

Underreporting of Musculoskeletal Injuries in the US Army:
Findings From an Infantry Brigade Combat Team Survey StudyThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Sports Health. 2016 (Nov); 8 (6): 507–513 ~ FULL TEXT
OPEN ACCESS CPT Laurel Smith, MS, OTR/L, MAJ Richard Westrick, PT, DSc, Specialist Sarah Sauers, MS, CPT Adam Cooper, PhD, Dennis Scofield, MS, Pedro Claro, BS, and MAJ Bradley Warr, PhD, PA-C
United States Army Research Institute of Environmental Medicine,
Natick, Massachusetts.
BACKGROUND: Musculoskeletal injury is a significant threat to readiness in the US Army. Current injury surveillance methods are constrained by accurate injury reporting. Input into electronic medical records or databases therefore may not accurately reflect injury incidence. The purpose of this study was to evaluate injury reporting among active-duty US Army soldiers to explore potential limitations of surveillance approaches.
HYPOTHESIS: A significant number of injuries go unreported to medical personnel.
STUDY DESIGN: Cross-sectional study.
LEVEL OF EVIDENCE: Level 4.
METHODS: Surveys were completed by soldiers assigned to an Army Infantry Brigade Combat Team. Survey questions inquired about injuries sustained in the previous 12 months, injury onset, and whether injuries were reported to a medical provider. Participants were asked to rank reasons for accurately reporting, underreporting, and/or exaggerating injuries. Chi-square analyses were used to compare differences among underreported injuries in terms of injury onset (gradual vs acute) and sex.
RESULTS: A total of 1,388 soldiers reported 3,202 injuries that had occurred in the previous 12-month period, including 1,636 (51%) that were reported and 1,566 (49%) that were identified as not reported to medical personnel. More than 49% of reported injuries were described as acute and 51% were described as chronic. Injury exaggeration was reported by 6% of soldiers. The most common reasons for not reporting injuries were fear that an injury might affect future career opportunities and avoidance of military "profiles" (mandated physical restrictions).
CONCLUSION: Approximately half of musculoskeletal injuries in a Brigade Combat Team were not reported.
CLINICAL RELEVANCE: Unreported and untreated injuries can lead to reinjury, chronic pain, performance decrements, and increased costs associated with disability benefits. Additionally, unreported injuries can undermine injury surveillance efforts aimed at reducing the musculoskeletal injury problem in the military.
KEYWORDS: injury exaggeration; injury reporting; military readiness; musculoskeletal injury
From the FULL TEXT Article:
Background
For decades, musculoskeletal injury (MSI) has remained a liability to military readiness. [2, 11, 21, 34] The MSI burden affects Service Members (SM), military units, and the Military Health System (MHS), with approximately 1.6 million hospital encounters per year resulting in millions of lost and limited duty days. [7, 10, 14] In addition to decreased productivity, MSIs can be associated with chronic pain, personnel attrition, and long-term disability. [29] Moreover, as one of the largest contributors to disability discharge, [6] MSIs can have long-term financial implications for the MHS.
The physical and occupational demands required by SMs in the US Military involve repetitive and highly dynamic movements including heavy lifting and load carriage requirements, [28] which are even greater during combat deployments. [27] The rigors of military service also require personnel to maintain a certain level of fitness through regular physical training. Despite mandated fitness requirements, there may be instances in which the physical demands of military occupational tasks exceed a soldier’s physical capacity to perform that task. [12] Jennings et al [13] found that 47% of injuries reported by soldiers are work related, with 29% of these occurring during mission-related training. Other causes of injuries included: running (9%), sports (5%), lifting (5%), motor vehicle–related injuries (4%), and falling (2%). Participants in that study also reported that their injuries affected job performance. The unique occupational demands of military service may predispose soldiers to various acute and overuse MSIs, impeding optimal job performance and posing risks to the mission and the well-being of the unit. Because injuries in the armed forces are regarded as a threat to military readiness, soldiers may be motivated to minimize or conceal injuries to avoid perceptions of weakness or ineptitude.
Concealment of work-related injuries in the civilian workplace has been widely cited, [4, 8, 19, 20, 25, 31, 32] with rates as high as 65% in some reports. [26] Injury minimization (ie, symptoms were not serious enough to seek help), [20] fear of job loss, separation from coworkers, [25] and desire to avoid filing a workers’ compensation claim [4] were cited as common reasons for civilian injury underreporting. In contrast to injury concealment, injury exaggeration is another potential concern within military populations. There are several reasons why soldiers may exaggerate injuries, including rationalizing substandard performance, release from mandatory requirements (eg, physical training, deployment, etc), to pursue military separation prior to contractual obligation, and to increase potential disability benefits upon separation. While the incidence of injury exaggeration has been investigated in both the civilian and military populations, most studies have investigated populations with psychosocial disorders. [18] These studies provide some understanding of injury exaggeration, although the literature investigating symptom exaggeration for MSIs in the military is limited.
Epidemiology and injury surveillance are essential aspects of injury prevention efforts, [15, 16] serving as an essential tool for determinations regarding required personnel, medical logistics, and anticipated direct/indirect costs for military medicine. Despite the benefit of these efforts, they are incapable of accounting for unreported injuries, and thus may not accurately reflect the true scale of readiness and potential reinjury risk concerns. To date, the accuracy of MSI reporting in the military has not been challenged. Without this information, it is difficult to fully understand the magnitude of MSIs within the military.
The purpose of this study was to evaluate MSI reporting among active-duty US Army soldiers in a Brigade Combat Team. A secondary purpose was to explore the factors influencing a soldier’s decision to report, conceal, or exaggerate MSIs. Despite the paucity of literature on injury reporting, we hypothesized that the incidence of injury concealment would be greater than injury exaggeration.
Methods
Participants
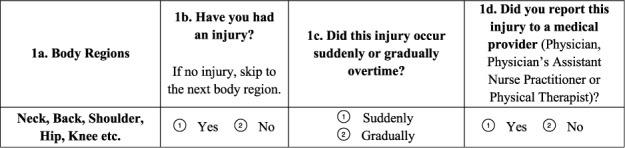
Figure 1

Table 1 Participants were soldiers from an Infantry Brigade Combat Team (BCT) composed of Military Occupational Specialties (MOS) from both combat (eg, infantry, armor, field artillery) and support (engineers, medics, mechanics, etc) branches. All active-duty soldiers aged 18 years and older were invited to participate regardless of sex, rank, or MOS. To encourage accurate and honest responses, participants were seated in an auditorium with at least 1 seat in between each person. To further encourage truthful responses, Junior Enlisted Soldiers (Specialists and below) were separated from Senior Enlisted and Officers (Sergeants and above). When responding to survey questions, participants were asked to reflect on MSI history within the previous 12 months. Participants were informed that the survey was voluntary, and completion of the survey implied consent. This study was reviewed and approved by the Institutional Review Board at the United States Army Research Institute of Environmental Medicine (USARIEM) for the ethical treatment of participants in human subject’s research. To maintain anonymity, a waiver of written informed consent was granted.
ProceduresSurvey Description An 11-page, 50-question survey was developed internally by the authors, who are experienced military health care providers (collectively more than 50 years of military experience) serving as researchers. Initial survey drafts were piloted and refined with a panel of military personnel composed of varying ranks and MOS. The survey, designed to be anonymous, assessed injury-reporting behaviors and factors that may contribute to injury reporting, as well as various topics related to injuries in the military. Soldiers were asked to respond to questions regarding injuries to various body regions, injury onset (sudden or gradual), and whether the injury was reported to a medical provider (Figure 1). To assess injury exaggeration or minimization, participants were asked whether they had misrepresented symptoms of an injury in the previous 12 months. Following these questions, participants were asked to rank reasons that may have influenced their decision to report, underreport, or exaggerate their injuries (Table 1). Participants were also presented with several statements regarding injuries and seeking medical evaluation and perceptions of injuries in the Army. Last, the survey included demographic information, recent Army physical fitness test (APFT) score, rank, time in service, and MOS. Survey questions were closed-ended in which the participants were provided a list of responses and were asked to select 1 answer, or in some instances, they were instructed to select all answers that applied.
Operational definitions of the terms used throughout the survey were explained to the participants. Injury was defined as “any ache, pain, or discomfort related to the musculoskeletal system (skin, bone, muscle, tendon, ligament, or nerves) that persisted for more than 7 days.” Medical providers were defined as licensed health care providers such as physicians, physician assistants, nurse practitioners, or physical therapists (for the purposes of this study, an Army Medic was not considered a medical provider). Accurate reporting was defined as “an injury that was reported to a medical provider.” Underreporting was defined as a “suspected injury that was not reported to a medical provider.” Injury exaggeration was defined as the symptoms of an injury being inflated to a medical provider.
Data Analysis
Surveys were scanned into a database using Remark Office–Optimal Mark Recognition Technology (Gravic Inc), and responses were converted into ordinal data. Data analyses were conducted using the statistical package SPSS (version 20.0; IBM Corp). Injury-reporting rates were calculated with descriptive statistics. Because of the possibility of reporting an injury in one body region and not another or reporting injuries in multiple body regions, each injury was treated individually and unreported injuries were filtered for analysis. Chi-square analyses were used to determine differences in underreporting related to injury onset (sudden vs gradual).
Results

Table 2

Table 3
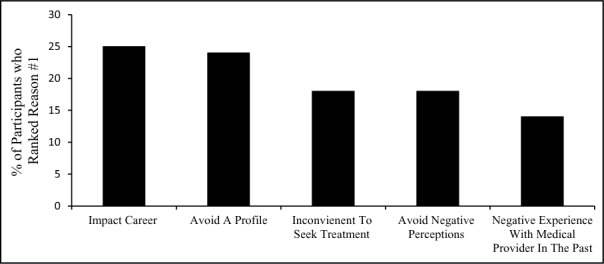
Figure 2 The survey was completed by 1,388 respondents (1,269 men, 74 women, 45 undisclosed), accounting for approximately 40% of the entire BCT. Participant demographics are summarized in Table 2. A total of 3,202 MSIs were described by this cohort during a 12-month time frame. Of those injuries, 1,636 (51%) were described as reported while 1,566 (49%) were not reported. During analysis, injuries characterized by sudden onset were considered acute while injuries with a gradual onset were considered chronic. Among the reported injuries, 49% were acute and 51% were chronic. Among the injuries revealed as unreported, 38% were described as acute and 62% were described as chronic. When compared with acute injuries, chronic injuries of the back, shoulder, knee, and ankle were statistically more likely to be unreported to a medical provider (Table 3). Injury exaggeration was reported by 6% (83) of soldiers.
Influential factors related to injury-reporting behavior varied. The most common reasons selected for underreporting injuries were fear of future impact on one’s career and avoidance of a duty-limiting “profile” (Figure 2). The 3 most common reasons for accurate reporting were the following: seeking medical documentation, concern about symptoms, and feeling that the injury affected job performance. The most common motivation cited for injury exaggeration was pursuing documentation in the medical record.
Discussion
The extent of MSI underreporting (49%) is similar to studies investigating injury concealment among construction, factory, and service-oriented industries. These findings reveal a potential challenge to our current understanding of the magnitude of MSI in the Army and identify various potential implications to medical readiness.
In the current study, the majority of unreported injuries occurred gradually, indicating chronic onset. Chronic injuries can be characterized by a slower onset, generally without an isolated traumatic incident, and are most commonly the result of repetitive movements related to job tasks and physical training. [35] Overuse injuries comprise the largest category of MSIs in the US Army. [14] Some jobs in the military are more physically strenuous than others and place high physical demands on soldiers assigned to those jobs (ie, infantrymen, mechanics, etc). [12] Bell et al [6] found that as physical occupational demands increased, so did one’s risk of injury, hospitalization, and eventually, disability. Roy et al [27] reported that 20% of MSIs in a BCT can be attributed to overuse injuries. With prolonged engagement in military activities, unreported injuries can deteriorate and lead to future injury, chronic pain, increased reinjury risk, or potentially even permanent disability, ultimately degrading individual and unit effectiveness. [29, 30, 38]
Interestingly, our study did not find differences in underreporting based on sex, which differs from previous findings suggesting women have a greater tendency to report symptoms5 and underreport injuries much less frequently. [3, 17] This finding may have been influenced by the relatively small number of female participants. Although with women now being integrated into occupations traditionally restricted to men, they might be confronted with different scenarios that may or may not affect their injury-reporting behavior. These findings have important implications for future studies that may want to evaluate the direct and indirect impact of integration efforts.
Consistent with civilian literature, this study revealed information about the perceived stigmatization of injuries and the impact on injury-reporting behavior. Reasons for underreporting injuries centered on the avoidance of duty-restricting “physical profiles” (profiles) and the potentially negative ramifications that injuries may have on one’s career. Per current doctrine, soldiers who are unable to participate in individual or unit tasks are placed on a profile by a medical provider. [1] The US Army’s profile system is designed as a mechanism allowing medical providers to communicate recommendations to military commanders regarding duty limitations as well as classify the soldier based on functional abilities. They are designed, in part, to protect the soldier from further injury and facilitate healing.
However, as evidenced by the number of underreported injuries rationalized by profile avoidance, it is possible that negative stereotypes associated with limited-duty profiles may be perpetuating the pervasive culture of injury minimization and concealment throughout the military. These findings are supported by Hauschild et al, [11] who found that respondents to a survey study about soldier perceptions reported a perceived lack of credibility of the profile system. Moreover, the stigmatization of injuries and profiles among leadership has been documented previously. [11, 13] These findings highlight challenges experienced by soldiers with MSIs and suggest barriers to injury reporting are inherent to military culture. Injury prevention and performance optimization awareness and training may benefit from targeting leadership at the small-unit level (ie, First Sergeants, Drill Sergeants, Platoon Sergeants, etc), with individuals who have a significant role in shaping the culture of injuries for soldiers and future military leaders.
The current study found that injury exaggeration is relatively rare among soldiers, with only 83 (6%) reporting exaggerating symptoms of an injury. These findings are consistent with previous literature suggesting that diagnosed injury exaggeration (malingering) in military populations is scarce. [18] In that study, the authors interestingly found that the majority of diagnoses were made by providers not credentialed in behavioral health.18 Because of the potential legal ramifications associated with the diagnosis, they postulate that the incidence may be slightly underestimated, but overall, the occurrence is still rare.
Reasons for injury exaggeration in our study were motivated by a desire to validate the presence of an injury for the purpose of documentation and/or to rationalize substandard performance. In a profession where physical performance is a key contributor to career advancement, injury exaggeration has the potential to be misused to justify poor performance. Furthermore, documented injuries are often used to qualify soldiers for disability compensation when the injury occurred while on active duty and/or was exacerbated as a result of military service. [33] Thus, soldiers may be motivated to pursue medical documentation in an effort to increase potential disability compensation at discharge. While injury exaggeration likely exists, it appears as though injury concealment is far more common.
Injury reporting has previously been underrecognized as a problem in need of targeted attention and intervention by both military leaders in the medical and operational community. Interestingly, there are no requirements to provide training on injury prevention in the military. [11] Previous recommendations to enhance physical readiness in the military [21] proposed several initiatives emphasizing increased education and awareness that could easily be modified to address injury reporting at the soldier and leader level.
Limitations
Injury-reporting behavior is an elusive concept to define and measure with objective metrics, particularly when the nature of the construct being measured relies on self-report data. While self-report measures have been criticized for their limited reliability and validity, these methodologies can provide valuable insight into cognitive processes that impact attributions, plans, attitudes, beliefs, and behavior [9] as they allow for investigation of emotional and behavioral aspects of a given problem that may not be detected by other methodologies. Other studies of military personnel have reported encouraging results when a self-report measure was used to obtain data on potentially sensitive topics, [24, 37] especially when an anonymous survey was used. [23, 36] However, given the self-reported data in this study, findings should still be interpreted carefully. Current demographic reports state that women comprise approximately 16% of the US Army. [22] While the sample was intended to be representative of the entire Army, women were slightly underrepresented in this study (accounting for approximately 5% of the total population), which may have influenced the results. Additionally, the suboptimal response rate of 40% lends itself to a potential for response bias.
The study design excluded medics from the definition of medical provider, which could be viewed as a limitation. Injuries characterized as “unreported” by our definition may have in fact been reported to a unit medic. Nonlicensed providers were excluded to avoid gathering data on injuries that would not have been formally captured in the SMs medical record and could have been reported casually to a medic. It is not uncommon (especially on deployment) for soldiers to casually discuss nonemergent medical ailments. Often these “reports” do not make it into the electronic medical record. Therefore, by excluding medics from our definition of medical providers, we aimed to avoid capturing informal instances of injury reporting. The number of injuries “reported” to a medic remains unknown, which could impact the generalizability of the results.
Three months prior to survey administration, the unit returned from a 9-month deployment to Afghanistan. Because the survey asks about injuries sustained in the past 12 months, data include injuries in both the training and deployed environments. While this could be viewed positively, it can be argued that injury-reporting behaviors and influential factors may differ in the deployed environment, and therefore, the survey may not have included all of the potential reasons for various injury-reporting behaviors among this group.
The survey tool was developed through multiple refinements and piloting; however, it would benefit from a validation study using another BCT. Additionally, diagnoses were not correlated to injury reports so the extent of reported injuries is unknown. The methodology employed provides a foundation on which to base further investigation into the aspects of injury reporting within the military. While results of this study are encouraging and contribute to improved understanding of MSI reporting in the military, generalizing these data should be cautioned.
Conclusion
The findings of this survey reveal injury exaggeration is rare but that MSI underreporting occurs regularly. Untreated injuries have the potential to degrade individual and unit effectiveness, thereby negatively impacting operations on various levels. Medical providers and military leaders need to be aware of the perceptions around injuries and how these perceptions may deter soldiers from seeking medical evaluation for injuries in both the training and deployed environments.
Acknowledgments
The authors would like to thank the soldiers of the 172nd Infantry Brigade Combat Team as well as COL Edward Bohnemann, CPT Joanie Baca, CPT Fernando Najera, and CPT Jeanette Rivera for their assistance in completing this research. Additionally, the authors would like to thank LTC Kathleen Yancosek for inspiring the initial research question.
Conflicts of Interest
The authors report no potential conflicts of interest in the development and publication of this article.
References:
Army Regulation 40-501.
Standards of Medical Fitness.
Washington, DC: Headquarters, Department of the Army; 2004:66-72Atlas of injuries in the United States Armed Forces.
Mil Med. 1999;164(8 suppl):633Almeida SA, Trone DW, Leone DM, Shaffer RA, Patheal SL, Long K.
Gender differences in musculoskeletal injury rates: a function of symptom reporting?
Med Sci Sports Exerc. 1999;31:1807-1812Azaroff LS, Levenstein C, Wegman DH.
Occupational injury and illness surveillance: conceptual filters explain underreporting.
Am J Public Health. 2002;92:1421-1429Barsky AJ, Peekna HM, Borus JF.
Somatic symptom reporting in women and men.
J Gen Intern Med. 2001;16:266-275Bell NS, Schwartz CE, Harford T, Hollander IE, Amoroso PJ.
The changing profile of disability in the U.S. Army: 1981-2005.
Disabil Health J. 2008;1:14-24Cross JD, Ficke JR, Hsu JR, Masini BD, Wenke JC.
Battlefield orthopaedic injuries cause the majority of long-term disabilities.
J Am Acad Orthop Surg. 2011;19(suppl 1):S1-S7Dong XS, Fujimoto A, Ringen K, et al.
Injury underreporting among small establishments in the construction industry.
Am J Ind Med. 2011;54:339-349Haeffel GJ, Howard GS.
Self-report: psychology’s four-letter word.
Am J Psychol. 2010;123:181-188Hauret KG, Taylor BJ, Clemmons NS, Block SR, Jones BH.
Frequency and causes of nonbattle injuries air evacuated from Operations Iraqi Freedom
and Enduring Freedom, U.S. Army, 2001-2006.
Am J Prev Med. 2010;38(1 suppl):S94-S107Hauschild VD, Schuh A, Jones BH.
What soldiers know and want to know about preventing injuries:
a needs survey regarding a key threat to readiness.
US Army Med Dep J. 2016;Jan-Mar:10-19Hollander IE, Bell NS.
Physically demanding jobs and occupational injury and disability in the U.S. Army.
Mil Med. 2010;175:705-712Jennings BM, Yoder LH, Heiner SL, Loan LA, Bingham MO.
Soldiers with musculoskeletal injuries.
J Nurs Scholarsh. 2008;40:268-274Jones BH, Canham-Chervak M, Canada S, Mitchener TA, Moore S.
Medical surveillance of injuries in the U.S. Military descriptive epidemiology and recommendations for improvement.
Am J Prev Med. 2010;38(1 suppl):S42-S60Jones BH, Canham-Chervak M, Sleet DA.
An evidence-based public health approach to injury priorities and prevention recommendations
for the U.S. Military.
Am J Prev Med. 2010;38(1 suppl):S1-S10Jones BH, Perrotta DM, Canham-Chervak ML, Nee MA, Brundage JF.
Injuries in the military: a review and commentary focused on prevention.
Am J Prev Med. 2000;18(3 suppl):71-84Kazman JB, de la, Motte S, Bramhall EM, Purvis DL, Deuster PA.
Physical fitness and injury reporting among active duty and National Guard/Reserve women:
associations with risk and lifestyle factors.
US Army Med Dep J. 2015;Apr-Jun:49-57Lande RG, Williams LB.
Prevalence and characteristics of military malingering.
Mil Med. 2013;178:50-54Menzel NN.
Underreporting of musculoskeletal disorders among health care workers: research needs.
AAOHN J. 2008;56:487-494Moore JT, Cigularov KP, Sampson JM, Rosecrance JC, Chen PY.
Construction workers’ reasons for not reporting work-related injuries: an exploratory study.
Int J Occup Saf Ergon. 2013;19:97-105Nindl BC, Williams TJ, Deuster PA, Butler NL, Jones BH.
Strategies for optimizing military physical readiness and preventing musculoskeletal injuries in the 21st century.
US Army Med Dep J. 2013;Oct-Dec:5-23Office of the Deputy Chief of Staff.
Army Demographics.
Washington, DC: US Department of the Army; 2014Olson CB, Stander VA, Merrill LL.
The influence of survey confidentiality and construct measurement in estimating rates
of childhood victimization among navy recruits.
Mil Psychol. 2004;16:53-69Pell JP, Haw SJ, Cobbe SM, et al.
Validity of self-reported smoking status: comparison of patients admitted to hospital
with acute coronary syndrome and the general population.
Nicotine Tob Res. 2008;10:861-866Pransky G, Snyder T, Dembe A, Himmelstein JAY.
Under-reporting of work-related disorders in the workplace: a case study and review of the literature.
Ergonomics. 1999;42:171-182Rosenman KD, Kalush A, Reilly MJ, Gardiner JC, Reeves M, Luo Z.
How much work-related injury and illness is missed by the current national surveillance system?
J Occup Environ Med. 2006;48:357-365Roy TC, Ritland BM, Sharp MA.
A description of injuries in men and women while serving in Afghanistan.
Mil Med. 2015;180:126-131Roy TC, Springer BA, McNulty V, Butler NL.
Physical fitness.
Mil Med. 2010;175(8 suppl):14-20Ruscio BA, Jones BH, Bullock SH, et al.
A process to identify military injury prevention priorities based on injury type and limited duty days.
Am J Prev Med. 2010;38(1 suppl):S19-S33Sanders JW, Putnam SD, Frankart C, et al.
Impact of illness and non-combat injury during Operations Iraqi Freedom and Enduring Freedom (Afghanistan).
Am J Trop Med Hyg. 2005;73:713-719Scherzer T, Rugulies R, Krause N.
Work-related pain and injury and barriers to workers’ compensation among Las Vegas hotel room cleaners.
Am J Public Health. 2005;95:483-488Siddharthan K, Hodgson M, Rosenberg D, Haiduven D, Nelson A.
Under-reporting of work-related musculoskeletal disorders in the Veterans Administration.
Int J Health Care Qual Assur Inc Leadersh Health Serv. 2006;19:463-476Songer TJ, LaPorte RE.
Disabilities due to injury in the military.
Am J Prev Med. 2000;18(3 suppl):33-40Teyhen DS, Shaffer SW, Butler RJ, et al.
What risk factors are associated with musculoskeletal injury in US Army Rangers?
A prospective prognostic study.
Clin Orthop Relat Res. 2015;473:2948-2958van Tulder M, Malmivaara A, Koes B.
Repetitive strain injury.
Lancet. 2007;369:1815-1822Warner CH, Appenzeller GN, Grieger T, et al.
Importance of anonymity to encourage honest reporting in mental health screening after combat deployment.
Arch Gen Psychiatry. 2011;68:1065-1071Weiss RD, Najavits LM, Greenfield SF, Soto JA, Shaw SR, Wyner D.
Validity of substance use self-reports in dually diagnosed outpatients.
Am J Psychiatry. 1998;155:127-128Yancosek KE, Roy T, Erickson M.
Rehabilitation programs for musculoskeletal injuries in military personnel.
Curr Opin Rheumatol. 2012;24:232-236
Return to CHIROPRACTIC CARE FOR VETERANS
Since 9-02-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |