The Relationship Between Spinal Pain and Comorbidity:
A Cross-sectional Analysis of 579 Community-Dwelling,
Older Australian WomenThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2017 (Sep); 40 (7): 459–466 ~ FULL TEXT
Katie E. de Luca, MChiro, PhD, Lynne Parkinson, PhD, Scott Haldeman, DC, MD, PhD, Julie E. Byles, PhD, Fiona Blyth, MPH, PhD
Research Centre for Generational Health and Ageing,
University of Newcastle,
Callaghan, New South Wales, Australia.
FROM: DeLuca 2019
Welcome back to SpineIQ’s BackBlog! This week, we are highlighting a WFC-NCMIC Louis Sportelli Research Award winning paper led by Dr. Katie De Luca, titled “The relationship between spinal pain and comorbidity: cross-sectional analysis of community-dwelling, older Australian women.” Similar to our previous blogs this month, we are once again honoring Women’s History Month by highlighting important studies led by women investigators.
While we have a lot of research showing the large health and financial burden caused by spine pain. There is limited research looking at how spine pain is associated with number and type of comorbidities. This is clinically impactful as a higher number of comorbidities influences prognosis, treatment decisions, and referral or co-management decisions. While spine care clinicians see patients with multiple comorbid conditions every day, many may not think directly about the correlation between spine pain and other serious comorbidities their patients experience. An opportunity exists for an easy transition for the clinician to ask several questions during the initial clinical intake history, which may provide huge insight into the overall health and progress. Therefore, Dr. De Luca and her team sought to understand the relationship between spinal pain and comorbidities.Result(s)
Of the 579 participants, 55.8% (n=323) had spinal pain. It is interesting, as well as instructive, to note that participants reporting spinal pain had worse health-related quality of life compared to participants without spinal pain. Additionally, participants with spinal pain were more likely to have comorbidities compared to people without spinal pain.
In fact, people with spinal pain compared to people without spinal pain were significantly more likely by:
44 times to have 2 comorbidities
07 times to have 3 comorbidities
05 times to have 4 comorbidities.
Finally, people with spinal pain compared to people without spinal pain were significantly more likely by:
93 times to have diabetes
57 times to have cardiovascular disease
66 times to have pulmonary disease
60 times to have mental disorder
98 times to be overweight
12 times to have obesity.
Thanks to Ann Hileman and SpineIQ (Mar 23, 2022) for access to this material!
Objectives: The aims of this study were to (1) report the prevalence and explore the influence of spinal pain on quality of life and (2) assess the relationship between spinal pain and the type and number of comorbidities.
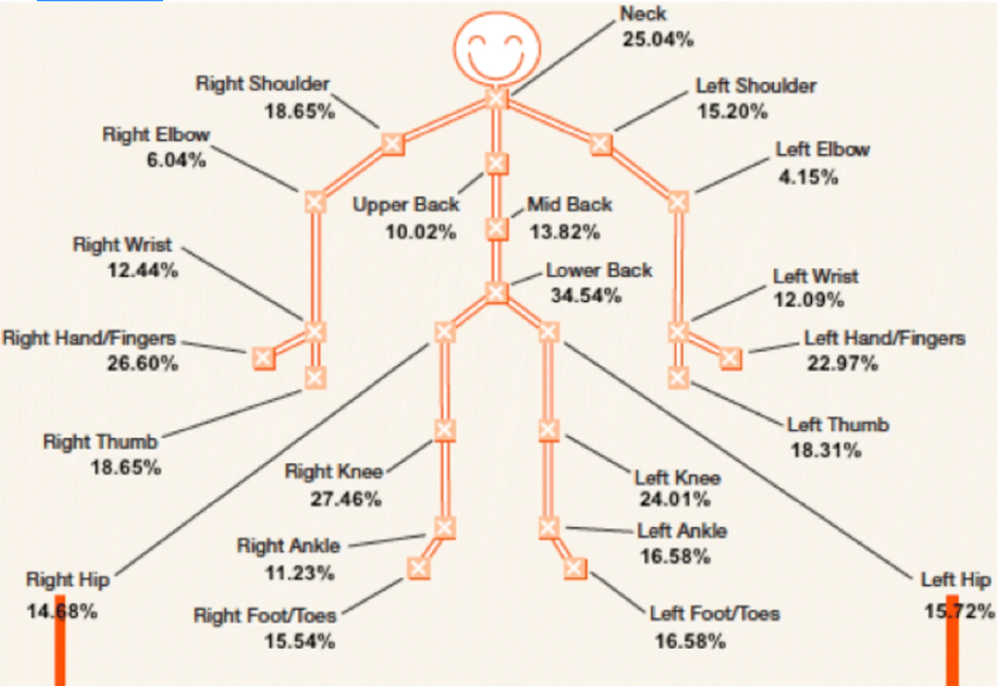
Methods: This cross-sectional study comprised 579 community-dwelling, older Australian women. Women had "spinal pain" if they marked "yes" to neck pain, upper back pain, mid-back pain, and/or lower back pain. Descriptive statistics and binary logistic regression were performed to report the prevalence and explore the relationship between spinal pain and the type and number of comorbidities.
Results: A majority of women (55.8%) who returned surveys had spinal pain. Women with spinal pain had significantly lower physical and mental quality of life scores than women without spinal pain (Medical Outcomes Study: 36 Item Short Form Survey [SF-36] physical component summary: 40.1 ± 11.1 vs 49.0 ± 9.0, and SF-36 mental component summary: 50.0 ± 10.5 vs 53.9 ± 8.2, respectively). Having spinal pain was significantly associated with overweight and obesity (odds ratio 1.98 [95% confidence interval 1.3-2.96] and 2.12 [1.37-3.28]), diabetes (1.93 [1.01-3.67]), pulmonary comorbidity (1.66 [1.04-2.65]), and cardiovascular comorbidity (1.57 [1.07-2.28]). More than half of the women with spinal pain reported 2 or more comorbidities, with comorbidities significantly more common among women with spinal pain than among women without spinal pain. The odds of having spinal pain increased with an increasing number of comorbidities (2 comorbidities: 2.44 [1.47-4.04], 3 comorbidities: 3.07 [1.66-5.67], 4 comorbidities: 5.05 [1.64-15.54]).
Conclusions: Spinal pain is common in community-dwelling, older Australian women and is associated with greater disability and poorer quality of life. Diabetes, cardiovascular disease, pulmonary disease, and obesity appear to have a relationship with spinal pain. There was an incremental increase in the risk of spinal pain associated with increasing comorbidity count.
Keywords: Comorbidity; Epidemiology; Pain; Women’s Health.

Return to SPINAL PAIN MANAGEMENT
Since 3-25-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |