

Cervical Musculoskeletal Impairment in Frequent
Intermittent Headache. Part 2: Subjects
with Concurrent Headache TypesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Cephalalgia 2007 (Aug); 27 (8): 891898 ~ FULL TEXT
OPEN ACCESS M Amiri, G Jull, J Bullock-Saxton, R Darnell, C Lander
Division of Physiotherapy,
The University of Queensland,
St Lucia, Australia.
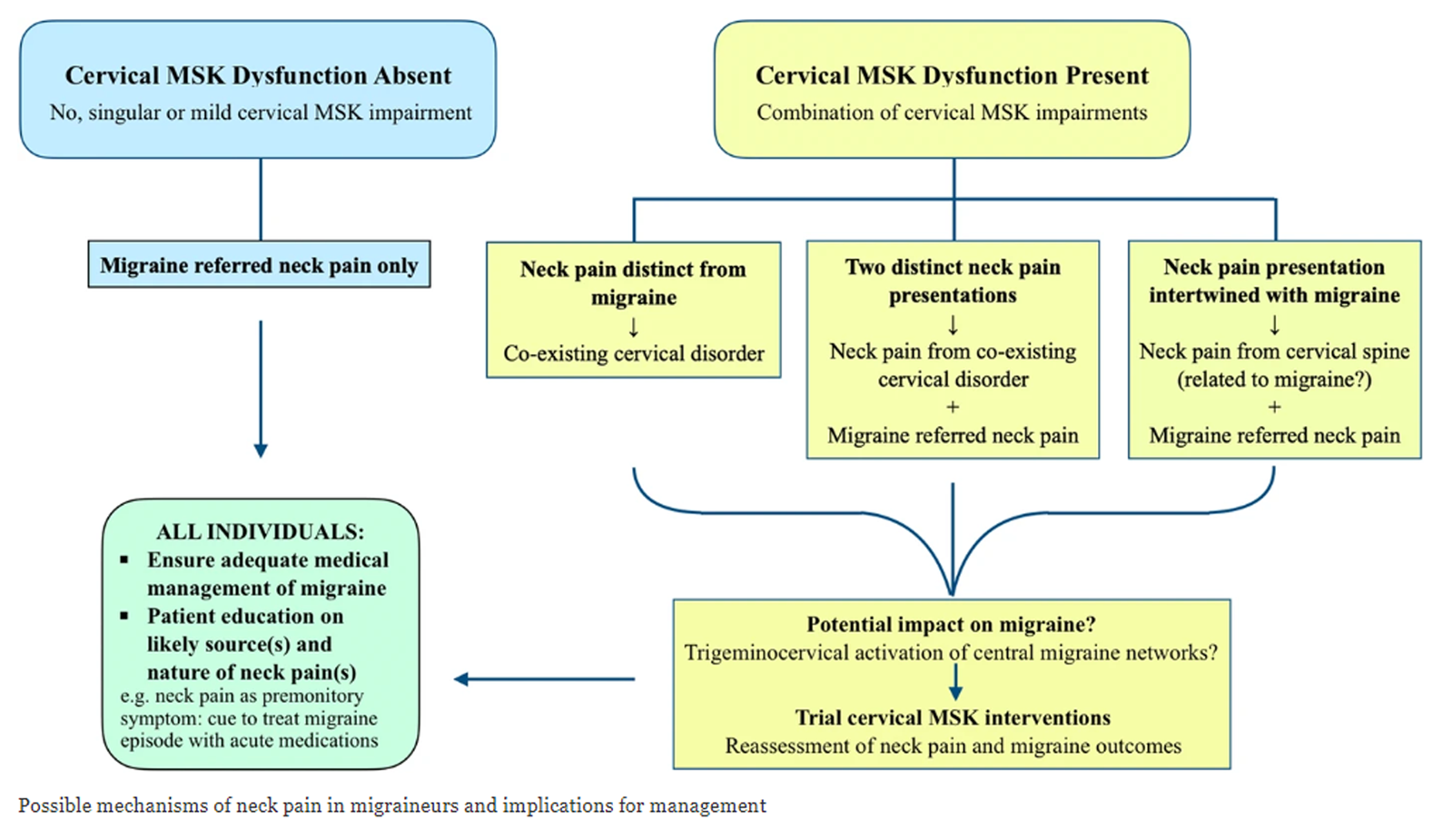
FROM: Archives of Physiotherapy 2021A pattern of musculoskeletal impairment inclusive of upper cervical joint dysfunction, combined with restricted cervical motion and impairment in muscle function, has been shown to differentiate cervicogenic headache from migraine and tension-type headache when reported as single headaches. It was questioned whether this pattern of cervical musculoskeletal impairment could discriminate a cervicogenic headache as one type of headache in more complex situations when persons report two or more headaches. Subjects with two or more concurrent frequent intermittent headache types (n = 108) and 57 non-headache control subjects were assessed using a set of physical measures for the cervical musculoskeletal system. Discriminant and cluster analyses revealed that 36 subjects had the pattern of musculoskeletal impairment consistent with cervicogenic headache. Isolated features of physical impairment, e.g. range of movement (cervical extension), were not helpful in differentiating cervicogenic headache. There were no differences in measures of cervical musculoskeletal impairment undertaken in this study between control subjects and those classified with non-cervicogenic headaches.
From the FULL TEXT Article:
Introduction
Symptomatic overlap is well documented in the frequent headache types such as of migraine, tension-type and cervicogenic headache. [1] This presents challenges for accurate differential diagnosis between these common frequent headache types. [26] Neck pain is a symptom commonly associated with headache in general and there is also a high prevalence of headache in persons with chronic cervical musculoskeletal symptoms. [7]
We have shown that neck pain is not associated with cervical musculoskeletal impairment in persons classified as having migraine or tension-type headache when suffered as a single headache type. [8] Rather, cervical musculoskeletal impairment was shown to be characteristic of cervicogenic headache only. From a set of physical measures, a pattern of musculoskeletal impairment [palpably painful upper cervical joint dysfunction, associated with a restricted range of cervical extension and impairment in the cervical flexor muscle system measured as elevated levels of sternocleidomastoid (SCM) activity in the second and third stages of the five-staged test of cranio-cervical flexion] emerged and was shown to have 100% sensitivity and 94% specificity in distinguishing a cervicogenic headache from migraine and tension-type headache.
Investigations of large cohorts of chronic headache patients, however, have revealed that many patients report more than one headache type. [9, 10] We questioned whether this pattern of cervical musculoskeletal impairment which characterized cervicogenic headache but not migraine and tension-type headache in persons suffering a single headache could discriminate a distinct headache in persons reporting two or more headaches (suggesting cervicogenic), or if boundaries blurred between the multiple headaches. A better understanding of the role of cervical spine dysfunction in concurrent frequent intermittent headache types could aid diagnosis and guide the implementation of appropriate treatment.
Materials and methods
Subjects
Volunteers from the community (age range 1855 years) reporting benign frequent intermittent headache were sought for the study through advertisement in local media. To be included in the headache group, volunteers had to have a minimum of a 1year history of headache with a headache frequency of one per month or greater. Control subjects of a similar age range and gender were recruited provided they were either headache free or experienced no more than occasional mild headache (less than five times per year), for which they had never sought any medical treatment. Exclusion criteria for both groups included any general health problems, e.g. diabetes, pulmonary disease or myopathic diseases.
Volunteers (n = 336) responded to the advertisements and were initially screened by a telephone interview. There were 304 eligible subjects, the remainder being outside the age limits. A further 51 subjects failed to attend their scheduled testing session. Thus 253 subjects entered the study (196 headache subjects and 57 non-headache control subjects). Within the headache group, 88 reported one headache type and 108 reported multiple headaches. The latter group included 77 subjects with two headache types, 27 with three headache types and four who reported four types of headache. The 108 subjects with two or more headaches were the focus of this study. Ethical approval for the study was granted by the Institutional Medical Research Ethics Committee and all procedures were conducted according to the Declaration of Helsinki. Written informed consent was provided before participation.
MeasurementsTests of the cervical musculoskeletal system
The primary measures in this study were a series of tests of the cervical musculoskeletal system. The tests were chosen on the basis that they have revealed cervical musculoskeletal impairment in other studies of cervical disorders. The measures included cervical range of motion [11], manual palpation of the cervical joints to detect symptomatic levels [12, 13], cervical flexor and extensor strength [14, 15], cross-sectional area of the semispinalis capitis, longissimus capitis and upper trapezius at the C2 level using ultrasound imaging [16], activity [electromyography (EMG)] in the sternocleidomastoid in the performance of the cranio-cervical flexion test (CCFT) [1719] and cervical kinaesthetic sense. [20] The procedures for these tests as well as data extraction have been previously described in full. [8]
Questionnaire
A questionnaire was constructed, which included subject demographics and the major criteria for migraine with and without aura, tension-type headache, substance abuse headache [1] and cervicogenic headache as established by the Cervicogenic Headache International Study Group. [21] Subjects completed separate questionnaires for each headache.
Procedure
The physical measures of the cervical musculoskeletal system were conducted by an examiner blinded to the headache or non-headache status of the subject. At the completion of data collection for the entire population, two researchers independently classified the headache from the questionnaires (n = 251 headaches from the 108 subjects) using the information documented in the questionnaire for each headache. This process was conducted with researchers blind to the results of the physical measures. Headaches were classified using the International Headache Society [1] criteria and cervicogenic headache was classified on the criteria of a symptomatic pattern which included: unilateral or unilaterally dominant headache, without sideshift, associated with ipsilateral neck, shoulder or arm pain, pain began in the neck, and headache was aggravated by neck movement or neck postures. [21]
Data management and analysis
The threshold values of the discriminant function coefficients of the physical measures which, as a set, had high sensitivity and specificity to detect cervicogenic headache when suffered as a single headache [8] were applied to the data of 108 subjects reporting multiple frequent intermittent headaches as well as the 57 control subjects [values for palpably painful joint dysfunction in the upper cervical segments (C03), range of motion of cervical extension and right and left SCM activity in the second and third stages (denoted as 24 mmHg and 26 mmHg, respectively) of the five-staged cranio-cervical flexion muscle test]. In addition, a cluster analysis was used as an independent method of judging the discriminant analysis. Cluster analysis attempts to force a number of different groups from the dataset. The candidate variables to define the clusters were the measures found to be most useful in discriminating cervicogenic headache in the single headache population [i.e. dysfunction in C01, C12, C23 joints, cervical extension range and (L) and (R) SCM activity at the 2nd and 3rd stages of the CCFT]. No difference had been found in the measures of physical impairment between the subjects with migraine and tension-type headache and control subjects in subjects with one headache type. [8] Thus for this analysis, three clusters were forced, namely, cervicogenic headache, non-cervicogenic headache and control subjects. This would show if some subjects classified as non-cervicogenic headache, using the set of discriminant functions coefficients, demonstrated signs of physical impairment of the neck.
The 251 headaches of the 108 subjects were also classified from the questionnaire data. There was examiner agreement for 75 instances of migraine (with and without aura), 76 of tension-type headache, 44 of cervicogenic headache, eight of mixed headaches, five of headaches associated with substance abuse, one of headache associated with temporomandibular dysfunction and six headaches associated with a sinus condition. There were 36 occasions of disagreement. Some subjects reported the same headache as two different headaches with the difference being, for example, a greater or lesser intensity or duration. In line with the aim of this study and the analysis of physical data, each subject was grouped into one of two categories based on examiner agreement, as either having a cervicogenic headache or not having a cervicogenic headache (non-cervicogenic) as one of their headache types. For this purpose, the 36 cases of disagreement were categorized as non-cervicogenic. These headache classifications derived from the questionnaire (cervicogenic or non-cervicogenic) were cross-tabulated with the headache grouping gained from the physical impairment data to determine agreement between symptomatic and physical features. Finally, the physical impairments were compared between the groups with and without cervicogenic headache as one of the multiple headaches and the control group.
Results

Table 1
page 4

Table 2

Table 3
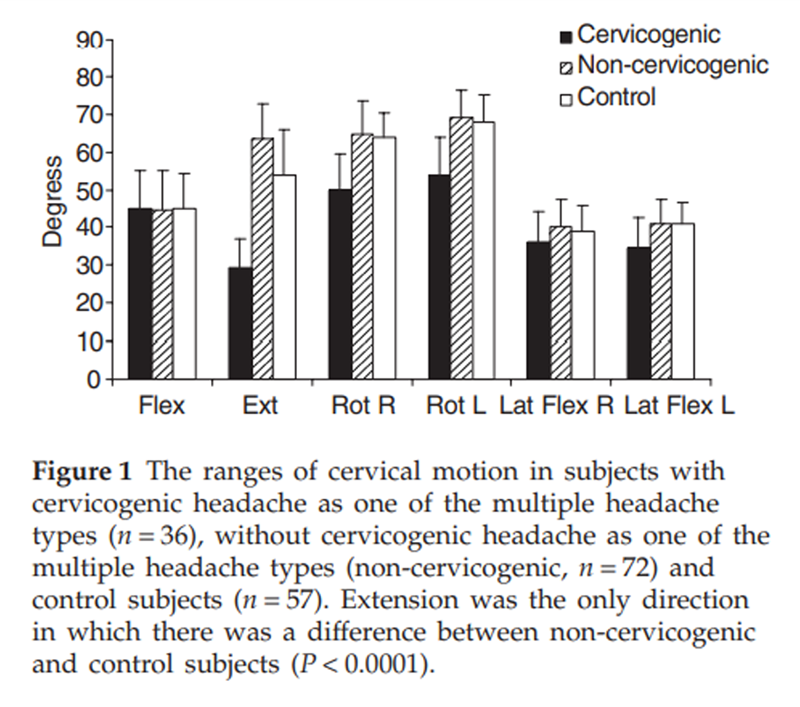
Figure 1
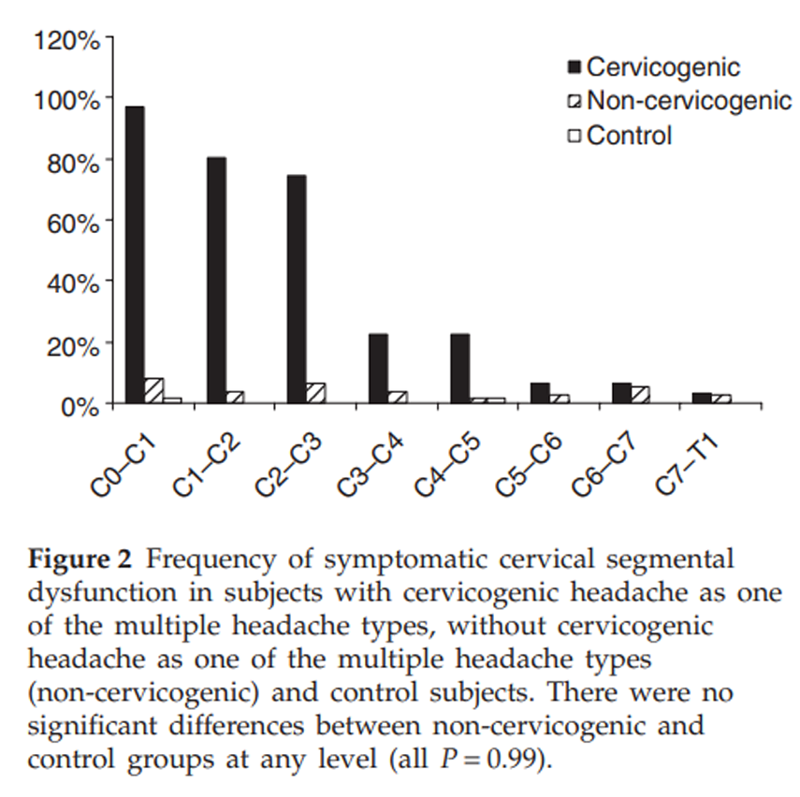
Figure 2
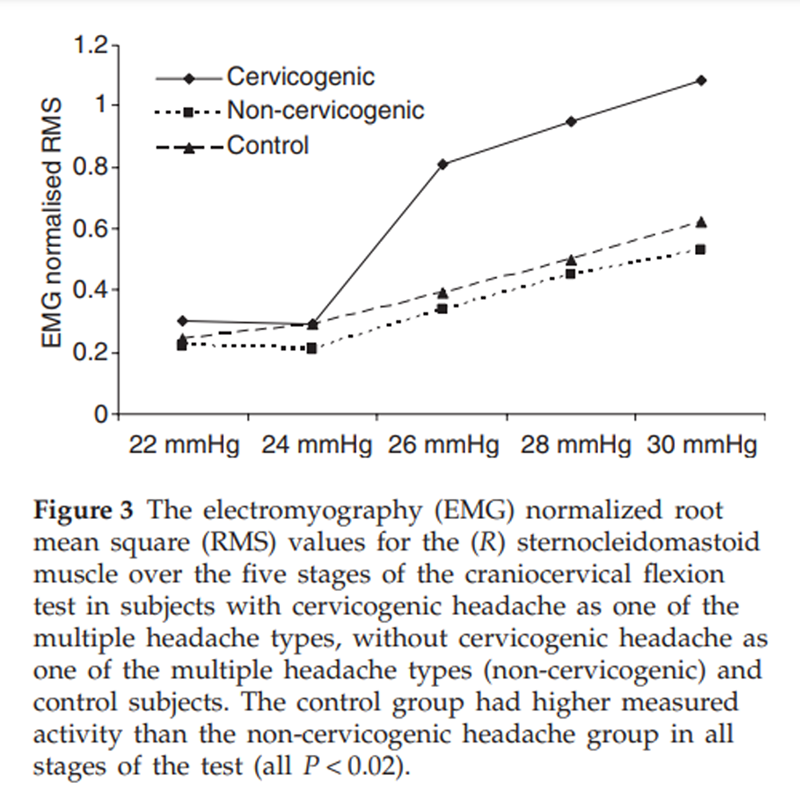
Figure 3 Table 1 presents the results of the discriminant and cluster analyses. The discriminant analysis indicated that 36 of the 108 subjects with two or more headaches had a cervicogenic headache as one of their multiple headache types on the basis of the combined presence of joint, movement and muscle impairment. The cluster analysis created three distinct groups. These groups were predominantly clustered on the variables of cervical spine extension and the presence of palpable cervical segmental joint dysfunction. The first and second clusters were inclusive of subjects from the control group and from the headache group where, according to the discriminant analysis, none of the multiple headaches was classifiable as cervicogenic. The third cluster generated included all subjects with a cervicogenic headache as one of their headache types (according to the discriminant analysis), but also one subject with a non-cervicogenic headache as well as 12 control subjects. The major variable of difference for the one non-cervicogenic headache subject was a lesser range of neck extension (mean = 40°). Similarly, the 12 control subjects who were clustered into the third group were clustered on neck extension and they demonstrated an even lesser range of cervical extension (mean = 29.5°). However, similar to subjects in clusters one and two, none of these subjects showed upper cervical joint dysfunction or differences in SCM EMG values for the CCFT. Table 2 presents the subject demographics for all groups, indicating that both headache subgroups had a long history of headache.
In the classification of headache type from the questionnaires, there was examiner agreement that 40 of the 108 subjects had a cervicogenic headache as one of the multiple headaches types. The remaining 68 subjects were judged not to have a headache classifiable as cervicogenic as one of the multiple headache types (non-cervicogenic headache). These classifications were cross-tabulated with the cervicogenic headache and non-cervicogenic subjects identified in the discriminant analysis (Table 3). There was a discrepancy between the classification systems for 14 of the 108 subjects (12.9%).
Figures 13 present the values of the three measures of musculoskeletal impairment for the group with a cervicogenic headache as one of the multiple headache types, the group without cervicogenic headache as one of the headache types and the control group. The distinction of the group with cervicogenic headache as one of the headache types is evident for the pattern of measures found to characterize this headache type, namely restricted cervical extension (Fig. 1), the presence of palpably painful upper cervical joint dysfunction (Fig. 2) and the higher measured levels of activity in the SCM in the CCFT in the three higher level stages of the test (Fig. 3). To answer the question whether the non-cervicogenic headache group had any musculoskeletal impairment associated with their headache, their values were compared with the control group. Post hoc t-tests determined no differences between the groups for range of movement in any direction (all P = 0.99) with the exception of extension, where the non-cervicogenic headache group had greater range than the control group (P < 0.0001). Likewise, there was no significant difference (Fisher's exact test) between the non-cervicogenic and control groups in the presence of palpably painful upper cervical joint dysfunction (all P = 0.99, where cell counts permitted analysis). There were differences (t-tests) between measured activity in the SCM between the non-cervicogenic and control groups in each stage of the test (all P < 0.02), with the control group having more measured activity than the non-cervicogenic headache group.
Discussion
The co-occurrence of two or more headache types is common in patients presenting to headache or pain clinics with frequent intermittent headaches. [9, 10] This was also found to be the case in our community-based study, where 55% of volunteers with headache reported two or more headache types. Neck pain is often associated with the common frequent intermittent headache types, but this study has determined that a pattern of cervical musculoskeletal impairment is characteristic of one headache type only (cervicogenic). Subjects could have two or more frequent intermittent headaches without evidence of physical impairment in the cervical musculoskeletal system. Thus, even though a complex history of concurrent headaches can be prolonged and neck pain may be reported, unless one of the component headache types is classifiable as cervicogenic, there should be no expectation that there is secondary involvement of a cervical musculoskeletal disorder.
The discriminant analysis (Table 1) identified that 36 subjects were categorized as having a cervicogenic headache, based on the pattern of physical impairment, as one of their headache types and 72 were categorized as not having a cervicogenic headache as one of their multiple headache types (non-cervicogenic). The findings, when both cluster analysis and discriminant analysis were applied to the data, revealed the importance of the pattern of musculoskeletal impairment in the categorization of cervicogenic headache, rather than the presentation of just a single feature, such as a restricted range of neck movement. The range of neck extension was the variable responsible for the cluster of subjects into three groups. The range of cervical extension was greatest in subjects in cluster 1 (36 non-cervicogenic headache subjects and 14 control subjects). Thirty-six headache subjects classed as non-cervicogenic by the discriminant analysis (35 in cluster 2 and one subject in cluster 3) as well as 43 of the control subjects (31 in cluster 2 and 12 in cluster 3) demonstrated a lesser range of cervical extension. However, in these subjects this singular sign was not accompanied by palpably painful cervical segmental dysfunction or by the more marked muscle impairment in the CCFT. In contrast, the 36 subjects who were classified on the discriminant analysis as having a cervicogenic headache had the least range of cervical extension, but in this case it was associated with palpably painful upper cervical segmental joint dysfunction and muscle impairment in the CCFT, i.e. these subjects demonstrated a combination of joint, movement and muscle impairment.
Restriction of neck motion and tenderness to external pressure over the upper cervical or occipital region on the symptomatic side are the main physical criteria listed in Sjaastad et al.'s [21] classification criteria for cervicogenic headache. However, range of cervical movement is highly variable in the general population and decreases as a factor of age. [22] Thus, because of its variability between people, it cannot be relied upon as a single sign, as shown in the cluster analysis of this study, supporting Bogduk's [23] contention of the futility of a single physical sign to indicate a cervical origin of headache. It is well recognized that tenderness over neck or cranial muscles is a common finding in cervicogenic, migraine and tension-type headaches as well as in asymptomatic populations. [2428] It is contended that this feature is insufficient for accurate differential diagnosis of cervicogenic headache, a point also made by van Suijlekom et al. [29] However, this and our previous study have shown that cervicogenic headache, whether suffered as a single or one of multiple headaches, can be distinguished from other types of frequent intermittent headache through the presence of a pattern of musculoskeletal impairment, decreased range of cervical movement, in combination with palpably painful upper cervical segmental dysfunction and impairment in cervical flexor muscle function as measured in the CCFT.
Importantly, this study has revealed the similarity of the cervical musculoskeletal measures in subjects without a cervicogenic headache as one of their headache types and in control subjects (Figs 13). Paradoxically, the non-cervicogenic headache group had a greater range of cervical extension than the control group and performed a little better on the CCFT (less measured activity in the SCM). Thus, there is no evidence from this study for a cervical musculoskeletal component of frequent intermittent headaches even when suffered as multiple headache types, when one of the headaches cannot be classified as cervicogenic. These findings concur with those of Zwart [30], who found no difference in range of cervical motion, and Marcus et al. [28], who found no difference in the incidence of palpably painful cervical segmental joint dysfunction between migraine, tension-type headache and control subjects.
There is considerable overlap in headache symptoms, including the symptom of neck pain, in the common frequent intermittent headache types of migraine without aura, tension-type and cervicogenic headache. [27] Classification can be more challenging when patients report multiple headache types. There was an 84% concordance between the predicted categorization of the discriminant analysis on physical signs and the broad classification from the questionnaires for the presence or not of a cervicogenic headache as one of the multiple headache types. However, there were 14 subjects who were misdiagnosed symptomatically. This probably reflects the difficulties arising from the symptomatic overlap in common frequent intermittent headaches, which could be assisted by a specific physical examination of the neck.
On the basis of the results of this study, it is suggested that when patients present with concurrent multiple headaches, cervicogenic headache as one of the headache types can be differentiated from other frequent headache types with greater confidence when a pattern of headache suggestive of cervicogenic headache is associated with a pattern of cervical musculoskeletal impairment inclusive of symptomatic dysfunction in the upper cervical joints, associated with restricted cervical motion and impairment in cervical flexor muscle function. Furthermore, all tests can be applied in a clinical setting. A final step is to validate this clinical diagnosis of cervicogenic headache against the current gold standard of diagnostic blockades. [20]
References:
Headache Classification Subcommittee of the International Headache Society.
The International Classification of Headache Disorders, 2nd Edition.
Cephalalgia 2004; 24 (Suppl. 1):1151.Antonaci F, Fredriksen T, Sjaastad O.
Cervicogenic headache: clinical presentation,
diagnostic criteria and differential diagnosis.
Curr Pain Headache Rep 2001; 5:38792.Fishbain D, Lewis J, Cole B, Cutler R, Rosomoff R, Rosomoff H.
Do the proposed cervicogenic headache diagnostic criteria demonstrate
specificity in terms of separating cervicogenic headache from migraine.
Curr Pain Headache Rep 2003; 7:38794.Rokicki L, Semenchuk E, Bruehl S, Lofland K, Houle T.
An examination of the validity of the IHS classification system for
migraine and tension-type headache in the college student population.
Headache 1999; 39:7207.Srikiatkhachorn A, Phanthumchinda K.
Prevalence and clinical features of chronic daily headache in a headache clinic.
Headache 1997; 37:27780.Xiaobin Y, Cook A, Hamill-Ruth R, Rowlingson J.
Cervicogenic headache in patients with presumed migraine:
missed diagnosis or misdiagnosis?
J Pain 2005; 6:7003.Hagen K, Einarsen C, Zwart J, Svebak S, Bovim G.
The co-occurrence of headache and musculoskeletal
symptoms amongst 51,050 adults in Norway.
Eur J Neurol 2002; 9:52733.Jull G, Amiri M, Bullock-Saxton J, Darnell R, Lander C.
Cervical Musculoskeletal Impairment in Frequent Intermittent Headache.
Part 1: Subjects with Single Headaches
Cephalalgia 2007 (Jul); 27 (7): 793802Fishbain D, Cutler R, Cole B, Rosomoff H, Rosomoff R.
International Headache Society headache diagnostic patterns
in pain facility patients.
Clin J Pain 2001; 17:7893.Pfaffenrath V, Kaube H.
Diagnostics of cervicogenic headache.
Funct Neurol 1990; 5:15964.DallAlba P, Sterling M, Treleaven J, Edwards S, Jull G.
Cervical range of motion discriminates between asymptomatic
and whiplash subjects.
Spine 2001; 26:20904.Jull G, Bogduk N, Marsland A.
The Accuracy of Manual Diagnosis for Cervical
Zygapophysial Joint Pain Syndromes
Med J Aust 1988 (Mar 7); 148 (5): 233236Jull G, Zito G, Trott P, Potter H, Shirley D, Richardson C.
Inter-examiner reliability to detect painful upper cervical joint dysfunction.
Aust J Physiother 1997; 43:1259.Dumas JP, Arsenault AB, Boudreau G, Magnoux E, Lepage Y, Bellavance A et al.
Physical impairments in cervicogenic headache:
traumatic vs. nontraumatic onset.
Cephalalgia 2001; 21:88493.Watson D, Trott P.
Cervical Headache: An Investigation of Natural Head Posture
and Upper Cervical Flexor Muscle Performance
Cephalalgia 1993 (Aug); 13 (4): 272284Rankin G, Stokes M, Newham D.
Size and shape of the posterior neck muscles measured by ultrasound
imaging: normal values in males and females of different ages.
Man Ther 2005; 10:10615.Falla D, Jull G, Hodges P.
Neck pain patients demonstrate reduced activity of the deep neck flexor
muscles during performance of the craniocervical flexion test.
Spine 2004; 29:210814.Jull G, Barrett C, Magee R, Ho P.
Further characterisation of muscle dysfunction in cervical headache.
Cephalalgia 1999; 19:17985.Jull G, Kristjansson E, DallAlba P.
Impairment in the cervical flexors:
a comparison of whiplash and insidious onset neck pain patients.
Man Ther 2004; 9:8994.Treleaven J, Jull G, Sterling M:
Dizziness and Unsteadiness Following Whiplash Injury:
Characteristic Features and Relationship
with Cervical Joint Position Error
J Rehabil Med 2003 (Jan); 35 (1): 3643Sjaastad O, Fresriksen TA, Pfaffenrath V.
Cervicogenic headache: diagnostic criteria.
Headache 1998; 38:4425.Chen J, Solinger AB, Poncet JF, Lantz CA.
Meta-analysis of normative cervical motion.
Spine 1999; 24:15718.Bogduk N.
The neck and headaches.
Neurol Clin 2004; 22:15171.Bovim G, Sand T.
Cervicogenic headache, migraine without aura and tension-type headache.
Diagnostic blockade of greater occipital and supra-orbital nerves.
Pain 1992; 51:438.Graff-Radford SB, Reeves JL, Jaeger B.
Management of chronic head and neck pain:
effectiveness of altering factors perpetuating myofascial pain.
Headache 1987; 27:18690.Jensen R, Rasmussen BK.
Muscular disorders in tensiontype headache.
Cephalalgia 1996; 16:97103.Langermark M, Jensen K, Jensen TS, Olesen J.
Pressurepain thresholds and thermal nociceptive thresholds
in chronic tension-type headache.
Pain 1989; 38:20310.Marcus DA, Scharff L, Mercer S, Turk DC.
Musculoskeletal abnormalities in chronic headache:
a controlled comparison of headache diagnostic groups.
Headache 1999; 39:217.van Suijlekom H, de Vet H, van den Berg S, Weber W.
Interobserver reliability in physical examination of
the cervical spine in patients with headache.
Headache 2000; 40:5816.Zwart JA.
Neck mobility in different headache disorders.
Headache 1997; 37:611.
Return to HEADACHE
Since 3-06-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |