Spinal Pain, Chronic Health Conditions and Health Behaviors: Data from the 2016–2018 National Health Interview Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Measurements
2.2.1. Spinal Pain
2.2.2. Chronic Health Conditions
2.2.3. Confounders
Health Behaviors
Functional Disability
Cognitive Impairment
Mental Health Conditions
Demographic Characteristics
2.3. Statistical Analysis
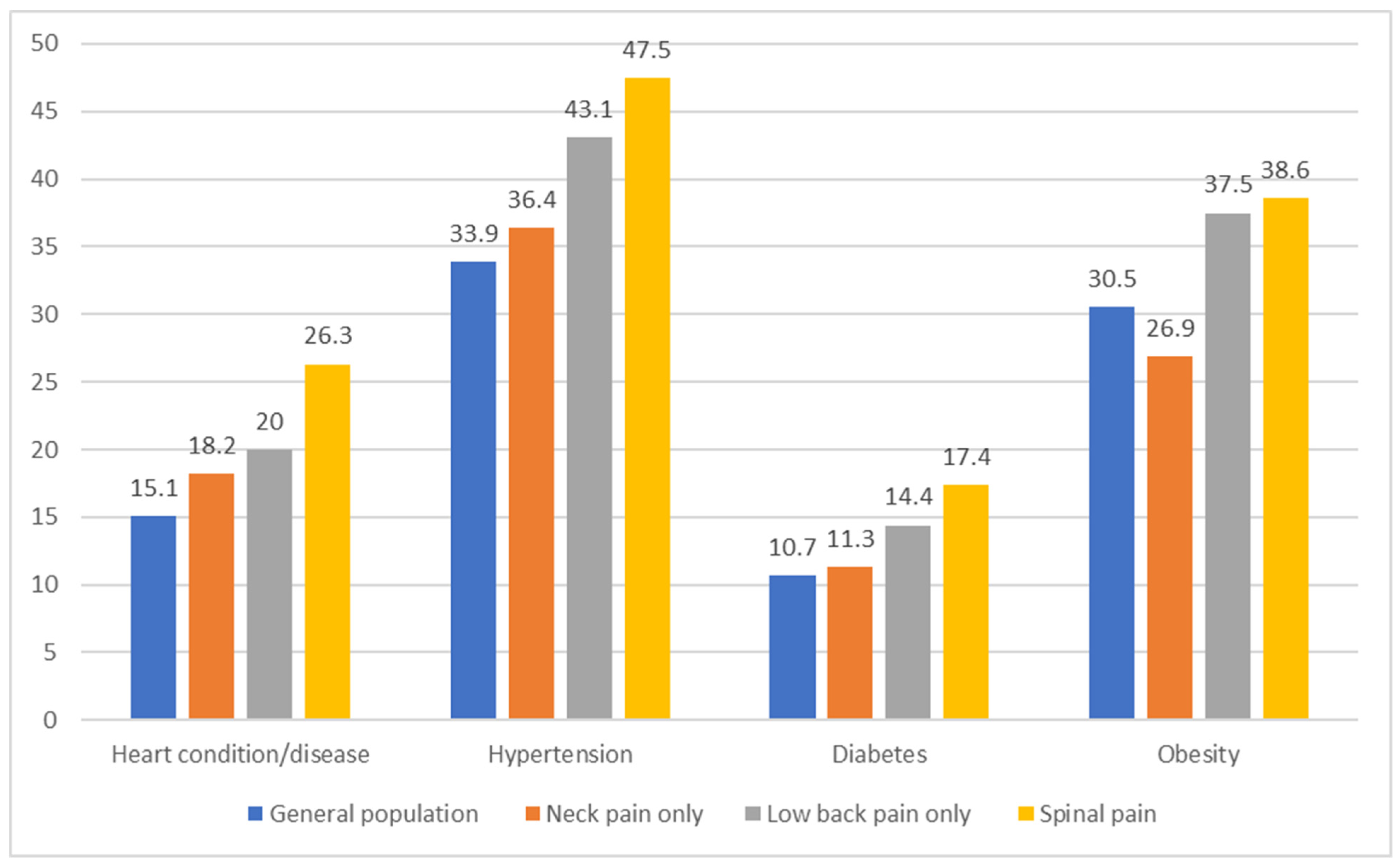
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hurwitz, E.L.; Randhawa, K.; Yu, H.; Côté, P.; Haldeman, S. The Global Spine Care Initiative: A summary of the global burden of low back and neck pain studies. Eur. Spine J. 2018, 27 (Suppl. S6), 796–801. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.L.; de Luca, K.; Haile, L.; Steinmetz, J.; Culbreth, G.; Cross, M.; Kopec, J.; Ferreira, P.H.; Blyth, F.; Buchbinder, R.; et al. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: A systematic Analysis of the global burden of disease study 2021. Lancet Rheumatol. 2023. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Oliveira, C.B.; Maher, C.G.; Franco, M.R.; Kamper, S.J.; Williams, C.; Silva, F.G.; Pinto, R.Z. Co-occurrence of chronic musculoskeletal pain and cardiovascular diseases: A systematic review with meta-analysis. Pain Med. 2020, 21, 1106–1121. [Google Scholar] [CrossRef]
- Zhu, K.; Devine, A.; Dick, I.M.; Prince, R.L. Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine 2007, 32, 2012–2018. [Google Scholar] [CrossRef]
- Shcherbina, A.; Longacre, M. The Association Between Atherosclerosis and Low Back Pain: A Systematic Review. PM&R 2017, 9, 1144–1156. [Google Scholar]
- Samartzis, D.; Bow, C.; Karppinen, J.; Luk, K.D.K.; Cheung, B.M.Y.; Cheung, K.M.C. Hypertension is independently associated with lumbar disc degeneration: A large-scale population-based study. Glob. Spine J. Conf. World Forum Spine Res. 2014, 4. [Google Scholar] [CrossRef]
- Bae, Y.H.; Shin, J.S.; Lee, J. Association between Hypertension and the Prevalence of Low Back Pain and Osteoarthritis in Koreans: A Cross-Sectional Study. PLoS ONE 2015, 10, e0138790. [Google Scholar] [CrossRef]
- Pozzobon, D.; Ferreira, P.H.; Dario, A.B.; Almeida, L.; Vesentini, G.; Harmer, A.R.; Ferreira, M.L. Is there an association between diabetes and neck and back pain? A systematic review with meta-analyses. PLoS ONE 2019, 14, e0212030. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Min, K.B.; Min, J.Y.; Kim, D.H.; Seo, K.M.; Kim, D.K. Strong association of type 2 diabetes with degenerative lumbar spine disorders. Sci. Rep. 2021, 11, 16472. [Google Scholar] [CrossRef]
- Zhang, T.T.; Liu, Z.; Liu, Y.L.; Zhao, J.J.; Liu, D.W.; Tian, Q.B. Obesity as a Risk Factor for Low Back Pain: A Meta-Analysis. Clin. Spine Surg. 2018, 31, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Strine, T.W.; Hootman, J.M. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum. 2007, 57, 656–665. [Google Scholar] [CrossRef] [PubMed]
- de Luca, K.E.; Parkinson, L.; Haldeman, S.; Byles, J.E.; Blyth, F. The Relationship Between Spinal Pain and Comorbidity: A Cross-sectional Analysis of 579 Community-Dwelling, Older Australian Women. J. Manip. Physiol Ther. 2017, 40, 459–466. [Google Scholar] [CrossRef]
- Green, B.N.; Johnson, C.; Haldeman, S.; Griffith, E.; Clay, M.B.; Kane, E.J.; Castellote, J.M.; Rajasekaran, S.; Smuck, M.; Hurwitz, E.L.; et al. A scoping review of biopsychosocial risk factors and co-morbidities for common spinal disorders. PLoS ONE 2018, 13, e0197987. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Haldeman, S. Behavior-Related Factors Associated With Low Back Pain in the US Adult Population. Spine (Phila Pa 1976). 2018, 43, 28–34. [Google Scholar] [CrossRef]
- Green, B.N.; Johnson, C.D.; Snodgrass, J.; Smith, M.; Dunn, A.S. Association Between Smoking and Back Pain in a Cross-Section of Adult Americans. Cureus 2016, 8, e806. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software, Release 12; StataCorp LP.: College Station, TX, USA, 2011. [Google Scholar]
- Briggs, A.M.; E Jordan, J.; O’Sullivan, P.B.; Buchbinder, R.; Burnett, A.F.; Osborne, R.H.; Straker, L.M. Individuals with chronic low back pain have greater difficulty in engaging in positive lifestyle behaviours than those without back pain: An assessment of health literacy. BMC Musculoskelet. Disord. 2011, 12, 161. [Google Scholar] [CrossRef]
- Van Looveren, E.; Bilterys, T.; Munneke, W.; Cagnie, B.; Ickmans, K.; Mairesse, O.; Malfliet, A.; De Baets, L.; Nijs, J.; Goubert, D.; et al. The Association between Sleep and Chronic Spinal Pain: A Systematic Review from the Last Decade. J. Clin. Med. 2021, 10, 3836. [Google Scholar] [CrossRef]
- Zhou, Z.; Hui, E.S.; Kranz, G.S.; Chang, J.R.; de Luca, K.; Pinto, S.M.; Chan, W.W.; Yau, S.-Y.; Chau, B.K.; Samartzis, D.; et al. Potential mechanisms underlying the accelerated cognitive decline in people with chronic low back pain: A scoping review. Ageing Res. Rev. 2022, 82, 101767. [Google Scholar] [CrossRef]
- Buchbinder, R.; van Tulder, M.; Öberg, B.; Costa, L.M.; Woolf, A.; Schoene, M.; Croft, P.; Lancet Low Back Pain Series Working Group. Low back pain: A call for action. Lancet 2018, 391, 2384–2388. [Google Scholar] [CrossRef]
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W.; et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef] [PubMed]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef] [PubMed]
- Ramond-Roquin, A.; Bouton, C.; Bègue, C.; Petit, A.; Roquelaure, Y.; Huez, J.F. Psychosocial Risk Factors, Interventions, and Comorbidity in Patients with Non-Specific Low Back Pain in Primary Care: Need for Comprehensive and Patient-Centered Care. Front. Med. (Lausanne) 2015, 2, 73. [Google Scholar] [CrossRef]
- Charlson, M.E.; Carrozzino, D.; Guidi, J.; Patierno, C. Charlson Comorbidity Index: A Critical Review of Clinimetric Properties. Psychother. Psychosom. 2022, 91, 8–35. [Google Scholar] [CrossRef] [PubMed]
- Meghani, S.H.; Buck, H.G.; Dickson, V.V.; Hammer, M.J.; Rabelo-Silva, E.R.; Clark, R.; Naylor, M.D. The conceptualization and measurement of comorbidity: A review of the interprofessional discourse. Nurs. Res. Pract. 2013, 2013, 192782. [Google Scholar] [CrossRef] [PubMed]
| Demographic and Socioeconomic Variables | General Population | Neck Pain Only | Low Back Pain Only | Spinal Pain |
|---|---|---|---|---|
| Total, % | 5.4 | 21.7 | 12.3 | |
| Age Group | ||||
| 18–25 | 26.4 | 2.4 | 9.4 | 3.9 |
| 25–34 | 14.8 | 4.5 | 17.9 | 8.6 |
| 35–44 | 13.7 | 5.1 | 19.6 | 11.6 |
| 45–54 | 14.2 | 5.9 | 20.7 | 15.0 |
| 55–64 | 14.1 | 6.3 | 23.6 | 15.2 |
| 65–74 | 10.0 | 5.3 | 25.2 | 12.5 |
| 75 and above | 6.80 | 5.6 | 26.4 | 11.3 |
| Sex | ||||
| Female | 51.1 | 5.8 | 21.8 | 13.3 |
| Male | 48.9 | 4.6 | 20.0 | 10.0 |
| Race/Ethnicity | ||||
| Non-Hispanic White | 61.8 | 5.8 | 22.1 | 12.5 |
| Non-Hispanic Black | 12.9 | 3.5 | 21.1 | 10.4 |
| Hispanic | 18.1 | 4.3 | 18.1 | 11.0 |
| Non-Hispanic Asian and Others | 7.2 | 4.6 | 15.6 | 8.2 |
| Education | ||||
| Less than high school | 27.6 | 4.6 | 24.7 | 14.6 |
| High school/GED | 21.3 | 4.7 | 23.9 | 12.7 |
| Some college | 15.5 | 5.1 | 21.9 | 12.8 |
| Bachelor’s/Associate’s degree | 25.9 | 5.5 | 18.9 | 10.7 |
| Master’s/Doctorate/professional | 9.7 | 6.1 | 16.9 | 8.3 |
| Earnings | ||||
| <USD 14,999 | 18.5 | 4.9 | 11.1 | 19.5 |
| USD 15,000–USD 24,999 | 13.6 | 4.8 | 10.5 | 20.8 |
| USD 25,000–USD 44,999 | 25.0 | 4.5 | 10.5 | 19.1 |
| USD 45,000–USD 74,999 | 22.6 | 5.9 | 8.7 | 18.4 |
| USD 75,000 and above | 20.2 | 5.5 | 8.0 | 17.4 |
| Chronic Health Condition and Confounders | No Spinal Pain | Neck Pain Only | Low Back Pain Only | Spinal Pain | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||
| Cardiovascular conditions | Reference | 1.27 | (1.02,1.58) | 0.03 | 1.15 | (1.00,1.31) | 0.05 | 1.58 | (1.35,1.85) | <0.001 |
| Health behaviors | ||||||||||
| Current smokers | 1.08 | (0.90,1.30) | 0.386 | 1.37 | (1.25,1.51) | <0.001 | 1.46 | (1.28,1.65) | <0.001 | |
| Leisure-time physical activity | ||||||||||
| Sufficiently active | Reference | Reference | Reference | |||||||
| Physically inactive | 0.92 | (0.76,1.12) | 0.417 | 1.05 | (0.95,1.17) | 0.32 | 0.94 | (0.82,1.08) | 0.367 | |
| Insufficiently active | 1.10 | (0.92,1.31) | 0.285 | 1.11 | (1.01,1.21) | 0.04 | 1.19 | (1.06,1.33) | 0.002 | |
| Sleep problems | 1.81 | (1.58,2.07) | <0.001 | 1.70 | (1.57,1.84) | <0.001 | 2.80 | (2.52,3.12) | <0.001 | |
| Functional disability | 2.01 | (1.62,2.48) | <0.001 | 2.61 | (2.31,2.94) | <0.001 | 4.24 | (3.67,4.89) | <0.001 | |
| Cognitive impairment | 1.45 | (0.77,2.73) | 0.246 | 1.06 | (0.71,1.59) | 0.76 | 1.90 | (1.35,2.67) | <0.001 | |
| Mental health conditions | ||||||||||
| Anxiety | 1.51 | (1.22,1.87) | <0.001 | 1.39 | (1.23,1.58) | <0.001 | 1.76 | (1.53,2.03) | <0.001 | |
| Depression | 1.36 | (1.02,1.82) | 0.039 | 1.24 | (1.02,1.50) | 0.03 | 1.70 | (1.41,2.05) | <0.001 | |
| Chronic Health Condition and Confounders | No Spinal Pain | Neck Pain Only | Low Back Pain Only | Spinal Pain | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||
| Hypertension | Reference | 1.23 | (1.05,1.43) | 0.01 | 1.31 | (1.2,1.43) | <0.001 | 1.40 | (1.25,1.56) | <0.001 |
| Health behaviors | ||||||||||
| Current smokers | 1.09 | (0.91,1.30) | 0.344 | 1.38 | (1.25,1.51) | <0.001 | 1.46 | (1.29,1.65) | <0.001 | |
| Leisure-time physical activity | ||||||||||
| Sufficiently active | Reference | Reference | Reference | |||||||
| Physically inactive | 0.91 | (0.75,1.11) | 0.35 | 1.04 | (0.94,1.15) | 0.455 | 0.93 | (0.81,1.07) | 0.329 | |
| Insufficiently active | 1.09 | (0.91,1.30) | 0.346 | 1.09 | (0.99,1.20) | 0.071 | 1.17 | (1.05,1.31) | 0.005 | |
| Sleep problems | 1.81 | (1.58,2.07) | <0.001 | 1.69 | (1.57,1.83) | <0.001 | 2.81 | (2.53,3.13) | <0.001 | |
| Functional disability | 2.00 | (1.62,2.48) | <0.001 | 2.54 | (2.26,2.87) | <0.001 | 4.23 | (3.67,4.88) | <0.001 | |
| Cognitive impairment | 1.45 | (0.77,2.74) | 0.249 | 1.06 | (0.71,1.58) | 0.784 | 1.94 | (1.39,2.71) | <0.001 | |
| Mental health conditions | ||||||||||
| Anxiety | 1.51 | (1.22,1.86) | <0.001 | 1.39 | (1.23,1.57) | <0.001 | 1.78 | (1.54,2.05) | <0.001 | |
| Depression | 1.38 | (1.03,1.84) | 0.031 | 1.23 | (1.02,1.49) | 0.03 | 1.71 | (1.42,2.06) | <0.001 | |
| Chronic Health Condition and Confounders | No Spinal Pain | Neck Pain Only | Low Back Pain Only | Spinal Pain | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||
| Diabetes | Reference | 1.12 | (0.88,1.44) | 0.353 | 1.2 | (1.05,1.38) | 0.009 | 1.25 | (1.05,1.49) | 0.01 |
| Health behaviors | ||||||||||
| Current smokers | 1.10 | (0.92,1.32) | 0.29 | 1.37 | (1.24,1.51) | <0.001 | 1.45 | (1.28,1.65) | <0.001 | |
| Leisure time physical activity | ||||||||||
| Sufficiently active | Reference | Reference | Reference | |||||||
| Physically inactive | 0.9 | (0.74,1.09) | 0.283 | 1.03 | (0.93,1.15) | 0.537 | 0.95 | (0.82,1.09) | 0.424 | |
| Insufficiently active | 1.08 | (0.90,1.29) | 0.428 | 1.11 | (1.01,1.22) | 0.029 | 1.20 | (1.08,1.35) | 0.001 | |
| Sleep problems | 1.83 | (1.59,2.10) | <0.001 | 1.69 | (1.56,1.83) | <0.001 | 2.83 | (2.54,3.16) | <0.001 | |
| Functional disability | 2.15 | (1.75,2.66) | <0.001 | 2.65 | (2.35,2.99) | <0.001 | 4.29 | (3.7,4.96) | <0.001 | |
| Cognitive impairment | 1.17 | (0.62,2.23) | 0.63 | 1.03 | (0.69,1.56) | 0.869 | 2.00 | (1.42,2.81) | <0.001 | |
| Mental health conditions | ||||||||||
| Anxiety | 1.47 | (1.18,1.82) | <0.001 | 1.41 | (1.25,1.59) | <0.001 | 1.77 | (1.53,2.05) | <0.001 | |
| Depression | 1.34 | (0.99,1.81) | 0.058 | 1.23 | (1.02,1.48) | 0.033 | 1.72 | (1.43,2.08) | <0.001 | |
| Chronic Health Condition and Confounders | No Spinal Pain | Neck Pain Only | Low Back Pain Only | Spinal Pain | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||
| Obesity | Reference | 0.82 | (0.71,0.96) | 0.011 | 1.34 | (1.25,1.45) | <0.001 | 1.17 | (1.07,1.28) | 0.001 |
| Health behaviors | ||||||||||
| Current smokers | 1.06 | (0.89,1.28) | 0.504 | 1.41 | (1.28,1.55) | <0.001 | 1.50 | (1.32,1.7) | <0.001 | |
| Leisure-time physical activity | ||||||||||
| Sufficiently active | Reference | Reference | Reference | |||||||
| Physically inactive | 0.95 | (0.78,1.15) | 0.57 | 1.04 | (0.93,1.15) | 0.502 | 0.95 | (0.82,1.09) | 0.435 | |
| Insufficiently active | 1.13 | (0.95,1.35) | 0.178 | 1.07 | (0.97,1.18) | 0.163 | 1.19 | (1.06,1.33) | 0.003 | |
| Sleep problems | 1.82 | (1.58,2.08) | <0.001 | 1.70 | (1.57,1.83) | <0.001 | 2.84 | (2.54,3.16) | <0.001 | |
| Functional disability | 2.14 | (1.73,2.65) | <0.001 | 2.47 | (2.19,2.79) | <0.001 | 4.31 | (3.73,4.98) | <0.001 | |
| Cognitive impairment | 1.46 | (0.77,2.76) | 0.246 | 1.05 | (0.70,1.58) | 0.804 | 1.99 | (1.43,2.78) | <0.001 | |
| Mental health conditions | ||||||||||
| Anxiety | 1.48 | (1.20,1.84) | <0.001 | 1.40 | (1.24,1.59) | <0.001 | 1.80 | (1.56,2.08) | <0.001 | |
| Depression | 1.42 | (1.06,1.91) | 0.019 | 1.22 | (1.01,1.48) | 0.042 | 1.68 | (1.39,2.03) | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Luca, K.; Tavares, P.; Yang, H.; Hurwitz, E.L.; Green, B.N.; Dale, H.; Haldeman, S. Spinal Pain, Chronic Health Conditions and Health Behaviors: Data from the 2016–2018 National Health Interview Survey. Int. J. Environ. Res. Public Health 2023, 20, 5369. https://doi.org/10.3390/ijerph20075369
de Luca K, Tavares P, Yang H, Hurwitz EL, Green BN, Dale H, Haldeman S. Spinal Pain, Chronic Health Conditions and Health Behaviors: Data from the 2016–2018 National Health Interview Survey. International Journal of Environmental Research and Public Health. 2023; 20(7):5369. https://doi.org/10.3390/ijerph20075369
Chicago/Turabian Stylede Luca, Katie, Patricia Tavares, Haiou Yang, Eric L. Hurwitz, Bart N. Green, Hannah Dale, and Scott Haldeman. 2023. "Spinal Pain, Chronic Health Conditions and Health Behaviors: Data from the 2016–2018 National Health Interview Survey" International Journal of Environmental Research and Public Health 20, no. 7: 5369. https://doi.org/10.3390/ijerph20075369