Subluxation Reviewed, Revisited, Revitalized This section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




SOURCE: Dynamic Chiropractic ~ March 12, 2010 ~ FULL TEXT
By Malik Slosberg, DC, MSOur understanding of the biomechanics and neurology of the subluxation continues to evolve as more research is published which helps explain the nature of this lesion. Historically, the subluxation has been at the heart of the identity and purpose of the chiropractic profession.
Contemporary models provide new insights into this elusive and sometimes mysterious problem which we attempt to find by various clinical means and correct by the application of high-velocity, low-amplitude thrusts. Let's review past models, but focus primarily on the latest evidence concerning the subluxation published in the recent scientific literature in order to improve our understanding, insight, and application of clinical interventions to improve patient outcomes with chiropractic care.
Older Models of Subluxation: Static Malposition and Pathology
Over the 115-year history of chiropractic, there have been many varied attempts to explain and clarify the subluxation. In the past, descriptions of this lesion were phrased in pathological terms and often included malposition, distortion of the intervertebral foramen and impingement of nerves as primary components. Henderson, et al., [1] described early notions of subluxation as static mechanical lesions, a misalignment or a bone out of place, as seen on a neutral radiograph. The authors explain that this static model has been vigorously challenged in the scientific literature.
Lantz [2] raised concerns about the strictly static, structural interpretation of vertebral subluxation and introduced his own hierarchical model including kinesiopathology, neuropathology, myopathology, connective tissue pathology, vascular abnormalities, as well as inflammatory response, histopathology, and biochemical abnormalities. Similarly, Dishman [3] described the vertebral subluxation complex in terms of various pathologies including neuropathology, myopathology, kinesiopathology, histopathology, and biochemical abnormalities.
Newer Terminology: Functional Spinal Lesion, Joint Dysfunction With Hypomobility, Joint Complex Dysfunction
In 2001, the World Federation of Chiropractic Congress, in its consensus document, described the subluxation as a complex of functional and/or structural and/or pathological articular changes that compromise neural integrity and may influence organ system function and general health. Pickar [4] described two mechanistic models of the subluxation: 1) compression/traction of peripheral nerve in the vicinity of the intervertebral foramen; and 2) altered sensory input leading to central facilitation and altered somato-somato and/or somatovisceral reflexes.
Triano [5] noted that the word subluxation has no consistent definition. In addition, he explained that the lesion is often treated as a syndrome, a clinical disorder, and suggests the term functional spinal lesion because it expresses a spine-related disorder involving function and does not imply pathomechanics, pathophysiology or symptomatology. Triano also noted that there is no method yet which can unequivocally detect and describe its presence. Its detection represents the art of the clinical practice, not its science.
In agreement, with Triano, Seaman [6] described the subluxation as a dysfunctional joint, not necessarily a pathological one, and suggested the term joint complex dysfunction to express this. Vernon and Mrozek [7] advocated for the term joint dysfunction with hypomobility to describe these dysfunctional joints as means to achieve some consensus about the nature of this lesion, which has been variously described in terms of "fixation," "somatic dysfunction," "blockage," "loss of joint play," and "hard end feel" by various clinical professions including DCs, MDs, DOs, and PTs.
Vernon and Mrozek described a more contemporary model of a dynamic biomechanical lesion wherein an error of movement is present that may or may not be associated with misalignment. Gatterman [8] described subluxation as a joint with impaired mobility with or without positional alteration. From her perspective, the subluxation is seen as a functional entity involving restricted vertebral movement. After all, she argues, it is the restriction of movement which responds to thrust procedures.
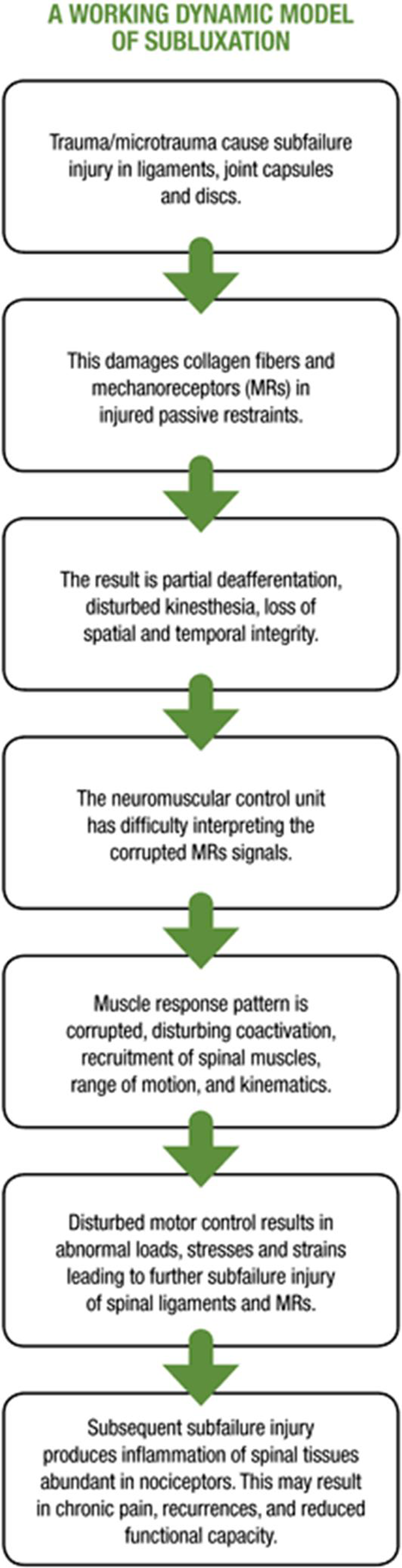
A Working Dynamic Model of Subluxation
A working dynamic model of subluxation Recently, Panjabi [9] offered a unique model of joint dysfunction with disturbed kinematics, loss of spatial and temporal integrity of received receptor signals, and corrupted motor programs. This model provides a dynamic explanation which offers distinctive insights into the mechanism and progression of the lesion DCs commonly describe as a subluxation. According to Panjabi's paradigm, difficulties arise because trauma or cumulative microtrauma cause subfailure injury in passive restraints including ligaments, joint capsules, and discs. He described subfailure injury as caused by the stretching of tissue beyond its physiological limit, but less than its failure point. Panjabi [10-11] documented these injuries in simulated whiplash studies which used whole cervical sections of human cadaver spines.
Subfailure injury has been described by other researchers as a result of microruptures of collagen fibers, [12] or microdamage of collagen tissues. [13] With these overstretch injuries, not only are bonds in the connective tissue matrix disrupted, but mechanoreceptors within these structures are also damaged, resulting in partial de-afferentation. This sensory/neurological dimension of overstretching/sprain of passive ligamentous restraints was described by neurosurgeons Freeman and Wyke. [14] The authors documented that a traction injury to a ligament or joint capsule resulted in ruptures of nerve fibers as well as collagen fibers. Nerve fibers have lower tensile strength than the molecular bonds of the connective-tissue matrix. If there is enough tensile force to damage collagen fibers, nerve fibers have been damaged as well.
Loss of Spatial and Temporal Integrity
With this partial de-afferentation, Panjabi [15] explained, there is loss of spatial and temporal integrity of received transducer signals from mechanoreceptors in the damaged ligament or joint capsule. The disturbance in precise, continuous sensory input has been described by other researchers [16-17] as false kinesthetic perception, which introduces errors in the precision of movement and may result in injury. This aberrant feedback is transmitted to the neuromuscular control unit (motor cortex, basal ganglia, cerebellum, motor neurons), which has difficulty interpreting the corrupted transducer signals because there is a mismatch between normally expected signals and the corrupted signals actually received.
Corrupted Muscle Response Pattern
As a result, the muscle response pattern generated is corrupted, affecting coordination and activation of each spinal muscle. The corrupted muscle response pattern affects the choice of which spinal muscles to activate, the force of onset, intensity, and shut-off. As a consequence, changes in the coordination, sequencing, and recruitment of spinal muscles responsible for spinal stability, posture and motion become disrupted. [18]
The corrupted muscle response patterns result in abnormal stresses and strains in spinal components, leading to further subfailure injury of spinal ligaments, joint capsules, mechanoreceptors within them, and disturbed kinematics. Errors in onset of muscle activation (delayed onset) and force production (reduced or excess force generation) may result in soft-tissue injury and explain acute low back pain where negligible loads are involved. [19] These changes can set up an inflammatory cascade, producing inflammation of spinal tissues abundant in nociceptors, resulting in chronic pain, recurrences, disturbed kinematics and reduced functional capacity.
Progressive Joint Complex Dysfunction
The process of progressive joint complex dysfunction involves many components including passive stabilizers (subfailure injury of ligaments, joint capsules, discs), somatosensory input (loss of spatial and temporal integrity, and false kinesthetic perception), and neuromotor control (corrupted motor programs, coactivation, sequencing, and recruitment). Disturbances in these systems combine to produce what may be catastrophic acute problems or, perhaps more commonly, a downward spiral of reduced functional capacity, increased risk of reinjury and chronicity.
This dynamic process of joint dysfunction offers an explanation which helps to clarify the clinical presentation of many of our patients and reinforce, with scientific evidence, the clinical observations chiropractors make in practice. The combination of clinical observations and scientific support can increase clinicians' confidence in and quality of our patient education, as well as the benefits we have to offer our patients.
References:
Henderson C, Cramer G, Zhang Q, et al.
Introducing the external link model for studying spine fixation and misalignment Part 1
Need, rationale, and applications
J Manipulative Physiol Ther 2009 (May); 32 (4): 294–302
C Lantz
The Vertebral Subluxation Complex PART 1:
An Introduction to the Model and Kinesiological Component
Chiropractic Research Journal 1989; 1 (3): 23-36Dishman RW:
Static and dynamic components of the chiropractic subluxation complex: a literature review
J Manipulative Physiol Ther. 1988 (Apr); 11 (2): 98-107Pickar J. Neurophysiological issues of the subluxation lesion. Top Clin Chiro, 2001;8:9-15.
Triano JJ.
The subluxation complex: outcome measure of chiropractic diagnosis and treatment.
Chiro Tech, 1990;2:114-20.
Seaman D.
Joint complex dysfunction: a novel term to replace subluxation/subluxation complex: etiological and treatment considerations.
JMPT, 1997;20:634-44.
Vernon H, Mrozek J.
A revised definition of manipulation
J Manipulative Physiol Ther 2005 (Jan); 28 (1): 68–72
Gatterman M.
Foundations of Chiropractic: Subluxation. 2nd Edition.
Elsevier Science Health Science, 2005.
Panjabi MM.
A Hypothesis of Chronic Back Pain: Ligament Subfailure Injuries Lead to
Muscle Control Dysfunction
European Spine Journal 2006 (May); 15 (5): 668–676Panjabi MM, et al.
Simulation of whiplash trauma using whole cervical spine specimens.
Spine, 1998;23:17-24.
Panjabi MM, Pearson AM, Shigeki I, et al.
Cervical spine ligament injury during simulated frontal impact.
Spine, 2004;29(21):2395-403.
Le B, Davidson B, Solomonow D, et al.
Neuromuscular control of lumbar instability following static work of various loads.
Muscle Nerve, 2009;39(1):71-82.
Solomonow M.
Sensory-motor control of ligaments and associated neuromuscular disorders.
J Electromyo Kinesiol, 2006;16:549-67.
Freeman MAR, et al.
The etiology and prevention of functional instability of the foot.
J Bone Joint Surg, 1965;47B(4):678-85.
Panjabi MM.
A hypothesis of chronic back pain.
Op Cit.
Solomonow M, Op Cit.
Akuthota V, Ferreiro A, Moore T, et al.
Core stability exercise principles.
Curr Sports Med Rep, 2008;7:39-44.
Teyhen DS, et al.
Fluoroscopic video to identify aberrant lumbar motion.
Spine, 2007;32:E220-9.
Panjabi MM.
The stabilizing system of the spine. Part I.
J Spinal Disorders, 1992;5(4):383-9Dr. Malik Slosberg, a 1981 valedictorian of Life Chiropractic College, has been in private practice for 25 years. He also holds a master’s of science degree (clinical counseling) from California State University, Hayward and a physician’s assistant degree from Dartmouth College. Dr. Slosberg has served on the postgraduate faculty of 10 chiropractic colleges and is currently a professor at Life Chiropractic College West.
Dr. Slosberg lectures throughout the United States and internationally. He has also written numerous articles that have been published in chiropractic journals, and produced educational materials including videos, wall charts and patient handouts used by many chiropractic colleges and thousands of chiropractors throughout the world.
Dr. Slosberg is a founding board member of the National Institute of Chiropractic Research, a funding agency for chiropractic research.

Return to SUBLUXATION THEORY


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |