A Patient's Guide to Biceps Rupture
Introduction
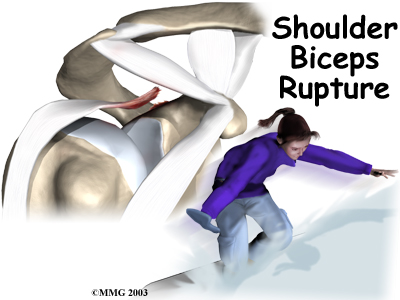
A biceps rupture involves a complete tear of the
main tendon that attaches the top of the biceps muscle to
the shoulder. It happens most often in middle-aged people
and is usually due to years of wear and tear on the
shoulder. A torn biceps in younger athletes sometimes occurs
during weightlifting or from actions that cause a sudden
load on the arm, such as hard fall with the arm
outstretched.
This guide will help you understand
- what parts of the shoulder are affected
- the causes of a biceps rupture
- ways to treat this problem
Anatomy
What parts of the shoulder are affected?
The biceps muscle goes from the shoulder to the elbow on
the front of the upper arm. Two separate tendons (tendons attach
muscles to bones) connect the upper part of the biceps
muscle to the shoulder. The upper two tendons of the biceps
are called the proximal biceps tendons, because they
are closer to the top of the arm.
The main proximal tendon is the long head of the biceps. It connects the biceps
muscle to the top of the shoulder socket, the
glenoid. Beginning at the glenoid, the tendon of the
long head of the biceps travels down the front of the upper
arm. The tendon runs within the bicipital groove and
is held in place by the transverse humeral
ligament.
The short head of the biceps connects on the
corocoid process of the scapula. The corocoid process
is a small bony knob just in from the front of the shoulder.
The lower biceps tendon is called the distal biceps tendon. The word distal
means the tendon is further down the arm. The lower part of
the biceps muscle connects to the elbow by this tendon.
The muscles forming the short and long heads of the
biceps stay separate until just above the elbow where they
unite and connect to the distal biceps tendon.
Tendons are made up of strands of a material called
collagen. The collagen strands are lined up in
bundles next to each other.
Because the collagen strands in tendons are lined up,
tendons have high tensile strength. This means they
can withstand high forces that pull on both ends of the
tendon. When muscles work, they pull on one end of the
tendon. The other end of the tendon pulls on the bone,
causing the bone to move.
Contracting the biceps muscle can bend the elbow
upward. The biceps can also help flex the shoulder, lifting
the arm up, a movement called flexion. And the muscle
can rotate, or twist, the forearm in a way that points the
palm of the hand up. This movement is called
supination, which positions the hand as if you were
holding a tray.
Related Document: A
Patient's Guide to Shoulder Anatomy
Causes
Why did my biceps rupture?
Biceps ruptures generally occur in people who are between
40 and 60 years old. People in this age group who've had
shoulder problems for a long time are at most risk. Often
the biceps ruptures after a long history of shoulder pain
from tendonitis (inflammation of hte tendon) or
problems with shoulder impingement. Shoulder impingement is a
condition where the soft tissues between the ball of the
upper arm and the top of the shoulder blade
(acromion) get squeezed with arm motion.
Related Document: A
Patient's Guide to Shoulder Impingement
Years of shoulder wear and tear begin to fray the biceps
tendon. Eventually, the long head of the biceps weakens and
becomes prone to tears or ruptures. Examination of the
tissues within most torn or ruptured biceps tendons commonly
shows signs of degeneration. Degeneration in a tendon
causes a loss of the normal arrangement of the collagen
fibers that join together to form the tendon. Some of the
individual strands of the tendon become jumbled due to the
degeneration, other fibers break, and the tendon loses
strength.
A rupture of the biceps tendon can happen from a
seemingly minor injury. When it happens for no apparent
reason, the rupture is called nontraumatic.
Aging adults with rotator cuff tears also commonly have a
biceps tendon rupture. When the rotator cuff is torn, the
ball of the humerus is free to move too far up and forward
in the shoulder socket and can impact the biceps tendon. The
damage may begin to weaken the biceps tendon and cause it to
eventually rupture.
Related Document: A
Patient's Guide to Rotator Cuff Tears
Symptoms
What does a ruptured biceps feel like?
Patients often recall hearing and feeling a snap in the
top of the shoulder. Immediate and sharp pain follow. The
pain often subsides quickly with a complete rupture because
tension is immediately taken off the pain sensors in the
tendon. Soon afterward, bruising may develop in the middle
of the upper arm and spread down to the elbow. The biceps
may appear to have balled up, especially in younger patients
who've had a traumatic biceps rupture. The arm may feel weak
at first with attempts to bend the elbow or lift the
shoulder.
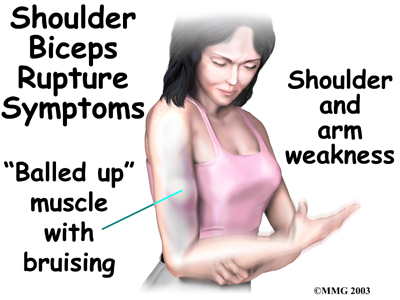
The biceps tendon sometimes only tears part of the way.
If so, a pop may not be felt or heard. Instead, the front of
the shoulder may simply be painful, and the arm may feel
weak with the same arm movements that are affected with a
complete biceps rupture.
Diagnosis
How can my doctor be sure my biceps ruptured?
Your doctor will first take a detailed medical history.
You will need to answer questions about your shoulder, if
you feel pain or weakness, and how this is affecting your
regular activities. You'll also be asked about past shoulder
pain or injuries.
The physical exam is often most helpful in diagnosing a
rupture of the biceps tendon. Your doctor may position your
arm to see which movements are painful or weak. By feeling
the area of the muscle and tendon, the doctor can often tell
if the tendon has ruptured. The muscle may look and feel
balled up in the middle of the arm, and a dent can sometimes
be felt near the top of the shoulder.
X-rays may be ordered. X-rays show the bones that form
the shoulder joint and may show bony changes that have
contributed to a ruptured biceps. For example, bone
spurs (small projections of bone) may be seen on the
X-ray. Spurs that form near the biceps tendon will often
puncture the tendon as the arm is used with activity. X-rays
can also show if there are other problems, such as a
fracture. Plain X-rays do not show soft tissues like tendons
and will not show a biceps rupture.
Your doctor may also order a magnetic resonance
imaging (MRI) scan. This is the most reliable way to
check whether the biceps tendon is only partially torn or if
the tendon actually ruptured. An MRI is a special imaging
test that uses magnetic waves to create pictures of the
shoulder in slices. The MRI can also show if there are other
problems in the shoulder.
Treatment
What treatment options are available?
Nonsurgical Treatment
Doctors usually treat a ruptured long head of biceps
tendon without surgery. This is especially true for older
individuals who can tolerate loss of arm strength or if the
injury occurs in the nondominant arm.
Not having surgery usually only results in a moderate
loss of strength. The short head of the biceps is still
attached and continues to supply strength to raise the arm
up. Flexion of the elbow may be affected, but supination
(the motion of twisting the forearm such as when you use a
screwdriver) is usually affected more. Not repairing a
ruptured biceps reduces supination strength by about 20 percent.
Nonsurgical measures could include a sling to rest the
shoulder. Patients may be given anti-inflammatory medicine
to help ease pain and swelling and to help return people to
activity sooner after a biceps tendon rupture. These
medications include common over-the-counter drugs such as
ibuprofen.
Doctors may have their patients work with a physical or
occupational therapist. At first, your therapist will give
you tips how to rest your shoulder and how to do your
activities without putting extra strain on the sore
area.
Your therapist may apply ice and electrical stimulation
to ease pain. Exercises are used to gradually strengthen
other muscles that help do the work of a normal biceps
muscle.
Surgery
Surgery is reserved for patients who need arm strength,
are concerned with cosmetics of the balled up biceps, or who
have pain that won't go away.
Biceps Tenodesis
Biceps tenodesis is a surgery to anchor the
ruptured end of the biceps tendon. A common method, called
the keyhole technique, involves anchoring the
ruptured end to the upper end of the humerus. The
keyhole describes the shape of a small hole made by
the surgeon in the humerus. The end of the tendon is slid
into the top of the keyhole and pulled down to anchor it in
place.
The surgeon begins by making an incision on the front of
the shoulder, just above the axilla (armpit). The
overlying muscles are separated so the surgeon can locate
the damaged end of the biceps tendon. The end of the biceps
tendon is prepared by cutting away frayed and degenerated
tissue.
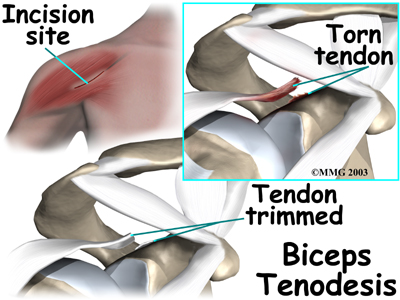
The transverse humeral ligament is split, exposing the bicipital groove. An incision is made along the floor
of the bicipital groove. The bleeding from the incision gets
scar tissue to form that will help anchor the repaired
tendon in place.
A burr is used to form a keyhole-shaped cavity within the bicipital groove. The
top of the cavity is round. The bottom is the slot of
the keyhole. It is made the same width as the biceps tendon.
The surgeon rolls the top end of the biceps tendon into a
ball. Sutures are used to form and hold the ball. The elbow
is bent, taking tension off the biceps muscle and tendon.
The surgeon pushes the tendon ball into the top part of the
keyhole. As the elbow is gradually straightened, the ball is
pulled firmly into the narrow slot in the lower end of the
keyhole.
The surgeon tests the stability of the attachment by
bending and straightening the elbow. When the surgeon is
satisfied with the repair, the skin incisions are closed,
and the shoulder is placed in a protective sling.
Acromioplasty and Direct Tenodesis
This procedure may be used for younger patients who've
had a recent traumatic biceps rupture, have problems with
impingement, and who have an injured rotator cuff.
Acromioplasty involves cutting and reshaping the
acromion, the bone that forms the top part of the shoulder.
Some surgeons will also sever the corocohumeral
ligament, which arches over the top of the shoulder
joint. These steps relieve pressure on the tissues between
the ball of the humerus and the acromion, including the
biceps and rotator cuff tendons. For this reason, this
procedure is sometimes called subacromial
decompression. The ruptured end of the biceps is then
anchored to the upper end of the humerus. This is called
direct tenodesis.
The surgeon begins by making an incision across the top
of the shoulder. The shoulder muscles are separated to
expose the top of the humerus. Bone spurs are removed, along
with part of the acromion. The surgeon then smooths the
rough ends of the bone.
After the acromioplasty procedure, the surgeon focuses on
the biceps tendon. When the bicipital groove is in view, the
transverse humeral ligament is cut. Next, an
osteotome is used to open the joint capsule and
create a trough next to the bicipital groove. Three small
holes are drilled along each side of the trough. The surgeon
places the loose end of the biceps tendon in the new
groove.
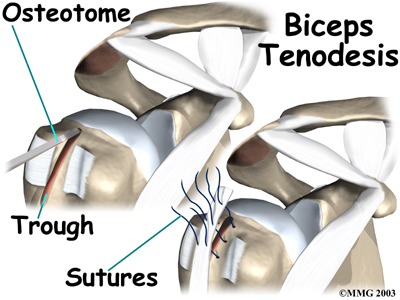
Sutures are woven into one drill hole, through the
tendon, and out the opposite drill hole. This is repeated
for the remaining two sets of drill holes. Next, the top end
of the ruptured tendon is cut off. Finally, the three sutures are firmly secured.
When the surgeon is satisfied with the repair, the
transverse humeral ligament and joint capsule are sutured,
followed by the skin incision. The arm is bent at the elbow
and placed in a light splint that is to be worn for four
weeks after surgery.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
In cases where the ruptured biceps tendon is treated
nonsurgically, you will need to avoid heavy arm activity for
three to four weeks. As the pain and swelling resolve, you
should be safe to begin doing more normal activities.
If the tendon is only partially torn, however, recovery
takes longer. Patients usually need to rest the shoulder
using a protective sling. As symptoms ease, a carefully
progressed rehabilitation program under the supervision of a
physical or occupational therapist usually follows. This
often involves four to six weeks of therapy.
After Surgery
Immediately after surgery, you'll need to wear your
shoulder sling for about four weeks. Some surgeons prefer to
have their patients start a gentle range-of-motion program
soon after surgery. When you start therapy, your first few
therapy sessions may involve ice and electrical stimulation
treatments to help control pain and swelling from the
surgery. Your therapist may also use massage and other types
of hands-on treatments to ease muscle spasm and pain.
You will gradually start exercises to improve movement in
the forearm, elbow, and shoulder. You need to be careful to
avoid doing too much, too quickly.
Heavier exercises for the biceps muscle are avoided until
at least four to six weeks after surgery. Your therapist may
begin with light isometric strengthening exercises. These
exercises work the biceps muscle without straining the
healing tendon.
At about six weeks, you start doing more active
strengthening. As you progress, your therapist will teach
you exercises to strengthen and stabilize the muscles and
joints of the elbow and shoulder. Other exercises will work
your arm in ways that are similar to your work tasks and
sport activities. Your therapist will help you find ways to
do your tasks that don't put too much stress on your
shoulder.
You may require therapy for six to eight weeks. It
generally takes three to four months, however, to safely
begin doing forceful biceps activity after surgery. Before
your therapy sessions end, your therapist will teach you a
number of ways to avoid future problems. |