

Overcoming Overuse Part 2: Defining and Quantifying
Health Care Overuse for Musculoskeletal ConditionsThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Orthop Sports Phys Ther 2020 (Nov); 50 (11): 588-591 ~ FULL TEXT
Zoe A Michaleff, Joshua R Zadro, Adrian C Traeger, Mary O'Keeffe, Simon Décary
Institute for Evidence-Based Healthcare,
Faculty of Health Sciences and Medicine,
Bond University,
Robina, Australia.
In this series on "Overcoming Overuse," we explore the issue of health care overuse and how it may be identified in musculoskeletal physical therapy. In part 2, we frame health care overuse as a continuum from overuse to appropriate care, and consider how to measure overuse. We describe how overuse can be defined within a framework of care that is ineffective, inefficient, and misaligned, depending on the perspective of the person delivering or receiving care-the clinician, society, or patient. To ensure that musculoskeletal health care is of high value and sustainable, we encourage physical therapists to reflect on their practice.
Keywords: appropriate care; health care; musculoskeletal; physical therapy; provider; services.
From the FULL TEXT Article:
Background
Health care overuse, commonly referred to as overuse, is a health service (clinic visit, test, or treatment) that provides no net benefit or causes harm to a patient or the wider population. [4, 10] Overuse is typically considered a problem within medicine, and less so within ancillary health services. Between 10% and 30% of health care might be overuse. All treatments have the potential to cause harm in terms of physical, psychological, social, financial, and treatment burden. [4] Many physical therapists will understand the traditional definition of overuse. But what does overuse look like in practice? In part 2 of the Overcoming Overuse series, we (1) define overuse on a continuum from overuse to appropriate care, (2) consider how the definition of overuse depends on the perspective of the physical therapist, society, and the patient, and (3) discuss ways health care overuse can be measured.
A Continuum From Overuse to Appropriate Care
Clinical practice is complex, and quantifying health care as either overuse or appropriate in physical therapy is, as with other professions, not black and white. Appropriate care occurs along a continuum (FIGURE). [4] At one end of the continuum is overuse: care that is ineffective, inefficient (cost-effectiveness relative to alternatives), and misaligned with the patient’s values and preferences. [11] At the other end is appropriate care: clearly effective (beneficial based on best available evidence), efficient, and aligned with the patient’s values and preferences. Between the two extremes of overuse and appropriate care lies the “gray zone,” the area in which most real-world practice is located, with all its subtleties and nuances. The “gray zone” includes tests or treatments that offer only small benefits; have incomplete or inconclusive evidence for benefits, harms, and cost-effectiveness; where the evidence is not generalizable to the patient; or where the patient’s preferences don’t align with best evidence. It is in the “gray zone” where defining, identifying, and measuring overuse are challenging.

Table 1 Defining overuse depends on the perspective of the person vewing the problem. [11] Consumers, clinicians, health care institutions/organizations, policy makers, industry, and government likely all have different criteria when defining overuse and appropriate health care. In accordance with the framework proposed by Verkerk et al, [11] we consider overuse of musculoskeletal health care in terms of care that is ineffective, inefficient, and misaligned. [11] For each section, we include physical therapy–specific examples and encourage readers to reflect on their own practice (TABLE 1).
Health Care Overuse: Ineffective, Inefficient, and Misaligned Care
Ineffective care considers overuse from the physical therapist’s perspective and focuses on evidence-based practice. Ineffective care includes any test or treatment that, based on high-quality evidence, provides little to no beneficial effect, is not cost-effective compared to available alternatives, or for which the risk of harm outweighs the probable benefit. [11] Examples include prolonged bed rest, electrotherapy, back supports, imaging, or injections for low back pain, [7] and arthroscopic surgery for degenerative knee disorders (eg, osteoarthritis) or rotator cuff–related shoulder pain. [3] Strategies aimed at reducing ineffective care target clinicians and include de-implementation initiatives (eg, the Choosing Wisely do-not-do recommendations, available at https://www.choosingwisely.org, audit and feedback, and multicomponent implementation strategies (eg, guidelines dissemination, peer comparison, and education).

Table 2 Inefficient care can be summarized by the phrase “less is more.” Inefficient care considers overuse from a societal perspective. It includes care that is delivered in a way that increases costs without improving the patient’s outcomes, particularly when compared to alternatives that involve lower treatment volume (ie, frequency/duration), are less complex/invasive, or can be delivered in less costly settings (TABLE 2). [10, 11] Inefficient care may occur where care provision is not contingent on outcomes and is poorly coordinated between health care providers. Strategies aimed at reducing inefficient care target policy and include removing coverage for lowvalue care, reorganizing care pathways, and improving communication between health care providers. [10, 11]
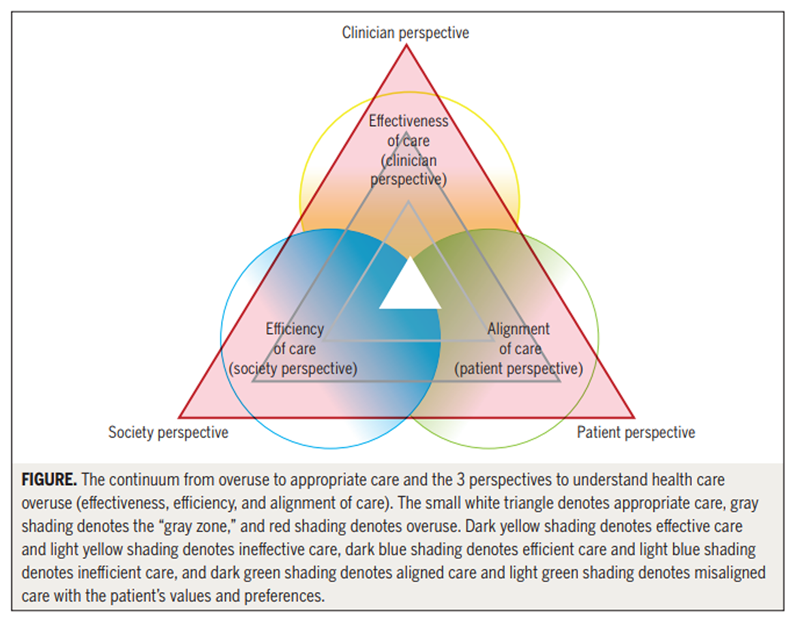
Figure Misaligned care considers overuse from the patient’s perspective and is care that does not align with the patient’s values and preferences. [11] That is, a mismatch exists between care that is recommended in clinical practice guidelines and care that aligns with the patient’s perspective. [5] This mismatch highlights the need to listen and understand the patient’s perspective for 2 reasons: (1) the patient’s values and preferences can act as a driver of overuse (TABLE 1) and will be explored further in part 3 of the series, and (2) misaligned care provides the opportunity to engage the patient as an active collaborator—especially in scenarios where care includes treatments that fall within the “gray zone” (FIGURE). [5] Shared decision making (further explored in part 5 of the series) is a strategy to engage the patient in a discussion about treatment decisions and, in turn, to overcome overuse.
Quantifying Health Care Overuse
Currently, measuring overuse is limited by a lack of systematic collection of detailed patient-level data. [10] Many systems lack data related to clinical decision making (ie, why a specific treatment was delivered) and patient preferences. [10] This level of detail is necessary to determine the appropriateness of care.
Approaches to measuring overuse are classified as direct or indirect. [4, 10] Direct measurement includes use of medical registries or patient records to determine the specific care provided and patient outcomes. For example, audits of clinical records of people with acute low back pain show that approximately 70% of physical therapists provide appropriate care, including advice to keep active, and that 16% may overuse ineffective electrotherapy modalities. [12] In the absence of direct measures, indirect measures can identify potential areas of overuse, such as variations in health care delivery within and between countries or regions that are not attributable to differences in the populations or health systems. [4] Indirect measurement includes the use of quality indicators from primary care and hospitals (eg, administrative data or surveys of patients/clinicians to identify the type and amount of care delivered). [12] The Australian Atlas of Healthcare Variation uses indirect measures to demonstrate regional variations in the use of surgery for musculoskeletal conditions (eg, knee replacements, spinal decompression, and fusion). [2] Improving our ability to identify and measure overuse is critical to progress. [10]
Am I Contributing to or Reducing Health Care Overuse?
We encourage readers to reflect on their practice from the 3 perspectives of health care overuse (clinician, society, and patient) and consider to what degree their practice is helping to overcome this problem. As physical therapists, if we are aware of factors that may contribute to overuse, reflect on our practice, and aim to deliver treatments considered appropriate from multiple perspectives (FIGURE), we are heading toward overcoming overuse. Delivering care that is effective, efficient, and aligns with the patient’s values and preferences will ensure that physical therapists remain leaders in managing musculoskeletal conditions.
References:
Artz N, Elvers KT, Lowe CM, Sackley C, Jepson P, Beswick AD.
Effectiveness of physiotherapy exercise following total knee replacement:
systematic review and meta-analysis.
BMC Musculoskelet Disord. 2015;16:15.
https://doi.org/10.1186/ s12891-015-0469-6Australian Commission on Safety and Quality in Health Care.
The Second Australian Atlas of Healthcare Variation. Sydney, Australia:
Australian Commission on Safety and Quality in Health Care; 2017.Brignardello-Petersen R, Guyatt GH, Buchbinder R, et al.
Knee arthroscopy versus conservative management in patients
with degenerative knee disease: a systematic review.
BMJ Open. 2017;7:e016114.
https://doi.org/10.1136/bmjopen-2017-016114Brownlee S, Chalkidou K, Doust J, et al.
Evidence for overuse of medical services around the world.
Lancet. 2017;390:156-168.
https://doi.org/10.1016/S0140-6736(16)32585-5Lim YZ, Chou L, Au RT, et al.
People with low back pain want clear, consistent and personalised
information on prognosis, treatment options and self-management strategies:
a systematic review.
J Physiother. 2019;65:124-135.
https://doi.org/10.1016/j.jphys.2019.05.010Michaleff ZA, Maher CG, Lin CW, et al.
Comprehensive physiotherapy exercise programme or advice for chronic
whiplash (PROMISE): a pragmatic randomised controlled trial.
Lancet. 2014;384:133-141.
https://doi.org/10.1016/S0140-6736(14)60457-8NSW Agency for Clinical Innovation.
Management of People With Acute Low Back Pain:
Model of Care.
Chatswood, Australia: New South Wales Ministry of Health; 2016.Oosterhuis T, Ostelo RW, van Dongen JM, et al.
Early rehabilitation after lumbar disc surgery is not effective or cost-effective
compared to no referral: a randomised trial and economic evaluation.
J Physiother. 2017;63:144-153.
https://doi.org/10.1016/j.jphys.2017.05.016Pellatt R, Fomin I, Pienaar C, et al.
Is buddy taping as effective as plaster immobilization for adults
with an uncomplicated neck of fifth metacarpal fracture?
A randomized controlled trial.
Ann Emerg Med. 2019;74:88-97.
https://doi.org/10.1016/j.annemergmed.2019.01.032Scott IA, Duckett SJ.
In search of professional consensus in defining and reducing low-value care.
Med J Aust. 2015;203:179-181.
https://doi.org/10.5694/mja14.01664Verkerk EW, Tanke MAC, Kool RB, van Dulmen SA, Westert GP.
Limit, lean or listen? A typology of low-value care that
gives direction in de-implementation.
Int J Qual Health Care. 2018;30:736-739.
https://doi.org/10.1093/intqhc/mzy100Zadro J, O’Keeffe M, Maher C.
Do physical therapists follow evidence-based guidelines
when managing musculoskeletal conditions? Systematic review.
BMJ Open. 2019;9:e032329.
https://doi.org/10.1136/bmjopen-2019-032329
Return NON-PHARMACOLOGIC THERAPY
Since 3-13-2023


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |