Validity and Reliability of Clinical Prediction Rules used to
Screen for Cervical Spine Injury in Alert Low-risk Patients
with Blunt Trauma to the Neck:Part 2. A Systematic Review from the Cervical Assessment
and Diagnosis Research Evaluation (CADRE) Collaboration
This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: European Spine Journal 2018 (Jun); 27 (6): 1219–1233 ~ FULL TEXT
N. Moser, N. Lemeunier, D. Southerst, H. Shearer, K. Murnaghan, D. Sutton, P. Cote
Division of Graduate Education and Research,
Canadian Memorial Chiropractic College (CMCC),
6100 Leslie Street,
Toronto, ON, Canada.
PURPOSE: To update findings of the 2000-2010 Bone and Joint Decade Task Force on Neck Pain and its Associated Disorders (Neck Pain Task Force) on the validity and reliability of clinical prediction rules used to screen for cervical spine injury in alert low-risk adult patients with blunt trauma to the neck.
METHODS: We searched four databases from 2005 to 2015. Pairs of independent reviewers critically appraised eligible studies using the modified QUADAS-2 and QAREL criteria. We synthesized low risk of bias studies following best evidence synthesis principles.
RESULTS: We screened 679 citations; five had a low risk of bias and were included in our synthesis. The sensitivity of the Canadian C-spine rule ranged from 0.90 to 1.00 with negative predictive values ranging from 99 to 100%. Inter-rater reliability of the Canadian C-spine rule varied from k = 0.60 between nurses and physicians to k = 0.93 among paramedics. The inter-rater reliability of the Nexus Low-Risk Criteria was k = 0.53 between resident physicians and faculty physicians.
CONCLUSIONS: Our review adds new evidence to the Neck Pain Task Force and supports the use of clinical prediction rules in emergency care settings to screen for cervical spine injury in alert low-risk adult patients with blunt trauma to the neck. The Canadian C-spine rule consistently demonstrated excellent sensitivity and negative predictive values. Our review, however, suggests that the reproducibility of the clinical predictions rules varies depending on the examiners level of training and experience.
KEYWORDS: Canadian C-spine rule; Clinical prediction rule; Neck pain; Nexus low-risk criteria; Reliability; Validity
From the FULL TEXT Article:
Introduction
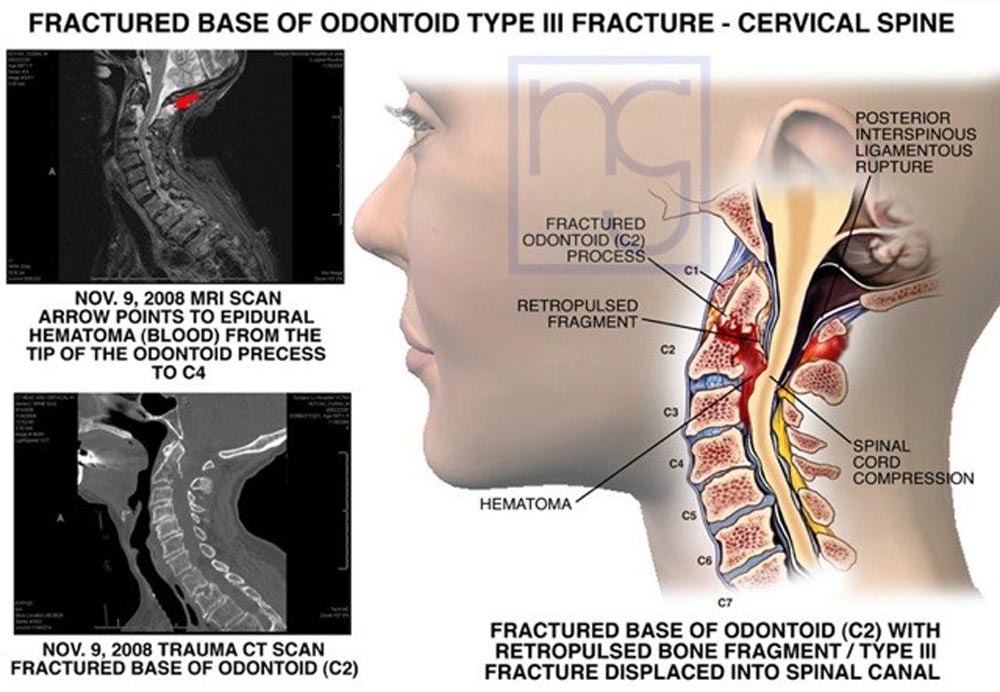
The incidence of a potentially serious cervical spine injury, including cervical spine fracture, dislocation, and ligamentous instability in the Norwegian population, is an estimated 16.5/100,000/year. [1] In the United States, more than a million patients are assessed each year. [2] Failure to diagnose these injuries in a timely manner may have significant consequences, including spinal cord injury and even death. [3] Thus, highly sensitive and reliable assessment methods are required to screen patients who are at risk of serious cervical spine injury.
The primary focus of an assessment for patients with acute neck pain following blunt trauma is to rule out the presence of major pathology, such as fractures and dislocations. [4] Assessment of the anatomical integrity of the cervical spine involves diagnostic imaging, such as plain radiography, computed tomography, or magnetic resonance imaging. However, relying on these procedures is an inefficient practice. [5–8] More than 98% of all cervical spine radiographs ordered following acute blunt trauma are negative for fracture. [6, 9–11] This low diagnostic yield is associated with significant costs and places a significant strain on health care resources]. [5, 12, 13] Furthermore, patients are exposed to potentially harmful radiation when imaging may not be clinically indicated. [14]
Clinical practice guidelines for the assessment of neck pain [15, 16] advocate for the use of clinical prediction rules to identify those at low risk of serious cervical spine injuries. Clinical prediction rules serve as a decision matrix, incorporating three or more variables from the patient’s history, physical examination, and/or simple diagnostic tests. Their intent is to guide the diagnostic and treatment decision-making process. [17, 18]
In 2008, The 2000–2010 Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders (Neck Pain Task Force) reported on the diagnostic accuracy of clinical prediction rules used to screen alert low-risk adults with blunt trauma to the neck. [4] They concluded that two clinical prediction rules, The Nexus Low-Risk Criteria (NLC) and The Canadian C-spine rule (CCR), demonstrated high sensitivity and negative predictive values. The Neck Pain Task Force did not identify any low risk of bias studies assessing their reliability. More recently, a systematic review by Michaleff et al. reported that these clinical prediction rules yielded consistently high sensitivity. [19] The emergence of new evidence regarding the reliability and validity of the NLC and CCR warrants an updated review of the literature.
This systematic review aims to update the findings of the Neck Pain Task Force on the validity and reliability of clinical prediction rules used to screen for cervical spine injury in alert low-risk adult patients, aged 16 and older, with blunt trauma to the neck. This review is the second of a series of five systematic reviews updating the NPTF on the reliability and validity of clinical tests and tools used to assess patients with NAD. Subsequent reviews focus on screening for anatomical integrity of the cervical spine [20], measurement of pain and disability [21]; palpation and cervical mobility [22], and functional tests of the cervical spine. [23] Together, the purpose of these reviews is to inform the development of a clinical practice guideline for the clinical assessment of the cervical spine.
Method
Registration
We registered this review protocol with the International Prospective Register of Systematic Reviews (PROSPERO) on February 4, 2016 (CRD42016033896).
Eligibility criteriaPopulation We included studies of alert low-risk adults (16 years of age or older) with NAD (grades I–IV), including WAD (grades I–IV) after blunt trauma to the neck. We defined NAD according to the Neck Pain Task Force [24] and WAD according to the Québec Task Force. [25] Alert low-risk patients are defined as cooperative, non-intoxicated, conscious patients that have scored 15 on the Glasgow Coma Scale (GCS) and have no distracting injuries. [26–29] We excluded studies targeting high-risk patients, defined as those who are unconscious, sedated, intoxicated or noncooperative, or those with distracting injuries or an altered mental state (GCS < 15). [26, 27]
Evaluation of assessment We restricted our review to studies assessing the validity and reliability of clinical prediction rules used to screen for cervical spine injury in alert low-risk patients with blunt trauma to the neck. Validity is the degree to which the data measure what they were intended to measure—that is, the results of a measurement correspond to the true state of the phenomenon being measured. [30] Reliability is the extent to which repeated measurements of a stable phenomenon by different people and instruments at different times and places to produce similar results. [30]
We chose not to use the standard thresholds or cut-off values for the kappa statistic to classify reliability findings (i.e., weak, moderate, or strong). Since there is no standardized interpretation for the kappa statistic, our judgement on the reproducibility of the clinical prediction rules focused on the importance of ruling out these injuries with little margin for error.
Study characteristics To be included in our systematic review, studies had to fulfill the following inclusion criteria:(1) English or French language;
(2) published from January 1, 2005 to November 5th, 2015 to ensure overlap with the NPTF literature search, which ended in 2005 and was updated in 2007 [4];
(3) published in a peer-reviewed journal;
(4) validity or reliability studies of clinical prediction rules used to screen alert lowrisk patients with blunt trauma to the neck;
(5) study population including alert low-risk adult patients (≥ 16 years of age) with grades I–IV neck pain (including non-traumatic neck pain and neck pain subsequent to a traffic collision) with or without its associated disorders;
(6) sample size of at least 20 per group; and
(7) if studies included a mixed population with individuals less than 16 years of age, results must be stratified for adults 16 years of age and older.
Studies fulfilling any of the following criteria were excluded:(1) publication types including guidelines, letters, editorials, commentaries, unpublished manuscripts, dissertations, government reports, books and book chapters, conference proceedings, meeting abstracts, lectures and addresses, consensus development statements, and guideline statements;
(2) study designs including systematic and non-systematic reviews, and case studies;
(3) cadaveric or animal studies;
(4) studies solely targeting individuals with serious pathology (e.g., fractures, dislocations, myelopathy, neoplasms, infection), and systemic disease; and
(5) sample size less than 20 per group. The exclusion criteria replicate what was used by the NPTF except for publication types. [4]Data sources A search strategy was developed in consultation with a health sciences librarian and reviewed by a second librarian. We systematically searched the following electronic databases from January 1st, 2005 to November 5th, 2015: MEDLINE, PubMed, Cochrane Central Register of Controlled Trials, and CINAHL.
Search terms consisted of subject headings specific to each database (e.g., MeSH in MEDLINE and PubMed) and free text words relevant to NAD, diagnosis, validity, reliability, blunt trauma, spinal fracture, and clinical prediction rules (Appendix I). In addition, the reference lists of included studies and related systematic reviews [4, 19] were screened to identify any studies that we may have missed using our search strategy.
Study selection Pairs of independent reviewers (NM, NL, and DS) screened articles in two phases. The first phase involved screening titles and abstracts for relevant and possibly relevant citations based on the inclusion and exclusion criteria. Possibly, relevant citations from the first phase were reviewed in the second phase using the full text. Disagreements between paired reviewers were resolved by discussion to reach consensus. If consensus could not be reached, a third reviewer independently screened the citation and discussed with the other two reviewers to reach consensus.
Quality assessment Pairs of reviewers (NM, NL, and DS) independently critically appraised all relevant studies. We assessed internal validity using the modified Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) [31] criteria for diagnostic accuracy studies and the modified Quality Appraisal Tool for Studies of Diagnostic Reliability (QAREL) [32] criteria for diagnostic reliability studies. We modified the original QUADAS-2 and QAREL instruments to include:1) a question on whether the study objective was clear;
2) ‘not applicable’ options for some items; and
3) the Sackett and Haynes classification for validity studies (in the QUADAS-2 instrument). [33]Consensus between reviewers was reached through discussion. Following appraisal, we considered studies with adequate internal validity as low risk of bias and included them in our best evidence synthesis (Tables 1, 2).
Classification of diagnostic studies We classified each low risk of bias study according to the classification system by Sackett and Haynes based on the type of research question being addressed. [33] Studies classified as phases I and II are exploratory in nature; therefore, they cannot confirm validity and require further evaluation. In phase III studies, the ability of the test to distinguish between patients with and without the target disorder is assessed and may be compared to a gold standard. Due to their design, the results from phase III studies are hypothesis confirming and form the basis for widespread adoption. Phase IV studies measure utility by assessing whether patients undergoing a test have better health outcomes than patients who do not receive the test.
Data extraction and synthesis of results The lead author (NM) extracted data from low risk of bias studies to build evidence tables (Tables 3, 4) and a second reviewer (DS) independently checked the data extraction. Meta-analysis was not performed due to heterogeneity of studies with low risk of bias regarding patient population, clinical setting, clinical prediction rules being evaluated, and the background and experience of assessors. We, therefore, performed a qualitative synthesis of findings from low risk of bias studies according to principles of best evidence synthesis. [34] Finally, we interpreted our findings in the context of findings from admissible studies summarized by the Neck Pain Task Force. [4]
Statistical analyses
We computed the inter-rater reliability for the screening of articles using the kappa coefficient (κ) and 95% confidence intervals (CI). [35] We calculated the percent agreement for classifying studies into high or low risk of bias following independent critical appraisal.Reporting Our review complies with the Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [36] and Statement for Reporting Studies of Diagnostic Accuracy (STARD). [37]
Results
Study selection

Figure 1 Our search identified 679 citations (Figure 1); six articles met our eligibility criteria and were critically appraised. Five of six critically appraised articles had a low risk of bias and were included in our synthesis.
The inter-rater agreement for screening citations and selection of relevant studies was k = 0.91 (95% CI: 0.83, 1.00). The percent agreement for the independent critical appraisal of studies was 83% (5/6). Disagreements were resolved through discussions between assigned reviewers without the need to involve a third reviewer. We contacted authors from one study during critical appraisal to request additional information; however, we did not receive a response. [38]
Study characteristics
Validity and reliability studies included in our synthesis are summarized in Tables 2 and 3. The prevalence of clinically important cervical spine injury ranged between 0.40% [39] and 1.15% [40] with a median of 0.55%.
Of the five low-risk bias studies, four assessed validity [39–42] and four assessed reliability. [40–43] Three of the five studies evaluated the Canadian C-spine rule (CCR). [39–41] One study evaluated a modified version of the CCR for field use by paramedics. [42] In this modified version, the criterion related to ‘delayed onset of neck pain’ was removed. One study evaluated the Nexus Low-Risk Criteria (NLC). [43] Among all the studies, physicians were instructed to use the clinical prediction rules to decide whether or not to image. However, nurses [40, 41] and paramedics [42] were asked to record their decision regarding the need for cervical spine immobilization.
Three of the five studies [39–41] included alert (GCS 15) adult patients with potential cervical spine injury presenting to emergency departments within 48 h of injury. In another study, paramedics examined alert (GCS 15), stable adult patients transported by ambulance to local hospitals within 8 h of sustaining acute blunt trauma with potential injury to the neck. [42] One study applied a clinical prediction rule in active duty military personnel, family members, and retirees (aged at least 18 years), who suffered blunt trauma and presented to a military hospital emergency department with complaints of cervical spine pain. [43]
All four validity studies [39–42] were phase III cohorts comparing the CCR to a reference standard. The reference standard that was selected included radiographic imaging and a follow-up via telephone or mail to confirm the absence of clinically important cervical spine injury. All four reliability studies examined inter-rater reliability:(1) between nurses and physicians [40, 41];
(2) within a single group of practitioners: nurses [41] and paramedics [42]; and
(3) among physicians of varying experience levels. [43] The background and experience levels of the assessors applying the clinical prediction rules varied among studies (Tables 2, 3).
Risk of biasValidity studies All four low-risk bias studies used a clear research question, appropriate reference standard, appropriate index reviewer blinding methods, and valid and reliable outcome measures (Table 1a). However, these studies had the following limitations:
(1) utilization of a convenience sample [39, 40, 42];
(2) unclear information on whether interpretation of the reference standard was done without knowledge of the index test [39, 40]; and
(3) participants received different reference standards. [39–42]Reliability studies All four reliability studies with low risk of bias used a clear research question, appropriate reference standard, appropriate index reviewer blinding methods, and valid and reliable outcome measures (Table 1b). Included studies had the following limitations: (1) unclear inter-rater blinding methods [41] and (2) unclear methods for concealment of clinical information. [40–43]
Summary of evidenceValidity of the Canadian C–spine rule Three low-risk bias studies (Table 2) assessed the validity of the Canadian C-spine rule (CCR) for screening alert, stable patients presenting to emergency departments. [39–41] Stiell et al. reported a sensitivity of 1.00 (95% CI: 0.91, 1.00), a specificity of 0.43 (95% CI: 0.42, 0.45), and a negative predictive value of 100% when physicians applied the CCR. [41] When triage nurses applied the CCR, the sensitivity was 0.90 (95% CI: 0.76, 0.95). [41] Miller et al. also investigated the CCR when administered by emergency nursing staff and reported a sensitivity of 1.00 (95% CI: 0.91, 1.00), a specificity of 0.51 (95% CI: 0.42, 0.45), and a negative predictive value of 100%. [40] Coffey et al. reported a sensitivity of 1.00 (95% CI: 0.91, 1.00), specificity of 0.43 (95% CI: 0.39, 0.54), and negative predictive value of 100% when emergency department physicians applied the CCR. [39]
One low-risk bias study investigated the validity using two different applications of the CCR: 1) CCR applied in the field by paramedics and 2) CCR applied by investigators reviewing paramedic care reports (Table 2). When applied in the field by paramedics, the CCR had a sensitivity of 1.00 (95% CI: 0.74, 1.00), specificity of 0.38 (95% CI: 0.36, 0.40), and negative predictive value of 100% (95% CI: 99, 100). When applied by investigators using the paramedics’ care reports, the CCR had a sensitivity of 1.00 (95% CI: 0.74, 1.00), specificity of 0.43 (95% CI: 0.40, 0.45), and negative predictive value of 100% (95% CI: 0.99, 1.00).
Reliability of the Canadian C–spine rule Miller et al. found an inter-rater reliability of k = 0.60 (95% CI 0.50, 0.62) between physicians and nurses. [40]Stiell et al. found inter-rater reliability of k = 0.75 (95% CI 0.67, 0.84) between physicians and nurses and k = 0.78 (95% CI 0.72, 0.84) among nurses only. [41] One additional study investigated the reliability of a modified version of the Canadian C-spine rule (CCR). [42]They reported an inter-rater reliability among paramedics of k = 0.93 (95% CI 0.87, 0.99) (Table 3).
Reliability of the NEXUS low–risk criteria Matteucci et al. reported an inter-rater reliability of k = 0.53 (95% CI 0.35, 0.72). [43] The items of the tool with the lowest agreement were altered mental status (k = 0.22 95% CI: 0.11, 0.55), focal neurological deficit (k = 0.21 95% CI: 0.19, 0.62), and distracting injury (k = 0.13 95% CI: -0.19, 0.44). [43]
Discussion
Summary of evidence
Our systematic review examined the validity and reliability of clinical prediction rules used to screen for cervical spine injury in alert low-risk adult patients with blunt trauma to the neck. We summarized the findings from five low-risk bias studies on the diagnostic accuracy and reproducibility of the Canadian C-spine rule (CCR) and Nexus Low-Risk Criteria (NLC).
Evidence from four studies [39–42] reported consistently high sensitivity and negative predictive values for the CCR, suggesting that a negative test result is highly informative to clinicians for excluding a clinically significant cervical spine injury. Conversely, and as expected, the specificity of the CCR was lower in all four studies. [39–42] Therefore, using the CCR results is associated with an important number of false positives.
In three studies, triage nurses and paramedics demonstrated acceptable agreement using the CCR to determine the necessity for immobilization. [40–42] Only one study evaluated the NLC and found unacceptable levels of agreement between emergency medicine (EM) physicians and EM residents. [43] The findings suggest that there may be subjectivity in how NLC criteria are interpreted. Furthermore, examiners of different expertise, backgrounds, and levels of experience may interpret the NLC differently. A recent study by Tran et al. examined the improved diagnostic accuracy of a modified version of the NLC, which included two changes, modified definition of distracting injury and the definition of normal mentation. [44] They reported a sensitivity of 1.00 (95% CI: 0.68, 1.00), a specificity of 0.48 (95% CI: 0.44, 0.51), and a negative predictive value of 1.00 (95% CI: 0.99, 1.00). They suggest that the modifications to the NLC may improve the tool’s accuracy. [44] Clarifying the definitions of distracting injuries and mental status may also positively impact the reliability of the tool.
Previous systematic reviews
The Neck Pain Task Force summarized evidence from 11 studies on the validity of clinical prediction rules for screening alert low-risk patients with blunt trauma to the neck. [4] The CCR and the NLC demonstrated high sensitivity and negative predictive values for ruling out significant cervical spine injury. In one of the articles included, CCR was reported superior to the NLC with respect to sensitivity [99.4% (95% CI: 96–100) vs. 90.7% (95% CI: 85–94), respectively] and specificity [45.1% (95% CI: 44–46) vs. 36.8% (95% CI: 36–38), respectively] for cervical spine injury, and its use would result in reduced rates of radiography. [12] The NPTF concluded that these instruments effectively inform clinicians on the necessity of further diagnostic imaging. Another systematic review reported on the accuracy of the CCR and the NLC. Michaleff et al. reported evidence from 15 studies and noted that both rules demonstrated consistently high sensitivity. [19] They concluded that a negative prediction is highly informative in the exclusion of clinically significant cervical spine injury and the necessity for radiographic examination.
Our findings expand on the conclusions of the previous reviews by summarizing findings regarding the reliability of the CCR and NLC. Although these instruments demonstrate consistent performance in terms of high sensitivity and negative predictive values, the inter-examiner reliability of the NLC may vary depending on the expertise, background, experience, and training of the health professional. Specifically, a lack of reproducibility when the NLC is applied by multiple examiners of varied experience levels may jeopardize its validity.
Additional findings
In addition to being valid and reliable, the Canadian C-spine rule appears to improve the efficiency of health care resource use in practice. Coffey et al. reported that a reduction in cervical spine radiographs of 17.4% (95% CI 15 to 19%) would have been achieved without compromising patient safety. [39] Furthermore, two studies reported a reduction in the rate of cervical spine immobilization by triage nurses of 25% (95% CI: 21, 29%) [40] and 40% [41] when the CCR was followed. Similarly, Vaillancourt et al. reported that if paramedics had instituted their findings from the modified CCR, only 62.2% (95% CI 60 to 64%) of recruited patients would have required immobilization in the field. [42]
In addition, evidence suggests that the majority of professionals reported feeling comfortable (‘comfortable’ or ‘very comfortable’) using the clinical prediction rules, with values ranging among professionals from 82 to 90%. [39–42] Comfort with use of the NLC was not reported.
Recommendations for future studies
Our review found only one article with a low risk of bias that evaluated the reliability of the Nexus Low-Risk Criteria (NLC). Future studies may focus on the validity and reliability of this clinical prediction rule among health care professionals with varied expertise, backgrounds, and levels of experience and in multiple health care settings.
Clinical relevance and implications
There is strong consistent evidence that using clinical prediction rules for adult patients with blunt trauma to the neck effectively clears the cervical spine without the need for imaging. The clinical prediction rules have the potential, if globally adopted, to standardize practice and improve efficiency in the use of cervical spine radiography without compromising patient safety.
Strengths and limitations
Our review has a number of strengths. We utilized an extensive and rigorous search strategy. We pre-defined explicit inclusion and exclusion criteria to identify possibly relevant studies. We utilized two pairs of independent reviewers to minimize error and potential bias. Furthermore, we used the QUADAS-2 and QAREL tools to standardize the critical appraisal process and inform our scientific judgement on study admissibility. Finally, we utilized principles of best evidence synthesis, excluding studies with high risk of bias.
Our review also has limitations. First, we limited our search to the English and French language literature. Second, the critical appraisal process entailed judgement by the reviewers, which may be subjective. This potential bias was limited by training the reviewers and using standardized critical appraisal methods.
Conclusion
When synthesized with the Neck Pain Task Force, the evidence consistently demonstrates that the Canadian C-spine rule (CCR) has excellent sensitivity and negative predictive values, indicating strong clinical value in ruling out serious cervical spine injury and informing the need for further diagnostic imaging. Furthermore, our review adds new information regarding the tools’ reproducibility. We identified that the CCR has acceptable inter-examiner reliability. We found only one study evaluating the reliability of the NLC demonstrating underwhelming levels of reproducibility. Therefore, there is insufficient evidence to conclude on the validity or reliability of the Nexus Low-Risk Criteria (NLC).
Acknowledgments
The authors acknowledge and thank Mrs. Sophie Despeyroux, librarian at the Haute Autorité de Santé, for her suggestions and review of the search strategy. The authors also acknowledge Dr. Jessica Wong, who provided methodological guidance and training for several co-authors. This research was undertaken, in part, thanks to funding and supervision from the Canada Research Chairs program to Dr. Pierre Cote, Canada Research Chair in Disability Prevention and Rehabilitation at the University of Ontario Institute of Technology.
Funding
This study was funded by the Institut Franco-Européen de Chiropraxie, the Association Française de Chiropraxie and the Fondation de recherche en chiropraxie in France. None of these associations was involved in the collection of data, data analysis, interpretation of data, or drafting of the manuscript.
Conflict of interest
We have no potential conflict of interest.
References:
Fredø HL, Bakken IJ, Lied B, Rønning P, Helseth E (2014)
Incidence of traumatic cervical spine fractures in the Norwegian population: a national registry study.
Scand J Trauma Resusc Emerg Med 18(22):78National Center for Health Statistics (2012)
Health, United States, 2011: With Special Feature on Socioeconomic Status and Health.
Hyattsville, MDDavis JW, Phreaner DL, Hoyt DB, Mackersie RC (1993)
The etiology of missed cervical spine injuries.
J Trauma 34(3):342–346Nordin M, Carragee EJ, Hogg-Johnson S, Weiner SS, Hurwitz EL, Peloso PM, et al.
Assessment of Neck Pain and Its Associated Disorders:
Results of the Bone and Joint Decade 2000–2010 Task Force on
Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S101–S122Griffith B, Bolton C, Goyal N, Brown ML, Jain R (2011)
Screening cervical spine CT in a level I trauma center: overutilization?
AJR Am J Roentgenol 197(2):463–467Vandemark RM (1990)
Radiology of the cervical spine in trauma patients: practice pitfalls and recommendations for improving efficiency and communication.
AJR Am J Roentgenol 155(3):465–472McNamara RM, Heine E, Esposito B (1990)
Cervical spine injury and radiography in alert, high-risk patients.
J Emerg Med 8(2):177–182Roberge RJ, Wears RC, Kelly M, Evans TC, Kenny MA, Daffner RD, Kremen R (1988)
Selective application of cervical spine radiography in alert victims of blunt trauma: a prospective study.
J Trauma 28(6):784–788Bayless P, Ray VG (1989)
Incidence of cervical spine injuries in association with blunt head trauma.
Am J Emerg Med 7(2):139–142Jacobs LM, Schwartz R (1986)
Prospective analysis of acute cervical spine injury: a methodology to predict injury.
Ann Emerg Med 15(1):44–49Daffner RH (1993)
Cervical radiography in the emergency department: who, when, how extensive?
J Emerg Med 11(5):619–620Stiell IG, Clement CM, McKnight RD, Brison R, Schull MJ, Rowe BH, Worthington JR (2003)
The Canadian C-spine rule versus the NEXUS low-risk criteria in patients with trauma.
N Engl J Med 349(26):2510–2518Moloney TW, Rogers DE (1979)
Medical technology – a different view of the contentious debate over costs.
N Engl J Med 301(26):1413–1419Stiell IG, Wells GA, Hoag RH, Sivilotti ML, Cacciotti TF, Verbeek PR, Greenway KT (1997)
Implementation of the Ottawa knee rule for the use of radiography in acute knee injuries.
JAMA 278(23):2075–2079Como JJ, Diaz JJ, Dunham CM, Chiu WC, Duane TM, Capella JM, Holevar MR, Khwaja KA (2009)
Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee.
J Trauma 67(3):651–659National Clinical Guideline Centre (UK) (2016)
Spinal injury: assessment and initial management.
National Institute for Health and Care Excellence (UK), LondonLaupacis A, Sekar N, Stiell IG (1997)
Clinical prediction rules. A review and suggested modifications of methodological standards.
JAMA 77(6):488–494Stiell IG, Wells GA (1999)
Methodologic standards for the development of clinical decision rules in emergency medicine.
Ann Emerg Med 33(4):437–447Michaleff ZA, Maher CG, Verhagen AP, Rebbeck T, Lin CW (2012)
Accuracy of the Canadian C-spine rule and NEXUS to screen for clinically important cervical spine injury in patients following blunt trauma: a systematic review.
CMAJ 184(16):E867–E876Lemeunier N, da Silva-Oolup S, Chow N, et al (2017)
Reliability and Validity of Clinical Tests to Assess the Anatomical Integrity of the Cervical Spine
in Adults with Neck Pain and its Associated Disorders: Part 1- A Systematic Review from the
Cervical Assessment and Diagnosis Research Evaluation (CADRE) Collaboration
European Spine Journal 2017 (Sep); 26 (9): 2225–2241Lemeunier N, da Silva-Oolup S, Olesen K, Carroll LJ, Shearer H, Wong JJ, Brady OD (2017)
Reliability and validity of clinical tests to assess measurements of pain and disability in adults with neck pain and its associated disorders: Part 3. A systematic review from the Cervical Assessment and Diagnosis Research Evaluation (CADRE) Collaboration.
European Spine Journal. in submissionLemeunier N, Jeoun EB, Suri M, Tuff T, Shearer H, Mior S, Wong JJ, da Silva-Oolup S (2017)
Reliability and validity of clinical tests to assess the posture, pain location and cervical mobility in adults with neck pain and its associated disorders: Part 4. A systematic review from the Cervical Assessment and Diagnosis Research Evaluation (CADRE) Collaboration.
European Spine Journal; in submissionLemeunier N, Suri M, Welsh P, Shearer H, Nordin M, Wong JJ, Torres, da Silva-Oolup S (2017)
Reliability and validity of clinical tests to assess the functionality of the cervical spine in adults with neck pain and its associated disorders: Part 5. A systematic review from the Cervical Assessment and Diagnosis Research Evaluation (CADRE) Collaboration.
European Spine Journal; in submissionGuzman J, Hurwitz EL, Carroll LJ, Haldeman S, Cote P, Carragee EJ, Peloso PM (2008)
A New Conceptual Model Of Neck Pain: Linking Onset, Course, And Care Results of
the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S14–23Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Gonzalez RP, Fried PO, Bukhalo M, Holevar MR, Falimirski ME (1999)
Role of clinical examination in screening for blunt cervical spine injury.
J Am Coll Surg 189(2):152–157Teasdale G, Jennett B (1974)
Assessment of coma and impaired consciousness. A practical scale.
Lancet 2(7872):81–84Saltzherr TP, Fung Kon Jin PH, Beenen LF, Vandertop WP, Goslings JC (2009)
Diagnostic imaging of cervical spine injuries following blunt trauma: a review of the literature and practical guideline.
Injury 40(8):795–800Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G (2014)
The Glasgow Coma Scale at 40 years: standing the test of time.
Lancet Neurol. 13(8):844–854
(Review. Erratum in: Lancet Neurol 13(9):863)Fletcher RH, Fletcher SW, Fletcher GS (2012)
Clinical epidemiology: the essentials (Fifth edition).
Lippincott Williams & Wilkins, a Wolter Kluwer businessWhiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM (2011)
QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies.
Ann Intern Med 155(8):529–536Lucas N, Macaskill P, Irwig L, Moran R, Rickards L, Turner R, Bogduk N (2013)
The reliability of a quality appraisal tool for studies of diagnostic reliability (QAREL).
BMC Med Res Methodol 13:11Sackett DL, Haynes RB (2002)
The architecture of diagnostic research.
BMJ 324:539–541Slavin RE (1995)
Best evidence synthesis: an intelligent alternative to meta-analysis.
J Clin Epidemiol 48:9–18Viera AJ, Garrett JM (2005)
Understanding interobserver agreement: the kappa statistic.
Fam Med 37:360–363Moher D, Liberati A, Tetzlaff J, Altman DG (2009)
Preferred Reporting Items for Systematic Reviews and Meta-Analyses:
The PRISMA Statement
Int J Surg 2010; 8 (5): 336–341Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, Lijmer JG (2003)
Standards for reporting of diagnostic accuracy. toward complete and accurate reporting of studies of diagnostic accuracy. The STARD initiative.
Am J Clin Pathol 119(1):18–22Duane TM, Mayglothling J, Wilson SP, Wolfe LG, Aboutanos MB, Whelan JF, Malhotra AK (2011)
National emergency X-radiography utilization study criteria is inadequate to rule out fracture after significant blunt trauma compared with computed tomography.
J Trauma 70(4):829–831Coffey F, Hewitt S, Stiell I, Howarth N, Miller P, Clement C et al (2011)
Validation of the Canadian c-spine rule in the UK emergency department setting.
Emerg Med J: EMJ 28(10):873–876Miller P, Coffey F, Reid A, Stevenson K (2006)
Can emergency nurses use the Canadian cervical spine rule to reduce unnecessary patient immobilisation?
Accid Emerg Nurs 14(3):133–140Stiell IG, CeM Clement, O’Connor A, Davies B, Leclair C, Sheehan P et al (2010)
Multicentre prospective validation of use of the Canadian C-spine rule by triage nurses in the emergency department.
CMAJ 182(11):1173–1179Vaillancourt C, Stiell IG, Beaudoin T, Maloney J, Anton AR, Bradford P et al (2009)
The out-of-hospital validation of the Canadian C-spine rule by paramedics.
Ann Emerg Med 54(5):663-71Matteucci MJ, Moszyk D, Migliore SA (2015)
Agreement between resident and faculty emergency physicians in the application of NEXUS criteria for suspected cervical spine injuries.
J Emerg Med 48(4):445–449Tran J, Jeanmonod D, Agresti D, Hamden K, Jeanmonod RK (2016)
Prospective validation of modified NEXUS cervical spine injury criteria in low-risk elderly fall patients.
West J Emerg Med. 17(3):252–257
Return to RADIOLOGY
Return to CLINICAL PREDICTION RULE
Since 10-08-2017


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |