A Patient's Guide to Adhesive Capsulitis
Introduction
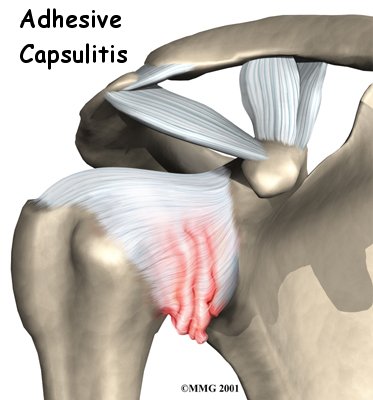
Adhesive capsulitis, also called frozen
shoulder, is a painful condition. It results in a
severe loss of motion in the shoulder. It may follow
an injury, or it may arise gradually with no injury or
warning.
This guide will help you understand
- what causes frozen shoulder
- what tests your doctor will do to diagnose it
- how you can regain use of your shoulder.
Anatomy
What part of the shoulder is affected?
The shoulder is made up of three
bones: the scapula (shoulder blade), the
humerus (upper arm bone), and the
clavicle (collarbone). The joint capsule
is a watertight sac that encloses the joint and the
fluids that bathe and lubricate it. The walls of the
joint capsule are made up of ligaments.
Ligaments are soft connective tissues that attach
bones to bones. The joint capsule has a considerable
amount of slack, loose tissue, so the shoulder is
unrestricted as it moves through its large range of
motion.
In frozen shoulder, inflammation
in the joint makes the normally loose parts of the
joint capsule stick together. This seriously limits
the shoulder's ability to move, and causes the
shoulder to freeze.
Related Document: A
Patient's Guide to Shoulder Anatomy
Causes
Why did my shoulder freeze up?
The cause of frozen shoulder is largely a mystery.
One theory is that it may be caused by an
autoimmune reaction. In an autoimmune reaction,
the body's defense system, which normally protects it
from infection, mistakenly begins to attack the
tissues of the body. This causes an intense
inflammatory reaction in the tissue that is under
attack.
No one knows why this occurs so suddenly. Frozen
shoulder may begin after a shoulder injury, fracture,
or surgery. It can also start if the shoulder is not
being used normally. This can happen after a wrist
fracture, when the arm is kept in a sling for several
weeks. For some reason, immobilizing a joint after an
injury seems to trigger the autoimmune response in
some people.
Frozen shoulder has also been known to occur after
surgery unrelated to the shoulder, even after
recovering from a heart attack. Other shoulder
problems like bursitis, rotator cuff tears, or
impingement syndrome can end up causing a frozen
shoulder. Doctors theorize that the underlying
condition may cause chronic inflammation and pain that
make you use that shoulder less. This sets up a
situation that can create frozen shoulder. Usually,
the frozen shoulder must be treated first to regain
its ability to move before the underlying problem can
be addressed.
Related Document: A
Patient's Guide to Impingement Syndrome
Related Document: A
Patient's Guide to Rotator Cuff
Tears
Symptoms
What are the symptoms of frozen shoulder?
The symptoms of frozen shoulder are primarily
shoulder pain and a very reduced range of motion in
the joint. The range of motion is the same whether you
are trying to move the shoulder yourself or someone
else is trying to move the arm for you. There comes a
point in each direction of movement where the motion
simply stops, as if something is blocking it. At this
point, the shoulder usually hurts. The shoulder can
also be quite painful at night. The tightness in the
shoulder can make it difficult to do regular
activities like getting dressed, combing your hair, or
reaching across a table.
Diagnosis
What tests will my doctor run?
The diagnosis of frozen shoulder is usually made on
the basis of your medical history and physical
examination. One key finding that helps differentiate
a frozen shoulder from a rotator cuff tear is how the
shoulder moves. With frozen shoulder, the shoulder
motion is the same whether the patient or the doctor
tries to move the arm. With a rotator cuff tear, the
patient cannot move the arm. But when someone else
lifts the arm it can be moved in a nearly normal range
of motion.
Simple X-rays are usually not helpful. An
arthrogram may show that the shoulder capsule
is scarred and tightened. The arthrogram involves
injecting dye into the shoulder joint and taking
several X-rays. In frozen shoulder, very little dye
can be injected into the shoulder joint because the
joint capsule is stuck together, making it smaller
than normal. The X-rays taken after injecting the dye
will show very little dye in the joint.
As your ability to move your shoulder increases,
your doctor may suggest tests to rule out an
underlying condition, such as impingement or a rotator
cuff tear. Probably the most common test used is
magnetic resonance imaging (MRI). An MRI scan
is a special imaging test that uses magnetic waves to
create pictures that show the tissues of the shoulder
in slices.
.jpg)
The MRI scan shows tendons and other soft tissues
as well as the bones.
.jpg)
Colorized to illustrate soft tissues
revealed in MRI
Treatment
What treatment options are available?
Nonsurgical Treatment
Treatment of frozen shoulder can be frustrating and
slow. Most cases eventually improve, but the process
may take months. The goal of your initial treatment is
to decrease inflammation and increase the range of
motion of the shoulder. Your doctor will probably
recommend anti-inflammatory medications, such as
aspirin and ibuprofen.
Physical or occupational therapy treatments are a
critical part of helping you regain the motion and
function of your shoulder. Treatments are directed at
getting the muscles to relax. Therapists use heat and
hands-on treatments to stretch the joint capsule and
muscle tissues of the shoulder. You will also be given
exercises and stretches to do as part of a home
program. You may need therapy treatments for three to
four months before you get full shoulder motion and
function back.
Your doctor may also recommend an injection of
cortisone and a long-acting anesthetic,
similar to lidocaine, to get the inflammation under
control. Cortisone is a steroid that is very effective
at reducing inflammation. Controlling the inflammation
relieves some pain and allows the stretching program
to be more effective. In some cases, it helps to
inject a long-acting anesthetic with the cortisone
right before a stretching session. This allows your
therapist to manually break up the adhesions while the
shoulder is numb from the anesthetic.
SurgeryManipulation under Anesthesia
If progress in rehabilitation is slow, your doctor
may recommend manipulation under anesthesia.
This means you are put to sleep with general
anesthesia. Then the surgeon aggressively stretches
your shoulder joint. The heavy action of the
manipulation stretches the shoulder joint capsule and
breaks up the scar tissue. In most cases, the
manipulation improves motion in the joint faster than
allowing nature to take its course. You may need this
procedure more than once.
This procedure has risks. There is a very slight
chance the stretching can injure the nerves of the
brachial plexus, the network of nerves running
to your arm. And there is a risk of fracturing the
humerus (the bone of the upper arm), especially in
people who have osteoporosis (fragile bones).
.jpg)
Arthroscopic Release
When it becomes clear that physical therapy and
manipulation under anesthesia have not improved
shoulder motion, arthroscopic release may be
needed. This procedure is usually done using an
anesthesia block to deaden the arm. The surgeon
uses an arthroscope to see inside the shoulder.
An arthroscope is a slender tube with a camera
attached. It allows the surgeon to see inside the
joint.
During the athroscopic procedure, the surgeon cuts
(releases) scar tissue, the ligament on top of the
shoulder (coracohumeral ligament), and a small
portion of the joint capsule. If shoulder movement is
not regained or if the surgeon is unable to complete
the surgery using the arthroscope, an open
procedure may be needed. An open procedure requires a
larger incision so the surgeon can work in the joint
more easily.
At the end of the release procedure, the surgeon
gently manipulates the shoulder to gain additional
motion. A steroid medicine may be injected into the
shoulder joint at the completion of the
procedure.
Rehabilitation
What can I expect after treatment?
Nonsurgical Rehabilitation
The primary goal of physical therapy is to help you
regain full range of motion in the shoulder. If your
pain is too strong at first to begin working on
shoulder movement, your therapist may need to start
with treatments to help control pain. Treatments to
ease pain include ice, heat, ultrasound, and
electrical stimulation. Therapists also use massage or
other types of hands-on treatment to ease muscle spasm
and pain.
When your shoulder is ready, therapy will focus on
regaining your shoulder's movement. Sessions may begin
with treatments like moist hot packs or ultrasound.
These treatments relax the muscles and get the
shoulder tissues ready to be stretched. Therapists
then begin working to loosen up the shoulder joint,
especially the joint capsule. You can also get a good
stretch using an overhead shoulder pulley in the
clinic or as part of a home program.
If your doctor recommends an injection for your
shoulder, you should plan on seeing your therapist
right after the injection. The extra fluid from the
injection stretches out the tissues of the joint
capsule. An aggressive session of stretching right
afterward can help maximize the stretch to the joint
capsule.
After Surgery
After arthroscopic release, you'll likely begin
using a shoulder pulley on a daily basis. You'll
probably be encouraged to use the treated arm in
everyday activities. Strengthening exercises are not
begun for four to six weeks after the procedure. You
might participate in physical or occupational therapy
for up to two months after arthroscopic release.
After manipulation under anesthesia, your surgeon
may place your shoulder in a continuous passive
motion (CPM) machine. CPM is used after many
different types of joint surgeries. You begin using
CPM immediately after surgery. It keeps the shoulder
moving and alleviates joint stiffness. The machine
simply straps to the arm and continuously moves the
joint. This continuous motion is thought to reduce
stiffness, ease pain, and keep extra scar tissue from
forming inside the joint.
Some surgeons apply a dynamic splint to the
shoulder after manipulation surgery. A dynamic splint
puts the shoulder into a full stretch and holds it
there. Keeping the shoulder stretched gradually
loosens up the joint capsule.
You'll resume therapy within one to two days of the
shoulder manipulation. Some surgeons have their
patients in therapy every day for one to two weeks.
Your therapist will treat you with aggressive
stretching to help maximize the benefits of the
shoulder manipulation. The stretching also keeps scar
tissue from forming and binding the capsule again.
Your shoulder movement should improve continually
after the manipulation and therapy. If not, you may
require more than one manipulation.
Once your shoulder is moving better, treatment is
directed toward shoulder strengthening and function.
These exercises focus on the rotator cuff and shoulder
blade muscles. Your therapist will help you retrain
these muscles to help keep the ball of the humerus
centered in the socket. This lets your shoulder move
smoothly during all your activities.
The therapist's goal is to help you regain shoulder
motion, strength, and function. When you are well
under way, regular visits to the therapist's office
will end. Your therapist will continue to be a
resource, but you will be in charge of doing your
exercises as part of an ongoing home
program. |