

Chiropractic Spinal Manipulation and the Risk for Acute
Lumbar Disc Herniation: A Belief Elicitation StudyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: European Spine Journal 2018 (Jul); 27 (7): 1517–1525 ~ FULL TEXT
Cesar A. Hincapie, J. David Cassidy, Pierre Côté, Raja Rampersaud
Alejandro R. Jadad, George A. Tomlinson
Injury Prevention Research Office, Division of Neurosurgery,
Li Ka Shing Knowledge Institute, St. Michael’s Hospital,
Toronto, Canada
Background Chiropractic spinal manipulation treatment (SMT) is common for back pain and has been reported to increase the risk for lumbar disc herniation (LDH), but there is no high quality evidence about this. In the absence of good evidence, clinicians can have knowledge and beliefs about the risk. Our purpose was to determine clinicians’ beliefs regarding the risk for acute LDH associated with chiropractic SMT.
Methods Using a belief elicitation design, 47 clinicians (16 chiropractors, 15 family physicians and 16 spine surgeons) that treat patients with back pain from primary and tertiary care practices were interviewed. Participants’ elicited incidence estimates of acute LDH among a hypothetical group of patients with acute low back pain treated with and without chiropractic SMT, were used to derive the probability distribution for the relative risk (RR) for acute LDH associated with chiropractic SMT.
Results Chiropractors expressed the most optimistic belief (median RR 0.56; IQR 0.39–1.03); family physicians expressed a neutral belief (median RR 0.97; IQR 0.64–1.21); and spine surgeons expressed a slightly more pessimistic belief (median RR 1.07; IQR 0.95–1.29). Clinicians with the most optimistic views believed that chiropractic SMT reduces the incidence of acute LDH by about 60% (median RR 0.42; IQR 0.29–0.53). Those with the most pessimistic views believed that chiropractic SMT increases the incidence of acute LDH by about 30% (median RR 1.29; IQR 1.11–1.59).
Conclusions Clinicians’ beliefs about the risk for acute lumbar disc herniation (LDH) associated with chiropractic SMT varied systematically across professions, in spite of a lack of scientific evidence to inform these beliefs. These probability distributions can serve as prior probabilities in future Bayesian analyses of this relationship.
Keywords Chiropractic Spinal manipulation Risk Intervertebral disc displacement Bayesian approach Belief elicitation
From the Full-Text Article:
Introduction
Spinal manipulation is commonly used for back pain and considered to be safe, although concern has been raised about its potential link with lumbar disc herniation (LDH) [1, 2]. Several systematic reviews have found that spinal manipulation can benefit low back pain, with little evidence of serious harm [3, 4]. In addition, randomized clinical trial evidence supports the use of spinal manipulation for the treatment of LDH with radiculopathy [5–7]. On the other hand, some believe, on the basis of case reports and small case series, that spinal manipulation is contraindicated for the treatment of disc herniation and could cause it [8–14]. Therefore, a disconnect seems to exist between the scientific evidence and some clinical beliefs in this area.
Understanding of the risk for serious adverse events related to spinal manipulation faces several challenges. First, there has been insufficient study in this area. No valid estimate of the risk for acute disc herniation following chiropractic spinal manipulation treatment is available in the scientific literature. Second, the valid study of uncommon events, such as acute LDH with radiculopathy following spinal manipulation treatment, is limited by the rarity of this outcome. Well-designed prospective studies are difficult to undertake due to the challenge of recruiting and following the numbers of patients needed to ensure that sufficient events are observed. Third, methodological pitfalls exist. For instance, case–control designs based on retrospective measurement of exposure to hypothesized iatrogenic harm are highly susceptible to information biases including recall and observer bias. Fourth, a necessary prerequisite for interest in scientific pursuit is a finding of community uncertainty [15] (a situation where not all within a community of “experts” agree on the potential risk of an intervention).
A Bayesian approach to health services research and evaluation presents an opportunity to advance knowledge despite the above challenges [16, 17]. Bayesian methods start with existing “prior” beliefs, formally quantified as probability distributions, and update these using new data to arrive at “posterior” beliefs, which may be used as the basis for inferential decisions [18]. Quantifying currently held beliefs can determine the magnitude of a potential risk expected by experts and describe the presence of uncertainty, discrepancies or clinical equipoise about an exposure–outcome association. Experts in a field can have knowledge of the risk of using a treatment through years of clinical experience. When quantified, the knowledge gained from their clinical experience can be included in Bayesian models estimating risk and may help to bridge the gap between beliefs and evidence. A particular strength of this approach is that probability distributions obtained through the elicitation of beliefs can be used to augment scarce data [16, 17, 19, 20], and be formally incorporated into Bayesian risk analyses. Beliefs about risk or harm influence clinicians’ practice and may also influence their receptiveness to new research findings. In the absence of risk estimates based on data, experts may be the best currently available source of evidence. Although infrequently used in epidemiologic research, a Bayesian approach may have important utility in the study of treatment-related rare serious adverse events, particularly in the absence of definitive scientific evidence [16, 17, 21, 22].
Our objective was to describe and quantify clinicians’ beliefs about the association between chiropractic spinal manipulation and the development of acute LDH. We elicited beliefs from three groups of clinicians that treat patients with back pain and disc herniation: chiropractors, family physicians and spine surgeons. We hypothesized that beliefs about the risk following chiropractic care would vary by clinician group, with chiropractors believing spinal manipulation to be less risky than spine surgeons.
Methods
Study participants
Since belief elicitation is best conducted through a face-toface interaction between participant and investigator [19, 23], we considered eligible only those participants available for an interview within a 2-h drive of the City of Toronto. Chiropractors were sampled from active registered members with the College of Chiropractors of Ontario within the Greater Toronto Area. Family physicians were sampled from primary care active registered members with the College of Physicians and Surgeons of Ontario who refer to a spine surgery service at a tertiary care hospital in Toronto. Spine surgeons invited to participate were all eligible active members of the Ontario Division of the Canadian Spine Society. We also imposed a requirement (self-reported) that the clinician’s practice involve caring for patients with low back pain and LDH.
There is no consensus on the preferred sampling method or sample size for a belief elicitation study [19, 23, 24]. A systematic review of belief elicitation methods found a median sample size in elicitation studies of 11 participants, and recommended the use of purposive sampling to capture a range of opinions of the target population [23]. We hypothesized that beliefs might vary on the basis of clinician group, years of clinical experience or gender, so in our intended purposive sample of 15 members of each clinician group, we attempted to balance these characteristics.
Study design
We conducted a belief elicitation study using a computer adaptation of a validated approach to belief elicitation that has previously been used with various groups of clinicians [24–26]. A face-to-face interactive interview with each participant was conducted by one interviewer (CAH), using a standardized questionnaire, script and elicitation software (Online Resource 1 and 2). The interview, script and software were pilot tested with a group of ten clinicians (six chiropractors, two family physicians and two spine surgeons) for face and content validity, clarity and time feasibility (≤15-min duration), with good results: 9/10 found the questions clear; 9/10 found the response option easy to use; the median time to completion was 15 min. We obtained ethics approval for our study from the research ethics board of the University Health Network (REB #11-0240-AE).
Belief elicitation interview
The interview incorporated best practices for belief elicitation [19, 23, 24], and began with a short introduction, followed by informed written consent. The participant was then guided through a worked example (Online Resource 1, Example Scenario) of a belief elicitation to introduce the elicitation process and computer software. Following this, beliefs were elicited for two clinical outcome scenarios: acute LDH and acute severe LDH that is surgically managed (we report on the first of these scenarios here; for information on the second scenario, see doctoral thesis [27]). Acute LDH was defined as acute onset of lumbar radiculopathy due to LDH. For each scenario, a participant was asked to consider the following at-risk population: a hypothetical average group of 1000 newly diagnosed acute low back pain patients without current LDH. We used a denominator of 1000 because it is an observable and conceivable sample of patients. This facilitates the probabilistic mental manipulations that have to be made during the elicitation interview, increases the reliability of the elicitation, and reduces some of the common elicitation biases (e.g., tendency to think in terms of percentages) [19, 23, 24].
Each participant was asked to estimate the 2-month cumulative incidence of acute LDH among an average group of 1000 newly diagnosed acute low back pain patients without current LDH that are treated with and without chiropractic care. Chiropractic care was defined as a course of spinal manipulation to the lumbar spine by a chiropractor. Participants were also asked to indicate their uncertainty around their estimate among chiropractic-treated patients by expressing the lower and upper bounds of what they believed to be a plausible range for the incidence. Using the belief elicitation software (detailed below), participants were then asked to indicate the distribution of the weight of their belief along this plausible range.
We also asked participants to categorize their belief regarding the overall effect of chiropractic care, compared to primary medical care (defined as a course of NSAIDs/ painkillers prescribed by a family physician), on the risk of developing acute LDH, using the response options: “decreases the risk,” “no effect on the risk,” or “increases the risk.”
Finally, we recorded other demographic and clinical characteristics of the participants (e.g., gender, age group, clinical background, number of years in practice treating low back pain patients, number of new low back pain patients seen per year) to gather some descriptive information.
Belief elicitation software
We used an open source computer protocol (modified SHELF [28] application in R [29]) that allowed participants to graphically specify a point estimate of incidence and a plausible range of incidence values that they believed likely for acute LDH among patients treated with chiropractic care (Online Resource 3 provides screenshots of the computer interface and details of the modifications we made to the base SHELF software). They indicated their weight of belief for the incidence values along their specified range by allocating 20 virtual “chips”, each representing 5% probability, thereby creating a probability distribution representing 100% probability, from which the software estimated a smooth curve of best fit. This curve provided participants a real-time graphical representation of their probability distributions. Participants were asked to review the placement of chips and the smooth curve to ensure that these accurately reflected their true belief prior to proceeding in the interview.
Statistical analysis
Medians and proportions were used to summarize characteristics of the respondents. On each participant, the distribution of the absolute risk of acute LDH with chiropractic spinal manipulation was converted to the distribution for the relative risk (RR). To estimate the RR, values of the absolute risk of acute LDH among patients treated with chiropractic spinal manipulation (the values on the x-axis of the bottom figure in Online Resource 3) were divided by the point estimate of incidence of acute LDH among untreated patients.
We aggregated the smooth best-fitting curve from each participant to generate an overall summary of belief about the RR. We also aggregated curves within each of the clinician groups. Finally, optimistic and pessimistic probability distributions were estimated by aggregating respondents within the lowest and highest quartiles of mean RR estimates, respectively. For each summary curve, the probability placed on a RR greater than one (RR > 1) was calculated as the area under the curve for RR values greater than 1.
Prespecified secondary analyses were undertaken to describe and quantify beliefs by gender, clinician age (≤50 years and ≥51 years), and years of clinical experience (<12, 12–24 and ≥25). We used R, version 3.1.2 [29] to carry out our statistical analysis.
Role of the funding source
The sponsors of the study had no role in the study design, data collection, data analysis, data interpretation, the writing of the report, or in the decision to submit the report for publication.
Results
Study participants
Of 165 eligible potential participants invited, 87 did not respond and 31 declined to participate (reason not given). Overall participation was 28% (47/165), and ranged from 70% among spine surgeons (16/23), to 37% among chiropractors (16/43), and 15% among family physicians (15/99).

Table 1 Table 1 describes characteristics of the study participants. Spine surgeons were all men and on average older than the other groups. Most participants (94%) reported some formal post-secondary statistical training and had many years of experience treating low back pain patients (median 18; IQR 10–26 years). Chiropractors had slightly less experience (median 13 years) and spine surgeons more (median 23 years).
Clinicians’ beliefs about the baseline risk for acute LDH
The median elicited 2-month incidence of acute LDH among patients with acute low back pain not treated with chiropractic care across all participants was 5.0% (IQR 2.3–10.0%). All three clinician groups expressed very similar beliefs about the baseline risk for acute LDH.
Clinicians’ beliefs about the risk for acute LDH
associated with chiropractic care

Table 2
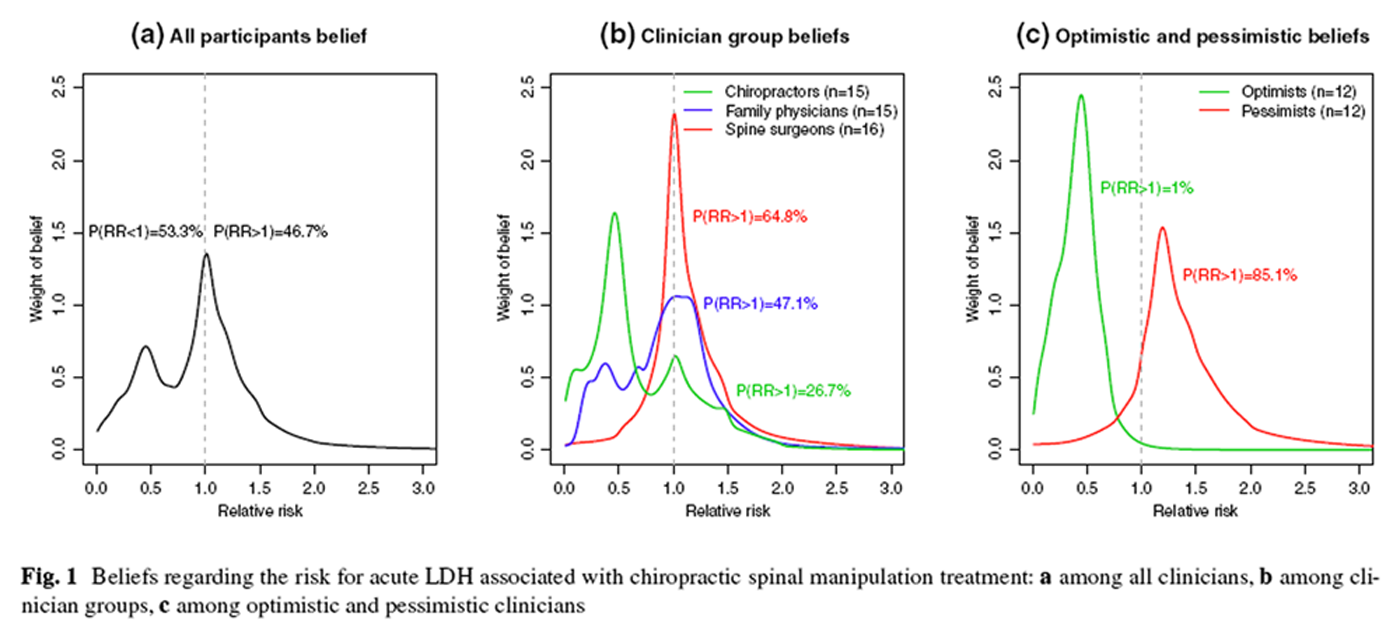
Figure 1 The median RR for acute LDH across all clinicians was 0.97 (IQR 0.57–1.20), with a probability for a RR > 1 of 46.7% (Figure 1a; Table 2). Beliefs varied by clinician group (Fig. 1b), with chiropractors reporting the most optimistic belief (median RR 0.56, IQR 0.39–1.03; probability for a RR > 1 26.7%). Family physicians held a more neutral belief, with a median RR of 0.97 (IQR 0.64–1.21) and probability for a RR > 1 of 47.1% (Table 2). Bimodal probability distributions were observed for both chiropractors and family physicians (Fig. 1b), reflecting the presence of two subgroups for each clinician type: one believing there is a protective effect of spinal manipulation on the risk for acute LDH with radiculopathy, and another believing there is not only little effect on average but also some chance of harm. Spine surgeons reported a slightly more pessimistic belief, with a median RR of 1.07 (IQR 0.95–1.29) and probability for a RR > 1 of 64.8%. The unimodal distribution for the spine surgeons showed them to be a more homogeneous group, which on average, felt there was close to no benefit, but with more chance of harm than benefit.
Optimistic and pessimistic beliefs

Table 3 Optimistic clinicians—those in the lowest quartile of RR estimates—included three family physicians and nine chiropractors. These clinicians expressed a belief that chiropractic spinal manipulation reduces the incidence of acute LDH by about 60% (median RR 0.42; IQR 0.29–0.53) (Figure 1c; Table 2). Pessimistic clinicians—those in the highest quartile of RR estimates—included six spine surgeons, three family physicians and three chiropractors, who believed that chiropractic care increases the incidence of acute LDH by about 30% (median RR 1.29; IQR 1.11–1.59). Compared to optimists, pessimists were more commonly men, older and reported a greater number of new low back patients per year (Table 3). More pessimists than optimists also reported having seen a patient whose disc herniation was attributed to chiropractic spinal manipulation (58 versus 8%).
Beliefs by gender, age groups and years of clinical experience
Table 2 shows that some differences in belief about the risk for acute LDH associated with chiropractic care were found between women (n = 11) and men (n = 35) clinicians, with women reporting a more optimistic belief (median RR 0.77; IQR 0.41–1.10; 34% probability for a RR > 1) and men, a more neutral belief (median RR 1.00; IQR 0.68–1.23; 51% probability for a RR > 1). There were no differences in beliefs according to age group or years of clinical experience treating patients with low back pain (Table 2).
Discussion
This belief elicitation study quantified, described and provided important insights into beliefs about the risk for acute LDH associated with chiropractic spinal manipulation held by clinicians with experience treating patients with back pain and disc herniation. Clinician beliefs about the incidence of acute LDH with and without chiropractic spinal manipulation treatment varied, with interesting and important differences observed across professions and specializations. On average, clinicians believed that the incidence of acute LDH is about the same with and without chiropractic spinal manipulation treatment; in other words, clinicians believed that exposure to chiropractic care has no major effect on the risk for acute LDH. However, it is striking to note the stark difference in beliefs across professions and between optimistic and pessimistic clinicians (Fig. 1). There is a divergence of opinion within these back pain clinicians, indicating the presence of community uncertainty.
Our study advances knowledge of the potential link between chiropractic spinal manipulation and acute LDH in several important ways. First, our study is the first to examine and provide estimates of clinician beliefs regarding this potential exposure–outcome association. There are no published estimates of the association between chiropractic care and the incidence of acute LDH with which to compare our findings. In the absence of estimates of risk based on data, experts may be the best currently available source of evidence. By quantifying currently held clinician beliefs, our results shed light on the magnitude of a potential risk expected by experts and describe the community uncertainty surrounding this relationship. Experts in a field can have knowledge of the risk of using a treatment through years of clinical experience. Beliefs about risk or harm influence clinicians’ practice and will also influence their receptiveness to new research findings. Second, the probability distributions elicited in this study may be relevant and useful to researchers choosing to use a Bayesian approach to investigate this relationship, whereby elicited beliefs in the form of prior probability distributions can be used to augment limited data [19–21, 30, 31]. Finally, our results act as a benchmark against which future quantitative studies could be assessed using Bayesian methods. For example, if a future study found harm associated with spinal manipulation, one could evaluate whether the evidence should be strong enough to convince chiropractors as a group, or, in the whole sample, persons with the most strongly held beliefs about benefit. Likewise, if a future study found benefit associated with SMT, one could assess if the new evidence should be compelling enough to persuade those with the most strongly held beliefs about harm to update their beliefs. The Bayesian approach appears particularly reasonable and appropriate in the context of investigating contentious potential treatmentrelated rare serious adverse events in the absence of definitive scientific data and evidence [16, 17].
Our study has limitations that need to be considered. These mainly relate to characteristics of the study respondents. One of the ongoing debates in the belief elicitation literature is the definition of an “expert” when eliciting expert opinion [19, 23, 24]. As there is no formal definition for back pain clinician expert, we defined an “expert” as a chiropractor, family physician or spine surgeon with a self-reported active practice treating patients with low back pain. The large number of years treating patients with low back pain and large number of new patients with low back pain seen per year (Table 1) supports the notion that the participants were experienced clinicians. However, the overall response rate to our survey was low. If reasons for study participation were associated with beliefs regarding chiropractic care safety, then our findings could be subject to nonresponse bias. We hypothesize that respondents may have had more extreme beliefs than nonrespondents (i.e., those with strong opinions might have been more likely to participate). If this was the case, our findings may overestimate differences between clinician groups and between optimists and pessimists. However, if the propensity to respond was similar in those with extreme positive and extreme negative views, then our average relative risk may be representative of that in the target population. We would have preferred a more balanced study sample with respect to gender and age distribution. However, this was challenging, as Ontario spine surgeons are predominantly male and older compared with the more balanced family physician population and the younger population of chiropractors in the Greater Toronto Area (Table 1). We acknowledge that our outcome measurement did not determine if respondents believed that LDH specifically occurred at the lumbar spinal segment treated with SMT or at a lumbar segment distant from the lumbar spine area treated. Finally, this is an exploratory study involving a relatively small number of clinicians that may not be representative of the clinician source populations. However, our main objective was to describe the beliefs of our study sample and generate hypotheses, rather than to make strong generalizable inferences about beliefs in these healthcare professions.
Our study is part of a growing body of literature on the successful quantification of clinicians’ beliefs about the safety or effectiveness of an intervention or treatment exposure. For example, this method has been used to elicit beliefs regarding: treatment efficacy in pulmonary arterial hypertension [25] and pediatric intestinal failure-associated liver disease [26]; and risk factors for falls in community-dwelling older people [32]. The belief elicitation methodology used in our work can be generalized to the study of many uncommon diseases and conditions [19], and could have potential web-based research applications [33].
A strength of our elicitation procedure is that participants were asked to estimate the incidence of acute LDH with and without chiropractic spinal manipulation treatment, rather than to directly provide their belief about the relative risk. The probability distribution for the relative risk was derived by first obtaining the estimate of risk without chiropractic care and then, with this in mind, obtaining the distribution of incidence with chiropractic care. The elicited incidence with chiropractic care was conditional on the incidence without chiropractic care, which acted as a baseline value. We took this approach because evidence shows that it is much more difficult for respondents to directly specify relative risk distributions as relative risks are not directly observable [19]. A clinician can reflect on knowledge and experience to estimate a frequency representation of the probability for acute LDH, however, it is a much more challenging task to abstract that information and elicit a valid distribution for the ratio of probabilities (i.e., the RR).
Interesting questions remain. What are the reasons for the differences in clinician beliefs? Do these clinicians interpret the same evidence, as limited as it is, differently? Do they see different types of patients, so that their beliefs actually reflect their personal clinical experience? Does their understanding of the pathogenesis of LDH and its associated clinical presentation affect the manner in which different health professionals are likely to view LDH? Does spine surgeons’ experience with the more severe end of the clinical spectrum raise their index of suspicion for viewing spinal manipulation as potentially harmful? Do they have built-in biases based on their professions and specializations? Would similar beliefs be observed in healthcare settings where the education of these clinician groups is more integrated (e.g., Denmark [34], Switzerland [35]), or where family physicians and spine surgeons deliver spinal manipulation? In Germany, for example, general practitioners and ambulatory orthopaedic surgeons are often specially trained in spinal manipulation and offer it to their patients [36]. This highlights the need for future well-designed studies to examine determinants of beliefs, confirm clinicians’ beliefs about the safety of chiropractic spinal manipulation in other settings, and investigate the association between chiropractic care and acute LDH in the population. More research is warranted to better understand the risk–benefit profiles of manual therapeutic interventions for spinal pain and dysfunction [37, 38].
Conclusion
Our study is the first to describe and evaluate clinician beliefs about the association between chiropractic spinal manipulation and the development of acute LDH. We found that beliefs were diverse, with important interprofessional differences. Our probability distributions quantify and describe these differing beliefs and can be used as prior probabilities in Bayesian analyses of this relationship.
Acknowledgements
We thank Drs. Sindhu Johnson and Ivan Diamond for their assistance with the development of the belief elicitation interview and questionnaire. We acknowledge Drs. Jeremy Oakley and Anthony O’Hagan for their development and open source sharing of the SHELF elicitation framework. We thank all the clinician experts who participated in the belief elicitation interviews.
Author contributions
CAH conceived and designed the study, acquired, cleaned and analysed the data, interpreted the results, and drafted and revised the paper. GT conceived and designed the study, analysed the data, interpreted the results, and revised the paper. PC, YRR, ARJ and JDC designed the study, interpreted the results, and revised the paper. CAH acts as guarantor.
Funding sources
Canadian Institutes of Health Research [Grant ID: 200902KPD-205299-111612], and Canadian Chiropractic Research Foundation.
Conflict of interest
All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/coi_disclosure.pdf (available from the corresponding author) and declare: CAH was funded by Fellowship Awards in the Area of Knowledge Translation from Canadian Institutes of Health Research [Grant ID: 200902KPD-205299-111612] and Canadian Chiropractic Research Foundation, PC is funded by a Canada Research Chair in Disability Prevention and Rehabilitation at the University of Ontario Institute of Technology; PC consults for European Spine Society, National Judicial Institute of Canada, Canadian Memorial Chiropractic College, Canadian Chiropractic Protective Association, Society of Musculoskeletal Manual Practitioners of Saskatchewan, Société des experts en évaluation médico-légale du Québec, YRR consults for Medtronic, outside the submitted work; no other relationships or activities that could appear to have influenced the submitted work. The funders played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
References:
Gouveia LO, Castanho P, Ferreira JJ (2009)
Safety of chiropractic interventions: a systematic review.
Spine 34:E405–E413Snelling NJ (2006)
Spinal manipulation in patients with disc herniation: a critical review of risk and benefit.
Int J Osteopath Med 9:77–84Cherkin DC, Sherman KJ, Deyo RA, Shekelle PG (2003)
A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for back pain.
Ann Intern Med 138:898–906Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Van Tulder M, Santaguida L, et. al.
A Systematic Review and Meta-analysis of Efficacy, Cost-effectiveness, and Safety
of Selected Complementary and Alternative Medicine for Neck and Low-back Pain
Evidence-Based Complementary and Alternative Medicine. 2012 (Nov 24); 2012: 953139Santilli V, Beghi E, Finucci S.
Chiropractic Manipulation in the Treatment of Acute Back Pain and Sciatica
with Disc Protrusion: A Randomized Double-blind Clinical Trial
of Active and Simulated Spinal Manipulations
Spine J. 2006 (Mar); 6 (2): 131—137McMorland G, Suter E, Casha S, du Plessis SJ, Hurlbert RJ.
Manipulation or Microdiskectomy for Sciatica?
A Prospective Randomized Clinical Study
J Manipulative Physiol Ther. 2010 (Oct); 33 (8): 576–584Bronfort G, Hondras MA, Schulz CA, Evans RL, Long CR et al (2014)
Spinal Manipulation and Home Exercise With Advice for Subacute
and Chronic Back-related Leg Pain: A Trial With Adaptive Allocation
Annals of Internal Medicine 2014 (Sep 16); 161 (6): 381—391Huang SL, Liu YX, Yuan GL, Zhang J, Yan HW (2015)
Characteristics of lumbar disc herniation with exacerbation of presentation due to spinal manipulative therapy.
Medicine 94:e661Assendelft WJ, Bouter LM, Knipschild PG (1996)
Complications of spinal manipulation: a comprehensive review of the literature.
J Fam Pract 42:475–480Powell FC, Hanigan WC, Olivero WC (1993)
A risk/benefit analysis of spinal manipulation therapy for relief of lumbar or cervical pain.
Neurosurgery 33:73–79Schmidley JW, Koch T (1984)
The noncerebrovascular complications of chiropractic manipulation.
Neurology 34:684–685Morandi X, Riffaud L, Houedakor J, Amlashi SF, Brassier G et al (2004)
Caudal spinal cord ischemia after lumbar vertebral manipulation.
Jt Bone Spine 71:334–337Tamburrelli FC, Genitiempo M, Logroscino CA (2011)
Cauda equina syndrome and spine manipulation: case report and review of the literature.
Eur Spine J 20(Suppl 1):S128–S131Oppenheim JS, Spitzer DE, Segal DH (2005)
Nonvascular complications following spinal manipulation.
Spine J 5:660–667Gifford F (2001)
Uncertainty about clinical equipoise. Clinical equipoise and the uncertainty principles both require further scrutiny.
BMJ 322:795Spiegelhalter DJ (2004)
Incorporating Bayesian ideas into health-care evaluation.
Stat Sci 19:156–174Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR (1999)
Methods in health service research. An introduction to bayesian methods in health technology assessment.
BMJ 319:508–512Spiegelhalter DJ, Rice K (2009)
Bayesian statistics.
Scholarpedia 4:5230O’Hagan A, Buck CE, Daneshkhah A, Eiser JR, Garthwaite PH et al (2006)
Uncertain judgements: eliciting experts’ probabilities.
Wiley, West SussexLilford RJ, Thornton JG, Braunholtz D (1995)
Clinical trials and rare diseases: a way out of a conundrum.
BMJ 311:1621–1625Dunson DB (2001)
Commentary: practical advantages of Bayesian analysis of epidemiologic data.
Am J Epidemiol 153:1222–1226Hampson LV, Whitehead J, Eleftheriou D, Brogan P (2014)
Bayesian methods for the design and interpretation of clinical trials in very rare diseases.
Stat Med 33:4186–4201Johnson SR, Tomlinson GA, Hawker GA, Granton JT, Feldman BM (2010)
Methods to elicit beliefs for Bayesian priors: a systematic review.
J Clin Epidemiol 63:355–369Johnson SR, Tomlinson GA, Hawker GA, Granton JT, Grosbein HA et al (2010)
A valid and reliable belief elicitation method for Bayesian priors.
J Clin Epidemiol 63:370–383Johnson SR, Granton JT, Tomlinson GA, Grosbein HA, Hawker GA et al (2011)
Effect of warfarin on survival in sclerodermaassociated pulmonary arterial hypertension (SSc-PAH) and idiopathic PAH. Belief elicitation for Bayesian priors.
J Rheumatol 38:462–469Diamond IR, Grant RC, Feldman BM, Tomlinson GA, Pencharz PB et al (2014)
Expert beliefs regarding novel lipid-based approaches to pediatric intestinal failure–associated liver disease.
J Parenter Enteral Nutr 38:702–710Hincapié CA (2015)
Chiropractic care and risk for acute lumbar disc herniation: a mixed methods approach.
Dissertation, University of TorontoOakley JE, O’Hagan A (2010)
SHELF: the Sheffield Elicitation Framework (version 2.0).
School of Mathematics and Statistics,
University of Sheffield.
http://tonyohagan.co.uk/shelf
Accessed 19 Dec 2012R Development Core Team (2011)
R: a language and environment for statistical computing. R Foundation for Statistical Computing.
http://www.R-project.org
Accessed 30 Jan 2013Billingham L, Malottki K, Steven N (2012)
Small sample sizes in clinical trials: a statistician’s perspective.
Clin Investig 2:655–657Chaloner K, Rhame FS (2001)
Quantifying and documenting prior beliefs in clinical trials.
Stat Med 20:581–600Deandrea S, Negri E, Ruggeri F (2014)
Integrating clinicians’ opinion in the Bayesian meta-analysis of observational studies: the case of risk factors for falls in community-dwelling older people.
Epidemiol Biostat Public Health (Online) 11:e8909Morris DE, Oakley JE, Crowe JA (2014)
A web-based tool for eliciting probability distributions from experts.
Environ Model Softw 52:1–4Myburgh C, Mouton J (2008)
The development of contemporary chiropractic education in Denmark: an exploratory study.
J Manip Physiol Ther 31:583–592Humphreys BK, Peterson CK, Muehlemann D, Haueter P.
Are Swiss Chiropractors Different Than Other Chiropractors?
Results of the Job Analysis Survey 2009
J Manipulative Physiol Ther 2010 (Sep); 33 (7): 519–535Chenot JF, Becker A, Leonhardt C, Keller S, Donner-Banzhoff N et al (2007)
Use of complementary alternative medicine for low back pain consulting in general practice: a cohort study.
BMC Complement Altern Med 7:42Paige NM, Myiake-Lye IM, Booth MS, et al.
Association of Spinal Manipulative Therapy with Clinical Benefit and Harm
for Acute Low Back Pain: Systematic Review and Meta-analysis
JAMA. 2017 (Apr 11); 317 (14): 1451–1460National Institute for Health and Care Excellence (NICE):
Low Back Pain and Sciatica in Over 16s: Assessment and Management (PDF)
NICE Guideline, No. 59 2016 (Nov): 1–1067
Return to LOW BACK PAIN
Return to DISC HERNIATION
Since 9-19-2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |