

The Physical and Psychological Impact of
Neurogenic Claudication: The Patients' PerspectivesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Can Chiropr Assoc 2017 (Mar); 61 (1): 18–31 ~ FULL TEXT
OPEN ACCESS Carlo Ammendolia, DC, PhD, Michael Schneider, DC, PhD, Kelly Williams, MPH, Susan Zickmund, PhD, Megan Hamm, PhD, Kent Stuber, DC, MSc, Christy Tomkins-Lane, PhD, and Y Raja Rampersaud, MD
University of Toronto,
Institute for Health Policy, Management and Evaluation,
Faculty of Medicine.
Background: The patient perspective regarding the impact of neurogenic claudication (NC) has not been well studied. The objectives of this study were to determine what is most bothersome among patients with NC and how it impacts their lives and expectations with surgical and non-surgical treatment.
Methods: Semi-structured telephone interviews were conducted, audio recorded and transcribed verbatim. A thematic analysis categorized key findings based on relative importance and impact on participants.
Results: Twenty-eight individuals participated in this study. Participants were most bothered by the pain of NC, which dramatically impacted their lives. Inability to walk was the dominant functional limitation and this impacted the ability to engage in recreational and social activities. The most surprising finding was how frequently participants reported significant emotional effects of NC.
Conclusions: From a patients' perspective NC has a significant multidimensional effects with pain, limited walking ability and emotional effects being most impactful to their lives.
Keywords : chiropractic; neurogenic claudication; outcome measurement; qualitative research; spinal stenosis.
From the FULL TEXT Article:
Introduction
Neurogenic claudication (NC) is the clinical syndrome associated with symptomatic lumbar spinal stenosis (LSS). It is characterized by bilateral or unilateral buttock, thigh or calf discomfort, pain, numbness or weakness precipitated by walking or prolonged standing and relieved by sitting and lumbar flexion. [1, 2] Low back pain may or may not be present in individuals with NC. The pathophysiology is thought to be compression and/or ischemia of the lumbosacral nerve roots due to narrowing of the lateral and central vertebral canals, usually as a consequence of degenerative osteoarthritic changes in the lumbar spine. [1, 3] Neurogenic claudication due to LSS is one of the most common causes of disability and loss of independence in older adults [4] and the most common reason for spine surgery in this population. [5]
New cases of NC due to LSS are expected to rise dramatically over the next 20 years when an estimated 25% of the population in both the U.S. and Canada will be over the age of 65. [6] Studies evaluating the effectiveness of both operative and non-operative treatments for NC have used a wide variety of primary and secondary outcome measures. [7–10] These outcome measures assess various constructs including bodily pain, bodily function, low back pain disability, back and leg pain, other leg symptoms, walking capacity (distance and time), walking performance, global improvement, quality of life, ranges of motion, treatment satisfaction and medication use.
In most studies the outcome measures used are reflective of the bias of the investigator(s) and is often inferred as the desired outcome of the patient. However, rarely has the perspective of the patient regarding the most important outcome been considered. For example, limitation in walking is felt to be the hallmark of NC and is used as a primary outcome measure in clinical trials. [7, 11, 12, 28] However, previous systematic reviews by this group [7, 11, 12] have demonstrated that many interventions for NC did not significantly improve walking performance or capacity. Despite this, several interventions were still associated with good patient satisfaction and/or pain relief.
Given the burden of NC, a lack of understanding of what outcomes are most important to those afflicted with NC represents a significant gap in both clinical and academic knowledge. Clinicians need to know what is most important to a patient in order to recommend effective intervention(s) that address the patient’s concerns. Researchers need to know what to measure in order to assess the most relevant patient outcome for a given intervention. Moreover, to make valid comparisons across studies and enable the pooling of data, a standardized set of outcome measures unique to this population and most relevant to patients is essential. In addition, there may be other constructs beyond those currently measured that may help to explain how this condition impacts people in different ways, and how these other factors can affect the patients experience and outcomes of NC.
The objectives of this study were to determine what outcomes matter most among individuals with NC due to LSS and to assess patients’ expectations and their experiences with surgical and non-surgical treatment.
Methods
Participant population and setting
We recruited a purposeful sample [13] of participants from two university-affiliated hospital surgical and non-surgical spine clinics both located in Toronto, Canada. To be eligible to participate, patients had to experience NC with axial imaging-confirmed LSS, and be able to communicate in English. To gain maximum variation of patient perspectives regarding their condition and success with treatment an attempt was made to select participants along the continuum of care. Specifically, we recruited participants scheduled for non-surgical (early, less severe symptoms) or surgical care (late, more severe symptoms), as well as those who had received surgical and non-surgical treatment. We included individuals of varying ages (50–90 years), gender, intensity and type of symptoms, as well as duration of symptoms (months to years).
All participants provided written informed consent. Research Ethics Board (REB) approval was received from the Mount Sinai Hospital REB Registration Number 13-0184-E and University Health Network REB Registration Number 13-6914-BE, as well as the Institutional Review Board (IRB) at the University of Pittsburgh (PRO13090531).
Semi-structured interviews
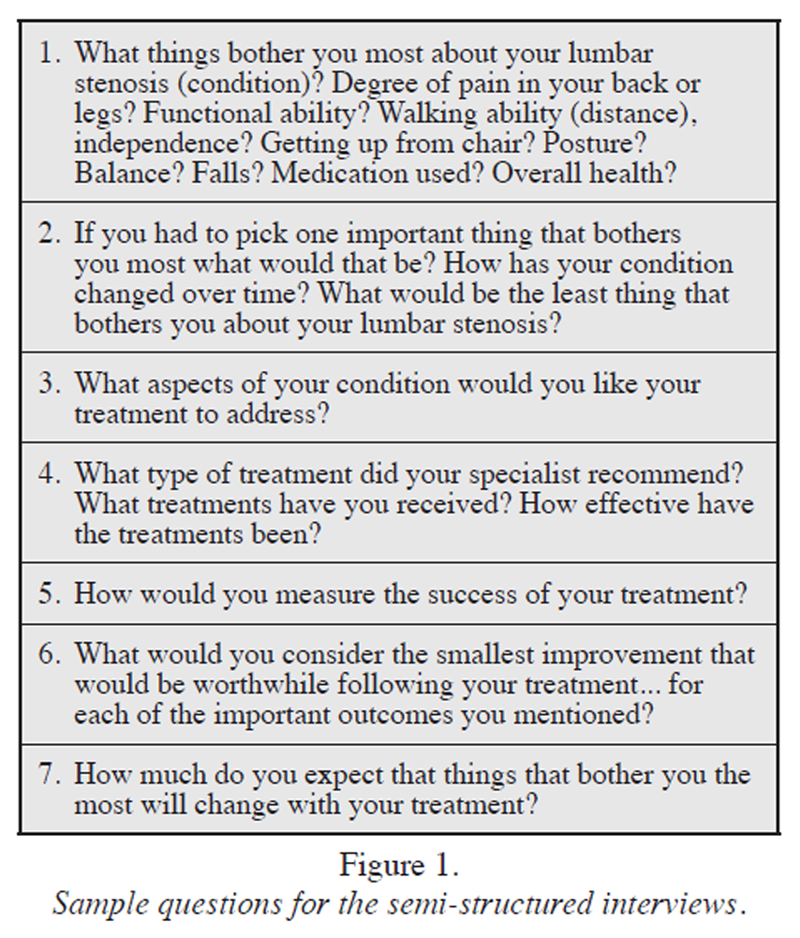
Figure 1
Box 1 Research assistants, trained by a qualitative research expert (SZ), conducted semi-structured telephone interviews lasting between 40 and 60 minutes. Interviews were audio recorded, and transcribed verbatim. Interviewers followed a standardized set of open-ended questions asking participants about their condition, focusing on what bothered them most and expectations regarding treatment. Figure 1 outlines a sample list of open-ended questions that were used.
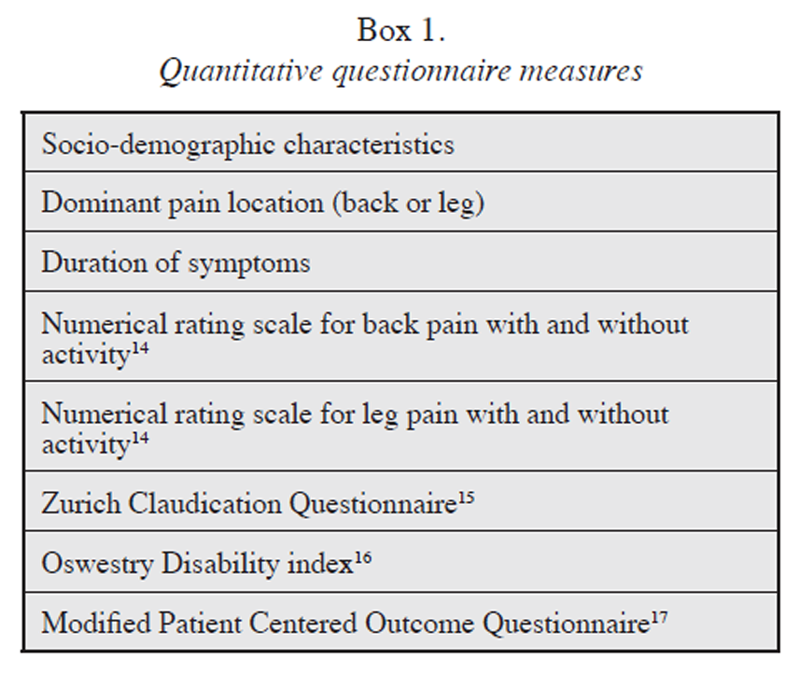
Quantitative measures questionnaire
A questionnaire was administered by telephone directly following the completion of the semi-structured interview. The aim of the questionnaire was to characterize the participant sample with respect to demographics, duration of symptoms, pain intensity and functional status and to compare surgical and non-surgical participants. Box 1 below lists the measures included in the questionnaire.
Analysis
Descriptive statistics were used to analyze the questionnaires. We compared pain, function and symptom outcomes among and between participants recruited from surgical and non-surgical clinics.
For the semi-structured interviews the frequency and types of responses were determined using the Crabtree and Miller “editing” approach to qualitative data. [18] Coding categories were developed through an open, iterative process that involved reading the interviews with a focus that included physical and emotional effects of NC. From this process, a master code list of categories was developed. These codes were refined with inclusion and exclusion criteria, and then applied to the transcribed interviews. Two analysts [KW and MH], the qualitative expert [SZ], and the study team discussed the coding categories (e.g. coping) and worked to integrate the codes into the larger analysis.
Primary coding was completed on all transcripts, and secondary coding was completed on 25% of the transcripts. Cohen’s Kappa statistics19 were then calculated on each code to determine inter-coder reliability. A mean Kappa score of 0.71 was obtained, indicating substantial agreement. [19] Discrepancies in coding between the analysts were resolved via discussion and then recorded in a final dataset for use in the analysis. Coded passages were then examined to better understand patients’ views and perspectives. The software program Atlas.ti (Scientific Software, Berlin, Germany) was used to assist in data organization and management. Quotations were chosen based on representativeness and their capacity to convey common participant views and themes.
Results
Participant characteristics

Table 1

Table 2

Table 3 A total of 28 participants agreed to participate in a phone interview and complete a questionnaire. Table 1 describes the characteristics of the participants. Sixteen were recruited from a non-surgical clinic and 12 from a surgical clinic. The majority of participants (82%) were between 60 and 79 years of age, 54% were female, 68% were retired and over 80% received post-secondary education. Most participants reported that their dominant symptoms involved chiefly the leg(s) (57%) or their back and leg(s) equally (32%). Almost half of the participants had symptoms for more than five years and over 75% experienced symptoms within 30 minutes of commencing walking. Participants from the surgical clinic appeared to have greater functional limitations and longer duration of symptoms compared to participants from the non-surgical clinic (see Table 2).
Major themes from interviews: Participants’ experiences with LSS (see Quotes Table 3)
Physical effects: The most commonly reported symptoms were pain and discomfort; mentioned by each of the 28 participants. The location of the pain varied but included lower back pain and leg pain. Other reported discomforts included: tingling, leg and knee failure (i.e. sudden inability to stand, sit or walk, including falling), burning, a sensation of something crawling just under the skin (i.e. paresthesia), and a sensation of fullness or heaviness in the legs (Table 3: Theme 1 Quotes A.1–3). Problems with fatigue centred on the legs or other body parts tiring quickly such that walking for long distances or, in the case of a school teacher, standing at work all day became impossible (Table 3: 1 A.4–5).
While a few participants did not describe their pain from stenosis as particularly intense, most regarded their pain as debilitating. One described it as “pure hell.” For some participants the pain had always been intense, whereas for others it had gradually increased to the point of causing debilitation (Table 3: 1 A.6). In addition to concerns about the severity of their pain, participants described the emotional impact of the wearing, grinding nature of having to endure ongoing pain, including feelings of resentment (Table 3: 1 A.7).Activity effects: Participants mentioned a wide range of activities that their NC interfered with including: walking, recreational activities (such as sports and exercise), standing, social activities, household activities, controlling comorbid health conditions, working, sleeping and lifting.
Each participant mentioned that their NC interfered with their ability to walk. Interference with walking was most frequently mentioned as the “most bothersome” aspect of the condition, identified as such by 17 of the 28 participants. For some participants this was a minor concern or one that had affected them profoundly in the past but with successful treatment was no longer an issue. For many however, the walking limitations caused major disruptions in their lives, from being unable to walk or run for exercise, to being unable to do basic social and daily activities such as grocery shopping, holiday shopping, going to the mall with family and friends, or even visiting neighbors (Table 3: 2 A.1–3). Related to walking, many participants described being unable to participate in recreational activities. Recreational activities mentioned included walking itself or hiking, various sports (football, cricket, soccer, golf, badminton, curling, snowshoeing, cross-country skiing, squash), travel (due to the walking that travel entails), dancing, bicycling, and aerobics (Table 3: 2 B. 1–3). Many participants described themselves as active, outdoorsy people who, as a result of their NC, had become sedentary and were unable to participate in what had been previously seasonal outdoor activities (Table 3: 2 B.4). Inability to participate in recreational activities was mentioned as the “most bothersome” aspect of having LSS by 11 of the 28 participants.
Interference with social activities was mentioned fairly often, and was linked to participants’ difficulties with walking, standing, or doing recreational activities. Many described limiting time with family and friends, difficulties standing while socializing or being unable to play with grandchildren in the way that they wanted (Table 3: 2 C.1–3). Often the inability to stand or pain upon standing was linked with an inability to do household/daily activities, such as cleaning or other chores, in the way that the participants were used to doing. For many there was difficulty with transitioning between positions or activities, describing not being able to walk immediately after standing for example, or having extreme difficulty sitting and standing back up. This difficulty in transitioning made a wide range of activities difficult or impossible, from social events to using the toilet.
For some participants, the amount of pain experienced while standing meant that they could not wait in lines, go shopping without physical support such as a shopping cart or another person, clean their households, cook, or even stand in the bathroom to do their hair or makeup in the morning (Table 3: 2 C.4–8). This directly impacted individuals’ sense of independence, and for some, eliminated activities that they had previously found enjoyable, such as cooking or gardening (Table 3: 2 C.4).Emotional effects: In addition to their physical symptoms, participants reported an array of emotional responses to their condition. Twenty-two of the 28 participants reported emotional impacts that were associated with their NC. The most frequent of these was depressed mood, although not always specified by name. Instead they described their feelings as sadness, loss of interest in activities, or hopelessness (Table 3: 3 A.1). These participants were likely to mention deep feelings of sadness, discouragement, social isolation or loss, as their NC prevented them from doing activities that they enjoyed (i.e., walking or other outdoor activities) or from which they derived meaning (i.e., work, volunteer work, being independent, socializing, lifting and holding grandchildren) (Table 3: 3 A.2–4). Additionally, for some of these participants, the perceived incurable/untreatable nature of NC was described as “depressing” in and of itself.
Eight of the participants mentioned anxiety, expressing deep worries that family members would have to take care of them, or that their condition would worsen significantly (Table 3: 3 B.1–2). Seven participants expressed feelings of frustration with their NC (Table 3: 3 C.1–2). For some, this was focused on the physical limitations imposed on them by NC, such as only being able to walk for short distances or the ongoing relationship between exercise and pain relief.
Lastly, six of the participants described NC as having hurt their pride. Most of these participants mentioned in passing feeling embarrassed at having to rest frequently, or lamented the loss of complete independence (Table 3: 3 D.1). One participant had concerns about loss of independence that were so severe that he spoke favourably of assisted suicide. Similarly, another participant spoke of the embarrassment of dealing with NC in social situations, describing the limitations that always having to sit at parties imposed on her, and describing NC as having pushed her into an older, different phase of life (Table 3: 3 D.2).Treatment effects, non-surgical: Participants had experienced a wide array of treatments for their NC. The most common treatments were manual therapy and supervised exercise (rehab therapy), and pain medication (see Table 2). Of the two, rehab therapy was spoken of more favourably. Rehab therapy was described as significantly to relieving pain and increasing mobility. For some participants, it provided complete relief, although that relief was contingent upon continuing the therapy. Some participants noted that the frequency with which one had to do the therapeutic exercises was sometimes frustrating (Table 3: 5 A.1). For others, however, while rehab therapy did not provide complete relief, it reduced pain or discomfort in ways that were meaningful, such as allowing them to sleep at night, or increasing the distance they could walk at one time from under 100 metres to one kilometre. Others mentioned that rehab therapy could provide temporary relief, interspersed with some relapses (Table 3: 5 A.2). More participants found it efficacious than those who did not, and some found that it completely relieved their symptoms.
Treatment effects, surgical: Seven participants had undergone surgery for their NC, four of whom directly praised the surgery as effective (Table 3: 5 B.1). Two participants found that their surgeries were initially successful but that over time, their symptoms were beginning to return. Another two participants found their surgeries to be helpful, but had them so recently that they weren’t sure what level of function they would ultimately achieve in the longer term.
Expectations from treatments: When it came to the relief that participants expected from their treatment, the most frequently mentioned expectations were decreased/eliminated pain and increased physical abilities. Overall, the majority of participants (n=20/28) felt that treatment would have to improve (rather than simply maintain) their condition in order to be worthwhile.
(i) Pain relief: Many participants expected and accepted that they would live with some level of chronic pain. Those who expected to live in pain frequently indicated that simply being in less pain would be adequate for them, and that any amount by which it could be lessened would be beneficial. They described themselves as going through life by just dealing with it (Table 3: 6 A.1). For example, one participant called her desire to be without pain “greedy,” and described pain as her “partner in life.” Two others indicated that if 10 were the worst pain possible, they would be willing to live at a constant two. Another participant indicated that a five out of 10 would be acceptable. These participants seemed aware and accepting of the fact that they would never be completely pain free (Table 3: 6 A.2)
Rarely, participants expected complete and total relief of their symptoms, and expressed a desire to have no pain whatsoever (Table 3: 6 B.1). It seemed that participants expected more in terms of absolute pain relief from surgery than they did from other interventions, such as rehab therapy, although relatively few participants spoke about this issue (Table 3: 6 B.2).
(ii) Physical abilities: Relief from pain overwhelmingly appeared to be the single most important thing that could be done for these NC sufferers. However given that decreased pain should lead to increased physical ability, these two outcomes generally go hand-in-hand.
When participants spoke about increased mobility, they generally did not expect 100% recovery but rather would set an individual benchmark, which generally meant being able to do “more” than they currently could do. Benchmarks included: being able to walk a greater distance, being able to handle household chores alone, being able to transition from sitting to standing without pain, being able to perform activities like playing with grandchildren, or being able to “get out of vehicles” (Table 3: 6 C.1–3). Echoing the data discussed earlier about activities impacted by LSS, the most commonly mentioned activity in this area was walking: participants strongly want to be able to walk without pain (Table 3: 6 C.4).
Discussion
In this study we interviewed 28 individuals with NC due to LSS with the goals of better understanding how this condition impacts their lives and what they expected from non-surgical and surgical treatments. This study uniquely confirms that from the perspectives of patients, NC has a multidimensional impact on individuals with pain, limited walking ability, and depressed mood arising as the most common and significant symptoms. Most participants had undergone multiple treatments for their NC, many of which they found to be ineffective. The most effective treatments were rehab therapy/exercise and surgery. Pain medication was also frequently used but participants generally indicated that they wanted to reduce or eliminate use of medications. Patients felt that treatment would have to improve (rather than simply maintain) their condition in order to be worthwhile. Finally, a consistent theme arose amongst participants suggesting that pain, physical abilities, emotional state, and their expectations of treatment are strongly inter-related and at times inseparable.
By far our participants were most bothered by the pain associated with NC. Described pain ranged from somewhat mild and well controlled to absolutely crippling and debilitating. For most participants, the pain from their NC had dramatically impacted their lives; the impact of which cannot be overstated. Beyond the experience of pain itself, participants regularly expressed the desire to re-engage in their regular day-to-day, recreational and social activities. The activity most frequently mentioned, and the source of the most frustration, was the inability to walk and/or stand. In a study using focus groups to assess important outcomes among 33 older patients receiving epidural injections for NC, Edward et al. [20] had similar findings. In their study the highest rated problem areas were “experiencing pain/discomfort” (88% of participants), “problems with physical function” (85%), “difficulty exercising” (73%), “difficulty participating in hobbies and leisure activities” (55%), and “problems with weakness” (52%). [20]
In a recent qualitative study by Lyle et al. [21] assessing 15 patients undergoing physiotherapy for NC, pain and the threat of pain was the most prominent feature leading to a loss of engagement in meaningful activities and sense of self. Similarly in our study the majority of patients perceived pain as the central cause of their other symptoms, with relief from pain overwhelmingly being the single most important thing that could be done for them. This finding was also prominent in the study by Lyle et al. [21], where most participants wished to get rid of the pain completely as they felt that was key to getting back to their normal activities. While others implied complete relief was unlikely and they would be happy if they could get relief of some of the pain. In our study participants hoped for their pain levels to decrease and walking to return to the levels that they were capable of prior to their symptoms arising. However, the majority of participants were willing to accept any achievable improvement over their current symptoms.
Perhaps the most surprising finding was how frequently participants reported various emotional effects that resulted from living with NC. The most common was an expression of depressed mood. In addition to depressed mood, participants mentioned experiencing anxiety (i.e., fear that it would become worse or that they would be debilitated), frustration and hurt pride (i.e., hurt pride at having to be taken care of or being viewed as disabled or unattractive) as a result of their NC. In the study by Lyle et al. [21], the authors noted fluctuating and unpredictable symptoms resulted in anxiety and uncertainty, however, they did not report depressed mood as a prevalent theme. Although we did not specifically ask about treatment for psychological illness in our interviews, it is worth noting that patients did not report receiving treatment for their mood alteration. The apparent emotional (psychosocial) impact of NC on patients suggests that these factors should be considered during assessment and management not unlike patients who suffer from chronic pain. Current diagnostic criteria for neurogenic claudication due to degenerative lumbar spinal stenosis do not include psychosocial factors. [2, 29]
Our findings strongly suggest that the emotional aspects of NC, particularly given the high prevalence of depressed mood, need to be considered and that treatment for depression and/or anxiety is possibly an unmet need in this population. Specifically, the emotional effects of NC may be important mediators of pain intensity, and/or related to limitations in walking and standing ability, and recreational activity. Emotional effects may also explain why there is a lack of correlation between decreased pain or disability scores and improved walking ability. [12] It is also possible that the emotional effects may explain why patients’ symptoms and functional status are variable, as noted in the Lyle et al. [21] study and concurs with recent clinical trial data (Ammendolia et al. and Schneider et al., unpublished data). These results are consistent with the literature on psychosocial impacts of NC. Studies have shown that high levels of depression and hopelessness may have a compounding effect on walking ability and recreational activity in individuals with NC, as well as surgical outcomes. [22] A systematic review of prognostic factors in NC showed that pre-operative depression is likely a prognostic factor for post-operative NC related symptom severity and disability. However, the prognostic value of depression on the outcome of pain and walking capacity was less clear. [22] Therefore, interventions directed at addressing psychosocial issues associated with NC might improve pain levels and functional activity through better coping mechanisms. [22, 23]
For the most part participants’ expectations for treatment seemed realistic, likely in part because most received education on what they could expect from treatment by their practitioners (CA, RR). Patient expectations are known to impact outcomes24,25 and the ability to mitigate unrealistic expectations prior to treatment would likely reduce the risk of disappointment and despair, as well as facilitate the acceptance of some degree of pain and physical limitation. In this study, patient expectations for improvement appeared higher for surgery than non-surgical treatment. This suggests that the minimally clinically important difference (MCID) may be different between patients in these two groups. This has been demonstrated in quantitative studies evaluating the MCID for the Spinal Stenosis Survey and Oswestry Disability Index. [26, 27] This may have implications in clinical trials when comparing the proportion of participants achieving MCID among subjects receiving surgery and those receiving non-surgical treatment for NC.
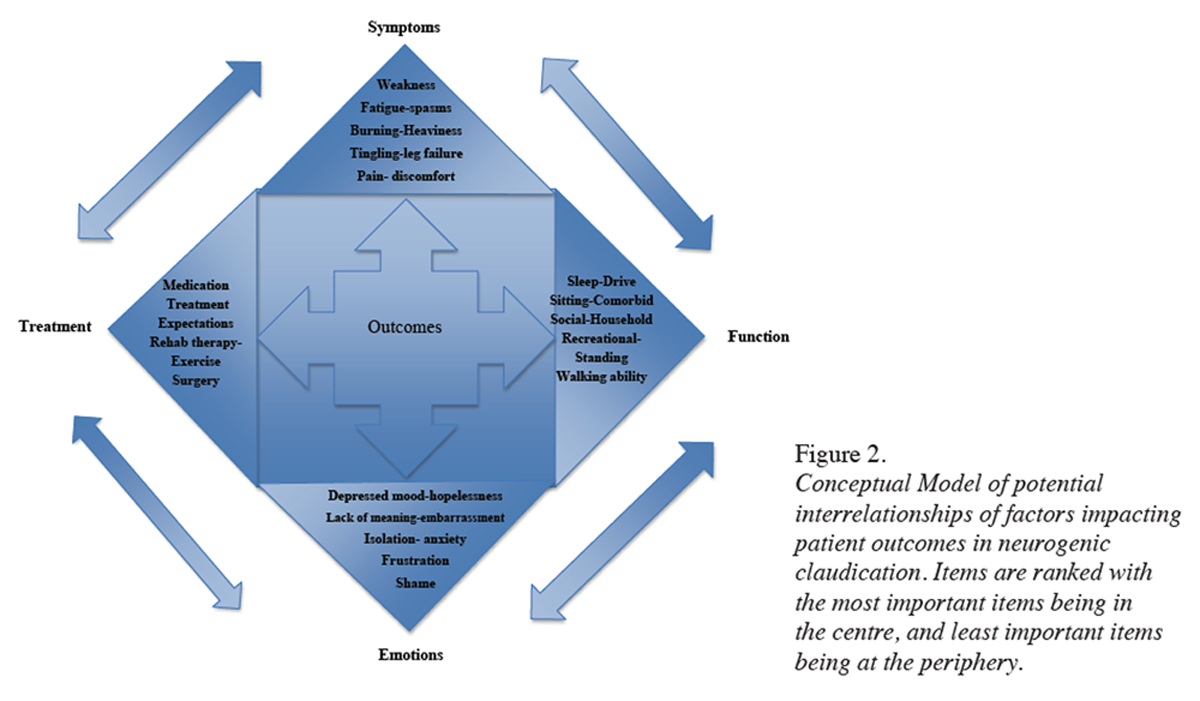
Figure 2 Based on our patient-centred findings, we propose that both clinicians and researchers need to address NC as a multidimensional entity when considering management options and designing or evaluating specific intervention(s). We have proposed a theoretical framework to illustrate the potential inter-relationships of factors that impacts patient outcomes in NC (Figure 2). In this framework we ranked, based on our participants’ experiences, the most bothersome symptoms, functional limitations, emotional aspects and treatment successes and hypothesized how these factors potentially interact. Patients who are depressed are not likely good surgical candidates, and this is an example of how psychosocial factors can impact treatment decisions. Treatment outcomes can change the direction of future treatment is another potential interaction. This framework can provide a guide to clinicians to establish how NC individually affects their patients and to inquire about their treatment expectations. This can allow for a more stratified approach to management ranging from rehabilitation therapy, psychosocial support and /or surgery that may lead to better individual patient outcomes. Future research is needed to validate and quantify these proposed interactions between pain, physical ability, emotional state and treatment expectations in NC.
Future studies should address and measure priority areas including pain, walking and standing ability, recreational and social activity and emotional well being. In a Cochrane review examining non-operative interventions to improve outcomes in symptomatic LSS, none of the 21 studies reviewed directly assessed recreational activity, while only seven of 21 studies assessed psychosocial status, and 12 of 21 studies used an objective walking measure. [12] This paper provides valuable insight from a patient’s perspective and this information can influence how we treat LSS patients in future and how we select outcomes for research.
Study limitations
Our study is not without limitations. Our qualitative approach is not designed to be generalizable, but instead to provide depth and insight into patients’ lived experience. For that reason we sought to achieve thematic saturation per group, which can be achieved with 10–12 interviews per group. We were able to recruit additional subjects per group and in our thematic coding we noted saturation, which occurs when key themes such as physical limitations are present for all participants. However, it is still possible that if more patients were interviewed different themes may have emerged.
Another potential limitation is that our purposeful sample focused on a Canadian sample in a hospital setting. Variations in health care system characteristics and related factors such as access to treatment may impact patients’ outcomes and expectations. Recruiting from a hospital setting may result in participants with more severe symptoms and physical limitations. Although an attempt was made to recruit a representative sample of patients with NC due to LSS, it may be that the participating sample was not a true general reflection of this population. This selection bias may also be reflected in our conceptual model of factors that impact patient outcomes and their potential interactions. These hypothesized interactions should be determined quantitatively using a random representative sample.
Conclusions
The results of this qualitative study show that NC should be considered as multidimensional in its impact on patients. We found that pain, and limited walking and standing ability were the most bothersome aspects of NC that significantly impacted important activities of daily living, as well as meaningful recreational and social activities. Additionally, this study is the first to qualitatively identify the significant emotional impact of NC. This is a finding that should not be overlooked in clinical practice and future research. A holistic understanding of how psychosocial and other factors impact outcomes in this population is needed. We present a conceptual model of potential interactions between important outcomes in LSS as a framework for future study.
Acknowledgements
The following organizations have provided funding for this research: The Canadian Chiropractic Research Foundation (Ammendolia), NCMIC Foundation (Ammendolia and Schneider) and The Toronto General and Western Hospital Foundation (Rampersaud). Dr. Zickmund is supported by the VA Salt Lake City Medical Center and the Health Services Research & Development IDEAS 2.0 Center (Award number ISOHX001240).
Footnotes
The authors’ report no related conflict of interest. The following organizations have provided funding for this research: The Canadian Chiropractic Research Foundation (Ammendolia), NCMIC Foundation (Ammendolia and Schneider) and the Veterans Administration Health Services Research and Development Program, award number 5150HX001240 (Zickmund) and The Toronto General and Western Hospital Foundation (Rampersaud).
References:
Katz JN, Harris MB.
Clinical practice. Lumbar spinal stenosis.
N Engl J Med. 2008;358:818–825.Suri P, Rainville J, Kalichman L, Katz JN.
Does this older adult with lower extremity pain have
the clinical syndrome of lumbar spinal stenosis?
JAMA. 2010;304:2628–2636.Comer CM, Redmond AC, Bird HA, Conaghan PG.
Assessment and management of neurogenic claudication associated with
lumbar spinal stenosis in a UK primary care musculoskeletal service:
a survey of current practice among physiotherapists.
BMC Musculoskelet Disord. 2009;10:121.Kalichman L, Cole R, Kim DH, Li L, Suri P, Guermazi A, et al.
Spinal stenosis prevalence and association with symptoms: the Framingham Study.
Spine J. 2009;9:545–550.Deyo RA.
Treatment of lumbar spinal stenosis: a balancing act.
Spine J. 2010;10:625–627.Government of Canada .
Statistics Canada. Statistics Canada; Nov 6, 2006.
Government of Canada, accessed November 2, 2008 at:
www.statcan.gc.ca/bsolc/olc-cel/olccel?lang=eng&catno=11-008-XAmmendolia C, Stuber K, de Bruin LK, Furlan AD, Kennedy CA, Rampersaud YR.
Non-operative treatment for lumbar spinal stenosis
with neurogenic claudication: a systematic review.
Spine. 2012;37:E609–616.Kovacs FM, Urrútia G, Alarcón JD.
Surgery versus conservative treatment for symptomatic lumbar
spinal stenosis: a systematic review of randomized controlled trials.
Spine. 2011;36:E1335–1351.Moojen WA, Arts MP, Bartels RH, Jacobs WC, Peul WC.
Effectiveness of interspinous implant surgery in patients with intermittent
neurogenic claudication: a systematic review and meta-analysis.
Eur Spine J. 2011;20(10):1596–1606.Zaina F, Tomkins-Lane C, Carragee E, Negrini S.
Surgical versus nonsurgical treatment for lumbar spinal stenosis.
Spine. 2016;41:E857–868.Ammendolia C, Stuber KJ, Rok E, Rampersaud R, Kennedy CA, Pennick V.
Nonoperative treatment for lumbar spinal stenosis
with neurogenic claudication.
Cochrane Database Syst Rev. 2013;8:CD010712.Ammendolia C, Stuber K, Tomkins-Lane C, Schneider M, Rampersaud YR, Furlan AD, Kennedy CA.
What interventions improve walking ability in neurogenic
claudication with lumbar spinal stenosis?
A systematic review.
Eur Spine J. 2014;23:1282–1301.Coyne Imelda T.
Sampling in qualitative research. Purposeful and
theoretical sampling; merging or clear boundaries?
J Advanc Nurs. 1997;26:623–630.Jensen MP, Karoly P, Braver S.
The measurement of clinical pain intensity: a comparison of six methods.
Pain. 1986;27:117–126.Stucki G, Daltroy L, Liang MH, Lipson SJ, Fossel AH, Katz JN.
Measurement properties of a self-administered outcome measure
in lumbar spinal stenosis.
Spine. 1996;21:796–803.Fairbank JC, Couper J, Davies JB, O’Brien JP.
The Oswestry low back pain disability questionnaire.
Physiother. 1980;66:271–273.Ruta DA, Garratt AM, Russell IT.
Patient centred assessment of quality of life for patients with four common conditions.
Qual Health Care. 1999;8(1):22–29.Crabtree BF, Miller WL.
Doing Qualitative Research: Multiple Strategies.
Thousand Oaks: Sage Publications; 1992.Landis JR, Koch GG.
The measurement of observer agreement for categorical data.
Biometrics. 1997;33:159–174.Edwards TC, Lavallee DC, Bauer Z, Comstock BA, Jarvik JG, Patrick DL.
Problem areas identified as important to older adults with lumbar spinal stenosis.
Spine J. 2015;15:1636–1644.Lyle S, Williamson E, Darton F, Griffiths F, Lamb SE.
A qualitative study of older people’s experience of living with neurogenic
claudication to inform the development of a physiotherapy intervention.
Disabil Rehabil. 2016;23:1–9.McKillop AB, Carroll LJ, Battié MC.
Depression as a prognostic factor of lumbar spinal stenosis: a systematic review.
Spine J. 2014;14:837–846.Tomkins-Lane CC, Lafave LM, Parnell JA, Rempel J, Moriartey S, Andreas Y.
The spinal stenosis pedometer and nutrition lifestyle intervention (SSPANLI):
development and pilot.
Spine J. 2015;15:577–586.Saban KL, Penckofer SM.
Patient expectations of quality of life following lumbar spinal surgery.
J Neurosci Nurs. 2007;39:180–189.Gepstein R, Arinzon Z, Adunsky A, Folman Y.
Decompression surgery for lumbar spinal stenosis in the elderly:
preoperative expectations and postoperative satisfaction.
Spinal Cord. 2006;44:427–431.Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY.
Minimum clinically important difference in lumbar spine surgery patients:
a choice of methods using the Oswestry Disability Index,
Medical Outcomes Study questionnaire Short Form 36,
and pain scales.
Spine J. 2008;8:968–974.Cleland JA, Whitman JM, Houser JL, Wainner RS, Childs JD.
Psychometric properties of selected tests in patients with lumbar spinal stenosis.
Spine J. 2012;12:921–931.Conway J, Tomkins C, Haig A.
Walking assessment in people with lumbar spinal stenosis:
capacity, performance, and self-report measures.
Spine J. 2011;11(9):816–823.Tomkins-Lane C, Melloh M, Lurie J, Smuck M, Battié MC, Freeman B, et al.
ISSLS Prize Winner: Consensus on the Clinical Diagnosis of Lumbar
Spinal Stenosis: Results of an International Delphi Study. Spine.
2016;41(15):1239–1246.
Return to LOW BACK PAIN
Return to SPINAL STENOSIS
Since 1-04-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |