Adjusting the Pediatric Spine This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Topics in Clinical Chiropractic 1997; 4 (4): 59–69 ~ FULL TEXT
Gregory Plaugher, DC,
Gregory Plaugher, DC
Associate Professor
Director of Research
Palmer College of Chiropractic - West
Gonstead Clinical Studies SocietyJoel Alcantara, DC
Instructor
Palmer College of Chiropractic-West San Jose, California
Research Associate
Gonstead Clinical Studies Society Mount Horeb, Wisconsin
Associate Professor,
Palmer College of Chiropractic-West,
90 East Tasman Drive,
San Jose, CA 95134
The authors wish to thank Dr. Claudia, Dr. Ernst, Dr. Daniel, and Dr. Susi Anrig
for providing the illustrations used in this article
The subject of chiropractic care of children must by necessity include a discussion of the various techniques chiropractors use to address a subluxation. [1–2] The act of introducing a force into a spinal joint in an effort to restore mobility or alignment is termed an adjustment. This article discusses the technical aspects of adjusting the pediatric spine (ie, occiput to pelvis). Adjustment of the cranial bones and extremity articulations is not covered. The reader is referred to other resources for a discussion of these topics. [3–6]
Although rare, vertebrobasilar injury and stroke can occur following rotational motions of the neck, including those sustained during a rotational-thrust type of adjustive technique. [7] This subject is discussed along with recommendations for technique application in children.
Subluxation
Although it is obvious to practicing chiropractors and their patients, the outside observer may not be aware of the clinical necessity of the spinal adjustment, since few may understand the "why" of this form of therapy. Basically, chiropractors adjust the vertebrae of the spine because signs of articular dysfunction (eg, restricted mobility, abnormal alignment, or inflammation) are present. This "dysfunction" is termed subluxation.
Subluxation, or sprain of a joint, [1] occurs when excessive loads are placed on the spinal column that exceed the elastic limits of the articulation. If the load that is applied is resisted by the individual within his or her normal range of motion, then injury is unlikely. If, instead, the motion segment is moved into the plastic zone, two changes occur simultaneously. First, trauma to the soft tissue-restraining elements (eg, annulus fibrosis or interspinous ligament) can occur, and second, there may be abnormal displacement of the motion segment, but usually less than that seen in a dislocation. Excessive loads can also occur due to compression trauma, leading to damage of the hyaline cartilage end plate8 or fracture of the bony elements. Fracture-subluxations and subluxations combined with additional dislocations can also occur [9–10]
In utero constraint, [11] birth trauma, [12] and a child's everyday activities or specific types of sports or recreational injuries can all potentially lead to damage of the spinal joints. The specific signs associated with spinal subluxation can include pain, limitation of motion, point tenderness, edema, redness, and neurologic changes (eg, altered joint proprioception, nerve irritation, and asymmetric skin temperature). These physical manifestations can vary somewhat in the newborn compared to an adult or adolescent. The positional displacement of the spinal segment can be assessed radiographically, and altered patterns of movement, fixation dysfunction, and hypermobility or instability are further assessed with radiographs taken at the end ranges of movement ( eg, flexion-extension). Gross changes in spinal position can often be detected posturally (eg, structural scoliosis).
In some newborn patients the normal elasticity of the neonatal spine exceeds that of the stretch of the spinal cord, leading to severe injury. This can occur in the absence of significant radiographic alterations and is referred to as spinal cord injury without radiographic abnormality (SCIWORA).
Subluxation Pathology and Back Pain in Children and Adolescents
Clinical research has shown that a variety of pathologic alterations can occur at spinal joints in adolescents. Erkintalo and colleagues [13] studied the development of degenerative changes in lumbar intervertebral discs. In this prospective randomized study, 31 subjects with back pain and 31 subjects without this complaint were sequestered from an original cohort of 1,503 14-year-old school children. The authors concluded that degenerative changes of the spine, including dehydration of the disc (ie, the nucleus pulposus), protrusion, and Scheuermann's changes emerge rapidly following the adolescent growth spurt. The degenerative process occurred in many asymptomatic as well as symptomatic patients.
However, the signs associated with degeneration appeared more commonly in children with back pain and also occurred at an earlier age. These changes, including those ascribed to the Danish physician Scheuermann, are believed to be related to spinal trauma, [14] although genetic factors do playa role.
A study of 640 14-year-old children followed from 1965 through 1990 attempted to determine risk factors for the development of low back pain in adulthood. [15] Low back pain occurring during the growth period and family history were both associated with an increased risk. The lifetime prevalence for back pain was 84% for this cohort. Radiologic findings of lumbar or thoracic Scheuermann's disease were also evaluated and occurred in 13% of subjects. Irregular end plates occurred in 11 % in subjects and disc degeneration was detected in 12%. Four subjects had spondylolisthesis, one subject had a structural scoliosis combined with Scheuermann's changes, and one had a congenital block formation between T–7 and T–8. The proportion of subjects having radiographic abnormalities was 36%. The studied radiographic changes were not associated with an increased incidence of back pain in adulthood. Interestingly, the investigators also found that there was a higher frequency of mental problems (eg, fear or depression) in the group of patients with radiographic changes in the T11–L2 area.
Taimela and colleagues [16] studied the prevalence of low back pain among children and adolescents in a nationwide, cohort-based survey in Finland. The subjects were 594 girls and 577 boys from 45 different schools. The questionnaire included items that investigated the subjects' past and current history of low back pain. Low back pain was classified based on its timing, duration, and location. Subjects with pain in the low back area that interfered with schoolwork or leisure activities during the preceding 12 months were defined as having back pain. Seven-year-olds had a low prevalence of back pain (1 %), but 6% of 10-year-olds reported the problem. Eighteen percent of 14- to 16- year-olds had back pain. Over all, 26% of boys and 33% of girls reported chronic pain. The authors concluded that low back pain is a relatively common complaint during adolescence. By 14 years of age, a significant percentage of children report chronic and recurrent conditions.
Trauma to the intervertebral disc from excessive loading resulting in pain may first be noticed by the patient during adolescence, but many injuries cause only minimal symptoms or perhaps none at all. Salminen and colleagues [17] studied the association of disc abnormalities and low back pain in adolescents. Subjects were followed for 3 years. Nineteen percent of 15-year-olds without back pain had degenerated discs. This rose to 26% in the asymptomatic group by age 18. In subjects with back pain, 42% had degenerated discs at age 15, a percentage that rose to 58% by age 18. Disc protrusions had a similar pattern. No subject without back pain had a disc protrusion at age 15. By age 15, however, 16% of asymptomatic patients had signs of disc protrusion. Disc protrusion occurred in 65% of the 15-year-olds with back pain. Twenty-six percent of l8-year-olds with back pain had disc protrusions.
Ebrall [18] investigated the epidemiology of male adolescent low back pain in 610 12- to 19-year-old males from north suburban Melbourne, Australia. Point prevalence was 16.7%. A history of back pain at some point in the subjects' lives was reported by 57%. Most subjects with pain reported chronic problems, a few days at a time for several times a month, confirming results seen in other longitudinal studies.
Osteopaths [19] and European manual medicine physicians [20] have also discussed "somatic dysfunction" and "blockages" of the spinal articulations. Heligm [19] noted that the longer the duration of osseous development during which asymmetric forces are acting, the greater the occurrence, duration, and extent of spinal damage. He also stated that if aberrant spinal function could be recognized and improved early on, there was a greater likelihood that normal developmental patterns would be established. Addressing the osteopathic profession, Helig appealed to his colleagues to consider spinal manipulation for children, since developmental changes can be most easily affected at an early age.
The studies cited above provide compelling evidence of motion segment injury in adolescents. How these variables relate to misalignment of the motion segment or motion dysfunction (eg, fixation) is presently unknown. In addition, the proportion of adolescents or other children who show alterations in cervical lordosis, retrolisthetic segments, or mal positions in lateral flexion or other directions of displacement is also unknown and deserves further study. Even in adults, this type of epidemiologic information is sorely lacking. Hopefully, spinal findings relating to childhood sports injuries (eg, gymnastics) [21] will provide the impetus for further work in this area. Unfortunately, many physicians as well as parents believe that the child's spine is nearly impervious to trauma, and only severe injuries (often neurologic), including motion segment dislocation, deserve clinical attention.
Biedermann, [22] a manual medicine practitioner, studied biomechanical problems (ie, subluxation) of the upper cervical spine in newborns. One hundred thirty-five infants who were available for follow-up were reviewed in this case series report. The infants were referred to the author because of asymmetric posture, and the case histories included tilt posture of the head or torticollis, head tilt in flexion, uniform sleeping patterns, crying when the mother tried to change the child's position, fixation of the sacroiliac joints, extreme sensitivity of the neck to palpation, and loss of appetite. Biedermann stated that if motor asymmetries, sleeping alterations, or facial scoliosis are present, then suboccipital articulations should be evaluated for blockages (ie, fixation dysfunction or subluxation). He also advocated the use of plain film radiographs for determining malalignment of the suboccipital region and for determining the appropriate direction for the force (ie, adjustment). The radiograph is also used for the detection of anomalies. Most patients in the series required one to three adjustments before returning to normal. The effects of chiropractic care on the newborn with suboccipital subluxation needs to be addressed in prospective randomized or comparison investigations.
Back pain is a highly prevalent condition in children. A large-scale survey [23] of 1,178 schoolchildren found that the cumulative prevalence of back pain was 51.2%. Lumbar, leg, and thoracic pain were the most common forms. Multivariate analysis showed that age, previous back injury, volleyball playing, female sex, and time spent watching television were positively correlated with the presence of back pain. Findings of a significant impact on low back pain among adolescent schoolchildren have been confirmed by other researchers. [24–25]
Low back pain is even more common among adolescent athletes. The excessive spinal loading that accompanies many sporting activities (eg, gymnastics and ice hockey) involves additional risk for acute low back injuries during the growth spurt and is harmful to the lower back. [26]
Manga and colleagues report on several independent evaluations of the effectiveness of chiropractic care in the management of adult patients with low back pain. [27] With regard to pain reduction, lost time from work, and patient satisfaction, chiropractic methods have continually been shown to be of greater benefit to patients than medical or physiotherapeutic treatments. [27–29] Children with these disorders have yet to be studied in large-scale investigations. However, the basic biologic nature of the lesion and therapeutics is likely to be similar in children and adults. Evidence of chronic problems developing in juveniles and adolescents and continuing into adulthood is provided above. This information provides further support for the clinical necessity of chiropractic care in children, despite the lack of specific clinical trial data in younger populations. Although studies of adult patients with back pain and the effects of chiropractic adjustments may be compelling, the specific issues surrounding the care of individual patients remains largely clinician driven, owing largely to the lack of substantive research on which to base clinical decision making. This is even more true in the pediatric population.
Adjustive Technique Modifications in Children
Compared to adjusting the adult spine, adjusting the pediatric spine requires a number of modifications depending on the age and clinical presentation of the patient. These changes can be made readily by the seasoned clinician familiar with differing strategies for the adjustment. For example, a 6-foot, 200-pound man will be adjusted somewhat differently than a 5-foot, 100-pound woman. Although treating children may not be a large portion of practice for the average chiropractor, the fact that adjustments are modified constantly in adults should provide some assurance that both similar and unfamiliar modifications can be made in children, producing a safe and efficacious clinical encounter.
Age-related changes
The age and size of the patient should help guide the application of force. Older adolescents are adjusted similar to young adults. In the juvenile, however, one must consider some force modification, table positioning, and clinician contact points. The amount of force needed to produce the desired movement and positioning of the segment is less in smaller patients. These are, of course, generalizations, and a patient in acute pain with muscle spasm may need to be adjusted with a force similar to that used in a much older patient with substantially greater muscle mass, but not necessarily spasm.
The needs of young toddlers are quite substantial in comparison with those of other patient groups. The patient is beginning to demonstrate more muscle control, combined with an equally robust will. When these factors are combined, along with perhaps an ineffective understanding of the clinicians's needs in terms of patient relaxation and clinical presentation (eg, an acute asthma attack), one has a rather complex adjusting situation. It is not recommended that one try to surmount these challenges by treating the patient with less care or specificity or by forcing something on the patient that he or she does not wish to receive. Communication appears to be the only reasonable way of surmounting these difficulties. Communication can happen in a number of ways beyond the usual verbal (eg, affect-body language or demonstrations). If children are familiar with the protocol when their parents are being adjusted, then they may be more receptive to participate in the process once their turn comes. On the other hand, some clinicians generally avoid demonstrating the procedure prior to performing it, since some adjustments may appear more forceful and perhaps uncomfortable than the adjustment required by the patient. An element of surprise may also be helpful in executing the initial thrust, especially when the patient has a more serious disorder, and this cannot be discounted. If the patient can understand instructions, then in general the element of surprise should be used less. Ultimately, the patient may be under care for a long period of time, and almost always for more than one visit, so a patient who is trying to understand the procedures and cooperate with the clinician is favored over the patient who succumbs to a "surprise attack." Sometimes a combination of the two approaches can be made- perhaps an element of less education and surprise for the first adjustment, followed by gradually more patient information in order to make the encounter more similar to that of the older child. One of the authors' preferences is to provide minimal information except regarding how the adjustment may feel (eg, audible aspects) and how it will help the patient at the initial encounter, especially if the patient is acutely ill. The child-patient also should not watch the parent's care if such care is being provided at the same visit. If required, the parent is adjusted after the child. For infants, an explanation of the adjustment process is provided only to the parent.
Specificity of Contact Points
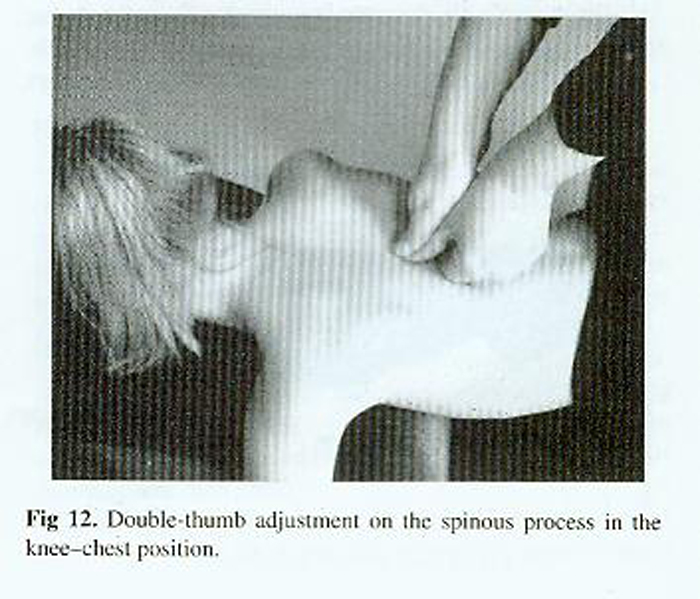
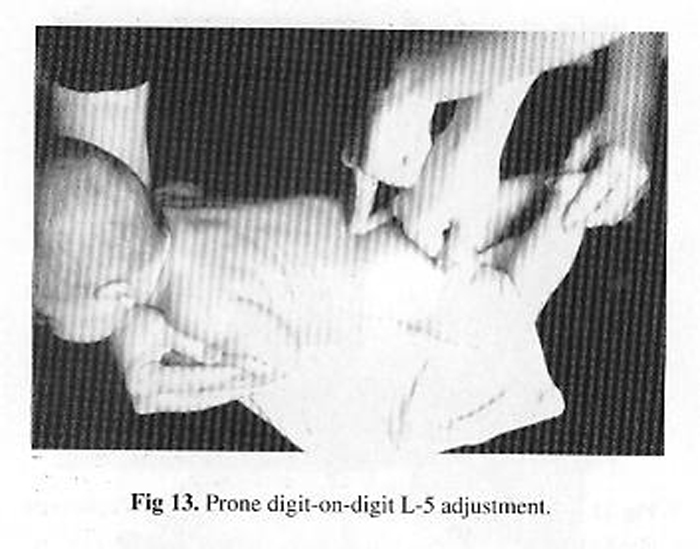
Because of the smaller dimensions of the child's spine, specificity of segmental contact points is necessary to avoid introducing forces into adjacent normal or hypermobile motion segments. In some instances smaller digits will have to be used in combination to achieve the desired level of specificity (Fig 1).
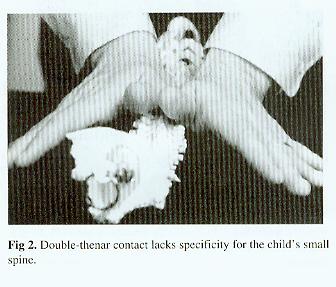
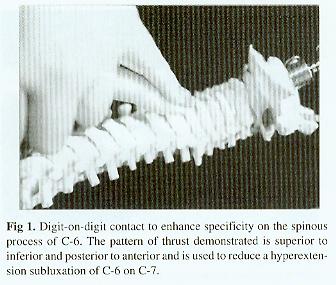
The lack of specificity seen in double-thenar contacts (Fig 2) or the anterior dorsal adjustment (Fig 3) makes them unsuitable for the small child's spine.
Adjusting Apparatus and Positioning Options for the Child Patient
If the clinician's hand is small enough and the patient is older, then the pisiform contact can be used (Fig 5). If specificity cannot be achieved, then the procedure is contraindicated.
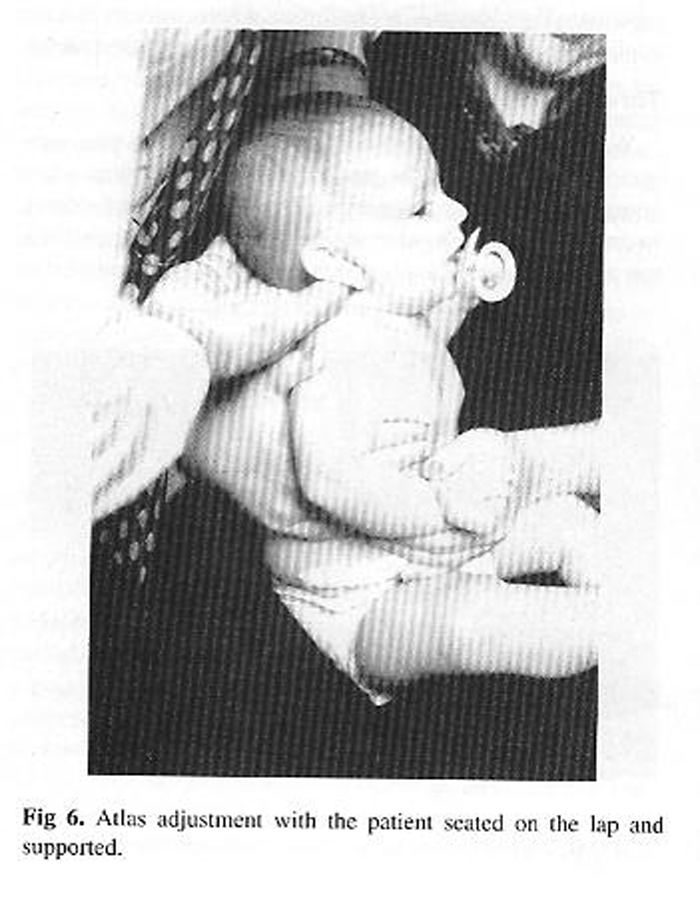
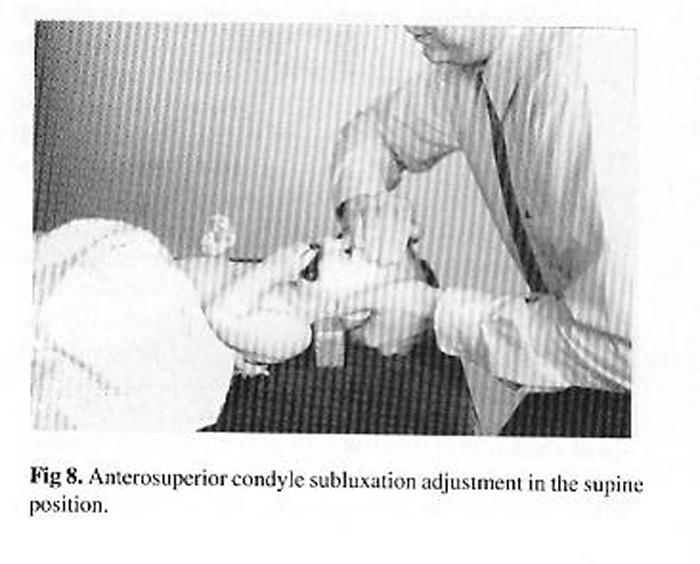
Adjustment of the atlas in an infant, with the thumb used as the clinician's contact point, is shown in Fig 6. The patient can be seated on a parent's or an assistant's lap.
The cervical chair can also be used if the child is large enough (Fig 7).
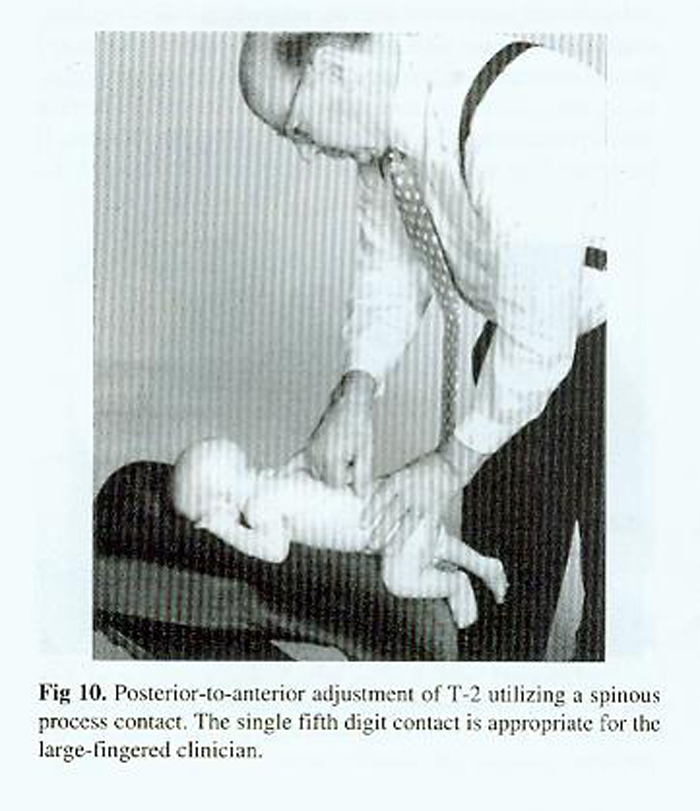
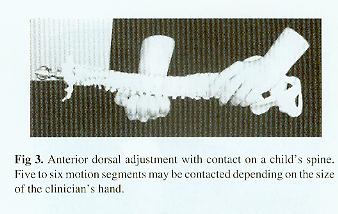
Thoracic adjustments can be performed in the prone position. In the case of the newborn, the patient can be positioned on the clinician's lap (Fig 9).
The knee-chest table's head-piece can also be used for prone adjustments of the newborn
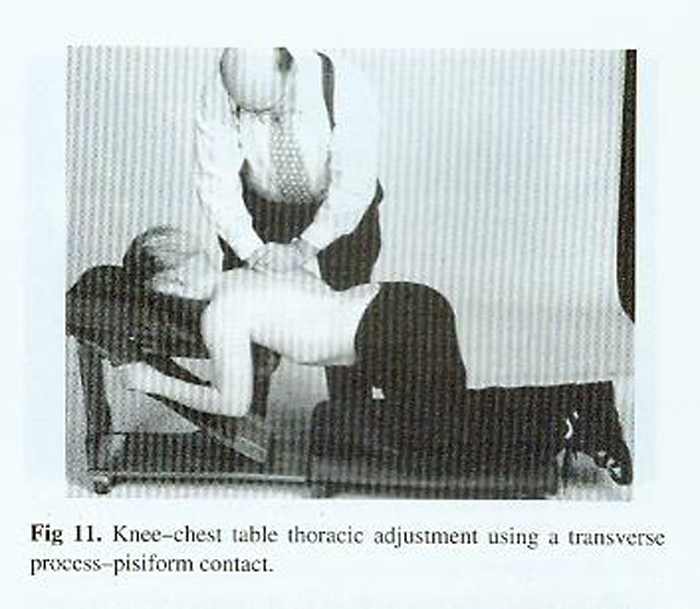
(Fig 10). In the juvenile and adolescent, the knee-chest table can also be used for specific adjustments. The knee-chest table can be modified to the small child's dimensions. [30]
Fig 11 shows the knee-chest table being used in an adolescent and configured to the adult sizing position.
The infant can also be adjusted in the side posture position for both lumbar and sacral subluxations
(Fig 14).
The clinician should avoid excessive Y-axis torsion. Preload is applied at the level of the segment rather than attempting to achieve tension by winding up the spine from the top down (Fig 15).
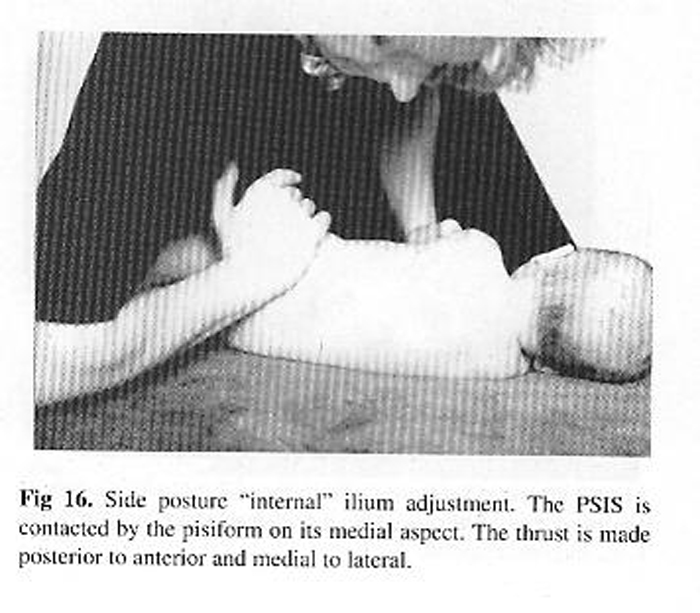
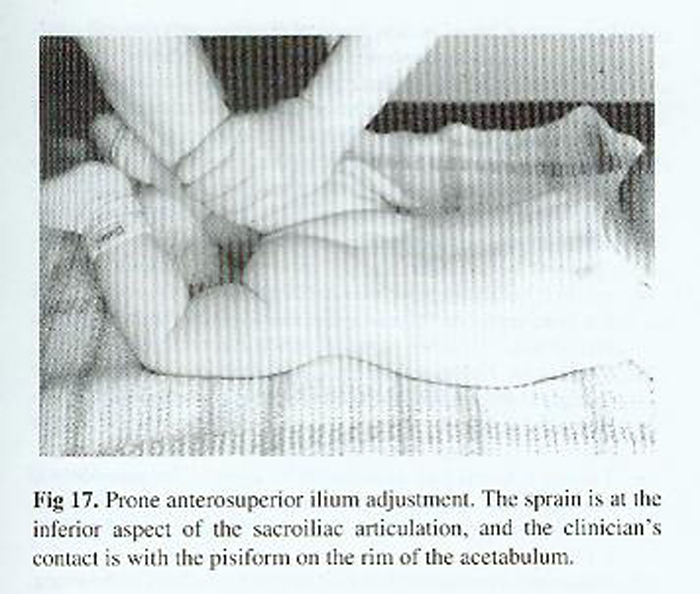
The ilium can also be adjusted in the side posture and prone positions (Figs 16 and 17). The different force vectors that are applied are dependent on the specific findings of the patient.
Thrust characteristics
With high-velocity-low-amplitude thrust techniques, substantial alterations can be made in the pediatric spine when compared to the adult spine, especially in toddlers and infants. In order to bring the motion segment "to tension," or preload, the pediatric spine usually requires a greater amount of displacement forward (ie, posterior to anterior). This excursion of the articulation is essentially work (ie, force x distance). The increased range of motion in flexion-extension necessitates the increased preload. If the patient is agitated by the contact or loading provided by the clinician, then alterations and accommodations must be made. Only in rare circumstances should the thrust be made as the patient resists the force. The segment should be moved with as gentle a force as possible. Taking into account the different planes of the facet joints and the disc angles should result in a minimal amount of force being imparted to the patient.
In addition to enhanced preload, the high-velocity thrust will generally require an increased distance over the application (ie, work) owing to the greater flexibility in the child's spine. Although increased "depth" of the thrust may be required, the clinician should be aware that the thrust (the load) should be ceased immediately following the movement of the segment (usually combined with cavitation and an audible). The high-velocity loading should be decreased much more than what is usually performed in an adult. In the adult, a set-hold procedure is usually well tolerated. The patient in essence can "stop" the thrust of the clinician. Therefore, "follow-through" is very important to achieving the desired movement. However, in the small child's spine, the follow-through is eliminated. Due to the potential danger of imparting too much force after joint cavitation, loading should be ceased immediately following cavitation of the articulation.
Increased acceleration during the thrust is generally required in the smaller spine. The infant or newborn is especially demanding in this regard. Little preload can be applied in many circumstances, necessitating that the clinician overcome the inertia of the segment in a more neutral position. This requires greater acceleration (high velocity) to accomplish the desired joint movement with cavitation. The cavitation may be very small, especially in the infant. It can be considered a benign by-product of the adjustment. The clinician should be focused instead on the extent of movement detected by his or her contact point. This important feedback provides information about the health of the articulation and how the adjustment can be accomplished in the future. Each adjusting encounter can be used by the clinician to "perfect" his or her technique with the individual patient. If the clinician gives some attention to these matters, then the patient receives a more safe and comfortable adjustment. Adjustment's should never be traumatic or cause inflammation. Inflammation associated with the delivery of the adjustment may further prolong the recovery from the sprain. Pain at a segment following an adjustment should be regarded as a contraindication for further treatment until a more thorough assessment can be made of the patient. The longer lasting the pain, the more serious the clinician's concern should be.
VERTEBROBASILAR STROKE IN CHILDREN
Incidence and Mechanism of Injury
Stroke in children is a very uncommon event, with an incidence estimated at about 2.52 cases per 1,000 per year in all racial and ethnic groupS. [31] The mechanism of ischemic injury to the brain may be similar in children and adults (ie, embolism, thrombosis, or decreased systemic blood supply), but the causes of such injury differ. Adults are largely predisposed due to hypertension or atherosclerosis, whereas strokes in children are due in a large part to congenital heart disease (eg, heart valve stenosis, ventricular septal defects, or air and fat embolus), infection (eg, viral infection), metabolic disorders (eg, Ehlers-Danlos Syndrome, homocystinuria, and Fabry disease), hematologic diatheses (eg, protein Sand C deficiency), and vasculopathy (eg, sickle cell disease or trauma) [32] Our discussion will focus mainly on traumatic cervical vascular injury.
Injuries to the carotid arteries may occur following traumatic insults to the neck and head due to motor vehicle and bicycle accidents, athletic injuries, falls, diving, or fights. Injury may also result intraorally, such as in a child who falls with a penetrating object (ie, a pencil) in his or her mouth. If the injury is to the common carotid arteries, hemiparesis is a common presentation. Angiographic studies show that injury is most common at the level of the carotid bifurcation. Pathologic findings may range from an intimal tear with a resulting thrombus to luminal obstruction from arterial dissection.
Injuries to the vertebral arteries may also occur due to trauma, as described above. However, traction injuries of the neck appear to especially cause injuries to the blood vessels, particularly at the atlanto-axial segment. Garg and colleagues [33] described three cases of children suffering from stroke due to trauma to the vertebral artery. They also described 16 other cases in the literature of children who had strokes due to pathologic abnormality in the vertebral arteries. In a majority of the cases, the significant damage was at the C1–C2 level.
One case reported involved a 7 -year-old boy who sustained a left vertebral artery occlusion at the C2 level after a chiropractic adjustment. Reported patient signs involved recurrent headaches, vomiting, left face weakness, ataxia, diplopia, and dysarthria manipulation.[33–34] In the upper cervical spine, the vertebral artery traverses superiorly in a posterolateral direction from the axis to the atlas. It is here that the vertebral artery is most vulnerable to compression and stretching, as well as forced lateral flexion, during head rotation. [35] Garg and Edwards-Brown [36] reported the case of a 21-month-old girl who suffered a thalamic stroke due to vertebral artery compression as a result Of head turning. The child did not have vertebral anomalies such as spondylosis or osteophytes. The caveat regarding rotary adjustments– particularly excessive rotation and lateral flexion to achieve "tension"– must be kept in mind. The resultant injuries occur at the vertebrobasilar portion of the circulation. The central nervous system structures possibly affected are the brain stem, cerebellum, thalamus, and occipital and temporal lobes. [37] Symptoms of ischemic injury may include ataxia, facial paresis, tinnitus, vertigo, anisocoria, eye muscle palsies, dysmetria, dysesthesia, cortical blindness, difficulty swallowing, and changes in mental status, as well as general sensory-motor deficits. [38] Diagnosis relies heavily on recognition of the various signs of focal cerebral injury, as well as on familiarity with disorders mimicking cerebral infarction (eg, acute hemiplegia due to epileptic seizure). The chiropractor must obtain an accurate history and perform a complete physical examination.
The prognosis for the cases described by Garg and colleagues [33] was quite good. The reasons for better outcome in children are not clear but may be due in part to younger age and the state of the arteries. For example, there is a greater amount of vascular collateral reserve in the young brain, as well as greater scope for functional recovery (ie, brain plasticity). Also, children may have less exposure to risk factors such as hypertension, diabetes, smoking, and atherosclerosis. [33, 39]
Rotational adjustments of the cervical spine
Although stroke following rotational spinal manipulation (Fig 18) is rare (l per 1.46 million manipulations) , [40] the results of such injuries can often be catastrophic (eg, lifetime disability or death). Screening procedures are very ineffective in identifying those patients at increased risk, [7] necessitating the use of nonrotational methods for this reason alone.
For biomechanical reasons, purely rotational forces directed at motion segments that normally exhibit primarily flexion-extension motion (eg, CO–C1, C2–L5) are unlikely to change fixation or altered position (eg, retrolisthesis) in this sagittal plane dimension.
In the upper cervical spine (eg, atlas) the neutral zone or "free play" of the C1–C2 motion segment is approximately 30° in the adult. [41] Rotational thrust techniques must move into this zone of movement and beyond in order to bring the joint to tension. The rotational thrust is intended to move the joint to its end range, approximately 40°, without exceeding the anatomic limits. These are generalities, and the individual patient's characteristics and the extent of any joint fixation can alter these values. A purely rotational method of achieving tension, combined with a thrust in Y–axis rotation, can stretch the vertebral artery. The ipsilateral artery on the side of rotation becomes kinked at approximately 30° and the contralateral vessel at 40°. Fortunately, the arteries are quite resilient to rotational forces. After all, humans were meant to turn their head. However, in a very small percentage of patients, the rotational thrust can cause an injury where none was previously present or aggravate an arterial injury already in progress from the patient's initial trauma.
Rotational adjustments of the cervical spine remain a part of the collection of various techniques a practitioner may use, but their use seems to be on the decline, at least in Perth, Australia, [42] along with, apparently, a commensurate reduction in stroke injuries. [43] In the adult, these types of procedures should be avoided in preference to adjustments that are associated with less risk of injury. [7, 44] It appears reasonable that their use as first-line treatment in children should not be recommended.
References:
Oxford Dictionary of the English Language.
Oxford University Press; 1990
Gatterman MI, Hansen DT
Development of Chiropractic Nomenclature Through Consensus
J Manipulative Physiol Ther. 1994;17:302-309
Up ledger JE, Vredevoogd JD.
Craniosacral Therapy.
Seattle, Wash:
Eastland Press; 1983
Upledger JE.
Craniosacral Therapy II: Beyond the Dura.
Seattle, Wash:
Eastland Press; 1987
Phillips C.
Craniosacral therapy.
In: Anrig CA, Plaugher G, eds. Pediatric Chiropractic.
Baltimore, Md:
Williams & Wilkins; 1998
Collins SL, Sill MS, Ginsberg DA.
Extravertebral disorders: Upper and lower extremities.
In: Plaugher G, ed. Textbook of Clinical Chiropractic:
A Specific Biomechanical Approach
Baltimore, Md: Williams & Wilkins; 1993
Terrett AGJ.
Vertebrobasilar Stroke Following Spinal Manipulation.
Des Moines, Iowa:
National Chiropractic Mutual Insurance Co; 1995
Farfan HF.
Biomechanics of the lumbar spine.
In: Kirkaldy-Willis WH, ed. Managing Low Back Pain
New York, NY:
Churchill Livingstone; 1983
Plaugher G, Alcantara J, Hart CR.
Management of the patient with a Chance fracture of the lumbar spine
and concomitant subluxation
J Manipulative Physiol Ther 1996;19:539-551
Alcantara J, Plaugher G, Abblett D.
Management of a patient with a lamina fracture of the sixth cervical vertebra
and concomitant subluxation
J Manipulative Physiol Ther. 1997;20:113-123
Dunne KB, Clarren SK
The origin of prenatal and postnatal deformities
Pediatr Clin North Am. 1986;33:1,277-1,297
Gottlieb M.
Neglected spinal cord, brain stem and musculoskeletal injuries
stemming from birth trauma
J Manipulative Physiol Ther 1993;16:537-543
Erkintalo MO, Salminen JJ, Alanen AM, Paajanen HEK, Kormano MJ
Development of degenerative changes in the lumbar intervertebral disk:
Results of a prospective MR imaging study in adolescents with and without low-back pain
Radiology. 1995;196:529-533
Ascani E, La Rosa G.
Scheuermann's kyphosis.
In: Weinstein SL, ed. The Pediatric Spine: Principles and Practice.
New York, NY: Raven Press; 1994
Harreby M, Neergaard K, Hesselsoe G, Kjer J
Are radiologic changes in the thoracic and lumbar spine of adolescents
risk factors for low back pain in adults. A 25-year prospective cohort study
of 640 school children
Spine. 1995;20:2,298-2,302
Taimela S, Kujala UM, Salminen jj, Viljanen T
The prevalence of low back pain among children and adolescents.
A nationwide, cohort-based questionnaire survey in Finland.
Spine. 1997;22:1,132-1,136
Salminen JJ, Erkintalo M, Laine ML, Pentti J
Low back in the young.
Spine. 1995;20:2,101-2,108
Ebrall PS
The epidemiology of male adolescent low back pain in a north suburban population
of Melbourne, Australia.
J Manipulative Physiol Ther. 1994;17:447-453
Helig D
Osteopathic pediatric care in prevention of structural abnormalities.
J Am Osteopath Assoc. 1949;48:478-481
Lewit K
Manipulative Therapy in Rehabilitation of the Locomotor System.
London, England: Butterworth & Co; 1985
Hager HJ.Junghans
Clinical Implications of Normal Biomechanical Stresses on Spinal Function.
Rockville, Md:
Aspen Publishers; 1990
Biedermann H
Kinematic imbalances due to suboccipital strain in newborns.
J Manual Med 1992; 6: 151-156
Troussier B, Davoine P, deGaudemaris R,
Fauconnier J, Phelip X
Back pain in school children. A study among 1178 pupils.
Scand J Rehabil Med. 1994; 26: 143-146
Olsen TL, Anderson RL, Dearwater SR, et al
The epidemiology of low back pain in an adolescent population
Am J Public Health 1992; 82: 606-608
Balague F, Dutoit G, Waldburger M
Low back pain in school children.
Scand J Rehabil Med 1988; 20: 175-179
Kujala UM, Taimela S, Erkintalo M,
Salminen JJ, Kaprio J
Low back pain in adolescent athletes
Med Sci Sports Exerc 1996; 28: 165-170
Manga P, Angus D, Papadopoulos C, Swan W.
The Effectiveness and Cost-Effectiveness of Chiropractic Management of Low-Back Pain
Ottawa: Kenilworth Publishing; 1993.
Stanley J. Bigos, MD, Rev. O. Richard Bowyer, G. Richard Braen, MD, et al.
Acute Lower Back Problems in Adults. Clinical Practice Guideline No. 14.
Rockville, MD: Agency for Health Care Policy and Research, [AHCPR Publication No. 95-0642].
Public Health Service, U.S. Department of Health and Human Services; 1994
Shekel Ie PG, Adams AH, Chassin MR, Hurwitz EL, Brook RH
Spinal manipulation for low-back pain
Ann Intern Med 1992; 117: 590-598
Plaugher G, Lopes MA
The knee chest table: Indications and contraindications
Chiro Tech 1990; 2: 163-167
Schoenberg BS, Mellinger JF, Schoenberg DG
Cerebrovascular disease in infants and children: A study of incidence, clinical features and survival
Neurology 1978; 28: 763-768
Rivkin MJ, Volpe JJ
Strokes in children
Pediatr Rev 1996; 17: 265-278
Garg BP, Ottingger CJ, Smith RR, Fishman MA
Strokes in children due to vertebral artery trauma
Neurology 1993; 43: 2, 555-2,553
Zimmerman AW, Kumar AJ, Gadoth N, Hodges FJ III
Traumatic vertebrobasilar occlusive disease in childhood
Neurology 1973; 23: 135-133
Frisoni GB, Anzola GP
Vertebral basilar ischemia after neck motion
Stroke 1991; 22: 1 ,452 ,460
Garg BP, Edwards-Brown MK
Vertebral artery compression due to head rotation in thalamic stroke
Pediatr Neurol 1995; 12: 162-164
Martin JH.
Neuroanatomy, Text and Atlas.
2nd ed. Norwalk, Conn:
Appleton & Lange; 1996
Waxman SG, deGroot J
Correlative Neuroanatomy 22nd ed. Norwalk, Conn:
Appleton & Lange, 1995
Martin PJ, Enevoldson TP, Humphrey PRD
Cause of ischaemic stroke in the young
Postgrad Med J 1997; 73: 3-16
Coulter 10, Hurwitz EL, Adams AH, et al
The Appropriateness of Manipulation and Mobilization of the Cervical Spine.
Santa Monica, Calif:
RAND; 1996
WhiteAA, Panjabi MM.
Clinical Biomechanics of the Spine. 2nd ed.
Philadelphia, Pa: JB Lippincott; 1990
Haynes MJ
Stroke following cervical manipulation in Perth
Chiro J Aust 1994 (Jun); 24 (2): 42-46
Haynes MJ
Cervical Spine Adjustments by Perth Chiropractors and Post-Manipulation Stroke: Has a Change Occurred?
Chiro J Aust 1996 (Jun); 14 (2): 43-46
Klougart N, Leboeuf-Yde C, Rasmussen LR
Safety in chiropractic practice, Part I; The occurrence of cerebrovascular accidents after manipulation to the neck in Denmark from 1978-1988
J Manipulative Physiol Ther 1996 (Jul); 19 (6): 371-377

Return to ChiroZINE
Return to PEDIATRICS
Return to ABOUT SPINAL ADJUSTING
Return to CHIROPRACTIC TECHNIQUE


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |