

Overcoming Overuse:
Improving Musculoskeletal Health CareThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Orthop Sports Phys Ther 2020 (Mar); 50 (3): 113–115 ~ FULL TEXT
OPEN ACCESS Joshua R Zadro, Simon Décary, Mary O'Keeffe, Zoe A Michaleff, Adrian C Traeger
School of Public Health,
Sydney Medical School,
The University of Sydney,
Camperdown, Australia.
This is the first article in a series on "Overcoming Overuse" in musculoskeletal health care. Overuse is the use of services that are unlikely to improve patient outcomes, result in more harm than benefit, and would not be desired by an informed patient. The Overcoming Overuse series explores the myriad ways diagnostic tests and treatments are overused in musculoskeletal health care, and proposes ways to ensure patients receive appropriate care. We focus on strategies to promote guideline-concordant care in rehabilitation practice and strategies to overcome overuse.
Keywords: musculoskeletal; overuse; physical therapy.
From the FULL TEXT Article:
Background
Care for musculoskeletal conditions is evolving. For more than 2 decades, clinical practice guidelines for conditions such as knee pain and low back pain recommended medication as first-line care, then surgery for selected patients who did not respond. Current recommendations now prioritize nonpharmacological interventions. Advice and exercise for musculoskeletal conditions, such as low back pain and hip and knee osteoarthritis, have replaced medication as first-line care, and some surgical procedures are actively discouraged. [11] What prompted the changes to recommendations? An increase in high-quality research evidence and awareness of the harms of overuse. [2, 10]
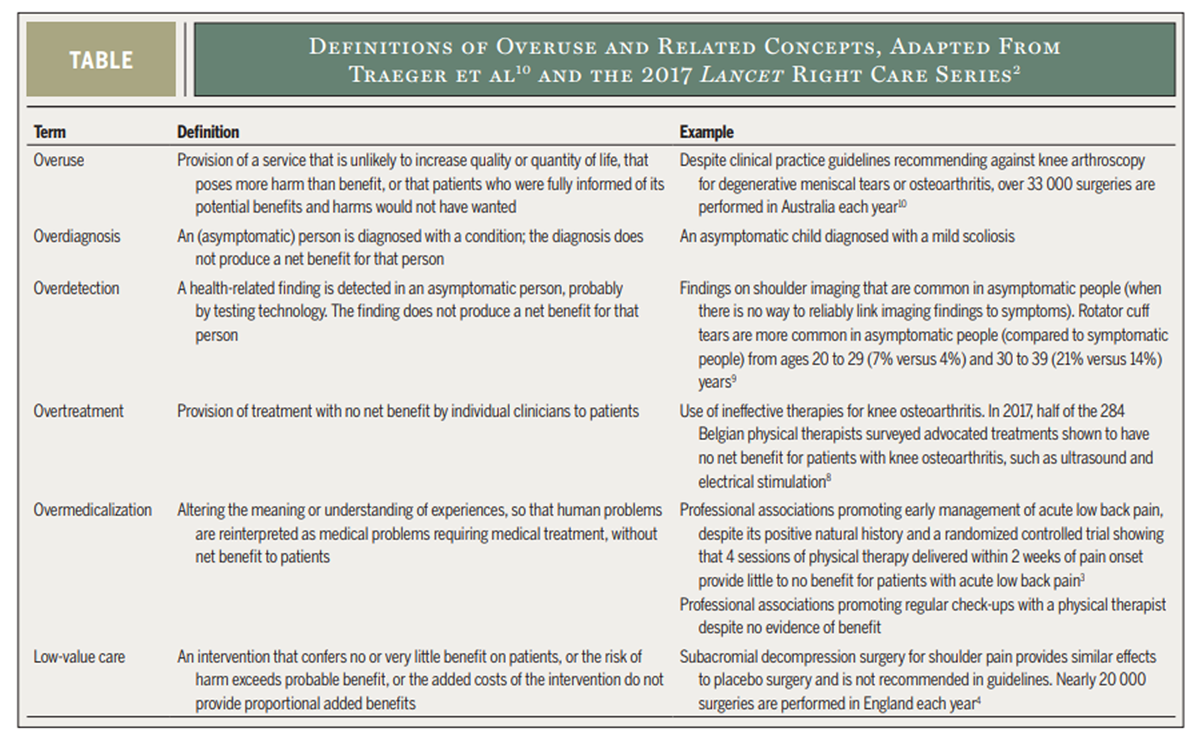
Table Overuse of health care is the use of services that have no net benefit or cause harm. [2, 10] Overuse includes overlapping concepts of low-value care and overtreatment (TABLE). Changes in clinical practice guidelines provide an unprecedented opportunity for physical therapists to prevent overuse and lead the evidence-based management of musculoskeletal conditions. In the “Overcoming Overuse” series, we explore the evidence of overuse in musculoskeletal health care and propose potential solutions.
Global Awareness of Overuse in Musculoskeletal Care
Greater awareness of the enormous waste due to overuse (estimated to be as high as 30% of total health care spending) [1] has spurred global initiatives to tackle the issue. For example, Choosing Wisely (http://www.choosingwisely.org) aims to reduce overuse by engaging with professional bodies to publish their own “do-not-do” lists of tests and treatments. There are over 150 Choosing Wisely recommendations that focus on musculoskeletal conditions (eg, low back pain, knee osteoarthritis, shoulder pain, rheumatoid arthritis).
Opportunity cost is an important consequence of overuse. Today, finite health care resources are being used to fund ineffective (eg, knee arthroscopy) and unproven health services for musculoskeletal conditions (eg, opioids for acute low back pain). [1] These funds could be better spent on services known to improve musculoskeletal health (eg, exercise and weight-loss programs for knee osteoarthritis). Overuse compounds when ineffective or unproven health services crowd out recommended care.
The CareTrack study in Australia monitored 35,573 health care encounters and found that only 43% of patients with osteoarthritis and 72% with low back pain received recommended care when they visited a health care professional. [6] There were similar results in the United States (57% for osteoarthritis and 68% for low back pain). [5] We found that 1 in every 3 physical therapists across 19 countries did not provide recommended care for common musculoskeletal conditions, such as back pain, knee osteoarthritis, and ankle sprains. [11] However, it is difficult to disentangle overuse from these numbers. We will explore the challenge of directly measuring overuse later in this series.
Physical Therapy: Friend or Foe?
As the physical therapy profession grows and clinical practice guidelines increasingly encourage people to seek nonpharmacological care, [11] it is vital to consider how physical therapists can help prevent overuse. In the United States, there are nearly 250,000 physical therapists, and the profession is estimated to grow 28% within the next 10 years. In Australia, there are now more practicing physical therapists than general practitioners, and 1 in 10 Australians visit a physical therapist each year. Growth in the physical therapy workforce will undoubtedly raise awareness of the profession, and may drive use of physical therapy services. This is an important opportunity for physical therapists to draw from the large evidence base that underpins the profession to improve the quality of the musculoskeletal health care they provide.
While physical therapy treatment may be less expensive and carry fewer risks than imaging, surgery, and opioids, the value of the care provided is critical. The annual cost of physical therapy is estimated at $1 billion in Australia and over $25 billion in the United States. [11] If physical therapists do not provide recommended care, it is possible that increased emphasis on nonpharmacological care could reduce overuse in one area (eg, surgery) but create overuse in another (eg, electrophysical agents for low back pain).
One in 4 physical therapists provide treatments for musculoskeletal conditions that guidelines recommend against, and nearly half provide treatments that have not been well researched. [11] Not all agree with recommendations to reduce some services (eg, only 52% of physical therapists agree that electrotherapy should not be provided for low back pain). [12] Without considering the type or amount of treatment, blind advocacy for physical therapy as a blanket alternative to medication or surgery could lead to overuse.
Understanding the Drivers of Overuse in Musculoskeletal Care
Although data on the drivers of overuse in physical therapy are scarce, the 2017 Lancet Right Care series highlighted several relevant drivers of overuse in medicine. [7] Economic incentives, such as fee-for-service and volume-based payments, likely influence clinicians' decisions. In countries where physical therapists bill for specific treatments, health insurance coverage and payment models could encourage the use of profitable, yet ineffective or untested, treatments. The knowledge, beliefs, expectations, assumptions, and biases of physical therapists and their patients can also drive overuse. Any strategy to overcome overuse will therefore require understanding of a diverse set of contributors to the problem.
The Overcoming Overuse Series
We are optimistic that physical therapists can seize the opportunity to “overcome overuse” and lead evidence-based health care for musculoskeletal conditions. In this series, we will explore the many facets of overuse in musculoskeletal diagnosis and treatment. We will propose solutions to support evidence-based, patient-centered, safe, and appropriate musculoskeletal care.
The Overcoming Overuse series has 5 key objectives:
Define and measure overuse of diagnostic tests and treatments in musculoskeletal health care
Outline the potential drivers of overuse
Explore how vested interests can increase the risk of overuse
Discuss funding arrangements that foster quality care delivery
Consider the evidence base for using shared decision making to reduce overuse
We hope to engage the JOSPT community on a variety of themes relevant to avoiding overuse of musculoskeletal health care. We encourage users to follow the series using the #overcomeoveruse hashtag. Suggest further ideas for the Overcoming Overuse series by e-mailing jospt@jospt.org or via social media (@JOSPT).
References:
Brownlee S, Chalkidou K, Doust J, et al.
Evidence for overuse of medical services around the world.
Lancet. 2017;390:156-168.
https://doi.org/10.1016/S0140-6736(16)32585-5Elshaug AG, Rosenthal MB, Lavis JN, et al.
Levers for addressing medical underuse and overuse: achieving high-value health care.
Lancet. 2017;390:191-202.
https://doi.org/10.1016/S0140-6736(16)32586-7Fritz JM, Magel JS, McFadden M, et al.
Early physical therapy vs usual care in patients with
recent-onset low back pain: a randomized clinical trial.
JAMA. 2015;314:1459-1467.
https://doi.org/10.1001/jama.2015.11648Judge A, Murphy RJ, Maxwell R, Arden NK, Carr AJ.
Temporal trends and geographical variation in the use of subacromial
decompression and rotator cuff repair of the shoulder in England.
Bone Joint J. 2014;96-B:70-74.
https://doi.org/10.1302/0301-620X.96B1.32556McGlynn EA, Asch SM, Adams J, et al.
The quality of health care delivered to adults in the United States.
N Engl J Med. 2003;348:2635-2645.
https://doi.org/10.1056/NEJMsa022615Runciman WB, Hunt TD, Hannaford NA, et al.
CareTrack: assessing the appropriateness of health care delivery in Australia.
Med J Aust. 2012;197:100-105.
https://doi.org/10.5694/mja12.10510Saini V, Garcia-Armesto S, Klemperer D, et al.
Drivers of poor medical care.
Lancet. 2017;390:178-190.
https://doi.org/10.1016/S0140-6736(16)30947-3Spitaels D, Hermens R, Van Assche D, Verschueren S, Luyten F, Vankrunkelsven P.
Are physiotherapists adhering to quality indicators for
the management of knee osteoarthritis? An observational study.
Musculoskelet Sci Pract. 2017;27:112-123.
https://doi.org/10.1016/j.math.2016.10.010Teunis T, Lubberts B, Reilly BT, Ring D.
A systematic review and pooled analysis of the
prevalence of rotator cuff disease with increasing age.
J Shoulder Elbow Surg. 2014;23:1913-1921.
https://doi.org/10.1016/j.jse.2014.08.001Traeger AC, Moynihan RN, Maher CG.
Wise choices: making physiotherapy care more valuable.
J Physiother. 2017;63:63-65.
https://doi.org/10.1016/j.jphys.2017.02.003Zadro J, O’Keeffe M, Maher C.
Do physical therapists follow evidence-based guidelines when
managing musculoskeletal conditions? Systematic review.
BMJ Open. 2019;9:e032329.
https://doi.org/10.1136/bmjopen-2019-032329Zadro J, Peek AL, Dodd RH, McCaffery K, Maher C.
Physiotherapists’ views on the Australian Physiotherapy Association’s
Choosing Wisely recommendations: a content analysis.
BMJ Open. 2019;9:e031360.
https://doi.org/10.1136/bmjopen-2019-031360
Return NON-PHARMACOLOGIC THERAPY
Since 3-13-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |