A Patient's Guide to Trigger Finger and Trigger
Thumb
Introduction
Trigger finger and trigger thumb are
conditions affecting the movement of the tendons as
they bend the fingers or thumb toward the palm of the
hand. This movement is called flexion.
This guide will help you understand
- how trigger finger and trigger thumb develop
- how doctors diagnose the condition
- what can be done for the problem
Anatomy
Where does the condition develop?
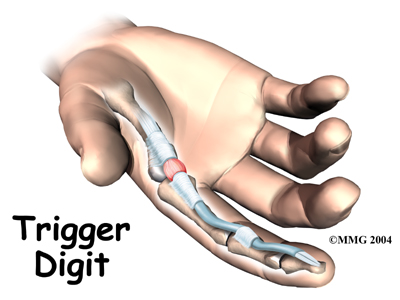
The tendons that move the fingers are held in place
on the bones by a series of ligaments called pulleys.
These ligaments form an arch on the surface of the
bone that creates a sort of tunnel for the tendon to
run in along the bone. To keep the tendons moving
smoothly under the ligaments, the tendons are wrapped
in a slippery coating called tenosynovium.
The tenosynovium reduces the friction and allows the
flexor tendons to glide through the tunnel formed by
the pulleys as the hand is used to grasp
objects.
Related Document: A
Patient's Guide to Hand Anatomy
Causes
Why do I have this problem?
Triggering is usually the result of a thickening in
the tendon that forms a nodule,
or knob. The pulley ligament may thicken as well. The
constant irritation from the tendon repeatedly sliding
through the pulley causes the tendon to swell in this
area and create the nodule. Rheumatoid arthritis,
partial tendon lacerations, repeated trauma from
pistol-gripped power tools, or long hours grasping a
steering wheel can cause triggering. Infection or
damage to the synovium causes a rounded swelling
(nodule) to form in the tendon.
Triggering can also be caused by a congenital
defect that forms a nodule in the tendon. The
condition is not usually noticeable until infants
begin to use their hands.
Symptoms
What does a trigger finger or thumb feel like?
The symptoms of trigger finger or thumb include
pain and a funny clicking sensation when the finger or
thumb is bent. Pain usually occurs when the finger or
thumb is bent and straightened. Tenderness usually
occurs over the area
of the nodule, at the bottom of the finger or
thumb. The clicking sensation occurs when the nodule
moves through the tunnel formed by the pulley
ligaments. With the finger straight, the nodule is at
the far edge of the surrounding ligament. When the
finger is flexed, the nodule passes under the ligament
and causes the clicking sensation. If the nodule
becomes too large it may pass under the ligament, but
it gets stuck at the near edge. The nodule cannot move
back through the tunnel, and the finger is locked in
the flexed
trigger position.
Diagnosis
How do doctors identify the condition?
The diagnosis of trigger finger and thumb is
usually quite obvious on physical examination. Usually
a palpable click can be felt as the nodule snaps under
the first finger pulley. If the condition is allowed
to progress, the nodule may swell to the point where
it gets caught and the finger is locked in a bent, or
flexed, position. No special tests or X-rays are
required.
Treatment
What can be done for the condition?
Nonsurgical Treatment
Treatments provided by a physical or occupational
therapist may be effective when triggering has been
present for less than four months. Therapists often
build a splint to hold and rest the inflamed area.
Special exercises are used to encourage normal gliding
of the tendon. You might be shown ways to change your
activities to prevent triggering and to give the
inflamed area a chance to heal. Therapy sessions
sometimes include iontophoresis, which uses a
mild electrical current to push anti-inflammatory
medicine to the sore area. This treatment is
especially helpful for patients who can't tolerate
injections.
A cortisone
injection into the tendon sheath may be needed to
decrease the inflammation and shrink the nodule. This
can help relieve the triggering, but the results may
be short lived. A splint may be used after the
injection to rest the tendon and help decrease the
inflammation and shrink the nodule.
Surgery
The usual solution for treating a trigger digit is
surgery to open the pulley that is obstructing the
nodule and keeping the tendon from sliding smoothly.
This surgery can usually be done as an outpatient
procedure, meaning you can leave the hospital the same
day.
.jpg)
The surgery can be done using a general
anesthetic (one that puts you to sleep) or a
regional anesthetic. A regional anesthetic
blocks the nerves going to only a portion of the body.
Injection of medications similar to lidocaine are used
to block the nerves for several hours. This type of
anesthesia could be an axillary block (only the
arm is asleep) or a wrist block (only the hand
is asleep). The surgery can also be performed by
simply injecting lidocaine around the area of the
incision.
Once you have anesthesia, your surgeon will make
sure the skin of your palm is free of infection by
cleaning the skin with a germ-killing solution. An
incision will be made in the skin. There are several
types of incisions that can be made, but most are made
along the natural creases and lines in the hand. This
will help make the scar less noticeable once the hand
is healed.
The skin and fascia are separated so the doctor can
see the tendon pulley. Special care is taken not to
damage the nearby nerves and blood vessels.
Next, your surgeon carefully divides the tendon
pulley. Once the tendon pulley has been separated, the
skin is sewn together with fine stitches.
Rehabilitation
What should I expect following treatment?
Nonsurgical Rehabilitation
When triggering has been present for more than four
months, nonsurgical treatment is usually short-lived.
You may get some relief of symptoms with a cortisone
injection. If you wear a splint, the nodule may shrink
temporarily, but patients often end up needing surgery
for this problem.
After Surgery
You'll wear a bandage over the area after surgery
until the stitches are removed. You will probably have
a fairly large padded bandage on your hand when you
return from surgery. This is to provide gentle
compression and reduce the bleeding and swelling that
occurs immediately after surgery. This can be removed
fairly quickly, and usually only a bandage is required
after the first 24 to 48 hours. You'll begin gentle
range-of-motion exercises a few days after
surgery.
Most patients won't need to participate in a formal
rehabilitation program unless the finger or thumb was
locked for a while before surgery. In these cases, the
finger or thumb may not straighten out right away
after the surgery. A physical or occupational
therapist may apply a special brace to get the finger
or thumb to straighten. The therapist may also apply
heat treatments, soft-tissue massage, and hands-on
stretching to help with the range of motion.
Some of the exercises you'll begin to do are to
help strengthen and stabilize the muscles and joints
in the hand. Other exercises are used to improve fine
motor control and dexterity. You'll be given tips on
ways to do your activities while avoiding extra strain
on the healing tendon. You may need to return to
therapy two to three sessions each week for up to six
weeks. |