

Impact of Musculoskeletal Pain on Balance and Concerns
of Falling in Mobility-limited, Community-dwelling Danes
over 75 Years of Age: A Cross-sectional StudyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Aging Clin Exp Res. 2018 (Aug); 30 (8): 969–975 ~ FULL TEXT
Julie C. Kendall, Lars G. Hvid, Jan Hartvigsen, Azharuddin Fazalbhoy,
Michael F. Azari, Mathias Skjřdt, Stephen R. Robinson, Paolo Caserotti
School of Health and Biomedical Sciences,
RMIT University,
PO Box 71,
Bundoora, Melbourne, 3083, VIC, Australia.
julie.kendall@rmit.edu.au
BACKGROUND: In older adults, musculoskeletal pain is associated with increased concerns of falling, reduced balance and increased occurrence of falls. In younger adults, the intensity of neck pain and low back pain is associated with increased postural sway. It is not known if pain further impairs balance and concerns of falling in mobility-limited older adults, and if so, whether this is associated with different intensities of pain.
OBJECTIVE: This study examined whether mobility-limited older adults with mild or intense neck pain and/or low back pain have significantly increased postural sway as measured by centre of pressure (COP) changes and concerns of falling compared to those without pain.
METHODS: 48 older adults with a gait speed of < 0.9 m/s from Odense, Denmark were recruited through the public health service. Self-reported neck pain, low back pain, and concerns of falling were recorded on questionnaires. Sway range, velocity and area were recorded on a force plate in a comfortable standing stance. Pain intensity was rated on an 11 point numerical rating scale (0-10). Participants were sub-grouped into mild (0-4) and intense (> 5) neck pain or low back pain.
RESULTS: Intense neck pain was associated with increased anterior-posterior sway range and area of sway. Intense low back pain was associated with increased concerns of falling.
CONCLUSION: Intense neck pain in mobility-limited older adults is associated with significant changes in postural balance, and intense low back pain is associated with significantly higher concerns of falling.
KEYWORDS: Balance; Falls risk; Mobility-limitation; Musculoskeletal pain; Older adults
From the FULL TEXT Article:
Introduction
Falls are one of the leading health concerns facing older adults, affecting their capacity to engage in activities of daily living, loss of independence, and the risk of sustaining moderate–severe injury. Several factors have been identified that lead to an increased risk of falls in this age group, including reduced gait speed. [1] One of the determinants gait speed is good postural control, and it has been observed that musculoskeletal pain is associated with reduced balance, increased concerns of falling, and increased occurrence of falls in older adults. [2–4]
Previous studies have demonstrated that older adults with a history of falls displayed an increased range and velocity of sway when their balance was tested in a static standing position on a force plate. [5] It has been hypothesised that deteriorating anterior to posterior (AP) postural control occurs as a natural consequence of ageing, particularly of the lower limb muscles tibialis anterior and biceps femoris, which demonstrate increased activity in static standing when compared to young healthy controls. [6] The resulting flexed posture and increase in rigidity may be an adaptation that facilitates the forward displacement of the centre of gravity, to reduce the likelihood of falling. [6] A retrospective study, in older adults, conducted to analyse balance control parameters in fallers and non-fallers suggested that fallers had increased medial–lateral (ML) sway rather than AP sway. [7] Despite these preliminary observations, the relationship between increased sway and falls risk in older adults remains to be fully investigated.
The speed of postural sway is influenced by a range of factors that are likely to be linked to the risk of falls. For instance, it has been demonstrated in older adults that a concern of falling, indicated by high Falls Efficacy Scale International Questionnaire (FES-I) scores, is associated with significant reductions in both AP and ML velocity. [8] In contrast, in studies on younger adults, neck pain and low back pain increase the extent of sway in the AP direction more so than the ML direction, and high intensity neck pain increases the velocity of both AP and ML sway. [9, 10] Yet, these studies on balance and musculoskeletal pain have been conducted in younger adults. There is a need to determine if mobility-limited older adults with musculoskeletal pain exhibit significant increases in sway and poor balance. This retrospective cross-sectional study examined neck pain, low back pain, postural stability, and concerns of falling in a group of mobility-limited older adults (low gait speed). Postural stability was assessed in terms of both the range and velocity of AP sway and ML sway.
The aims of this study were to:(1) examine whether mobility-limited older adults with mild or intense neck pain and/or low back pain have significantly increased centre of pressure (COP) sway compared to those without pain; and
(2) examine whether concerns of falling are associated with increases in COP sway in this population.
Methods
Older adults were recruited from Odense, Denmark, through a preventative home visit program from the municipality. This program includes interviews, with cognitive and physical assessments, to evaluate risk factors for disability and loss of independence. Participants included in this analysis were those who underwent COP analysis recruited to a randomised controlled trial aimed at increasing functional ability. [11] These data were baseline data before any intervention was delivered. This trial was part of the Healthy Ageing Network of Competence (HANC) study (Clinical trial registration NCT02051725, The Regional Scientific Ethical Committees for Southern Denmark approval S-20120149). To be included in the HANC trial, participants had to be ≥ 75 years of age, have a self-paced gait speed of < 0.9 m/s, and a mini-mental state examination score of > 21/30 [12]. The cutpoint for MMSE of 21/30 was chosen to take into account those with low educational levels. [13] Additionally, participants underwent a medical screening including a general medical history and blood pressure assessment. They were excluded if they had an amputated limb or other serious physical impairment, terminal or critical disease (such as cancer, severe heart failure, etc.), recent surgery (within the last 6 months) or a recent bone fracture (within the last 3 months). A total of 65 participants were recruited into the trial. Force plate data for 15 participants was not recorded properly, of those remaining 50; two participants did not respond to the neck pain and low back pain questionnaires, leaving data from 48 participants included in this analysis. Where there was additional missing data, these data were excluded pairwise from analyses.
Self-reported neck pain and low back pain within the previous 4 weeks was recorded via two questionnaires based on a low back pain questionnaire developed by an international consensus of experts in the field of low back pain. [14] In the first questionnaire, participants were asked whether they had experienced low back pain within the previous 4 weeks, and if so, to rate the intensity of pain on a numerical rating scale (NRS) from 0 to 10 (0 = no pain, 10 = severe pain). The second questionnaire was identical, except that it asked about the presence and intensity of neck pain. Concerns of falling were reported on the Falls Efficacy Scale Questionnaire (FES-I), a 16–item questionnaire that measures the concerns of falling whilst performing daily routines and activities. FES-I is a valid and reliable measure of concerns of falling, and the following cut-off points were used to denote low (< 20), medium (20–27) and high (> 27) concerns of falling. [15]
Participants were instructed to remove their shoes before stepping onto the force plate. Balance was measured on a force plate (Kistler, 9281 B) in comfortable standing stance with the participants’ heels separated by 13.5 cm. Participants were given time to step onto the force plate, find the correct foot position and compose themselves prior to testing. Participants kept their eyes open, gazing straight ahead and were asked to stay as still as possible during both trials, carried out in quiet laboratory. 30 s of continuous recording from the force plate was used for analysis. Two trials were recorded and the second trial was used for analysis. COP postural sway was analysed in three parameters: area of sway, range and velocity. Range and velocity were calculated in the AP and ML directions. Range was the difference between the maximum points of sway in each direction (mm). Velocity was the distance travelled divided by the recording time in (mm/s). Area was calculated using the area of an ellipse covering 90% of data points (mm2) [16]. Participants reporting neck pain or low back pain were categorised into intense (≥ 5/10) or mild (1–4/10) pain according to their numerical pain rating score.
Once the numerical data were extracted from the recordings, further data analysis was conducted in IBM SPSS (version 22). Normality of the data was determined by examination of histograms, Q–Q plots and Shapiro–Wilk tests of normality. Non-parametric tests were used where data were not normally distributed.
Demographic differences between groups of participants with no pain compared to participants with neck pain were analysed using t tests for continuous variables (height) and chi-squared tests for dichotomous variables (gender). Weight was not normally distributed and a Mann–Whitney U test was conducted instead of t test. Similarly, differences between groups of participants with and without low back pain were compared for continuous, dichotomous and nonnormally distributed data as above.
Data for all COP parameters and FES-I scores were not normally distributed. Differences on each COP parameter between groups of participants without pain, with mild neck pain and intense neck pain were examined using Kruskal–Wallis tests. Where these tests indicated a significant difference between groups pairwise post hoc tests were conducted and adjusted with a Bonferroni correction (Dunn-Bonferroni test). To examine differences between no pain, mild low back pain and intense low back pain, Kruskall–Wallis and post hoc tests were conducted likewise. Similarly, differences on FES-I scores were examined using Kruskall–Wallis and post-hoc tests between intensities of both neck pain and low back pain using the same methods as with COP parameters.
Significance was set at p = 0.05. Data were plotted in GraphPad Prism 7.02 with Tukey box and whisker plots.
Results
Musculoskeletal pain was common, with 24 (48%) reporting low back pain and 14 (28%) reporting neck pain. Of these participants, 9 (18%) reported both neck pain and low back pain. A total of 19 (38%) participants reported not having experienced neck pain or low back pain within the previous 4 weeks. Of the 48 participants, 46 responded to the FES-I questionnaire. Most of the participants reported concerns of falling, with 24 (52%) respondents scoring between 20 and 27 (medium concern of falling), 6 (13%) scoring 28 or more points (high), and 16 (35%) scoring 19 or less (low).

Table 1
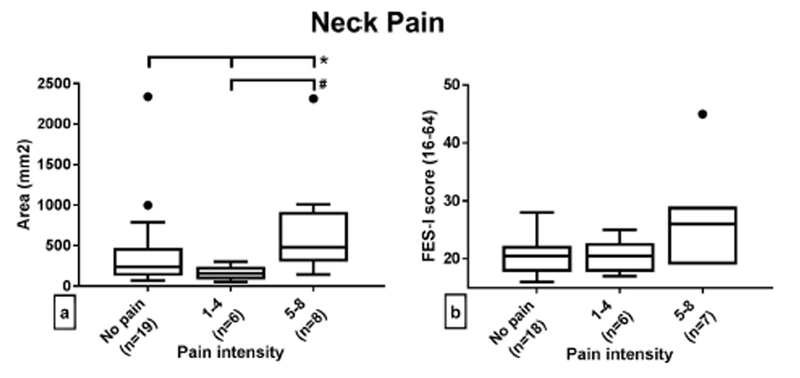
Figure 1 When comparing participants with or without neck pain and /or low back pain, there were no significant differences between groups with respect to gender, height, weight, FES-I score or any COP parameter. However, participants with neck pain were significantly older than participants (84.21+/– 4.93, SD) without neck pain (81.11+/– 4.38, SD) (t test p = 0.033) (Table 1). The maximum pain intensity rating for either neck pain or low back pain was 8/10, indicating a high-intensity of musculoskeletal pain.
Examination of the results from groups with no pain, mild neck pain, and intense neck pain elucidated several differences (Fig. 1). COP sway area was significantly different between no pain, mild pain, and intense neck pain (p = 0.02) (Fig. 1, Panel a). Post-hoc analysis identified that this difference was primarily due to the difference between the mild and intense pain groups (p = 0.02). Similarly, AP sway range was different between pain intensities (p = 0.006). Again, the post-hoc analysis identified a significant difference between the mild and intense neck pain groups (p = 0.006). There were no significant differences between the neck pain intensity groups on sway velocity (both AP and ML), ML sway range, or FES-I scores (Fig. 1 panels b, d, e and f).

Table 2
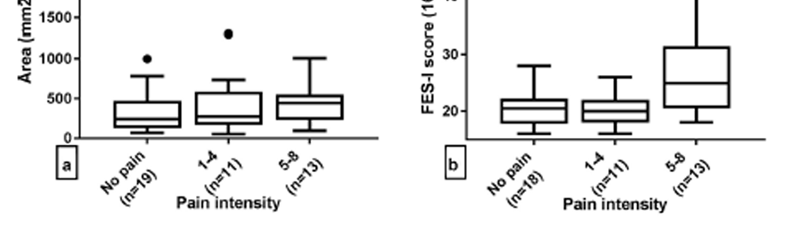
Figure 2 Participants with no low back pain, mild back pain or intense low back pain did not show any significant differences on any COP parameter (Fig. 2 panels a, c, d, e and f). Participants with intense low back pain had significantly higher FES-I scores (mean 26.77, 95% CI 21.87–31.67) compared to those with no neck pain or low-intensity back pain (mean 20.44 95% CI 18.77–22.12) (p = 0.046) (Fig. 2, panel b). When comparing participants with high concerns of falling to participants with low concerns of falling, there was a general trend for the former group of participants to have increased range, velocity and area of sway (Table 2). However, none of these trends reached statistical significance.
Discussion
This study examined mobility-limited older adults with slow gait speed (< 0.9 m/s), and explored the relationships between back and neck pain, postural stability and concerns of falling. Participants with higher intensity of neck pain were found to have a significantly increased range of AP sway and area of sway, and those with higher intensity of low back pain had significantly increased concerns of falling. In experimental pain studies, significant changes in postural stability have been observed with strong pain intensity induced by noxious electrical stimulation of the skin overlying the upper trapezius muscle [17], and not with mild pain intensity induced by bolus injections into the upper trapezius muscle belly. [18] Results of the current study show that in mobility-limited older adults postural sway is only increased with high intensity of neck pain. This is also consistent with findings in younger adults with neck pain [9] where a linear relationship has been reported between neck pain intensity and increased postural sway. Indeed, these findings indicate that there may be a tendency for mild neck pain to increase COP sway; however, this was not the case with mild low back pain. This result is in contrast to a previous study in younger adults, which did observe a relationship between increasing COP sway and increasing intensities of low back pain. [10]
Neck pain has been shown to alter the muscle recruitment pattern in the neck during balance correction tasks [19], and this may contribute to the reduced balance and motor coordination in older adults with poor mobility and neck pain, above and beyond expected deterioration due to the ageing process. [20] The high density of proprioceptors in the neck, particularly the upper neck [21], may explain why high intensity neck pain was significantly associated with increased sway, and not low back pain. Whilst there was no statistically significant difference in COP parameters when comparing participants with high, medium, or low concerns of falling, the trend observed may suggest that COP parameters tend to be higher in those with high concerns of falling. Medium concerns of falling was similar, or slightly higher compared to those with low concern.
One of the strengths in the current study was that the participants are representative of the mobility-limited older population of Denmark, due to the recruitment process within the public healthcare system. This study is of clinical relevance, since all of the participants were over the age of 75 years and had reduced gait speed, placing them at high risk of experiencing a fall in the future. [1] The present results suggest that a subgroup of this sample population, those with intense neck or back pain, may have an increased risk of having a fall, and hence it might be prudent to target interventions alleviating this pain. However, the study sample was relatively small; consequently, it was not possible to conduct detailed subgroup analyses of the effects of age and gender on neck pain and low back pain. The group with neck pain was significantly older than the group without neck pain. So, it is possible that a proportion of the difference observed in sway between the groups may be attributable to age. Furthermore, the sample size was too small to subgroup participants into neck pain only or low back pain only groups. Also, the study did not consider additional factors that affect balance such as, cognitive function [22], current medications [23], and the presence of dizziness. [24] Increased medication use is associated with mobility impairment and spinal pain in older people. [25] It is therefore, possible that people in this study with pain, particularly intense pain, may be taking more medications and this may have produced their poor performance on COP. Likewise, dizziness is associated with spinal pain [26] and could have similarly impacted the results. As a fairly small sample from Odense, Denmark, the findings in this study will need to be confirmed with larger numbers of participants and drawn from other populations.
Conclusion
This study demonstrated that mobility-limited older adults with intense neck pain have significantly poorer postural balance when compared to frail older adults without neck pain. Also, intense low back pain is associated with significantly higher concerns of falling. While these findings support the view that intense neck or back pain contribute to an increased risk of falls, consistent with data observed in younger adults, the current study and cross-sectional design did not permit a prospective examination of the participants’ subsequent falls history. Future studies may examine whether high intensity neck or back pain are predictive of future falls risk in older frail individuals.
Conflict of interest
All authors declare they do not have any conflict of interest.
Funding
This work was supported by an international stipend from the Foundation for Chiropractic Research and Postgraduate Education (Denmark) (Grant No. 14/603). The HANC study is supported by the European funding program INTERREG Iva (Grant No. 11/23147). Neither funding source had any involvement in: study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Statement of human and animal rights
This trial was part of the Healthy Ageing Network of Competence (HANC) study (Clinical trial registration NCT02051725) and obtained ethics approval from the Regional Scientific Ethical Committees for Southern Denmark (approval S-20120149)
Informed consent
All participants gave informed consent as part of the HANC study.
References:
Shimada H, Suzukawa M, Tiedemann A et al (2009)
Which neuromuscular or cognitive test is the optimal screening tool to predict falls in frail community-dwelling older people?
Gerontology 55:532–538Stubbs B, Eggermont LH, Patchay S et al (2014)
Pain interference is associated with psychological concerns related to falls in community-dwelling older adults: multisite observational study.
Phys Ther 94:1410–1420Stubbs B, Schofield P, Patchay S et al (2016)
Musculoskeletal pain characteristics associated with lower balance confidence in community-dwelling older adults.
Physiotherapy 102:152–158Leveille SG, Jones RN, Kiely DK et al (2009)
Chronic musculoskeletal pain and the occurrence of falls in an older population.
JAMA 302:2214–2221Piirtola M, Era P (2006)
Force platform measurements as predictors of falls among older people—a review.
Gerontology 52:1–16Laughton CA, Slavin M, Katdare K et al (2003)
Aging, muscle activity, and balance control: physiologic changes associated with balance impairment.
Gait Posture 18:101–108Melzer I, Kurz I, Oddsson LI (2010)
A retrospective analysis of balance control parameters in elderly fallers and non-fallers.
Clin Biomech (Bristol Avon) 25:984–988del-Rio-Valeiras M, Gayoso-Diz P, Santos-Perez S et al (2016)
Is there a relationship between short FES-I test scores and objective assessment of balance in the older people with age-induced instability?
Arch Gerontol Geriatr 62:90–96Ruhe A, Fejer R, Walker B (2013)
On the relationship between pain intensity and postural sway in patients with non-specific neck pain.
J Back Musculoskelet Rehabil 26:401–409Ruhe A, Fejer R, Walker B (2011)
Center of pressure excursion as a measure of balance performance in patients with non-specific low back pain compared to healthy controls: a systematic review of the literature.
Eur Spine J 20:358–368Hvid LG, Strotmeyer ES, Skjodt M et al (2016)
Voluntary muscle activation improves with power training and is associated with changes in gait speed in mobility-limited older adults—a randomized controlled trial.
Exp Gerontol 80:51–56MacKenzie DM, Copp P, Shaw RJ et al (1996)
Brief cognitive screening of the elderly: a comparison of the mini-mental state examination (MMSE), abbreviated mental test (AMT) and mental status questionnaire (MSQ).
Psychol Med 26:427–430Kahle-Wrobleski K, Corrada MM, Li B et al (2007)
Sensitivity and specificity of the mini-mental state examination for identifying dementia in the oldest-old: the 90+ study.
J Am Geriatr Soc 55:284–289Dionne CE, Dunn KM, Croft PR et al (2008)
A consensus approach toward the standardization of back pain definitions for use in prevalence studies.
Spine 33:95–103Delbaere K, Close JC, Mikolaizak AS et al (2010)
The falls efficacy scale International (FES-I). A comprehensive longitudinal validation study.
Age Ageing 39:210–216Doyle RJ, Hsiao-Wecksler ET, Ragan BG et al (2007) Generalizability of center of pressure measures of quiet standing. Gait Posture 25:166–171
Vuillerme N, Pinsault N (2009)
Experimental neck muscle pain impairs standing balance in humans.
Exp Brain Res 192:723–729Madeleine P, Prietzel H, Svarrer H et al (2004)
Quantitative posturography in altered sensory conditions: a way to assess balance instability in patients with chronic whiplash injury.
Arch Phys Med Rehabil 85:432–438Boudreau SA, Falla D (2014)
Chronic neck pain alters muscle activation patterns to sudden movements.
Exp Brain Res 232:2011–2020Uthaikhup S, Jull G, Sungkarat S, Treleaven J.
The Influence of Neck Pain on Sensorimotor Function in the Elderly
Arch Gerontol Geriatr. 2012 (Nov); 55 (3): 667–672Liu JX, Thornell LE, Pedrosa-Domellof F (2003)
Muscle spindles in the deep muscles of the human neck: a morphological and immunocytochemical study.
J Histochem Cytochem 51:175–186Deschamps T, Beauchet O, Annweiler C et al (2014)
Postural control and cognitive decline in older adults: position versus velocity implicit motor strategy.
Gait Posture 39:628–630Richardson K, Bennett K, Kenny RA (2015)
Polypharmacy including falls risk-increasing medications and subsequent falls in community-dwelling middle-aged and older adults.
Age Ageing 44:90–96Ekvall Hansson E, Magnusson M (2013)
Vestibular asymmetry predicts falls among elderly patients with multi-sensory dizziness.
BMC Geriatr 13:77Karttunen N, Lihavainen K, Sipila S et al (2012)
Musculoskeletal pain and use of analgesics in relation to mobility limitation among community-dwelling persons aged 75 years and older.
Eur J Pain (London England) 16:140–149Menant JC, Wong A, Sturnieks DL et al (2013)
Pain and anxiety mediate the relationship between dizziness and falls in older people.
J Am Geriatr Soc 61:423–428
Return to SENIOR CARE
Return to LOW BACK PAIN
Since 12–27–2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |