

Treatment Targets of Exercise for Persistent
Non-specific Low Back Pain: A Consensus StudyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Physiotherapy 2021 (Sep); 112: 78–86 ~ FULL TEXT
OPEN ACCESS Lianne Wood, Annette Bishop, Martyn Lewis, Rob J E M Smeets, Gert Bronfort, Jill A Hayden, Nadine E Foster
Primary Care Centre Versus Arthritis,
School of Primary, Community and Social Care,
Faculty of Medicine and Health Sciences,
Keele University,
Newcastle-under-Lyme ST5 5BG, UK

Objectives: Despite several hundred previous randomised controlled trials (RCTs), the key treatment targets of exercise for persistent non-specific low back pain (NSLBP) remain unclear. This study aimed to generate consensus about the key treatment targets of exercise interventions for patients with NSLBP.
Design: Consensus was generated using modified nominal group technique in two, sequential, workshops. The results of a previous systematic review informed the first, national, workshop idea generation and the results of this workshop informed the second, international, workshop. The authors generated a starting list of 30 treatment targets from the systematic review. A pre-specified consensus threshold of 75% was used in the voting stage.
Participants: Workshop participants included people with experience of using exercise to manage their persistent NSLBP, clinicians who prescribe exercise for persistent NSLBP, and researchers who design and evaluate exercise interventions in RCTs. All participants generated, voted and ranked the treatment targets in each workshop using an online platform.
Results: A total of 39 participants contributed to the consensus (15 in the national workshop and 24 in the international workshop), comprising two people with NSLBP, six clinicians and 31 researchers/clinicians. A total of 40 exercise treatment targets were generated, and 25 were retained after voting and ranking. The prioritised targets of exercise for persistent NSLBP were: improving function, improving quality of life, reducing pain, meeting patient-specific goals and reducing fear of movement.
Conclusions: Future RCTs of exercise should specify the targets of their exercise intervention and consider assessing these treatment targets as well as including mediation analyses.
Keywords: Consensus workshop; Exercise; Low back pain; Treatment targets.
There are more articles like this @ our:
EXERCISE AND CHIROPRACTIC Page
From the FULL TEXT Article:
Introduction
Exercise is a core recommended treatment for persistent non-specific low back pain (NSLBP) [1-3], although no single approach to exercise is consistently superior over others. [4, 5] There is strong evidence that exercise has moderate benefits for pain and function in the short-term. [6-8] Exercise is a subgroup of physical activity, which is planned, repeated, structured and intends to improve one’s physical fitness. [9] Regular and adequate levels of physical activity have significant health benefits at all ages: improving muscular and cardiorespiratory fitness, bone and functional health; preventing falls and depression; improving general cardiovascular health; and maintaining energy levels and weight control. [9] Exercise may reduce the severity of chronic pain as well, and lead more generally to improved overall physical and mental health, and physical functioning. [10] However, the biological targets and mechanisms of action of exercise in persistent NSLBP are not fully understood nor yet agreed within the clinical and research community of NSLBP. [11] A treatment target should reflect the aims and or goals of the intervention(s) [12], but in the field of persistent NSLBP, the treatment targets of exercise are poorly defined compared to other fields of healthcare such as coronary heart disease [13, 14], and diabetes. [15, 16]
A recent systematic review [17] identified numerous direct and indirect treatment targets from published trials of exercise for persistent NSLBP. Only 67% of included trials specified a clear rationale for their exercise intervention, while 22% indirectly inferred treatment targets from the language used to describe the rationale for the exercise interventions. However, there was considerable heterogeneity between exercise types and treatment targets identified, confirming a lack of consensus about the treatment targets of exercise for persistent NSLBP. The most frequently reported treatment targets were reducing pain (nine trials), improving spinal stabilisation (eight trials) and muscle strengthening (eight trials). [17] Furthermore, even trials that evaluated similar exercise approaches, for example, the McKenzie approach [18, 19], described different treatment targets. This study aimed to generate consensus among major stakeholders about the key treatment targets of exercise interventions for patients with persistent NSLBP.
Methods
Design
Consensus was generated using modified nominal group technique in two, sequential, workshops as part of an exploratory study. The nominal group methodology was selected as it has previously been successfully used when incorporating both researchers, clinicians and patients, and ensures that the voices of all participants are heard and included. [20] Each workshop moved through five stages: introduction, idea generation, idea sharing, group discussion, voting and ranking [21], modified for each of two workshops in this study. The finalranking stage provided consensus as an aggregation of the participants’ views rather than a communal viewpoint. [22] Ethical approval was obtained from the University Research Ethics committee for both workshops.
Participants
This study included people with lived experience of using exercise to manage their persistent NSLBP, clinicians who prescribe exercise for persistent NSLBP, and researchers who design and evaluate exercise interventions for NSLBP in trials. The authors set a limit of 25 participants per workshop to ensure manageable group discussion and input as part of the workshop process. [23] The first, national, workshop (October 2018) targeted clinicians (predominantly physiotherapists), people who had used exercise, and researchers(as described above) by using advertisements, telephone calls, targeted emails, social media, and contact with local patient groups for arthritis and back pain. Despite extensive advertisement,few people with a lived experience of using exercise for NSLBP enquired for thisstudy. The second, international, workshop was held as part of an international conference (June 2019):The International Forum for Back and Neck Pain Research in Primary Care, held in Quebec City, Canada. This workshop targeted researchers who may or may not also be clinicians.
Workshop process
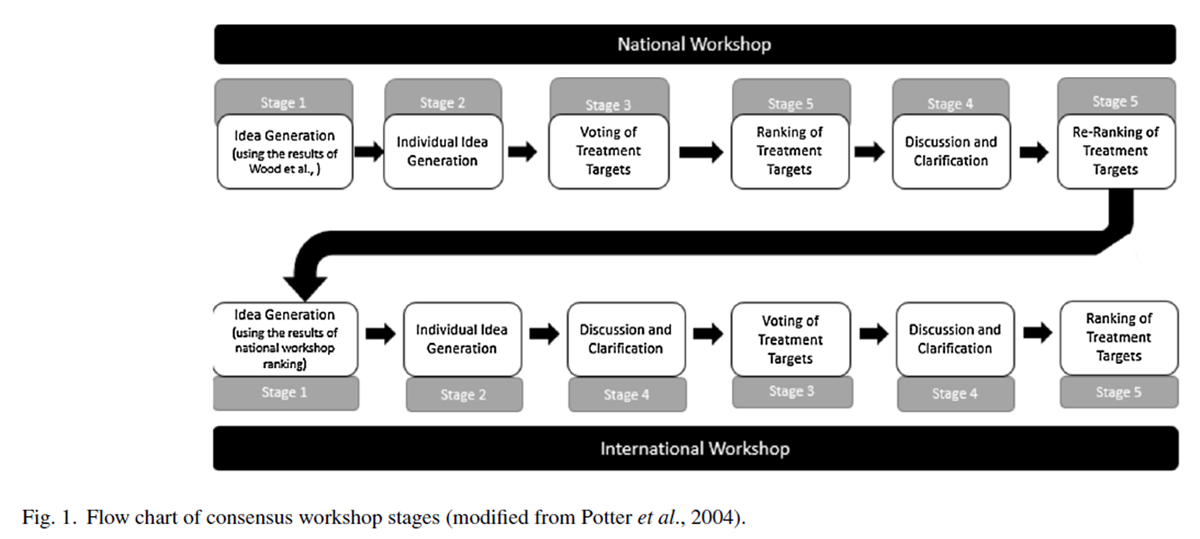
Figure 1 Both workshops began with silent idea generation. The national workshop was informed by a systematic literature review [17], and the results of the national workshop informed the international workshop. Figure 1 summarises the study process, and each of the stages is outlined below. During the workshop processes, the stages were not always completed sequentially, as portrayed in Fig. 1 with order delineated by the stage number above each workshop process.
National workshop
Pre-workshop (stages 1 and 2)
Participants provided informed consent and baseline demographic information online on registering for the workshop. Before the workshop, access to the online portal was provided through GroupMap to view the list of pre-generated treatment targets. Participants were able to add to this, as desired, prior to the workshop. Participants’ additions were private to the rest of the group until the workshop. Idea generation items that were similar were merged by the research team to avoid duplication, and a total list of all potential treatment targets generated was created at the end of this process.
Within workshop (stages 3–5)
Participants were able to participate virtually through the use of Skype (SkypeCommunications S.a r.l.) or face-to-face. All participants in the workshop brought a mobile device to engage with the online platform during the workshop. The workshop took two hours. The results of the idea generation stage were visually displayed to all participants, with the opportunity to add any omitted items to the list, and for discussion ofitems displayed. Due to the range of participants and the number of additional constructs added in the second stage, discussion of the individual potential treatment targets was delayed until after the voting and ranking had reduced the number of targets.
Participants then privately voted (yes/no) for their ten most important treatment targets (stage 3) using the online platform. The potential treatment targets that obtained at least one vote were carried through to the next stage and were presented to the group via the online platform. No thresholds for consensus were used within this workshop as it was the first stage in an exploratory study. Items were then individually ranked in order of importance through an online ranking process (stage 5) where participants allocated ten points to their most important treatment target, descending to one point for the least important.
The results of this ranking process were discussed within the workshop (stage 4): treatment targets were discarded, grouped and amended as required through discussion and verbal agreement from the workshop participants. A further ranking stage was undertaken online two weeks after the workshop due to the delayed discussion and clarification stage.
International workshop
Pre-workshop (stages 1 and 2)
Before the workshop, registered attendees provided informed consent and baseline demographic information. They were also supplied with a list of the final ranked treatment targets from the national workshop and asked to add any other potential treatment targets. Google sheets was used to develop these online forms.
Within workshop (stages 3–5)
The results of the idea generation were presented to the workshop participants visually, allowing the opportunity for potential treatment targets of a similar construct to be clarified and grouped, discarded or amended as agreed by the group. Voting (stage 3), occurred individually on a document developed on Google Sheets; participants were able to vote for any number of itemsthey felt to be potential treatment targets (yes/no).
In the voting stage, a pre-specified consensus threshold of 75% wasset for items where 75% of participants agreed that the item was not a treatment target of exercise. [24] These treatment targets were excluded from future voting and ranking rounds. All targets meeting the pre-specified consensusthreshold were carried through to the nextstage for ranking. There was then further discussion and clarification (stage 4) before participants individually ranked the treatment targets in order of priority (stage 5).
Ranking occurred in order of importance from one to ten and amended to reflect the same scaling as in the national workshop (i.e. the greatest score has the most importance). The results were then presented to the participants of the workshop, who agreed with the order of importance of treatment targets, and declined the opportunity to re-rank treatment targets. These were then grouped into functional (relating to physical function), psychosocial (including psychological and social), behavioural (for example health service use) and impairment-based (such as strength or flexibility) targets. [25]
Results
Participants
A total of 39 participants contributed to the consensus workshops (15 in the national workshop and 24 in the inter-national workshop). A total of 32 participants completed all stages of each workshop (12 in the national workshop, and 20 in the international workshop). Participants of the two workshops were from ten different countries (UK, Canada, Brazil, USA, Australia, Denmark, Finland, Norway, Sweden, Netherlands). Ninety percent of participants had experienced NSLBP at some point in their lives. Demographic information is summarised in Table 1 below for 36 of the 39 participants. Three participants in the national workshop were unable to take part in the workshop but completed the pre-workshop idea generation and post-workshop ranking. Only 21 participants provided baseline demographic data in the international workshop due to the nature of the conference environment.
National workshop results
Idea generation (stage 1–2)
Fifteen participants completed the pre-meeting idea generation for the workshop. A further 25 treatment targets were added to the original list of 30 targets (informed by the previous systematic review [17]), creating a total list of 55 treatment targets (see Appendix 1 in supplementary material).
Voting of treatment targets (stages 3)
Discussion and clarification of the potential treatment targets were delayed until after the ranking stage (stage 5). Twelve participants voted for their ten most important potential treatment targets. At least half of the participants voted for‘reducing pain’ (66.7%), reducing fear of movement (50%) and increasing functional capacity (50%). Only 43 potential targets received votes and were carried through to the next stage, as seen in Appendix 2 in supplementary material.
Ranking and discussion of treatment targets (stage 4 and 5)
As the grouping stage had not been performed adequately in stage 4, significant overlap remained across treatment targets during the ranking stage (e.g. most important was reduce pain, second most important was reduce back pain). Three constructs were removed. Grouping of targets was performed, with an average of 2.4 (range 1–7) linked targets to a potential treatment target. This reduced the list of treatment targets from 43 to 18 (see Appendix 3 in supplementary material). For example, “increase physical function” was grouped with “reduce disability” and “increase functional capacity”. Re-ranking of the 18 potential treatment targets was then performed online two weeks after the workshop with all participants who initially consented to participation (n = 15) with the final ranking results summarised in Table 2.
International workshop results
Idea generation (stages 1–2)
Twenty-one participants completed the pre-meeting idea generation for this workshop and added a further 15 targets to the original list of 18 treatment targets (Appendix 4 in supplementary material).
Voting of treatment targets (stages 3–4)
A total of 24 participants voted for treatment targets from the list of 33 potential treatment targets. The potential treatment targets that received the most votes were ‘reducing fear of movement’ (92%), ‘increasing function’ (87%), ‘improving self-efficacy’ (87%), ‘reducing anxiety and depression’(87%) and ‘improving quality of life’ (87%). No potential treatment targets met the pre-specified criteria for exclusion. Potential treatment targets of a similar construct were clarified and grouped, discarded or amended as agreed by consensus of the group. Six items were removed during this stage, including ‘general health and well-being’ which was grouped within ‘improved quality of life’.
Ranking of treatment targets (stage 5)
Twenty-five of twenty-seven treatment targets received sufficient votes for prioritisation. Twenty participants ranked the final list of prioritised treatment targets, as displayed in Table 3. Four psychological constructs were prioritised, three functional constructs and one impairment construct, as well as reducing pain and improving quality of life were included in the top ten. Participants declined the opportunity to perform a further ranking.
Discussion
Principal findings
With 39 participants from ten countries, this consensus study found that1) increasing functional ability,
2) improving quality of life,
3) reducing pain,
4) patient-specific targetsand
5) reducing fear of movement,were the most important treatment targets of exercise interventions for patients with persistent NSLBP. The two sequential workshops generated consensus from people with lived experience of NSLBP, clinicians and researchers involved in developing exercise interventions in clinical practice and in trials of persistent NSLBP. From an initial list of 30 treatment targets informed by a systematic review [17], participants ranked a final list of 27 treatment targets. Psychosocial constructs (40%) and functional constructs (30%) were prioritised in the top tentreatment targets.
Consideration of the findings in relation to other studies
This study is the first, to our knowledge, to develop consensus about the treatment targets of exercise for persistent NSLBP with key stakeholders involved in developing, delivering and participating in exercise interventions. The results are similar to the treatment targets of exercise for persistent NSLBP suggested by Rainville et al. [25] (addressing functional impairments, reducing pain and back pain-related disability). However, in a recent systematic review [17], the most frequently reported treatment targets identified by trials of exercise in persistent NSLBP were reducing pain, improving strength and spinal stabilisation. Of those, only pain reduction was prioritised as a treatment target in this consensus study, while improving strength was ranked 19 out of 27, and improving motor control (incorporating spinal stabilisation) was ranked 21 out of 27. This demonstrates a potential shift in contemporary understanding of how exercise may work to reduce NSLBP, and improve function and quality of life.
The psychological constructs of reducing fear of movement, improving self-efficacy, and reducing anxiety and depression were voted for by many participants in the final workshop (91%, 87%, 87%, respectively). However, reducing anxiety and depression was not voted to be in the top ten priorities, despite the evidence for exercise in treating depressive symptoms. [27] Both reducing fear of movement and self-efficacy have been shown to partially mediate the relationship between pain and disability in persistent NSLBP. [28, 29]
Recent research on the mechanisms of exercise for chronic musculoskeletal pain suggests reducing fear of movement, improving self-efficacy (both in the final top ten treatment targets), enhancing self-management and improving beliefs, cognitions and attitudes, may explain how painful exercises provide benefit. [30]
The psychological benefits of exercise are well-documented [31, 32] so the prioritisation of psychological targets by our workshop participants over other performance targets is perhaps not surprising. As the aetiology of persistent NSLBP is increasingly understood to comprise psychological, biomedical and social components [33], the emphasis placed on the psychological targets of exercise for persistent NSLBP seems to make sense. Increasingly, trials are including mediation analyses of these and other psychological constructs to establish whether these treatment targets lie on the causal pathway between the exercise treatment and the outcomes most important to patients (most commonly pain and disability. [34-39]
A mediator is a variable which explains how a treatment may work. [35] In certain situations, treatment targets may be the same as or similar to surrogate markers, or intermediate variables (mediators), whereas, in other situations, treatment targets may have more direct effects on outcomes. These terms (treatment targets and mediators) are conceptually different, yet they are terms that are sometimes used inter-changeably.
It is unknown whether treatment targets have an indirect effect on the causal pathway, similar to the action of a mediator [40], as demonstrated in Fig. 2. For example, increasing functional ability can be reached by decreasing fear of movement. So, in fact, a treatment could be targeted at reducing fear of movement, but the overall aim could be improving function. [41]
Distinguishing intermediate targets and final outcomes will also help the exercise and back pain community to better define treatment targets. This will inform how the exercise intervention should be developed and specified, and how the impact of the exercise intervention should be measured (for example, by using terms such as mediating factors and final outcome(s)). It may be that participants in the workshops in this study prioritised treatment targets that they were familiar with (such as reducing pain, increasing function and quality of life, comprising the recommended core outcome set in this field) rather than considering the likely mechanisms of effect for exercise.
Reducing pain, improving function and quality of life are well-established as important core outcome domains, and are the most commonly reported primary outcomes in RCTs of persistent NSLBP. [42, 43] When comparing these results, it can be seen that these are the same variables providing evidence that the most important treatment targets of exercise may be those prioritised by the core outcome domains. This suggests that the uptake and acceptance of the core outcome domains by both clinicians and researchers has been widespread, and remain a high priority for people with NSLBP, but their role as treatment targets (or mediators) of exercise interventions remains unclear.
Strengths and limitations
This consensus study is the first to our knowledge to develop a consensus about the treatment targets for exercise interventions in persistent NSLBP with key stakeholders involved in the use of, development, evaluation and prescription of exercise interventions. Other research on this topic has not included stakeholders. [25] The use of two sequential workshops allowed refinement of the potential treatment targets, informed by a recent systematic review, with both national and international nominal group workshops. Con-sensus was generated with numerous stakeholders, including people with lived experience of using exercise to manage persistent NSLBP, clinicians prescribing exercise for persistent NSLBP, and researchers who design and evaluate exercise interventions in RCTs.
However, this consensus study included only two people with lived experience of persistent NSLBP due to lack of response, but most included researchers and clinicians had themselves experienced backpain. Although the national and international workshop included a sample of clinicians and researchers from across the world, this remains a small sample (n = 39), and the results may not be representative of the wider, lower to middle income international community. Further, the majority of the included clinicians were physiotherapists, which may be representative of the breadth of clinicians who use exercise. The results obtained may have been different had this workshop been held in a different conference environment with a more clinical focus.
Implications for future research and clinical practice
This consensus study has explored the most important treatment targets for exercise interventions in persistent NSLBP, with priorities including improving function and quality of life, and reducing pain. This study provides the foundation for further consensus studies involving larger and more diverse groups of participants to generate more robust consensus for exercise as a whole, but may also provide a platform for more targeted consensus workshops aligned to specific exercise types. Overall, 25 targets were ranked and prioritised, which may be useful for future mediation analysis within trials, helping to further understand how exercise works for patients with NSLBP.
These targets may be targeted individually when identified at assessment or alongside multiple treatment targets when prescribing, designing, and/or evaluating exercise interventions for persistent NSLBP. By having a greater understanding of the sequential importance of these treatment targets, clinicians may be encouraged to target their exercise intervention to ensure they select the most appropriate exercises to get the most benefit for their patients.
As clinicians, by assessing patients for potential contributing factors such as strength deficits, fear avoidance, self-efficacy etc., they can identify priorities for their exercise treatment to target, and thereby select the most appropriate exercise. This can be performed within the framework of shared-decision making, to allow the best fit for each patient. These agreed treatment targets may guide the design of trials of exercise interventions for persistent NSLBP by helping to target exercise interventions to achievable, measurable outcomes that match the aim(s) of the intervention.
Future trial design may benefit from intervention logic models to map out the role of treatment targets, and select the most appropriate outcome domains and measures for complex interventions,such as exercise, with multiple intervention targets. [44, 45] The identified treatment targets may, therefore, help in the identification of potential mediators of exercise that should be measured in future studies and used in pre-specified mediation analysis within RCTs.
Conclusion
This consensus study with key stakeholders prioritised increasing function, improving quality of life, reducing pain, meeting patient-specific goals and reducing fear of movement, as the most important treatment targets of exercise interventions for patients with persistent NSLBP. Formal testing of these agreed treatment targets in future research is needed to establish their role on the pathway to improved outcomes.
Key messages
This study provides for the first time a consensus of stakeholders about the agreed treatment targets of exercise for persistent LBP.
Future clinical trials of exercise for persistent LBP would benefit from clear specification of the targets of their exercise interventions, through, for example, intervention logic models.
Testing whether these agreed treatment targets havea clear role in the pathway to clinical outcomes for patients is now needed.
Ethical approval:
Obtained from the Keele University Research Ethics committee for both workshops: on the 17 August 2018 (reference ERP 2393) and an amendment was approved on the 15 April 2019 (reference MH-190019). All participants gave written informed consent before data collection began.
Funding:
L Wood was a beneficiary of a Travel Fellowship awarded by the Society of Back Pain Research, UK. L Wood’s PhD is funded by the Primary Care Centre Versus Arthritis, School of Primary, Community and Social Care, Faculty of Medicine and Health Sciences, Keele University. Prof NE Foster is a National Institute for Health Research (NIHR) Senior Investigator and was supported by an NIHR Research Professorship (NIHR-RP-011-015). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Conflict of interest:
None declared.
References:
Stochkendahl MJ, Kjaer P, Hartvigsen J et al.
National Clinical Guidelines for Non-surgical Treatment of Patients with
Recent Onset Low Back Pain or Lumbar Radiculopathy
European Spine Journal 2018 (Jan); 27 (1): 60–75National Institute for Health and Care Excellence (NICE):
Low Back Pain and Sciatica in Over 16s: Assessment and Management (PDF)
NICE Guideline, No. 59 2016 (Nov): 1–1067Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, et al.
Prevention and Treatment of Low Back Pain:
Evidence, Challenges, and Promising Directions
Lancet. 2018 (Jun 9); 391 (10137): 2368–2383
This is the third of 4 articles in the remarkable Lancet Series on Low Back PainSaragiotto BT, Maher CG, Yamato TP, Costa LO, MenezesCosta LOC, Ostelo RW, et al.
Motor control exercise for chronic non-specific low-back pain.
In: Saragiotto BT, editor. Cochrane Database Syst Rev 2016;(1):CD012004. Available from:
http://www.ncbi.nlm.nih.gov/pubmed/26742533Hayden J, van Tulder M, Tomlinson G.
Systematic review: strategies for using exercise therapy
to improve outcomes in chronic low back pain.
Ann Intern Med 2005;142(9). Available from:
http://www.ncbi.nlm.nih.gov/pubmed/15867410Babatunde OO, Jordan JL, Van der Windt DA, Hill JC, Foster NE, Protheroe J.
Effective treatment options for musculoskeletal pain in primary care:
a systematic overview of current evidence.
In: Fleck-enstein J, editor.
PLoS One 2017;12(6):e0178621Hayden J, van Tulder MW, Malmivaara A, Koes BW.
Exercise therapy for treatment of non-specific low back pain.
In: Hayden J, editor. Cochrane database of systematic reviews.
Chichester,UK: John Wiley & Sons, Ltd; 2005.:CD000335. Available from:
http://www.ncbi.nlm.nih.gov/pubmed/16034851Searle A, Spink M, Ho A, Chuter V.
Exercise interventions for the treatment of chronic low back pain:
a systematic review and meta-analysis of randomised controlled trials.
Clin Rehabil 2015;29(12):1155–67.World Health Organization. WHO
Physical activity.
WHO. World Health Organization; 2017. Available from:
http://www.who.int/mediacentre/factsheets/fs385/en/Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH.
Physical activity and exercise for chronic pain in adults:
an overview of cochrane reviews.
Cochrane Database Syst Rev 2017;4(4):CD011279.Available from:
http://www.ncbi.nlm.nih.gov/pubmed/28436583Helmhout PH, Staal JB, Maher CG, Petersen T, Rainville J, ShawWS.
Exercise therapy and low back pain: insights and proposals to improve
the design, conduct, and reporting of clinical trials.
Spine (Phila Pa 1976) 2008;33(16):1782–8.Justice L, Sofka A, McGinty A.
Targets, techniques, and treatment contexts in emergent literacy intervention.
Semin SpeechLang 2007;28(1):014–24.Fonarow Gregg.
Treatment targets in heart failure continued emodynamics
in decompensated heart failure.
Rev CardiovascMed 2001;2(suppl 2):s7–12. Available from:
http://medreviews.com/sites/default/files/2016-11/RICM 2suppl2 s7.pdfSchmieder RE, Tschöpe D, Koch C, Ouarrak T, Gitt AK.
Individualised treatment targets in patients with
type-2 diabetes and hypertension.
Cardiovasc Diabetol 2018;17(1):18.Cefalu WT, Kaul S, Gerstein HC, Holman RR, Zinman B,Skyler JS, et al.
Cardiovascular outcomes trials in type 2 diabetes:
where do we go from here? Reflections from a diabetes
care editors’ expert forum.
Diabetes Care 2018;41. Available from:
http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dci17-0057/-/DC1.
http://www.diabetesjournals.org/content/diabetes-core-update-podcastsKong APS, Yang X, Ko GTC, So W-Y, Chan W-B, Ma RCW, et al.
Effects of treatment targets on subsequent cardiovascular events
in Chinese patients with type 2 diabetes.
Diabetes Care 2007;30(4):953–9.Wood L, Foster NE, Lewis M, Bishop A.
Exercise interventions for persistent non-specific low back pain –
does matching outcomes to treatment targets make a difference?
Asystematic review and meta-analysis.
J Pain 2021;22(2):107–26,
http://dx.doi.org/10.1016/j.jpain.2020.04.002.Moffett JK, Jackson DA, Gardiner ED, Torgerson DJ, Coulton S,Eaton S, et al.
Randomized trial of two physiotherapy interventions for primary care
neck and back pain patients: “McKenzie” vs brief physiotherapy pain management.
Rheumatology 2006;45(12):1514–21.Garcia AN, Costa L da CMLOP, Hancock MJ, De Souza FS, de OGomes GVF, De Almeida MO, et al.
McKenzie method of mechanical diagnosis and therapy was slightly more
effective than placebo for pain, but not for disability, in
patients with chronic non-specific lowback pain:
a randomised placebo controlled trial with short
and longer term follow-up.
Br J Sports Med 2018;52(9):594–8. Available from:
http://bjsm.bmj.com/lookup/doi/10.1136/bjsports-2016-097327Harvey N, Holmes CA.
Nominal group technique: an effective method for obtaining group consensus.
Int J Nurs Pract 2012;18(2):188–94. Available from:
http://doi.wiley.com/10.1111/j.1440-172X.2012.02017.xPotter M, Gordon S, Hamer P.
The Nominal Group technique: a useful consensus methodology
in physiotherapy research.
New Zeal J Physiother 2004;32(3):126–30. Available from:
http://physiotherapy.org.nz/assets/Professional-dev/Journal/2004-November/2004NovHamner.pdfBlack N.
Consensus development methods.
In: Pope C, Mays N, editors.
Qualitative research in health care. third edition 2006 [chapter 12].Mc Sharry J, Fredrix M, Hynes L, Byrne M.
Prioritising target behaviours for research in diabetes: using the
nominal group technique to achieve consensus from key stakeholders.
Res InvolvEngagem 2016; 2(1):14. Available from:
http://researchinvolvement.biomedcentral.com/articles/10.1186/s40900-016-0028-9Mc Sharry J, Fredrix M, Hynes L, Byrne M.
Prioritising target behaviours for research in diabetes:
using the nominal group technique to achieve consensus from key stakeholders.
Res Involv Engagem2016;2(1).Rainville J, Hartigan C, Martinez E, Limke J, Jouve C, Finno M.
Exercise as a treatment for chronic low back pain.
Spine J 2004;4(1):106–15.Available from:
http://www.ncbi.nlm.nih.gov/pubmed/14749199World Health Organization.
Towards a common language for functioning, disability and health:
ICF. Int Classif2002;1149:1–22. Available from:
http://www.who.int/classifications/icf/training/icfbeginnersguide.pdfCooney G, Dwan K, Mead G.
Exercise for depression.
JAMA2014;311(23):2432–3.Costa CM, Maher CG, Mcauley JH, Hancock MJ, SmeetsRJEM.
Self-efficacy is more important than fear of movement in mediating
the relationship between pain and disability in chronic low back pain.
Eur J Pain 2011;15(2):213–9
http://dx.doi.org/10.1016/j.ejpain.2010.06.014Marshall PWM, Schabrun S, Knox MF.
Physical activity and themediating effect of fear, depression, anxiety,
and catastrophizing on pain related disability in people with chronic low back pain.
In:Yang J, editor.
PLoS One 2017;12(7):e0180788. Available from:
http://dx.plos.org/10.1371/journal.pone.0180788Smith BE, Hendrick P, Bateman M, Holden S, Littlewood C, SmithTO, et al.
Musculoskeletal pain and exercise—
challenging existing paradigms and introducing new.
Br J Sports Med 2019;53(14):907–12.Stathopoulou G, Powers MB, Berry AC, Smits JAJ, Otto MW.
Exercise interventions for mental health:
a quantitative and qualitative review.
Clin Psychol Sci Pract 2006;13(2):179–93. Available from:
http://doi.wiley.com/10.1111/j.1468-2850.2006.00021.xKnapen J, Vancampfort D, Moriën Y, Marchal Y.
Exercise therapy improves both mental and physical health
in patients with major depression.
Disabil Rehabil 2015;37(16):1490–5. Available from:
http://www.tandfonline.com/doi/full/10.3109/09638288.2014.972579Falla D, Hodges PW.
Individualized exercise interventions for spinal pain.
Exerc Sport Sci Rev 2017;45(2):105–15. Available from:
http://insights.ovid.com/crossref?an=00003677-201704000-00008Froud R, Ellard D, Patel S, Eldridge S, Underwood M.
Primary outcome measure use in back pain trials may need radical reassessment.
BMC Musculoskelet Disord 2015;16(1):88.Mansell G, Kamper SJ, Kent P.
Why and how back pain interventions work: what can we do to find out?
Best Pract Res Clin Rheuma-tol 2013;27(5):685–97. Available from:
http://linkinghub.elsevier.com/retrieve/pii/S1521694213000776Lee H, Hübscher M, Moseley GL, Kamper SJ, Traeger AC,Mansell G, et al.
How does pain lead to disability? A systematic review and meta-analysis
of mediation studies in people with back and neck pain.
Pain 2015;156(June (6)):988–97
http://dx.doi.org/10.1097/j.pain.0000000000000146.Lee H, Mansell G, McAuley JH, Kamper SJ.
Causal mechanisms in the clinical course and treatment of back pain.
Best Pract Res Clin Rheumatol 2017:1–10, http://dx.doi.org/10.1016/j.berh.2017.04.001Mansell G, Hill JC, Main C, Vowles KE, van der Windt D.
Exploring what factors mediate treatment effect: example of the STarT back study high-risk intervention.
J Pain 2016;17(11):1237–45. Available from:
http://www.ncbi.nlm.nih.gov/pubmed/27565304Stevens ML, Boyle E, Hartvigsen J, Mansell G, Søgaard K, JørgensenMB, et al.
Mechanisms for reducing low back pain: a mediation analysis of
a multifaceted intervention in workers in elderly care.
Int Arch Occup Environ Health 2019;92(January (1)):49–58
http://dx.doi.org/10.1007/s00420-018-1350-3Whittle R, Mansell G, Jellema P, Van Der Windt D.
Applying causal mediation methods to clinical trial data:
What can we learn about why our interventions (don’t) work?
Eur J Pain 2017;21:614–22.Woby SR, Watson PJ, Roach NK, Urmston M.
Are changes in fear-avoidance beliefs, catastrophizing, and appraisals of
control, predictive of changes in chronic low back pain and disability?
Eur J Pain2004;8(3):201–10.Gianola S, Frigerio P, Agostini M, Bolotta R, Castellini G, Corbetta D, et al.
Completeness of outcomes description reported in low back pain
rehabilitation interventions: a survey of 185 randomized trials.
Physiother Can 2016;68(3):267–74. Available from:
http://utpjournals.press/doi/10.3138/ptc.2015-30Froud R, Patel S, Rajendran D, Bright P, Bjørkli T, Buchbinder R, et al.
A systematic review of outcome measures use, analytical approaches,
reporting methods, and publication volume by year in low back
pain trials published between 1980 and 2012:
Respice, adspice, et prospice.
PLoS One 2016;11(10):1–16.Rohwer A, Pfadenhauer L, Burns J, Brereton L, Gerhardus A, Booth A,et al.
Logic models help make sense of complexity in systematic reviews nd health technology assessments.
J Clin Epidemiol 2017;83:37–47.Available from:
https://doi.org/10.1016/j.jclinepi.2016.06.012Hurley DA, Murphy LC, Hayes D, Hall AM, Toomey E,McDonough SM, et al.
Using intervention mapping to develop a theory-driven, group-based complex
intervention to support self-management of osteoarthritis and low back pain (SOLAS).
ImplementSci 2016;11(1):56. Available from:
http://implementationscience.biomedcentral.com/articles/10.1186/s13012-016-0418-2
Return to LOW BACK PAIN
Return to EXERCISE AND CHIROPRACTIC
Since 10-12-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |