Medicare Documentation Requirements:
The Hurdle That Continues to Block Our ProgressThis section was compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Dynamic Chiropractic ~ April 9, 2012 ~ FULL TEXT
By David Seaman, DC, MS, DABCN,
Albert J. Luce, DC and
Anthony Hamm, DC, FACO, DABFP
At present, the chiropractic profession has difficulty being compliant with Medicare documentation requirements. The 2009 report from the Office of the Inspector General reported the following: "Distinct from the undocumented claims, 83 percent of reviewed chiropractic claims failed to meet one or more of the documentation requirements.
Concerning treatment, file reviewers reported that only 76 percent contained some form of treatment plan, 43 percent lacked treatment goals, 17 percent lacked objective measures, and 15 percent lacked the recommended level of care." [1]
In January 2011, the California Chiropractic Association reported the following on its Web site: [2] "Palmetto GBA has released the results of its review of chiropractic Medicare claims and found an "unacceptable" error rate of 68 percent for Northern California and 77 percent for Southern California. These results are very troubling, as Congressional leaders have threatened to remove chiropractic from Medicare if the profession [does] not improve its billing practices."
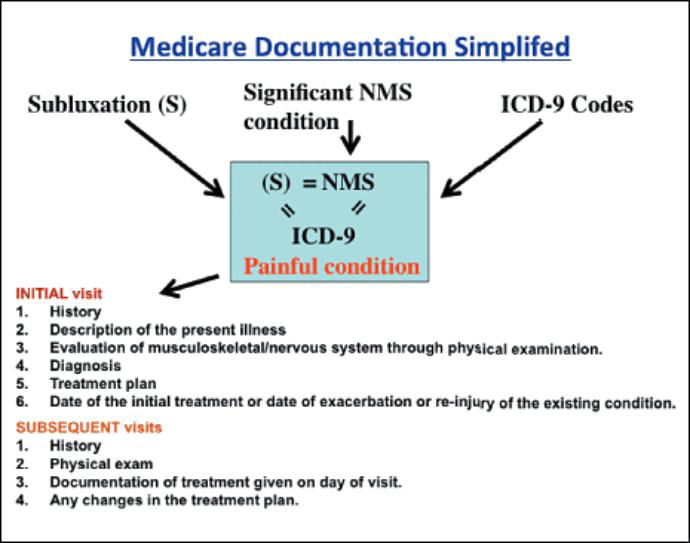
Perhaps two primary issues may be at work. Either an inaccurate message is being delivered to chiropractors regarding appropriate Medicare documentation requirements and/or chiropractors are misinterpreting the message. Let's attempt to clear up some of the confusion, outline documentation requirements based on several Medicare publications, and provide a flow chart for easy visualization of the required process.
What Does Medicare Want? The rules for Medicare are spelled out in section 240 of chapter 15 of the Medicare Benefit Policy Manual [3] and in your local carrier's or administrator's Local Coverage Determination (LCD). The terminology is generally consistent; however, it can be confusing based on how the language is misinterpreted by chiropractors and those who teach documentation and coding seminars.
Contrary to what many believe, Medicare documentation is not subluxation-based, even though parts of section 240 can mislead one in this direction. Why do we say this? Because "subluxation-based" to chiropractors is a different concept compared to subluxation-based to Medicare, and this fact is clearly spelled out in the rules.
Subluxation-based chiropractors view the adjustment of the asymptomatic spine as an acceptable practice. However, this is not the case for Medicare – for Medicare, subluxation is synonymous with a painful neuromusculoskeletal condition of the spine that disables the patient from engaging in routine functional activities of daily living. In the context of treating Medicare patients, consider the following statements from various LCDs throughout the United States.From the Florida LCD: "Chiropractic services involve manual manipulation of the spine by a licensed chiropractor to alleviate painful symptomatology due to subluxation of the spine as demonstrated by x-ray or physical exam."
From the LCD for Upstate New York: "Most primary neuromusculoskeletal disorders manifest primarily by a painful response. Standardized measurement scales (e.g., Visual Analogue Scale (VAS), Oswestry Disability Questionnaire, and the Quebec Back Pain Disability Scale) may be used to measure improvement or lack thereof."
From the Trailblazer LCD for Colorado, New Mexico, Oklahoma and Texas: "For the purpose of Medicare, subluxation means a motion segment in which alignment, movement integrity and/or physiological function of the spine are altered although contact between joint surfaces remains intact. A subluxation usually falls into one of two categories: [1]. Acute, such as strains and sprains. [2]. Chronic, such as loss of joint mobility."In a senior citizen, an acute strain/sprain or chronic reduction in joint mobility is always painful. This is why the Florida LCD states that manipulation is to "alleviate painful symptomatology." This is also why the Upstate New York LCD requires the use of outcome assessment tools that measure pain and disability.
This view is further evidenced by structural and process measures reported through the 2011 CMS Physician Quality Reporting System (PQRS). Two of the three measures that doctors of chiropractic may report are pain assessment and functional outcome assessment. According to PQRS standards, functional outcome deficiencies are defined as "impairment or loss of physical function related to neuromusculoskeletal capacity, including but not limited to restricted flexion, extension and rotation, back pain, neck pain, pain in the joints of the arms and legs, and headaches."
So, what does Medicare want? Medicare wants us to treat beneficiaries who are disabled by spinal pain. Getting caught up in PART requirements and because "subluxation" is written into section 240 and all LCDs does not change the fact that Medicare is about pain and disability. In short, the chiropractic profession needs to reconcile its historical view of subluxation in the context of current Medicare rules. That congressional leaders are actually thinking about dropping us from Medicare demonstrates this need. [2]
Readjusting Our Notion of Subluxation In section 240 and all the LCDs, three concepts appear in a fashion that can lead a DC to think they are distinct entities. We read about subluxation, the significant neuromusculoskeletal condition, and the ICD-9 diagnostic code as if they are separate and causally related.
In fact, from an operational perspective, each is referring to the exact same entity: a painful spinal condition that is significant enough to create disability and must be documented in the context of the initial and subsequent visits.Consider factors that must be documented in the history which relate to the nature of the painful spinal condition:
Description of present illness/symptoms causing patient to seek treatment; these symptoms must bear a direct causal relationship to the spine
Mechanism of trauma
Quality and character
Onset, duration, intensity, frequency, location and referral/radiation
Aggravating and relieving factors
These history factors are about a painful spinal condition. In fact, all of the key components relevant to Medicare documentation are designed to demonstrate that there is a painful spinal condition present and that it is amenable to chiropractic manipulative treatment. (See Table)
Please notice that the word subluxation does not appear in the table. This is because Medicare documentation is not about "subluxation" in the context that chiropractors perceive it. Rather, as described above, Medicare operationally defines subluxation as a painful spinal condition that creates disability. The sooner we embrace this fact, the sooner we will move toward compliance and hopefully, reimbursement for our full scope of care.
DOCUMENTATION REQUIREMENTS AND PROCEDURES Management Flow Per Medicare But Applicable to all Patients Management/Documentation Components Required To Be Medicare Compliant Procedure and Action Steps to Ensure Medicare Compliance 1. Medicare patient enters office complaining of low back pain that extends into their buttocks. They cite various functional limitations (disabilities) due to their pain. Must establish medical necessity for spinal manipulation. Is the beneficiary experiencing a significant neuromusculoskeletal health problem necessitating manual manipulation by the chiropractor?
Based on this presentation, the answer is yes, which permits us to proceed to the history.NOTE: Numbers 2-8 relate to the initial visit 2. History
• Symptoms causing the patient to seek treatment
• Family history, if relevant
• Past health history
– prior injuries/traumas
– prior surgeries
– prior hospitalizations
– current medications
• Check for contraindications
• Description of present illness / symptoms causing patient to seek treatment; these symptoms must bear a direct causal relationship to the spine
– mechanism of trauma
– quality and character
– onset, duration, intensity, frequency, location, and referral/radiation
– aggravating and relieving factors
– prior interventions, treatments and medications
• Secondary complaintsThe history demonstrates medical necessity only if the patient is functionally limited, which is almost always due to pain. The chance of a functional limitation without pain is exceedingly rare.
Chiropractors should acquire or develop a new patient history form that addresses the history components required by Medicare.
It is important to note is that Medicare's history requirements are a basic guideline. A comprehensive history is required due to all the probable red flag and non-red-flag disorders that need to be considered.
Proceed with examination only if the history substantiates medical necessity.3. Red flags
Reds flags (RF) are signs and/or symptoms reflective of a visceral disorder, or a serious or potentially life-threatening disease.In Medicare terminology, RF conditions refer to relative and absolute contraindications (RC & AC):
Relative Contraindications
1. Articular hypermobility and circumstances in which the stability of the joint is uncertain
2. Severe demineralization of bone
3. Benign bone tumors of the spine
4. Bleeding disorders and anticoagulant therapy
5. Radiculopathy with progressive neurological signs
Absolute Contraindications
1. Acute arthropathies characterized by acute inflammation and ligamentous laxity, and anatomic subluxation or dislocation including acute rheumatoid arthritis and ankylosing spondylitis
2. Acute fractures and dislocations or healed fractures and dislocations with signs of instability
3. An unstable os odontoideum
4. Malignancies that involve the vertebral column
5. Infections of bones or joints of the vertebral column
6. Signs and symptoms of myelopathy or cauda equina syndrome
7. For cervical spinal manipulations, vertebrobasilar insufficiency syndrome
8. A significant major artery aneurysm near the proposed manipulationRed flags (RC & AC) can be identified in a new- patient / history form and from an individual red flag form.
If absolute contraindication(s) are identified, then consider immediate referral.
For relative contraindications, consider a referral and precautions to HVLA thrusts.
The patient record must indicate the presence or absence of contraindications.
Chiropractors should acquire or create history forms that include screening questions for these contraindications.4. Physical examination Medicare clearly mandates that the physical exam must demonstrate a causal relationship between the spine and the patient's presenting complaint, which demonstrates medical necessity for spinal manipulation.
In addition, the manipulation must have a direct beneficial therapeutic relationship to the patient's condition. The manipulative service must provide reasonable expectation of recovery or improvement of function.The physical examination leads to the generation of three important documentation requirements: (1) the selection of the vertebral level that is capable of generating the painful symptoms, (2) PART and (3) an appropriate ICD-9 code, all of which establish medical necessity for spinal manipulation. 5. PART The acronym PART has been used to describe the examination components indicating that a patient is suffering from a spinal condition amenable to manipulation.
A least 2 of the 4 PART criteria must be met, with at least one of them being the "A" or "R" component.
What about radiographs? They are not required to satisfy Medicare documentation requirements.
When should radiographs be used? For pathological diagnosis purposes.The designation of PART in the record demonstrates to Medicare that the stated spinal level of dysfunction, as per the listed regional 739 code, has been examined/ identified and correlated to the secondary ICD-9 code.
The following quote from the 2009 OIG report demonstrates that we have not met the above documentation expectations:
From page 11 of the 2009 OIG report: [3] "The records would indicate a problem in one area of the spine which was examined, but indicated treatment to three to four areas of the spine and charged according to procedure without correlation to diagnosis."
We suggest using/developing examination forms that lead to appropriate documentation of the correlation between PART and the 739 and secondary ICD-9 codes.6. Generation of a diagnosis and related ICD-9 code With the exception of regular Medicare in Florida, Puerto Rico and the U.S. Virgin Islands, the primary diagnosis for Box 21 of the 1500 billing form will be the 739 code series; one 739 code for each spinal region billed.
Each primary 739 code should be followed by a secondary diagnosis, which should reflect the correlated (and correctable) significant neuromusculoskeletal condition that is painful and limiting a patient's function.
In Florida, regular Medicare* billed to First Coast Services Options, the 739 code series is not billed as a diagnosis code, but all other examination, treatment, and documentation requirements are identical.
* Railroad Medicare and Medicare Advantage require 739 series on the bill.A thorough history to include pain diagrams that is followed by an appropriate exam can help to identify the most likely pain generator, which leads to:
(1) the selection of the offending vertebral level, and
(2) the generation of an appropriate secondary diagnosis code.
Chiropractors can accomplish this by developing forms that utilize appropriate spinal examination criteria:
1. Pain drawings.
2. Souza's spinal examination chapters [4]
3. Murphy's Diagnosis-Based Clinical Decision Rule [5-9]
4. Laslett's criteria for SIJ pain [10]
5. Laslett's criteria for lumbar Z-joint pain [10]
6. Wainer's criteria for cervical radiculopathy [10]
7. History predictors for lumbar stenosis [10]
8. Clinical prediction rules for spinal manipulation [10]
9. Prediction rule for spinal stability [10]7. Treatment plan
A comment from the 2009 OIG report, page 17:
"In my (medical reviewer) 29 years of practice, I rarely saw documentation of a plan which included frequency, duration, goals, and objective measures… they apparently have not been incorporated into the profession."Medicare requires the following components in the treatment plan:
1. Recommended level of care (duration and frequency of patient visits)
2. Specific treatment goals*
3. Objective measures to evaluate treatment effectiveness
*For long-term goals, write out what the predicted maximum improvement will be for the patient; this will help you identify when the AT modifier is no longer supported and it must be changed to GA for maintenance care.The treatment plan must be outlined in the patient's medical record. This will vary on a case-by-case basis.
We suggest using outcome assessment instruments such as the Quad VAS, Oswestry Disability Index, Bournemouth Neck and Back, Pain Disability Questionnaire (PDQ), etc.
It is advisable to label the patient's spinal condition as "acute" or "chronic" in accordance with the Medicare Benefit Policy Manual, Chapter 15, and Section 240.1.5. This label relates to the required goals (treatment expectations), treatment frequency, duration and the prognosis for recovery or improvement. [2]8. Prognosis According to Medicare: [2]
“The chiropractor should be afforded the opportunity to effect improvement or arrest or retard deterioration in such condition within a reasonable and generally predictable period of time.”
(Medicare Benefit Policy Manual, Chapter 15, and Section 240.1.5.)A reasonable prognosis can be generated based on the acute / chronic nature of the condition and based on any perpetuating factors such as biopsychosocial issues, lifestyle, nutritional, behavior, health status etc. Factors that influence prognosis should be included in your forms / patient record – they need to be documented.
9. Subsequent visits The following documentation is required by Medicare:
1. Date
2. History3. Physical Exam
- review of chief complaint
- changes since last visit
- system review, if relevant
4. Evaluation of treatment effectiveness
- examination of area of spine involved in diagnosis
- assessment of change in patient condition since the last visit
5. Describe treatment given on this visit
6. Any changes in treatment planWe suggest developing a form that allows for consistent documentation of each Medicare patient visit so that each required component is satisfied. A SOAP note to include PART is most appropriate.
For exacerbations or new complaints, a new initial sequence is warranted, which requires Box 14 to be updated.Compiled by Drs. David Seaman and Albert Luce (2009-2011)
References:
Office of the Inspector General.
Inappropriate Medicare Payments for Chiropractic Service PDF
Washington, DC: US Department of Health and Human Services; 2009"Palmetto CERT Review Finds ‘Unacceptable' Chiropractic Medicare Denial Rate."
CCA Advantage, January 2011.
Center for Medicare Services.
Medicare Benefit Policy Manual
Chapter 15 – Covered Medical and Other Health Services.
Souza TA.
Differential Diagnosis and Management for the Chiropractor:
Protocols and Algorithms. 4th Edition. Boston: Jones and Bartlett; 2009.
Murphy DR.
A Clinical Model for the Diagnosis and Management of Patients with Cervical Spine Syndromes
Australasian Chiropractic & Osteopathy 2004 (Nov); 12 (2): 57–71Murphy DR Hurwitz EL:
A Theoretical Model for the Development of a Diagnosis-based Clinical Decision Rule for
the Management of Patients with Spinal Pain
BMC Musculoskelet Disord. 2007 (Aug 3); 8: 75Murphy D, Hurwitz E, Nelson C:
A Diagnosis-based Clinical Decision Rule For Spinal Pain Part 2: Review Of The Literature
Chiropractic & Osteopathy 2008 (Aug 11); 16: 7Murphy DR, Hurwitz EL, McGovern EE.
Outcome of pregnancy-related lumbopelvic pain treated according to a diagnosis-based decision rule: a prospective observational cohort study.
J Manipulative Physiol Ther, 2009; 32 (8): 616-24
Murphy DR, Hurwitz EL, McGovern EE:
A Nonsurgical Approach to the Management of Patients With Lumbar Radiculopathy
Secondary to Herniated Disk: A Prospective Observational Cohort Study With Follow-Up
J Manipulative Physiol Ther 2009, 32(9):723-733Cleland JA, Koppenhaver S.
Netter's Orthopedic Clinical Examination: An Evidence-Based Approach. 2nd Edition. Philadelphia: Saunders Elsevier; 2011.
Return to MEDICARE
Return to DOCUMENTATION
Since 5-02-2012


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |