

Joint Assessment – P.A.R.T.S. This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: Topics in Clinical Chiropractic 2000; 7 (3): 1–10 ~ FULL TEXT
Thomas F. Bergmann, DC, Bradley A. Finer, DC, DACAN
Professor, Clinical Science Division
Northwestern Health Sciences University
College of Chiropractic
Bloomington, Minnesota
Purpose: An approach to systematically perform clinical work-up for chiropractic subluxation is proposed. Literature on assessment approaches is reviewed and a discussion is presented.
Method: A qualitative review of clinical and scientific literature related to assessment methodologies for subluxation was performed.
Summary: Variation in assessment techniques exists for identification of spinal and other articular joint dysfunction. Useful scientific data also are limited to only a few approaches, and there is a need for a more systematic assessment approach profession wide.
There are more articles like this @ our:
LOCATING SUBLUXATIONS PageKey words: Articular range of motion, chiropractic, Medicare, palpation, physical examination, subluxation
From the FULL TEXT Article
Background
Doctors of chiropractic are portals of entry to the health care system for many patients seeking health care services. As such, they must maintain broad and thorough assessment/diagnostic skills. Before employing any therapy, a clinician must first determine if there is a need for treatment. Therefore, the clinical information that any primary contact provider would want, including a case history, physical examination, clinical laboratory findings, radiographic findings, and any other tests necessary to check for suspected health problems, is needed. Having gathered and interpreted this information, it must be processed in order to arrive at a sound clinical conclusion. The role of this assessment process in the chiropractic office is to determine whether the patient should receive chiropractic care only, chiropractic care in concert with other forms of health care, or a referral to another health care professional for some other form of stand-alone management such as acute, crisis care. This article suggests the need for, and possible form of, a standardized assessment procedure for use by chiropractic clinicians.
INTRODUCTION
Most patients seeking the services of health care professionals, including doctors of chiropractic, present with problems or complaints. It is therefore necessary to identify the nature and extent of the patient's problem before initiating treatment. A comprehensive examination is a critical step in the management of patients with musculoskeletal problems. The role of the evaluative process is to differentiate a particular pathologic process from other possible causes of the presenting signs and symptoms. It also aids the clinician in clarifying the nature and extent of the lesion and to establish a basis on which to judge progress. This information allows a clinician to develop and implement indicated treatment procedures and determine their effectiveness.
While the chiropractic examination considers all aspects, it especially emphasizes the assessment of the spinal column and the nervous system. The chiropractic articular spinal examination is unparalleled in the healing arts. As the most specialized and significant therapy used by the doctor of chiropractic involves the adjustment of the articulations of the human body, the articular examination becomes the focal point of the patient's evaluation. There remains, however, a great deal of controversy among chiropractors, as well as other practitioners of manual therapy, as to the most valid, objective, and efficient means of detecting joint dysfunction.
The fundamental malady treated by doctors of chiropractic is the joint dysfunction commonly referred to as subluxation, vertebral subluxation complex (VSC), or vertebral subluxation syndrome (VSS). The traditional chiropractic portion of physical examination identifies the subluxation. The balance of the examination portion can be considered to focus on identification of pathophysiologic problems that may be associated with the subluxation. The identification of other findings will serve as a modifier or qualifier to the subluxation. Identifying the various attributes of subluxation may help clarify why one patient responds quickly to treatment while another responds slowly or not at all. The evaluation data also may serve as a means for deciding which form of manual therapy is best suited for the particular patient. Because a subluxation is considered an abnormal change in the normal function of the joint, specific criteria should be used to identify it. A plethora of technique procedures is available to the chiropractic practitioner. The literature identifies more than 100 individual named techniques. [1] Most of the chiropractic technique systems were started by interested and probing doctors who noticed regularity in their results. These approaches typically developed into systems of assessment and treatment. The fallacy of many of the system approaches is that the evaluation procedures that are linked to the manipulative procedures are often singular and very simplistic. These systems are often alluring because the assessment normally takes only a short period of time and the indicated therapy is directly determined.

Figure 1

Figure 2 In addition, little mental energy needs be expended. However, because the human body is a very complex and integrated organism, relying on a single evaluative tool to determine the specific therapeutic intervention is not considered sound clinical practice. Figures 1 and 2 demonstrate the evaluative sequence to consider when addressing patients with neck and low back pain, respectively. Furthermore, confusion abounds when patients go from one practitioner to another, being evaluated and treated in significantly different ways. Third-party payers and legal professionals have difficulty determining what is being treated. Finally, communication between practitioners is difficult because of the number of evaluative procedures.
Therefore, the chiropractic profession could benefit from greater standardization of the approach to the evaluation of joint structure and function leading to the identification of subluxation. A standard approach will allow for comparisons regarding effectiveness and efficiency of different treatment methods. Standardization will also help to diminish the confusion that occurs when patients see different chiropractors. It is quite likely, however, that the detection of joint dysfunction/subluxation may never be a precise science. Any method of joint dysfunction detection is susceptible to false positive, false negative, and equivocal findings. More research must be done to demonstrate that the techniques chiropractors use to identify a subluxation are reliable and valid and provide information for further refinement of accurate, efficient, and effective methods. However, in the absence of such research, clinicians still need a rational approach to assessment, based on best available information, sound judgment, and clinical experience.
THE PARTS EVALUATION
Structural evaluation of joint dysfunction will be viewed in terms of a multidimensional index of segmental abnormality. However, the examination of musculoskeletal system is not done in isolation, but within the context of the history and physical examination of the patient. The methods used in articular examination are the same as those used in other aspects of the evaluation process (ie, observation, palpation, percussion, and auscultation). Practitioners using various forms of manual therapy must use all of their senses to decide where and how to treat the patient, making the examination much more than history taking and performing orthopaedic tests. [2]
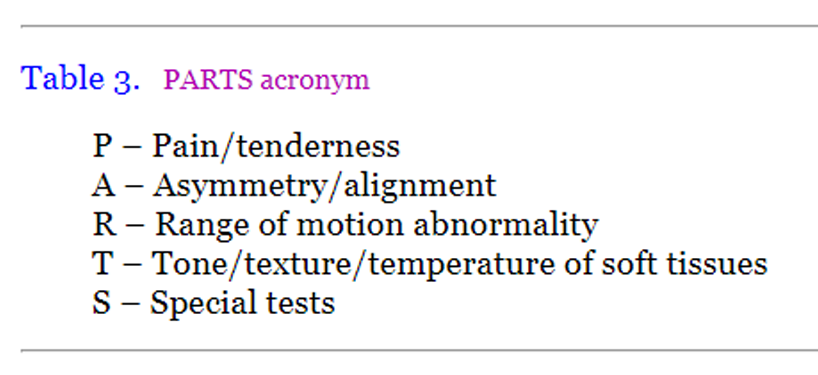
Given the complexity of the musculoskeletal system and the relative inconclusiveness in published studies that attempt to evaluate the reliability and validity of single assessment procedures, an approach to the examination that employs multiple evaluative procedures is worth consideration. The accumulation of examination data determines if there is a preponderance of evidence indicating the specific diagnosis of subluxation. The proposed multidimensional index for spinal evaluation is derived from the acronym PARTS. It comprises a five-part assessment that provides a wide variety of data, and thus builds, in a systematic way, upon the concept of employing multiple evaluative procedures. Although the individual components are objective and used daily by most chiropractors, this information is unfortunately not commonly recorded in any systematic fashion. The five diagnostic criteria for subluxation that constitute PARTS are listed in Table 1.
Table 3. PARTS acronym
P – Pain/tenderness
A – Asymmetry/alignment
R – Range of motion abnormality
T – Tone/texture/temperature of soft tissues
S – Special tests
Pain/tenderness
Findings of pain and tenderness are identified through observation, percussion, provocation, and palpation. The perception of pain and tenderness is evaluated in terms of location, quality, and intensity. Many musculoskeletal disorders are made evident principally by pain. The patient's description and location of pain may be obtained verbally, physically, or by a pain drawing. The location and intensity of tenderness produced by palpation of osseous and soft tissues should be noted. Furthermore, changes in pain intensity should be objectified through the use of a visual analog scale (VAS), algometer, or pain questionnaire. The production of palpatory pain over osseous and soft tissues has been found to have high degrees of inter- and intra-examiner reliability. [3–5] However, validity studies have not been done.
Pain is the usual reason that individuals seek the services of a physician, and it is considered a subjective finding. There is a general contention that subjective findings have less significance than findings that are "objective." However, many so-called objective tests rely on the patient's report of pain. For example, the straight leg raise test is considered an objective test, however, it is the patient report ofleg pain that constitutes a positive test. This is no different from applying pressure over osseous or soft tissue structures and having the patient report the presence or absence of pain. Therefore, the use of provocative tests to localize a painful area is a useful means for identifying musculoskeletal problems, including subluxation. These manual physical maneuvers are designed to reproduce the patient symptoms or verify the location of pain, thereby supporting the local presence of a dysfunctional process. Typically, these tests stretch, compress, or distract specific anatomic structures while the doctor solicits a report of pain by the patient. When patients experience pain due to one of these mechanical tests, there is likely to be a local mechanical component contributing to their condition.
Unfortunately, a frequent clinical difficulty arises because the site of pain does not always correspond well with the site of lesion. The patient often describes radiating patterns of pain, cutaneous patterns of hyperalgesia/hypalgesia, or tenderness to palpation at sites distant from the site of pathophysiology. These patterns may correspond to known patterns of myotomes, dermatomes, and sclerotomes. Dermatomal pain will usually be sharp, shooting, superficial, and well localized. Sclerotomal pain is typically deep, dull, aching, and poorly localized. Charts are available depicting these various patterns of peripheral pain. [6]
Asymmetry/alignment
Asymmetric qualities on a sectional or segmental level are noted. It includes observation of posture and gait, as well as palpation for misalignment of joint structures. Findings of asymmetry are identified through observation (posture and gait analysis), static palpation, and static X-ray analysis. Static palpation is performed with the patient in a stationary position, and it is often further subdivided into bony and soft tissue palpation.
The major goal of bony palpation is to locate bony landmarks and assess contour for any joint malpositions, anomalies, or tenderness. Typically, the palmar surfaces of the fingers or thumbs are used because they are richly endowed with sensory receptors. Light pressure is used for superficial structures, gently increasing pressure for deeper landmarks. During spinal palpation, the pelvic, lumbar, and thoracic regions are customarily evaluated with the patient in the prone position and the patient's cervical spine in the sitting or supine position. The spinous processes (SPs), transverse processes (TPs) in the thoracic spine, articular pillars (APs) in the cervical spine, and mammillary processes (MPs) in the lumbar spine are palpated for tenderness and compared for contour and alignment. Individual motion segments are often located relative to these bony landmarks. It is important to appreciate the anatomic relationship of the lateral processes (TPs, MPs, APs) to the corresponding spinous processes. Rotational and lateral flexionmal positions are usually determined by the relationship of the lateral processes, while flexion and extension malpositions are usually determined by the spinous processes. Misaligned articular structures do suggest joint subluxation/dysfunction, but appareht joint malpositions may result from anomaly or compensation without dysfunction. Spinal landmarks, especially the spinous process, are prone to congenital or developmental malformation. Disrelationship between adjacent spinous process can be misinterpreted when a physical malformation exists. Therefore, static palpation using the SPs should not be relied on to identify true misalignment in rotation or lateral flexion. Furthermore, the spine functions as a kinetic chain, and disease or dysfunction at one level may force adaptational alterations in neutral alignment at adjacent levels. These sites of compensatory change may palpate as being malpositioned (out of ideal neutral alignment) yet have normal and pain-free function.
Radiographic assessment and determination of joint subluxation have been integral parts of chiropractic evaluation since the early 1900s. [7–9] Relative to the assessment of biomechanical relationships, the primary focus has been on the measurement and description (listing) of spinal joint malpositions. To that end, the profession and many of its individual technique innovators have developed specific radiographic measurement techniques (spinography) to quantify and classify spinal malpositions and subluxations. [10–16] Proponents of radiographic evaluation for the detection of spinal subluxations claim that the X-ray is the best method for accurately determining the level and direction of vertebral malposition. [8] Spinal X-rays are routinely taken with the patient in an upright (weight-bearing) position and may include the selection of full spine or sectional anterior to posterior and lateral views.
Traditionally, the alignment of the upper vertebrae is compared with the lower vertebrae, and any malpositions are recorded accordingly. [8, 10, 11] Though much of the profession uses some form of radiographic measurement and assessment of spinal subluxation, there is considerable controversy as to whether radiographic evaluation should play a significant role in the diagnosis of spinal subluxation syndromes. [7, 9, 12, 17–20] Claims of accuracy in detecting minor joint malpositions may not be supportable against the technical limitations of radiography. [7, 9, 12, 17, 21–26] Inherent radiographic magnification and distortion, patient positional errors, and the exactness of marking procedures are common concerns. Interrater and intrarater reliability have been investigated on a few of the profession's unique spinographic procedures, and the results are mixed. [7, 13, 24, 27–40] Harrison and colleagues [19] reviewed the literature regarding the reliability of spinal displacement analysis using plain film X-rays and concluded that X -ray line drawing is reliable. This conclusion is based on their assertion that there is an ideal normal spinal configuration based on a mathematical model and that radiographic marking procedures can identify real spinal displacements. However, the vast majority of cited reliability studies were on curve measurements not spinal segment position. Furthermore, they did not address validity. Haas and coworkers [20] challenged these conclusions by questioning the biologic plausibility of an ideal spine, the clinical sensibility, lack of validation, clinical utility, and appropriateness. They concluded that there is currently no justification for the routine use of radiographic spinal displacement analysis in clinical practice. Although recent attempts [7, 23, 29, 30, 35] have been made to address issues of spinographic reliability, very little has been done to investigate the validity of radiographic measurement in diagnosing and treating spinal dysfunction.
Range of motion abnormality
Changes in active, passive, and accessory joint motions are noted. These changes may be an increase or decrease in mobility. An interosseus decrease in motion is a common component of joint dysfunction. Range of motion abnormalities are identified through motion palpation and stress X-ray. Motion palpation is performed during active or passive joint movement and involves the evaluation of accessory joint movements. In most joint positions, a joint has some "play" because joint surfaces do not fit tightly and the capsule and ligaments remain somewhat lax. This joint play is essential for normal joint function. Movement at a joint cannot occur around a rigid axis because the joint surfaces are of varying radii. The joint capsule must allow some play in order for full movement to occur. The joint demonstrates joint play in the neutral close-packed position, followed by a range of active movement that is under the control of musculature. A small degree of passive movement then occurs that is followed by an elastic barrier of resistance called end feel. Joint play in the neutral close-packed joint position and end feel at the end point of joint movement are both accessory joint movements that are necessary for normal joint function. A loss of either movement can result in a restriction of motion, pain, or both.
Motion palpation procedures have been an integral part of chiropractic since its inception; but only through the cultivation of Gillet, Faye, and Schafer [42–48] and colleagues have formalized techniques been widely disseminated. Both active and passive joint ranges of motion are assessed. During active range of motion assessment, the patient performs the movement, and during passive motion assessment the examiner produces the movement. When acute joint pain and muscle splinting are involved, the patient may be unable to relax sufficiently to allow for true motion assessment. In such cases, the procedure is deferred, relying on other findings to determine treatment or deferring treatment until the evaluation can be performed.
During both active and passive motion assessments, the clinician evaluates the total range, symmetry, and pattern of movement as well as muscle tone. Any painful limitations, abnormal movements, or painful arcs should be recorded. Unless contraindicated by joint injury, additional "overpressure" should be applied at the end of passive movement to assess for pain and end feel. Significant limitation and/or asymmetry of movement are evidence of neuromusculoskeletal (NMS) impairment. [49] Noted reductions in joint movement, however, must be placed within the context of the normal variations that exist between sexes and age groups.
Many different methods of measurement are employed in the evaluation of joint and spinal range of motion. They range from visual estimates and goniometric and inclinometric measurements to the more technical approaches of computerized digitation. [50, 51] The use of inclinometers for spinal range of motion and inclinometers or goniometers for extremity range of motion is becoming a minimal standard for determining impairment and for monitoring outcomes. [49] Range of motion abnormalities are potential signs of dysfunction in both extremity and spinal joints, but regional restrictions to spinal movement do not confirm the presence or absence of segmental spinal joint dysfunction. Spinal injuries may affect the nonsegmental somatic tissues and spare the vertebral joints. In these circumstances, altered regional movements are present, and individual segmental range of joint movement may be limited. However, the loss of mobility is uniform, and the individual spinal motion segments demonstrate normal joint play and end feel. Conversely, disorders that produce individual spinal joint restrictions may still demonstrate normal regional movements, as individual joint restriction is concealed by compensatory hypermobility at adjacent joints. Therefore, spinal abnormalities in global range of motion are more valuable in identifying general NMS dysfunction and the possibility of segmental dysfunction than they are in confirming a specific level of dysfunction.
During the performance of motion palpation, the examiner characteristically uses one hand to palpate joint movement (palpation hand) while the other hand (indifferent hand) produces or guides movement. The palpation hand establishes bony or soft tissue contacts over the joint as attention is directed to the assessment of joint range, pattern, and quality of movement. When assessing joint motion, the palpator is evaluating the quality and quantity of movement from the starting or zero point to the end range of passive movement.
Stress X-ray evaluation may reveal regional or segmental alterations in movement. However, stress X-rays involve ionizing radiation and therefore are not routinely used. The high cost of this type of evaluation also limits its clinical use.
Tissue tone, texture, temperature abnormality
Changes in the characteristics of contiguous and associated soft tissues, including skin, fascia, muscle, and ligament, are noted. These changes are identified through observation, palpation, instrumentation, and tests for length and strength.
Muscle tone is the result of continuous mild contraction of muscle dependent upon the integrity of nerves and their central connections with the complex properties of muscles such as contractibility, elasticity and extensibility. [6] Normal . muscle at rest possesses resilience; thus, when joint movement passively stretches a muscle, a certain amount of involuntary resistance is encountered. The maintenance and control of muscle tone are dependent on normal function of the pre-central motor cortex, the basal ganglia, the midbrain, the vestibulum, the spine, and the neuromuscular system. Normal muscle tone may be increased or decreased. Hypertonic muscles are noted in spasticity, rigidity, and flexor spasms with increased resistance to sudden passive movements. Hypotonic/atonic muscles feel soft and flabby and offer less than normal resistance to passive movement. The spinal cord is the seat of the stretch reflex that functions in the maintenance of muscle tone. The impulses pass through a simple reflex arc, which includes the neuromuscular spindles, afferent nerves, spinal cord connections to the anterior horn cells, and the efferent motor nerves. Tests for muscle strength and reflex integrity are used to identify spinal and peripheral nerve involvement. In addition, tests for muscle length can help to identify spastic, shortened, or hypertonic muscles (eg, Thomas test to determine hip flexor contracture, straight leg raise to determine hamstring length).
Muscles that have had an abnormally high tone for long periods may decompensate and develop nodular changes that become palpable. These contracted, firm, tender areas are often called trigger points. Depending on the muscle involved, local or regional decreases in joint movement may be associated with muscle hypertonicity.
Local temperature regulation results from the interaction of the multilevel spinal reflexes with the central autonomic control mechanism. Control of the thermal regulatory system is under the influence of the sympathetic nervous system via vasomotor reflex mechanisms. [52] In a healthy individual, paraspinal temperature radiation is regionally symmetric to within O.5°C to 1°C. [53, 54] Temperature-detecting instruments are used to localize segmental increases or decreases in surface temperature. It is postulated that spinal subluxation and dysfunction may produce a local inflammatory reaction or reflex alteration in sympathetic tone, which in turn alters this segmental temperature symmetry. [6, 55–58]
Another method to assess spinal dysfunction is paraspinal electromyography scanning. Although it has garnered enthusiasm in the chiropractic profession, the use of surface paraspinal electromyography must be questioned. Surface-scanning paraspinal electromyography gives a rough estimation of transient muscle activity. It cannot give information about specific muscles because the recording electrodes are placed over the skin and not into a muscle. In attempting to document intersegmental dysfunction, the profession has jumped too quickly onto an unproven technology. [59]
Special tests and considerations
Those testing procedures that are specific to a technique system are performed (eg, leg check, arm fossa test, therapy localization). Any other testing procedures deemed necessary based on findings in data previously obtained are performed. In addition, visceral relationships are considered. [60] Reflexive or autonomic effects relate to evidence of change in tissues or structures distal to or distant from the site of therapeutic application. Moreover, involvement of the autonomic nervous system may be activated through connections with the lateral horn cells in the cord to produce vasomotor, trophic, visceral, and/or metabolic changes. The impulse-based paradigm of neurodysfunction that has been developed from the work of Homewood [61] suggests that somatic dysfunction and/ or joint dysfunction may induce persistent nociceptive and altered proprioceptive input. [62] This persistent afferent input triggers a segmental cord response, which in turn induces the development of pathologic somatosomatic or somatovisceral reflexes. [63–65] If these reflexes persist, they are hypothesized to induce altered function in segmentally supplied somatic or visceral structures.
Numerous conditions have been linked to hyperactivity of the sympathetic nervous system, including various types of cardiovascular, gastrointestinal, and genitourinary disorders and certain musculoskeletal disorders such as reflex sympathetic dystrophy. Most disease states have early manifestations of symptoms and signs that are part of a common reaction pattern to injury or stress. Pain in the somatic tissues is a frequent presenting symptom in acute conditions related to visceral dysfunction. Common examples include gallbladder disease producing right shoulder pain, cardiac disease producing left arm pain, and kidney disease producing flank pain. Palpatory cues of transient muscle hypertonicity and irritation or subcutaneous edema may be accompaniments of ill-defined subclinical states. [66] Moreover, subtle changes in tissue texture, joint position, and joint mobility identified by discerning palpatory skills appear to be latent manifestations of the somatic component of visceral disease. A study [67] performed on cardiac patients in an intensive care unit identified autonomic spinal reference site changes for the involved viscera (Table 2).
Autonomic changes in soft tissues identified in patients with viscera problems
Sudomotor reaction – Increase in skin moisture
Muscle tonelcontraction – Increase (hypertonicity)
Skin texture changes – Thickening
Subcutaneous fluid – Increased
A number of individuals have identified the segmental sympathetic nerve supply for the viscera. [68–75] While there is some variation among authors, the accepted range is shown in Table 3.
Table 3. Segmental sympathetic nerve supply for the viscera

CONCLUSION
Any finding can have some significance when taken in context with other clinical, historical, and laboratory findings. In recent years, greater emphasis has been placed on the dynamic concepts of the subluxation complex. In some cases static biomechanical relationship concepts have been totally disregarded. Sandoz [76] feels that this shift of emphasis is counterproductive. He suggests considering the mechanical, static, and dynamic concepts in harmony with the neurologic and reflex elements of spinal dysfunction/subluxation. Manual therapies, including soft tissue techniques and other forms of adjustive therapy, have the hypothetical potential for arresting or slowing both the local and distant somatic and visceral effects by terminating the altered neurogenic reflexes that are associated with somatic/joint dysfunction. However, clinical studies of the effectiveness ofthe use of manual manipulative therapy in visceral conditions are limited.
The compilation of findings from a PARTS evaluation serves as a guide in decision making regarding areas of the spine in need of a chiropractic adjustment. In addition, this multidimensional spinal index can be used in conjunction with the remainder of the examination to decide whether an adjustment will be made and precisely how, when, and where it is to be applied. A recommended minimum evaluation would be an asymmetry or range of motion abnormality with at least one other finding. However, more findings associated with a single joint dysfunction will increase the confidence level that it indeed represents a subluxation. The mere presence or absence of a single characteristic of subluxation (ie, misalignment) in a patient is not in itself sufficient evidence of the need for adjustive therapy. Neurologic changes result from many etiologies and may not occur each time with any single characteristic of subluxation. A PARTS assessment can serve as a tool for understanding the underlying cause and mechanical components that produce subluxation.
Health care is in an era of accountability, and there is great interest in outcome measures that support effectiveness and efficiency of care. Objective findings determined by the doctor can be used in planning a management strategy. The objective manifestations of subluxation (PARTS) would logically be targeted for improvement as a goal of treatment in a chiropractic office. Using the PARTS evaluation will docu- ment the doctor's effectiveness in the care of the patient. Certainly, if a chiropractic therapeutic intervention (adjustment) has the effect of reducing a subluxation, it would be expected that the manifestations of subluxation should diminish as well. Sequential PARTS evaluations confirming the effectiveness of care and the need to cease care can track these improvements over time. The PARTS evaluation can also be used as a means to determine when care is not effective, prompting the doctor to use alternative care strategies.
Medicare's adoption of the PART portion of the PARTS physical evaluation as the new alternative to X-ray for substantiation of spinal subluxation indicates the interest insurance carriers may have in this type of evaluation. Hopefully, Medicare's identification of a need to examine the patient will also result in changes in federal law to provide coverage for these examinations.
References:
Bergmann TF.
Various forms of chiropractic technique.
Chiro Tech. 1993;5(2):53-55Hammer Warren I.
Functional Soft Tissue Examination and Treatment by Manual Methods.
2nd ed. Gaithersburg, MD: Aspen Publishers, Inc; 1999Keating JC, Bergmann TF, Jacobs GE, Finer BA, Larson K.
lnterexaminer reliaability of eight evaluative dimensions of lumbar segmental abnormality.
J Manipulative Physiol Ther. 1990;13(8):463-470Boline PD, Haas M, Meyer JJ, et al.
Interexaminer reliability of eight evaluative dimensions of lumbar segmental abnormality: part II.
J Manipulative Physiol Ther. 1993;16:363-374Hubka Mj, Phelan SP.
Interexaminer reliability of palpation for cervical spine tenderness.
J Manipulative Physiol Ther. 1994;17(9):591-595Chusid JG.
Correlative Neuroanatomy & Functional Neurology.
17th ed. Los Altos, CA: Lange Medical Publications; 1979Phillips R, Frymoyer j, MacPherson B, et al.
Low back pain: a radiographic enigma.
J Manipulative Physiol Ther. 1986;9(3):183-187Hildebrandt R.
Chiropractic spinography and postural roentgenology: part I. History of development.
J Manipulative Physiol Ther. 1980;3(2):87-92Howe J.
Some considerations in spinal X-ray interpretations.
J Clin Chiro Arch. Spring 1971 :75Hildebrandt RW.
The scope of chiropractic as a ciinical science and art: an introductory review of concepts.
J Manipulative Physiol Ther. 1978;1 (1 ):7Herbst R.
Gonstead Chiropractic Science and Art. The Chiropractic Methodology of Clarence S. Constead, DC.
Mt. Horeb, WI: SCI- CHI Publications; 1980Howe JW.
Facts and fallacies, myths and misconceptions in spionography.
J Clin Chiro Arch. Winter 1972;34:1-7Plaugher G, Hendricks A.
The inter- and intraexaminer reliability of the Gonstead pelvic marking system.
J Manipulative Physiol Ther. 1991 ;14(9);503-508Logan HB.
Textbook of Logan Basic Methods.
St. Louis: Logan Chiropractic College; 1950Gregory RR.
Manual for Upper Cervical X-ray Analysis.
Monroe, MI: National Upper Cervical Chiropractic Association; 1971Blair WG.
Blair clinic of Lubbock, Texas.
Dig Chiro Econ. 1971 ;14(1):10Peterson C, Gatterman MI, Wei T.
Chiropractic radiology.
In: Gatterman MI, ed. Chiropractic Management of Spine Related Disorders.
Baltimore: Williams & Wilkins; 1990Howe JW.
The chiropractic concept of subluxation and its roentgenological manifestations.
J Clin Chiro Arch. Fall 1973:64Harrison DE, Harrison DD, Troyanovich SJ.
Reliability of spinal displacement analysis on plain X-rays: a review of commonly accepted facts and fallacies with implications for chiropractic education and technique.
J ManipulativePhysiol Ther. 1998;21 :252-266Haas M, Taylor JAM, Gillette RG.
The routine use of radiographic spinal displacement analysis; a dissent.
J Manipulative Physiol Ther. 1999;22(4);254-259Troyanovich Sj, Robertson GA, Harrison DD, Holland B.
lntra- and interexaminer reliability of the chiropractic biophysics lateral lumbar radiographic menstruation procedure.
J Manipulative Physiol Ther.1995;18:519-524Jackson BL, Harrison DD, Robertson GA, Barker WF.
Chiropractic biophysics lateral cervical film analysis reliability.
J Manipulative Physiol Ther. 1993;16:384-391Taylor JAM.
The role of radiology in evaluating subluxation.
In: Gatterman MI, ed. Foundations of Chiropractic Subluxation.
St. Louis: Mosby; 1995Sigler DC, Howe JW.
Inter- and intraexaminer reliability of the upper cervical X-ray marking system.
J Manipulative Physiol Ther. 1985;8:75-80Schram SB, Hosek R, Silverman HL
Spinographic positioning errors in Gonstead pelvic X-ray analysis.
J Manipulative Physiol Ther.1981;4(4):179-181Schram SB, Hosek RS.
Error limitations in X-ray kinematics of the spine.
J Manipulative Physio! Ther. 1982;5(1 ):5-10Haas M.
The reliability of reliability.
J Manipulative Physiol Ther. 1991 ;14(3):199-208Phillips RB.
An evaluation of the graphic analysis ofthe pelvis on the A-P full spine radiograph.
J Am Chiro Assoc. 1975;9:5139-5148Grostic JD, DeBoer KF.
Roentgenographic measurement of atlas laterality and rotation: a retrospective pre- and post-manipulation study.
J Manipulative Physiol Ther. 1982;5:63-71Anderson RT.
A radiographic test of upper cervical chiropractic theory.
J Manipulative Physiol Ther. 1981 ;4:129Jackson BL, Barker W, Bentz J, et al.
Inter- and intraexaminer reliability of the upper cervical X-ray marking system: a second look.
J Manipulative Physiol Ther. 1987;10:157-163Jackson BL, Barker WF, Gamble- AG.
Reliability of the upper cervical X-ray marking system: a replication study.
Chiro Res J 1988;1 (1 ):10Reinert OC.
An analytical survey of structural aberrations observed in static radiographic examinations among acute low back cases.
J Manipulative Physiol Ther. 1988;11 :24-30Keating JC, Boline PD.
The precision and reliability of an upper cervical marking system: lessons from the literature.
Chiropractic. 1988;1 :43Plaugher G, Cremata E, Phillips RB.
A retrospective consecutive case analysis of pretreatment and comparative static radiological parameters following chiropractic adjustments.
J Manipulative Physiol Ther. 1990;13(9):498-506Owens EF.
Line drawing analysis of static cervical X-rays used in chiropractic.
J Manipulative Physiol Ther. 1992;15:442-449Troyanovich SJ, Robertson GA, Harrison DD, Holland B.
lntra- and interexaminer reliability of the chiropractic biophysics lateral lumbar radiographic menstruation procedure.
J Manipulative Physiol Ther. 1995;18:519-524Jackson BL, Harrison DD, Robertson GA, Barker WF.
Chiropractic biophysics lateralcervical film analysis reliability.
J Manipulative Physiol Ther. 1993;16:384-391Plaugher G, Hendricks AH, Doble RW, Bachman T, Araghi H, Hoffart VM.
The reliability of patient positioning for evaluating static radiographic parameters of human pelvis.
J Manipulative Physio! Ther. 1993;16:517-522Burk JM, Thomas RR, Ratliff CR.
Intra- and interexaminer agreement of the Gonstead line marking method.
Am J Chiro Med. 1990;3 :114-116Gillet H.
Vertebral fixations: an introduction to movement palpation.
Ann Swiss Chiro Assoc. 1960;1 :30Gillet H.
The anatomy and physiology of spinal fixations.
J Natl Chiro Assoc. Dec 1963:22Gillet H, Liekens M.
A further study of spinal fixations.
Ann Swiss Chiro Assoc. 1969;4:41Gillet H.
Spinal and related fixations.
Dig Chiro Econ. 1973;14(3):22Gillet H, Liekens M.
Belgian Chiropractic Research Notes.
Huntington Beach, CA: Motion Palpation Institute; 1984Gillet H.
The history of motion palpation.
Eur J Chiro. 1983;31 :196Faye LJ.
Motion Palpation of the Spine: From MPI Notes and Review of Literature.
Huntington Beach, CA: Motion Palpation Institute; 1981Schafer RC, Faye LJ.
Motion Palpation and Chiropractic Technique: Principles of Dynamic Chiropractic.
Huntington Beach, CA: Motion Palpation Institute; 1989Guides to the Evaluation of Permanent Impairment. 3rd ed.
Chicago: American Medical Association; 1990Johnston W, Allan BR, Hondra I, et al.
Interexaminer study of palpation in detecting location of spinal segmental dysfunction.
J Am Osteopath Assoc. 1983;82(11):839-845Mayer TG, Tencer AF, Kristoferson S, Mooney, V, et al.
Use of noninvasive techniques for quantification of spinal range-of-motion in normal subjects and chronic low-back dysfunction patients.
Spine. 1984;;J(6):588-595Christiansen J.
Thermographic anatomy and physiology.
In: Christiansen J, Gerow G, eds. Thermography.
Baltimore: Williams & Wilkins; 1990Uemtsu S.
Symmetry of skin temperature comparing one side of the body to the other.
Thermology. 1985;1 :4Silverstein EB, Bahr GJM, Katan B.
Thermographically measured normal skin temperature asymmetry in the human male.
Cancer. 1975;36:1506Swenson RS.
Clinical investigations of reflex function.
In: Haldeman S, ed. Principles and Practice of Chiropractic. 2nd ed.
Norwalk, CT: Appleton & Lange; 1992: 110Peterson AR, ed.
Segmental Neuropathy.
Toronto, Canada: Canadian Memorial Chiropractic College (undated).Jones CH.
Physical aspects of thermography in relation to clinical techniques.
Bibl Radiol. 1974;&:1-8ludavich B, Bates W.
Pain Syndromes-Diagnosis and Treatment. 4th ed.
Philadelphia: F.A. Davis; 1954Meeker W, Matheson D, Wong A.
Lack of evidence for a relationship between low back pain and asymmetrical muscle activity using scanning electromyography.Grainger HG.
The somatic component in visceral disease.
In: Academy of Applied Osteopathy 19S8 Yearbook.
Newark, OH: American Academy of Osteopathy; 1958Homewood AE.
Neurodynamics of the Vertebral Subluxation.
St. Petersburg, FL: Valkyrie Press, Inc; 1977Korr 1M, ed.
The Neurobiologic Mechanisms in Manipulative Therapy.
New York: pfenum; 1978Sato A.
The somatosympathetic reflexes: their physiologic and clinical significance.
In: Goldstein M, ed. The Research Status of Spinal Manipulative Therapy.
Washington, DC: Government Printing Office; 1975Leach RA.
The Chiropractic Theories. 2nd ed.
Baltimore: Williams & Wilkins; 1986Sato A.
Spinal reflex physiology.
In: Haldeman 5, ed. Principles and Practice of Chiropractic. 2nd ed.
Norwalk, CT: Appleton & Lange; 1992Beal MC
Viscerosomatic reflexes: a review.
J Am Osteopath Assoc. 1985;85(12):786-801Larson NJ.
Summary of site and occurrence of paraspinal soft tissue changes of patients in the intensive care unit.
J Am Osteopath Assoc. 1976;75:840-842Bonica JJ.
Autonomic innervation of the viscera in relation to nerve block.
Anesthesiology. 1968;29:793-813Head H.
On disturbances of sensation with special reference to the pain of visceral disease.
Brain. 1893;16:1-13Gray H; Warwick R, Williams PL, eds.
Gray's Anatomy. 35th (Brit) ed.
Philadelphia: W.B. Saunders Co; 1973House EL, Pansky B.A
Functional Approach to Neuroanatomy. 2nd ed.
New York: McGraw-Hill; 1967Crosby EC, Humphrey T, Lauer EW.
Correlative Anatomy of the Nervous System.
New York: Macmillan; 1962Bhagat BD, Young PA, Biggerstaff DE.
Fundamentals of Visceral Innervation.
Springfield, IL: Charles C Thomas; 1977White JC, Smithwick RH, Simeone FA.
The Autonomic Nervous System.
New York: Macmillan; 1952Hansen K, Schliak H.
Segmental Innervation.
Stuttgart, Germany: G. Thieme; 1962Sandoz R.
Some reflections on subluxations and adjustments.
Ann. Swiss Chiro Assoc. 1989:7-29
Return to LOCATING SUBLUXATIONS
Since 7-11-2014


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |