

Patient Characteristics and Physicians' Practice Activities
for Patients with Chronic Low Back Pain: A Practice-based
Study of Primary Care and Chiropractic PhysiciansThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Manipulative Physiol Ther 2001 (Feb); 24 (2): 92–100 ~ FULL TEXT
OPEN ACCESS Joanne Nyiendo, PhD, Mitchell Haas, DC, Bruce Goldberg, MD, Gary Sexton, PhD
Western States Chiropractic College,
Division of Research, Center for Outcomes Studies,
Portland, Ore 97230, USA.
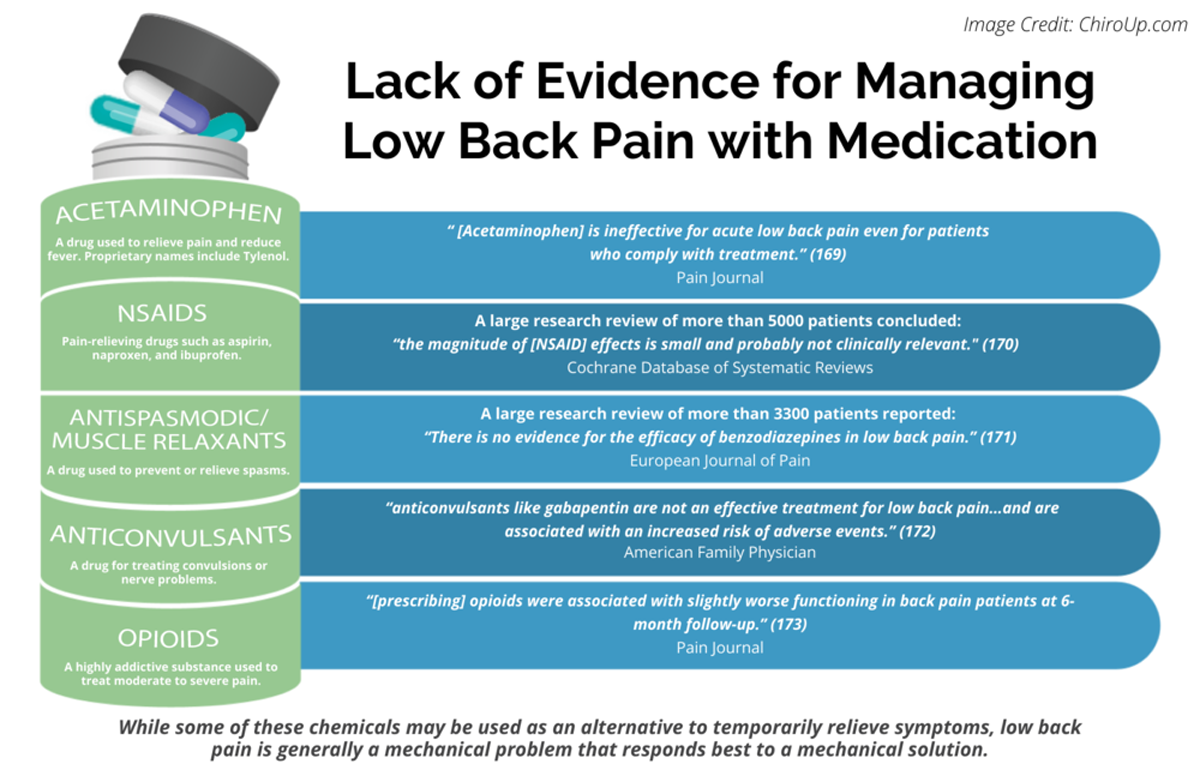
FROM: Pain 2019 (Dec)
FROM: Cochrane Database 2020 (Apr)
FROM: European Journal of Pain 2017 (Feb)
FROM: American Family Physician 2019 (Mar 15)
FROM: PAIN 2013 (Jul)
Thanks to ChiroUP 2021 Chiropractic Outcomes SynopsisBackground: Chronic low back pain sufferers are among those who account for the greatest usage of health care resources. Primary care medical (MD) physicians and chiropractic (DC) physicians treat most of these patients.
Objectives: To study patient characteristics and physician practice activities for patients with chronic low back pain treated by DC physicians and MD physicians.
Methods: A longitudinal, practice-based observational study was undertaken in 14 general practice and 51 DC community-based clinics. A total of 2,945 consecutive patients with ambulatory low back pain of mechanical origin were enrolled; 835 patients were in the chronic subgroup. Patients were followed for 12 months. Data were obtained on all of the following: patient demographics, health status, and psychosocial characteristics; history, duration, and severity of low back pain and disability; physicians' practice activities; and low back complaint status at 1 year.
Results: Patients treated by MD physicians were younger and had lower incomes; their care was more often paid for by a third party; their baseline pain and disability were slightly greater. In addition, patients treated by MD physicians had one fourth as many visits as patients treated by DC physicians. Utilization of imaging procedures by enrolling physicians was equivalent for the two provider groups. Medications were prescribed for 80% of the patients enrolled by MD physicians; spinal manipulation was administered to 84% of patients enrolled by DC physicians. Physical modalities, self-care education, exercise, and postural advice characterized low back pain management in both provider groups. Patients' care-seeking was not exclusive to one provider type. Most patients experienced recurrences (patients treated by MD physicians, 59.3%; patients treated by DC physicians, 76.4%); 34.1% of patients treated by MD physicians and 12.7% of patients treated by DC physicians reported 12 months of continuous pain. Only 6.7% of patients treated by MD physicians and 10.9% of patients treated by DC physicians reported 1 resolved episode during the year.
Conclusions: Differences in sociodemographics, present pain intensity, and functional disability may distinguish patients with chronic low back pain seeking care from primary care medical physicians from those seeking care from DC physicians. Although the primary treatment modality differs, the practice activities of MD physicians and DC physicians have much in common. Long-term evaluation suggests that chronic back pain is persistent and difficult to treat for both provider types.
Keywords Low Back Pain, Patient Characteristics, Medical Physicians, Chiropractic
From the Full-Text Article:
INTRODUCTION
Back problems are common, and they frequently result in disability. [1, 2] One in 4 people with low back pain will seek treatment from a health care professional. Once that decision has been made, 70% of patients will go to either a primary care medical (MD) physician or a chiropractic (DC) physician. [2] Numerous therapies and management approaches exist for treatment of low back pain, but there is little consensus regarding appropriate treatment for patients whose low back problems persist beyond 1 month. [3, 4] Systematic reviews of randomized clinical trials have found insufficient scientific evidence to substantiate the effectiveness of spinal manipulation for chronic low back problems. [3–5]
In the last decade, the focus of low back pain research has shifted, influenced by MD physicians’ desire for information relevant to back pain management in the community setting. The traditional focus on basic biomedical and biomechanical research on low back disorders has been supplanted by an emphasis on epidemiologic and outcomes research. As a consequence of this new way of thinking, investigators have begun to embrace new approaches to back pain research that complement randomized clinical trials (eg, observational, cohort, cross-sectional, and prevalence studies) to better understand the complexity of low back problems and the care that is rendered by physicians in community settings.
In late 1994, we initiated a long-term study of ambulatory low back pain in the offices of 111 MD and 60 DC physicians. Using a practice-based, observational design, [6, 7] we conducted a prospective study of patients with low back problems seeking care from MD and DC physicians. We sought information that could improve understanding of which patients are most likely to benefit from which of the two provider types and under what circumstances. We included assessment of a broad range of sociodemographic, psychosocial, health status, and care-seeking variables. Patient follow-up was for 1 year. This first article is descriptive, focusing on patient and clinical characteristics of chronic ambulatory patients with low back pain and their physicians’ practice activities. Subsequent articles will report on patients’ clinical outcomes and predictors of outcomes, costs of care, and the relationship between psychosocial factors and patient outcomes.
METHODS
Study Design
Data for this report were obtained as part of a prospective, longitudinal, nonrandomized, practice-based, observational study of self-referring patients treated by MD and DC physicians. Patient data were obtained through use of selfadministered questionnaires at the initial visit and at 5 follow-ups up to 1 year. Data on physician practice activities were obtained by means of a questionnaire at each patient visit for treatment of low back pain and by chart audit at the end of the study.
The study did not seek to alter or interfere with the usual management of low back pain by the practitioners involved.
Subjects
A patient was eligible for the study if low back pain was the primary complaint and he or she had not seen the participating provider or a provider of the same type for a low back complaint during the 6 weeks before the baseline visit. Low back pain was defined as pain in the area below the 12th rib and above the gluteal folds. Additional criteria were an(1) age of 18 years or greater and
(2) English literacy.Patients were not eligible for inclusion if any of the following applied:
pregnancy, malignancy, infection, vertebral fracture, lumbar instability, low back surgery within 1 year of the initial visit, or low back pain of nonmechanical origin (eg, referred pain of organic origin).
Both patients with acute low back pain and patients with chronic low back pain were enrolled. Chronic was defined as designating an episode duration of 6 weeks or longer. [8]
Eligible patients were invited to participate in the study at the initial visit. Patients were informed about the protocol and assured that their responses would be kept confidential and their treatment would not be altered in any way if they consented to participate as study subjects. Each patient was required to sign an informed consent form before enrollment. Neither patients nor doctors were paid honoraria for the time they spent on behalf of the study.
The study was approved by the institutional review boards of Western States Chiropractic College and its subcontractor, Oregon Health Sciences University.
Physicians
The study was carried out by physician volunteers from 14 multidoctor MD practice clinics (77 family practice and 34 general internal medicine physicians) and 51 DC clinics (60 chiropractors). Ten of the medical clinics were in urban and suburban areas along the I–5 corridor from Corvallis, Ore, north to Vancouver, Wash. Three medical clinics were in rural areas and 4 were teaching facilities; participating physicians included residents in family practice. DC clinics were 80% solo and 20% 2–doctor practices. Two thirds were in the Portland metropolitan area and the surrounding suburbs; one third were in rural areas of the state, including the Oregon coast and central and southern Oregon.
Physicians provided information on clinical impressions, use of radiographs and special imaging procedures, referrals, and procedures used.
Data Collection Procedures and Data Collected
Both the patient and the physician completed questionnaires on the first visit. The patient baseline questionnaire was administered in the clinic waiting room before the clinical encounter. A follow-up questionnaire was mailed to each patient with a postage-paid, addressed reply envelope at 2 weeks and 1, 3, 6, and 12 months. A patient satisfaction questionnaire was administered by telephone interview at 10 days and 12 months. The physician’s baseline questionnaire was completed during or immediately after the patient’s enrollment visit. Doctor follow-up questionnaires were required to be completed at all subsequent visits for treatment of the low back problem up to 1 year from the initial visit.
Organizational support for the practices was provided by the Center for Outcomes Studies (COS) at Western States Chiropractic College. Each clinic with 4 or more doctors was assisted in this study by a member of the COS staff who worked on-site at the clinic determining patient eligibility, obtaining consent, and ensuring completion of patient and doctor questionnaires. All clinics requiring onsite staff were medical clinics. DC clinics were overwhelmingly solo practices, the front desk staff assuming the project responsibilities. Clinics were oriented to the protocol and logistics of data collection by the COS staff during the first 3 months of the study (in late 1994). Clinicspecific strategies were developed for integrating the study into the daily routine with minimal disruption of normal operations and without jeopardy to either patient care services or the integrity of the study.
Nine months into the study (approximately halfway through data collection), clinic audits were undertaken in 5 MD clinics and nearly all of the DC clinics to ascertain levels of compliance with the study protocol in clinics without on-site staff.
Measurements
Information on low back pain history, duration and severity of the current episode, general health status, demographics, and selected psychosocial factors was collected at baseline. The severity of present pain was assessed by means of a 100– mm visual analog scale with the descriptive anchors “no pain” and “excruciating pain.” [9, 10] Functional disability was measured with the Revised Oswestry Disability Questionnaire (RODQ), a 10–item instrument designed to measure outcomes in patients with low back pain. [11, 12] Episode characteristics and questions related to symptoms were assessed through use of InterStudy’s Low Back Pain TyPE Specification. [13] The SF 12 [14] a shorter version of the SF-36, [16–17] was selected to measure the 8 dimensions of health status.
Psychosocial measurements included a satisfaction questionnaire, [18] questions related to stress, and the Krantz Health Opinion Survey. [19] This measure consists of a total score and 2 subscale scores that yield an assessment of patient preferences regarding information related to their medical care and patient attitudes toward self-care and active behavioral involvement in medical care.
Each of the forms and questionnaires were tested in one or more pilot studies and in a 6–month feasibility investigation before the present study. On completion of the community-based data collection phase of the study, chart abstraction and billing data were compared with doctor-provided information for selected questions to estimate physician compliance with the protocol (eg, number of visits, use of imaging procedures, number of chiropractic manipulations, number and type of prescriptions).
Outcomes
The primary outcomes were present pain severity and functional disability at the 5 follow-up time points (2 weeks and 1, 3, 6, and 12 months). Satisfaction was a secondary outcome. Findings for these variables are reported in a separate paper.
Statistical Analysis
Baseline differences between patient groups were tested for significance through use of an unpaired t test for continuous variables. χ2 analysis was used for categoric variables. All tests of statistical significance were conducted at the .01 level for a 2–tailed test. Analysis was conducted through use of SPSS-PC 5.0 statistical software. [20]
RESULTS
During a 3–week prospective clinic audit in August, only 5.1% of DC patients who were eligible were not asked; the reasons given were time constraints and patient back-up. Some (10.1%) of the eligible patients who were asked to participate refused to consent. On average, 50% to 60% of eligible patients at the smaller MD clinics (without on-site staff) were invited to participate. When patients were not approached, it was because the clinics were too busy and the study was considered by clinic staff to be less of a priority than patient care. Prospective audits were not undertaken in the large MD clinics. On-site study personnel ensured maximum enrollment at these clinics. We did review study records maintained at one of these clinics during a 6–month period: 16% of patients who were eligible refused to consent; 80% of these nonconsenters were elderly.
Total patient enrollment was 2,945. Administrative error (eg, no consent form or physician-patient encounter initiated before the baseline questionnaire was completed) resulted in disqualification of 1.2% of the MD enrollees and 1.1% of the DC enrollees. 2.9% of the MD patients and 0.6% of the DC patients were misdiagnosed and disqualified. 1.4% of the MD patients and 1.5% of the DC patients were eliminated from the present analysis for other reasons (eg, patient withdrawal before first follow-up). The size of the final patient sample was 2,775: 993 MD patients and 1,952 DC patients. The chronic subgroup consisted of 309 MD patients and 526 DC patients. Response rates for follow-up questionnaires for patients enrolled by MD physicians were 68.6% of all patients at the 2–week follow-up, 71.9% at 1 month, 66.2% at 3 months, 63.5% at 6 months, and 62.9% at 12 months; for patients enrolled by chiropractors, the corresponding response rates were 71.0%, 72.5%, 67.5%, 63.3%, and 64.0%. MD patients responding to the 6– and 12–month follow-up questionnaires were distinguished from MD nonrespondents by slightly greater pain and disability scores. Similar findings were found in the DC cohort. In addition, DC respondents were more often women and slightly older than DC nonrespondents.
DC and MD physicians failed to comply with the followup protocol in 11% to 15% of patient visits. In addition, write-in responses on the study forms were sometimes incomplete or illegible. Because the patient record was generally typewritten, chart abstraction data were used to identify medications prescribed. All other data presented in this article were derived from the study forms.

Table 1 Demographic characteristics are shown in Table 1. Medical patients were slightly younger, and more were at the lower end of the income scale (26.2% vs 9.5%; P < .01). Large differences were noted with regard to method of payment for physician services. The proportion of DC patients who paid out of pocket for treatment was nearly 8 times greater than the proportion of medical patients who did so (P < .01). The SF-12 general health status scores suggest greater physical impairment and bodily pain and greater limitations on activities of daily living for medical patients at baseline (Table 2). A 24–point difference was noted for physical function and a 16–point difference was noted for role physical (P < .01). Smoking was more prevalent in MD patients (31.5% vs 21.9%; P < .01).

Table 2 Regarding psychosocial characteristics (Table 2), the greatest differences between the MD and DC cohorts were higher levels of physical and financial stress (P < .01) in the medical patients. Scores on the Health Opinion Survey also differed significantly in the two provider groups. Higher total scores and higher subscale scores represent more favorable attitudes toward informed or self-directed treatment in the MD patient cohort.
More than one half of MD patients (53.7%) were using medication at the time of enrollment in the study: 26.7% were taking prescription drugs for their low back pain or leg pain (sciatica), and 34% were using over-the-counter medications. In contrast, 42.9% of DC patients were on medication for low back pain or sciatica; 12.9% were taking prescription drugs, and 32.0% were using over-the-counter medications.

Table 3 Low back pain complaint characteristics are presented in Table 3. The vast majority of patients (84% to 89%) had previous histories of low back pain. There were striking differences between MD and DC patients with respect to pain radiation: 40% vs 28% with pain below the knee and 27% vs 41% with no leg pain (P < .01). The means and SDs for pain severity (visual analog scale) and functional disability (RODQ) are presented in Table 3. The higher scores for MD patients indicate overall greater pain severity and greater functional disability.
DC Practice

Table 4 As shown in Table 4, DC patients had a median of 4 visits; MD patients had a median of 1 visit. Radiographs were taken in 25.6% of cases; computed tomography (CT) and magnetic resonance imaging (MRI) were rarely reported. Most DC patients received manipulation at some time over the course of their treatment for low back pain. Manual high-velocity, low-amplitude manipulation [21] was the most commonly used form (88% of all DC patients). Physiotherapy modalities were an integral part of the DC therapeutic approach. Nearly one half of the chronic patients (42.7%) received electrotherapy on at least 1 visit; 10% had 5 or more treatments. Chiropractors’ use of massage and heat application was similar to that reported for electrotherapy. Ultrasound was used for 22.7% of DC patients. Cold application, traction, and mobilization were included in patient management in 5% to 10% of cases.
Patient education in self-care and exercise were important elements of DC patient management (Table 4).
MD Practice
One in 4 MD patients had radiographs taken. MRI was performed in 8.3% of cases; CT in 1.3%. Sixteen percent of MD patients were referred for evaluation and/or treatment on the first visit: 61.5% to a physical therapist (PT), 8.8% to a neurosurgeon, 6.6% to an orthopedic surgeon, and 4.4% to a chiropractor.
During the 1–year study period, 20% of medical patients were given more than 5 prescriptions; for another 20%, no medication was prescribed. The mean number of prescriptions was 3.3 (SD = 4.8), the median being 2 and the range 1–40. More than one half of the MD patients were given prescriptions for nonnarcotic analgesics. Used most frequently was naproxen; used second most frequently was ibuprofen. Together, these 2 drugs accounted for 75% of all nonnarcotic analgesics prescribed for patients with chronic low back pain. Narcotic analgesics and muscle relaxants were each prescribed in one third of cases. Vicodin, tramadol and apap/codeine accounted for 74% of all narcotic analgesics prescribed. Cyclobenzaprine was by far the most frequently prescribed muscle relaxant (75%). Nearly 1 in 5 MD patients with chronic low back pain (18.7%) were given prescriptions for antidepressants. This was most often (74.5%) amitriptyline, paroxetine, or imipramine.
Exercise plans, self-care education, and postural advice were frequently used by MD physicians in the management of the patients with chronic low back pain (Table 4).

Table 5 At each follow-up, patients were asked if they were still in care for their low back problems and if so, who was providing the care (Table 5). Although this question provided only single-point-specific information on care-seeking behavior, the replies do offer some insight into multiple-provider use. One third of patients in both cohorts were still in care at the 6– and 12–month follow-ups. At 12 months, there was little difference between the cohorts in the proportions of patients under the care of PTs, under the care of alternative health care providers (acupuncturist, massage therapist), and under self-care. The higher percentage of MD patients in the care of surgeons at 6 months was also reported at the 1–year follow-up.
Low Back Status at 1–year Follow-up

Table 6 One third of MD patients and 12% of DC patients reported continuous pain from the date of study enrollment (Table 6). Few patients in either cohort reported that the index episode was resolved without any recurrence in the year after study enrollment (<11%). Among patients who did experience recurrences, DC patients averaged more recurrences, but these were of shorter duration than the recurrences reported by MD patients. DC patients averaged 6.1 recurrences, whereas medical patients averaged 5.1. Most respondents reported recurrences lasting <1 week, but 11% of MD and 4% of DC patients reported recurrence durations of >1 month.
DISCUSSION
Regional and national physician networks have been shown to be useful vehicles for studying communitybased health problems. [22–24] In the absence of any formal network including both medical doctors and chiropractors, we assembled a group of MD physicians and DC physicians for this study. Our investigation was set in community clinics and enrolled patients who selected those clinics/physicians for care of their low back problem. We acknowledge that this method is susceptible to various types of bias. The representativeness of participating physicians (volunteers) and patients (self-selected) is not known, so selection bias cannot be ruled out. Some patients who were eligible for participation were not asked. This generally occurred during periods of intense clinic activity. Although this should not have led to any systematic bias in patient enrollment, we cannot be certain. Information bias from chart abstraction and patientreported data cannot be ruled out. Patients who did not respond to follow-up questionnaires might not have been representative of the group of patients who did respond, though our analysis suggests that bias from this source was inconsequential. Finally, as with all observational studies, one can never be sure that all of the vital factors affecting patient outcomes are known and are reflected in the data. We cannot presume cause and effect. These limitations are reflected in the interpretation of data.
It is generally accepted that response rates of 75% or higher introduce minimal bias for observational studies when differences do exist between respondents and nonrespondents. [25] Our mailed survey response rates for patients were quite acceptable (63% for the 6– and 12–month followups). The differences reported in our study between respondents and nonrespondents will be accounted for in subsequent articles comparing patient outcomes.
In any study involving patient self-selection to treatment, it is important to identify whether the patients in the treatment groups differ with respect to any relevant variables. We did find provider group differences in patient sociodemographics and psychosocial and complaint characteristics. DC patients were characterized by lower levels of unemployment, higher average income, more out-of-pocket health care expenses, better general health, lower levels of stress, and less low back pain and functional disability, and a smaller proportion of them had radiating pain below the knee.
Carey et al [26] examined patient and clinical factors associated with care-seeking for patients with chronic low back pain in North Carolina. They reported that individuals seeking care from chiropractors had better health insurance, whereas in our study DC patients (in comparison with MD patients) were characterized by a strikingly higher proportion without insurance and/or paying out-of-pocket for their care. Direct comparison between our findings and those of Carey et al is made difficult because both the research questions and the methods were different. It is not known whether “good health insurance,” referred to by Carey et al, meant coverage for DC care. The proportion of North Carolina patients’ out-of-pocket expenses is also unknown. There is some evidence that the patient sample studied by Carey et al was characterized by lower income (and lower educational) levels.
Although statistically significant, it is unlikely that the cohort differences observed with respect to information and behavioral involvement preferences are clinically meaningful. [19] Scores for both cohorts fall within the same preference category: “high” preference for behavioral involvement and “medium” preference for information.
Similarities were found between our study and that of Carey et al [26] with respect to DC patients’ better overall health and lower pain severity ratings at enrollment. Interestingly, Carey et al reported that 76% of individuals with chronic low back pain had leg pain (similar to the 72.6% with leg pain in our MD patient group), but they did not report on this variable within the two provider groups, nor did they distinguish radiating pain above the knee from pain below the knee. We found an impressive difference: a much higher proportion of MD patients than of DC patients presented with pain radiating below the knee. Overall chronic back pain severity in the North Carolina study appears to have been higher than that in our study. This may be related to differences in state economies or health care markets, which are known to influence care-seeking by patients. [27, 28]
The higher number of patient visits to chiropractors is consistent with earlier studies comparing chiropractic with family practice. [26, 29, 30] The “hands-on” nature of chiropractic practice makes this inevitable. Frequency of use of all imaging modalities (radiography, CT, MRI) for patients with chronic back pain in this study was considerably lower than that reported by Carey et al [26] for patients with chronic low back pain in North Carolina. They obtained information on special imaging from patient recall for all providers seen during the previous year (not broken down by provider type). The comparatively low utilization of imaging procedures reported in our study might be a consequence of differences in health care organizational systems; the extent of penetration of managed care systems in Oregon is among the greatest in the country. [31] The factors influencing physicians’ practice patterns are extremely complex. Wennberg, [32, 33] Ware, [34] Eisenberg, [35] and others have published extensively on regional differences in physicians’ practice patterns and the influence of non–health-related economic, psychologic, and sociologic factors on physician decisions related to provision of medical care. Finally, our research design, unlike that of Carey et al, [26] could not capture imaging procedures ordered by specialists or providers other than the enrolling physicians.
Practice activities of both MD and DC physicians included the use of physiotherapy and referral to a PT. PTs did not participate in this study, and data on the specifics of physical therapy treatment regimens were seldom available in the patients’ charts. Thus we were unable to further describe patient management by PTs or assess similarites and differences of physical therapy management with use of physiotherapy modalities by chiropractors.
Drug therapy is one of the most common treatments for low back pain. [36] However, actual patterns of medication use and their associated costs for low back pain have not been well studied. The 1995 study by Hart et al [36] of National Ambulatory Medical Care Survey (single point in time) data looked at prescription drug use associated with all low back pain (acute and chronic). Their findings were, in order of prescription frequency, nonsteroidal anti-inflammatory drugs, muscle relaxants, and narcotic analgesics. In our study, MD prescribing patterns for muscle relaxants and for no medication were comparable to those reported by Cherkin et al, [37] who mostly studied patients with acute low back pain. However, in comparison with the North Carolina study, [37] our medical doctors prescribed nonsteroidal antiinflammatory drugs less frequently (57% vs 69%) and narcotic analgesics more frequently (31% vs 12%). The use of narcotic analgesics for chronic pain syndromes is controversial, and evidence-based recommendations do not exist. [38] The use of antidepressant drugs is fairly common for patients with chronic back pain who have symptoms of depression. [38] The use of antidepressants in this study was consistent with the proportion of medical patients enrolled with chronic depression.
One half of all patients seeking care from MD and DC physicians were reported by their physicians to have received postural advice, self-care education, or an exercise plan as part of treatment for the low back complaint. Evidence from a number of studies, such as the Medical Outcomes Study [39] and the Direct Observation of Primary Care study, [40] suggest that generalist physicians, especially family physicians, [41] are conservative in their use of medical technology and medical interventions. Management guidelines for MD treatment of chronic low back pain emphasize preservation of function, patient education, and self-care. [42] Chiropractic has long distinguished itself as uniquely patient-centered and focused on wellness. [43, 44] Recent studies have reported that chiropractic practice routinely includes patient counseling for posture, fitness exercise, stress management, ergonomics, injury prevention, and weight loss. [45] It should be noted that explicit operational definitions for these practice activities were not provided within the physician questionnaires. We do not know to what extent MD physicians and DC physicians had similar interpretations of the levels of performance constituting these activities.
Current research on the course of low back pain suggests that the proportion of patients presenting for ambulatory patient care whose pain is not completely resolved at 6 months or 1 year is considerably higher than previously thought by most physicians. [8, 42, 46, 47] Our study findings are consistent with this new understanding. A very high proportion of these patients are still reporting low back problems 1 year after enrollment, and the proportion reporting long bouts of continuous pain is certainly not trivial. DC patients did report more recurrences, but they reported shorter durations (of recurrent spells) than MD patients and one third the frequency of continuous pain during the study period. This article is descriptive only, and these data are uncorrected for baseline differences.
CONCLUSION
Our data suggest that patients seeking care from participating MD physicians and patients seeking care from DC physicians may differ with respect to some sociodemographic characteristics and that MD patients may present with somewhat greater severity and disability. Patients’ careseeking was not exclusive to one provider type. Although prescription medications were central to MD physicians’ management of chronic low back pain and spinal manipulation was central to DC management, physicians’ practice activities in the two disciplines were similar in their eclectic approach to patient care.ACKNOWLEDGMENTS
This study would not have been possible without the enthusiastic contributions of the staff of the COS and the personal commitment of the participating MD and DC physicians. We are especially grateful for the technical and clerical support provided by the following people: Michael Attwood, Bonnie Ganger, Rebekah Jones, Carol Lloyd, and Kris White.
References:
Cypress BK.
Characteristics of physician visits for back symptoms:
a national perspective.
Am J Public Health 1983;73:389-95.Deyo RA, Tsui-Wu Y.
Descriptive epidemiology of low back pain and
its related medical care in the United States.
Spine 1987;12:264-8.Bigos SJ, Bowyer OR, Braen GR, Brown K, Deyo R, Haldeman S, et al.
Acute Lower Back Problems in Adults
Clinical Practice Guideline 14
Rockville (MD): Agency for Health Care Policy and Research; 1994.
(AHCPR publication no. 95-0642).Rosen M.
Report of a CSAG (Clinical Standards Advisory Group) committee on back pain.
London: Her Majesty’s Stationery Office; 1994.Koes BW, Assendelft WJJ, Van Der Heijden GJMG, Bouter LM.
Spinal manipulation for low back pain: an updated
systematic review of randomized clinical trials.
Spine 1996;21: 2860-73.Gordis L.
Epidemiology.
Philadelphia: WB Saunders; 1996. p. 116-23.D’Agostino RB, Kwan H.
Measuring effectiveness.
Med Care 1995;33:AS95-AS105.Philips HC, Grant L.
The evolution of chronic back pain problems:
a longitudinal study.
Behav Res Ther 1991;29:435-41.Scott J, Huskisson EC.
Graphic representation of pain.
Pain 1976;2:175-84.Price DD, McGrath PA, Rafii A, Buckingham B.
The validation of visual analogue scales as ratio
scale measures for chronic and experimental pain.
Pain 1983;17:45-56.Fairbank JCT, Couper J, Davies JB, O’Brien JP .
The Oswestry low back pain disability questionnaire.
Physiotherapy 1980; 66:271-3.Hudson-Cook N, Tomes-Nicholson K.
The revised Oswestry low back pain disability questionnaire [thesis].
Bournemouth, United Kingdom: Anglo European College of Chiropractic; 1988.Users manual: low back pain TyPE specification. Version 1.
Bloomington (MN): Quality Quest; 1989.Ware JE Jr, Kosinski M, Keller SD.
A 12-item short-form health survey.
Med Care 1996;34:220-33.Brazier J, Harper R, Jones SN.
Validating the SF-36 Health Survey Questionnaire:
New Outcome Measure for Primary Care
British Medical Journal 1992 (Jul 18); 305 (6846): 160-164Ware JE, Sherbourne CD.
The MOS 36-item short-form health survey (SF-36), I:
conceptual framework and item selection.
Med Care 1992;30:473-83.McHorney CA, Ware JE, Raczek AE.
The MOS 36-item shortform health survey (SF-36), II:
psychometric and clinical tests of validity in
measuring physical and mental health constructs.
Med Care 1993;31:247-63.Cherkin, D.C. and MacCornack, F.A.
Patient Evaluations of Low Back Pain Care From
Family Physicians and Chiropractors
Western Journal of Medicine 1989 (Mar); 150 (3): 351–355Krantz DS, Baum A, Wideman MV.
Assessment of preferences for self-treatment and information in health care.
J Pers Soc Psychol 1980;39:977-90.Norusis MJ.
SPSS/PC+ base manual/statistics 5.0/advanced statistics 5.0.
Chicago: SPSS, Inc; 1992.Bergmann T, Peterson D, Lawrence D, editors.
Chiropractic technique: principles and procedures.
New York: Churchill Livingston; 1993.Clancy CM.
Conducting studies in practice-based primary care research networks.
In: Grady ML, editor. Challenges of practice based research.
Proceedings of the 3rd AHCPR conference on primary care.
Rockville (MD): US Department of Health and Human Services; 1993.Green LA, Hames CG, Nutting PA.
Potential of practice-based research networks: experiences from ASPN.
J Fam Pract 1994;38:400-6.Culpepper L, Froom J.
The international primary care network:
purpose, methods, and policies.
Fam Med 1988;20:197-201.Guadagnoli E, Cunningham S.
The effects of nonresponse and late response
on a survey of physician attitudes.
Evaluation and the Health Professions 1989;12:318-28.Carey TS, Evans A, Hadler N, Kalsbeek W, McLaughlin C, Fryer J.
Care-seeking among individuals with chronic low back pain.
Spine 1995;20:312-7.Hafner-Eaton C.
Physician utilization disparities between the uninsured and insured.
JAMA 1993;269:787-91.Hadley J, Steinberg EP, Feder J.
Comparison of uninsured and privately insured hospital patients:
condition on admission, resource use, and outcome.
JAMA 1991;265:374-9.Carey TS, Garrett J, Jackman A, et al.
The Outcomes and Costs of Care for Acute Low Back Pain Among Patients
Seen by Primary Care Practitioners, Chiropractors, and Orthopedic Surgeons
New England J Medicine 1995 (Oct 5); 333 (14): 913–917Shekelle PG, Markovich M, Louie R.
Comparing the costs between provider types of episodes of back pain care.
Spine 1995;20:221-7.Interstudy regional market analysis.
St Paul (MN): Decision Resources, Inc; 1999.Wennberg JE.
Dealing with medical practice variations: a proposal for action.
Health Aff 1984;3:6-32.Wennberg JE.
Understanding geographic variations in health care delivery.
N Engl J Med 1999;340:52-3.Ware JE, Sherbourne CA, Davies AR, Wennberg J, Gittelsohn A.
Variations in medical care among small areas.
Sci Am 1982;246:120-34.Eisenberg JM.
Physician utilization: The state of research
about physicians’ practice patterns.
Med Care 1985;23:461-83.Hart LG, Deyo RA, Cherkin DC.
Physician office visits for low back pain.
Spine 1995;20:11-9.Cherkin DC, Wheeler KJ, Barlow W, Deyo RA.
Medication use for low back pain in primary care.
Spine 1998;23:607-14.Deyo RA.
Drug therapy for back pain: which drugs help which patients?
Spine 1996;21:2840-50.Greenfield S, Nelson EC, Zubkoff M, Manning W, Rogers W, Kravitz RL, et al.
Variations in resource utilization among medical specialties and
systems of care: results from the medical outcomes study.
JAMA 1992;267:1624-30.Stange KC, Zyzanski SJ, Jaen CR, Callahan EJ, Kelly RB, Gillanders WR, et al.
Illuminating the “Black Box.”
J Fam Pract 1998;46:377-89.Bertakis KD, Robbins JA.
Utilization of hospital services: a comparison of internal medicine and family practice.
J Fam Pract 1989;28:91-6.Von Korff M.
Perspectives on management of back pain in primary care.
In: Gebhart FF, Hammond DL, Jensen TS, editors.
Proceedings of the 7th World Congress on Pain,
Progress in Pain Research and Management. Vol 2.
Seattle: IASP Press; 1994. p. 97-110.Gatterman MI.
A patient-centered paradigm: a model for chiropractic education and research.
J Altern Complement Med 1995;1:371-86.Coulter ID.
Alternative philosophical and investigatory paradigms for chiropractic.
J Manipulative Physiol Ther 1993;16:419-25.Hawk C, Dusio ME.
A survey of 492 U.S. chiropractors on primary care
and prevention-related issues.
J Manipulative Physiol Ther 1995;18:57-64.Cherkin DC, Deyo RA, Street JH, Barlow W.
Predicting poor outcomes for back pain seen in primary care
using patients’ own criteria.
Spine 1996;21:2900-7.Croft, P., Macfarlane, G., Papageorgiou, A. (1998).
Outcome of low back pain in general practice:
A prospective study
British Medical Journal 1998 (May 2); 316 (7141): 1356–1359
Return to LOW BACK PAIN
Return to PATIENT SATISFACTION
Since 2-18-2002


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |