

An Investigation of Musculoskeletal Dysfunctions in Infants
Including a Case Series of KISS Diagnosed ChildrenThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Clinical Chiropractic Pediatrics 2012 (Jun); 13 (1): 958–967 ~ FULL TEXT
OPEN ACCESS Josefa Langkau and Joyce Miller BS, DC , DABCO, FCC (UK), FEAC, FACO(US)
Josefa Langkau 34 Morley Road,
BH5 2JL, Bournemouth,
United Kingdom
Joyce Miller, BS, DC, DABCO, FCC (UK), FEAC, FACO(US)
Associate Professor, Anglo-European College of Chiropractic,
Bournemouth, United KingdomObjective: The purpose of this study was to describe etiology, presentation and treatment of musculoskeletal issues in early infancy by integrating a case series of infants diagnosed with kinematic imbalance due to suboccipital sprain (KISS) and treated in a teaching clinic in the United Kingdom with a critical review of the concept of KISS. The concept has been developed by Heiner Biedermann and medical doctors in Germany and contributed significantly to the development of manual therapy in children in that country.
Methods: A literature review was conducted. The search was focused on German studies about KISS syndrome and English studies about musculoskeletal issues in infants. Search strategy: ZDB, ZB MED and PubMed and hand search in German libraries. The data were collected by survey via a data collection system and files in the Anglo European College of Chiropractic (AECC) teaching clinic.
Results: The primary differences between the diagnosis and treatment recommended by Biedermann and that in the AECC clinic are 1) the recommended use of x-ray prior to treatment by Biedermann and 2) recommended force used in treatment (4 N at AECC versus 70 N with Biedermann).
Conclusion: Musculoskeletal issues caused by birth and intrauterine posture are commonly observable and early treatment is often recommended; however, the grounding in evidence is not yet known. What this study adds to the literature is that:
Radiologic evaluation of every child cannot be justified without any red flags due to known radiation hazards.
Different treatments involve very different forces. Future studies about effectiveness and safety should focus on specific treatment style and force.
There is no genetic component to develop KISS syndrome and the predisposition of male sex is more likely related to a bigger than average size at birth.
From the Full-Text Article:
Introduction
Musculoskeletal dysfunctions in the infant including torticollis, infantile scoliosis and facial asymmetry have been noted by various authors in the past two decades. [1–7] Facial asymmetries and head deformities in neonates are common and dysfunctional hip development has also been noted. [4]
The surgeon, Heiner Biederman, who contributed significantly to the development of manual therapy in children in Germany, also developed the concept of the kinematic imbalance due to suboccipital strain or “KISS-syndrome”. It suggests that functional abnormality in the atlantooccipital and atlanto-axial joints (for example, caused by birth trauma) might lead to a spectrum of symptoms and complaints in newborns. [8]
Infant positional preferences are common with this being present in 8%–12% of infants. [9, 10] About 2.4% retained restricted range of motion and/or flattening of the skull at the age of 2 to 3 years. Other long term effects have been found. Sacher, for example, found that although dysfunction of the suboccipital joints might be asymptomatic during childhood, untreated functional abnormalities are thought to become persistent during skeletal maturity, leading to a fixed dysfunction causing symptoms in older children and adults. [11]
It is controversial as how to best react to asymmetric posture in infants. On the one hand it might be considered as being self-limiting. [12] On the other hand more recent studies imply the importance of treatment to avoid postural fixed dysfunctions causing long term problems in later childhood. [8, 11, 13–15]
Therefore it is important to investigate musculoskeletal diagnosing in infants with the help of early markers and examine whether the concept of early treatment might be justified. This paper aims to give a deeper understanding of musculoskeletal issues in children by putting KISS and KISS-induced Dyspraxia and Dyslexia (“KIDD”), Biedermanns’ diagnostic concepts, into context within practice. Moreover, the presented case series on 23 symptomatic subjects adds to a critical evaluation of current treatment procedures for musculoskeletal problems in infants.
Methods
The paper is a hybrid-type study, a narrative review combined with a case series. The literature review focused on German studies about KISS syndrome and English studies about musculoskeletal issues in infants. ZDB, ZB MED and PubMed were searched and the following search strategy was used:“Manipulation Spinal”,
“KISS + syndrome”,
”Kopfgelenk + Asymmetrie”,
“Suboccipital +strain”
“Cervical-diencephal-statisches syndrome”
“paediatric”.Finally, the reference lists of relevant reviews were screened.
Additionally a wider search was done in libraries in Germany (Deutsche Nationalbibliothek Leipzig, Medizinische Bibliothek Chariete Berlin) to gather older articles and journals which were not accessible in any internet database. The library was searched for relevant text book information.
For additional information and literature, telephone and email correspondence with Dr. Heiner Biedermann, specialist for KISS syndrome, have been used. The data were collected by survey via a data collection system and files in the clinic to determine, describe and interpret the number of children presenting with KISS and identify the history, cause of presentation, physical findings and treatment given at the AECC teaching clinic. All consent forms had been signed and no individual child can be identified. All data are held completely confidential and data collection was approved by the ethics committee.
Case series

Table 1

Table 2A

Table 2B A review of recent records showed that, between 2003 and 2010, 23 infants presenting to the chiropractic teaching clinic in Bournemouth, United Kingdom had been diagnosed with KISS syndrome. The data collected included information suspected to be risk factors in Table 1 and treatment specific data shown in Table 2.
The mean presenting age was 7–8 weeks and with a male:female ratio of 1.6:1.
13 of the 23 patients had a difficult and/or instrumental assisted labor. The children were all full term and the mean birth weight of 3,512 grams at the 50th centile in the growth chart.
Most common presenting complaints were restriction of rotation towards one side with or without difficulties breastfeeding. General restrictions and tenderness in the upper cervical segments and muscular tightness in the suboccipital region, as well as pelvic and SI joint fixations were noted. The most common differential diagnosis was irritable infant syndrome of musculoskeletal origin (IISMO) or biomechanical cervical dysfunction and treatment consisted mainly of touch and hold and occipital-sacral decompression technique.
Discussion
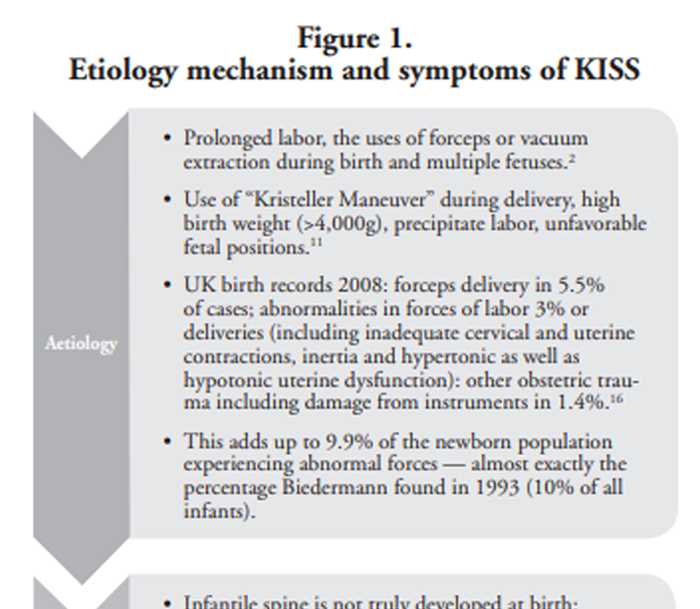
Figure 1

Table 3 KISS syndrome is thought to be caused by irritation of the cervical spine during birth, [8] which is a very demanding procedure for the infant and its spine. [16] Other authors found that asymmetry and restrictions are related to intrauterine posture rather than birth trauma. [4, 7] Children with a head preference to the right usually had an intrauterine posture to the right. [17] Nevertheless there is a correlation between craniofacial asymmetry and birth injuries. [7] It is most likely that both the intrauterine environment and birth injury contribute to the antalgic postures and asymmetries. The relationship between etiology mechanism and symptoms of KISS is shown in Figure 1.
The clinical picture of untreated KISS syndrome consists of four stages: [20]
Up to 3 months: unspecific preliminary stage with symptoms of autonomic irritation and dysphoria (restlessness) e.g. crying babies and colic.
3–12 months: asymmetry during time scale of gaining head control until verticalization. The typical clinical presentation of KISS in this stage is summarized in Table 3.
Verticalization until 4/5 years: symptom free, silent period.
KISS-induced dysgnosia and dyspraxia (“KIDD syndrome”): sensory-motor deficits leading to signs and symptoms of dysgnosia — relating to a form of intellectual impairment prohibiting learning; and dyspraxia — a form of cognitive dysfunctions that impair the ability to learn/use new motor-patterns. [47]
The data collection at the teaching clinic corroborates previous findings that males more commonly present with KISS syndrome. [11] Furthermore instrumental assisted delivery was common which is thought to be another risk factor contributing to the development of the KISS-syndrome. [8]
The cases collected at the teaching clinic further supported the general literature [24] that manipulative therapy is very effective after 4–6 treatments for musculoskeletal issues in infants. When a fixation was detected, range of motion could almost always be improved. Although there was not always complete recovery, improvement was noted.
Comparing the common differential diagnosis to the symptomatic picture of KISS, a lot of similarities can be noted. A major difference is rather the perceived cause and consequent treatment plan. Whereas for IISMO it is suggested that the whole musculoskeletal system of the infant might lead to symptoms, [6] the whole spine will be in focus and specific imbalances will be treated. KISS on the other hand is thought to develop due to an imbalance in the cervico-occipital region; therefore the treatment plan involves only manipulation to the upper cervical spine. [8] Moreover, Biedermann suggests that one treatment might be enough to resolve symptoms in 80% of patients and recommends not treating too often with leaving a pause of 2–3 weeks. [8]
Most often touch and hold technique (TAH) is used as pediatric manipulative therapy. Up to 3 months of age, only light finger pressure should be used, [21] because the infantile cervical spine is not ossified [22] and therefore susceptible to compression forces. A gentle manipulation is not recommended until the child is one year of age. [21] Pressure should not exceed 85–141 grams [21] and the joint is not taken to its end range of motion.
Another technique used quite commonly was occipitalsacral decompression. With the infant supine a very gentle, light distraction is applied for 30 seconds, by contacting the occiput and sacral base, aimed to reduce tension and restrictions. [23]
This style of treating differs quite a lot from the treatment described by Biedermann. At the teaching clinic a very gentle approach to the whole spine is used to treat, and that the force applied in those pediatric manipulations not exceed 4 Newton. [21] In contrast, Biedermann describes that to manipulate the fixation, a short impulse is given with the index finger towards the lateral mass of C1 or transverse process of C2, aiming to affect the cervical receptors. As the highest amount of proprioceptive muscle spindles is found in the upper cervical spine, it is thought to have the biggest effect on biomechanical motor function and balance. [25] Koch and Girnus [26] measured the force of an impulse for a pediatric manipulation done by Biedermann and Koch to be 70 Newton.
This is one of the major differences between treatments — the treatment at the teaching clinic involves one twentieth of the force compared to the force applied by Biedermann. Since the major issue of manipulative therapy is safety, especially for pediatric patients who have delicate anatomy, this difference might be important. However, hardly any paper actually refers to a specific style of treatment and there is no report of adverse events associated with the Beidermann methods versus the low force techniques performed in the chiropractic clinic setting.
In future studies about adverse effects, focus should be put on the force of treatment as well as the type of treatment used to give a more detailed picture.
A genetic component has been suggested to the predisposition to developing KISS, [8] since males were affected more frequently than females. However, when comparing the growth charts of male and females, a difference in head circumference is noticeable. Whereas for girls a head circumference of 37 cm at birth is in the 99.6th centile, in boys the 99.6th centile is related to a head circumference of 39 cm. [27] It is further known that male infants have a more prominent occipital protuberance. [28] According to the WHO growth charts, male neonates are usually bigger as well. A bigger head circumference and size is a known predisposing factor for injuries, [11, 29, 30] leading to the conclusion that size is more likely to explain the ratio than an unknown genetic component.
In contrast to the diagnostic procedure in the teaching clinic where no child will be x-rayed, Biedermann states that an x-ray of the cervico-occipital region needs to be made before treating the patient to rule out any pathology and important anomalies. This diagnostic process is criticized by the German association for neuro-pediatrics because it adds an additional risk of radiation hazards. [31] Infants may be more susceptible to the effects of radiation. [32] Especially in newborns the cells are still developing; therefore they are rapidly dividing. [33] It is known that dividing cells are easily affected by radiation, [32] which might lead to genetic mutations. Even if the consequences of one-time radiation are not fully researched, various studies show a correlation between long-term radiation in childhood and the incidence of acute and chronic side effects including malignancy. [34–36]
It is always important to consider potential risks and benefits when deciding to x-ray a patient. [34] The prevalence of KISS-syndrome is thought to be relatively high; therefore long-term effects of radiation should be considered. The manipulating therapist should have a very good education about contraindications of manipulation. A thorough history and examination for every patient might be enough to obtain suspicious findings or potential contraindications to treatment. Then an x-ray could be done to prove suspicion of a specific pathology instead of x-raying every infant presenting to the practice.
Therefore we suggest the following:
There is no genetic component to developing KISS syndrome as stated by Biedermann — predisposition of male sex is rather caused by bigger average size at birth.
Radiologic evaluation of every child cannot be justified without any red flags due to known radiation hazards.
Future studies about effectiveness and safety should focus on specific treatment style and force.
Suspected long term effects of untreated KISS syndrome
Musculoskeletal imbalances, such as KISS syndrome are functional problems of the cervical spine which is still plastic and changeable. [37] Therefore it can be resolved by early treatment, whereas untreated it might become a structural problem of the cervical spine. [38–40] Some authors state, based on case studies, that the symptomatic cases will resolve spontaneously [12, 41] questioning if early therapy is effective and if it is needed. [12] However, children may become asymptomatic but still have reduced head range of motion with sensory-motor dysfunctions [8, 9, 15, 40, 42, 43] which may lead to other functional problems.
Studies reveal that positional head deformities are still persistent in one third of the affected children after 2–3 years, [9] and early treatment and education [7] for infants might effectively reduce neck problems, and head preferences otherwise leading to cosmetically significant [44] long-term plagiocephaly. [3, 5, 45] The association can also be noted by the trends in clinician referral with suspicion of KISS. In 1999 the prevalence of children referred to Biedermann with suspicion of KISS was due to torticollis in 89.3%; in 2003 53% of children have been referred for torticollis but 67.6% for cranial asymmetry. [46]
It is suggested that in a dysfunctional upper cervical spine, tonic neck reflex receptors cannot transmit the information correctly, leading to impaired perception. [47] The cervical spine musculature has many more muscle spindles and proprioceptive receptors than the lower back musculature, [48] meaning that the upper cervical spine might be important for smooth functioning of perception and motor control. [49] This thesis is supported by a study by Owens et al. [50] which evaluates the repositional accuracy of students with contracted, shortened muscles, concluding that cervical paraspinal musculature contraction influence the proprioceptive accuracy of the neck. Therefore dysfunction in the upper cervical spine may have an impact on the quality of the kinesthetic system, leading to impairment in sensation causing a dysfunction in development of fine motor skills. [8] This theory finds anecdotal evidence in studies from whiplash patients. The traumatic acceleration-deceleration injury of the neck and surrounding structures [51] was found to cause muscular imbalance and cervical spine dysfunction, leading to poorer motor control, especially reduced joint position sense. [52, 53] Even if the mechanism of injury is different from birth, these studies provide evidence that injuries to the cervical spine might lead to dysfunctions that affect the sensory-motor system, especially proprioception. Moreover, a recent meta-analysis found an association between regulatory problems like crying, feeding problems and sleeping problems (that contribute to the symptomatology of KISS) and later behavioral problems. [13]
The symptoms of KISS are thought to progress and it is suspected that, because “form follows function,” longterm effects might develop from untreated KISS. Many sources in the literature recommended early treatment and case studies showed manipulative therapy to be effective in reducing early dysfunctions and therefore signs and symptoms of KISS and preventing long-time deformities. However there is minimal evidence for observed behavioral changes and attention deficits as described. Even if sensation and proprioception might be altered by dysfunctional joints, it is questionable if this accounts for a variety of long term effects. More research is needed to give a clearer picture.
Other studies about infant torticollis, asymmetry and head deformities also conclude that early treatment is favorable to prevent long-term deformities. [3, 7] Especially sufficient education [4, 5] and adequate amount of “tummy time” is suggested to be favorable, because it stretches the tight musculature (especially SCM) and strengthens trunk stability. [7] Further physical therapy is recommended in infants with reduced neck range of motion. [7]
Limitations
It might be concluded that, apart from the small number of patients and the subjectivity of reporting, chiropractic treatment for KISS syndrome at the teaching clinic appears to be effective and safe (although this type of study cannot adequately determine either). The limitations of case series do not allow for statements of efficacy, but can merely show trends. Randomized controlled trials would be best to address effectiveness of treatments. Moreover a long-term follow up has not been made. Considering the suspected long-term effects
Conclusion
In general, this paper was intended to give a better understanding about musculoskeletal issues in infants. By using many German research articles and combining it with cases from the teaching clinic, it gives a deeper insight and a better understanding of the concepts of KISS syndrome and its long-term effects.
References:
Buchmann J. and Bulow B.
Funktionelle Kopfgelenkstorungen bei Neugeborenen im Zusammenhang mit Lagerfunktionsverhalten und Tonusassymeterie.
Man Med 1983; 21:59-62Biedermann H.
Das KISS- Syndrom der Neugeborenen und Kleinkinder.
Man Med 1993; 31:97-107Capiter G, Dessauge D, Picot MC, Bigorre M, Gossard C, El Ammar J and Leboucq N.
Classification and Pathogenic Models of Unintentional Postural Cranial Deformities in Infants: Plagiocephalies and Brachycephalies.
J Craniofac Surg 2011; 22(1):33-41Hamanishi C, and Tanaka S.
Turned head-adducted hip-truncal curvature syndrome.
Arch dis child 1994; 70:515-9Hutchinson K J, Hutchinson LAD, Thompson JM. and Mitchell E.
Plagiocephaly and brachycephaly in the first two years of life: a prospective cohort study.
Pediatr 2004;114:970-80Miller JE.
Cry Babies: A Framework For Chiropractic Care
Clinical Chiropractic 2007 (Dec); 10 (3): 139–146Stellwagen L, Hubbard E, Chambers C and Lyons Jones K.
Torticollis, facial asymmetries and plagiocephaly in normal newborns.
Arch dis child 2008; 93:827-31Biedermann H. Kiss-Kinder-Ursachen,
(Spat-)Folgen und manualtherapeutische Behandlung fruhkindlicher Asymmetrie.
3 Auflage, Stuttgart: Thieme; 2007Boere-Boonekamp M and Van der Linden-Kuiper L.
Positional Preference: Prevalence in Infants and Follow-Up After Two Years.
Pediatr 2001; 107(2):339-43Happle C, Wetzke M, Hermann EJ, Krauss JK, Hartmann H and Lucke T.
Cases against “KISS”:
Ein diagnostischer Algorithmus des fruhkindlichen Torticollis.,
Hannover: Medizinische Hochschule Hannover, Kinderheilkunde; 2009Sacher R.
Geburtstrauma und (Hals-)Wirbelsaule — Teil II: Peripartale Risikofaktoren fur die Entstehung von fruhkindlichen Kopfgelenkblockierungen — eigene Untersuchungen unter Berucksichtigung der ISG-Funktion.
Man Med 2003; 41:15-21Fernandez-Alvarez E.
Transient movement disorders in children.
An Investigation of Musculoskeletal Dysfunctions in Infants Including a Case Series of KISS Diagnosed Children
J Neurol 1998; 245(1):1-5Hemmi MH, Wolke D and Schneider S.
Associations between problems with crying in sleeping and/or feeding in infancy and long term behavioral outcomes in childhood: a meta-analysis.
Arch dis child 2011; 96:622-9Ho BCS, Lee EH and Singh K.
Epidemiology, Presentation and Management of Congenital Muscular Torticollis.
Singapore Med J 1999; 40(11):675-9Williams-Frey S.
Management of atypical infant colic — a pain syndrome of infancy — and the emotional stress associated with it: Why treat a benign disorder?
Clinical chiropractic 2011; 14(3):91-6Moeckel E and Mitha N.
Textbook of pediatric osteopathy.
Philadelphia: Elsevier; 2008Michel GF and Goodwin R.
Intrauterine birth position predicts newborn supine head position preferences.
Infant behav dev 1979; 2:29-38The Health and Social Care Information Centre, 2009.
Table 22: Complications recorded during the delivery episode, 2008-09.UK
Available from
http://www.chiroandosteo.com
[Accessed 20.10.2010]The Cervical spine research society editorial committee.
The cervical spine. Fourth Edition.
Philadelphia: Lippincott Williams & Wilkins; 2005Biedermann H. and Koch L.
Zur Differentialdiagnose des KISS syndroms.
Man Med 1996; 34:73-81Miller JE.
Pediatric Essentials for the Chiropractor.
Bournemouth: AECC Manual; 2009Fysh PN.
Chiropractic Care for the pediatric patient.
Arlington: International Chiropractors Association Council on Chiropractic Pediatrics; 2002Browning M, Miller J.
Comparison of the Short-term Effects of Chiropractic Spinal Manipulation and Occipito-sacral Decompression
in the Treatment of Infant Colic: A Single-blinded, Randomised, Comparison Trial
Clinical Chiropractic 2008 (Sep); 11 (3): 122–129Vallone SA, Miller J, Larsdotter A and Barham-Floreani J.
Chiropractic Approach to the Management of Children
Chiropractic & Osteopathy 2010 (Jun 2); 18: 16Marks V and Kemlein W.
Symptomatik und Diagnostik des Tonusasymmetrie - Syndroms im Sauglingsalter.
Pädiatrische praxis 2001; 60:243-53Koch LE and Girnus U.
Kraftmessung bei Anwendung der Impulstechnik in der Chirotherapie.
Man Med 1998; 36:21-6WHO Department of Health, RCPCH.
UK-WHO Growth Charts: Early Years.
Glasgow: WHO, Department of Health, RCPCH; 2009.
Available from:
http://www.rcpch.ac.uk
[Accessed 14.December 2010]Steele DG and Bramblett CA.
The anatomy and biology of the human skeleton. 8th edition.
College Station: Texas A & M University Press;1988Hughes C A, Harley EH, Milmoe G, Bala R and Martorella A.
Birth Trauma in the Head and Neck.
Arch ontolarynol head neck surg 1999;125(2):193-9Perlow JH, Wington T, Hart J, Strassner HT, Nageotte MP and Wolk BM.
Birth trauma: A Five-Year Review of Incidence and Associated Perinatal Factors.
Obstet Gynecol Surv 1997; 52(6): 339-40Karch D, Boltshauser E, Groß-Selbeck G, Pietz J and Schlack HG.
Manualmedizinische Behandlung des Kiss-Syndroms und Atlastherapie nach Arlen: Stellungnahme der Gesellschaft fur Neuropadiatrie e.V.
Man Med 2005; 43:100-5Folkers C and Olson M.
Radiation and children: The ignored victims.
Nuclear Information and Resource Service; 2004.
Available from:
http://www.nirs.org
[Accessed 07. January 2011]Siegelman CK, Rider EA.
Life-Span Human Develoment. 6th edition.
Belmont: Wadsworth Cenage Learning; 2009Boelling T, Schuck A, Rube C, Hesselmann S, Pape H,
Dieckmann K, Pollinger B, Kortmann RD, Speiser-Held I, Meyer FM, Martini C,
Asadpour B, Timmermann B, Beck JD, Langer T, Paulides M, Schmidt B and Willich N.
Study protocol of the German “Registry for the Detection of Late Sequelae after Radiotherapy in Childhood and Adolescence” (RISK).
Radiat Oncol 2008.
Available from:
http://www.ro-journal.com
[Accessed 07. January 2011]Danoff BF, Cowchock S, Marquette C, Mulgrew L and Kramer S.
Assessment of the long-term effects of primary radiation. Therapy for brain tumors in children.
Cancer 2006; 49(8):1580-6Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM,
Meadows AT, Friedman DL, Marina N, Hobbie W, Kadan-Lottick NS, Schwartz CL,
Leisenring W and Robison LL.
Chronic health conditions in Adult Survivors of Childhood Cancer.
N Engl J Med 2006; 355:1572–82Akbar M, and Wiedenhofer B.
Korrektur der Adoleszentenkyphose. Was ist State of the Art?
Der Orthopäde 2011; 40(8): 682-9Coenen W.
Bewegungsstorungen im Sauglingsalter-Klinische Differenzierung zentraler und peripherer Ursachen.
Man Med. 2011; 49(3):171-88G oebelt T.
Effektivitat Manueller Therapie bei der Behandlung von Kindern mit KISS-Syndrom-Vorstellung eines biomechanischfunktionellen Behandlungsansatzes. Thesis, (B.Sc.).
Fachhochschule Schloss Hohenfels; 2010Saedt E., Schamberger T. and van der Woude B.,
KISS in den Niederlanden-Aktueller Stand. Manuelle Therapie 2010; 14(1): 7-13. Original article: Saedt E, Schamberger T and van der Woude B., KISS in Nederland — The state of the art. T
ijdschrift voor Manuele Therapie (TMT) 2008;1:30-6Basheer SN.
Paroxysmal torticollis.
J Pediatr Neurol 2010; 8:69-71Miller JE and Phillips HL.
Long-Term Effects of Infant Colic: A Survey Comparison of Chiropractic Treatment and Nontreatment Groups
J Manipulative Physiol Ther 2009 (Oct); 32 (8): 635–638Stuecker R.
Die mit Plagiozephalus assoziierte Sauglings asymmetrie.
Zeitung für Orthopädie und Unfallchirogie 2009; 147(4):503-12Hudgins RJ, Boydston WR, Reisner A and Brahma B.
Neuroupdate. Atlanta: Children’s healthcare of Atlanta; 2008Sergueef N, Nelson KE and Glonek T.
Palpatory diagnosis of plagiocephaly.
Complement Ther Clin Prac 2006; 12(2):101-10Biedermann H.
Manual therapy in children.
London: Churchill Livingstone; 2004Sacher R. Handbuch
KISS KIDDs-Entwicklungsauffalligkeiten im Sauglings-Kleinkindsalter und bei Vorschul-/Schulkindern-Ein manualmedizinischer Behandlungsansatz.
Dortmund: Verlag modernes lernen; 2007Bein-Wirzbinski B, Scheunenmann R and Sepke C.
Mogliche Zusammenhange zwischen Kopfgelenkdysfunktionen und blickmotorischen Auffalligkeiten bei Grundschulkindern mit Schulschweirigkeiten.
Man Med 2008; 46:307-15Boyd-Clark LC, Briggs CA, Galea MP.
Muscle Spindle Distribution, Morphology and Density in Longus Colli and Multifidus Muscles of the Cervical Spine.
Spine 2002; 27(7):694-701Owens EF, Henderson C, Gudavalli RM and Pickar JG.
Head repositioning errors in normal student volunteers: a possible tool to assess the neck’s neuromuscular system.
Chiropr Osteopat 2006;14(5)Foreman SM and Croft AC.
Whiplash injuries — The cervical acceleration/deceleration syndrome. Third Edition,
Philadelphia: Lippincott Williams & Wilkins; 2002Jull GA.
Deep cervical neck flexor dysfunction in whiplash.
J musculoskelet pain 2008; (1-2):143-154Sterling M, Jull G, Vicenzino B, Kenardy J and Darnell R.
Development of Motor System Dysfunction Following Whiplash Injury
Pain. 2003 (May); 103 (1-2): 65–73
Return to PEDIATRICS
Since 1–30–2016


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |