

Providing Information at the Initial Consultation to
Patients with Low Back Pain Across General Practice,
Chiropractic and Physiotherapy - A Cross-sectorial
Study of Danish Primary CareThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Scand J Prim Health Care 2022 (Oct 31); 1–9 ~ FULL TEXT
OPEN ACCESS Lars Morsø, Jesper Lykkegaard, Merethe Kirstine Andersen, Anders Hansen, Mette Jensen Stochkendahl, Simon Dyrløv Madsen, Berit Schiøttz Christensen
Department of Clinical Research,
Research Unit OPEN,
University of Southern Denmark,
Odense, Denmark
Objective: Clinical guidelines for managing low back pain (LBP) emphasise patient information, patient education and physical activity as key components. Little is known about who actually receives information. This study investigates to what extent information at the first consultation with general practitioner (GP), chiropractor (DC) and physiotherapist (PT) in Danish primary care is provided to patients with LBP.
Design and setting: This cross-sectorial study was conducted as a prospective survey registration of LBP consultations at the three primary health care professions in Denmark.
Intervention: Clinicians ticked off a paper survey chart during or after consultations with patients who visited the clinic for LBP (Approval number: ID # 11.220).
Subjects: 33 GPs, 43 DCs and 61 PTs registered first-time consultations.
Main outcome measures: The primary outcome was provision of information, overall and across care settings.
Results: The overall proportion of patients provided with information was 72%, but this varied among professions(GP, 44%;
DC, 76%; and
PT, 74%).Provision of information increased to 78% if patients had increased emotional distress or back-related leg pain below the knee. The strongest association with provision of information was having two or three signs of elevated distress (OR 2.58 and 5.05, respectively, p= 0.00) or physical disability (OR 2.55, p= 0.00).
Conclusion: In more than a quarter of first-time consultations, patient information was not provided. Large variation in providing information was found across the settings. The proportion provided with information increased for sub-populations having elevated distress or back-related leg pain below the knee.
Keywords: Low back pain; clinical guidelines; primary care; prospective survey registration; provision of information.
Key Points
Clinical guidelines recommend patient information, patient education and physical activity for managing low back pain (LBP)
Information is not provided in more than a quarter of first-time consultations in Danish primary care settings that manage these patients.
Information increased for the sub-populations having elevated distress and back-related leg pain below the knee.
The conducted primary care surveys monitored clinical activity and illustrated variations in provision of information.
From the FULL TEXT Article:
Introduction
Low back pain (LBP) is common globally. [1] In Denmark, the point prevalence estimate is 13.7% [2], and most primary care consultations regarding musculoskeletal conditions are for LBP. [3] The vast majority of patients with LBP are managed in primary care in general practice or at chiropractor and physiotherapy clinics. The yearly Danish treatment cost for LBP is €240 million, and Danes with LBP have 3.3 million more visits at the general practitioner (GP), and 2.3 million more visits at the chiropractor (DC) and physiotherapist (PT), per year than people without LBP. [4]
Internationally, clinical guidelines for managing LBP emphasise patient information, patient education and physical activity as key components. [5, 6] In the Danish guidelines, patient information and education are recommended, and the guidelines state that initial LBP management should include information on prognosis, warning signs and staying active. [6] Further, the Danish guidelines recommend patient education consisting of dialog-based reassurance with cognitive and behavioural components to patients with low self-efficacy or self-management skills, or at risk of a poor prognosis. [5, 6]
Several factors may negatively affect the LBP prognosis, including psychosocial and cognitive components [7-9], disability [10] and back-related leg pain. [11] According to guideline recommendations, LBP patients with indications of poor prognosis, elevated distress or leg pain should receive information and/or education as a central part of the initial management, but the clinical reality may differ from guideline recommendations. [12] Previous studies indicate large variations in clinicians’ approaches to LBP [10, 13] and suboptimal compliance with guideline recommendations. [12] For example, in 2013, different health care professionals in Danish primary care gave information regarding back symptoms and prognosis in 60% to 80% of LBP consultations. [14] However, little is known about which patients actually receive information and/or patient education or if information and education are given to those intended, especially if patients with a poor prognosis, distress or leg pain are managed as recommended in the guidelines.
This study aims to investigate to what extent information at the first consultation with one of the three professions of GP, DC and PT in Danish primary care is provided to patients with LBP. We investigate patient characteristics associated with provision of information, and we analyse if patients with elevated psychological/cognitive distress or back-related leg pain below the knee are provided information differently than patients without these characteristics.
Material and methods
Design
The study is observational and cross-sectorial. We conducted a consecutive survey registration of consecutive LBP consultations in the three main primary health care provider groups (GP, DC and PT) in Denmark. The registration also included the regional secondary care spine centre, but this paper only regards primary care. The Danish health care system is generally tax-funded and offers free and equal access for all Danish citizens to consult a GP and to receive a subsidy that partly covers expenses for DC and PT treatment in primary care. The subsidy for PT treatment requires a GP referral.
In the study, we used a well-tested paper survey chart method [15] developed by Audit Project Odense (APO). We invited all registered GP, DC and PT primary care clinics in the Region of Southern Denmark (covering approx. 1.2 million inhabitants) to participate in the survey. The survey registration was conducted during November and December 2019. Each clinician was asked to tick off the paper survey chart during or after consecutive consultations with adults (>16 years) who visited the clinic for LBP. The registration durations, 2 weeks for DC and PT clinicians and 4 weeks for GP clinicians, were based on the estimated prevalence of patients consulting for LBP.
All the clinicians participated voluntarily and signed a written consent form before study entry. All collected patient data were anonymous, and no written consent was necessary. In accordance with Danish legislation, the authorised legal department at the University of Southern Denmark approved the study (ID # 11.220).
The survey
The survey chart contained 45 variables for PTs and 47 for GPs and DCs within ten domains (Appendix 1) and started with registration of the consultation number (i.e. number of consultations during current pain episode). The ten domains covered items assessed during the consultation, including pain location and duration, psychosocial risk factors of LBP, initiated treatment, recommendations on medication, and referral. Most questions (40 of 45/47) were identical across professions, but some were adapted to fit the scope of practice of each profession. The items reflected the scientific literature, the clinical guidelines for LBP [6] and common clinical practice as determined by consensus of a development group within the project with representatives from all three professions. This approach was chosen to ensure coverage of common clinical practice not included in the clinical guidelines. Domains were designed with exhaustive answer categories. If a full domain was left unticked, it was coded as missing. Each registration obtained the clinician’s subjective valuations based on the interaction with the patient. To assist the clinicians with interpretation of the items, a definition and description of each item was included in the survey. Prior to distribution of the survey, the survey chart was pilot tested by a sample of GPs, DCs and PTs and revised according to the feedback. A common coding manual was provided to all participants prior to the survey.
Participating clinicians also completed a background questionnaire containing information on age, gender, profession, experience, type of clinic, primary care collaborators and knowledge about and application of regional management procedures [16] and the STarT Back Tool. [7]
Analysis
All first-time consultations with patients experiencing a new episode of LBP were included in the analysis. The primary outcome was provision of information (reflected in item number 24 ‘information on back symptoms including prognosis’), overall and across care settings.
Supplementary analyses were conducted for two subgroups of patients with increased risk of disability. [17](1) Patients with elevated psychological/cognitive distress (defined as experiencing one of three items of impairments or disability, including poor sleep, emotional distress and 2 or more pain sites in addition to LBP; the three variables were significantly correlated, indicating that all three reflected distress),
(2) patients with back-related leg pain below the knee.The two sub-populations were collapsed, and differences for receiving information if ‘not in a sub-population’ versus being ‘in a sub-population’ were tested using Kruskal–Wallis. The overall results were displayed as univariate and multivariate analyses adjusted for setting, age, gender, duration of episode, prior episodes, pain location, distress, sick leave, physical disability and pain medication. Odds ratios (ORs) for provision of information at the initial consultation were analysed and modelled using Stata®, release 15.0 (StataCorp, College Station, TX). p Values of <0.05 were considered statistically significant.
Results

Table 1 In total, 33 GPs registered 149 first-time consultations, 43 DCs registered 683 first-time consultations and 61 PTs registered 308 first-time consultations (Table 1). Overall, 53% of the included patients were women, and the median age was 52 years (interquartile range [IQR] 40–64 years). The median symptom duration at the time of consultation was 2 weeks (IQR 0–8 weeks), and 62% of all included patients had had previous episodes of LBP. Across professions, there were significant differences in all these variables, with PTs seeing more women, patients that were older and patients with longer pain duration (Table 1).

Table 2 The overall proportion of patients provided with information was 72%, but this proportion varied, with 44% at GPs, 76% at DCs and 74% at PTs. If patients were classified into one of the two pre-defined sub-populations of having increased emotional distress or back-related leg pain below the knee, the overall proportion of patients who were provided with information at the first consultation increased to 78% for both sub-populations. Provision of information for the ‘distress sub-population’ increased to 47% at GPs, 84% at DCs and 77% at PTs. For the ‘leg pain sub-population,’ provision of information increased at GPs to 54% and at DCs to 89%, but decreased at PTs to 73%. Compared with patients not belonging to any of the subgroups, patients in either one of the subgroups were more likely to receive information (Table 2).

Table 3 Patient characteristics associated with provision of information at the first visit in the overall population are displayed in Table 3. In the univariate analysis, several variables were associated with the provision of information. The strongest association with the provision of information was having two or three signs of elevated distress (OR 2.58 and 5.05, respectively, p= 0.00) and physical disability (OR 2.55, p= 0.00). GPs were significantly less likely to provide information (OR 0.25, p= 0.00).
In the multivariate analysis, the association of providing information with distress, physical disability and attending a GP consultation was largely retained, whereas patients having >2 previous episodes were negatively associated with the provision of information (OR 0.54, p= 0.00). In the multivariate model, association with sick leave was washed out (Table 3).

Table 4

Table 5 Across the three professions, the associations for providing information at the first consultation showed considerable variation. For GPs, the multivariate analysis washed out all significant associations from the overall analysis (Table 4). For DCs, the multivariate analysis revealed significant associations with episode (OR 0.31, p= 0.00), level of distress (OR 2.30, 3.37 and 4.10, p= 0.00–0.03) and physical disability (OR 2.92, p= 0.00). Further, the DCs were more likely to give male patients information compared with female patients (OR 1.48, p= 0.05) (Table 4). For PTs, the statistically significant associations in the multivariate analysis were having ‘severe’ elevated distress (all three signs) and physical disability (OR 4.33, p= 0.03, and 2.13, p= 0.02, respectively) (Table 4).
The secondary analyses included the two sub-populations defined by elevated distress (subgroup 1) or patients having back-related leg pain below the knee (subgroup 2). Analysis showed that information provision increased in both subgroups compared with patients not belonging to a subgroup. In subgroup 1, multivariate analysis showed that GPs registered provision of information at the first consultation significantly less often (OR 0.21, p= 0.00), while physical disability was positively associated with information (OR 1.94, p= 0.02) (Table 5).
In the second subgroup with back-related leg pain, both GPs and PTs were significantly less likely to provide information compared with DCs (OR 0.17 and 0.31, respectively). In this subgroup, physical disability was associated with provision of information (OR 3.19, p = 0.03) (Table 5).
Discussion
The study aimed to investigate the extent to which GPs, DCs and PTs in Danish primary care provide information to patients with LBP at their first consultation. We found that in 72% of all first-time consultations, the professional registered having provided information on LBP symptoms and prognosis to the patient, but with considerable variation across professions (Figure 1). High-risk sub-populations were more often provided with information at their initial consultation, and elevated distress and physical disability were associated with an increased proportion of patients provided with information.
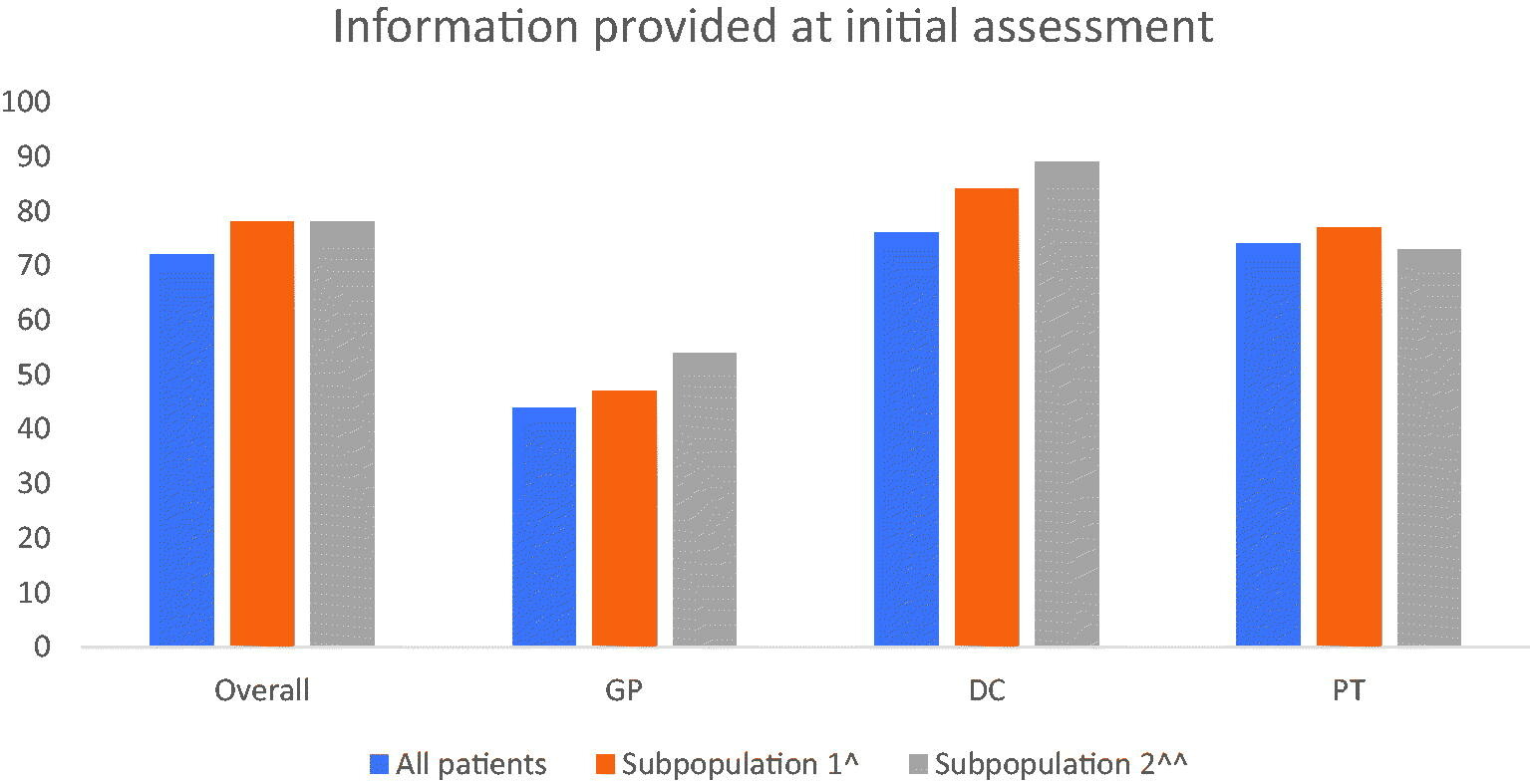
Figure 1 Figure 1. Information at first visit. Proportion of patients who receive information on LBP including prognosis and differences across subpopulations. ^Sub-population 1 is defined as having increased ‘distress’. Distress is defined by having ‘yes’ on one of the following three variables: 2 or more pain sites in addition to LBP, poor sleep, emotional distress. ^^Sub-population 2 is defined by having ‘pain below knee’.
Even though provision of information is generally recommended in clinical guidelines on LBP [5, 6], more than one in four PT and DC patients and more than half of the GP patients did not receive this. This may relate to the recommendations being relatively new and the uptake of the recommendation not complete yet. In one paper of the Lancet LBP series from 2018, it was stated that there are gaps between guidelines and daily clinic care, and that focus should be placed on implementing best practice and alignment of practice with evidence. [18] Further, clinical guidelines seldom provide specific and operationalised guidance on what to say to individual patients, which might offer another explanation for the inadequate implementation. [19]
This study showed distinct variation across the professions and in the patient populations, which also has been shown earlier. [20] The proportion of patients given information by GPs was significantly lower than by DCs and PTs. The lower provision of information by GPs was observed not only in patients in general, but also in subgroups to which clinic guidelines specifically recommend information on diagnosis and prognosis. In Danish primary care, the tasks of each profession differ. Among the GP’s main tasks are gatekeeping and diagnostics, including referring to relevant primary and secondary health care. In LBP patients, referral has traditionally been mainly to PTs (and to a lesser degree DCs) for treatment. Therefore, it could be speculated that the GP leaves it to the PT (or DC) to provide patient information, and provides information more sparsely. Another explanation could be that most of the patients (62%) have had prior episodes, and GPs may think that sufficient information has already been provided at an earlier stage. This contrasts with DCs and PTs who still provide information in more consultations even though their patients also have had prior episodes. Nonetheless, our findings and suggested explanations are at direct odds with the health information needs of people with LBP: They request general information related to LBP, its cause and underlying pathology, information of general management approaches and self-management strategies – especially in situations with flare-ups. [21]
Systemic and organizational procedures, such as time allocated to each patient and referral rights, also differ across the professions, and the differences in allocated time may reflect the differences in provision of information. This is well in line with time restraint being a main clinician barrier to adherence to guidelines. [22] Further, the patient population differs across the three settings, with GPs providing information to fewer patients with LBP compared with PTs and DCs, which may explain the variation in emphasis on providing information across settings.
The study showed that the professionals were overall more likely to give information to patients with elevated distress (widespread pain, poor sleep and emotional distress). Cognitive/psychological distress has been shown to affect prognosis and prolong LBP episodes [9, 23], and information on strategies for handling distress has been suggested as a viable means to minimise the risk of a poor outcome. Nevertheless, large differences were seen across professions. In the DC setting, having one of the three distress signs was significantly associated with provision of information, whereas this was only the case in the PT setting if all three signs were present, and non-associated in the GP setting. It has been shown that psychological elements defining the psychosocial profile of patients change across an LBP episode, with high levels of emotional distress in the early stages. [24] This might explain why elevated distress is highly significantly associated with providing information in the DC setting, where patients have significantly shorter duration compared with the GP and PT settings [24]. Differences in patient population may also explain why associations with gender and number of previous episodes are different in the DC setting.
Back-related leg pain has also been described to affect LBP prognosis [11], and the overall level of information provided for this subgroup was higher than for the overall population. Nevertheless, the odds for giving information to this sub-population were significantly lower at PTs and GPs compared with DCs. There are several possible explanations for these differences. First, is the perception of the importance of leg pain in regard to prognosis, and second is the nature of the leg pain (referred or radiating). Further, duration may be a factor in shifting the focus away from back-related leg pain. Patients referred to PTs have a duration of 5 weeks; the prolonged timeframe might explain lower awareness about providing information for this subgroup on prognosis and instead the focus on advice on daily activities. In contrast, an increased focus on leg pain might be a result of the regional reimbursement agreement for DCs introducing a standardised care package for patients presenting with symptoms of lumbar radiculopathy. The structural incentive might increase focus on radiculopathy symptoms, and DCs might allocate more time, be more aware of the representation of leg pain and, therefore, be more vigilant in providing information.
The analyses showed that physical disability was addressed across professions. This is in line with the usual assessment of LBP problems [10] and reflects the expectations of patients who consult for assistance in pain relief and functional improvement. [25]
Strength and limitations
An obvious limitation is the nature of the data. All variables are based on registration from the professionals. Although instructions specified that data entering should be done consecutively, we do not know if data were entered during the consultation, immediately after the consultation or at the end of the day. Further, we do not know how strict the clinicians followed the definitions of single items when entering data. Nevertheless, we know from previous studies using prospective survey registration that data are highly useful and reflect daily clinic activities. [15] In the study, it was recorded whether information was provided or not. We are not able to detect the specific information given or if it was given orally or in writing. Therefore, we are not able to specify the quality or relevance of the given information.
Despite providing clinicians with a common coding manual, the single items in the survey might be understood differently and could therefore affect the data quality. We tried to avoid this by piloting the questionnaire and giving the clinicians the opportunity to consult with the project managers during the project. This resulted in minor rephrasing of paragraphs and adjusting of single items.
A strength of the study is the number of participants across the professions. The large number of consultations allowed us to model the analyses, adjusting for several parameters.
Perspectives
We have observed substantial differences between the settings as to providing patient information. This may to some extent be explained by inter-professional cultural differences regarding the priority of the various elements of managing patients with LBP, but also by remuneration. It could be argued that future price determination on remuneration and time-slots should better accommodate guideline adherent behaviour by recognising that a full examination, including assessment of important risk factors, and provision of patient information is time consuming.
Regular primary care surveys can be a way to monitor clinical activity and provide information on variations. This could advantageously be combined with interviews to qualify data.
Conclusion
Across the Danish primary care settings that manage patients with LBP, the guideline-recommended emphasis on patient information is not provided in more than a quarter of first-time consultations. Large variation in providing information exists across the settings, and the proportions provided with information increase for the sub-populations having elevated distress and back-related leg pain below the knee.
Supplementary Material
Acknowledgements
The authors would like to thank Susanne Døssing Berntsen, Audit Project Odense, for handling and mailing the survey charts to the participants. The authors would also like to acknowledge the work done by the primary care consultants to enrol clinicians in the study. We acknowledge Søren Bie Bogh, OPEN, for valuable help in data analysis. The study was funded by the Association of Danish Physiotherapists foundation for clinical practice, the Foundation for Promotion of Chiropractic Research and Postgraduate Education and the General Practitioners’ Quality and Postgraduate Foundation in the Region of Southern Denmark. The funders did not have any influence on study design, data collection, management, analysis, interpretation or the publication of results.
Disclosure statement
All authors declare no conflict of interest in the study.
Funding
The study was funded by the Association of Danish Physiotherapists foundation for clinical practice, the Foundation for Promotion of Chiropractic Research and Postgraduate Education and the General Practitioners’ Quality and Postgraduate Foundation in the Region of Southern Denmark.
References:
Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, Croft P.
Low Back Pain: A Call For Action
Lancet. 2018 (Jun 9); 391 (10137): 2384–2388
This is the fourth of 4 articles in the remarkable Lancet Series on Low Back PainKent PM, Keating JL.
The epidemiology of low back pain in primary care.
Chiropr Osteopat. 2005;13:13Moth G, Olesen F, Vedsted P.
Reasons for encounter and disease patterns in Danish primary care:
changes over 16 years.
Scand J Prim Health Care. 2012;30(2):70–75Flachs EM, Koch EL, Ryd MB, et al.
The health burden in Denmark [Sygdomsbyrden i Danmark – sygdomme].
København, Denmark: Statens Institut for Folkesundhed,
Syddansk Universitet; 2015Corp N, Mansell G, Stynes S, et al..
Evidence-based treatment recommendations for neck and low back pain
across Europe: A systematic review of guidelines
European J Pain 2021 (Feb); 25 (2): 275–295Stochkendahl MJ, Kjaer P, Hartvigsen J et al.
National Clinical Guidelines for Non-surgical Treatment of Patients
with Recent Onset Low Back Pain or Lumbar Radiculopathy
European Spine Journal 2018 (Jan); 27 (1): 60–75Hill JC, Dunn KM, Lewis M, et al.
A Primary Care Back Pain Screening Tool:
Identifying Patient Subgroups For Initial Treatment
(The STarT Back Screening Tool)
Arthritis and Rheumatism 2008 (May 15); 59 (5): 632–641Hill JC, Fritz JM.
Psychosocial influences on low back pain, disability, and response to treatment.
Phys Ther. 2011;91(5):712–721Hill JC, Whitehurst DG, Lewis M, Bryan S, Dunn KM, Foster NE,
K onstantinou K, Main CJ, Mason E, Somerville S, et al:
Comparison of Stratified Primary Care Management For Low Back Pain
With Current Best Practice (STarT Back): A Randomised Controlled Trial
Lancet. 2011 (Oct 29); 378 (9802): 1560–1571Kent PM, Keating JL, Taylor NF.
Primary care clinicians use variable methods to assess
acute nonspecific low back pain and usually focus on impairments.
Man Ther. 2009;14(1):88–100Konstantinou K, Dunn KM, Ogollah R, et al.
Prognosis of sciatica and back-related leg pain in primary care: the ATLAS cohort.
Spine J. 2018;18(6):1030–1040Bishop FL, Dima AL, Ngui J, et al.
Lovely pie in the sky plans”: a qualitative study of clinicians’ perspectives
on guidelines for managing low back pain in primary care in England.
Spine (Phila Pa 1976). 2015;40(23):1842–1850Kent PM, Keating JL.
Can we predict poor recovery from recent-onset nonspecific low back pain?
A systematic review.
Man Ther. 2008;13(1):12–28A DJM.
Patents with low back pain in the Danish region of Seeland
[Patienter med laenderygproblemer i Region Sjaelland].
Odense, Denmark: Syddansk Universitet; 2013Munck AP, Hansen DG, Lindman A, et al.
A Nordic collaboration on medical audit. The APO method for
quality development and continuous medical education (CME)
in primary health care.
Scand J Prim Health Care. 1998;16(1):2–6Styregruppe I Region S.
In: Banke J, Hatvigsen L, Pedersen FML, editors.
Patientforloebsprogram for Rygomrdet i Region Syddanmark.
Region Syddanmark, Denmark: 2010Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J et al.
What Low Back Pain Is and Why We Need to Pay Attention
Lancet. 2018 (Jun 9); 391 (10137): 2356–2367
This is the second of 4 articles in the remarkable Lancet Series on Low Back PainFoster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH (2018)
Prevention and Treatment of Low Back Pain:
Evidence, Challenges, and Promising Directions
Lancet. 2018 (Jun 9); 391 (10137): 2368–2383
This is the third of 4 articles in the remarkable Lancet Series on Low Back PainKongsted A, Hartvigsen J, Boyle E, et al.
GLA:D(R) Back: group-based patient education integrated with exercises
to support self-management of persistent back pain – feasibility of
implementing standardised care by a course for clinicians.
Pilot Feasibility Stud. 2019;5:65Morso L, Kongsted A, Hestbaek L, et al.
The prognostic ability of the STarT Back Tool was affected by episode duration.
Eur Spine J. 2016;25(3):936–944Lim YZ, Chou L, Au RT, et al.
People with low back pain want clear, consistent and personalised
information on prognosis, treatment options and self-management strategies:
a systematic review.
J Physiother. 2019;65(3):124–135Slade SC, Kent P, Patel S, et al.
Barriers to primary care clinician adherence to clinical guidelines
for the management of low back pain: a systematic review
and metasynthesis of qualitative studies.
Clin J Pain. 2016;32(9):800–816Morso L, Kent P, Albert HB, et al.
The predictive and external validity of the STarT back tool in Danish primary care.
Eur Spine J. 2013;22:1859–1867Morso L, Kent P, Albert HB, et al.
Is the psychosocial profile of people with low back pain seeking care
in danish primary care different from those in secondary care?
Man Ther. 2012;18:54–59Kongsted A, Ris I, Kjaer P, et al.
Self-management at the Core of Back Pain Care:
10 Key Points for Clinicians
Braz J Phys Ther 2021 (Jul); 25 (4): 396–406
Return to LOW BACK PAIN
Return to INITIAL PROVIDER/FIRST CONTACT
Since 11-02-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |