Cerebrovascular Accidents:
The Rest of The StoryThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




Our thanks to Dr. Anthony Rosner for permission to reproduce this article, exclusively at Chiro.org! This paper was presented Friday June 20, 2003 at the International Spinal Trauma Conference in Chicago, IL.
Anthony L. Rosner, Ph.D.
Introduction
During the past decade, the issues of cerebrovascular accidents [CVAs] and spinal manipulation have become linked in a debate of ever–increasing intensity. A copious number of studies have investigated spinal manipulation as a putative causative factor of CVAs; [ 1–5] however, a common theme among these is the failure to adequately explore the possibility that the majority of CVAs may be spontaneous, cumulative, or caused by factors other than spinal manipulation itself. The problem is only exacerbated by the sometimes hysterical reactions apparent in the mass media over the past three years in reaction to the flawed investigations. [6–11]
In light of these recent reports, the issue of CVAs needs to be revisited from the multiple vantage points of:[I] plausible mechanisms,
[II] relative risks and benefits, and
[III] spontaneous dissections.
I. PLAUSIBLE MECHANISMSArterial Dissections:
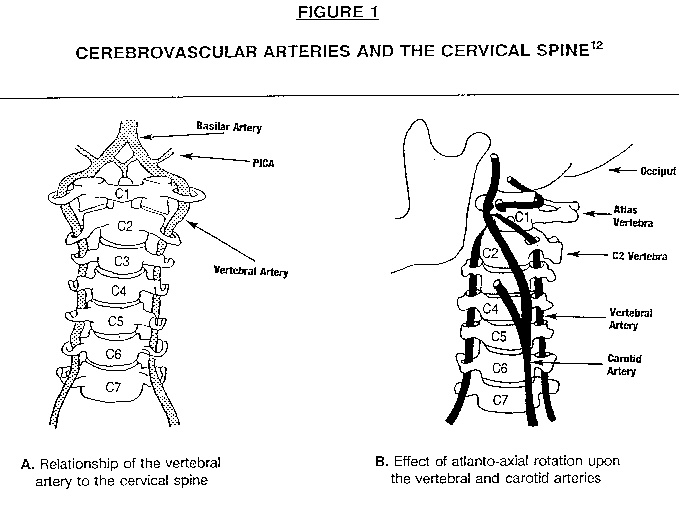
The vertebral artery [VA], threaded along both sides of the cervical spine [Figure 1A ], appears to be most vulnerable to stretching, compression, or torquing forces in the upper cervical region–especially when compared to the carotid artery [Figure 1A] in which less than 5% of injuries following spinal manipulative therapy have been reported. [3, 12–15] Following cervical manipulations, in particular, the most common site of injury to the vertebral artery system appears to be in the vicinity of the atlanto-axial joint, where the vertebral artery bends into a horizontal configuration as shown in Figure 1B. By a large majority, most postmanipulative strokes and stroke-like symptoms have been described to occur in the segment of the vertebral artery bounded by the transverse foramen of the C2 vertebra and the foramen magnum. [16] One might imagine that significant rotation of the neck in this region could cause the kinking of the artery which triggers the CVA; indeed, it is precisely in the C1–C2 region in which rotational maneuvers have been suggested to be a possible risk factor for CVAs. [17–18]
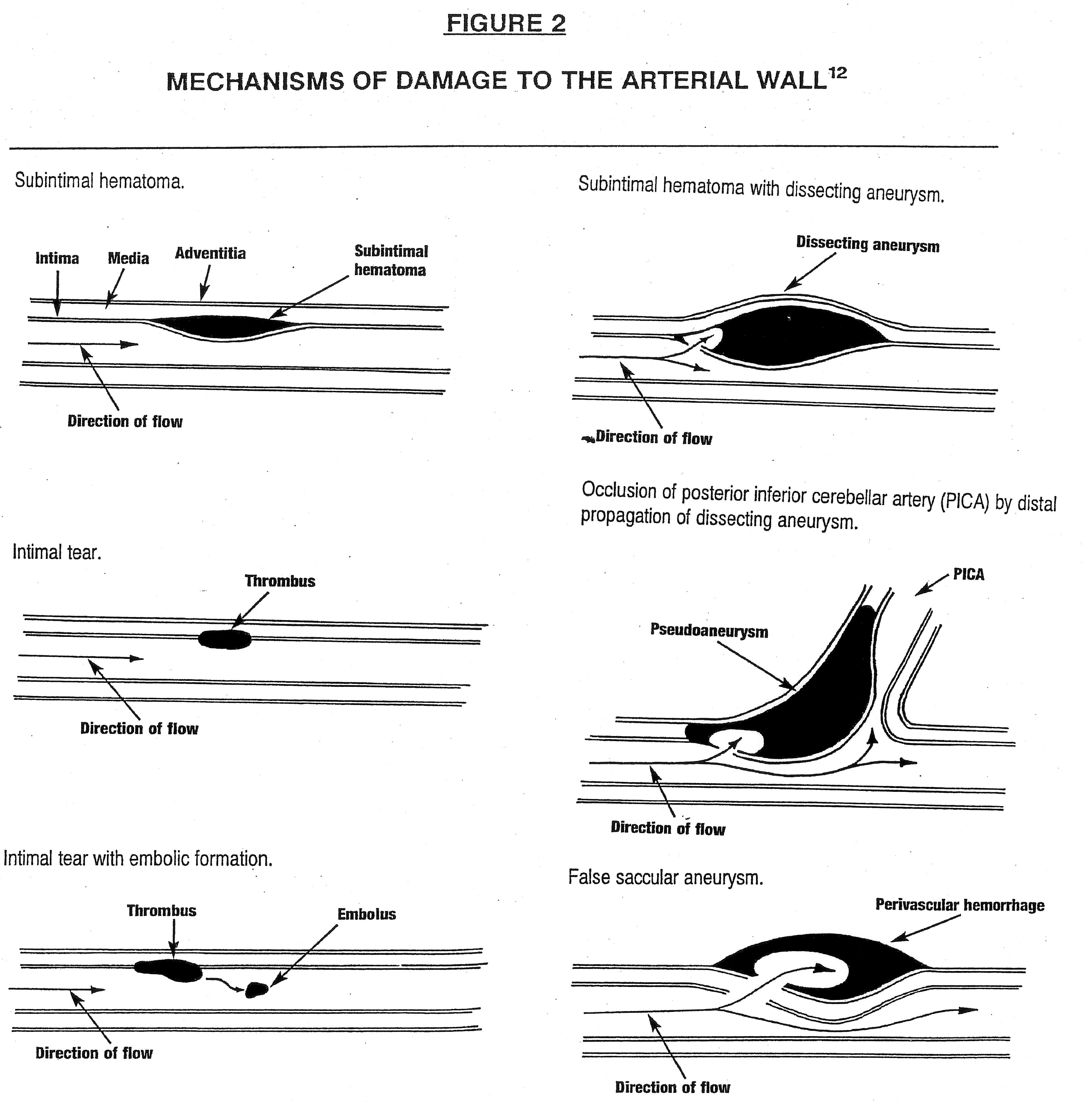
Brainstem ischemia is produced by trauma to the arterial wall, producing either vasospasm or damage to arterial wall itself. Vasospasm may trigger a cascade of events leading 0to fibrin deposition and resulting thrombus formation; injuries to the arterial wall could involve tearing, dissection, or branch occlusion. As described by Terrett, arterial traumatic mechanisms may be classified by one of six categories as shown in Figure 2:[i] subintimal hematoma,
[ii] intimal tear,
[iii] intimal tear with embolic formation,
[iv] vessel wall dissection with subintimal hematoma (dissecting aneurysm),
[v] vessel wall dissection with pseudoaneurysm formation, and
[vi] perivascular bleeding (false saccular aneurysm). [12]Because stretching, shearing, or crushing are the forces leading to these arterial problems, they are suspected to be the main culprits producing CVAs – produced under certain circumstances involving the rotation and/or extension of the head. Any head movement that produces occlusion of a vertebral artery, in cases in which the flow in the contralateral artery is already compromised, has the potential to lead to a CVA. Although one might suspect altered vertebral artery hemodynamics and reduced basilar perfusion to be consequences of diagnostic testing and/or spinal manipulation, it is primarily the vertebral arterial dissections [VADs] which have been implicated in the majority of stroke or stroke-like incidents [16] directly attributable to spinal manipulation. VADs, therefore, will form the basis of the ensuing discussion.
Measurement of Forces upon the Vertebral Artery
From a mechanistic viewpoint, the most direct means of assessing the effects of spinal manipulative therapy upon the integrity of the VAs would be to directly measure how the forces anticipated during manipulations might be transmitted through the various skeletal and soft-tissue layers of the cervical milieu to the region of the VA, and how such forces compare to the limits of arterial integrity assessed by deliberately stretching the VA until it ruptures. Such a study was recently accomplished at the University of Calgary upon the VAs excised from unembalmed post-rigor patients who had died within the past 72 hours.
In this investigation, the distal CO–C1 and proximal C6–subclavian loops of the VAs were exposed and fitted with a pair of piezoelectric ultrasonic crystals. Strains between each crystal pair were recorded during range of motion testing, diagnostic tests, and a variety of procedures employed in spinal manipulation. Afterwards, the VA was dissected and strained on a materials testing machine until mechanical failure occurred. For manipulation, the elongations of the CO–C1 and C6–subclavian artery segments of the VA were 6.2% and 2.1% respectively. For normal head rotation, on the other hand, these elongations were respectively 12.5% and 4.8%. The elongations of these same regions needed to reach VA failure were 53.1% and 62.3% respectively. Two conclusions are readily apparent:[i] the values measured during spinal manipulative therapy were less than those recorded during range of motion and diagnostic testing; and
[ii] the VA strains measured during spinal manipulation were less than 1/9 those needed to achieve arterial failure. [19]The implications of this study shed considerable light upon the controversy regarding VADs and spinal manipulation. First, it is evident that the forces experienced during spinal manipulation are virtually an order of magnitude below those needed to produce an arterial failure in a single event. Secondly, it is apparent that routine neck maneuvers during the assessments [rather than the manipulations] registered greater forces in the region of the VAs. This immediately raises the possibility that spontaneous rather than induced CVAs are likely to occur in the VA, an issue which will be explored in depth in a section to follow.
There are a number of significant cautionary notes that must be sounded to this study, however:
The portion of the artery most commonly involved in VA dissections associated with spinal manipulation [C1–C2, as pointed out earlier] was not measured; rather, the entire VA was used to obtain mechanical failure points; [20]
Stretch by tensile forces, rather than compression by combined forces [particularly at the C2 foramen, proposed to be the actual force causing damage during manipulation [21] was measured, which may not reflect the suspected type of artery deformation occurring in patients; [20]
The strain created to the thrust side VA when the neck is fully rotated contralaterally was not evaluated, representing the most forceful manipulation, was not measured; [20]
The ranges of motion from the 80–99–year old cadavers would be expected to be more restricted than those typical of younger patients seen in chiropractic offices, limiting the strains on the VAs that were measured by the researchers and perhaps not representative of those seen in actual practice; [20]
There were wide variations in force ranges [4–18N] and of strains [31%–75%]; [20]
Preparing the arterial specimens in ultrasound gel may have artificially increased their flexibility; [20]
One may question whether the overall failures observed are similar enough to the intimal tearings experienced in vivo in spontaneous events; and finally
Since arterial dissections may well represent the culmination of multiple arterial insults as outlined in the ensuring text, it is necessary that this experiment be repeated to assess arterial integrity after dozens and perhaps hundreds of applied stretches to the VA.
II. RELATIVE RISKS AND BENEFITSBenefits:
Regarding benefits, the effects of cervical spinal manipulation upon neck pain, whiplash, and headache have been extensively outlined elsewhere, [22] a systematic review of which designates no less than 20 randomized clinical trials having addressed this issue, with the majority indicating positive, and the remainder yielding equivocal results. Neither negative results, nor significant adverse events to these cervical manipulations were shown, [23–24] the absence of side effects also having been observed in three case series in which children underwent cervical manipulations for the treatment of Otis media. [25–27]
Risks:
Regarding the risks of cervical manipulation in producing VADs, a large number of retrospective studies against large population bases have been conducted. As shown in Table 1, a large number of such studies indicate that the number of serious complications or CVAs as established by researchers from both the chiropractic and medical professions ranges from 1 case per 400,000 manipulations to zero cases in 5 million. Data from the RAND Corporation suggests the rate of vertebrobasilar accident or other complications (cord compression, fracture, or hematoma) to be 1.46 per million manipulations, with the rates of serious complications and death from cervical spine manipulation estimated to be 0.64 and 0.27 per million manipulations, respectively. [33] The most recent retrospective review, involving the largest number of presumed cervical manipulations performed (134.5 million) over the longest period of time (10 years), used malpractice claims from the Canadian Chiropractic Protective Association. It revealed a total of 43 cases of neurological symptoms retrieved from patient records, 23 of which involved stroke. The total yield of strokes, therefore, was 23/134.5 million, a frequency rate of 1 per 5.85 million (0.17 per million) cervical manipulations, equivalent to one stroke per 1430 chiropractic practice-years, or a stroke occurrence rate of one per 48 chiropractic practice careers. [36]
The risk estimates attributed to cervical manipulation are significantly less [by orders of magnitude] than those associated with various medical procedures and lifestyle activities ,as shown in Table 2. [33, 37–43] In an exhaustive review of risk estimates from multiple phases of life, Rome points out that the substantially greater risks attributed to the medical procedures have been deemed "acceptable" by the routine adoption of such terminologies as "risk-adjusted mortality rates" and "net clinical benefits." The problem becomes all the more ironic in that, in Rome's words, "there seems a reluctance to concede the application of these terms outside the medical profession. [44] The risks inherent in other lifestyle activities, also appearing to be readily accepted by the public at large, are apparent in Table 2 and again outweigh those associated with cervical manipulation by several orders of magnitude. In striking contrast to the dire media warnings about the risks of cervical manipulation alluded to earlier, [6–11] there appears to be little attention or resentment attached to the medical and lifestyle activities shown in Table 2.
The published reports mentioned at the beginning of this discussion have attempted to attribute cerebrovascular accidents to chiropractors at many times the prevailing rate, primarily based upon the physician's recollection of patients who have encountered cerebrovascular problems within a relatively close time frame of their visit to a chiropractor. [1–5] Serious design deficiencies in these reports which create the impression of substantially greater CVA rates than those reported here have been addressed elsewhere, [45–46] the most vexing being that the practitioner actually involved in many of these cases may not have been a chiropractor, but rather an individual with inadequate professional training, but incorrectly represented in the medical literature as a chiropractor. [47] A more thorough discussion of the deficiencies in these studies is to follow.
III. SPONTANEOUS DISSECTIONS
Perhaps the most compelling information that needs to be brought forward to bring the debate about cervical manipulations onto a level playing field has to do with the fact that a significant number and most likely the majority of VADs happen to be spontaneous [sCADs] (Table 3). As will be demonstrated in numerous reports addressing both the frequency of occurrence of VADs, and their association with virtually any activity associated with turning the head, should reduce the utility of attributing strokes to cervical manipulations to virtually an academic exercise.
Prevalence:
As shown in Table 3, the annual incidence of spontaneous VADs in hospital settings has been estimated to occur at the rate of 1–1.5 per 100,000 patients. [48] The corresponding VAD incidence rate in community settings have been reported to be twice as high. [49–50]Using an estimated value of 10 from the literature to represent an average number of manipulations per patient, per episode, [51] it becomes apparent that the proposed exposure rate for CVAs attributed to spinal manipulation is equivalent to the spontaneous rates for cervical arterial dissections as reported. [48–50] If the threat of stroke or stroke-like symptoms is to be properly assessed, therefore, at least half our attention needs to be directed toward the spontaneous events instead of primarily or solely upon spinal manipulation.
Furthermore, a large number of common lifestyle activities have been shown to be associated with cerebral ischemia [Table 4A] [44] or CVAs themselves [Table 4B]. [52] All are decidedly non-manipulative. By way of illustration, one recent investigation has described beauty parlor stroke syndrome and salon sink radiculopathy confirmed by both patient symptoms and blood flow velocities in the bilateral vertebral and carotid arteries as measured by a diagnostic ultrasound instrument. [53]
Association of Homocysteine and Arterial Fragility:
For over 30 years, the amino acid homocysteine has been implicated as a key component of atherosclerotic disease. [54–62] More direct observations point toward the disruption of the structures of collagen and elastin in the arterial wall:
In the majority of skin biopsies taken from patients with cervical arterial dissections, irregular collagen fibrils and elastic fiber fragmentations have been found. [63]
Homocysteine activates metalloproteinases [63] and serine elastases, [64] directly or indirectly leading to the decrease in vitro of the elastin content of the arterial wall. The opening and/or enlargement of fenestrae in the medial elastic laminae would be expected to lead to the premature fragmentation of the arterial elastic fibers and degradation of the extracellular matrix. [63–64]
Homocysteine has been shown to block aldehydic groups in elastin, inhibiting the cross-linking needed to stabilize elastin. [65]
The cross-linking of collagen may also be impaired by homocysteine. [66]
Experimentally elevated levels of homocysteine produce patchy desquamation of 10% of the aortic surface in baboons. [60]
Endothelium-dependent and flow-mediated vascular dilation is impaired in individuals with elevated levels of homocysteine. [62]
In cell culture experiments, addition of homocysteine into the medium induces cell detachment from the endothelial cell monolayer. [67]
Yet, even a tighter coupling between sCADs and increased amounts of homocysteine have been shown by the following observations:
Patients undergoing sCADs are more than three times as likely as asymptomatic patients to yield plasma homocysteine levels exceeding 12 micromoles/L. They are also more than twice as likely to have elevated homocysteine as patients experiencing ischemic strokes without arterial dissection. [68]
CAD patients yield average homocysteine levels of 17.9 micromoles/L while asymptomatic patients report an average of 6.0 micromoles/L. [69]
Homocysteine levels exceeding 10.2 micromoles/L are associated with a doubling of vascular risk. [70]
A genetic defect in humans involving tetrahydrofolate reductase, the enzyme which produces the methyl-donating cofactor required to convert homocysteine to methionine, is associated with elevations in the rates of sCADs. [68] This metabolic block would be expected to cause homocysteine to accumulate intracellularly. [71]
The striking association of homocysteine with sCAD raises the possibility that a relatively simple diagnostic test is at hand for determining patients at risk for sCAD and who would accordingly be advised to avoid cervical manipulation. Until recently, the gold standard methodology for determining plasma homocysteine has been high pressure liquid chromatography, gas chromatography, and mass spectrometry. [72–74] Fortunately, this cumbersome technology has recently been correlated with a much simpler enzyme conversion immunoassay [EIA] [75] An even more rapid assay method, by means of an automated analyzer is also available, requiring only microliter amounts of reagent and sample. [76] This essentially means that homocysteine levels can be determined in any number of clinical reference laboratories already established to measure blood analytes.
To date, the assessment options for vertebrobasilar artery risk each have significant drawbacks, and as a whole have been unable to identify any particular factor that is useful for screening. [77–78] Provocation tests in particular are problematic in that in several aspects they replicate the risks associated with cervical manipulation by requiring the placement of the head and neck in extreme extension and rotation. [79] False negative findings compared to angiograms have been reported; [80] reliability and validity have not been reliably tested; [77] and the suggestion has been made that these tests be de-emphasized. [81]In the midst of this disorder, determining homocysteine levels as a predictor of arterial fragility seems to be a plausible, rapid and inexpensive procedure that is no more invasive than a routine blood glucose determination.
FLAWED AND MISINTERPRETED MEDICAL LITERATURE
In the many flawed and frankly politically-driven journal publications [1–5] and media releases [6–11] which have implicated cervical manipulation as a causative factor for stroke, there are a number of common themes which represent their major shortcomings:
They fail to disclose that the majority of VBAs are spontaneous, cumulative, or caused by factors other than spinal manipulation;
They fail to disclose the potential benefits of the procedure in the interest of reporting true risk-benefit ratios;
They fail to place the risks of manipulation in the context of those produced by other medical treatments or lifestyle activities;
They fail to indicate the actual frequency of the manipulations administered;
They fail to account for the possibility that patients undergoing CVAs are reported more than once;
They fail to report the rates of CVAs following manipulation by parties other than licensed chiropractors; and
They incorrectly assume that patients undergoing adverse events following a manipulation would not report such instances to either the attending chiropractor or an appropriate authority.
The five leading journal publications will be discussed in some detail at the conference. Their flaws are so deep and ill-conceived as to have prompted the following response to one of them from Scott Haldeman:"Unfortunately, this article [82] tells us more about the biases of the surveyed neurologists, the authors, and the editorial board of Neurology than it does about the complications of manipulation. It should never have been published." [83]
It would thus appear that there are more than adequate arguments at hand to dismiss the vast majority of medical journal publications, which have thus far attempted to implicate cervical manipulation as a significant risk factor for cervical artery dissections leading to stroke. Indeed, the biases implicit in many of these journal articles seem no less far-reaching than P.J. O'Rourke's provocative argument questioning the relationship of high-tension power lines and the incidence of cancer:
"Watch as I create ‛statistical evidence that power-line locations affect cancer rates.’ I can do this despite the fact that I know nothing about electricity, or medicine, and not much [says my bank] about math. Power lines are found all over the country, arranged in an orderly fashion aptly called a grid. Cancer occurs more randomly. Random, of course, does not mean evenly spread. Randomness comes in blots and clusters. Flip a penny a thousand times, and you'll see some long streaks of Lincolns, as if that coin did indeed have two heads. Now give me a map of the power grid, and a map of cancer occurrences. I will find groups of cancer victims near high-tension lines. I will also find groups of cancer victims near bookstores where Paul Brodeur, author of Currents of Death: Power Lines, Computer Terminals, and the Attempt to Cover Up Their Threat to Your Health made promotional appearances and signed books." [84]
Conclusions:
Thus, it would appear that the tearing of the arterial wall in a dissection is both cumulative and spontaneous: cumulative, in that repeated, low-grade insults to the artery would most likely be required to yield a dissection; and spontaneous, in that these more minor impositions occur by dint of any number of self-imposed maneuvers, as well as any by a practitioner– making it extremely difficult, if not impossible to distinguish between the two. Finally, spontaneous dissections appear to correlate with the fragility of the arterial wall, which may be attributable to inborn errors of metabolism, which might be detectable by means of a homocysteine assay.
Many signs point to intrinsic aberrations of arterial structure underlying CVAs, many brought on by elevated levels of homocysteine. When applied to cervical manipulations, the body of evidence outlined in this report suggests that the inherent fragility of the arterial wall of the cerebrovascular system, rather than any trauma associated with maneuvers by the attending physician, is the major culprit regarding arterial dissections. The actual risk of CVAs that can be directly attributable to spinal manipulation may be reduced to far less conspicuous levels when compared to everyday lifestyle risks, and those brought on by medical treatments widely accepted by the public. Certainly the propagation of risk estimates attributable to visits to the chiropractor's office without adequate justification from data does not perform a useful service to the public; indeed, it does just the opposite. The determination of homocysteine levels as a clinical tool would appear to afford the chiropractic physician a means to bring the actual risks of CVAs to even lower levels than those previously reported. In this regard, homocysteine determinations currently appear to be the most plausible means for assessing patients who are most at risk for experiencing CVAs from routine activities, let alone from cervical manipulations. CVAs have been listed as only the fifth most common cause of malpractice lawsuits, unlikely if chiropractors were conclusively found at fault for the majority of CVAs reported. [85]Indeed, the overall mortality rates of the general population [0.00057%] has been shown to more than twice that of patients specifically undergoing spinal manipulative therapy. [44]
References:
1. Lee KP, Carlini WG, McCormick GF, Walters GW.
Neurologic Complications Following Chiropractic Manipulation: A Survey of California Neurologists
Neurology 1995; 45 (6): 1213-1215
2. Bin Saeed A, Shuaib A, Al Sulaiti G, Emery D.
Vertebral Artery Dissection: Warning Symptoms, Clinical Features and Prognosis in 26 Patients
Canadian Journal of Neurological Sciences 2000 (Nov); 27 (4): 292–296
3. Hufnagel A, Hammers A, Schonle P-W, Bohrn K-D, Leonhardt G.
Stroke Following Chiropractic Manipulation of the Cervical Spine
Journal of Neurology 1999; 246 (8): 683-688
4. Norris JW, Beletsky V, Nadareishvili ZG.
Sudden Neck Movement and Cervical Artery Dissection
CMAJ. 2000 (Jul 11); 163 (1): 38–40
5. Rothwell DM, Bondy SJ, Williams JI.
Chiropractic Manipulation and Stroke:
A Population-based Case-control Study
Stroke 2001 (May); 32 (5): 1054-1060
6. Brody J.
When Simple Actions Ravage Arteries.
New York Times, April 30, 2001
7. Bill Carroll Show,
CFRB 1010 radio, February 6, 2002, posted on the internet
8. Evenson B.
National Post, February 7, 2002
9. Hamburg J,
Medical Minute,
WOR AM 710 radio, February 22,2002
10. Jaroff L.
Back Off, Chiropractors!
TIME.com, February 27, 2002
11. A Different Way To Heal ~ Episode of
Scientific American Frontiers
Public Broadcasting System telecast, June 4, 2002.
12. Terrett AGJ.
Current Concepts in Vertebrobasilar Complications Following Spinal Manipulation
West Des Moines, IA: NCMIC Group, Inc., 2001
13. Parenti G, Orlandi G, Bianchi M, Renna M, Martini A, Mum L.
Vertebral and Carotid Artery Dissection Following Chiropractic Cervical Manipulation
Neurosurgery Review 1999; 22 (2-3): 127-129
14. Peters M, Bohn J, Thomke F, Kallen KJ, Mahlzahn K, Wandel E, Meyer zum Buschenfelde KH.
Dissection of the Internal Carotid Artery After Chiropractic Manipulation of the Neck
Neurology 1995 (Dec); 45: 496-500
15. Beatty RA.
Dissecting Hematoma of the Internal Carotid Artery Following Chiropractic Cervical Manipulation
Journal of Trauma 1977 (Mar); 17 (3): 248-249
16. Terrett AGJ, Kleynhans AM. Cerebrovascular Complications of Manipulation.
In: Haldeman, S. Principles and Practice of Chiropractic, Norwalk, CT: Appleton & Lange, 1992, pp. 579-598
17. Klougart N, Leboeuf-Yde C, Rasmussen LR.
Safety in Chiropractic Practice Part II: Treatment to the Upper Neck
and the Rate of Cerebrovascular Incidents
J Manipulative Physiol Ther 1996 (Nov); 19 (9): 563–569
18. Haynes MJ, Cala LA, Melsom A, Mastaglia FL, Milne N, McGeachie JK.
Vertebral Arteries and Cervical Rotation: Modeling and Magnetic Resonance Angiography Studies
J Manipulative Physiol Ther 2002 (Jul); 25 (6): 370–383
19. Symons, B., Leonard, T.R., Herzog, W., 2002.
Internal Forces Sustained by the Vertebral Artery
During Spinal Manipulative Therapy
J Manipulative Physiol Ther 2002 (Oct); 25 (8): 504–510
20. Rosner A.
Musculoskeletal Research
In: Redwood OM, Cleveland C III. Fundamentals of Chiropractic.
New York, NY: Churchill Livingstone 2003, in press
21. Good C. Letter to the editor
J Manipulative Physiol Ther 2003; 26: Submitted for publication
22. Haynes MJ, Lesley AC, Melsom A, Mastaglia FL, Minle N, McGeachies JK.
Vertebral Arteries and Cervical Rotation: Modeling and Magnetic Resonance Angiography Studies
J Manipulative Physiol Ther 2002 (Jul); 25 (6): 370-383
23. Meeker WC, Mootz RO, Haldeman S.
Back To Basics...The State of Chiropractic Research
Topics in Clinical Chiropractic 2002; 9 (1): 1-13
24. Meeker WC, Haldeman S.
Chiropractic: A Profession at the Crossroads of Mainstream and Alternative Medicine
Annals of Internal Medicine 2002 (Feb 5); 136: 216-227
25. Froehle RM.
Ear Infection: A Retrospective Study Examining Improvement from Chiropractic Care and Analyzing for Influencing Factors
J Manipulative Physiol Ther 1996 (Mar); 19 (3): 169-177
26. Fallon J.
The Role of Chiropractic Adjustment in the Care and Treatment of 332 Children with Otitis media
Journal of Clinical Chiropractic Pediatrics 1997; 2 (2): 167-183
27. Degenhardt BF, Kuchera ML.
Efficacy of Osteopathic Evaluation and Manipulative Treatment in Reducing the Morbidity of Otitis media in Children
Journal of the American Osteopathic Association 1994; 94 (8): 673
28. Dvorak J, Orelli F.
How Dangerous is Manipulation of the Cervical Spine?
Manual Medicine 1985; 2: 1-4
29. Patijn J.
Complications in Manual Medicine: A review of the Literature
Manual Medicine 1991 ;6: 89-92
30. Haldeman S, Chapman-Smith D, Peterson OM.
Guidelines for Chiropractic Quality Assurance and Practice Parameters.
Gaithersburg, MO: Aspen Publishers, 1993, 170-172
31. Jaskoviak PA.
Complications Arising from Manipulation of the Cervical Spine
J Manipulative Physiol Ther 1980; 3: 213-219
32. Henderson OJ, Cassidy JO.
Vertebral artery syndrome:
In: Vernon H, ed. Upper Cervical Syndrome: Chiropractic Diagnosis and Treatment.
Baltimore: Williams & Wilkins, 1988. 195-222
33. Hurwitz EL, Aker PO, Adams AH, Meeker WC, Shekelle PG.
Manipulation and Mobilization of the Cervical Spine: A Systematic Review of the Literature
Spine (Phila Pa 1976) 1996 (Aug 1); 21 (15): 1746–1760
34. Carey PF.
A Report on the Occurrence of Cerebral Vascular Accidents in Chiropractic Practice
Journal of the Canadian Chiropractic Association 1993; 57 (2): 104-106
35. National Chiropractic Mutual Insurance Company, unpublished case records 1991-1993
36. Haldeman S, Carey P, Townsend M, Papadopoulos C.
Arterial Dissections Following Cervical Manipulation: The Chiropractic Experience
Canadian Medical Association Journal (CMAJ) 2001 2001 (Oct 2); 165: 905–906
37. RA Deyo, DC Cherkin, JD Loeser, SJ Bigos and MA Ciol
Morbidity and Mortality in Association with Operations on the Lumbar Spine. The Influence of Age, Diagnosis, and Procedure
Journal of Bone and Joint Surgery 1992 (Apr 1); 74 (4): 536–543
38. Seagroatt V, Tan HS, Goldacre M, Bulstrode C, Nugent I, Gill L
Elective Total Hip Replacement: Incidence, Emergency Readmission Rate, and Postoperative Mortality
British Medical Journal 1991 (Dec 7); 303 (6815): 1431–1435
39. Seagroatt V, Tan HS, Goldacre M, Bulstrode C, Nugent I, Gill L
Comparison of Postoperative Mortality and Morbidity in Veterans Affairs and Nonfederal Hospitals
Journal of Surgical Research 1994 (May); 56 (5): 405–416
40. Roebuck, DJ
Diagnostic Imaging: Reversing the Focus
Medical Journal of Australia 1995; 162 (5): 175
41. Horowitz SH
Peripheral Nerve Injury and Causalgia Secondary to Routine Venipuncture
Neurology 1994 (May); 44 (5): 962–964
42. Dabbs V Lauretti WJ
A Risk Assessment of Cervical Manipulation vs. NSAIDs for the Treatment of Neck Pain
J Manipulative Physiol Ther 1995 (Oct); 18 (8): 530–536
43. Dinman BD
The Reality and Acceptance of Risk
JAMA 1980 (Sep 12); 244 (11): 1226–1228
44. Rome PL.
Perspectives: An Overview of Comparative Considerations of Cerebrovascular Accidents
Chiropractic Journal of Australia 1999; 29 (3): 87-102 ~ FULL TEXT
45. Rosner A.
Chiropractic Manipulation and Stroke [Letter to the Editor]
Stroke 2001; 32 (9): 2207-2208
46. Haldeman S.
Chiropractic Complications [Letter to the Editor]
Neurology 1996;46: 885
47. Terrett AGJ.
Misuse of the Literature by Medical Authors in Discussing Spinal Manipulative Therapy
J Manipulative Physiol Ther 1995; 18 (4): 203-210
48. Shievink WT, Mokri, B, O'Falion WM.
Recurrent Spontaneous Cervical-artery Dissection
New England Journal of Medicine 1994; 330 (6): 393-397
49. Shievink WT, Mokri B, Whisnant JP.
Internal Carotid Artery Dissection in a Community: Rochester, Minnesota, 1987-1992
Stroke 1993; 24 (11): 1678-1680
50. Giroud M, Fayolle H, Andre N, Dumas R, Becker F, Martin D, Baudoin N, Krause D. Incidence of Internal Carotid Artery Dissection in the Community of Dijon [Letter]
J Neurol Neurosurg Psychiatry 1994; 57(11): 1443
51. Carey TS, Garrett J, Jackman A, et al.
The Outcomes and Costs of Care for Acute Low Back Pain Among Patients
Seen by Primary Care Practitioners, Chiropractors, and Orthopedic Surgeons
New England J Medicine 1995 (Oct 5); 333 (14): 913–917
52. Terrett, AGJ.
Malpractice Avoidance for Chiropractors.
1. Vertebrobasilar Stroke Following Manipulation
Des Moines, IA. National Chiropractic Mutual Insurance Company, 1996
53. Foye PM, Najar MP, Camme A Jr, Stitik TP, DePrince ML, Nadler SF, Chen B.
Prospective Study of Pain, Dizziness, and Central Nervous System Blood Flow in Cervical Extension: Vascular Correlations to Beauty Parlor Stroke Syndrome and Salon Sink Radiculopathy
American Journal of Physical Medicine and Rehabilitation 2002; 81 (6): 395-399
54. Graham 1M, Daley LE, Refsum HM, Robinson K, Brattstrom LE, Ueland PM, Palma-Reis RJ, Boers GH, Sheahan RG, Israelsson B, Uiterwaal CS, Meleady R, McMaster D, Verhoef P, Witterman J, Rubba P, Bellet H, Wautrecht JC, de Valk HW, Sales Luis AC, Parrot-Rouland RM, Tan KS, Higgins I, Garcon D, Medrano MJ, Candito M, Evans AE, Andria G.
Plasma Homocysteine as a Risk Factor for Vascular Disease: The European Concerted Action Project
Journal of the American Medical Association 1997; 277: 1775-1781
55. McCully KS.
Vascular Pathology of Homocysteinemia: Implications for Pathogenesis of Arteriosclerosis
American Journal of Pathology 1969; 56 (1): 111-128
56. Selhub J, Jacques PF, Bostom AG, D'Agostino RB, Wilson PW, Belanger AJ, O'Leary DH, Wolf PA, Schaefer EJ, Rosenberg IH.
Association Between Plasma Homocysteine Concentrations and Extracranial Carotid Artery Stenosis
New England Journal of Medicine 1995; 332(5): 286-291.
57. Wald NJ, Watt HC, Law MR, Weir DG, McPartlin J, Scott JM.
Homocysteine and Ischemic Heart Disease: Results of a Prospective Study with Implications Regarding Prevention
Archives of Internal Medicine 1998; 158 (8): 862-867
58. Nygard 0, Nordehaug JE, Refsum H, Ueland PM, Farstad M, Vollset SE,
Plasma Homocysteine Levels and Mortality in Patients with Coronary Artery Disease
New England Journal of Medicine 1997; 337 (4): 230-236
59. Stampfer MJ, Malinow R, Willett WC, Newcomer LM, Upson B, Ullmann D, Tishler PV, Hennekens CH.
A Prospective Study of Plasma Homycysteine and Risk of Myocardial Infarction in US Physicians
Journal of the American Medical Association 1992; 268 (7): 877-881
60. Harker LA, Slichter J, Scott CR, Russell R.
Homocysteinemia: Vascular Injury and Arterial Thrombosis
New England Journal of Medicine 1974; 291: 537-543
61. Lenz SR, Sobey CG, Piegors DJ, Bohoptakar MY, Faraci FM, Malinow MR, Heistad DD.
Vascular Dysfunction in Monkey with Diet-induced Hyperhomocysteinemia
Journal of Clinical Investigation 1996; 98: 24-29
62. Woo KS, Chook P, Lolin YI, Cheung AS, Chan L T, Sun YV, Sanderson JE, Metreweli C, Celermajar DS.
Hyperhomocysteinemia Is a Risk Factor for Endothelial Dysfunction in Humans
Circulation 1997; 96: 2542-2544
63. Charplot P, Bescond A, Augler T, Chereyre C, Fratermo M, Rolland PH, Garcon D.
Hyperhomocysteinemia Induces Elastolysis in Minipig Arteries: Structural Consequences, Arterial Site Specificity and Effect of Captoprilhydrochlorothiazide
Matrix Biology 1998; 17: 559-574
64. Rahmani DJ, Rolland PH, Rosset E, Branchereau A, Garcon D.
Homocysteine Induces Synthesis of a Serine Elastase in Arterial Smooth Muscle Cells From Multi-organ Donors
Cardiovascular Research 1997; 34 (3): 597-602
65. Jackson SH.
The Reaction of Homocysteine With Aldehyde: An Explanation of the Collagen Defects in Homocystinuria
Clinica Chimica Acta 1973; 45 (3): 215-217
66. Kang AH, Trelstad RL.
A Collagen Defect in Homocystinuria
Journal of Clinical Investigation 1973; 52 (10): 2571-2578
67. Wall RT, Hanan JM, Harker LA, Striker GF.
Homocysteine-induced Endothelial Cell Injury in Vitro: A Model for the Study of Vascular Injury
Thrombolytic Research 1980; 18: 113-121
68. Pezzini A, Del Zotto E, Archetti S, Negrini R, Bani P, Albertini A, Grassi M, Assanelli D, Gasparotti R, Vignola LA, Magoni M, Padovani A.
Plasma Homocysteine Concentration, C677T MTHFR Genotype, and 844-ins68bp Genotype in Young Adults with Spontaneous Cervical Artery Dissection and Atherothrombotic Stroke
Stroke 2002; 33(3): 664-669.
69. Gallai V, Caso V, Paciaroni M, Cardaioli G, Arning E, Bottiglieri T, Pernetti L.
Mild Hyperhomosycteinemia: A Possible Risk Factor for Cervical Artery Dissection
Stroke 2001; 32: 714-718
70. Graham 1M, Daley LE, Refsum HM, Robinson K, Brattstrom LE, Ueland PM, Palma-Reis RJ, Boers GH, Sheahan RG, Israelsson B, Uiterwaal CS, Meleady R, McMaster D, Verhoef P, Witterman J, Rubba P, Bellet H, Wautrecht JC, de Valk HW, Sales Luis AC, Parrot-Rouland RM, Tan KS, Higgins I, Garcon D, Medrano MJ, Candito M, Evans AE, Andria G.
Plasma Homocysteine as a Risk Factor for Vascular Disease: The European Concerted Action Project
Journal of the American Medical Association 1997; 277: 1775-1781.
71. Lehninger AL, Nelson DL, Cox MM.
Principles of Biochemistry.
2nd Edition. New York, NY: Worth, 1993, pp 524-526
72. Ueland PM, Refsum H, Stabler SP, Mainow MR, Anderson A, Allen RH.
Total Homocysteine in Plasma and Serum: Methods and Clinical Applications
Clinical Chemistry 1993; 39 (9): 1764-1779
73. Stabler SP, Marcell PO, Podell ER, Allen RH.
Quantitation of Total Homocysteine, Total Cysteine, and Methionine in Normal Serum and Urine Using Capillary Gas Chromatography-mass Spectrometry
Analytical Biochemistry 1987; 162(1): 185-196
74. Pietzsch J, Julius U, Hanefeld M.
Rapid Determination of Total Homocysteine in Human Plasma by Using N(O,S)-ethoxycarbonyl Ethyl Ester Derivatives and Gas Chromatography-mass Spectrometry
Clinical Chemistry 1997; 43 (10): 2001-2004
75. Frantzen F, Faaren AL, Alfheim I, Nordhei AK.
Enzyme Conversion Immunoassay for Determining Total Homocysteine in Plasma or Serum
Clinical Chemistry 1998; 44 (2): 311-316
76. Shipchandler MT, Moore EG.
Rapid, Fully Automated Measurement of Plasma Homocysteine with the Abbott IMx Analyzer
Clinical Chemistry 1995; 41(7): 991-994.
77. Haldeman S, Kohlbeck FJ, McGregor M.
Unpredictability of Cerebrovascular Ischemia Associated with Cervical Spine Manipulation Therapy:
A Review of Sixty-four Cases After Cervical Spine Manipulation
Spine (Phila Pa 1976) 2002 (Jan 1); 27 (1): 49–55
78. McGregor M, Haldeman S, Kohlbeck FJ.
Vertebrobasilar Compromise Associated With Cervical Manipulation
Topics in Clinical Chiropractic 1995; 2(3): 63-73.
79. Terrett AGL.
It Is More Important To Know When Not to Adjust
Chiropractic Technique 1990; 2: 1-9
80. Bolton PS, Stick PE, Lord RSA.
Failure of Clinical Tests to Predict Cerebral Ischemia Before Neck Manipulation
J Manipulative Physiol Ther 1989; 12 (4): 304-307
81. Ferezy JS.
Neural Ischemia and Cervical Manipulation: An Acceptable Risk
ACA Journal of Chiropractic 1988; 22: 61-63
82. Lee KP, Carlini WG, McCormick GF, Walters GW.
Neurologic Complications Following Chiropractic Manipulation: A Survey of California Neurologists
Neurology 1995; 45: 1213-1215
83. Haldeman S.
Letter to the editor.
Neurology 1996; 46: 885
84. 0'Rourke PJ.
All the Trouble in the World,
New York, NY: The Atlantic Monthly Press, 1994, pp. 154-155
85. Type of Loss Atudy: Malpractice Only For Loss Year 1995.
Des Moines, IA: National Chiropractic Mutual Insurance Company
as reported in Jagbandhansingh, MP.
Most common causes of chiropractic malpractice lawsuits.
J Manipulative Physiol Ther 1997; 20 (1): 60-64




Table 1
Probability of Stroke or Serious Adverse Events Following Cervical Manipulation Source Methods Risk Dvorak [28] Survey of 203 members of Swiss Society of Manual Medicine [all non-chiropractors] 1 serious complicaton /400,000 Patijn [29] Review of computerized registration system in Holland 1 serious complicaton /518,000 Haldeman [30] Extensive literature review to formulate practice guidelines 1-2 strokes /1,000,000 Jaskoviak [31] Clinical files of National College 0 complication/
5,000,000 in 15 year periodHenderson/
Cassidy [32]Canadian Memorial Chiropractic College Clinic 0 complication/
5,000,000 in 9 year periodHurwitz [33] RAND Cervical Study Literature Review 0.64 Serious Complications /1,000,000
0.27 Deaths/ 1,000,000Carey [34] Claim Review: Canada's Largest Malpractice Insurance Company 1 CVA/ 3,000,000
0 Deaths in 5 Year PeriodNCMIC [35] Claim Review: Principal Chiropractic Malpractice Insurance Company Within the U.S. 1 CVA/ 2,000,000
in a 3 Year PeriodHaldeman [36] Claim Review: Canada's Largest Malpractice Insurance Company 0.17 CVA/ 1,000,000
in a 10 Year Period




Table 2 Risk in Perspective:
Comparison of Death Rates Attributed to Various Causes [1]Risk Frequency
(per Million)Neurological Complications From Cervical Manipulations 0.3 [33] Canoeing 3 [43] Soccer or Football 39 [43] Venipuncture 40 [41] Drinking: 1 Bottle of Wine per Day 75 [43] Automobile Driving (United Kingdom) 169 [43] Nuclear Bone Scan 333 [40] GI Bleeding Due to NSAID Use 400 [42] Spinal Surgery 700 [37] Smoking: 20 Cigarettes per Day 5000 [43] Appendectomies 13,500 [39] Total Hip Replacement 4900-15,300 [38] Motorcycling 20,000 [43]




Table 3
Rates of Stroke Compared to Incidence of Arterial Dissections Attributed Cause Rate per Million Spontaneous, hospital-based [48] 10-15 Spontaneous, community-based [49-50] 25-30 Cervical manipulation [28] 25 Cervical manipulation [30] 10-20* Cervical manipulation [31] 0 Cervical manipulation [33] 6.4* Cervical manipulation [36] 1.7* *Corrected to represent the average incidence per patient, assuming the average number of manipulations per patient to equal 10, as reported in the literature. [51]




Table 4 A
Selected Activities Suspected of Disrupting Cerebral Circulation [ 44]
Angiography
Bleeding nose
Axial traction
Calisthenics
Cervical extension for xrays or CTS
Cervical rotation while backing up a car
Coughing
Dental procedure
Football
Gymnastics
Hanging out washing
Overhead work
Roller coaster
Telephone call
Traction and short wave diathermy
Trampoline
Watching aircraft
Yawning




Table 4 B
Nonmanipulative Maneuvers Associated With CVAs [ 52]
Archery
Beauty parlor stroke
By surgeon or anethetist during surgery
Calisthenics
Childbirth
Emergency resuscitation
Fitness exercise
Neck extension during radiography
Neck extension for a bleeding nose
Overhead work
Rap dancing
Sleeping position
Star gazing
Swimming
Tai Chi
Turning the head while driving a vehicle
Wrestling
Yoga










| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |