Awareness of Axial Spondyloarthritis Among Chiropractors
and Osteopaths: Findings From a UK Web-based SurveyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Rheumatol Adv Pract. 2019 (Sep 30); 3 (2): rkz034 ~ FULL TEXT
OPEN ACCESS Cee Y Yong, Jill Hamilton, Jatinder Benepal, Katie Griffiths, Zoë E Clark, Amanda Rush, Raj Sengupta, Jane Martindale, and Karl Gaffney
Department of Rheumatology,
North West Anglia NHS Foundation Trust,
Huntingdon.
OBJECTIVE: Chiropractors and osteopaths are important professional partners in the management of axial spondyloarthritis (axSpA). In view of recent advances in diagnosis and treatment, we sought to understand their current knowledge and working practices.
METHODS: A Web-based survey was advertised to chiropractors and osteopaths via the Royal College of Chiropractors and the Institute of Osteopathy.
RESULTS: Of 382 completed responses [237 chiropractors (62%) and 145 osteopaths (38%)], all were familiar with AS, but only 63 and 25% were familiar with the terms axSpA and non-radiographic axSpA, respectively. Seventy-seven per cent were confident with inflammatory back pain. Respondents routinely asked about IBD (91%), psoriasis (81%), acute anterior uveitis (49%), peripheral arthritis (71%), genitourinary/gut infection (56%), enthesitis (30%) and dactylitis (20%). Eighty-seven per cent were aware of the association between axSpA and HLA-B27. Only 29% recognized that axSpA was common in women. Forty per cent recommend an X-ray (pelvic in 80%) and, if normal, 27% would recommend MRI of the sacroiliac joints and whole spine. Forty-four per cent were aware of biologic therapies. Forty-three per cent were confident with the process of onward referral to rheumatology via the general practitioner (GP). The principal perceived barrier to onward referral was reluctance by the GP to accept their professional opinion.
CONCLUSION: Overall knowledge of ankylosing spondylitis is good, but the term axSpA is poorly understood. Specific learning needs include gender preponderance, awareness of acute anterior uveitis and the availability of biological therapies. There is lack of confidence in the onward referral process to rheumatology via the GP.
KEYWORDS: acute anterior uveitis; ankylosing spondylitis; axial spondyloarthritis; back pain; chiropractor; osteopath; survey
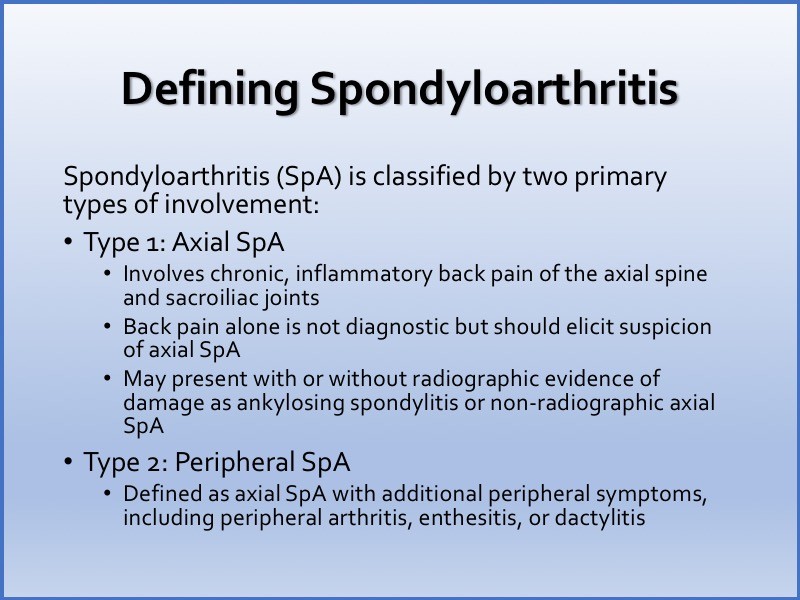
Edirorial Comment: Spondyloarthritis (SpA) is a group of chronic inflammatory diseases of autoimmune nature sharing common clinical and genetic features, such as involvement of the axial skeleton (sacroiliac joints and spine), a certain pattern of peripheral joint involvement (usually asymmetric monoarthritis or oligoarthritis predominantly affecting the joints of the lower extremities), the presence of enthesitis, dactylitis, typical extra-articular manifestations such as acute anterior uveitis, psoriasis and inflammatory bowel disease (i.e. Crohn’s disease and ulcerative colitis), and association with HLA-B27 antigen.
Current classification of SpA relies on the predominant clinical manifestation: either axial or peripheral [Rudwaleit et al. 2011]. Axial SpA (axSpA) is characterized by predominant involvement of the spine and/or sacroiliac joints: ankylosing spondylitis (AS), nonradiographic axial Spa (nr-axSpa, without definite sacroiliitis on X-ray), certain forms of psoriatic arthritis and reactive arthritis with axial involvement, and arthritis associated with inflammatory bowel disease.
Importantly, nr-axSpA and AS are considered nowadays as two stages of one disease (axSpA) [Rudwaleit et al. 2005], although there are patients with an abortive course of the disease who remain at the nonradiographic stage without progression to established AS.
In peripheral SpA, peripheral arthritis, enthesitis and/or dactylitis dominate in the clinical presentation setting [Rudwaleit et al. 2011]. Reactive arthritis, psoriatic arthritis, arthritis associated with inflammatory bowel disease and certain forms of undifferentiated (oligo)arthritis could be generally classified as a peripheral SpA.
FROM: Axial Spondyloarthritis: Is There a Treatment of Choice?
Ther Adv Musculoskelet Dis. 2013 (Feb); 5 (1): 45–54
From the FULL TEXT Article:
Introduction
Axial spondyloarthritis (axSpA) is a chronic inflammatory arthritis involving the spine and sacroiliac joints. In 2009, the Assessment of SpondyloArthritis international Society (ASAS) published the classification criteria for axSpA, encompassing both AS and non-radiographic axSpA. [1] The prevalence of axSpA in a primary care population in the UK was found to be 0.3% using ASAS criteria. [2]
Diagnosis of axSpA can be difficult, and therefore, it is important to maintain a high index of suspicion in order to reduce the delay to diagnosis, which currently stands at 8.5 years in the UK. [3] Typically, symptoms start in the second or third decade [4], and consequently, patients often endure intolerable symptoms during a formative phase of life when they are attempting to establish careers and relationships. Moreover, people have described having to fight to get their diagnosis, which has been upsetting, distressing and disheartening and resulted in feelings of anger and frustration. [5]
Many of these patients suffer from work disability, with almost one-third of patients unable to work and an additional 15% reporting changes to their work because of AS. [6] In the past, the treatment of AS was limited to NSAIDs, CSs and conventional synthetic DMARDs, which were often inadequate or ineffective. [7] Since the early 2000s, the introduction of TNF inhibitors and IL-17 inhibitors has revolutionized treatment and been shown to improve disease outcomes significantly. [8, 9] Patients with shorter disease duration have also been shown to have a better response to treatment, and therefore, early diagnosis is extremely important. [10]
Awareness of axSpA among UK medical professionals in primary and secondary care is variable and often poor. [11, 12] Some of the reasons contributing to the delayed diagnosis include difficulty in distinguishing inflammatory back pain from other types of back pain and lack of awareness of extra-articular manifestations. Consequently, patients may not be investigated appropriately or referred to rheumatologists. [3] The commonest presenting symptom of axSpA is chronic back pain, with many patients self-referring to an osteopath or chiropractor for advice and treatment.
Osteopaths take a holistic view of the body structure and function to treat a variety of medical conditions based on the principle that the well-being of an individual depends on the skeleton, muscles, ligaments and connective tissues functioning smoothly together. [13] They use manual therapy, exercise and health advice to promote the optimal environment for health. [13] All osteopaths in the UK are regulated by law through the General Osteopathic Council and recognized by the National Health Service (NHS) England as an allied health profession. [13, 14] They are trained to degree level and must have a minimum of 1000 patient-contact hours before qualification. There are currently >5300 osteopaths on the UK Statutory Regulator Register. [14]
Chiropractic is a health profession concerned with the diagnosis and treatment of mechanical disorders of the musculoskeletal system and the effects of these disorders on the function of the nervous system and the general health. They emphasize manual treatments, including spinal adjustment and other joint and soft tissue manipulation. [15] Chiropractors are trained to a degree level before registration with the General Chiropractic Council. Many chiropractors further their studies at Masters level in areas of special interest, such as sport, and some undertake professional doctorate or PhD studies. All chiropractors in the UK are regulated by the General Chiropractic Council, and there are currently 3,239 chiropractors registered on the statutory Chiropractic Register in the UK. [16]
A UK study has identified that 30% of newly diagnosed axSpA patients have seen either an osteopath or a chiropractor before diagnosis [17]; therefore, it is essential that these important groups of regulated health-care professionals have a comprehensive understanding of the condition in order to identify the symptoms and signs early and direct referral to rheumatology in order to establish a diagnosis and provide effective therapy.
In this survey, we sought to understand current knowledge of axSpA and working practices of chiropractors and osteopaths working in the UK.
Methods
The survey comprised 30 open and closed questions relating to the background of the health professionals, disease terminology, symptoms recognition, clinical features, investigations, treatment, and the onward referral process to rheumatologists via general practitioners (GPs). This survey materials were developed by the study team, who have the following professional backgrounds; rheumatology (3), osteopathy (2) and chiropractic (2). This study did not require ethical approval.
The first question on the survey was, ‘Are you a practising osteopath or chiropractor?’, in order to verify the professional identity of the respondent. The survey was administered by survey monkey and advertised to professional members via the Royal College of Chiropractors and Institute of Osteopathy using online mechanisms including e-news and promotion by social media for a period of 5 weeks in June and July 2018.
The Institute of Osteopathy is the professional body representing osteopaths in the UK, and it represents >70% of UK registered osteopaths. [18] The Royal College of Chiropractors is an apolitical professional membership body representing chiropractors and currently has >1,500 UK members [19].
Results
Demographics
Three hundred and eighty-two completed responses were received within 1 month; 237 chiropractors (62%) and 145 osteopaths (38%). The demographics of the responders were 59% female, 81% between 30 and 59 years of age, and 63% practicing for >10 years. There was a wide geographical spread, with the largest proportions from the south west (22%) and south east (21%). Thirty-eight per cent of respondents worked as sole practitioners, 30% in group practice, and 32% in a multidisciplinary clinic. Seventy-two per cent reported that between 20 and 60% of their patients presented with chronic back pain. A majority (59%) saw between 1 and 5 patients with chronic back pain per day, and 30% between 6 and 15.
Terminology
Regarding disease terminology, all respondents were familiar with the term AS, and 99% were confident with their understanding, 63% were familiar and 57% confident with their understanding of axSpA, and 25% were familiar and 22% confident with their understanding of non-radiographic axSpA.
Symptom recognition

Table 1

Table 2 Seventy-seven per cent were confident with the concept of inflammatory back pain, 19% somewhat confident, and 4% not confident. The results for awareness of individual features of inflammatory back pain are outlined in Table 1. Fifty-two per cent would also consider localized spinal tenderness as important, and 16% radicular pain. Regarding extra-articular manifestations and peripheral musculoskeletal manifestations, the proportion of respondents who would routinely ask about or examine for the features are shown in Table 2. In addition, 79% routinely asked about a family history of SpA.
Twenty-nine per cent recognized that axial spondyloarthritis (axSpA) was common in women, and 87% were aware of the association between axSpA and HLA-B27. Thirty-three per cent knew that >60% of patients are HLA-B27 positive, and 38% were unsure.
Investigations
Fifty-six per cent would enquire about inflammatory markers (ESR or CRP), and 67% would not exclude axSpA if the markers were normal. Forty per cent would recommend an X-ray for patients with suspected axSpA; 80% pelvic, 71% lumbar spine, 38% thoracic spine and 27% cervical. If the X-ray was normal, 50% would recommend an MRI of the lumbar spine and sacroiliac joints; 27% whole spine and sacroiliac joints; 10% CT of the lumbar spine and sacroiliac joints; 10% isotope bone scan; and 10% US of the sacroiliac joints.
Treatment
Forty-four per cent of respondents were aware of the availability of biologic therapies to treat axSpA. The most common themes that emerged from the open question regarding any specific need to improve confidence in treating axSpA were as follows: more in-depth knowledge on treatment; more information on signposting; more up-to-date knowledge on the latest developments; and help with forging better relationships with GPs to ease the issues with the referral pathway.
Referral
On a weighted average scale, respondents indicated a confidence level of 3.2 out of 5 with the onward referral via GPs; 43% were either confident or very confident. Sixty-one per cent routinely checked the outcomes of their recommendation for onward referral; 87% with the patient, 12% with the GP, and 1% with both. An open question asked respondents to comment on barriers to recommending onward referral, with the most common being a reluctance by GPs to accept findings and recommendations from chiropractors and osteopaths, in addition to a general unwillingness by GPs to refer to secondary care. Some commented on their own lack of confidence in their recommendation letters, whereas others found no barriers and saw development of a good relationship and strong communications with the local GPs as fundamental to the acceptance of any recommendations. Seventy-eight per cent were familiar with the National Ankylosing Spondylitis Society (NASS) and 35% referred their patients to NASS for information on axSpA.
Discussion
This survey shows that back pain is a common clinical presentation in both chiropractic and osteopathic practice. The concept of AS is well recognized and understood, but the terms axSpA and non-radiographic axSpA are less well known. This is compatible with a survey of patients and rheumatologists, in which only 44% of patients were aware of the term axSpA and 88% of rheumatologists accepted the term axSpA. [20]
There is a belief that axSpA affects only men. Historically, AS was seen as a predominantly male disease. However, more recent data have shown that axSpA has an equal male-to-female preponderance [1, 21], meaning that it is important to consider this diagnosis in women.
Recognition of the concept and typical characteristics of inflammatory back pain is good except for alternating buttock pain, which was recognized by only 35% of respondents. This was similar to a GP survey undertaken in 2008. [12] Awareness of extra-articular manifestations is also good, but acute anterior uveitis was recognized by only 49% despite the fact that it is the commonest extra-articular manifestation, with a prevalence of ~26%. [22] In a previous survey of GPs, acute anterior uveitis was also the least recognized extra-articular manifestation, meaning that targeted education of health-care professionals on this important extra-articular manifestation is warranted. Recent studies have shown that screening for chronic back pain among patients with acute anterior uveitis could potentially be used as a targeted strategy for the identification of undiagnosed axSpA and shortening the delay to diagnosis. [23, 24] There is also a lack of awareness about the availability of biological therapies. These findings all support the need to update chiropractors and osteopaths on aspects of axSpA.
General practitioners are the gatekeepers for onward referral to rheumatology for diagnosis and long-term management of axSpA. It has previously been shown that there is often a delay between patients presenting to their GP and subsequent onward referral and diagnosis. [25] In our study, we identified that both chiropractors and osteopaths perceive that there is a barrier to onward referral to rheumatologists and that GPs seem reluctant to accept the findings and recommendations of chiropractors and osteopaths. Given the significant delay in the diagnosis of axSpA [3], these barriers need to be overcome, especially given that earlier diagnosis and initiation of therapy translates into better clinical outcomes. [26]
This paper has a number of limitations. Firstly, we acknowledge that we have a relatively small sample size, although there was a wide geographical distribution. Secondly, the responses we received will have been from professionals who are interested in engaging, which might introduce a bias. There is also a potential for recall bias, especially in relationship to situations where there has been a perceived barrier to onward referral. Nonetheless, we consider that these data provide important clinical information that is highly relevant to the diagnosis and optimal management of axSpA patients in the UK.
As a consequence of this survey, NASS has developed the NASS Allies programme in collaboration with the Royal College of Chiropractors and Institute of Osteopathy. [27] A referral template letter has been developed and endorsed by both the Royal College of General Practitioners and the Chartered Society of Physiotherapy in order to facilitate onward referral to rheumatology via the GP. This template was launched at the Primary Care and Public Health Conference 2019 on 15 May 2019. [27] In addition, in order to educate osteopaths and chiropractors, a programme of seminars will be held throughout the UK during 2019–20, and a webinar will be developed.
We recommend that targeted education and training on axSpA be delivered to osteopaths and chiropractors as part of undergraduate and postgraduate training programmes.
Conclusion
AS, but not the wider spectrum of axSpA, is well understood by both chiropractors and osteopaths. The most striking findings were as follows: a belief that axSpA is a disease of men; poor recognition of acute anterior uveitis as an extra-articular manifestation; and the lack of awareness about the availability of biological therapies. Targeted education on the concept and recent advances in axSpA is warranted. The poor acceptance of osteopaths’ and chiropractors’ clinical assessment by GPs was strongly reflected in the lack of confidence around recommending onward referral.
Funding:
Supported by UCB through an educational Grant, UCB has no editorial involvement.
Disclosure statement:
K.G. has received research grants, consultancy and speaker fees from AbbVie, Celgene, Lilly, Pfizer, MSD, Novartis and UCB; J.M. has received honoraria from Abbvie, Pfizer, UCB and Novartis from educational lectures; R.S. has received speaker fees, support for conference attendance and grants from Abbvie, Biogen, Celgene, Novartis, Pfizer and UCB.
References:
Rudwaleit M, van der Heijde D, Landewé R. et al.
The development of assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection.
Ann Rheum Dis 2009;68:777–83Hamilton L, MacGregor AJ, Toms A. et al.
The prevalence of axial spondyloarthritis in the UK: a cross-sectional cohort study.
BMC Musculoskelet Disord 2015;16:392Sykes M, Doll H, Sengupta R, Gaffney K.
Delay to diagnosis in axial spondyloarthritis: are we improving in the UK?
Rheumatology 2015;54:2283–4Feldtkeller E, Khan MA, van der Heijde D. et al.
Age at disease onset and diagnosis delay in HLA-B27 negative vs. positive patients with ankylosing spondylitis.
Rheumatol Int 2003;23:61–6Martindale J, Goodacre L.
The journey to diagnosis in AS/axial SpA: the impact of delay.
Musculoskeletal Care 2014;12:221–31Barlow JH, Wright CC, Williams B, Keat A.
Work disability among people with ankylosing spondylitis.
Arthritis Rheum 2001;45:424–9Van der Heijde D, Ramiro S, Landewé R. et al.
2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis.
Ann Rheum Dis 2017;76:978–91Van der Heijde D, Kivitz A, Schiff MH. et al.
Efficacy and safety of adalimumab in patients with ankylosing spondylitis: results of a multicenter, randomized, double-blind, placebo-controlled trial.
Arthritis Rheum 2006;54:2136–46Baeten D, Sieper J, Braun J. et al.
Secukinumab, an interleukin-17a inhibitor, in ankylosing spondylitis.
N Engl J Med 2015;373:2534–48Rudwaleit M, Listing J, Brandt J, Braun J, Sieper J.
Prediction of a major clinical response (BASDAI 50) to tumour necrosis factor ? blockers in ankylosing spondylitis.
Ann Rheum Dis 2004;63:665–70Mathieson HR, Merashli M, Gaffney K. et al.
Poor awareness of inflammatory back pain and axial spondyloarthritis amongst secondary care specialists.
Clin Rheumatol 2016;35:2627–8Jois RN, Macgregor AJ, Gaffney K.
Recognition of inflammatory back pain and ankylosing spondylitis in primary care.
Rheumatology 2008;47:1364–6NHS England.
The 14 allied health professions.
https://www.england.nhs.uk/ahp/role/
(2 June 2019, date last accessed).General Osteopathic Council.
The General Osteopathic Council regulates osteopaths in the UK.
https://www.osteopathy.org.uk/home
(2 June 2019, date last accessed).General Chiropractic Council.
About chiropractic. https://www.gcc-uk.org/about-us/about-chiropractic/
(10 June 2019, date last accessed).General Chiropractic Council.
Registration statistics. https://www.gcc-uk.org/registration/the-chiropractic-register/registration-statistics.aspx
(10 June 2019, date last accessed).Sengupta R, Cook D, Gaffney K.
The importance of targeting education strategies for complementary therapists dealing with potentially axial spondyloarthritis patients.
Clin Exp Rheumatol 2014;32:803The Institute of Osteopathy.
For osteopaths. https://www.iosteopathy.org/for-osteopaths/
(10 June 2019, date last accessed).Royal College of Chiroprators.
Memberships. https://rcc-uk.org/membership-3/
(10 June 2019, date last accessed).Derakhshan MH, Pathak H, Cook D. et al.
Services for spondyloarthritis: a survey of patients and rheumatologists.
Rheumatology 2018;57:987–96Baumberger H, Khan M. SAT0417
Gradual progressive change to equal prevalence of ankylosing spondylitis among males and females in Switzerland: data from the Swiss ankylosing spondylitis society (SVMB).
Ann Rheum Dis 2017;76:929Stolwijk C, van Tubergen A, Castillo-Ortiz JD. et al.
Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis.
Ann Rheum Dis 2015;74:65–73Haroon M, O'Rourke M, Ramasamy P. et al.
A novel evidence-based detection of undiagnosed spondyloarthritis in patients presenting with acute anterior uveitis: the DUET (Dublin Uveitis Evaluation Tool).
Ann Rheum Dis 2015;74:1990–5Sykes MP, Hamilton L, Jones C. et al.
Prevalence of axial spondyloarthritis in patients with acute anterior uveitis: a cross-sectional study utilising MRI.
RMD Open 2018;4:e000553.Hamilton L, Gilbert A, Skerrett J, Dickinson S, Gaffney K.
Services for people with ankylosing spondylitis in the UK—a survey of rheumatologists and patients.
Rheumatology 2011;50:1991–8Seo MR, Baek HL, Yoon HH. et al.
Delayed diagnosis is linked to worse outcomes and unfavourable treatment responses in patients with axial spondyloarthritis.
Clin Rheumatol 2015;34:1397–405NASS Allies.
https://nass.co.uk/get-involved/campaign-with-us/nass-allies/
(18 June 2019, date last accessed).
Return to LOW BACK PAIN
Since 10-19-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |