A Patient's Guide to Dupuytren's Contracture
Introduction
Dupuytren's contracture is a fairly common
disorder of the fingers. It most often affects the ring or
little finger, sometimes both, and often in both hands.
Although the exact cause is unknown, it occurs most often in
middle-aged, white men and is genetic in nature, meaning it
runs in families. This condition is seven times more common
in men than women. It is more common in men of Scandinavian,
Irish, or Eastern European ancestry. Interestingly, the
spread of the disease seems to follow the same pattern as
the spread of Viking culture in ancient times. The disorder
may occur suddenly but more commonly progresses slowly over
a period of years. The disease usually doesn't cause
symptoms until after the age of 40.
This guide will help you understand
- how Dupuytren's contracture develops
- how the disorder progresses, and how you can measure
its progression
- what treatments are available
Anatomy
What part of the hand is affected?
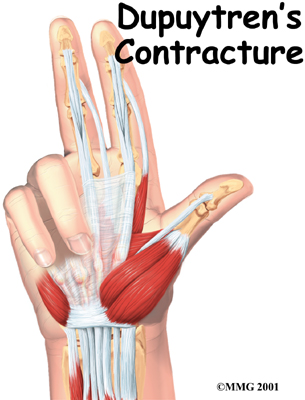
The palm side of the hand contains many nerves, tendons,
muscles, ligaments, and bones. This combination allows us to
move the hand in many ways. The bones give our hand
structure and form joints. Bones are attached to bones by
ligaments. Muscles allow us to bend and straighten
our joints. Muscles are attached to bones by tendons.
Nerves stimulate the muscles to bend and straighten. Blood
vessels carry needed oxygen, nutrients, and fuel to the
muscles to allow them to work normally and heal when
injured. Tendons and ligaments are connective tissue.
Another type of connective tissue, called fascia,
surrounds and separates the tendons and muscles of the
hand.
Lying just under the palm is the palmar fascia, a thin sheet of connective
tissue shaped somewhat like a triangle. This fascia covers
the tendons of the palm of the hand and holds them in place.
It also prevents the fingers from bending too far backward
when pressure is placed against them. The fascia separates
into thin bands of tissue at the fingers. These bands
continue into the fingers where they wrap around the joints
and bones. Dupuytren's contracture forms when the palmar
fascia tightens, causing the fingers to bend.
The condition commonly first shows up as a thick nodule
(knob) or a short cord in the palm of the hand, just below
the ring finger. More nodules form, and the tissues thicken
and shorten until the finger cannot be fully straightened.
Dupuytren's contracture usually affects only the ring and
little finger. The contracture spreads to the joints of the
finger, which can become permanently immobilized.
Related Document: A
Patient's Guide to Hand Anatomy
Causes
Why do I have this problem?
No one knows exactly what causes Dupuytren's contracture.
The condition is rare in young people but becomes more
common with age. When it appears at an early age, it usually
progresses rapidly and is often very severe. The condition
tends to progress more quickly in men than in women.
People who smoke have a greater risk of having
Dupuytren's contracture. Heavy smokers who abuse alcohol are
even more at risk. Recently, scientists have found a
connection with the disease among people who have diabetes.
It has not been determined whether or not work tasks can put
a person at risk or speed the progression of the
disease.
Symptoms
What does Dupuytren's contracture feel like?
Normally, we are able to control when we bend our fingers
and how much. How much we flex our fingers determines how
small an object we can hold and how tightly we can hold it.
People lose this control as the disorder develops and the
palmar fascia contracts, or tightens. This contracture is
like extra scar tissue just under the skin. As the disorder
progresses, the bending of the finger becomes more and more
severe, which limits the motion of the finger.
Without treatment, the contracture can become so severe
that you cannot straighten your finger, and eventually you
may not be able to use your hand effectively. Because our
fingers are slightly bent when our hand is relaxed, many
people put up with the contracture for a long time. Patients
with this condition usually seek medical advice for cosmetic
reasons or the loss of use of their hand. At times, the
nodules can be very painful. For this reason many patients
are worried that something serious is wrong with their
hand.
Diagnosis
How do doctors identify the problem?
Your doctor will ask you the history of your problem,
such as how long you have had it, whether you've noticed it
getting worse, and whether it has kept you from doing your
daily activities. The doctor will then examine your hand and
finger.
Your doctor can tell if you have a Dupuytren's
contracture by looking at and feeling the palm of your hand
and your fingers. Usually, special tests are unnecessary.
Abnormal fascia will feel thick. Cords and small nodules in
the fascia may be felt as small knots or thick bands under
the skin. These nodules usually form first in the palm of
the hand. As the disorder progresses, nodules form along the
finger. These nodules can be felt through the skin, and you
may have felt them yourself. Depending on the stage of the
disorder, your finger may have started to contract, or
bend.
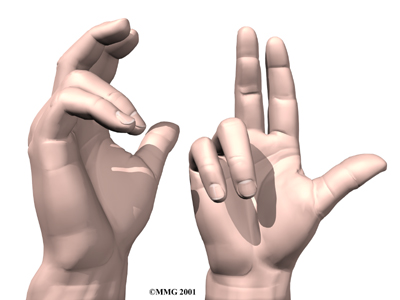
The amount you are able to bend your finger is called
flexion. The amount you are able to straighten the
finger is called extension. Both are measured in
degrees. Normally, the fingers will straighten out
completely. This is considered zero degrees of flexion (no
contracture). As the contracture causes your finger to bend
more and more, you will lose the ability to completely
straighten out the affected finger. How much of the ability
to straighten out your finger you have lost is also measured
in degrees.
Measurements taken at later follow-up visits will tell
how well treatments are working or how fast the disorder is
progressing. The progression of the disorder is
unpredictable. Some patients have no problems for years, and
then suddenly nodules will begin to grow and their finger
will begin to contract.
The tabletop test may also done. The tabletop test
will show if you can flatten your palm and fingers on a flat
surface. You can follow the progression of the disorder by
doing the tabletop test yourself. Your doctor will tell you
what to look for and when you should return for a follow-up
visit.
Treatment
What can be done for the condition?
There are two types of treatment for Dupuytren's
contracture: surgical and nonsurgical. The best course of
treatment is determined by how far the contractures have
advanced.
Nonsurgical Treatment
In the early stages of this disorder, frequent
examination and follow-up is recommended. Your doctor may
inject cortisone into the painful nodules. Cortisone can be
effective at temporarily easing pain and inflammation. Heat
and stretching treatments given by a physical or
occupational therapist may also be prescribed to control
pain and to try to slow the progression of the
contracture.
Treatment also consists of wearing a splint that keeps
the finger straight. This splint is usually worn at
night.
The nodules of Dupuytren's contracture are almost always
limited to the hand. If you receive regular examinations and
follow your doctor's advice, you may be able to slow the
problems caused by this disorder. However, Dupuytren's
contracture is known to progress, so surgery may be needed
at some point to release the contracture and to prevent
disability in your hand.
Surgery
No hard and fast rule exists as to when surgery is
needed. Surgery is usually recommended when the joint at the
knuckle of the finger reaches 30 degrees of flexion. When
patients have severe problems and require surgery at a
younger age, the problem often comes back later in life.
When the problem comes back or causes severe contractures,
surgeons may decide to fuse the individual finger joints
together. In the worst case, amputation of the finger may be
needed if the contracture restricts the nerves or blood
supply to the finger.
Surgery for the main knuckle of the finger (at the base
of the finger) has better long-term results than when the
middle finger joint is tight. Tightness is more likely to
return after surgery for the middle joint.
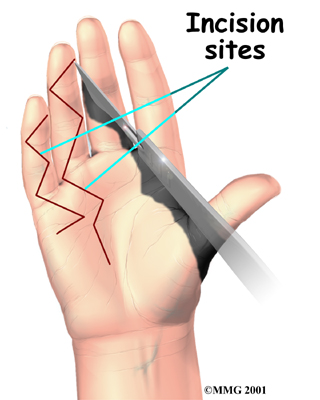 Tissue
Release Tissue
Release
The goal of tissue release surgery is to release the fibrous attachments between the palmar
fascia and the tissues around it, thereby releasing the
contracture. Once released, finger movement should be
restored to normal. If the problem is not severe, it may be
possible to free the contracture simply by cutting the cord
under the skin. If the palmar fascia is more involved and
more than one finger is bent, your surgeon may take out the
whole sheet of fascia. Palmar Fascia Removal
Removal of the entire palmar fascia will usually give a very good
result. The cure is often permanent but depends a great deal
on the success of doing the physical or occupational therapy
as prescribed. Little ill effect is caused by removing the
entire palmar fascia, although the fingers may bend backward
slightly more than normal. If you decide to have this
surgery, you must commit to doing the therapy needed to make
your surgery as successful as possible. Skin Graft
Method
A skin graft may be needed if the skin surface has
contracted so much that the finger cannot relax as it should
and the palm cannot be stretched out flat. Surgeons graft
skin from the wrist, elbow, or groin. The skin is grafted
into the area near the incision to give the finger extra
mobility for movement.
Related Document: A
Patient's Guide to Dupuytren's Contracture
Surgery
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
The ability of nonsurgical treatments to slow or actually
reverse the contracture is not all that promising. The
contracture usually requires surgery at some point. Heat,
stretching, and a finger splint seem to help the most. These
treatments may be directed by a physical or occupational
therapist. Sessions may be scheduled for a few visits per
week up for up to six weeks, but after that, you'll probably
be instructed to continue using the splint and doing the
stretches as part of a home program for several months.
After Surgery
Your hand will be bandaged with a well-padded dressing
and a splint for support after surgery. Physical or
occupational therapy sessions may be needed after surgery
for up to six weeks. Visits will include heat treatments,
soft tissue massage, and vigorous stretching. Therapy
treatments after surgery can make the difference in a
successful result after surgery. |