

Primary Care Management of Non-specific Low Back Pain:
Key Messages from Recent Clinical GuidelinesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Medical J Australia 2018 (Apr 2); 208 (6): 272–275 ~ FULL TEXT
Matheus Almeida, Bruno Saragiotto, Bethan Richards, Chris G Maher
Institute of Rheumatology and Orthopaedics,
Royal Prince Alfred Hospital,
Sydney, NSW.
Introduction: Research in the past decade supports some major changes to the primary care management of non-specific low back pain (LBP). The present article summarises recommendations from recently published United Kingdom, Danish, Belgian and United States guidelines to alert readers to the important changes in recommendations for management, and the recommendations from previous guidelines that remain unchanged.
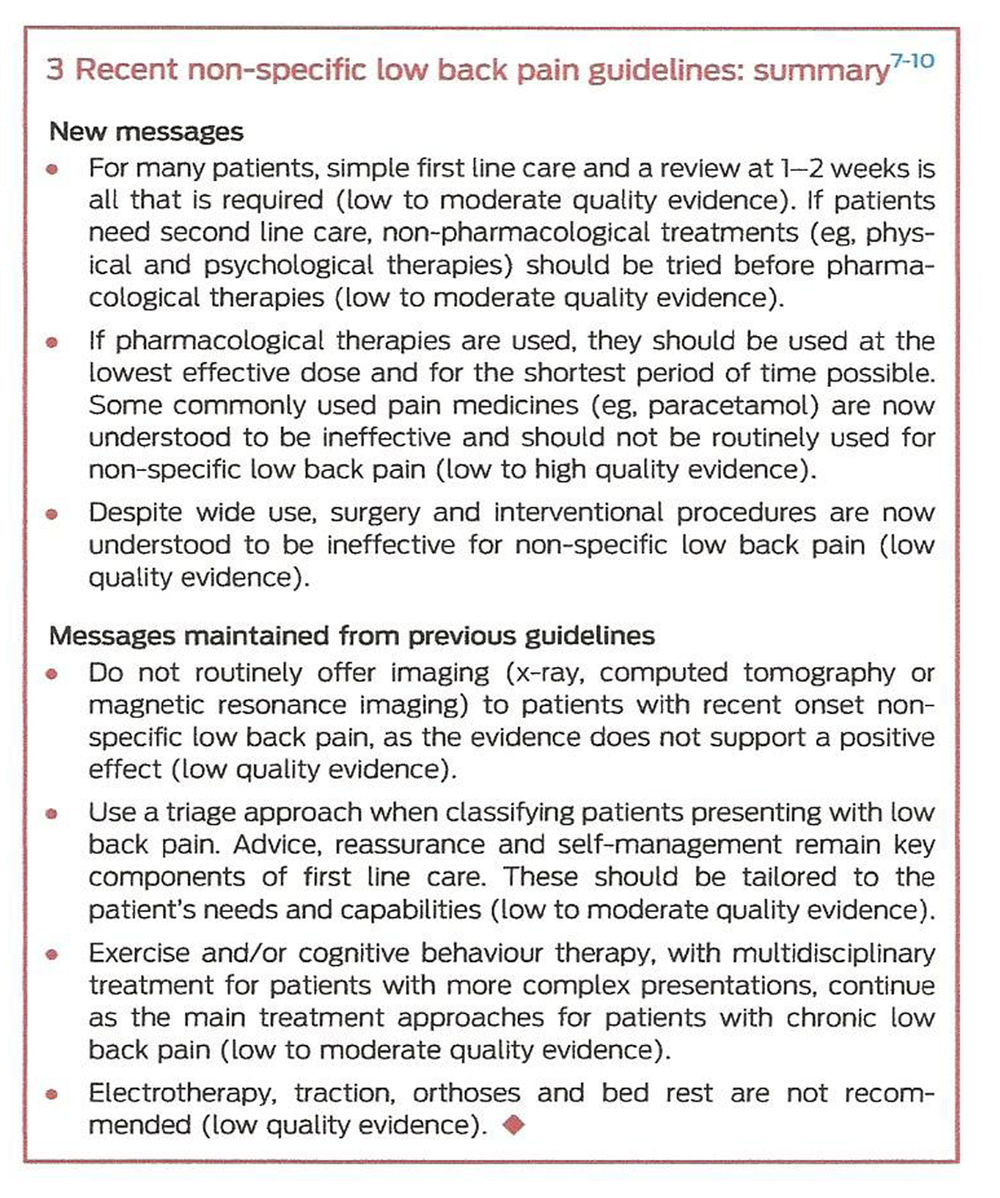
Main recommendations: Use a clinical assessment to triage patients with LBP. Further diagnostic workup is only required for the small number of patients with suspected serious pathology. For many patients with non-specific LBP, simple first line care (advice, reassurance and self-management) and a review at 1–2 weeks is all that is required. If patients need second line care, non-pharmacological treatments (eg, physical and psychological therapies) should be tried before pharmacological therapies. If pharmacological therapies are used, they should be used at the lowest effective dose and for the shortest period of time possible. Exercise and/or cognitive behavioural therapy, with multidisciplinary treatment for more complex presentations, are recommended for patients with chronic LBP. Electrotherapy, traction, orthoses, bed rest, surgery, injections and denervation procedures are not recommended for patients with non-specific LBP.
Changes in management as a result of the guidelines: The major changes include:
emphasising simple first line care with early follow-up;
encouraging non-pharmacological treatments over pharmacological treatments; and
recommending against the use of surgery, injections and denervation procedures.
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is a major health problem worldwide. According to the Global Burden of Disease Study 2016, LBP continues to be the leading global cause of years lived with disability. [1] The 2014–15 National Health Survey found that about 16% of Australians reported suffering from back pain over the previous year, being more common in older people (aged 65–79 years) and with similar rates between men and women. [2] About half the people who experience LBP seek care, [3] with LBP the most frequent musculoskeletal condition seen in general practice in Australia. [2] In 2015–16, LBP was responsible for about three in every 100 general practitioner-patient encounters. [2]
Episodes of acute LBP usually have a good prognosis, with rapid improvement within the first 6 weeks. [4] After this period, the improvement slows, and over 40% of patients may develop chronic LBP, [5] although usually with only low levels of pain and disability. [4, 5] About one-third of patients who initially recover suffer episodes of recurrence in the next year. [6]
In the past decade, there has been considerable research evaluating the management of LBP. This research provides the rationale for a quite different approach than was previously recommended in clinical practice guidelines. The present article distils the information from the most recent national clinical practice guidelines (from the United Kingdom, Denmark, Belgium and the United States) [7–10] to provide an update on the primary care management of non-specific LBP. We provide Grading of Recommendations Assessment, Development and Evaluation (GRADE) quality of evidence for eachrecommendation reportedinthese guidelines. The GRADE system rates the quality of evidence on a scale from very low to high, according to the level of confidence given the evidence available. [11] This article focuses on alerting readers to the important changes in management recommendations, and the recommendations from previous guidelines that remain unchanged.
Classifying and diagnosing low back pain
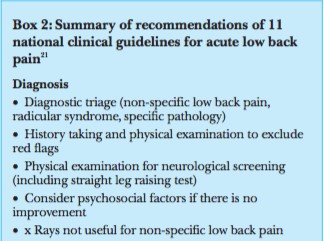
Guidelines continue to recommend a triage approach to classifying LBP. A diagnostic triage approach is used to identify patients whose LBP arises beyond the lumbar spine (eg, renal, aortic dissection), those with neurological deficit (radiculopathy, spinal canal stenosis, cauda equina syndrome), those with suspected or confirmed serious spinal pathology (malignancy, infection, fracture), and those with inflammatory disease (spondyloarthritis); remaining patients are considered to have non-specific LBP. Imaging is still not indicated for non-specific LBP. The complete diagnostic triage process for LBP in primary care has been comprehensively described by Bardin and colleagues in a recent article in the MJA. [12]
What is new in recent guidelines is a warning on the limited diagnostic accuracy of some individual red flags that were previously endorsed. [7, 9] Examples of red flags with limited diagnostic accuracy include thoracic pain, night pain and age over 50 years to screen for cancer. [13] The contemporary approach relies on a smaller set of red flags than previously and emphasises the use of clusters of red flags along with clinical expertise to guide decision making. [12]
Treating non-specific low back pain
Risk assessment and stratification
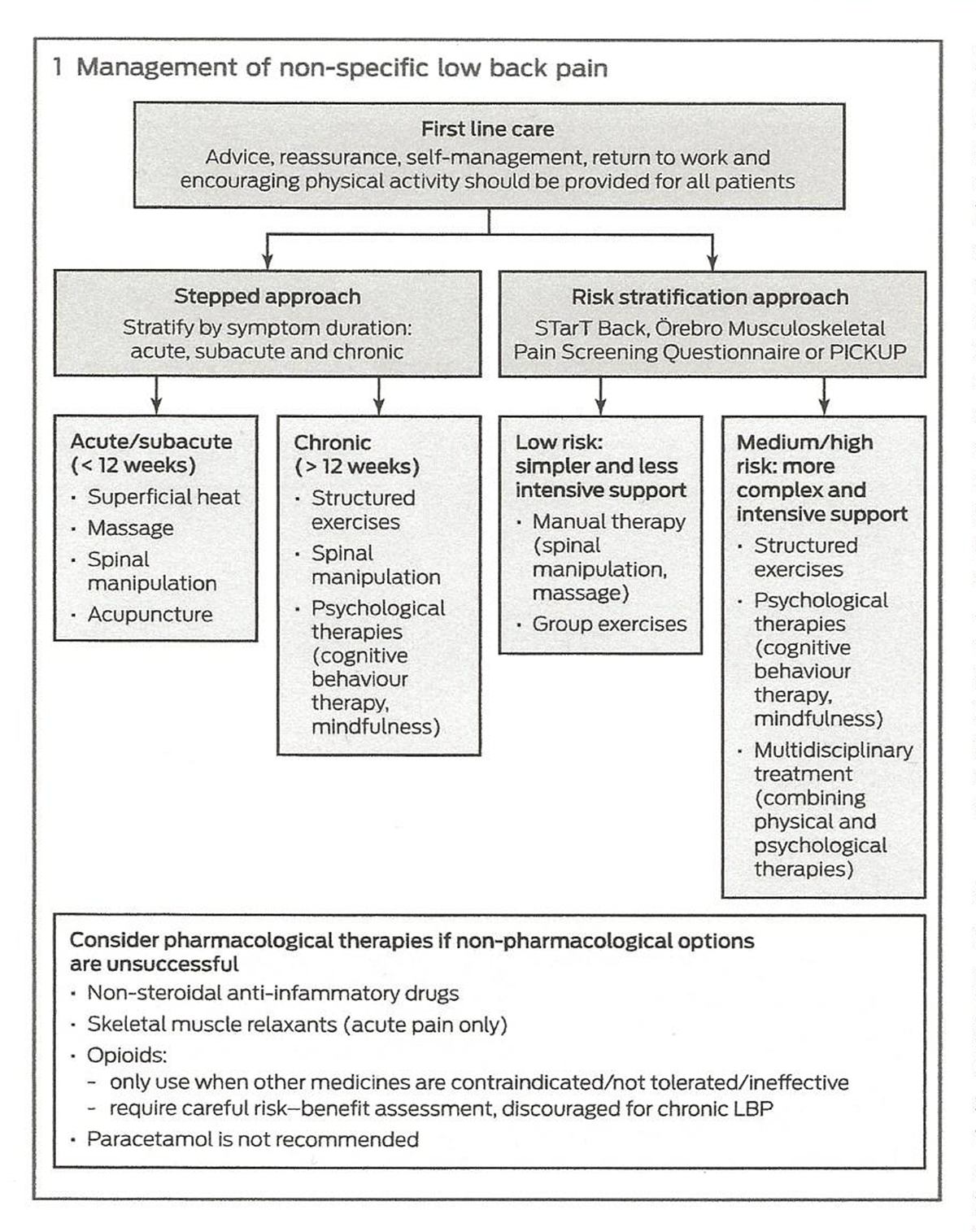
Box 1 There are now two approaches to guide the management of patients with non-specific LBP (Box 1). The traditional approach involves stratifying patients into those with acute (less than 6 weeks), subacute (6–12 weeks) or chronic (more than 12 weeks) symptom duration, and then use a stepped approach to care. The stepped approach begins with more simple therapies and only progresses to more complex treatments if there is insufficient improvement. This approach continues to be recommended in the US [10] and Danish [8] guidelines.
A newer approach, endorsed in the UK National Institute for Health and Care Excellence [7] and Belgian [9] guidelines, uses simple risk prediction tools to match patients to treatment packages based on their risk of poor clinical outcome: STarT Back (http://www.keele.ac.uk/sbst/startbacktool), [14] Örebro Musculoskeletal Pain Screening Questionnaire (https://painhealth.csse.uwa. edu.au/pain-self-checks/orebro-musculoskeletal-pain-screeningquestionnaire/) [15] and PICKUP (http://pickuptool.neura.edu.au). [16] These tools are freely available online; at present, it is unclear which is best.
First line care
Because many patients with non-specific LBP will improve over time regardless of the treatment received, recent guidelines now recommend minimal if any treatment as the starting point in care. [7–10, 17] For this approach to be sensible, it presumes that the clinician has conducted a thorough clinical assessment and that they are confident that the patient has non-specific LBP. It also presumes that if the clinician has used a risk prediction tool, the patient has screened as low risk for developing persistent pain. Guidelines previously recommended simple analgesics (eg, paracetamol) as part of first line care; however, these are now discouraged based on recent evidence that paracetamol is no more effective than placebo for non-specific LBP. [18]
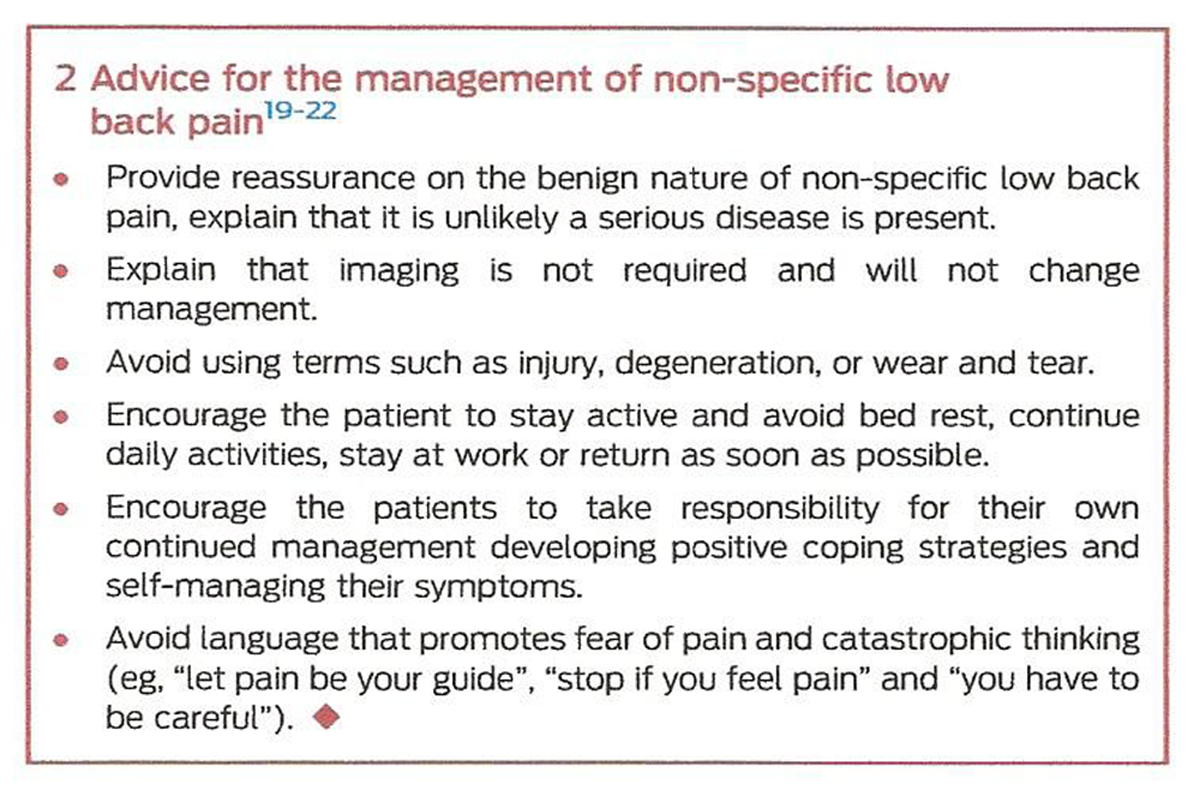
Box 2 Advice, reassurance and encouragement of physical activity continue to be recommended in guidelines as first line care for all patients with non-specific LBP, with overall low to moderate quality evidence (Box 1). Guidelines also reinforce the importance of teaching patients how to self-manage their LBP. [7–10] Important messages (Box 2) to convey to patients are that non-specific LBP is benign; most people have a favourable prognosis with substantial improvement in the first month; it is unlikely that there is a serious disease present; and imaging is not required and will not change management. [19] Misconceptions about LBP and its management, inappropriate fear avoidance beliefs and expectation of poor recovery should also be addressed. [20, 21]
Guidelines emphasise that patients should be encouraged to stay active and avoid bed rest, continue daily activities, stay atwork (or return as soon as possible), and self-manage their symptoms using simple strategies such as superficial heat. [7, 22] Although this approach appears to be simple, a survey of Australian general practice care using Bettering the Evaluation and Care of Health (BEACH) data revealed that only 20% of patients with LBP are provided with education and advice. [23] GPs should review patients’ progress at 1–2 weeks to make sure they have recovered. [12]
Second line care
Non-pharmacological treatment. All four recent guidelines place a greater emphasis on nonpharmacological treatments than previously but vary somewhat in the degree of emphasis. For example, the US guideline [10] is very clear in recommending that non-pharmacological treatments should be used first, with pharmacological options reserved for those who do not respond. However, the Danish guideline [8] is more extreme and does not recommend any pharmacological treatments at any stage of management.
There are now more consistent recommendations in favour of manual therapy (such as massage and spinal manipulation) and psychological therapies (cognitive behavioural therapy is preferred) as second line non-pharmacological options, as they can provide small to moderate improvements for pain and function with mostly low to moderate quality evidence. [7–10] While the US guideline [10] still does not recommend exercise in acute LBP, the UK and Belgian guidelines [7, 9] now recommend that manual and psychological therapies should be used as part of a treatment program combined with exercise to achieve intermediate and long term benefits for pain and disability (overall low to moderate quality evidence). The UK and Danish guidelines [7, 8] no longer recommend acupuncture in the treatment of LBP; the US guideline [10] still supports its use in acute patients but acknowledges that it may only have a small effect on pain.
For patients with chronic LBP or who are judged to be at medium to high risk by the stratification tools at initial contact, the recent guidelines endorse more complex and intensive treatments (Box 1). All guidelines continue to recommend exercise for chronic LBP but now also endorse various types of exercise (such as Tai Chi, [7, 10] Yoga, [7, 10] motor control, [8, 10] and aerobic [7]) and suggest group exercise to minimise costs to the patient. [7, 9] The type of exercise seems less important for effectiveness than how well the exercise program is structured. [7, 9] The guidelines recommend exercise for chronic LBP as a sole therapy (low to moderate quality evidence) and as a component of other recommended treatment programs such as multidisciplinary rehabilitation (moderate quality evidence). Multidisciplinary rehabilitation is still recommended for patients classified as high risk by stratification tools and for patients with chronic LBP who have not responded to uni-disciplinary approaches, and has been shown to result in moderate improvement in pain in the short term (Box 1). [7–10] However, the long term effects of multidisciplinary rehabilitation are smaller. [8]
Non-pharmacological therapies not endorsed in recent LBP guidelines are electrotherapies, [7. 9, 10] taping (eg, kinesio taping), [10] any type of brace and traction (low quality evidence). [7, 9, 10] These recommendations are unchanged from previous guidelines, except for kinesio taping, which is a new treatment not widely used at the time of production of the previous guidelines.
Pharmacological interventions. As mentioned above, recent clinical guidelines have discouraged the use of pharmacotherapy in first line care and suggest that medications should only be considered in patients who have not adequately responded to non-pharmacological interventions. [7–9] Guidelines now more explicitly emphasise that GPs should always discuss the known potential harms and realistic benefits of the medications with their patients before prescribing. There are also more firm recommendations that these medications should be offered for the shortest possible period at the lowest effective dose, taking into account gastrointestinal problems and other side effects. [7–10] Medications should be reviewed regularly for evidence of benefit and should be ceased if there has been no improvement. Such caution regarding the use of pain medicines is most strongly given in relation to opioid medicines.
Previous guidelines recommended paracetamol as the first option in the management of LBP; however, it is no longer recommended in updated guidelines for either acute or chronic patients (high and low quality evidence, respectively). [7–10] A recent Cochrane systematic review (1,825 participants) found that paracetamol does not result in better outcomes compared with placebo for patients with acute LBP, and its effect on chronic LBP is uncertain. [24] Non-steroidal anti-inflammatory drugs are endorsed in three of the four guidelines (moderate quality evidence), [7, 9, 10] which is consistent with a recent systematic review demonstrating the efficacy of this class of medicine for both acute and chronic LBP. [25] Howeer, the effect size for acute LBP is small (– 6.1 points [95% CI, – 9.5 to – 2.8] on a 0–100 scale) and some have argued that this may be too small to be clinically worthwhile. [25] Muscle relaxants continue to be recommended by the US guideline for acute but not chronic LBP, with overall moderate quality evidence. [10]
Opioids are one of the most commonly prescribed medications for LBP in primary care [26] but there is now greater appreciation of their potential for harm. [27] All recent guidelines suggest caution with the use of these medicines, but provide slightly different recommendations. The UK guideline [7] now only supports the use of weak opioids, in contrast to its previous recommendation of strong opioids. [28] Moreover, the recommendation is qualified, with opioids recommended only for cases of acute LBP where non-steroidal anti-inflammatory drugs are contraindicated, not tolerated or ineffective. The UK guideline [7] explicitly recommends against the use of opioids for chronic LBP. The Belgian guideline [9] differs from that of the UK by recommending opioids for chronic LBP, but advises that they should not be routinely used. The US guideline [10] promotes a slightly different position, recommending the use of opioids as a last resort for patients with chronic LBP who have not responded to other nonpharmacological and pharmacological options (moderate quality evidence). All guidelines consistently highlight that opioids should only be used if the expected benefits outweigh the risks for patients, and should not be used long term as they are associated with important harms, such as addiction and accidental overdose.
Invasive non-surgical treatment. This category of treatment includes injections of corticosteroids, anaesthetic agents, sclerosing agents and products derived from patients’ own tissues (platelet-rich plasma and stem cells) that are purported to promote healing. It also includes denervation procedures focused on the innervation of the anatomical structure that is believed to be the nociceptive source of the patient’s LBP. The recent guidelines continue to discourage the use of any type of spinal injection or denervation procedure for non-specific LBP (low quality evidence). [7–9]
The UK guideline [7] recommends the use of epidural injections of local anaesthesia and corticosteroids only in patients with acute and severe sciatica. They are not recommended for patients with non-specific LBP (very low to low quality evidence).
Radiofrequency denervation is cautiously supported by the UK guideline, [7] but is reserved for moderate or severe chronic LBP when previous conservative treatment has failed and if the pain is felt to come from the facet joints (low quality evidence). However, the results of the subsequently published Mint study [29] (three multicentre randomised controlled trials; 681 patients) demonstrated that denervation procedures targeting facet joints, sacroiliac joints or intervertebral disks do not have clinically important effects.
Surgical treatments. In the past, surgical interventions were recommended for patients with non-specific LBP who had failed conservative care; however, this approach is now discouraged. None of the recent clinical guidelines recommend surgery for patients with non-specific LBP (low quality evidence). The UK guideline [7] is very clear: “Do not offer spinal fusion for people with low back pain unless as part of a randomised controlled trial” and “Do not offer disc replacement in people with low back pain”. The UK guideline only recommends consideration of surgery for sciatica when conservative care has not worked and there are radiological and clinical findings to justify surgery (low quality evidence).
Box 3
Conclusion
Recent guidelines provide important changes and emphasise recommendations that are still endorsed in the management of nonspecific low back pain (Box 3). The key messages include discouraging routine imaging, emphasising simple first line care with early follow-up, encouraging non-pharmacological treatments over pharmacological treatments (opioids and paracetamol should be avoided), and recommending against the use of surgery, injections and denervation procedures.
Acknowledgments
Matheus Almeida is supported by a São Paulo Research Foundation grant. Chris Maher holds a fellowship funded by the National Health and Medical Research Council.
Competing interests:
No relevant disclosures.
References:
Disease GBD;
Global, Regional, and National Incidence, Prevalence, and Years Lived With
Disability for 328 Diseases and Injuries for 195 Countries, 1990-2016:
A Systematic Analysis for the Global Burden of Disease Study 2016
Lancet. 2017 (Sep 16); 390 (10100): 1211–1259Australian Institute of Health and Welfare.
Back problems: web report Canberra: AIHW, 2017.
https://www.aihw.gov.au/reports/arthritis-othermusculoskeletal-
conditions/back-problems/what-areback-problems
(viewed Feb 2018).Ferreira ML, Machado G, Latimer J, et al.
Factors defining care-seeking in low back paine a meta-analysis of population based surveys.
Eur J Pain 2010; 14: 747.e1-7.da Costa LMC, Maher CG, Hancock MJ, et al.
The prognosis of acute and persistent low-back pain: a meta-analysis.
CMAJ 2012; 184: E613-E624.da Costa LMC, Maher CG, McAuley JH, et al.
Prognosis for patients with chronic low back pain: inception cohort study.
BMJ 2009; 339: b3829.Stanton TR, Henschke N, Maher CG, et al.
After an episode of acute low back pain, recurrence is unpredictable
and not as common as previously thought.
Spine 2008; 33: 2923-2928.National Institute for Health and Care Excellence (NICE):
Low Back Pain and Sciatica in Over 16s: Assessment and Management (PDF)
NICE Guideline, No. 59 2016 (Nov): 1–1067Stochkendahl MJ, Kjaer P, Hartvigsen J et al.
National Clinical Guidelines for Non-surgical Treatment of Patients with
Recent Onset Low Back Pain or Lumbar Radiculopathy
European Spine Journal 2018 (Jan); 27 (1): 60–75Van Wambeke P, Desomer A, Ailliet L, et al.
Low Back Pain and Radicular Pain: Assessment and Management
KCE report 287Cs. Brussels: Belgian Health Care Knowledge Centre (KCE), 2017.Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Guyatt GH, Oxman AD, Vist GE, et al.
GRADE: An Emerging Consensus on Rating Quality of Evidence
and Strength of Recommendations
British Medical Journal 2008 (Apr 26); 336 (7650): 924–926Bardin LD, King P, Maher CG.
Diagnostic triage for low back pain: a practical approach for primary care.
Med J Aust 2017; 206: 268-273.Downie A, Williams CM, Henschke N, et al.
Red flags to screen for malignancy and fracture in patients with low back pain: systematic review.
BMJ 2013; 347: f7095.Hill JC, Whitehurst DG, Lewis M et al.
Comparison of Stratified Primary Care Management for Low Back Pain
with Current Best Practice (STarT Back): A Randomised Controlled Trial
Lancet. 2011 (Oct 29); 378 (9802): 1560–1571Linton SJ, Nicholas M, MacDonald S.
Development of a short form of the Örebro Musculoskeletal Pain Screening Questionnaire.
Spine 2011; 36: 1891-1895.Traeger AC, Henschke N, Hübscher M, et al.
Estimating the Risk of Chronic Pain: Development and
Validation of a Prognostic Model (PICKUP) for
Patients with Acute Low Back Pain
PLoS Med. 2016 (May 17); 13 (5): e1002019NSW Agency for Clinical Innovation.
Management of People with Acute Low Back Pain
Agency for Clinical Innovation 2016 Chatswood; NSW Health (39 pages)Williams CM, Maher CG, Latimer J, et al.
Efficacy of paracetamol for acute low-back pain: a double-blind, randomised controlled trial.
Lancet 2014; 384: 1586-1596.Hoffmann TC, Del Mar CB, Strong J, et al.
Patients’ expectations of acute low back pain management: implications for evidence uptake.
BMC Fam Pract 2013; 14: 7.Main CJ, Buchbinder R, Porcheret M, et al.
Addressing patient beliefs and expectations in the consultation.
Best Pract Res Clin Rheumatol 2010; 24: 219-225.Main CJ, Foster N, Buchbinder R.
How important are back pain beliefs and expectations for satisfactory recovery from back pain?
Best Pract Res Clin Rheumatol 2010; 24: 205-217.ÓSullivan P, Lin TB.
Acute low back pain. Beyond drug therapies.
Pain Manag Today 2014; 1: 8-13.Williams CM, Maher CG, Hancock MJ et al.
Low Back Pain and Best Practice Care: A Survey of General Practice Physicians
Archives of Internal Medicine 2010 (Feb 8); 170 (3): 271–277Saragiotto BT, Machado GC, Ferreira ML, et al.
Paracetamol for low back pain.
Cochrane Database Syst Rev 2016; (6): CD012230.Machado GC, Maher CG, Ferreira PH, et al.
Non-steroidal anti-inflammatory drugs for spinal pain: a systematic review and meta-analysis.
Ann Rheum Dis 2017; 76: 1269-1278.Kea B, Fu R, Lowe RA, et al.
Interpreting the National Hospital Ambulatory Medical Care Survey:
United States emergency department opioid prescribing, 2006-2010.
Acad Emerg Med 2016; 23: 159-165.Deyo RA, Von Korff M, Duhrkoop D.
Opioids for low back pain.
BMJ 2015; 350: g6380.National Institute for Health and Clinical Excellence (NICE).
Low Back Pain: Early Management of Persistent Nonspecific Low Back Pain
London: National Institute for Health and Care Excellence; 2009.
[Report No.: Clinical guideline 88].Juch JNS, Maas ET, Ostelo R, et al.
Effect of radiofrequency denervation on pain intensity among patients with
chronic low back pain: the Mint randomized clinical trials.
JAMA 2017; 318: 68-81.
Return to LOW BACK PAIN
Return to COST-EFFECTIVENESS
Return NON-PHARMACOLOGIC THERAPY
Return to INITIAL PROVIDER/FIRST CONTACT
Since 6-30-2021


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |