

Nonpharmacologic Therapies for Low Back Pain:
A Systematic Review for an American College
of Physicians Clinical Practice GuidelineThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Annals of Internal Medicine 2017 (Apr 4); 166 (7): 493505 ~ FULL TEXT
OPEN ACCESS Roger Chou, MD; Richard Deyo, MD, MPH; Janna Friedly, MD; Andrea Skelly, PhD, MPH;
Robin Hashimoto, PhD; Melissa Weimer, DO, MCR; Rochelle Fu, PhD; Tracy Dana, MLS;
Paul Kraegel, MSW; Jessica Griffin, MS; Sara Grusing, BA; Erika D. Brodt, BS
From Oregon Health and Science University,
Portland, Oregon, and University of Washington,
Seattle, and Spectrum Research,
Tacoma, Washington.

BACKGROUND: A 2007 American College of Physicians guideline addressed nonpharmacologic treatment options for low back pain. New evidence is now available.
PURPOSE: To systematically review the current evidence on nonpharmacologic therapies for acute or chronic nonradicular or radicular low back pain.
DATA SOURCES: Ovid MEDLINE (January 2008 through February 2016), Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, and reference lists.
STUDY SELECTION: Randomized trials of 9 nonpharmacologic options versus sham treatment, wait list, or usual care, or of 1 nonpharmacologic option versus another.
DATA EXTRACTION: One investigator abstracted data, and a second checked abstractions for accuracy; 2 investigators independently assessed study quality.
DATA SYNTHESIS: The number of trials evaluating nonpharmacologic therapies ranged from 2 (tai chi) to 121 (exercise). New evidence indicates that tai chi (strength of evidence [SOE], low) and mindfulness-based stress reduction (SOE, moderate) are effective for chronic low back pain and strengthens previous findings regarding the effectiveness of yoga (SOE, moderate). Evidence continues to support the effectiveness of exercise, psychological therapies, multidisciplinary rehabilitation, spinal manipulation, massage, and acupuncture for chronic low back pain (SOE, low to moderate). Limited evidence shows that acupuncture is modestly effective for acute low back pain (SOE, low). The magnitude of pain benefits was small to moderate and generally short term; effects on function generally were smaller than effects on pain.
LIMITATION: Qualitatively synthesized new trials with prior meta-analyses, restricted to English-language studies; heterogeneity in treatment techniques; and inability to exclude placebo effects.
CONCLUSION: Several nonpharmacologic therapies for primarily chronic low back pain are associated with small to moderate, usually short-term effects on pain; findings include new evidence on mind-body interventions.
PRIMARY FUNDING SOURCE: Agency for Healthcare Research and Quality. (PROSPERO: CRD42014014735).
From the FULL TEXT Article:
Background
Low back pain is very common and is associated with more global disability than any other condition [1]. Several nonpharmacologic, noninvasive therapies are available for low back pain, including exercise, complementary and alternative therapies (such as spinal manipulation, acupuncture, massage, and mindbody interventions), psychological therapies (such as cognitive behavioral and operant therapy), physical techniques (such as traction, ultrasound, transcutaneous electrical nerve stimulation, low-level laser therapy, superficial heat or cold, and back supports), and multidisciplinary rehabilitation.
A 2007 guideline [2] and an associated systematic review [3] from the American College of Physicians (ACP) and American Pain Society (APS) recommended spinal manipulation as a treatment option for acute low back pain and several nonpharmacologic therapies for subacute or chronic low back pain. New evidence is now available. The purpose of this article is to review the current evidence on the benefits and harms of nonpharmacologic therapies for low back pain. The ACP will use this review to develop an updated clinical practice guideline.
Methods
Detailed methods for this review, including the analytic framework, additional nonpharmacologic therapies (physical techniques), medications (addressed in a separate article) [4], search strategies, inclusion criteria, data extraction and quality-rating methods, and additional outcomes (such as quality of life, global improvement, and patient satisfaction) are available in the full report [5]. The protocol was developed by using a standardized process [6] with input from experts and the public and is registered in the PROSPERO database [7]. This article addresses the following question: What are the comparative benefits and harms of nonpharmacologic, noninvasive therapies for acute or chronic nonradicular or radicular low back pain or for symptomatic spinal stenosis?
Data Sources and Search
A research librarian searched several electronic databases, including Ovid MEDLINE (January 2007 through April 2015) and the Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews (through April 2015). We used the previous ACP/APS review to identify earlier studies [8]. Searches were updated through November 2016. We also reviewed reference lists and searched ClinicalTrials.gov.
Study Selection
Two investigators independently reviewed abstracts and full-text articles against prespecified eligibility criteria. The population was adults with acute (<4 weeks), subacute (4 to 12 weeks), or chronic (≥12 weeks) nonradicular or radicular low back pain. Excluded conditions were low back pain due to cancer, infection, inflammatory arthropathy, high-velocity trauma, or fracture; low back pain during pregnancy; and the presence of severe or progressive neurologic deficits. We included randomized trials of exercise, spinal manipulation, acupuncture, massage, mindbody interventions (yoga, tai chi, mindfulness-based stress reduction), psychological therapies, or multidisciplinary rehabilitation versus sham (functionally inert) treatment, wait list, or usual care (usually defined as care provided at the discretion of the clinician), as well as comparisons between 1 therapy and another. Outcomes were long-term (≥1 year) or short-term (≤6 months) pain, function, return to work, and harms.
Given the large number of interventions, we included systematic reviews of randomized trials [6, 9]. For each intervention, we selected the most recent, relevant, and comprehensive systematic review that was of the highest quality on the basis of a validated assessment tool [9, 10]. If more than 1 good-quality systematic review was available, we preferentially selected updates of reviews used in the ACP/APS review. We supplemented systematic reviews with additional randomized trials. We did not include systematic reviews identified in update searches but checked reference lists for additional studies. We excluded nonEnglish-language articles and abstract-only publications.
Data Extraction and Quality Assessment
One investigator extracted study data, and a second verified the accuracy of the extractions. For systematic reviews, we abstracted details about review methods and results (Supplement Table 1). For randomized trials not included in a systematic review, we abstracted details regarding the study, population, and treatment characteristics, as well as the results (Supplement Table 2).
Two investigators independently assessed the quality of each study as good, fair, or poor by using criteria developed by the U.S. Preventive Services Task Force [11] (for randomized trials [Supplement Table 3]) and AMSTAR (A Measurement Tool to Assess Systematic Reviews; for systematic reviews [Supplement Table 4]) [9].
For primary studies included in systematic reviews, we relied on the quality ratings as performed in the reviews. We used the overall grade (for example, good, fair, or poor; or high or low) as determined in the systematic review.

Table 1 We classified the magnitude of effects for pain and function by using the same system used in the ACP/APS review (Table 1) [2, 12]. We also reported risk estimates based on the proportion of patients achieving successful pain or function outcomes (such as >30% or >50% improvement).
Data Synthesis and Analysis
We synthesized data qualitatively for each intervention, stratified according to the duration of symptoms (acute, subacute, or chronic) and presence or absence of radicular symptoms. We reported meta-analysis results from systematic reviews. If statistical heterogeneity was present, we examined the degree of inconsistency and evaluated subgroup and sensitivity analyses. We did not conduct an updated meta-analysis; rather, we qualitatively examined whether the results of new studies were consistent with pooled or qualitative findings from previous systematic reviews. Qualitative assessments were based on whether the findings from the new studies were in the same direction as those of the previous systematic reviews and whether the magnitude of effects was similar; if previous meta-analyses were available, we assessed whether the estimates and CIs from the new studies were encompassed in the CIs of previous pooled estimates. We assessed the strength of evidence (SOE) for each body of evidence as high, moderate, low, or insufficient on the basis of aggregate study quality, precision, consistency, and directness [6].
Role of the Funding Source
This project was funded by the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services. Staff members of AHRQ assisted in developing the scope and key questions. The AHRQ had no role in study selection, quality assessment, or synthesis.
Results
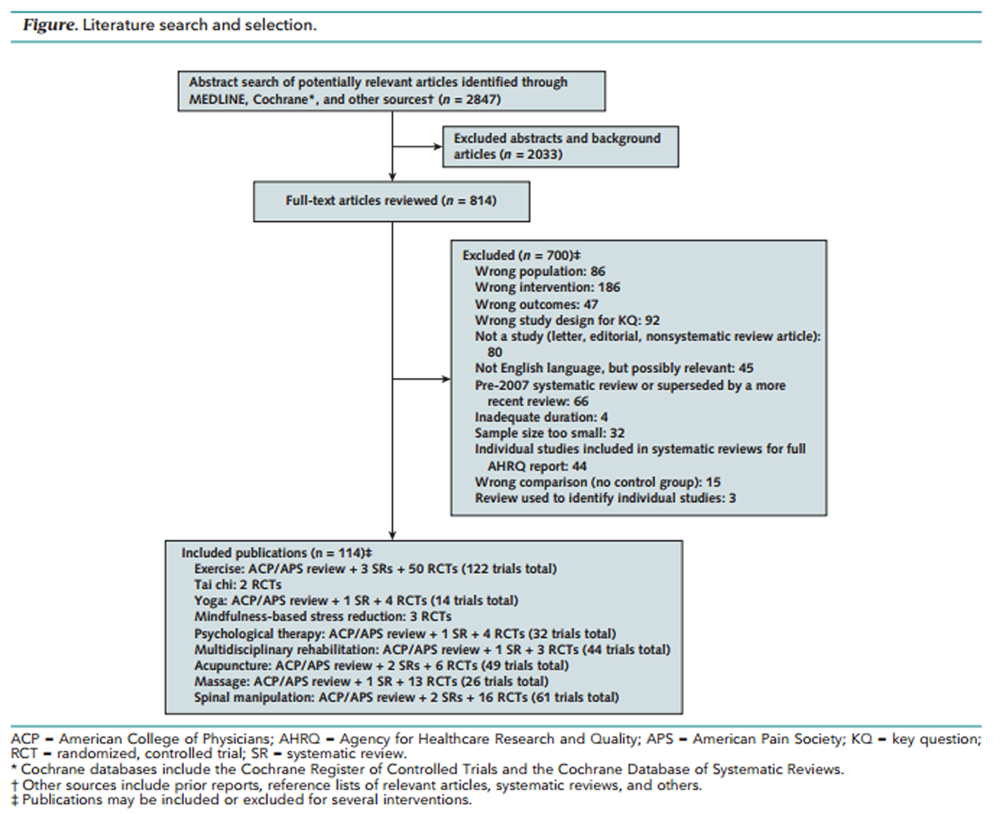
Figure The search and selection of articles are summarized in the literature flow diagram (Figure). Database searches resulted in 2,847 potentially relevant articles. After dual review of abstracts and titles, we selected 814 articles for full-text dual review; 114 publications met our inclusion criteria. Details for the systematic reviews included are shown in Supplement Table 1, and details for additional trials included are shown in Supplement Table 2; quality ratings are shown in Supplement Table 3 (systematic reviews) and Supplement Table 4 (trials).

Exercise
We found 122 trials that evaluated exercise. Three systematic reviews included 71 unique trials (total sample sizes ranged from 1993 to 4138) [1315], and we identified 51 additional trials (sample sizes, ≥100 in 18 trials [1634] and <100 in 33). One systematic review focused on exercise for chronic low back pain (37 trials) [14], 1 evaluated the effects of exercise on work disability in patients with subacute or chronic low back pain (23 trials) [15], and 1 examined the effects of motor control exercise (MCE) (16 trials) [13]. One review classified 41% of trials as low risk of bias, and another classified 62% as high quality; among the additional trials with 100 or more patients, we rated 4 good, 7 fair, and 7 poor quality.
For acute (3 trials) or subacute (5 trials) low back pain, the ACP/APS review previously found no difference between exercise therapy and no exercise on pain. Three additional trials of exercise versus no exercise or usual care reported inconsistent effects on pain and function [21, 31, 32].
For chronic low back pain, the ACP/APS review found that exercise was associated with greater pain relief than no exercise (19 trials: weighted mean difference [WMD], 10 on a 0- to 100-point scale [95% CI, 1.31 to 19.09]); the effects on function were small and not statistically significant (17 trials: WMD, 3.00 on a 0- to 100-point scale [CI, 0.53 to 6.48]). In a more recent systematic review that used more restrictive criteria, exercise therapy was associated with less pain intensity (3 trials: WMD, 9.23 [CI, 16.02 to 2.43]) and better function (3 randomized, controlled trials: WMD, 12.35 on a 0- to 100-point scale [CI, 23.0 to 1.69]) versus usual care at treatment end; the effects were smaller at long-term follow-up (mean difference, 4.94 [CI, 10.45 to 0.58] for pain and 3.17 [CI, 5.96 to 0.38] for function) [14]. Another systematic review found that compared with minimal intervention, MCE decreased pain intensity (2 trials: WMD, 12.48 on a 0- to 100-point scale [CI, 19.04 to 5.93] short term and 13.32 [CI, 19.75 to 6.90] long term) and improved function (3 trials: WMD, 9.00 on a 0- to 100-point scale [CI, 15.28 to 2.73] short term; 2 trials: WMD, 6.64 [CI, 11.72 to 1.57] long term) [13]. Still another systematic review found an association between exercise and a lower likelihood of work disability at long-term follow-up (about 12 months) (10 comparisons in 8 trials: odds ratio, 0.66 [CI, 0.48 to 0.92]), with no statistically significant effects in the shorter term [15]. Among trials of exercise versus no exercise or usual care not included in the systematic reviews, 15 of 22 found exercise to be more effective for pain and 12 of 17 found exercise to be more effective for function.
For radicular low back pain, 3 trials (n = 181 to 348) found exercise to be more effective than usual care or no exercise for pain or function, but the effects were small [16, 17, 25].
A systematic review found that compared with general exercise, MCE was associated with less pain intensity in the short term (6 trials: WMD, 7.80 on a 0- to 100-point scale [CI, 10.95 to 4.65]) and intermediate term (3 trials: WMD, 6.06 [CI, 10.94 to 1.18]); however, the differences were smaller and no longer statistically significant in the long term (4 trials: WMD, 3.10 [CI, 7.03 to 0.83]) [13]. In addition, MCE was associated with better short-term (6 trials: WMD, 4.65 on a 0- to 100-point scale [CI, 6.20 to 3.11]) and long-term (3 trials: WMD, 4.72 [CI, 8.81 to 0.63]) function. Three subsequent trials generally were consistent with the systematic review in finding MCE slightly more effective than general exercise for pain or function [30, 33, 34]. For comparisons involving other types of exercise techniques, no clear differences were observed in more than 20 head-to-head trials of acute or chronic back pain.

Tai Chi
Two fair-quality trials (n = 160 and 320) [35, 36] found that tai chi reduced pain versus wait list or no tai chi (mean differences, 0.9 and 1.3, respectively, on a 0- to 10-point scale); 1 trial [35] also found greater improvement in function (mean difference, 2.6 on the Roland Morris Disability Questionnaire [RDQ] [CI, 1.1 to 3.7]).

Yoga
Fourteen trials evaluated yoga for chronic low back pain. Ten trials (n = 1,056; range, 12 to 313) were in a systematic review [37], and we identified 4 additional trials (n = 375; range, 60 to 159) [38, 39]. Eight trials in the systematic review were rated as low risk of bias; we rated 2 other trials as fair and 2 as good quality.
One trial found that compared with usual care, Iyengar yoga was associated with lower pain scores (24 vs. 37 on a visual analogue scale [VAS] of 0 to 100; P < 0.001) and better function (18 vs. 21 on the 0- to 100-point Oswestry Disability Index; P < 0.01) at 24 weeks [40]. Five trials generally found yoga to be associated with lower pain intensity and better function versus exercise, although the effects were small and differences were not always statistically significant [38, 4144]. Compared with education, yoga was associated with lower short-term pain intensity (5 trials: standardized mean difference [SMD], 0.45 [CI, 0.63 to 0.26; I2 = 0%]), but the effects were smaller and not statistically significant at longer-term follow-up; yoga also was associated with better function at short-term (5 trials: SMD, 0.45 [CI, 0.65 to 0.25; I2 = 8%]) and long-term (4 trials: SMD, 0.39 [CI, 0.66 to 0.11; I2 = 40%]) follow-up [37].

Mindfulness-Based Stress Reduction
Three trials (n = 40, 282, and 342) evaluated mindfulness-based stress reduction (8 weekly group sessions) for chronic low back pain [4547]. Two trials were rated as good quality [45, 47] and 1 as poor quality. In 1 trial, participants in a mindfulness-based stress reduction program had greater improvement in short-term back pain (difference, 0.64 point on a 0- to 10-pont numeric rating scale) and function (difference, 1.37 on the RDQ) at 26 weeks than those receiving usual care [45]. They also were more likely to have pain reduction of 30% or more (relative risk, 1.64 [CI, 1.15 to 2.34]) and better function (relative risk, 1.37 [CI, 1.06 to 1.77]). The effects on pain (difference, 0.85 point) but not function remained at 52 weeks. No differences were observed between mindfulness-based stress reduction and cognitive behavioral therapy. Another good-quality trial found that compared with an education intervention, mindfulness-based stress reduction led to a greater increase in function at 8 weeks (difference, 1.1 on the RDQ [CI, 2.1 to 0.01]) but no statistically significant effects on average pain intensity [46]; no differences were seen in average pain intensity or function at 6 months. The third trial, a small (n = 40) pilot study, also found mindfulness-based stress reduction to be superior to an education intervention for pain and function, although the researchers reported baseline differences in these measures [47].

Psychological Therapies
Thirty-two trials evaluated psychological therapies for chronic low back pain. Of these studies, 28 were included in a systematic review (n = 3,090; range, 18 to 409) [48], and we identified 4 additional trials (n = 976; range, 54 to 701) [4953]. The review classified 13 trials as low risk of bias; we rated all the others as fair quality.
The systematic review found that compared with wait-list control or no psychological therapy, progressive relaxation (3 trials: mean difference, 19.77 on a 0- to 100-point VAS [CI, 34 to 5.20]), electromyography biofeedback (3 trials: SMD, 0.80 [CI, 1.32 to 0.28]), operant therapy (3 trials: SMD, 0.43 [CI, 0.75 to 0.1]), and cognitive behavioral therapy (5 trials: SMD, 0.60 [CI, 0.97 to 0.22]) resulted in lower posttreatment pain intensity [48]. Only progressive relaxation was associated with beneficial effects on function (3 trials: SMD, 0.88 [CI, 1.36 to 0.39]). No clear differences in pain intensity were seen between psychological therapies and exercise therapy (2 trials) or in pain or function between psychological therapies plus physiotherapy and physiotherapy alone (6 trials) [48]. Ten trials found no clear differences among several psychological therapies [48].

Multidisciplinary Rehabilitation
Multidisciplinary rehabilitation was evaluated in 44 trials. Of these studies, 41 (n = 6,858; range, 20 to 542) were included in a systematic review [54], and we identified 3 others (n = 20, 20, and 70) [5557]. The systematic review classified 13 trials as low risk of bias; we rated 2 others as good quality and 1 as fair quality.
The systematic review found that patients with chronic low back pain who received multidisciplinary rehabilitation had lower short-term pain intensity than those who received usual care (9 trials: SMD, 0.55 [CI, 0.83 to 0.28]), no multidisciplinary rehabilitation (3 trials: SMD, 0.73 [CI, 1.22 to 0.24]), or nonmultidisciplinary physical therapy (12 trials: SMD, 0.30 [CI, 0.54 to 0.06]) [54]. On a numerical rating scale of 0 to 10 points, the differences were approximately 1.4 to 1.7 points versus usual care or no multidisciplinary rehabilitation and approximately 0.6 point versus nonmultidisciplinary physical therapy. Multidisciplinary rehabilitation also was associated with less short-term disability (9 trials: SMD, 0.41 [CI, 0.62 to 0.19; I2 = 58%]; 3 trials: SMD, 0.49 [CI, 0.76 to 0.22]; and 13 trials: SMD, 0.39 [CI, 0.68 to 0.10], respectively). On the RDQ, the differences were approximately 2.5 to 2.9 points versus usual care or no multidisciplinary rehabilitation and approximately 1.2 points versus nonmultidisciplinary physical therapy. Multidisciplinary rehabilitation also was associated with less long-term pain intensity and disability than usual care (7 trials: SMD, 0.21 [CI, 0.37 to 0.04], and 6 trials: SMD, 0.23 [CI, 0.40 to 0.06], respectively) and nonmultidisciplinary physical therapy (9 trials: SMD, 0.51 [CI, 1.04 to 0.01], and 10 trials: SMD, 0.68 [CI, 1.19 to 0.16], respectively) and with greater likelihood of return to work compared with nonmultidisciplinary rehabilitation (8 trials: odds ratio, 1.87 [CI, 1.39 to 2.53]), with no difference versus usual care (7 trials: odds ratio, 1.04 [CI, 0.73 to 1.47]). Two trials in patients with subacute low back pain reported findings consistent with those in patients with chronic symptoms [55, 56].

Acupuncture
Acupuncture was evaluated in 49 trials. Of these studies, 11 (n = 1,163; range, 40 to 300) were in a systematic review of acupuncture for acute or subacute low back pain [58] and 32 (n = 5,931; range, 16 to 2,831) in a systematic review of acupuncture for chronic low back pain [59], and we identified 6 additional trials (n = 864; range, 80 to 275) [6064]. The systematic reviews categorized 22% and 45% of trials as low risk of bias; we rated 3 additional trials as good, 2 as fair, and 1 as poor quality.
For acute low back pain, a systematic review found that acupuncture decreased pain intensity more than sham acupuncture with nonpenetrating needles (2 trials: mean difference, 9.38 on a 0-to 100-point VAS [CI, 1.76 to 17.0]) [58]. Two other trials reported inconsistent effects on pain intensity [61, 65]. Acupuncture had no clear effects on function (5 trials) [58, 61, 62]. Compared with nonsteroidal anti-inflammatory drugs, acupuncture was associated with a slightly greater likelihood of overall improvement at the end of treatment (5 trials: relative risk, 1.11 [CI, 1.06 to 1.16]).
For chronic low back pain, the systematic review found that acupuncture was associated with lower pain intensity (4 trials: SMD, 0.72 [CI, 0.94 to 0.49]) and better function (3 trials: SMD, 0.94 [CI, 1.41 to 0.47]) immediately after the intervention compared with no acupuncture [59]. Mean effects on pain ranged from 7 to 24 points on a 0- to 100-point scale; for function, 1 trial reported an 8-point difference on a 0- to 100-point scale and 2 trials reported differences of 0.8 and 3.4 points on the RDQ. In the long term, 2 trials showed small or no clear differences. Acupuncture also decreased pain intensity more than sham acupuncture immediately after the intervention (4 trials: WMD, 16.76 [CI, 33.3 to 0.19]) and through 12 weeks (3 trials: WMD, 9.55 [CI, 16.5 to 2.58]), with no differences in function. Five trials that could not be pooled or were not included in the review reported results consistent with these findings [60, 6669]. The systematic review found that compared with medications (nonsteroidal anti-inflammatory drugs, muscle relaxants, or analgesics), acupuncture resulted in greater pain relief (3 trials: WMD, 10.56 on a 0- to 100-point scale [CI, 20.34 to 0.78]) and better function (3 trials: SMD, 0.36 [CI, 0.67 to 0.04]) immediately after the intervention.

Massage
Massage was evaluated in 26 trials, 13 of which (n = 1,596; range, 39 to 262) were included in a systematic review [70]; we identified another 13 trials (n = 1,633; range, 15 to 579) [29, 7182]. The systematic review classified 6 trials as low risk of bias, and we rated 3 additional trials [29, 71, 72] as good quality.
For chronic low back pain, 1 trial found that structural or relaxation massage had small effects on the RDQ (mean, 2.0 to 2.9 points) versus usual care at 10 to 12 weeks, with smaller effects at 52 weeks [71]; however, another trial found no RDQ effects from massage (Swedish massage, soft tissue release, and stretching) versus usual care [29]. Three trials found no clear difference in pain or function between foot reflexology and usual care or sham (light foot) massage [79, 81, 83].
Compared with several noninvasive interventions (manipulation, exercise, relaxation therapy, acupuncture, physiotherapy, transcutaneous electrical nerve stimulation), massage had better effects on short-term pain in 8 of 9 trials (mean differences, 0.6 to 0.94 points on a 0- to 10-point scale) and short-term function in 4 of 5 trials [70, 82]. Comparisons of various massage techniques were heterogeneous, and estimates were imprecise [7174, 80, 84, 85].

Spinal Manipulation
Spinal manipulation was evaluated in 61 trials. Of these studies, 19 (n = 2,674; range, 36 to 323) were included in a systematic review of manipulation for acute low back pain [86] and 26 (n = 6,070; range, 29 to 1,334) in a systematic review of manipulation for chronic low back pain [87], and we identified an additional 16 trials (n = 2,382; range, 40 to 400) [18, 88102]. The reviews classified 15 trials as low risk of bias, and we rated 1 additional trial [102] as good quality.
For acute low back pain, 2 trials found that spinal manipulation had greater effects on function than sham manipulation (these differences were statistically significant in 1 trial); 1 trial found no statistically significant effects on pain [97, 103]. The systematic review found no differences in pain relief at 1 week between spinal manipulation and treatments considered inactive (an educational booklet, detuned ultrasound, detuned or actual short-wave diathermy, antiedema gel, or bed rest) (3 trials: WMD, 0.14 on a 0- to 10-point scale [CI, 0.69 to 0.96]), although 1 trial found an association between manipulation and greater pain relief at 3 months (mean difference, 1.20 [CI, 2.11 to 0.29]); no differences in function were seen at 1 week (2 trials) or 3 months (1 trial) [86]. In addition, no differences were observed in pain relief between patients receiving spinal manipulation and those receiving interventions considered active (primarily exercise, physical therapy, and back school) at 1 week (3 trials: WMD, 0.06 on a 0- to 10-point scale [CI, 0.53 to 0.65]) through 1 year (1 trial: mean difference, 0.40 [CI, 0.08 to 0.88]), nor were any effects on function noted. A subsequent trial reported similar findings [96].
For chronic low back pain, a systematic review showed that spinal manipulation had small, statistically nonsignificant effects on pain at 1 month compared with sham manipulation (3 trials: WMD, 3.24 [CI, 13.62 to 7.15 on a 0- to 100-point scale]); 1 trial reported similar results for function (SMD, 0.45 [CI, 0.97 to 0.06]) [87]. A trial not included in the systematic review reported results that generally were consistent with it [94]. Compared with other active interventions, manipulation was associated with better short-term pain relief at 1 month (10 comparisons from 6 trials: WMD, 2.76 on a 0- to 100-point scale [CI, 5.19 to 0.32]) and 6 months (7 comparisons from 4 trials: WMD, 3.07 [CI, 5.42 to 0.71]), although the magnitude of effects was below the small or slight threshold. No effect was observed at 12 months (3 trials: WMD, 0.76 [CI, 3.19 to 1.66]). Manipulation resulted in greater improvement in function than other active interventions at 1 month (10 comparisons from 6 trials: SMD, 0.17 [CI, 0.29 to 0.06]); the effects were smaller and no longer statistically significant at 6 and 12 months. Three trials not included in the systematic reviews reported consistent findings with it [18, 90, 93].
For radicular low back pain, 1 good-quality trial found that spinal manipulation plus home exercise and advice resulted in greater improvement in leg and back pain at 12 weeks than home exercise and advice alone (mean difference, about 1 point on a 0- to 10-point scale); the effects were smaller (0.3 to 0.7 points) and not statistically significant at 52 weeks [99].

Harms
Across interventions, no serious harms were noted, although the reporting of harms was suboptimal. Typical harms reported were temporary increases in low back pain or other local effects (such as pain or bleeding from insertion of acupuncture needles).
Discussion

Table 2

Table 3

Table 4 Some evidence supports the effectiveness of several nonpharmacologic therapies for chronic low back pain (Table 2 and Supplement Table 5), and limited evidence shows that acupuncture is effective for acute low back pain (Table 3 and Supplement Table 6). These benefits generally were seen for short-term pain (usually <3 months and often immediately after the intervention) and of small (5 to 10 points on a 100-point VAS) to moderate (10 to 20 points) magnitude, on the basis of the ACP/APS categories [104]. Function was reported less consistently than pain, and effects typically were smaller or not observed. Exercise and multidisciplinary rehabilitation were associated with an increased likelihood of return to work. As described in the full report [5], evidence on other outcomes (such as quality of life, mood, analgesic use, and health care use) was sparse. Evidence on the effectiveness of nonpharmacologic therapies for radiculopathy was very limited (Table 4). Few clear differences were seen between various nonpharmacologic therapies in head-to-head trials, but evidence for most comparisons was limited.
This report updates and expands on the earlier ACP/APS review [105] with additional interventions and newer evidence. We found evidence that mindbody interventions not previously addressed tai chi (SOE, low) and mindfulness-based stress reduction (SOE, moderate) [4547] are effective for chronic low back pain; the new evidence also strengthens previous conclusions regarding yoga effectiveness (SOE, moderate). For interventions recommended as treatment options in the 2007 ACP/APS guideline [2], our findings were generally consistent with the prior review. Specifically, exercise therapy, psychological therapies, multidisciplinary rehabilitation, spinal manipulation, massage, and acupuncture are supported with some evidence of effectiveness for chronic low back pain (SOE, low to moderate). Unlike our previous report, which stated that higher-intensity multidisciplinary rehabilitation seemed to be more effective than lower-intensity programs, a stratified analysis based on currently available evidence [54] did not find a clear intensity effect. Our findings generally are consistent with recent systematic reviews not included in our evidence synthesis [106117]. Although harms were not well-reported, serious adverse events were not described.
As detailed in the full report, we found little evidence to support the use of most passive physical therapies (such as interferential therapy, short-wave diathermy, traction, ultrasound, lumbar supports, taping, and electrical muscle stimulation) for low back pain [5]. Exceptions were superficial heat, which was more effective than a nonheated control for acute or subacute low back pain (SOE, moderate), and low-level laser therapy, which was more effective than sham laser for pain (SOE, low) [118120].
We categorized the magnitude of effects for pain and function by using the thresholds in the ACP/APS review. Effects classified as small (for example, 5 to 10 points on a 0- to 100-point scale for pain or function) are below some proposed minimum thresholds for clinically important differences (such as 15 points on a 0- to 100-point VAS for pain, 2 points on a 0- to 10-point numerical rating scale for pain or function, 5 points on the RDQ, and 10 points on the Oswestry Disability Index) [12]. Factors that may support the use of interventions associated with small effects include low risk for harms, low costs, and strong patient preferences. The magnitude of effects may vary depending on baseline severity [121]; most trials enrolled patients with at least moderate pain (for example, rated as >5 on a 0- to 10-point numeric rating scale).
Our findings have implications for clinical practice. Current guidelines do not include mindfulness-based stress reduction, which was as effective as cognitive behavioral therapy for chronic low back pain [45]. Recent guidelines recommend nonopioid over opioid therapy for chronic pain; yet access to and reimbursement for certain nonpharmacologic therapies remain limited [122, 123]. For acute low back pain, most patients improve with or without therapy. Therefore, strategies that target effective therapies to patients at higher risk for chronicity may be most efficient [124].
Our review had limitations. Because of the large number of interventions, reviewing all of the primary literature was not feasible. We included higher-quality, recent systematic reviews that were most relevant to the review scope [125], supplemented with additional primary trials. We did not update meta-analyses reported in systematic reviews, but we qualitatively evaluated the consistency of results from new trials against pooled estimates. We excluded nonEnglish-language articles and did not search for abstract-only publications. We were limited in our ability to assess for publication bias because of the small numbers of trials for most comparisons, methodological limitations, and study heterogeneity. We did not address some nonpharmacologic interventions, including education [126, 127], advice to remain active [126, 128], mattresses, and shoe insoles [129], or compare nonpharmacologic therapies with surgical or interventional procedures.
Limitations also existed in the evidence base. Effects on pain and function typically were reported as mean differences at or shortly after intervention, making it difficult to determine whether benefits were sustained. Few studies reported the likelihood of clinically significant improvements [130]. For each intervention, trials were heterogeneous regarding the techniques used, the number of treatment sessions, and the duration or intensity of sessions. For example, acupuncture trials varied in needling sites; the length, number, and duration of acupuncture sessions; and the type of sham treatment (for example, nonpenetrating needles at the acupuncture site vs. penetrating needles at the nonacupuncture site) [58, 59]. For many nonpharmacologic interventions, effectively blinding patients or care providers to treatments is difficult, so some observed effects might have been the result of nonspecific effects related to needling, massage, manipulation, or other treatment administration aspects (such as attentional or placebo effects) [131, 132].
In conclusion, several nonpharmacologic therapies for low back pain were associated with small to moderate, primarily short-term effects on pain. Effects on function generally were smaller than those on pain, and most evidence was for chronic low back pain. New evidence supports the effectiveness of mindbody interventions. More research is needed to identify effective nonpharmacologic treatments for radicular and acute low back pain and to understand the incremental benefits of combining interventions, as well as which treatment combinations and sequences are most effective.
References:Please refer to the Full Text
NOTE: They will open in a separate screen
Just click on REFERENCES on the left-side of the screen.

Return to LOW BACK PAIN
Return to LOW BACK GUIDELINES
Return to SPINAL PAIN MANAGEMENT
Return NON-PHARMACOLOGIC THERAPY
Return to PRESCRIPTION RIGHTS DEBATE
Since 8-12-2008


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |