefore, reducing scoliotic curvatures, even in the absence of symptoms, seems to be a worthy outcome objective for clinical practice. This opinion is further supported by recent evidence of the deleterious effects of abnormal spinal loading [35–37]. Given that the average curvature progression in idiopathic scoliosis is 7.03° per year [38], the traditional method of regular observation without treatment seems to be reactionary rather than corrective or preventive.
Spinal manipulation alone does not appear to significantly alter spinal structure when administered as a sole treatment modality [39, 40]. Therefore, in the instance of scoliosis, treatment should include the use of both manipulative and rehabilitative procedures, so that structural changes can be attempted. It is important to stress that spinal manipulation was avoided, when possible, in the present study. Unpublished clinical observation by the authors has shown that over-manipulating or adjusting the spine seems to create a certain amount of instability, possibly leading to further buckling of the scoliotic curvature. The significance of home care to the results was not reported here. It is unknown how the omission of home care would have affected the outcome measurements, given that 3 subjects were dropped from the study for noncompliance in performing home care. Future research should account for this potential variable to determine its necessity and relevance.
The outcome measures for this study are divided into a series of both short-term and long-term goals. The outcome of the initial stage of care is to reduce forward head posture and improve the sagittal cervical and lumbar curves. As the position of the head migrates forward, or away from the body's vertical axis, increased strain is placed upon the muscles of the head, neck and shoulders. Cailliet and Zohn indicated that an additional 10 inch/lbs of leverage is added to the spinal system in a forward head posture [41, 42]. Additionally, this added leverage causes increased isometric contraction of various spinal muscles, such as the splenius capitis, trapezius, SCM, and levator scapula. Sjogaard et al [43] reported that blood flow through a given muscle is decreased as a muscles contraction increases, being virtually cut off at 50–60% contraction. The resultant lack of blood flow forces the muscle to rely on anaerobic metabolism. As anaerobic metabolism progresses, metabolites such as substance P, bradykinin, and histamine build up and excite chemosensitive pain receptors, causing a barrage of nociceptive afferent input [44], resulting in dysafferentation [45]. Being that postural control is largely dependant upon cervical joint mechanoreceptors and afferent input from ligament and musculotendinous sources [46, 47], correcting the postural distortions responsible for this pathophysiologic process may be beneficial in patient populations, such as scoliosis, where postural control is significantly altered [48].
The effects of the loss of cervical and lumbar lordosis have been previously reported [19, 35–37]. Rhee et al [49] noted that correction of the sagittal curves might be related to the long-term health of the spine in scoliosis management. Harrison et al [35] illustrated how a loss of the sagittal curve alters the mechanical properties of the spinal cord and nerve roots, which may change the firing patterns of involved neurons. Schafer illustrated how an increased demand is placed upon the cervical musculature when the cervical curve is straightened or reversed [50]. It is important that the cervical spine be in a normal structural alignment. A loss of the cervical lordosis and concomitant forward head posture may elicit the pelvo-ocular reflex, which causes an anterior pelvic translation to balance the head's center of gravity [51]. Wu et al [52, 53] point out that in postural control, preference is given to the position of the head, neck, and trunk. Therefore, correction of the cervical spine becomes imperative so that the rest of the spine can be rehabilitated in relation to a normal reference point in space.
Once the cervical and lumbar lordoses are corrected, coronal reduction of the scoliotic curvatures begins. Here this was accomplished by adding a shoulderweight to the right shoulder and a hipweight to the anterior right ilium and posterior left ilium. Wu and Essien [53] have previously reported the effects of adding external weight to the upper body via a shoulder weight. They identified predictable patterns in which the trunk would compensate for the amount and position of the weight. Wu and MacLeod [52] identified a shift in the center of mass toward the added weight when placed on the side of the pelvis. However, the trunk and head remained in the same position, while the pelvis and lower extremities shifted to counteract the weight while supporting the head and trunk [52]. In this protocol, we created an environment where external weight was added to the head, shoulder, and pelvic regions simultaneously. Knowing the predictable patterns of compensatory shifting to an altered center of gravity, we placed the headweight, shoulderweight, and hipweights in areas designed to reduce each patient's specific spinal distortion patterns.
Learning a new motor coordination skill can be divided into 3 phases: cognitive, associative, and autonomous [54]. In the cognitive phase, the patient performs the motor task repetitively to learn until the task requirements are understood. As the patient progresses through the associative and autonomous phases, the task becomes easier to perform, and may ultimately be performed in a variety of practical contexts with decreased repetitions [54]. While Lantz et al [2] have shown that chiropractic management, consisting of a combination of manipulative procedures, electric stimulation, and orthotic inserts did not significantly reduce a scoliosis, this treatment does not incorporate these physiotherapeutic procedures. Instead, this treatment requires the use of specific rehabilitative equipment that theoretically recruits the use of head, neck, trunk, and extremity postural reflexes to create specific adaptation to an altered center of gravity and field of gaze.
The study design used here does present specific limitations. Due to the lack of a control group, comparative data and conclusions cannot be made. Additionally, a retrospective design does not blind the practitioners to treatment. Although we attempted to select patient files at random from 3 separate spine clinics, nonrandomized sample populations such as ours do not necessarily reflect the potential outcomes in a general population. Therefore, future studies in this area should incorporate a control group and a randomized patient population. Follow-up studies should also focus on the potential long-term benefits of conservative scoliosis treatment, given the relative scarcity of biomedical literature available on long-term benefits from any scoliosis treatment.
Conclusions
Within the design limitations of the present study, the combined use of manipulative and neuromuscular rehabilitation seemed to reduce scoliotic curvatures in 19 subjects by an average of 17°. This reduction took place within a 4 to 6–week period. Although this treatment was not tested over the long term, the magnitude of the present results warrants further studies into its effectiveness. This treatment should also be tested on specific types of scoliosis in follow-up trials. A long-term investigation of this protocol is desirable.
References:
Feise RJ:
An inquiry into chiropractors' intention to treat adolescent idiopathic scoliosis: A telephone survey.
J Manipulative Physiol Ther 2001, 24:177-182
Lantz CA, Chen J.
Effect of Chiropractic Intervention on Small Scoliotic Curves in Younger Subjects: A Time-series Cohort Design
J Manipulative Physiol Ther. 2001 (Jul); 24 (6): 385–393Niesluchowski W, Dabrowska A, Kedzior K, Zagrajek T:
The potential role of brain asymmetry in the development of adolescent idiopathic scoliosis: a hypothesis.
J Manipulative Physiol Ther 1999, 22:540-544
Dobbs MB, Lenke L, Szymanski DA, Morcuende JA, Weinstein SL, Bridwell KH, Sponseller PD:
Prevalence of neural axis abnormalities in patients with infantile idiopathic scoliosis.
J Bone Joint Surg Am 2002, 84-A:2230-2234
Lowe TG, Edgar M, Margulies JY, Miller NH, Raso VJ, Reinker KA, Rivard CH:
Etiology of idiopathic scoliosis: current trends in research.
J Bone Joint Surg Am 2000, 82-A:1157-1168
Catanzariti JF, Salomez E, Bruandet JM, Thevenon A:
Visual Deficiency and Scoliosis.
Spine 2001, 26:48-52
Nault ML, Allard P, Hinse S, Le Blanc R, Caron O, Labelle H, Sadeghi H:
Relations between standing stability and body posture parameters in adolescent idiopathic scoliosis.
Spine 2002, 27:1911-1917
Chen PQ, Wang JL, Tsuang YH, Liao TL, Huang PI, Hang YS:
The postural stability control and gait pattern of idiopathic scoliosis adolescents.
Clin Biomech 1998, 13(Suppl 1):S52-S58
Blum CL:
Chiropractic and pilates therapy for the treatment of adult scoliosis.
J Manipulative Physiol Ther 2002, 25:e3
Tarola GA:
Manipulation for the control of back pain and curve progression in patients with skeletally mature idiopathic scoliosis: two cases.
J Manipulative Physiol Ther 1994, 17:253-257
Golembiewski GV, Catanzaro DJ:
Scoliosis reduction utilizing an exercise.
J Vertebral Subluxation Res 2001, 4:31-36
Morningstar MW, Strauchman MN, Gilmour G:
Idiopathic Scoliosis Treatment Using the Pettibon Corrective Procedures: A Case Report.
J Chiropr Med, in press
Harrison DE, Harrison DD, Colloca CJ, Betz J, Janik TJ, Holland B:
Repeatability over time of posture, radiograph positioning, and radiograph line drawing: an analysis of six control groups.
J Manipulative Physiol Ther 2003, 26:87-98
Troyanovich SJ, Harrison SO, Harrison DD, Harrison DE, Payne MR, Janik TJ, Holland B:
Chiropractic biophysics digitized radiographic mensuration analysis of the anteroposterior lumbopelvic view: a reliability study.
J Manipulative Physiol Ther 1999, 22:309-315
Jackson BL, Harrison DD, Robertson GA, Barker WF:
Chiropractic biophysics lateral cervical film analysis reliability.
J Manipulative Physiol Ther 1993, 16:384-391
Troyanovich SJ, Harrison DE, Harrison DD, Harrison SO, Janik T, Holland B:
Chiropractic biophysics digitized radiographic mensuration analysis of the anteroposterior cervicothoracic view: a reliability study.
J Manipulative Physiol Ther 2000, 23:476-482
Saunders ES, Woggon D, Cohen C, Robinson DH:
Improvement of cervical lordosis and reduction of forward head posture with anterior head weighting and proprioceptive balancing protocols.
J Vertebral Subluxation Res 2003, 4:000
Morningstar MW, Strauchman MN, Weeks DA:
Spinal manipulation and anterior headweighting for the correction of forward head posture and cervical hypolordosis: a pilot study.
J Chiropr Med 2003, 2:51-55
Harrison DE, Harrison DD, Troyanovich SJ, Harmon S:
A normal spinal position: it's time to accept the evidence.
J Manipulative Physiol Ther 2000, 23:623-644
Harrison DD, Janik TJ, Troyanovich SJ, Harrison DE, Colloca CJ:
Evaluation of the assumptions used to derive an ideal normal cervical spine model.
J Manipulative Physiol Ther 1997, 20:246-254
Harrison DE, Janik TJ, Harrison DD, Cailliet R, Harmon SF:
Can the thoracic kyphosis be modeled with a simple geometric shape? The results of circular and elliptical modeling in 80 asymptomatic patients.
J Spinal Disord Tech 2002, 15:213-220
Harrison DD, Cailliet R, Janik TJ, Troyanovich SJ, Harrison DE, Holland B:
Elliptical modeling of the sagittal lumbar lordosis and segmental rotation angles as a method to discriminate between normal and low back pain subjects.
J Spinal Disord 1998, 11:430-439
Kapandji IA:
The physiology of the joints. The trunk and vertebral column. Volume 3. 5th edition.
Churchill Livingstone; 1974:235-236
Morningstar MW:
Cervical hyperlordosis correction: a novel treatment method for mid thoracic pain.
J Chiropr Med 2003, 2:111-115
Morningstar MW:
Strength gains through lumbar lordosis restoration.
J Chiropr Med 2003, 2:137-141
West DT, Mathews RS, Miller MR, Kent GM:
Effective management of spinal pain in one hundred seventy-seven patients evaluated for manipulation
under anesthesia. J Manipulative Physiol Ther 1999, 22:299-308
Tjernstrom F, Fransson PA, Hafstrom A, Magnusson M:
Adaptation of postural control to perturbations- a process that initiates long-term motor memory.
Gait Posture 2002, 15:75-82
Johnson GM:
The correlation between surface measurements of head and neck posture and the anatomic position of the upper cervical vertebrae.
Spine 1998, 23:921-927
Fedorak C, Ashworth N, Marshall J, Paull H:
Reliability of the visual assessment of cervical and lumbar lordosis: how good are we?
Spine 2003, 28:1857-1859
Shapiro GS, Taira G, Boachie-Adjei O:
Results of surgical treatment of adult idiopathic scoliosis with low back pain and spinal stenosis: a study of long-term clinical radiographic outcomes.
Spine 2003, 28:358-363
Danielsson AJ, Nachemson AL:
Radiologic findings and curve progression 22 years after treatment for adolescent idiopathic scoliosis: comparison of brace and surgical treatment with matching control group of straight individuals.
Spine 2001, 26:516-525
Freidel K, Petermann F, Reichel D, Steiner A, Warschburger P, Weiss HR:
Quality of life in women with idiopathic scoliosis.
Spine 2002, 27:E87-E91
Schwab F, Dubey A, Pagala M, Gamez L, Farcy JP:
Adult scoliosis: a health assessment analysis by SF-36.
Spine 2003, 28:602-606
Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV:
Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study.
JAMA 2003, 289:559-567
Harrison DE, Cailliet R, Harrison DD, Troyanovich SJ, Harrison SO:
A review of biomechanics of the central nervous system- part III: spinal cord stresses from postural loads and their neurologic effects.
J Manipulative Physiol Ther 1999, 22:399-410
Harrison DE, Cailliet R, Harrison DD, Troyanovich SJ, Harrison SO:
A review of biomechanics of the central nervous system-part II: spinal cord strains from postural loads.
J Manipulative Physiol Ther 1999, 22:322-332
Harrison DE, Cailliet R, Harrison DD, Troyanovich SJ, Harrison SO:
A review of biomechanics of the central nervous system-part I: spinal canal deformations resulting from changes in posture.
J Manipulative Physiol Ther 1999, 22:227-234
Chuah SL, Kareem BA, Selvakumar K, Oh KS, Borhan Tan A, Harwant S:
The natural history of scoliosis: curve progression of untreated curves of different aetiology, with early (mean 2 year) follow up in surgically treated curves.
Med J Malaysia 2001, 56(Suppl C):37-40
Harrison DD, Jackson BL, Troyanovich SJ, Robertson G, DeGeorge D, Barker WF:
The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis: a pilot study.
J Manipulative Physiol Ther 1994, 17:454-464
Harrison DD, Harrison DE, Troyanovich SJ:
Structural Rehabilitation of the spine and posture: rationale for treatment beyond the resolution of symptoms.
J Manipulative Physiol Ther 1998, 21:37-50
Cailliet R:
In Neck and arm pain. 2nd edition. Edited by Davis FA. 1981.
Zohn DA:
In Musculoskeletal pain diagnosis and treatment. 2nd edition.
Edited by Little Brown. 1988.
Sjogaard G, Savard G, Juel C:
Muscle blood flow during isometric activity and its relation to muscle fatigue.
Eur J Appl Physiol Scand 1988, 57:327-335
Travell JG, Simons D:
Myofascial pain and dysfunction: the trigger point manual.
Williams & Wilkins; 1973
Seaman DR, Winterstein JF:
Dysafferentation: A Novel Term to Describe the Neuropathophysiological Effects of
Joint Complex Dysfunction. A Look at Likely Mechanisms of Symptom Generation
J Manipulative Physiol Ther 1998 (May); 21 (4): 267-280Grod JP, Diakow PR:
Effect of neck pain on verticality perception: A cohort study.
Arch Phys Med Rehabil 2002, 83:412-415
Dietz V, Muller R, Colombo G:
Locomotor activity in spinal man: significance of afferent input from joint and load receptors.
Brain 2002, 125:2626-2634
Gauchard GC, Lascombes P, Kuhnast M, Perrin PP:
Influence of different types of progressive idiopathic scoliosis on static and dynamic postural control.
Spine 2001, 26:1052-1058
Rhee JM, Bridwell KH, Won DS, Lenke LG, Chotigavanichaya C, Hanson DS:
Sagittal plane analysis of adolescent idiopathic scoliosis.
Spine 2002, 27:2350-2356
Schafer RC:
Clinical biomechanics: musculoskeletal actions and reactions. 2nd edition.
Williams & Wilkins; 1987.
Lewit K:
Muscular and articular factors in movement restriction.
Manual Medicine. 1985, 1:83-85
Wu G, MacLeod M:
The control of body orientation and center mass location under asymmetrical loading.
Gait Posture 2001, 13:95-101
Wu G, Essien I:
The regulation of human orientation and center of mass in the frontal plane during upright stance.
In Proceedings of North America Congress of Biomechanics. Waterloo, Canada 1988
Harbst KB, Wilder PA:
Neurophysiologic, motor control, and motor learning basis of closed kinetic chain exercise.
Orthop Phys Ther Clin N Am 2000, 9:137-149.
Return to SCOLIOSIS
Since 9-29-2006


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |