

Historical Overview and Update
on Subluxation TheoriesThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Chiropractic Humanities 2010 (Dec); 17 (1): 22–32 ~ FULL TEXT
Howard Vernon, DC, PhD
Division of Research,
Canadian Memorial Chiropractic College,
Toronto, Ontario
Objective This article presents a personal view of the historical evolution of theories of subluxation in the chiropractic profession.
Discussion Two major themes emerge from this review: those related to the mechanical behavior of the spine and those related to the neurologic implications of these mechanical issues. Chiropractic subluxation theory is one of the few health-related theories whereby these mechanical and neurologic theories have been unified into a comprehensive theory of disorder of spinal function. For this disorder, doctors of chiropractic have used the term subluxation. These theories, and their unification in the “subluxation concept,” have undergone evolution in the profession's history.
Conclusion The “subluxation concept” currently faces challenges, which are briefly reviewed in this article. The only way forward is to strengthen our efforts to investigate the “subluxation concept” with high-quality scientific studies including animal models and human clinical studies.
Key indexing terms: Chiropractic, Philosophy, Review
From the FULL TEXT Article:
Introduction
Manual therapy has, arguably, best been described by a Polish medical manipulation practitioner, Arkuszewski, [1] as “a mechanical therapy with reflex effects.” The phrase mechanical therapy can be further characterized by noting that it is performed in the musculoskeletal (MSK) system. The phrase reflex effects can be further qualified, at the very least, to indicate that these are “health-beneficial.” Therefore, a revised version would read as follows:“a manually-performed mechanical therapy to the MSK system with health-beneficial reflex effects.”
This formulation also provides a basis for describing the primary disorder posited by chiropractic theory: subluxation. Recognizing that, for chiropractic, the subluxation has always been viewed as the “thing for which adjustment (manual therapy) is done,” a first-pass definition of subluxation, a la Arkuszewski, would be “a mechanical problem in the musculoskeletal system with health-deleterious reflex effects.”
Since the founding of chiropractic and the other manual therapy professions, 2 fundamental issues have vexed us:
What kind and location of mechanical problem in the MSK system qualifies as a
subluxation (or any of the other terms used as synonyms within and outside of chiropractic)?What kind of health-deleterious effects are specifically associated with subluxation?
The author recognizes that numerous others have attempted to review the subluxation concept, including recent excellent reviews by Gatterman, [2] Peters, [3] and Ebrall. [5] These previously published discussions are not reviewed here. What follows is a nonsystematic overview of selected developments in the profession that have addressed these 2 questions.
Discussion
The archetypical and founding event in the history of the chiropractic profession is Daniel David Palmer's first treatment of Harvey Lillard. From Palmer's original work, [5] he describes his thinking leading up to this event as:“Displacement of any part of the skeletal frame may press against nerves,
which are the channels of communication, intensifying or decreasing
their carrying capacity, creating either too much or not enough
functionating [sic], as aberration known as disease.”
“Pressure on nerves causes irritation and tension with deranged functions
as a result. Why not release the pressure? Why not a just cause instead
of treating the effects? Why not?”
“I claimed to be the first person to adjust a vertebra by hand, using
the spinous and transverse processes as levers.
I developed the art known as adjusting.…”
“The basic principle, and the principles of chiropractic which have
been developed from it, are not new. They are as old as the vertebrae.…
I am not the first person to replace a subluxated vertebra, for
this art has been practiced for thousands of years.”Palmer relates that he came upon this theory and applied it first to a man with deafness. Keating [6] records this version of events:
“Harvey Lillard gave him the cue which opened a new field for research. Mr. Lillard was restored to hearing by two adjustments, a dorsal vertebrae was replaced in its normal position.”
Here is Harvey Lillard's rendition of these events according to Palmer's newsletter:
“I was deaf for 17 years and I expected to always remain so, for I had doctored a great deal without any benefit. I had long ago made up my mind to not take any more ear treatments, for it did me no good. Last January Dr. Palmer told me that my deafness came from an injury in my spine. This was new to me; but it is a fact that my back was injured at the time I went deaf. Dr. Palmer treated me on the spine; in two treatments I could hear quite well. That was 8 months ago. My hearing remains good.” Harvey Lillard, 320 W Eleventh St, Davenport, Iowa. [6]
Although Palmer articulated several versions of his theory, the archetypal elements of Palmer's theory follow a logical pattern, as follows:
Subluxation, which is a misalignment of one of the vertebrae, causes
pressure on nerves exiting around the vertebrae, causing
disease.
Therefore,
Removal of subluxation (by manually adjusting it to its correct position) causes
release of nerve pressure, causing
the restoration of health.
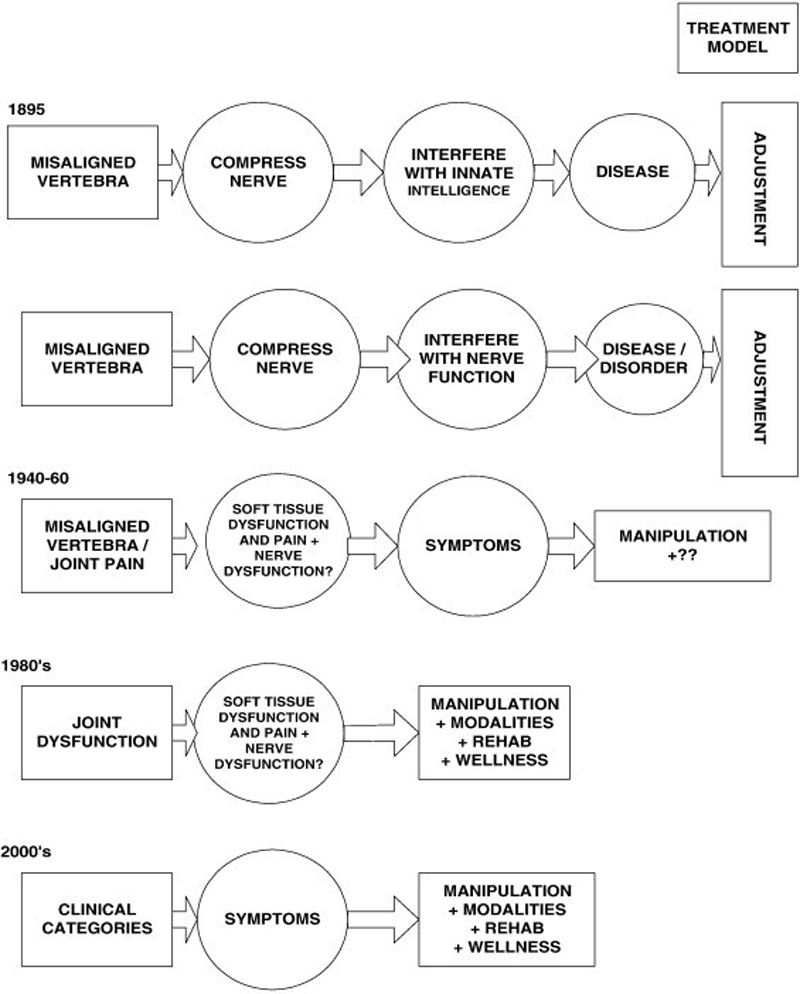
Figure 1 Figure 1 is a schematic depiction presenting this foundational chiropractic model. It also depicts the author's view of the evolution of this model through the 20th century. An important early advancement was the transformation of the understanding of the activity of the nervous system from a vitalistic interpretation, as the “flow of Innate Intelligence,” to a mechanistic or physiologically-based understanding of function in the nervous system. It appears that this understanding was not fully mature, as it focused only on the efferent neural activity that could be compromised by nerve compression, that is, neural conduction and efferent innervation of end organs. This produced a formulation whereby nerve compression was understood to result in an interference or derangement of nerve function, as understood in purely physiologic terms, which then resulted in end-organ dysfunction or disease. One manifestation of this approach was the development of the Meric system by BJ Palmer and James C Wishart7 that organized this “physiologic view” of neural regulation according to the spinal segmental level of the peripheral nerves and their end-organ territories of innervation. This development allowed many chiropractors to leave their vitalistic heritage behind to its rightful place in the history of ideas and move into a solidly, if not fully, mature physiologic/pathophysiologic model (Figure 1).
Another important advancement came with a change in the conception of the type of mechanical derangement that could constitute a subluxation. As noted above, for Palmer and the early chiropractors, this was ‘misalignment’ of the vertebra. By the 1920s, several chiropractic thinkers [8-11] had begun to shift their focus from static misalignment to some kind of “disturbance of function.” However, this required a fundamental change in thinking from a primary and very limited focus on “bone” (vertebra) to a more expanded focus on “joint” (spinal motion segment). This shift was critical in the evolution of a scientific model for chiropractors. It changed our practice, by emphasizing different technical procedures for the assessment of joint function, well beyond the limits of determining static misalignment of a bone. As well, it prepared the way for the other major changes described below by grounding the theory of subluxation at the level of the joint, not the level of a single bone, and the pressure it could exert on nerves.
This led the way to the next important shifts that characterize the major theoretical advancement of the late 1940s to the 1960s: maturation of the understanding of effects on and contribution of the nervous system (ie, “reflexes”) related to the subluxation. This work is associated with Dr Irwin Korr et al [12-19] and was echoed in chiropractic by many, including, but not limited to, Dr AE Homewood [20] in the late 1950s as well as his students, Drs R Gitelman [21, 22] and A Grice [23] from the Canadian Memorial Chiropractic College and Dr S Haldeman [24] from the Palmer College of Chiropractic.
This next step in the evolution of chiropractic thinking involved a shift from a focus solely on nerve compression to include the emerging understanding of the neural or reflex mechanisms that result directly from injury to the deep tissues of the vertebral motion segment. This shift incorporated the understanding of the effects of pain and inflammation from, for example, the facet joints of the spinal segments, on spinal cord mechanisms of sensory-motor integration and autonomic outflow. For Korr, this was termed the facilitated segment and led to his theory of “central excitatory state (CES)”. [14-20] The notion of “spinal irritability” had been developed as early as 100 years prior and had been part of the work of Head [25] and others in the early 20th century. [26-29] The work of Korr, Denslow, Wright, [12-19] and others revived this idea; and it was then applied in osteopathic and chiropractic thinking. Since that time, this model has come to be known as central sensitization (see below); and it has received enormous attention from pain researchers around the world.
A corollary to this development was the shift from a focus, especially in early chiropractic, which was solely on “efferent” or “downstream” neural mechanisms (those affected by compression), to a more comprehensive understanding of sensory-motor interactions within the central nervous system. In early chiropractic thinking, the “Big Idea” was to consider the action of “Innate Intelligence,” as it flowed through the nervous system, as working from “above-down, inside-out.” In this theory, blockage of a nerve by a misaligned vertebra resulted only in a blockage of the outward flow of health-giving “innate.”
Once the shift of thinking beyond static misalignment of a vertebra to dynamic behavior of a spinal motion segment (joint) occurred, chiropractors could begin thinking about the sensory implications of their “lesion.” Along with the shift away from spinal nerve compression mentioned above, this shift laid the groundwork for a much more sophisticated, fully scientifically grounded neural theory of “subluxation.”
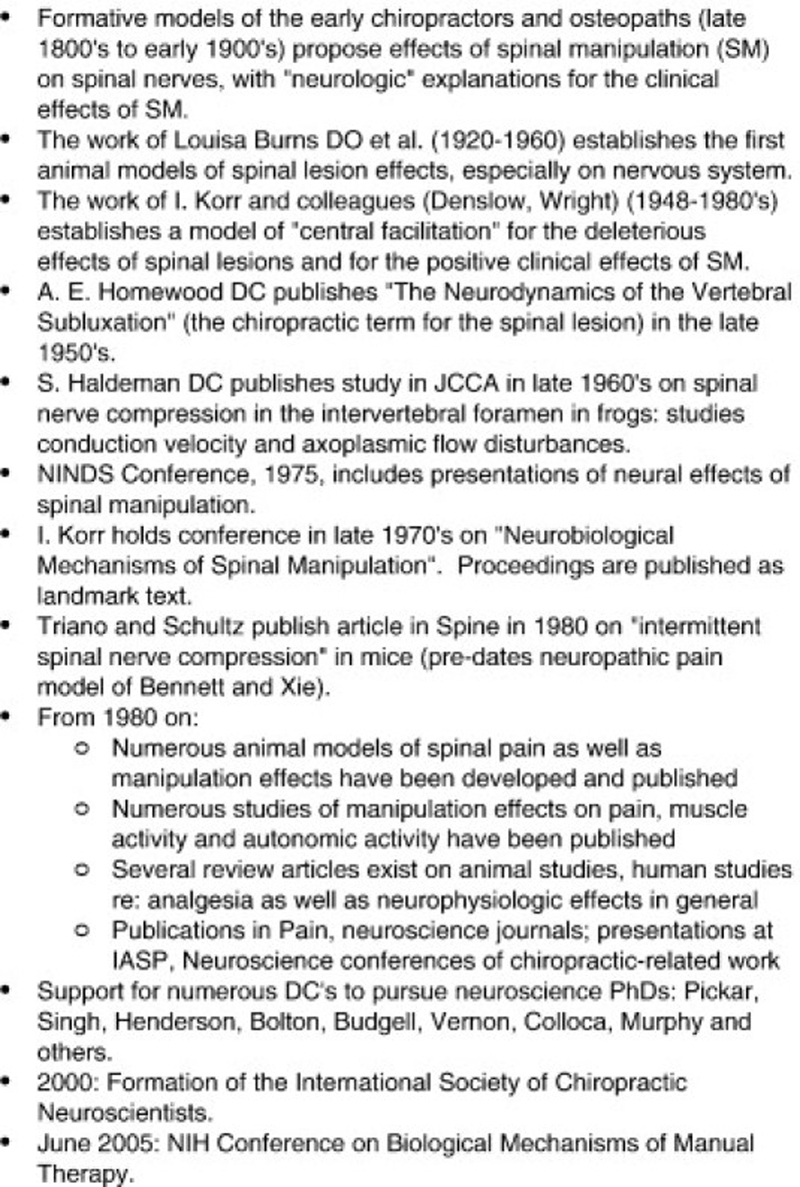
Figure 2 Korr summarized these developments in his famous categorization of “impulse-” and “non–impulse-based” mechanisms of the spinal lesion. It is actually better to consider these as “nerve compression–based” and “non–nerve compression–based” mechanisms. It will be instructive to fill in some of the voluminous work that has ensued on these themes since that time. This follows immediately after the next section. Figure 2 summarizes some of the notable historical developments in the neurosciences of manipulation.
Contemporaneous with this work on the “neural side” of the subluxation story was the work on the mechanical side undertaken by such notables as Drs Fred Illi, [30] Joe Janse, [31] Henri Gillet and his colleague Liekens, [32, 33] as well as their North American students, Drs L John Faye, [34] Ron Gitelman, [22] and Adrian Grice. [23]
Notable developments in these mechanical approaches to the “subluxation” were:
the development of motion palpation (although there is a history of interest in this going back to the 1930s with the work of Grecco and others)
the development of concepts such as “joint play,” “end-feel,” etc (the work of Mennel [35] is also important in this regard)
the elucidation of complex segmental motions by end-motion radiographs leading to an understanding of reference ranges of segmental motion, “coupled motion,” and axes of motion
the use of spinal-pelvic cineradiography
the use of weight scales and posturometers to assess full body posture
interest in gait mechanisms
an expanded biomechanical model that grounded single spinal subluxations within the larger context of the vertebral column and the locomotor system and considered the assessment and treatment of ‘patterns of findings’ (vs single separate findings) in these larger contexts. I call this model structural wholism.
Aside from this work representing a shift toward the dynamic, functional aspects of the spine, it also represented a shift away from single vertebral analysis (subluxation listings etc) to a more sophisticated analysis of, and interest in, the entire locomotor system. In fact, the definition of chiropractic developed at the Canadian Memorial Chiropractic College in the late 1960s was:
“A discipline of the scientific healing arts concerned with the pathogenesis, diagnostics, therapeutics, pain syndromes and neurological effects related to the statics and dynamics of the locomotor system, especially of the spine and pelvis.” [36]
The emphasis on the phrase locomotor system is mine, showing how that term predominated in the thinking of that time.
Notice that no mention of “subluxation” is found.
In a countermovement to this development, a new model called the vertebral subluxation complex was promulgated by Faye and Lantz. [34, 37] It is the author's opinion that this model may have created unwanted and unnecessary complexity in the numerous categories and aspects of tissue and physiologic functioning applied to the concept of subluxation, such as histopathology, myopathology, neuropathology, etc. All tissue sites or structures in the body — somatic, neural, and visceral — have these many dimensions or aspects (ie, all of these “ologies”). In the author's opinion, this model did not contribute to the scientific advancement, especially the scientific elucidation, of the subluxation concept.
In the author's opinion, another similar unfortunate development was the American Chiropractic Association paradigm statement on subluxation in 1996:“Chiropractic … focuses particular attention on the subluxation. A subluxation is a complex of functional and/or structural and/or pathological articular changes that compromise neural integrity and may influence organ system function and general health.” (from Gatterman [38])
This “definition” is too ambiguous and tentative, with its many “and/ors” and conditional assertions; and it has yet to be shown how this definition has contributed to the scientific development of the “subluxation concept.”
In more recent times, a consensus appears to have been reached in the manual therapy academic literature around the nature of the mechanical problem in the spine amenable to manual therapy, namely, hypomobility associated with a disturbance of joint function, hence, the terms joint dysfunction or, for the spine, spinal or segmental dysfunction.
The International Association for the Study of Pain Classification of Chronic Pain includes a definition of segmental dysfunction (in each of the spinal regions), as follows:“(spinal) pain, ostensibly due to excessive strains sustained by the restraining elements of a single spinal motion segment.
… features (spinal) pain, with or without referred pain, that can be aggravated by selectively stressing the particular spinal segment.Diagnostic criteria (all of the following should be satisfied):
The affected segment must be specified.
The patient's pain is aggravated by clinical tests that selectively stress the affected segment.
Stressing adjacent segments does not reproduce the patient's pain.
Pathology: Unknown. Presumably involves excessive strain incurred during activities of daily living by structures such as the ligaments, joints or intervertebral disc of the affected segment.” [39], p111
Recent and current concepts
The following recounts the development of ideas on the neurologic and mechanical issues relevant to subluxation from the 1960s onward and includes a short list of recent developments that are important to the development of the modern “subluxation model.”
A. Neurologic mechanismsA.i Nerve compression–based mechanisms
Chiropractors received considerable and protracted scorn for the idea of a “pinched nerve.” Crelin's [40] effort to debunk chiropractic focused directly on this phenomenon by putatively showing that there was ample room in the intervertebral foramen (IVF) for the nerve to never undergo such compression. The phenomenon of nerve compression became very strongly associated with disk herniation after Mixter and Barr's 1934 article. The role of minor intervertebral joint derangement in compression on nerves and in referred back pain became greatly diminished in the “medical model.”
However, the link between herniated disks and nerve compression did eventually loosen so that, by the 1970s, the phenomenon of lateral entrapment of the spinal nerve root had become well accepted. The work of Sharpless, [41] Sutherland, [42, 43] and Luttges and Gerren [44] on nerve root compression susceptibility and the work of Rydevik et al [45-53] “rehabilitated” the concept of the compressed nerve in spinal diagnosis.
Several chiropractic researchers investigated the effects of nerve root compression in the IVF by using animal models (see reviews by Vernon [54] and Henderson [55]). Disturbances of nerve conduction velocity and neural axoplasmic flow were demonstrated. However, these studies only provided an animal model of what might occur if “the subluxation really did result in compressed nerves.” Actual compression of nerves by something that most would agree was a subluxation was not studied. The mechanical derangement of the subluxation is not easy to create in an animal model.
Most importantly, for our purposes of discussion in modern pain research circles, this type of research goes under the name of neuropathic pain. It is clear that compression/irritation of the peripheral nerves, either as nerve roots or as nerve trunks, results in profound changes in sensorimotor processing throughout the central nervous system, but especially in the spinal cord. This means that, all along, compression of nerves was not just an “inside-out” matter. There is a whole dimension of “outside-in” (centripetal) processes that involve highly complex and clinically important changes in central sensorimotor processing that then results in profound changes in sensory, motor, and autonomic functions.
In other words, we now know that nerve compression/neuropathic pain is a much more complex matter than was originally conceived by the early chiropractors; and if, as part of the modernization of our thinking on subluxation, we believe that a role for nerve compression should be preserved, we should do so only with great respect and full regard for the body of data now available on the matter.Recent work has shown that facet inflammation can induce compressive radiculopathy by spread of inflammatory exudate anteriorly into the IVF. [56] Therefore, spinal joint dysfunction/inflammation can lead to direct nerve compression (ie, neuropathic pain) and not just “reflex” effects from pain (see below). Ironically, this work convincingly refutes Crelin's infamous report and finally provides confirmation of the oldest chiropractic theory: that relatively minor problems in the small joints of the spine can actually deleteriously compress or irritate the adjoining nerve!
A.ii Non–nerve compression–based mechanisms
Since the 1970s, a great deal has been learned about deep somatic pain mechanisms, that is, pain from deep somatic—muscle, joint, ligament—sources. This is an advance on the situation whereby the great preponderance of knowledge of pain mechanisms before that time came from studies of cutaneous sources only.
Deep pain mechanisms have been strongly associated with the development of central sensitization in the central pain transmission system: dorsal root ganglion cells, spinal cord dorsal horn, projection tracts to the brain, wide-ranging brain-based mechanisms in the medulla, midbrain, thalamus, and sensory cortex. As well, deep pain mechanisms are now known to evoke antinociceptive mechanisms local to the spinal cord as well as descending to the cord from midbrain nuclei.Central sensitization involves such changes in dorsal horn neurons as lowered thresholds of excitation, prolonged after-discharges, spread of reactivity of dorsal horn neurons, increases in the peripheral receptive fields, and a host of molecular and cellular/synaptic changes that underlie these functional changes. All of these changes are thought to be responsible for the clinical phenomena of spread of pain from an initial source, referral of pain from the original source, the development of allodynia and other hypersensitivity states, the development of chronicity of pain by virtue of the persistence of these changes (long-term potentiation), and the development of recurrence by virtue of the creation of persisting neural engrams or “pain memories.”
These changes are also now regarded as the mechanisms responsible for the efferent manifestations of the subluxation, as they were conceived in the theory of the “central excitatory state”: reflex muscular hypertonicity, reflex autonomic changes (somatovisceral mechanisms), and the functional changes that result from these manifestations, such as reduced mobility of the joints, contractures of muscles, altered patterns of joint use and function, altered tissue health, etc.
The fact that so much more is now known about the mechanisms of central sensitization and the particular mechanisms of deep somatic pain is owed to the advancement of animal models of joint and muscular pain. [57, 58] However, the vast majority of these studies, and therefore the vast majority of the data about these phenomena, comes from studies of the hind limbs of small animal models. Subcutaneous pain mechanisms typically involve the tissues of the hind paw; muscular mechanisms have involved mainly the gastrocnemius and soleus muscles; joint mechanisms have mainly involved either polyarthritic models of all the tissues of the hind quarters or, in monoarthritic models, the knee and ankle joints. This led one of the leaders in the field of muscle pain mechanisms, Siegfied Mense, to title an article in 2003 as “What's different about muscle pain?” [59]There has been a conspicuous absence of work on deep pain mechanisms from spinal (paraspinal) tissues. This leaves us with a critical question. Is what is now known about deep pain mechanism from the MSK tissues of the peripheral limbs automatically to be applied to deep pain arising from spinal tissues? Are there no important differences? If not, there is no compelling reason to hold on to theories that make the spine distinctive in any way; and there is no reason to develop animal models of spinal deep pain. So I now ask the question, “What's (or: Is there anything…) different about spinal muscular (and ligamentous) pain?”
Thankfully, there is a small but growing body of work on mechanisms of deep pain from paraspinal sources that is beginning to address this need. Chiropractic research in this area has been reviewed by Vernon [54] and Henderson. [55] A full list of chiropractic neurophysiological research is available from the Colloquium planners and is appended to this article. In addition, the works of Solomonow et al, [60-62] Indahl et al, [63] Tachihara et al, [56] and Taguchi et al [64, 65] must be recognized. All of these studies are elucidating the mechanisms of deep somatic pain of axial (spinal) tissues and helping to address the question of whether there are any unique features of such pain, especially those that might underlie the distinctive clinical phenomenology of spinal pain. The early results provide encouragement for the notion that there may be distinctive features of spinal pain mechanisms and that these might explain the distinctive features of spinal pain complaints in our patients.

B. Mechanical mechanisms
With respect to subluxation models, the recent work on spinal loading and spinal motor control patterns deserves mention. Notable models include the following:
spinal buckling [33, 67]
neutral zone [68-71]
ligamentomuscular reflexes [60-62, 72-75]
multisegmental motor control patterns
With respect to integrating the concept of ”subluxation” with more sophisticated motor control theories, an adage adapted from Korr (personal communication) is instructive:
Under normal, healthy conditions, spinal segments function in a multi-segmental pattern; no segment acts alone. Under conditions of pain and injury, segments can “act alone.” Therefore, we cannot expect to restore function by having injured segments move; they must be moved to accomplish this.
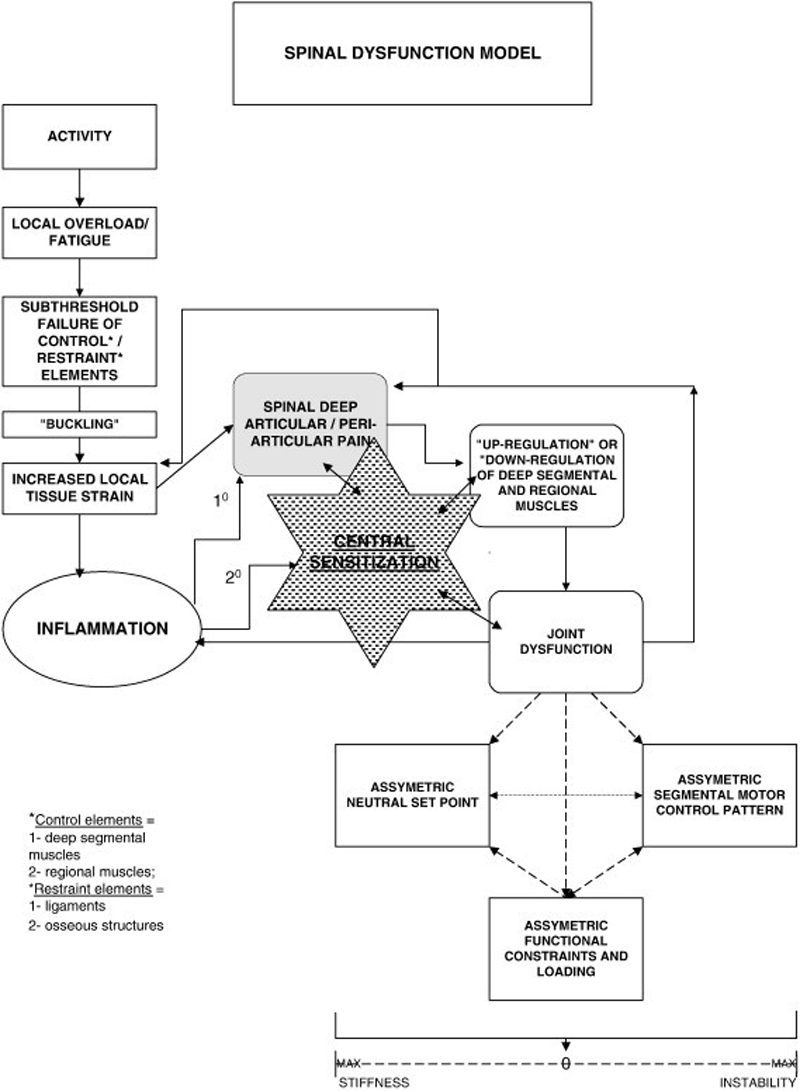
Figure 3 The notion of segments “acting alone” means that focal pain initiates
ligamentomuscular reflexes altering local segmental motor control, as well as
somatosympathetic reflexes altering local vaso- and sudomotor control (as well as distant end-organ function?).
Figure 3 depicts a comprehensive model of spinal dysfunction. Note that this is not a clinical model in the style of the vertebral subluxation complex; rather, it is a predictive model that, although based upon current knowledge, identifies areas of important future laboratory and clinical work.

C. Current challenges to subluxation
In this final section, some of the very current challenges to the subluxation model are reviewed.
For almost all of its history, chiropractic has posited that neurologic or reflex effects do result from subluxation and that it is these effects that underscore the importance of subluxation in the health of the patient. It is this proposal — or this side of the “Arkuszewski-like” formulation with which we began this article — that received the greatest amount of criticism from opponents of the profession. Throughout this time, the mechanical side of our original formula was not overly criticized, although the concept of “misalignment” has lost most of its favor.
Recent developments in manipulative sciences have created a unique challenge to the very concept of a “specific mechanical problem” toward which manipulation is directed.
Studies on the reliability of palpation of segmental motion have reported mixed results. [76] This has led some to discard this procedure in their analysis of spinal pain. This has led others to go further and become skeptical that a “segmental mechanical problem with a disturbance of motion” actually exists.
A small number of studies on the validity of palpation for segmental motion or for segmental findings have reported questionable results. These studies have taken the form of randomized clinical trials of a single session of manual therapy—manipulation, [77] mobilization, [78] and manual traction [79] — in which one group receives a single palpation-specific procedure and the other group receives the same procedure at sites distant from the target segment. The immediate clinical outcomes of these studies show no significant difference between groups, calling into question the need to identify a specific segment at all. The combination of 1 and 2 led some to suggest that the whole idea of a mechanical lesion is invalid and should be discarded.
Recently, classification-based approaches to treatment of spinal disorders based on apparently validated prediction rules (predicting positive outcome of treatment from symptom profiles) have been developed. [80-82] Some of these either exclude or downplay the results of palpatory examination for spinal hypomobility. [80-82] On the other hand, some of them do the opposite and strongly emphasize the findings of “motion palpation” for “spinal fixation.” [83] Clinicians are now able to choose among these predictive models, with one option being to discard, or at least greatly downplay, the role of a mechanical lesion.
few recent studies on healthy subjects appear to indicate that cavitations occurring during spinal manipulations are not localized to the segment putatively identified as the “lesion” and as the “target” of the maneuver. [84] This has been interpreted by some to mean that, even if a “specific mechanical lesion” does exist and even if it can be reliably identified in clinical assessment, such an exercise may be fruitless if the treatment cannot match this level of specificity.
The older challenge faced by the chiropractic profession was largely to the second half of our initial formulation of subluxation: “the health-deleterious effects.” Our critics have persistently questioned the premise that chiropractic subluxations caused anything more important than local, benign pain. The entire historical chiropractic project of attaching health-significant effects to subluxation (such as the Association of Chiropractic College's statement including the phrase that compromise neural integrity and may influence organ system function and general health) was challenged by these critics.
The newer challenge is now to the first part of our statement: “A subluxation is a mechanical problem in the musculoskeletal system.…” Recent research appears to challenge this premise as well; and some, within and outside of the profession, have adopted a completely skeptical view of the entire “subluxation project.” “If it doesn't exist in the first place,” they say, “how can it have any effects? If we can't find it, why look for it and why include it in our clinical decision-making? If we can't localize our treatment to one segment, why be concerned to do so?”
Conclusion
These challenges to the “subluxation concept” are in their early days and, in many instances, are based on only one or a few studies. In several instances, these studies have involved healthy subjects or those with relatively mild symptom severity. In several studies, the manual therapy intervention might be regarded as nonspecific and, therefore, would not qualify as an “adjustment.” On the other hand, critiques could be made of the quality of many of the studies that formed the basis for what might be called the “standard model” in chiropractic and the other manual therapy professions, including those which extend back several decades. Indeed, some of the modern challenges, especially in the area of manual diagnostic procedures, appear to derive precisely from the poorer quality of prior studies. The only way forward is to strengthen our efforts to investigate the “subluxation concept” with high-quality scientific
Funding sources and conflicts of interest
No funding sources or conflicts of interest were reported for this study.
References:
Arkuskewski Z.
The efficacy of manual treatment in low back pain:
a clinical trial.
Man Med. 1986;2:68–71Gatterman M.I.
Subluxation – Historical Perspectives
Chiropractic Journal of Australia 2009 (Dec); 39 (4): 151–164Peters R.
The Subluxation – Historical Perspectives Part II
Chiropractic Journal of Australia 2009 (Dec); 39 (4): 143–150Ebrall P.
Towards better teaching about the vertebral subluxation complex.
Chiropr J Aust. 2009;39:165–170Palmer D.D.
Portland Printing House Company of Portland;
Oregon: 1910.
The chiropractor's adjusterKeating J.
Dr. Palmer's Lifeline
Chiro.Org's History SectionHynes R.J.R., Callender A.K.
Technique in the classroom at Palmer College of Chiropractic:
a history of art in chiropractic.
J Chirop Human. 2008;15:55–66Carver W.
OK: self-published; Oklahoma City: 1921.
Carver's chiropractic analysisSchafer R.C.
Basic Principles of Chiropractic Neuroscience
American Chiropractic Association; Arlington, VA: 1990.Vladef T., Hardy M.
The theory of fixation points.
Nat Chirop J. 1945Grecco M.A.
Jarl Publishing Co.; New York, NY: 1953.
Chiropractic technic illustratedKorr I.M., Wright H.M., Thomas P.E.
Effects of experimental myofascial insults on
cutaneous patterns of sympathetic activity in man.
Acta Neuroveg (Wien) 1962;23:329–355Korr I.M.
Proprioceptors and somatic dysfunction.
J Am Osteopath Assoc. 1975;74(7):638–650Korr I.M.
The spinal cord as organizer of disease processes:
some preliminary perspectives.
J Am Osteopath Assoc. 1976;76(1):35–45Denslow J.S.
The somatic component.
J Am Osteopath Assoc. 1953;52(5):258–261Denslow J.S.
Neural basis of the somatic component in health and disease
and its clinical management.
J Am Osteopath Assoc. 1972;72(2):149–156Wright H.M.
Sympathetic activity in facilitated segments: vasomotor studies.
J Am Osteopath Assoc. 1955;54(5):273–276Denslow J.S.
Pathophysiologic evidence for the osteopathic lesion:
the known, unknown, and controversial.
J Am Osteopath Assoc. 1975;75(4):415–421Korr I.M., editor.
The neurobiological mechanisms in manipulative therapy.
Plenum Press; New York, NY: 1978Homewood A.E. 3rd ed.
Valkyrie; St. Petersburg, FL: 1977.
The neurodynamics of the vertebral subluxationGitelman R.
The Treatment of Pain by Spinal Manipulation.
In: Goldstein M., editor.
The Research Status of Spinal Manipulative Therapy
National Institutes of Health; Bethesda, MD: 1978.
pp. 261 of the PDFHaldeman S., editor.
Modern developments in the principles and practice of chiropractic.
Appleton-Century-Crofts; New York, NY: 1978.
pp. 297–330Haldeman S., editor.
Modern developments in the principles and practice of chiropractic.
Appleton-Century-Crofts; New York, NY: 1978.
pp. 331–358Haldeman S., Meyer B.J.
The effect of constriction on the conduction of the
action potential in the sciatic nerve.
South African Med J. 1970;44:903Head H.
Vol II. Henry Frowde and Hooder & Staughton, Ltd; London: 1920.
(Studies in neurology)Kellgren J.H.
Observations on referred pain arising from muscle.
Clin Sci. 1938;3:175Kellgren J.H.
On the distribution of pain arising from deep somatic
structures with charts of segmental pain areas.
Clin Sci. 1939;4:35–46Inman V.T., Saunders J.B.
Referred pain from skeletal structures.
J Nerv and Men Dis. 1944;99:660–667Sinclair D.C., Weddell G., Feindel W.H.
Referred pain and associated phenomena.
Brain. 1948;7:184–211Illi F.
National College of Chiropractic; Chicago, IL: 1950.
The spinal column: lifeline of the bodyJanse J. 1975.
A concept: the neurologic element as it relates to clinical chiropractic.
The ChirogramGillet H.
The anatomy and physiology of spinal fixation.
J Nat Chirop Assoc. 1963Gillet H., Liekens M.
A further study of joint fixations.
Ann Swiss Chirop Assoc. 1969;4:41–46Seaman D., Faye L.J.
The vertebral subluxation complex.
In: Gatterman M.I., editor.
Foundations of chiropractic: subluxation.
Elsevier Mosby; St. Louis, MO: 2005.
pp. 195–226Mennel J.M.
Aspen Publishers; Gaithersberg, MD: 1992.
The musculoskeletal system: differential diagnosis from symptoms and signsVear H.J.
Standards of chiropractic practice.
J Manipulative Physiol Ther. 1985;8(1):33–43Lantz C.A.
The vertebral subluxation complex.
ICA Int Rev Chirop. 1989:37–61Gatterman M.I.
What's in a word?
In: Gatterman M.I., editor.
Foundations of chiropractic: subluxation.
Elsevier Mosby; St. Louis, MO: 2005.
pp. 5–18Merskey H., Bogduk N., editors.
Classification of chronic pain: definitions of chronic
pain syndromes and definitions of pain terms.
IASP Press; Seattle, WA: 1994. p. 111Crelin E.S.
A scientific test of the chiropractic theory.
Amer Sci. 1973;61(5):574–580Sharpless S.K.
The Susceptibility of Spinal Nerve Roots to Compression Block.
In: Goldstein M., editor.
The Research Status of Spinal Manipulative Therapy
Government Printing Office; Washington, DC: 1975.
pp. 150 of the PDFSunderland S.
Meningeal-neural relations in the intervertebral foramen.
J Neurosurg. 1974 Jun;40(6):756–763Sunderland S.
The anatomy of the intervertebral foramen and mechanisms
of compression and stretch of nerve roots.
In: Haldeman S., editor.
Modern developments in the principles and practice of chiropractic.
Appleton-Century-Crofts; New York, NY: 1978.
pp. 45–64.Luttges M.W., Gerren R.A.
Compression physiology: nerves and roots.
In: Haldeman S., editor.
Modern developments in the principles and practice of chiropractic.
Appleton-Century-Crofts; New York: 1975.
pp. 65–92.Olmarker K., Rydevik B., Holm S., Bagge U.
Effects of experimental graded compression on blood flow in spinal
nerve roots. A vital microscopic study on the porcine cauda equina.
J Orthop Res. 1989;7(6):817–823Olmarker K., Rydevik B., Holm S.
Edema formation in spinal nerve roots induced by experimental, graded
compression. An experimental study on the pig cauda equina with special
reference to differences in effects between rapid and slow onset of compression.
Spine. 1989 Jun;14(6):569–573Rydevik B.L., Myers R.R., Powell H.C.
Pressure increase in the dorsal root ganglion following mechanical
compression. Closed compartment syndrome in nerve roots.
Spine. 1989;14(6):574–576Olmarker K., Holm S., Rosenqvist A.L., Rydevik B.
Experimental nerve root compression. A model of acute, graded compression
of the porcine cauda equina and an analysis of neural and vascular anatomy.
Spine. 1991;16(1):61–69Olmarker K., Rydevik B.
Pathophysiology of sciatica.
Orthop Clin North Am. 1991;22(2):223–234Rydevik B.L., Pedowitz R.A., Hargens A.R., Swenson M.R., Myers R.R., Garfin S.R.
Effects of acute, graded compression on spinal nerve root function
and structure. An experimental study of the pig cauda equina.
Spine. 1991;16(5):487–493Rydevik B.L.
The effects of compression on the physiology of nerve roots.
J Manipulative Physiol Ther. 1992;15(1):62–66Rydevik B.
Sciatica and herniated disk. Current aspects of
pathophysiology and pain mechanisms.
Nord Med 1994;109(3):74-6, 80Garfin S.R., Rydevik B., Lind B., Massie J.
Spinal nerve root compression.
Spine. 1995;20(16):1810–1820Vernon H.
Basic scientific evidence for subluxation.
In: Gatterman M.I., editor.
Foundations of chiropractic: subluxation.
Mosby; St. Louis, MO: 1995.
pp. 35–55Henderson C.N.R.
Animal models in the study of subluxation and manipulation.
In: Gatterman M.I., editor.
Foundations of chiropractic: subluxation.
Elsevier Mosby; St. Louis, MO: 2005.
pp. 47–103Tachihara H., Kikuchi S.I., Konno S.I., Sekiguchi M.
Does Facet Joint Inflammation Induce Radiculopathy? An Investigation
Using a Rat Model of Lumbar Facet Joint Inflammation
Spine (Phila Pa 1976) 2007 (Feb 15); 32 (4): 406–412Mense S.
Nociception from skeletal muscle in relation to clinical muscle pain.
Pain. 1993;54:241–249Mense S.
Muscle pain: mechanisms and clinical significance.
Dtsch Arztebl Int. 2008;105(12):214–219Mense S.
What is different about muscle pain?
Schmerz. 2003;17:459–463Solomonow M.
Ligaments: a source of musculoskeletal disorders.
J Body Mov Ther. 2009;13:136–154Solomonow M., Zhou B.H., Harris M., Lu Y., Baratta R.V.
The ligamento-muscular stabilizing system of the spine.
Spine. 1998;23:2552–2562Stubbs M., Harris M., Solomonow M., Zhou B., Lu Y., Baratta R.V.
Ligamento-muscular protective reflex in the lumbar spine of the feline.
J Electromyogr Kinesiol. 1998;8:197–204Holm S., Indahl A., Solomonow M.
Sensorimotor control of the spine.
J Electromyogr Kinesiol. 2002;12:219–234Taguchi T., John V., Hoheisel U., Mense S.
Neuroanatomical pathway of nociception in a low back
muscle (multifidus) in the rat.
Neurosci Lett. 2007;427:22–227Taguchi T., Hoheisel U., Mense S.
Dorsal horn neurons having input from low back structures in rats.
Pain. 2008;138:119–129Triano J.J.
Measurement of lumbar spine loads and motions during rotational mobilization.
J Manipulative Physiol Ther. 2005;28(9):731–732Triano J.J.
Buckling: a biomechanical model of subluxation.
In: Gatterman M.I., editor.
Foundations of chiropractic: subluxation.
Mosby, Inc.; St. Louis, MO: 2005.
pp. 283–295Panjabi M.M.
A hypothesis of chronic back pain: ligament subfailure injuries
lead to muscle control dysfunction.
Eur Spine J. 2006;15(5):668–676Panjabi M.M.
What happens in the motion segment?
Bull Hosp Jt Dis. 1996;55(3):149–153Kumar S., Panjabi M.M.
In vivo axial rotations and neutral zones of the thoracolumbar spine.
J Spinal Disord. 1995;8(4):253–263Klein G.N., Mannion A.F., Panjabi M.M., Dvorak J.
Trapped in the neutral zone: another symptom of
whiplash-associated disorder?
Eur Spine J. 2002;11:184–187Kang Y.M., Choi W.S., Pickar J.G.
Electrophysiologic evidence for an intersegmental
reflex pathway between lumbar paraspinal tissues.
Spine. 2002;27(3):E56–E63Pickar, JG and Wheeler, JD.
Response of Muscle Proprioceptors to Spinal
Manipulative-like Loads in the Anesthetized Cat
J Manipulative Physiol Ther. 2001 (Jan); 24 (1): 2–11McLain R.F., Pickar J.G.
Mechanoreceptor endings in human thoracic and lumbar facet joints.
Spine. 1998;23(2):168–173Pickar J.G., McLain R.F.
Responses of mechanosensitive afferents to manipulation
of the lumbar facet in the cat.
Spine. 1995;20(22):2379–2385Stochkendahl M.J., Christensen H.W., Hartvigsen J., Vach W., Haas M., Hestbaek L.
Manual Examination of the Spine: A Systematic
Critical Literature Review of Reproducibility
J Manipulative Physiol Ther 2006 (Jul); 29 (6): 475–485Haas M., Groupp E., Panzer D., Partna L., Lumsden S., Aickin M.
Efficacy of cervical endplay assessment as an indicator for spinal manipulation.
Spine (Phila Pa 1976) 2003;28(11):1091–1096Aquino R.L., Caires P.M., Furtado F.C., Loureiro A.V., Ferreira P.H., Ferreira M.L.
Applying joint mobilization at different cervical vertebral levels
does not influence immediate pain reduction in patients with
chronic neck pain: a randomized clinical trial.
J Man Manip Ther. 2009;17:95–100Schomacher J.
The effect of an analgesic mobilization technique when applied to
symptomatic or asymptomatic levels of the cervical spin in
subjects with neck pain: a randomized controlled trial.
J Man Manip Ther. 2009;17:101–108Brennan G.P., Fritz J.M., Hunter S.J., Thackeray A., Delitto A., Erhard R.E.
Identifying subgroups of patients with acute/subacute “nonspecific”
low back pain: results of a randomized clinical trial.
Spine. 2006;31(6):623–631Cleland J.A., Fritz J.M., Childs J.D., Kulig K.
Comparison of the effectiveness of three manual physical therapy techniques
in a subgroup of patients with low back pain who satisfy a clinical
prediction rule: study protocol of a randomized clinical trial
BMC Musculoskelet Disord. 2006;7:11Fritz J.M., Brennan G.P., Clifford S.N., Hunter S.J., Thackeray A.
An examination of the reliability of a classification
algorithm for subgrouping patients with low back pain.
Spine. 2006;31(1):77–82Christensen H.W., Vach W., Gichangi A., Manniche C., Haghfelt T., Høilund-Carlsen P.F.
Cervicothoracic angina identified by case history and palpation
findings in patients with stable angina pectoris.
J Manipulative Physiol Ther. 2005;28(5):303–311Ross J.K., Bereznick D.E., McGill S.M.
Determining cavitation location during lumbar and thoracic
spinal manipulation: is spinal manipulation accurate and specific?
Spine (Phila Pa 1976) 2004;29(13):1452–1457
Return to THE NAYSAYERS CORNER
Since 1-07-2011


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |