

Opioid Use Among Veterans of Recent Wars
Receiving Veterans Affairs Chiropractic CareThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Pain Medicine 2018 (Sep 1); 19 (suppl_1): S54–S60 ~ FULL TEXT
OPEN ACCESS Anthony J Lisi, DC, Kelsey L Corcoran, DC, Eric C DeRycke, MPH, Lori A Bastian, MD, MPH, William C Becker, MD, Sara N Edmond, PhD, Christine M Goertz, DC, PhD et al.
Pain Research, Informatics,
Multimorbidities and Education (PRIME) Center,
VA Connecticut Healthcare System,
West Haven, Connecticut.OBJECTIVE: To examine patient sociodemographic and clinical characteristics associated with opioid use among Veterans of Operations Enduring Freedom/Iraqi Freedom/New Dawn (OEF/OIF/OND) who receive chiropractic care, and to explore the relationship between timing of a chiropractic visit and receipt of an opioid prescription.
METHODS: Cross-sectional analysis of administrative data on OEF/OIF/OND veterans who had at least one visit to a Veterans Affairs (VA) chiropractic clinic between 2004 and 2014. Opioid receipt was defined as at least one prescription within a window of 90 days before to 90 days after the index chiropractic clinic visit.
RESULTS: We identified 14,025 OEF/OIF/OND veterans with at least one chiropractic visit, and 4,396 (31.3%) of them also received one or more opioid prescriptions. Moderate/severe pain (odds ratio [OR] = 1.87, 95% confidence interval [CI] = 1.72-2.03), PTSD (OR = 1.55, 95% CI = 1.41-1.69), depression (OR = 1.40, 95% CI = 1.29-1.53), and current smoking (OR = 1.39, 95% CI = 1.26-1.52) were associated with a higher likelihood of receiving an opioid prescription. The percentage of veterans receiving opioid prescriptions was lower in each of the three 30-day time frames assessed after the index chiropractic visit than before.
CONCLUSIONS: Nearly one-third of OEF/OIF/OND veterans receiving VA chiropractic services also received an opioid prescription, yet the frequency of opioid prescriptions was lower after the index chiropractic visit than before. Further study is warranted to assess the relationship between opioid use and chiropractic care.
KEYWORDS: inter-rater reliability; ergonomics; work demands; observation
From the FULL TEXT Article:
Introduction
Current clinical practice guidelines recommend specific nonpharmacological therapies as front-line treatments ahead of pharmacological treatment for the management of low back pain [1], neck pain [2], and osteoarthritis of the hip, knee, and hand. [3, 4] For military and veteran populations, the recent joint Department of Health and Human Services/Department of Defense/Department of Veterans Affairs (VA) Pain Management Collaboratory identified nonpharmacological approaches to pain management as a national research priority. [5] For the VA in particular, a 2016 VA Health Services Research and Development State of the Art conference on nonpharmacological treatments for pain recommended broader uptake of a group of evidence-based nonpharmacological therapies. A key set of the recommend therapies—spinal manipulation, massage, acupuncture, exercise, and patient education—are the core components of multimodal chiropractic care in the VA.
The VA began providing chiropractic services on-site at select medical facilities in 2004 and has expanded implementation each year thereafter. [6] Apart from the potential to reduce pain and improve function in patients with musculoskeletal conditions, chiropractic care may have an impact on opioid use in such patients. Prior work has presented a negative correlation between chiropractic use and opioid use in employer health plan, [7, 8] workers’ compensation [9], and Medicare [10] populations.
In recent years, the VA has seen initial success in reducing opioid use. From 2012 to 2016, the number of veterans receiving an opioid for any reason decreased approximately 25%, and one component of the VA’s approach has been expanding access to nonpharmacological pain therapies. [11]
Little is known about the use of opioids specifically among chiropractic patients in the VA. A case series found that 39% of veterans of Operations Enduring Freedom/Iraqi Freedom/New Dawn (OEF/OIF/OND) receiving care at one VA chiropractic clinic had received opioid therapy before initiating chiropractic treatment for the same condition. [12] As reduction in opioid use remains a national priority, a better understanding of the relationship between opioid use and chiropractic services is needed to inform research and policy efforts aimed to assess and/or optimize the delivery of chiropractic care in the VA.
The purpose of this study was to assess patient sociodemographic and clinical characteristics associated with opioid use among OEF/OIF/OND veterans who receive VA chiropractic care and to explore the relationship between timing of a chiropractic visit and receipt of an opioid prescription. It was hypothesized that rates of opioid use would be higher before and lower after an initial chiropractic visit.
Methods
Study Design/Population
This work is a cross-sectional analysis of VA administrative data. The study population is the OEF/OIF/OND roster, provided to the VA by the Department of Defense Manpower Data Center’s (DMDC’s) Contingency Tracking System. The roster is a list of veterans who separated from OEF/OIF/OND military service and enrolled in VA health care between October 1, 2001, and September 30, 2014. Our analyses included only veterans with one or more VA chiropractic visits starting in 2004, the year that the VA began providing these services. The study was approved by the institutional review board of the VA Connecticut Healthcare System.
Data Sources
The DMDC roster includes information on veterans’ gender, race/ethnicity, date of birth, date of last deployment, branch of service (Army, Navy, Air Force, or Marine Corps), component (National Guard, Reserve, or active duty), and rank (officer, including warrant officer, or enlisted). All roster data were current at the time of separation from military service. Data on eligible veterans were linked to VA administrative and clinical data contained within the Corporate Data Warehouse (CDW). These databases provide a record of inpatient and outpatient health care encounters including patient demographics, clinic visits, medication prescriptions, and other health care services.
Variable of Interest: Opioid Receipt
We defined opioid receipt as at least one filled prescription for opioids in the VA within a window of 90 days before to 90 days after the index chiropractic clinic visit. Opioid medications included formulations from the CN101 VA drug class such as butorphanol, codeine, dihydrocodeine, fentanyl, hydrocodone, hydromorphone, levorphanol, meperidine, morphine, nalbuphine, opium, oxycodone, oxymorphone, pentazocine, propoxyphene, and tapentadol. Buprenorphine and methadone were excluded as they are predominantly used to treat opioid use disorder. Although in some cases methadone may have been used to manage pain, we decided to exclude it so that we did not capture cases in which it was being used for substance use disorder in the absence of pain.
CovariatesDemographics Demographic variables including age, gender, and race/ ethnicity (i.e., black, Hispanic, other/unknown, white) were examined.
Pain-Related Variables Veterans presenting to VA clinics are screened for the presence and intensity of pain using a 0–10 numerical rating scale (NRS). Veterans are asked to “rate your current pain on a 0 (no pain) to 10 (worst pain imaginable)” scale, and the response is recorded in a data field in the electronic health record (EHR). We selected the highest current pain intensity (within+/–90 days of the index chiropractic visit). The highest score was chosen rather than an average of multiple scores to maximize subject data capture in instances when only one pain score was recorded. Pain intensity was categorized as none or mild (0–3) and moderate or severe (4–10). [13]
Mental Health Conditions The Agency for Healthcare Research and Quality’s Clinical Classifications Software International Classification of Disease (ICD-9) codes were used to identify mental health conditions. [14] We examined the following conditions based on their relatively high prevalence in veteran populations and their frequent comorbidity with painful conditions: mood disorders (i.e., major depressive disorder, depressive disorder not otherwise specified, dysthymia, bipolar disorder); post-traumatic stress disorder (PTSD); substance use disorders, including alcohol or drug use; and traumatic brain injury (TBI). ICD-9 codes for mental health conditions were collected if they appeared at any time in the veteran’s VA medical record.
Body Mass Index Body mass index (BMI; kg/m2) was extracted+/–90 days from chiropractic consultation using the height and weight recorded in the EHR. Using standard classification, veterans were categorized as obese (BMI ≥30 kg/m2) or nonobese (BMI<30 kg/m2. [15].
Smoking The most recent smoking status was collected. Smoking status was determined using methodology from McGinnis et al. that uses EHR Health Factors Smoking data from clinical reminders. Veterans were categorized as never, former, or current smokers using a comprehensive algorithm using key words (e.g., current smoker, never smoker, tobacco counseling) found in text entries and results from clinical reminders in CDW. [16] McGinnis et al. [16] found high agreement between EHR Health Factors smoking data and survey results.
Benzodiazepine Benzodiazepine receipt was collected during the period+/ – 90 days from the index chiropractic visit and was defined as at least one filled prescription in that time frame.
Analysis
The associations between opioid prescription receipt and demographics/comorbidities were examined among veterans who were seen at the chiropractic clinic. Chi-square tests were run for categorical data; t tests and Wilcoxon rank-sum tests were used for continuous variables. Multivariate logistic regression analyses were used to examine the association of pain-related variables on use of opioids, controlling for potential confounders such as age, gender, mental health diagnoses, smoking status, pain intensity, and BMI. We calculated the frequency of opioid prescription receipt within three 30-day windows before and three after the index chiropractic visit.
Results
We identified 14,025 OEF/OIF/OND veterans with at least one VA chiropractic visit. The majority of these veterans were male (84.1%) and white (68.7%), and the average age of the sample was 38 years. In terms of health status, 56.2% reported moderate to severe pain intensity, 54.2% had been disagnosed with PTSD, 47.6% had a diagnosis associated with depression, 33.8% were current smokers, 19.8% had a substance use disorder diagnosis, and the sample generally was overweight (average BMI = 29.8 kg/m2).

Table 1
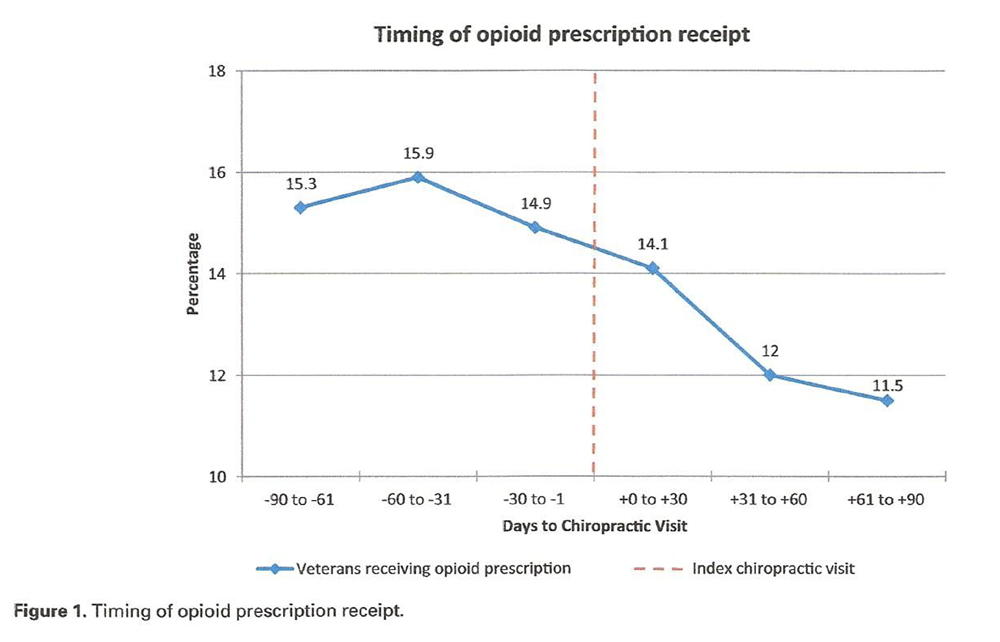
Figure 1

Table 2 Overall, 4,396 (31.3%) of these veterans received an opioid prescription within +/– 90 days of the initial chiropractic visit. The most commonly prescribed opioid was hydrocodone (42.7%), followed by tramadol (33.4%) and oxycodone (13.2%). Additional patient characteristics are organized by opioid receipt+/–90 days of chiropractic visit in Table 1.
The percentages of veterans receiving opioid prescriptions tended to be higher in each of the 30-day windows before the index chiropractic visit than in any of the 30- day windows after the visit. As seen in Figure 1, this ranged from a high of 15.9% at –60 to –31 days to a low of 11.5% at+61 to+90 days.
Several factors were associated with a higher likelihood of receiving an opioid prescription, includingmoderate to severe pain (odds ratio [OR] = 1.87, 95% confidence interval [CI] = 1.72–2.03),
PTSD (OR = 1.55, 95% CI = 1.41–1.69),
depression (OR = 1.40, 95% CI = 1.29–1.553), and
current smoking (OR = 1.39, 95% CI = 1.26–1.52).Additional factors associated with a higher likelihood of receiving an opioid are included in Table 2.
Discussion
First, our results demonstrate that veterans of recent wars receiving VA chiropractic services have a high illness burden. Moderate to severe pain, mental health conditions, and negative health characteristics were common. This is consistent with previous work showing that the overall population of veterans of recent wars has a high prevalence of musculoskeletal and mental health disorders [17], and the overall VA chiropractic patient population is most commonly seen for management of musculoskeletal disorders. [6]
Almost one-third of our sample received an opioid prescription around the time of receiving VA chiropractic services. This is consistent with prior reports of opioid prescription frequency in OEF/OIF/OND patients with noncancer pain, which have ranged from 23% to 41%. [19, 20]
Several factors were associated with an increased likelihood of OEF/OIF/OND veterans receiving an opioid prescription within +/- 90 days of presenting to chiropractic services. Male gender was associated with a higher likelihood of an opioid prescription in our sample, which is consistent with prior research demonstrating that women veterans with persistent pain are less likely to initiate chronic opioid therapy. [21] Data from the civilian population demonstrate that individuals who are white [22, 23] and who have higher severity pain complaints [23] are more likely to be prescribed opioids, consistent with our sample population. We also found obesity to be associated with opioid receipt. In a prior study of OEF/OIF/OND veterans, obesity was associated with persistent pain. [24] However, a recent study of all veterans receiving care at one VA chiropractic clinic found that 36.5% and 48.9% of patients were overweight or obese, but neither overweight nor obese was associated with an objective measure of pain severity or function. [25]
Both current and former cigarette smoking were associated with opioid receipt in the sample population, with a higher likelihood of receiving an opioid for current smokers than former smokers. Previous work has shown that opioid receipt was correlated with smoking status for OEF/OIF/OND veterans. [26] In the civilian population, tobacco use is associated with an increased likelihood of opioid receipt [27–30], and individuals reporting both cigarette smoking and chronic pain are more likely to receive opioids. [31–33]
Participants with PTSD had a higher rate of opioid use, which is consistent with substantial literature supporting this relationship. [19, 31] Depression, PTSD, and pain may share biological mechanisms, and these conditions may be influenced by similar psychosocial factors, such as lower socioeconomic status, disability, and motivation to engage with health care. [34]
The percentage of veterans receiving opioid prescriptions was lower in each of the three 30-day time frames assessed after the index chiropractic visit than before. Our work did not attempt to assess causation or otherwise explain this observation. Veterans may have been referred to chiropractic care as part of an opioid taper plan, or those who agreed to chiropractic care may have been inherently less likely to seek opioid prescriptions. However, it is also possible that the delivery of chiropractic care may have been a substitute for opioid use in our sample, which raises interesting research, policy, and practice considerations as the VA continues to expand chiropractic services. This is particularly relevant in light of other work that has shown a negative correlation between chiropractic use and opioid use in private sector populations.
A study of administrative claims data from three employer health plans identified 13,760 patients with episodes of mechanical low back pain (LBP), almost half (45%) of whom used narcotic medications, yet patients who used chiropractic services were less likely to take narcotic medications within seven days after services compared with patients who did not use chiropractic services. [7] A claims database review of a one-year period from the University of Pittsburg Medical Center Health Plan identified 17,148 patients who had services for LBP. Receiving physical therapy, spinal injections, magnetic resonance imaging or computed tomography, and emergency room services was positively associated with opioid use, whereas receiving chiropractic services was negatively associated with opioid use (OR=0.5). [9]
In a population-based study of injured workers in Washington State over a three-year period, Hispanic ethnicity and seeing a chiropractor at the time of injury were the only factors associated with lower odds of long-term opioid use. Both were substantial negative predictors, yet patients seeing chiropractors were even less likely (OR=0.29, 95% CI=0.10–0.84) than Hispanic patients (OR=0.42, 95% CI=0.19–0.92) to use long-term opioids. [35] A time-series analysis of administrative data from a self-insured workforce at a US manufacturing company identified 14,787 episodes of spinal pain conditions (mixed lumbar, thoracic, and/or cervical), in which patients receiving chiropractic services had the lowest rate of opioid use, as well as the lowest use of six other classes of medications, compared with patients receiving complex medical management, physical therapy, or advice. [8] Lastly, an analysis of 2011 Medicare Part B data found that a higher regional per-capita supply of chiropractors and spending on chiropractic manipulative therapy were strongly inversely correlated with the percentage of younger, disabled Medicare beneficiaries receiving opioid prescriptions. [10]
Our results add to the existing literature and illustrate the need for further work to assess the relationship between chiropractic use and opioid use in VA populations, particularly the impact of sequencing the initiation of these therapies. Comparison of chiropractic use over time can help assess this in light of general changes in opioid prescription trends. Future work should also aim to identify the optimal situations (patient factors, disease factors, treatment timing, and dosage) in which chiropractic care is more likely to be a replacement for, rather than an addition to, opioid therapy for chronic musculoskeletal pain conditions in the VA. Even while further research is needed, our results, along with the previous literature, suggest that expanding access to chiropractic care should be a key policy consideration for the VA, congruent with national initiatives aimed to increase the use of evidence-based nonpharmacological treatments for chronic musculoskeletal pain.
There are several limitations to our findings. Veterans from recent wars included for analysis had to have at least one visit to both VA primary care and chiropractic services. These results may not be generalizable to veterans of other service eras and veterans who have not accessed VA care.
This study is a cross-sectional examination, which inherently limits our ability to make any claims about causation. In this preliminary work, we did not assess dose and duration of opioid use, and these should be included in subsequent studies. The exclusion of buprenorphine and methadone from the opioid medications included in our study means that data were not captured from individuals receiving buprenorphine and methadone for pain management.
The pain intensity analyzed was a one-time collection of highest pain score within+/- 90 days of our index chiropractic visit; therefore, the precise pain scores on the day of the chiropractic visit and/or the day of opioid prescription receipt are unknown. We did not assess the specific diagnoses associated with the chiropractic visits in our sample; however, previous work has shown that VA chiropractic patients are seen overwhelmingly for low back and/or neck musculoskeletal pain conditions. [6]
Conclusion
Nearly one-third of OEF/OIF/OND veterans receiving VA chiropractic services also received an opioid prescription, yet the frequency of opioid prescriptions was lower in each of the three 30-day time frames assessed after the index chiropractic visit than before. Factors associated with an increased likelihood of receiving an opioid around the time of a chiropractic visit included moderate to severe pain, diagnoses of PTSD and/or depression, and current smoking.
Funding sources:
This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, and Health Services Research and Development IIR 12-118, CIN 13-407, and by the Palmer College Foundation, the NCMIC Foundation, and with resources from and the use of facilities at the VA Connecticut Healthcare System.
Disclosures:
The views expressed in this manuscript are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
Conflicts of interest:
There are no conflicts to disclose.
Prior presentations:
Presented at the 2018 International Congress on Integrative Medicine and Health, May 8-11, 2018, Baltimore, MD.
References:
Qaseem A, Wilt TJ, McLean RM, Forciea MA;
Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain:
A Clinical Practice Guideline From the American College of Physicians
Annals of Internal Medicine 2017 (Apr 4); 166 (7): 514–530Cote P, Wong JJ, Sutton D, et al.
Management of Neck Pain and Associated Disorders: A Clinical Practice Guideline
from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration
European Spine Journal 2016 (Jul); 25 (7): 2000–2022Bruyere O, Cooper C, Pelletier JP, et al.
An algorithm recommendation for the management of knee osteoarthritis in Europe and internationally:
A report from a task force of the European Society for Clinical and Economic Aspects of
Osteoporosis and Osteoarthritis (ESCEO).
Semin Arthritis Rheum 2014;44(3):253–63.Hochberg MC, Altman RD, April KT, et al.
American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic
therapies in osteoarthritis of the hand, hip, and knee.
Arthritis Care Res (Hoboken) 2012;64 (4):465–74.Department of Health and Human Services.
NIHDoD- VA Pain Management Collaboratory—Pragmatic Clinical Trials Demonstration Projects (UG3/UH3).
Bethesda, MD: Department of Health and Human Services, Department of Defense,
Department of Veterans Affairs; 2016. Available at:
https://grants.nih.gov/grants/guide/rfa-files/RFA-AT-17-001.html
(accessed December 2017).Lisi AJ, Brandt CA.
Trends in the Use and Characteristics of Chiropractic Services
in the Department of Veterans Affairs
J Manipulative Physiol Ther. 2016 (Jun); 39 (5): 381–386Rhee Y, Taitel MS, Walker DR, Lau DT.
Narcotic drug use among patients with lower back pain in employer health plans:
A retrospective analysis of risk factors and health care services.
Clin Ther 2007; 29(Suppl):2603–12.Allen, H, Wright, M, Craig, T et al.
Tracking Low Back Problems in a Major Self-Insured Workforce:
Toward Improvement in the Patient's Journey
J Occup Environ Med. 2014 (Jun); 56 (6): 604-620Vogt MT, Kwoh CK, Cope DK, et al.
Analgesic usage for low back pain: Impact on health care costs and service use.
Spine (Phila Pa 1976) 2005;30 (9):1075–81.Weeks WB, Goertz CM.
Cross-Sectional Analysis of Per Capita Supply of Doctors of Chiropractic
and Opioid Use in Younger Medicare Beneficiaries
J Manipulative Physiol Ther 2016 (May); 39 (4): 263–266Gellad WF, Good CB, Shulkin DJ.
Addressing the opioid epidemic in the United States: Lessons from the Department of Veterans Affairs.
JAMA Intern Med 2017;177(5):611–2.A.J. Lisi,
Management of Operation Iraqi Freedom and Operation Enduring Freedom
Veterans in a Veterans Health Administration Chiropractic Clinic: A Case Series
J Rehabil Res Dev. 2010; 47 (1): 1–6Goulet JL, Brandt C, Crystal S, et al.
Agreement between electronic medical record-based and self-administered pain numeric rating scale:
Clinical and research implications.
Med Care 2013;51 (3):245–50.Elixhauser A, Steinder C, Palmer L.
Clinical Classifications Software (CCS) for ICD-9-CM.
Rockville, MD: Agency for Healthcare Research and Quality; 2008. Available at:
https://hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp
(accessed December 2017).Centers for Disease Control and Prevention.
Healthy Weight: About Adult BMI. Atlanta, GA: Centers for Disease Control and Prevention; 2017. Available at:
https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html
(accessed December 2017).McGinnis KA, Brandt CA, Skanderson M, et al.
Validating smoking data from the Veteran’s Affairs Health Factors dataset, an electronic data source.
Nicotine Tob Res 2011;13(12):1233–9.US Department of Veterans Affairs.
Analysis of VA Health Care Utilization Among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF),
and Operation New Dawn (OND) Veterans.
Washington, DC: Veterans Health Administration; 2017. Available at:
https://www.publichealth.va.gov/docs/epidemiology/healthcare-utilization-report
-fy2015-qtr3.pdf
(accessed January 2018).Han L, Allore H, Goulet J, et al.
Opioid dosing trends over eight years among US Veterans with musculoskeletal disorders after returning from
service in support of recent conflicts.
Ann Epidemiol 2017;27 (9):563–9.e3.Edlund MJ, Austen MA, Sullivan MD, et al.
Patterns of opioid use for chronic noncancer pain in the Veterans Health Administration from 2009 to 2011.
Pain 2014;155(11):2337–43.Hudson TJ, Painter JT, Martin BC, et al.
Pharmacoepidemiologic analyses of opioid use among OEF/OIF/OND veterans.
Pain 2017;158(6):1039–45.Dobscha SK, Morasco BJ, Duckart JP, Macey T, Deyo RA.
Correlates of prescription opioid initiation and long-term opioid use in veterans with persistent pain.
Clin J Pain 2013;29(2):102–8.Tamayo-Sarver JH, Hinze SW, Cydulka RK, Baker DW.
Racial and ethnic disparities in emergency department analgesic prescription.
Am J Public Health 2003;93(12):2067–73.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R.
Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments.
JAMA 2008;299(1):70–8.Higgins DM, Kerns RD, Brandt CA, et al.
Persistent pain and comorbidity among operation enduring Freedom/Operation Iraqi Freedom/
operation New Dawn veterans.
Pain Med 2014;15(5):782–90.Okamoto CS, Dunn AS, Green BN, Formolo LR, Chicoine D.
Correlation of body composition and low back pain severity in a cross-section of US veterans.
J Manipulative Physiol Ther 2017;40(5):358–64.Bastian LA, Driscoll MA, Heapy AA, et al.
Cigarette smoking status and receipt of an opioid prescription among veterans of recent wars.
Pain Med 2017;18 (6):1089–97.Krebs EE, Bair MJ, Damush TM, et al.
Comparative responsiveness of pain outcome measures among primary care patients with musculoskeletal pain.
Med Care 2010;48(11):1007–14.Tetrault JM, Desai RA, Becker WC, et al.
Gender and non-medical use of prescription opioids: Results from a national US survey.
Addiction 2008;103(2):258–68.Skurtveit S, Furu K, Selmer R, Handal M, Tverdal A.
Nicotine dependence predicts repeated use of prescribed opioids. Prospective population-based cohort study.
Ann Epidemiol 2010;20(12):890–7.Stover BD, Turner JA, Franklin G, et al.
Factors associated with early opioid prescription among workers with low back injuries.
J Pain 2006;7(10):718–25.Hooten WM, Shi Y, Gazelka HM, Warner DO.
The effects of depression and smoking on pain severity and opioid use in patients with chronic pain.
Pain 2011;152(1):223–9.Hooten WM, Townsend CO, Bruce BK, Warner DO.
The effects of smoking status on opioid tapering among patients with chronic pain.
Anesth Analg 2009;108(1):308–15.Hooten WM, Townsend CO, Bruce BK, Shi Y, Warner DO.
Sex differences in characteristics of smokers with chronic pain undergoing multidisciplinary pain rehabilitation.
Pain Med 2009;10(8):1416–25.Bair MJ, Robinson RL, Katon W, Kroenke K.
Depression and pain comorbidity: A literature review.
Arch Intern Med 2003;163(20):2433–45.Franklin GM, Rahman EA, Turner JA, Daniell WE, Fulton-Kehoe D.
Opioid use for chronic low back pain: A prospective, population-based study among injured workers
in Washington state, 2002-2005.
Clin J Pain 2009;25(9):743–51.
Return to CHIROPRACTIC CARE FOR VETERANS
Since 3-09-2020


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |
