A Patient's Guide to Osgood-Schlatter Lesion of the
Knee
Introduction
An Osgood-Schlatter lesion involves pain and
swelling in the small bump of bone on the front of the
tibia (shinbone), right below the kneecap. It occurs
in children and adolescents. The problem affects the area
where bone growth occurs. Too much stress on the growing
bone causes the pain and swelling. The pain often worsens
with activity and eases with rest. Fortunately, the
condition is not serious. It is usually only temporary.
The condition is the most frequent cause of knee pain in
children between the ages of 10 and 15. The problem used to
happen mostly in boys. But with more girls playing sports,
boys and girls are now affected equally. Because girls'
skeletons begin to mature earlier than boys, girls tend to
have this condition when they are one to two years younger
than boys. Kids who play sports have this condition 20
percent more often than nonathletes. And the lesion seems to
run in families; when one child is affected, there's a 30
percent chance a sibling will have it, too.
This guide will help you understand
- why the condition develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What part of the knee is affected?
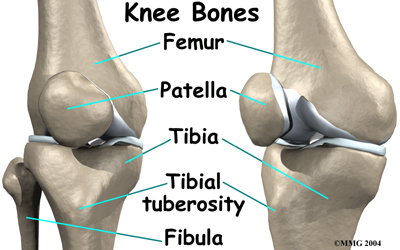
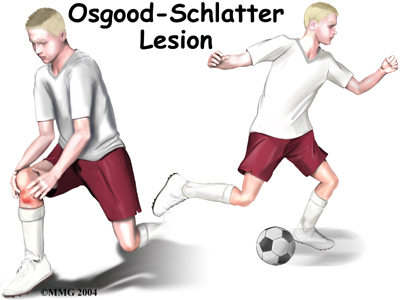
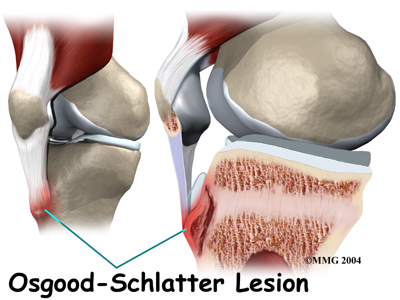
The Osgood-Schlatter lesion affects the tibial
tuberosity. The tibial tuberosity is the bump on the top
of the tibia (shinbone) where the patellar tendon
connects. Tendons connect muscles to bones. The
patellar tendon stretches over the top of the patella
(kneecap). The patellar tendon connects the large
quadriceps muscle on the front of the thigh to the
tibial tuberosity. As the quadriceps muscle works, it pulls
on the patellar tendon and extends (straightens) the knee
joint.
A small bursa sometimes develops where the
patellar tendon meets the tibial tuberosity. A bursa is a normal structure that often forms in areas
where friction occurs, such as between muscles, tendons, and
bones. A bursa is a thin sac of tissue filled with fluid.
The fluid lubricates the area and reduces friction.
Related Document: A
Patient's Guide to Knee Anatomy
Causes
How did this problem develop?
Osgood-Schlatter lesions fit in a category of bone
development disorders known as osteochondroses.
(Osteo means bone, and chondro means
cartilage.) In normal development, specialized bone growth centers (called growth plates)
change over time from cartilage to bone. The growth centers
expand and finally unite. This is how bones grow in length
and width. Bone growth centers are located throughout the
body.
Children with bone development problems in one area are
likely to develop similar problems elsewhere. For example,
among young athletes with growth plate problems in the back
of the heel (Sever's syndrome), about two-thirds also
develop an Osgood-Schlatter lesion. Children who have an
Osgood-Schlatter lesion also have a small chance of problems
at the top of the patellar tendon, where it attaches to the
bottom tip of the kneecap. This condition is known as
Sinding-Larsen-Johansson disorder.
Related Document: A
Patient's Guide to Sever's Syndrome
Related Document: A
Patient's Guide to Jumper's Knee in Children and
Adolescents
The main cause of Osgood-Schlatter lesions is too much
tension in the patellar tendon. The tension can come from
overuse from sports activity and from growth spurts. Usually
both happen together. Both put extra stress on the tibial
tuberosity.
During growth spurts, the tendon may not be able to keep
up with the growth of the lower leg. The tendon becomes too
short. It constantly pulls at the tibial tuberosity. Tension
from sports activity comes from overuse. When the quadriceps
muscle on the front of the thigh works, it pulls on the
patellar tendon. The tendon in turn pulls on the tibial
tuberosity. If the tension is too great and occurs too often
while the bone is developing, it can pull the growth area of
the tibial tuberosity away from the growth area of the
shinbone.
The bump forms because the separated growth plates keep growing and expanding. The area
between the bone fragments fills in with new tissue, either
cartilage or bone. The new tissue causes the tibial
tuberosity to become enlarged and painful.
Another possible cause of Osgood-Schlatter lesions is
abnormal alignment in the legs. Kids who are knock-kneed or
flat-footed seem to be most prone to the condition. These
postures put a sharper angle between the quadriceps muscle
and the patellar tendon. This angle is called the Q-angle. A large Q-angle puts more tension on the
bone growth plate of the tibial tuberosity, increasing the
chances for an Osgood-Schlatter lesion to develop. A
high-riding patella, called patella alta, is also
thought to contribute to development of Osgood-Schlatter
lesions.
Symptoms
What does an Osgood-Schlatter lesion feel like?
In an Osgood-Schlatter lesion, the tibial tuberosity will
probably be enlarged and painful. It hurts when bumped. It
also hurts when pressure is put on it, such as when
kneeling. Activities like running, jumping, climbing, and
kicking may hurt because of the tension of the patellar
tendon pulling on the tibial tuberosity.
Symptoms generally go away gradually over a period of one
to two years. However, the condition may leave a permanent,
painless bump below the knee. The area may always be tender.
Many adults who had a lesion as a child still have pain when
kneeling on that knee.
Complications can occur if the area between the bone
fragments fills in with cartilage rather than bone.
Normally, the bone growth plates join together with solid
bone in between. If cartilage fills in the space, the
condition is called a nonunion,.
Diagnosis
How do doctors diagnose the condition?
A doctor can usually make the diagnosis from the history
and physical examination. The doctor will want to know the
child's age and activity level, and whether there are any
siblings who've had an Osgood-Schlatter lesion.
The doctor will press on and around the patella and
patellar tendon to see if there is any tenderness. The
doctor will compare the sore knee and the healthy knee. The
doctor may also ask the patient to straighten the knee
against resistance. This makes the quadriceps muscle work,
putting tension on the patellar tendon. Pain during this
test can help the doctor make the diagnosis of an
Osgood-Schlatter lesion.
The history and physical examination are usually the only
tests necessary, but sometimes an X-ray is ordered. A knee
X-ray may show a raised area of irregular bone in the tibial
tuberosity. Most often it will show swelling in the soft
tissues in front of the tibial tuberosity. In more severe
cases, the X-ray may show small bony fragments that are
separated from the rest of the tibial tuberosity.
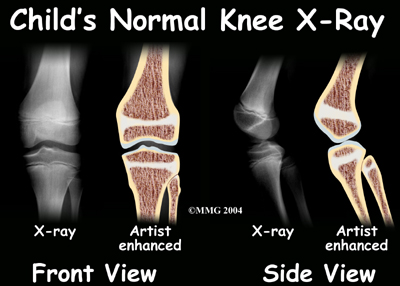
An X-ray is necessary if the tibial tuberosity hurts
after an injury such as a fall. In this case, the X-ray will
help the doctor see if the tibial tuberosity fractured as a
result of the trauma.
Treatment
What can be done for the problem?
Nonsurgical Treatment
The passing of time may be all that is needed. It takes
one to two years for the bone growth plates of the tibial
tuberosity to grow together and form one solid bone. When
this occurs, symptoms usually go away completely.
In some cases, the patient may need to stop sport
activities for a short period. This gets the pain and
inflammation under control. Usually patients don't need to
avoid sports for a long time. It is unlikely that the bone
will completely separate, so not all athletes need to
completely avoid sports.
The doctor may prescribe anti-inflammatory medicine to
help reduce swelling. Physical therapists might use ice,
heat, or ultrasound to control inflammation and pain. A variety of pads, straps, and sleeves are available
that can help keep pain to a minimum. For example, wearing a
knee pad cushions the sore area while kneeling.
As symptoms ease, the physical therapist works on
flexibility, strength, and muscle balance in the knee.
Posture exercises can help improve knee alignment. The
therapist may also design special shoe inserts, called
orthotics, to support flat feet or to correct
knock-kneed posture.
Cortisone injections are commonly used to control pain
and inflammation in other types of injuries. However, a
cortisone injection is usually not appropriate for
Osgood-Schlatter lesions. Cortisone injections haven't shown
consistently good results for this condition. There is also
a high risk that the cortisone will cause the patellar
tendon to rupture.
Severe pain and problems may require a knee brace or cast
for up to six weeks. The goal is to stop the knee from
moving so that inflammation and pain go away.
Surgery
Surgery is not considered unless bone growth is complete
and symptoms are still bothersome despite nonsurgical
treatments. Even then, surgery for an Osgood-Schlatter
lesion is rarely recommended.
When surgery is needed, the usual operation involves
removing the raised area of the tibial tuberosity, the
bursa, and irritated tissue nearby. The surgeon makes a
small incision down the front of the lower knee, just over
the tibial tuberosity. The patellar tendon is split in half.
Retractors are used to pull the skin and the patellar tendon
apart. This makes it easy for the surgeon to see and work on
the tibial tuberosity. The surgeon uses an osteotome
to cut away the raised area of the tibial tuberosity. Care
is taken while removing the bursa and nearby tissue.
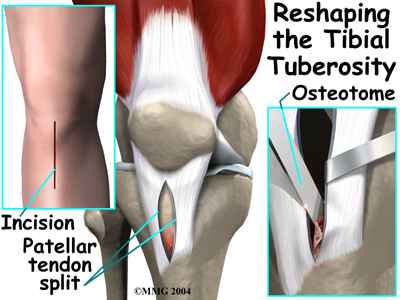
The retractors are removed. The cut edges of the patellar
tendon are brought together. Scar tissue eventually binds
the edges back together. To complete the operation, the
surgeon stitches up the skin.
Rehabilitation
What can be expected from treatment?
Nonsurgical Rehabilitation
With nonsurgical rehabilitation, the goal is to reduce
pain and inflammation. These measures can help. However,
most Osgood-Schlatter lesions still get better over time, as
the bones mature.
Some doctors have their patients work with a physical
therapist. Therapists work on the possible causes of the
problem. For example, flexibility exercises for the
hamstring and quadriceps muscles can help reduce tension in
the patellar tendon where it attaches to the tibial
tuberosity. Orthotics are sometimes issued to put the leg
and knee in good alignment. Strengthening exercises to
improve muscle balance can help the kneecap move correctly
during activity. Therapists work with athletes to improve
form and to reduce knee strain during sports.
When symptoms are especially bad, patients may be
instructed to avoid any activity that makes their pain
worse, including sports. In severe cases, bracing or casting
may be needed for up to six weeks.
After Surgery
After surgery, daily activities can be resumed gradually.
The knee should be propped up routinely during the day to
help reduce swelling and throbbing. Medicines should be
taken exactly as prescribed by the surgeon.
The surgeon may recommend using crutches or a cane for
awhile. Vigorous activities and exercise should be avoided
for six weeks after surgery. Athletes should not take part
in high-level sports for two to three months. Some surgeons
have their patients attend physical therapy after
surgery. |