

Comparison of Treatment Outcomes in Nonspecific Low-Back
Pain Patients With and Without Modic Changes
Who Receive Chiropractic TreatmentThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther. 2018 (Sep); 41 (7): 561–570 ~ FULL TEXT
Michèle Annen, MChiroMed, Cynthia Peterson, DC, MMedEd, B. Kim Humphreys, DC, PhD
Chiropractic Medicine Department,
Faculty of Medicine, University of Zurich,
Orthopaedic University Hospital Balgrist,
Zürich, Switzerland.
miky.annen@gmail.com
OBJECTIVE: The aim of this study was to determine if there was a difference in outcomes in patients with nonspecific low back pain, both with and without Modic changes (MCs), who received chiropractic care.
METHODS: This prospective outcomes study included 112 patients with low back pain without disc herniation on magnetic resonance imaging. All patients were treated with spinal manipulative therapy. At baseline, the numerical rating scale (NRS) and Bournemouth Questionnaire (BQ) for disability were collected. The NRS, BQ, and Patient's Global Impression of Change (primary outcome) were collected at the follow-up time points of 1 week, 1 month, and 3 months to assess overall improvement. Magnetic resonance imaging scans were analyzed for the presence of MCs and, if present, classified as Modic I or II. The χ2 test was used to compare the proportion of patients reporting clinically relevant "improvement" between patients with and without MCs and between Modic I and Modic II patients. The unpaired Student t test was used to compare NRS and BQ at baseline and change scores at all follow-up time points.
RESULTS: For the primary outcome measure, the proportion of patients reporting relevant "improvement" (Patient's Global Impression of Change), and for the secondary outcome measures (NRS and BQ change scores), there were no significant differences between Modic positive and Modic negative patients or between Modic I and Modic II patients.
CONCLUSION: Neither the presence nor absence of Modic changes (MCs) nor the Modic change category were related to treatment outcomes for patients with low back pain without disc herniation who received chiropractic care.
KEYWORDS: Chiropractic; Diagnostic Imaging; Manipulation, Spinal; Outcome Assessment (Health Care)
From the FULL TEXT Article:
Introduction
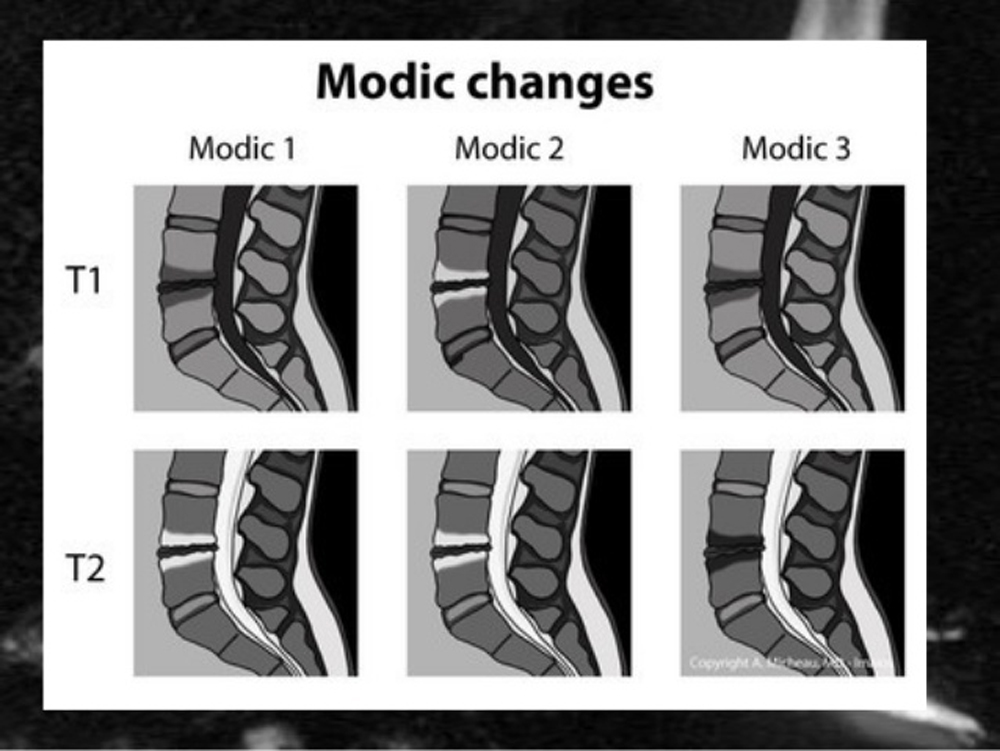
Modic changes (MC) categorize 3 types of degenerative abnormalities in the bone marrow around the vertebral endplates and are visible on magnetic resonance imaging (MRI). [1] They are most common in the lumbar spine and are associated with degenerative disc disease at the same level of involvement. [1] The combination of low-signal intensity on T1-weighted sequences and high-signal intensity on T2-weighted sequences is named MC type I and represents bone marrow edema. [1–3] The appearance of high-signal intensity on both T1-weighted and T2-weighted sequences corresponds to Modic type II changes, the same as fat. Modic type III changes are shown as low-signal intensity on both T1-weighted and T2-weighted sequences and would appear as sclerosis on routine radiograph. [1, 4–6] Many studies have already shown that the incidence of MC increases with age [4, 7] and that MC tend to convert to other types over time, mostly type I to type II. [8–10]
The role of MCs in the lumbar spine as pain generators is currently well known, [11, 12–15] especially regarding the activity of MC type I. It is also well known that patients with disc herniations are more likely to have MCs at the level of herniation. [16–19] In recent years, many studies have evaluated the effects of different types of treatment on MC and how patients with MC respond to various treatments. [2, 20–27]
The effect of invasive treatments on patients with low back pain (LBP) was recently studied by Lee et al. [25] They evaluated the outcome predictors of lumbar transforaminal epidural steroid injection in patients with radiculopathy owing to a herniated intervertebral disc (HIVD). They showed that the only good MRI-based predictor for improvement was the location of the HIVD. The HIVDs in the foraminal or in the extraforaminal zone were significantly more common in the very best outcome group than HIVDs in the central or in the subarticular region. Other MRI findings, such as grade of disc degeneration, disc height loss, or MCs, were not statistically significant in predicting good or bad outcomes from steroid injections.
In 2014, a study by Peterson et al [27] evaluated the outcomes of patients presenting with LBP caused by an MRI-confirmed symptomatic disc herniation with and without MCs who received an imaging-guided transforaminal lumbar nerve root block. Patients with an MRI-confirmed, symptomatic lumbar disc herniation who exhibited MC were less likely to improve after the lumbar nerve root block compared with patients without MC. However, although the presence of MC was related to less improvement, the differences in outcome between patients with and without MC did not reach statistical significance, even though the sample size was quite large.
In 2015, Bianchi et al [26] reported on the outcomes of lumbar therapeutic facet joint injections in patients with and without lumbar MC. Although there was a tendency for MC negative patients to do better after lumbar facet injections, the results once again showed no statistically significant difference between the 2 groups. The MCs were not significantly related to improvement in that study.
Few studies analyzed the effect of conservative treatment on patients with MCs and associated degenerative changes or disc herniations. One of the most recent studies on the subject found that a spontaneous resorption of a disc herniation is less likely when MCs are present. Therefore, the presence of MC may be associated with a poorer outcome in conservative treatment. [23]
The effect of high-velocity, low-amplitude chiropractic manipulation on acute and chronic LBP owing to a disc herniation was studied by Leemann et al [24] in 2014. In this study, the majority of acute and chronic disc herniation patients treated with spinal manipulation reported a clinically relevant improvement in the short and in the long term. However, a comparison of outcomes based on specific MRI findings, including MCs, was not done at that time. A follow-up study on a subgroup of these patients evaluated whether or not specific MRI findings were related to treatment outcomes, including the presence or absence of MCs. [4] This showed that patients with MCs and disc herniation responded well to spinal manipulation, especially when MC type II was present. [4] To date, no studies have been reported that compared treatment outcomes from other LBP patients receiving high-velocity, low-amplitude spinal manipulation with and without MCs.
To the authors’ knowledge, at the current time point, the studies regarding the outcomes of patients having MC and receiving conservative treatment were few, and the results were controversial. Therefore, the purpose of this study was to determine if there is any difference in outcomes in patients with nondisc herniation LBP, with and without MCs, who present to a university hospital–based chiropractic teaching clinic and receive chiropractic treatment.
Discussion
The aim of this prospective outcome study was to compare the treatment outcomes of patients with and without MCs presenting with LBP, a negative MRI scan for lumbar disc herniation, and who received chiropractic treatment, including high-velocity, low-amplitude spinal manipulation, in a single center, chiropractic outpatient clinic at a specialized musculoskeletal hospital. To the authors’ knowledge, this study is one of the few showing the role that the presence of MC could play in the conservative treatment of nonspecific LBP.
Comparing MC positive with MC negative patients and MC I with MC II patients, we did not find any significant differences in the proportion of patients who reported clinically relevant “improvement” in their condition and those who did not at any data collection time point. The percentage of patients reporting clinically relevant “improvement” increased in all categories (MC present or absent, MC I or MC II) over time. This means that the presence of MC or of a certain MC category did not influence the outcome of the patients undergoing chiropractic treatment.
Compared with a previous study on this subject, which included only patients with symptomatic, MRI confirmed disc herniation, [4] this current study on nondisc herniation patients showed a lower proportion reporting clinical relevant “improvement” of their condition over time. For example, after 3 months, in the previous study, 80% of patients with MC I were improved,” whereas in this current study only 52.2% of MC I patients in the same chronicity category reported “improvement.” This is most likely due to the much higher number of chronic patients included in this current study and less likely to be related to the presence or absence of a certain type of MC. In the previous study, at the 3 months follow-up time point, more than 80% of the patients reported clinically relevant “improvement,” irrespective of the MC category, whereas in this current study, between 50% and 58% of patients were “improved,” depending on the MC category. The percentage of chronic patients in this current study was 75.9% compared with only 26% chronic patients in a study on disc herniation patients. [4]
Comparing the baseline scores of NRS for back pain and of the BQ for pain and disability with the presence or absence of MC did not find any significant differences. The same results were found when comparing the baseline scores of NRS and BQ with the different MC categories (MC I and MC II). This is surprising because it is known that especially MC I acts as a pain generator because of its inflammatory nature. [11–15] Thus, a higher baseline pain and disability score for patients presenting with an MC type I would be expected.
The results also show that the Modic negative patients have slightly higher BQ change scores at every outcome time point; although, it did not reach statistical significance. However, surprisingly, when comparing Modic I with Modic II patients, Modic I patients had higher BQ change scores at both 1 week and 3 months, although not statistically significant. If Modic I (bone marrow edema) is indeed a significant contributor to LBP, this should not have occurred.
These results support the hypothesis already illustrated in a previous study,4 that the back pain is not generated only from the presence of MC or of a certain MC category, but it is more likely multifactorial in nature. The sole presence of MC (especially MC I) was not sufficient to explain the presence of back pain in those patients and should not be over emphasized in determining treatment. Certainly, the presence of MCs is not a contraindication for chiropractic treatment.
Many authors have already evaluated other, more invasive treatment methods for MCs, such as surgical procedures, antibiotic-based treatments, and lumbar steroid injections. [2, 25–36]
The etiopathogeny of MCs has been evaluated by many studies, [10, 37–40] especially regarding MCs type I. It was hypothesized that MCs type I were a consequence of repeated microtraumas, leading to segmental instability and thus to the production of proinflammatory substances and local inflammation. [37–39] Furthermore, these studies confirmed the association between MCs and disc herniations, often found at the same vertebral level, possibly indicating a continuum in a dynamic degenerative disc disease. [10, 39, 40] These facts are supported by other studies, [29, 30] which found that surgical stabilization of the involved vertebral levels could lead to pain relief in patients with MC I but not in patients with other MC types.
A study by Ohtori et al [31] evaluated the changes that occurred in the lumbar spine after posterolateral fusion surgery and found a conversion to Modic type II in 9 patients and the disappearance of MC I in 2 patients. This could support the instability-hypothesis as a cause for Modic type I changes. Chataigner et al [32] reviewed 56 patients who underwent anterior lumbar interbody fusion and found the best results in patients presenting with MC I at baseline compared with patients with MC II, who had poorer results after surgery. On the other hand, another study that evaluated the surgical procedure of lumbar disc replacement did not find any difference in outcomes between patients with and patients without MC. [33]
At the current time point, there are no published studies about the natural history of MCs versus surgical procedures, so the changes of MC category or the disappearance of MC may not be completely attributed to the surgical treatment. Furthermore, there is no agreement on the best surgical procedure for MCs because different studies show different results.
Another hypothesis in the etiopathogeny of MCs type I is the bacterial infection. Some studies confirmed the presence of local disc infection in patients presenting with an MC type I in the adjacent vertebrae, [34, 41] leading to the question if antibiotics could be a valid treatment for MCs. In recent years many authors have tried to evaluate the effect of antibiotics on MC type I, leading to controversial results. A recent study of Albert et al [34] found a significant improvement in the patients’ symptoms after long-term antibiotics when compared with placebo, whereas Wedderkopp et al [35] found no evidence of bacterial infection in the biopsy of patients presenting with MC type I. A very recent trial published in 2017 [36] included 28 patients with chronic LBP associated with MCs type I and no previous lumbar surgery, with all patients undergoing a long-term treatment based on the same antibiotic used in the previous trial of Albert et al.
Disappointedly, the results could not confirm the infectious nature of Modic I changes because the outcomes were similar to those of follow-up studies regarding patients with MC type I who did not receive any antibiotics. [42] The authors of this second trial suggested that the difference in outcomes between these 2 studies was that on the first trial of Albert et al, half of the included patients had undergone previous discal surgery, leading to the development of a postsurgical infectious type of MC I. To date, a treatment based on antibiotics remains controversial, and the role of a low-grade infection as the cause of the MC type I needs further study because Modic I subsets, such as infection-induced or instability-induced, may exist and may need specific types of treatment. [38] Certainly, the results of this current study do not support infection as an etiology of Modic I changes, and these patients had very similar treatment outcomes compared with patients with Modic II changes or no MCs at all.
Another treatment procedure that was studied in recent years is the lumbar steroid injection. Two different studies [2, 43] evaluated intradiscal steroid injection and found that it could represent a valid short-term treatment in patients with therapy-resistant chronic LBP presenting with MC type I because these patients did significantly better compared with the patients with LBP and MC type II. These results are supported by another study, [44] which found that intradiscal steroid injection and epidural steroid injections were beneficial for a small group of patients and were more effective if inflammatory vertebral endplate changes were found.
Conversely, a recent study [26] evaluated the outcome predictors of lumbar transforaminal epidural steroid injection in patients with radiculopathy owing to a herniated disc and found that the only good outcome predictor was the location of the herniated disc and not the presence or absence of other MRI findings, such as MCs. Another study in patients receiving lumbar facet injections, which included corticosteroids as treatment for LBP, found no significant difference between patients with and without MCs. [26] Furthermore, a recent study by Peterson et al [27] found that the transforaminal nerve root block for the treatment of symptomatic lumbar disc herniations was slightly more effective in terms of pain reduction in patients without MC, although the difference in outcome did not reach statistical significance.
To date, only a few studies have evaluated the effect of more conservative treatments on patients with LBP presenting with MCs. The effect of chiropractic treatment on acute and chronic LBP owing to a herniated disc was studied in 2014 by Leemann et al, [24] with significant improvement in the patients’ symptoms. A follow-up study included patients with LBP, lumbar disc herniation, with or without MCs, and evaluated if the presence of vertebral endplate changes could influence treatment outcomes. [4] This study showed that most patients responded well to the treatment, especially if MC II was present.
This current study supports the results of other studies on this subject in that chiropractic care is a safe and valid conservative treatment method not only in patients with a herniated disc, but also in patients presenting with a nonspecific type of LBP and MCs. Modic changes are not to be considered a contraindication for chiropractic treatment and are not related to a worse outcome.
Limitations
One of the main limitations of this study was that many parameters that are known to act as pain and disability perpetuating factors (eg, socio-economic status, educational level) were not considered. [45–47] The presence or absence of MC and the MC category was compared with the patients’ clinical outcomes that included only a few psychological factors, such as anxiety and depression reported through the BQ for LBP. The fact that many other known predictors for chronicity in LBP were not considered in this current study could represent a problem in interpreting the results because most of the patients that were included in this study were categorized as chronic (75.9%), and the relationship between chronicity and these perpetuating factors is well known.
Unfortunately, this information was not available for the included patients, making it impossible to determine if other, external factors were also playing a role in the reported “improvement” or “worsening” of the patients’ condition. Surprisingly, however, Modic negative patients scored significantly higher on both anxiety and depression levels at baseline compared to Modic positive patients. These 2 factors are known to be related to less favorable outcomes, [45–47] yet this was not found in this study.
This is surprising because on one hand depression is known to be a significant baseline predictor for the development of LBP chronicity and thus for a worse outcome in other studies, [45, 46] yet in this current study, the patients with higher baseline scores for depression and anxiety did not have significantly worse treatment outcomes. On the other hand, MC type I is known to act as a pain generator, so a worse outcome of the MC I patients would be expected, yet it could not be supported by the results of this study. Furthermore, another study about chronicity predictors found only a weak association between moderate to severe MCs and an adverse outcome, [47] underlining once more the importance of other factors in the development of pain chronicity.
Another main limitation is the fact that this study was not designed as a randomized controlled trial but as a prospective outcomes study, so the results cannot be definitively attributed to the chiropractic treatment.
The relatively small sample size and the fact that this study considers only the follow-up until 3 months could represent additional limitations.
In addition, MRI scans after the last follow-up time point were not available, so it is impossible to say if the MCs remained stable over the 3–month time period or if they changed category from MC I to MC II or disappeared entirely, a fact that could have influenced the patients’ conditions because of the known pain generating nature of MC I and less of MC II. Follow-up MRI scans would not be supported from the evidence-based imaging guidelines nor be cost-effective for the patients.
Conclusion
The presence or absence of Modic changes (MCs) and the category of MC, when present, were not related to the outcomes for LBP patients without lumbar disc herniations who were undergoing chiropractic treatment. This calls into question the clinical relevance of particularly MCs I as a serious pain generator and certainly challenges the theory that MCs are due to infection.
These results are consistent with the ones found for lumbar disc herniation patients treated with high-velocity, low-amplitude spinal manipulation. This also supports the hypothesis that chiropractic care is a safe conservative treatment for patients presenting with nonspecific LBP, despite the presence of MCs.
Furthermore, the results of this study show that the sole presence of MCs is not sufficient in explaining back pain in these patients. More research on the multifactorial cause of LBP is needed.
References:
Modic, MT, Steinberg, PM, Ross, JS, Masaryk, TJ, and Carter, JR.
Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging.
Radiology. 1988; 166: 193–199Fayad, F, Lefevre-Colau, MM, Rannou, F et al.
Relation of inflammatory modic changes to intradiscal steroid injection outcome in
chronic low back pain.
Eur Spine J. 2007; 16: 925–931Nguyen, C, Poiraudeau, S, and Rannou, F.
Vertebral subchondral bone.
Osteoporos Int. 2012; 23: S857–S860Annen, M, Peterson, C, Leemann, S, Schmid, C, Anklin, B, and Humphreys, BK.
Comparison of outcomes in MRI confirmed lumbar disc herniation patients with and without
modic changes treated with high velocity, low amplitude spinal manipulation.
J Manipulative Physiol Ther. 2016; 39: 200–209Thompson, KJ, Dagher, AP, Eckel, TS, Clark, M, and Reinig, JW.
Modic changes on MR images as studied with provocative diskography:
clinical relevance--a retrospective study of 2457 disks.
Radiology. 2009; 250: 849–855Ulmer, JL, Elster, AD, Mathews, VP, and Allen, AM.
Lumbar spondylolysis: reactive marrow changes seen in adjacent pedicles on MR images.
AJR Am J Roentgenol. 1995; 164: 429–433Villarreal-Arroyo, M, Mejia-Herrera, JC, and Larios-Forte, MC.
Incidence of Modic degenerative changes in patients with chronic lumbar pain at
Monterrey Regional ISSSTE Hospital.
Acta Ortop Mex. 2012; 26: 180–184Hutton, MJ, Bayer, JH, and Powell, JM.
Modic vertebral body changes: the natural history as assessed by consecutive magnetic resonance imaging.
Spine (Phila Pa 1976). 2011; 36: 2304–2307Jensen, RK, Leboeuf-Yde, C, Wedderkopp, N, Sorensen, JS, Jensen, TS, and Manniche, C.
Is the development of Modic changes associated with clinical symptoms?
A 14-month cohort study with MRI.
Eur Spine J. 2012; 21: 2271–2279Kuisma, M, Karppinen, J, Niinimäki, J et al.
A three-year follow-up of lumbar spine endplate (Modic) changes.
Spine (Phila Pa 1976). 2006; 31: 1714–1718Brinjikji, W, Diehn, FE, Jarvik, JG et al.
MRI findings of disc degeneration are more prevalent in adults with low back pain
than in asymptomatic controls: a systematic review and meta-analysis.
AJNR Am J Neuroradiol. 2015; 36: 2394–2399Järvinen, J, Karppinen, J, Niinimäki, J et al.
Association between changes in lumbar Modic changes and low back symptoms over a two-year period.
BMC Musculoskelet Disord. 2015; 16: 98Jensen, OK, Nielsen, CV, Sørensen, JS, and Stengaard-Pedersen, K.
Type 1 Modic changes was a significant risk factor for 1-year outcome in sick-listed low back pain patients:
a nested cohort study using magnetic resonance imaging of the lumbar spine.
Spine J. 2014; 14: 2568–2581Schistad, EI, Espeland, A, Rygh, LJ, Røe, C, and Gjerstad, J.
The association between Modic changes and pain during 1-year follow-up in patients
with lumbar radicular pain.
Skeletal Radiol. 2014; 43: 1271–1279Teraguchi, M, Yoshimura, N, Hashizume, H et al.
The association of combination of disc degeneration, end plate signal change, and Schmorl node
with low back pain in a large population study: the Wakayama Spine Study.
Spine J. 2015; 15: 622–628Jensen, TS, Kjaer, P, Korsholm, L et al.
Predictors of new vertebral endplate signal (Modic) changes in the general population.
Eur Spine J. 2010; 19: 129–135Mann, E, Peterson, CK, and Hodler, J.
Degenerative marrow (modic) changes on cervical spine magnetic resonance imaging scans:
prevalence, inter- and intra-examiner reliability and link to disc herniation.
Spine (Phila Pa 1976). 2011; 36: 1081–1085Luoma, K, Vehmas, T, Grönblad, M, Kerttula, L, and Kääpä, E.
Relationship of Modic type 1 change with disc degeneration: a prospective MRI study.
Skeletal Radiol. 2009; 38: 237–244Kerttula, L, Luoma, K, Vehmas, T, Grönblad, M, and Kääpä, E.
Modic type I change may predict rapid progressive, deforming disc degeneration:
a prospective 1-year follow-up study.
Eur Spine J. 2012; 21: 1135–1142Zhuang, CY, Cao, P, Zheng, T, Yang, YQ, Zhang, ZW, and Chen, W.
Intradiscal interventional therapy for degenerative chronic discogenic low back pain
with end-plate Modic changes.
Zhonghua Yi Xue Za Zhi. 2009; 89: 2490–2494Djurasovic, M, Carreon, LY, Crawford, CH, Zook, JD, Bratcher, KR
The influence of preoperative MRI findings on lumbar fusion clinical outcomes.
Eur Spine J. 2012; 21: 1616–1623Lurie, JD, Moses, RA, Tosteson, AN et al.
Magnetic resonance imaging predictors of surgical outcome in patients with lumbar
intervertebral disc herniation.
Spine (Phila Pa 1976). 2013; 38: 1216–1225Shan, Z, Fan, S, Xie, Q et al.
Spontaneous resorption of lumbar disc herniation is less likely when modic changes are present.
Spine (Phila Pa 1976). 2014; 39: 736–744Leemann, S, Peterson, CK, Schmid, C, Anklin, B, and Humphreys, BK.
Outcomes of Acute and Chronic Patients With Magnetic Resonance Imaging–Confirmed
Symptomatic Lumbar Disc Herniations Receiving High-Velocity, Low-Amplitude,
Spinal Manipulative Therapy: A Prospective Observational Cohort Study
With One-Year Follow-Up
J Manipulative Physiol Ther 2014 (Mar); 37 (3): 155-163Lee, JW, Choi, SW, Park, SH, Lee, GY, and Kang, HS.
MR-based outcome predictors of lumbar transforaminal epidural steroid injection for lumbar
radiculopathy caused by herniated intervertebral disc.
Eur Radiol. 2013; 23: 205–211Bianchi, M, Peterson, CK, Pfirrmann, CW, Hodler, J, and Bolton, J.
Are the presence of Modic changes on MRI scans related to "improvement" in low back pain
patients treated with lumbar facet joint injections?.
BMC Musculoskelet Disord. 2015; 16: 234Peterson, CK, Pfirrmann, CW, and Hodler, J.
Are Modic changes related to outcomes in lumbar disc herniation patients treated
with imaging-guided lumbar nerve root blocks?.
Eur J Radiol. 2014; 83: 1786–1792Ehrler M, Peterson C, Leemann S, Schmid C, Anklin B, Humphreys BK.
Symptomatic, MRI Confirmed, Lumbar Disc Herniations: A Comparison of Outcomes
Depending on the Type and Anatomical Axial Location of the Hernia in Patients
Treated With High-Velocity, Low-Amplitude Spinal Manipulation
J Manipulative Physiol Ther. 2016 (Mar); 39 (3): 192-199Esposito, P, Pinheiro-Franco, JL, Froelich, S, and Maitrot, D.
Predictive value of MRI vertebral end-plate signal changes (Modic) on outcome of surgically treated
degenerative disc disease. Results of a cohort study including 60 patients.
Neurochirurgie. 2006; 52: 315–322Vital, JM, Gille, O, Pointillart, V et al.
Course of Modic 1 six months after lumbar posterior osteosynthesis. (discussion 721)
Spine (Phila Pa 1976). 2003; 28: 715–720Ohtori, S, Yamashita, M, Yamauchi, K et al.
Change in Modic type 1 and 2 signals after posterolateral fusion surgery.
Spine (Phila Pa 1976). 2010; 35: 1231–1235Chataigner, H, Onimus, M, and Polette, A.
Surgery for degenerative lumbar disc disease. Should the black disc be grafted?.
Rev Chir Orthop Reparatrice Appar Mot. 1998; 84: 583–589Siepe, CJ, Mayer, HM, Wiechert, K, and Korge, A.
Clinical results of total lumbar disc replacement with ProDisc II: three-year results
for different indications.
Spine (Phila Pa 1976). 2006; 31: 1923–1932Albert, HB, Sorensen, JS, Christensen, BS, and Manniche, C.
Antibiotic treatment in patients with chronic low back pain and vertebral bone edema
(Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy.
Eur Spine J. 2013; 22: 697–707Wedderkopp, N, Thomsen, K, Manniche, C, Kolmos, HJ, Secher Jensen, T.
No evidence for presence of bacteria in modic type I changes.
Acta Radiol. 2009; 50: 65–70Palazzo, C, Ferrari, M, Lefevre-Colau, MM, Nguyen, C, Rannou, F.
Lack of effectiveness of antibiotics in chronic low back pain with Modic 1 changes.
Joint Bone Spine. 2017; 84: 507–508Crock, HV. Internal disc disruption.
A challenge to disc prolapse fifty years on.
Spine (Phila Pa 1976). 1986; 11: 650–653Nguyen, C and Poiraudeau, S. Rannou F.
From Modic 1 vertebral-endplate subchondral bone signal changes detected by MRI
to the concept of 'active discopathy.'.
Ann Rheum Dis. 2015; 74: 1488–1494Albert, HB and Manniche, C.
Modic changes following lumbar disc herniation.
Eur Spine J. 2007; 16: 977–982Adams, MA, Freeman, BJ, Morrison, HP, Nelson, IW, and Dolan, P.
Mechanical initiation of intervertebral disc degeneration.
Spine (Phila Pa 1976). 2000; 25: 1625–1636Albert, HB, Lambert, P, Rollason, J et al.
Does nuclear tissue infected with bacteria following disc herniations lead to
Modic changes in the adjacent vertebrae?.
Eur Spine J. 2013; 22: 690–696Mitra, D, Cassar-Pullicino, VN, and McCall, IW.
Longitudinal study of vertebral type-1 end-plate changes on MR of the lumbar spine.
Eur Radiol. 2004; 14: 1574–1581Beaudreuil, J, Dieude, P, Poiraudeau, S, and Revel, M.
Disabling chronic low back pain with Modic type 1 MRI signal: acute reduction in pain
with intradiscal corticotherapy.
Ann Phys Rehabil Med. 2012; 55: 139–147Buttermann, GR.
The effect of spinal steroid injections for degenerative disc disease.
Spine J. 2004; 4: 495–505Neubauer, E, Junge, A, Pirron, P, Seemann, H, and Schiltenwolf, M.
HKF-R 10 - screening for predicting chronicity in acute low back pain (LBP):
a prospective clinical trial.
Eur J Pain. 2006; 10: 559–566Melloh, M, Elfering, A, Egli Presland, C et al.
Predicting the transition from acute to persistent low back pain.
Occup Med (Lond). 2011; 61: 127–131Carragee, EJ, Alamin, TF, Miller, JL, and Carragee, JM.
Discographic, MRI and psychosocial determinants of low back pain disability and remission:
a prospective study in subjects with benign persistent back pain.
Spine J. 2005; 5: 24–35
Return to LOW BACK PAIN
Return to DISC HERNIATION
Since 11-27-2018


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |