

Is a Government-regulated Rehabilitation Guideline More Effective than
General Practitioner Education or Preferred-provider Rehabilitation
in Promoting Recovery from Acute Whiplash-associated Disorders?
A Pragmatic Eandomised Controlled TrialThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: BMJ Open. 2019 (Jan 24); 9 (1): e021283 ~ FULL TEXT
OPEN ACCESS Pierre Côté • Eleanor Boyle • Heather M Shearer • Maja Stupar • Craig Jacobs • John David Cassidy
Simon Carette • Gabrielle van der Velde • Jessica J Wong • Sheilah Hogg-Johnson
Carlo Ammendolia • Jill Alison Hayden • Maurits van Tulder • John W Frank
Faculty of Health Sciences,
University of Ontario Institute of Technology,
Oshawa, Ontario, Canada.
OBJECTIVE: To evaluate the effectiveness of a government-regulated rehabilitation guideline compared with education and activation by general practitioners, and to a preferred-provider insurance-based rehabilitation programme on self-reported global recovery from acute whiplash-associated disorders (WAD) grade I-II
DESIGN: Pragmatic randomised clinical trial with blinded outcome assessment.
SETTING: Multidisciplinary rehabilitation clinics and general practitioners in Ontario, Canada.
PARTICIPANTS: 340 participants with acute WAD grade I and II. Potential participants were sampled from a large automobile insurer when reporting a traffic injury.
INTERVENTIONS: Participants were randomised to receive one of three protocols: government-regulated rehabilitation guideline, education and activation by general practitioners or a preferred-provider insurance-based rehabilitation.
PRIMARY AND SECONDARY OUTCOME MEASURES: Our primary outcome was time to self-reported global recovery. Secondary outcomes included time on insurance benefits, neck pain intensity, whiplash-related disability, health-related quality of life and depressive symptomatology at 6 weeks and 3, 6, 9 and 12 months postinjury.
RESULTS: The median time to self-reported global recovery was 59 days (95% CI 55 to 68) for the government-regulated guideline group, 105 days (95% CI 61 to 126) for the preferred-provider group and 108 days (95% CI 93 to 206) for the general practitioner group; the difference was not statistically significant (χ2 = 3.96; 2 df: p = 0.138). We found no clinically important differences between groups in secondary outcomes. Post hoc analysis suggests that the general practitioner (hazard rate ratio (HRR) = 0.51, 95% CI 0.34 to 0.77) and preferred-provider groups (HRR = 0.67, 95% CI 0.46 to 0.96) had slower recovery than the government-regulated guideline group during the first 80 days postinjury. No major adverse events were reported.
CONCLUSIONS: Time-to-recovery did not significantly differ across intervention groups. We found no differences between groups with regard to neck-specific outcomes, depression and health-related quality of life.
TRIAL REGISTRATION NUMBER: NCT00546806
KEYWORDS: activation; physician education; physiotherapy; randomized controlled trial; treatment; whiplash-associated disorders
Strengths and limitations of this study
We included a large sample of participants with acute whiplash-associated disorders.
We used block randomisation to allocate participants to the treatment groups.
We concealed treatment allocation.
We used a patient-centred outcome (self-reported recovery) as the primary outcome, which was measured by a study interviewer who was blind to the treatment allocation.
The main threats to the validity of the trial are loss to follow-up and the inability to blind participants to the received treatment.
From the FULL TEXT Article:
Introduction
Whiplash-associated disorder (WAD) is the most common traffic injury. [1] WAD leads to a significant burden of disability and healthcare utilisation, and increases the risk of future health problems such as neck pain, headaches, low back pain, shoulder pain and sleep disturbances. [1–10] Poor prognostic factors for WAD include history of neck pain related to a traffic collision, older age, high initial pain levels and psychological factors (eg, poor expectation of recovery, depressive symptoms). [11, 12]
The clinical management of acute WAD is complex, and focuses on conservative interventions to manage symptoms and improve recovery. [13–16] Evidence suggests that the type, intensity and timing of healthcare delivery may impact recovery, but the evidence is mixed. [6, 7, 17–21] A randomised trial reported that multidisciplinary individualised treatments led to similar outcomes to usual care (from general practitioners, physiotherapists or chiropractors) in patients with acute WAD. [21] Patients receiving high-intensity healthcare from general practitioners, physiotherapists or chiropractors within the first month of injury experience slower recovery than patients who visited general practitioners once or twice. [6, 7] Similarly, patients attending an early intensive multidisciplinary rehabilitation programme report slower recovery than those who received usual insured individual care. [17] However, a randomised trial reported that a physiotherapy package (up to six sessions) provided slightly faster recovery than one additional physiotherapy advice session when added to emergency department consultations. [20] Overall, the body of evidence suggests that too much treatment too early after WAD may delay recovery, [22, 23] but further research is needed.
In 2008, the Bone and Joint Task Force on Neck Pain and its Associated Disorders (Neck Pain Task Force) recommended that the medical management of acute WAD without radiculopathy should include education, reassurance, pain management and rapid discharge. [24] Moreover, the Neck Pain Task Force recommended that rehabilitation providers use exercise, manual therapy and education to effectively manage acute WAD without radiculopathy. [25] Recently, exorbitant healthcare costs and increasing disability rates have led governments (through regulations and legislations) and insurers (through preferred-provider networks) to implement guidelines for the treatment of WAD. [1, 9, 17, 26–30] Most guidelines emphasise education, reassurance, mobility, return-to-activity and exercise, [29–31] but little evidence supports their effectiveness. [32] In Ontario, the provincial government introduced guidelines (in the form of regulations) to ensure timely access to rehabilitation services, improve the utilisation of healthcare resources and establish consistent fee schedules for insurers and healthcare providers. [29, 30]
Our primary objective was to evaluate the effectiveness of a government-regulated rehabilitation guideline compared with education and activation (promoting self-care and early return to normal activities of daily living) by general practitioners, and to a preferred-provider insurance-based rehabilitation programme on self-reported global recovery from acute WAD grades I–II. Our secondary objectives aimed to determine which of the three interventions was more effective in reducing time on insurance benefits, neck pain intensity, whiplash-related disability, depressive symptoms and in improving health-related quality of life.
Methods
Design and source population
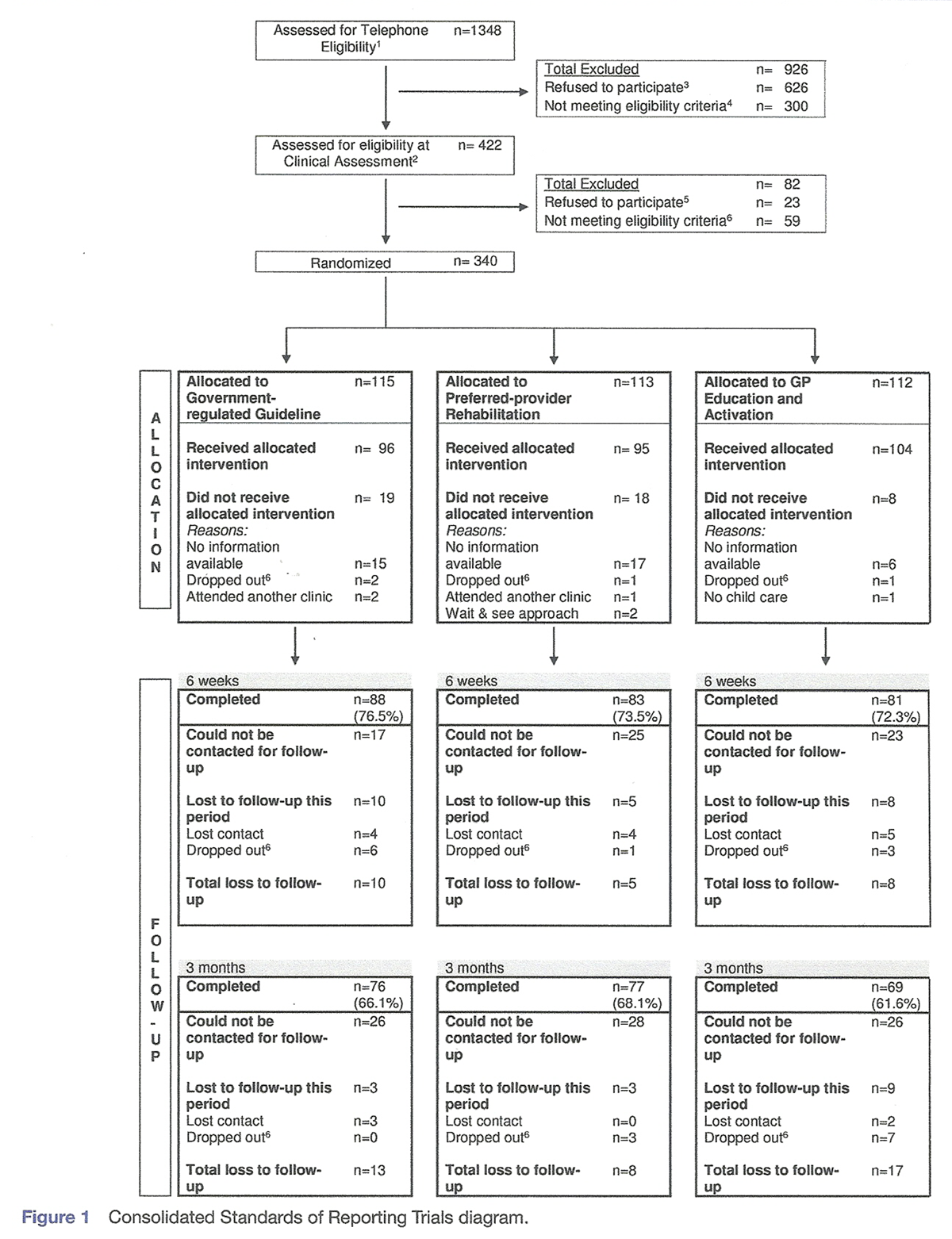
Figure 1
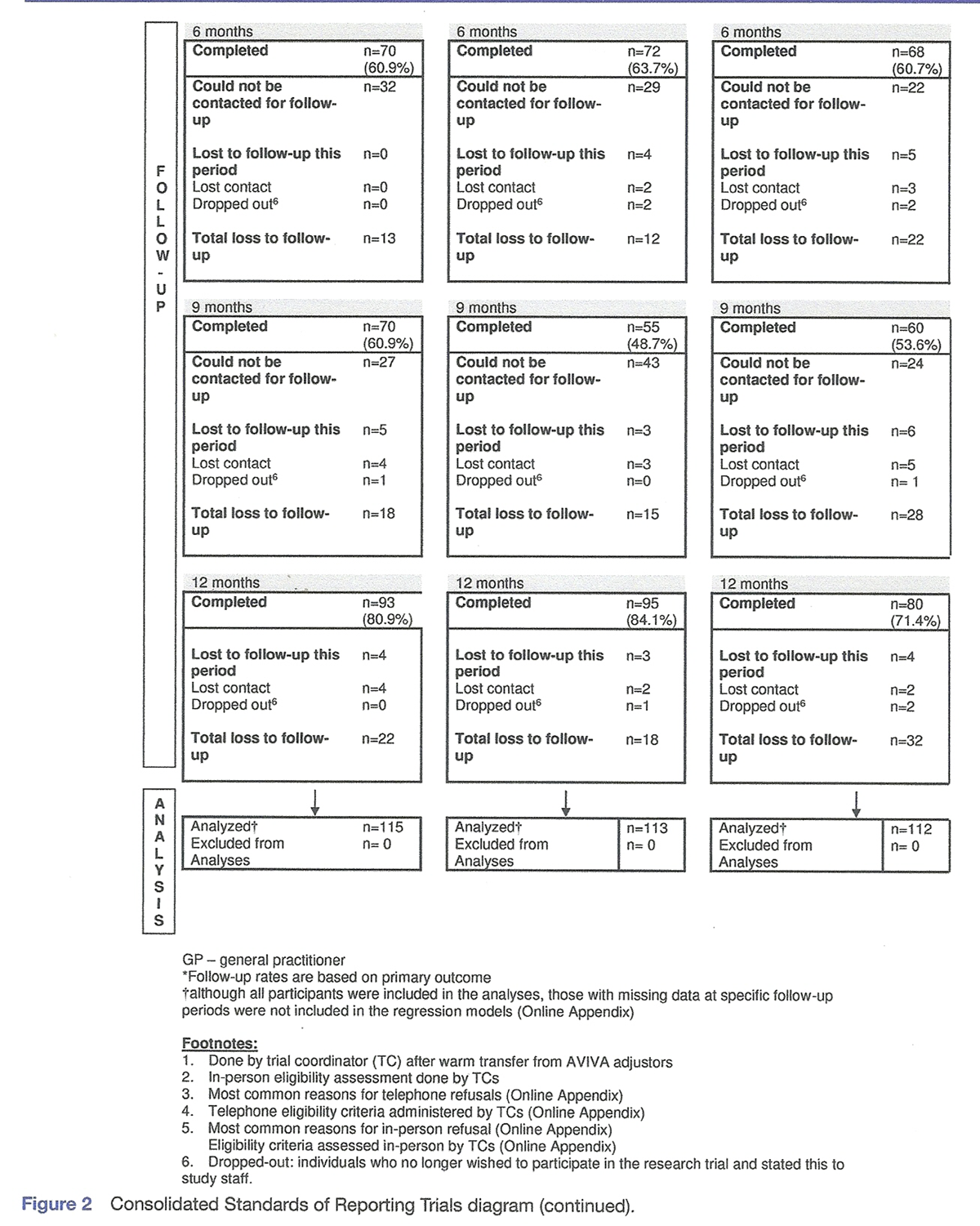
Figure 2 We conducted a pragmatic randomised controlled trial (Figures 1 and 2). [33] We registered the trial at www.clinicaltrials.gov (NCT00546806). Participants were eligible for the study if they:
1) were ≥18 years;
2) resided or worked within the Greater Toronto Area, Mississauga, Burlington, Cambridge, Kitchener, Ajax or Pickering and
3) were injured in a traffic collision and made an insurance claim to AVIVA Canada between February 2008 and March 2011.AVIVA Canada is a national casualty and property insurer that held 9.5% of the automobile insurance market in Ontario at the time of the study. [34]
Inclusion and exclusion criteria
Insurance adjusters (who manage insurance claims) informed claimants about the trial when making a claim. Claimants interested in the study were referred to a trial coordinator who confirmed eligibility and arranged for a clinical assessment. The trial coordinator assessed inclusion and exclusion criteria using a standardised history, physical examination and diagnostic imaging if clinically indicated.
Individuals who met the following criteria were included:1) insurance claim for physical injury and interviewed within 21 days of the traffic collision;
2) diagnosed with grade I–II WAD;
3) average neck pain since the collision ≥3/10 on the Numerical Rating Scale and
4) completed interviews in English.
Excluded were individuals with:1) fracture/dislocation of the spine or major bone;
2) head trauma with loss of consciousness;
3) past whiplash or work-related neck injury within the year;
4) active systemic diseases (cancer, inflammatory arthritis, disorders of central nervous system);
5) previous neck surgery and
6) treated by physiotherapist or chiropractor for neck pain in the 3 months before the injury.All participants provided written informed consent.
Randomisation to treatment groups
Participants were randomly allocated to:1) the government-regulated guideline;
2) education and activation by a general practitioner or
3) the preferred-provider insurance-based rehabilitation programme.Participants from the same motor vehicle were allocated to the same treatment arm to minimise contamination and cross-over. A co-principal investigator independently performed central randomisation using NQuery Advisor 7.09. [35] We used block randomisation with random block sizes of 3, 6, 9 and 12 participants for each study site; treatment allocation was concealed by providing trial coordinators with sequentially numbered sealed opaque envelopes for each study site.
Interventions
Participants received their interventions in person and individually within multidisciplinary rehabilitation (physiotherapists, kinesiologists, occupational therapists and massage therapists) or general practitioner clinics in Toronto, Mississauga, Cambridge, Ajax and Pickering, Ontario. All clinicians received training about the treatment protocols. Clinicians provided care to one treatment arm only. As recommended by the Ontario Government regulatory body, all participants received an educational brochure entitled ‘Getting the Facts about Whiplash'. [36]
Government-regulated guideline
The goal of the government-regulated guideline was to ensure timely access to rehabilitation services, improve healthcare utilisation and establish consistent fee schedules for insurers and healthcare providers. [29, 30] The treatment was multimodal, tailored to participants’ needs and could include:1) education, reassurance, home stretching exercises and encouragement to resume normal activities;
2) clinic-based exercises and functional activities;
3) manipulation or mobilisation;
4) pain management modalities (including massage therapy) and
5) coping skills education (supplementary appendix 1). [36]The physiotherapists determined the duration, frequency and number of visits, which was limited to 10 during the first 3 weeks of care, and to 9 after 3 weeks, for the period extending from weeks 4 to 6.
Participants with functional limitations were eligible for an assessment by an occupational therapist, which could lead to:1) recommendation to use aids or devices;
2) minor modifications in the work, home or school environment;
3) instructions on adaptive strategies or alternative approaches to fulfil functional tasks and
4) specific functional activities.Participants who reported significant improvement in the first 6 weeks of care, but had not reached satisfactory clinical recovery, were eligible to receive up to four additional treatment sessions over a 2-week period. The physiotherapist re-evaluated participants who had not recovered by 9 weeks and developed a new plan of management that was submitted to the insurer.
Preferred-provider insurance-based rehabilitation programme
The rehabilitation programme was designed by AVIVA Canada to initiate care within a preferred-provider network in a timely and efficient manner by removing administrative barriers (claim paper work) associated with the claim initiation process. The insurer hypothesised that providing quick access to care and reducing the administrative burden on claimants would prevent adversarial relationships and facilitate recovery.
The clinical interventions included in the preferred-provider insurance-based rehabilitation programme were similar to the government-regulated guideline (supplementary appendix 1). A maximum of nine treatments (including massage therapy) were allowed during first 3 weeks postcollision with an additional eight sessions (including massage therapy) during the subsequent 3 weeks if necessary. The physiotherapist determined the duration, interventions and frequency of visits, and recommended an in-home or job-site functional assessment if indicated. The primary differences between the government-regulated guideline and the preferred-provider insurance-based rehabilitation programme were:1) a reduction of the administrative burden for the claimant and
2) the possibility of participants who did not recover during the first 6 weeks of care to be referred (at the discretion of the physiotherapist) for a multidisciplinary evaluation at one of the study clinics.Education and activation by general practitioner
The education and activation intervention programme promoted self-care and early return to normal activities (supplementary appendix 1). Study general practitioners were asked to see participants once unless follow-up was clinically indicated. During the initial consultation, the general practitioner:1) reassured the participant about the favourable prognosis of WAD;
2) encouraged the participant to resume normal activities;
3) recommended home stretching exercises for the area of complaint (neck, shoulder, back and hip) and
4) if indicated, prescribed pain relief modalities or medication (heat/ice, acetaminophen or non-steroidal anti-inflammatory drug).Participants were informed to contact the general practitioner should their complaint persist or worsen. If follow-up visits were necessary, the general practitioner re-assessed the participant and the education and activation intervention was repeated. The maximum number of visits during the first 6 weeks was two for this treatment arm. Participants who did not recover during the first 6 weeks of care could be referred (at the discretion of the general practitioner) for a multidisciplinary evaluation at one of the study clinics.
Multidisciplinary evaluation
The multidisciplinary evaluation (by a physiotherapist and kinesiologist) involved a functional evaluation and recommendation for further physiotherapy care or an interdisciplinary rehabilitation programme to overcome psychosocial barriers to return to function, and facilitate physical and functional restoration if deemed appropriate. This programme included up to 5 weeks of daily intervention. The interdisciplinary team (involving a physiotherapist, general practitioner, occupational therapist, psychologist and kinesiologist) determined the frequency, duration and type of care, which could include:1) education and reassurance;
2) goal setting and advice on self-management;
3) psychological counselling and stress management;
4) relaxation therapy, psychotherapy and family counselling;
5) cognitive behavioural therapy;
6) instruction on pain management techniques and
7) strength, endurance, flexibility or cardiovascular exercises.Data collection and follow-up
Using a standardised questionnaire, a trial coordinator collected baseline data prior to randomisation (supplementary appendix 2). Participants were followed at 6 weeks, and 3, 6, 9 and 12 months postinjury. Research assistants blind to treatment allocation collected all follow-up data primarily via telephone, or in-person at the treating clinic, if requested. During the first year of the trial, participant feedback and the lower participation than expected suggested that answering the questionnaire was too burdensome. Therefore, we offered participants who did not wish to complete the full follow-up questionnaire to answer either:1) two outcome questions (self-reported global recovery and neck pain intensity) and a question used for the cost-effectiveness analysis (rating general health state on a Numerical Rating Scale) (data not reported in this paper) or
2) an abbreviated version of the full follow-up questionnaire (supplementary appendix 3).
OutcomesPrimary outcome Time to self-reported global recovery: self-reported global recovery was measured with the self-reported global recovery question, which is valid and reliable in patients with WAD. [17, 37–39] This ordinal transition scale has previously been used in randomised trials and cohort studies of neck pain. [17, 40, 41] In patients with WAD, we have previously reported that perceived recovery is consistently associated with less neck pain, better physical functioning and fewer depressive symptoms. [17] Participants were asked: "How well do you feel you are recovering from your injuries?” and had the following choices: completely better; much improved; slightly improved; no change; slightly worse; much worse and worse than ever. Time to self-reported global recovery was measured as the number of days between the date of injury and the first follow-up date at which a participant reported being ‘completely recovered’ or ‘much improved’.
Secondary outcomes Neck pain intensity in the past 24 hours: the 11-point Numerical Rating Scale is a global measure of pain intensity anchored by two extremes of pain intensity ranging from 0 (‘no pain’) to 10 (‘pain as bad as it could be’). It has good short-term test-retest reliability, good construct validity and can distinguish levels of pain in subjects with chronic pain. [42, 43]Whiplash disability: the Whiplash Disability Questionnaire consists of 13 items that measure the effect of whiplash on pain, personal care, work/home/study duties, driving/public transportation, sleep, tiredness/fatigue, social activity, sporting activity, non-sporting leisure activity, depression/sadness, anxiety, anger and concentration. Each item is scored from 0 to 10, with a total sum of 130, with higher global scores indicating more disability. [26] It has adequate reliability, validity and responsiveness. [26, 44–47]
Health-related quality of life: the 36-item Short Form Survey (SF-36) includes eight individual scales (physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional and mental health) used to compute the physical component and mental component scores in the past 4 weeks. It is valid, reliable and responsive in participants with musculoskeletal conditions. [48–51]
Depressive symptomatology: the Centre for Epidemiological Studies-Depression Scale (CES-D) is a widely used 20-item self-report scale designed to measure current level of depressive symptomatology. [52, 53] The CES-D is scored from 0 to 60 with higher scores indicating greater depressive symptomatology. [54, 55] It has good test-retest reliability, and good factorial and discriminant validity. [54–59]
Time on insurance benefit: we measured number of days between date of injury and date of insurance claim closure. Claim closure corresponds to the end of treatment, attainment of maximal medical improvement, termination of income replacement benefits or date of payment of the last outstanding bill incurred by the claimant (eg, device purchased). AVIVA Canada provided the claim closure dates. Time to claim closure is a valid marker of time to health recovery (ie, lower levels of neck pain, better physical functioning and no depression). [60, 61]The secondary outcomes of
1) satisfaction with care and satisfaction with treatment and
2) recurrence described in our protocol are not reported in this manuscript.The full follow-up questionnaire was deemed too burdensome to participants and these outcomes were subsequently eliminated.
Co-interventions
We measured co-interventions by asking participants to self-report the type of healthcare provider consulted beyond those involved in delivering trial interventions (ie, chiropractor, physiotherapist, massage therapist, medical specialist, psychologist or counsellor and other healthcare providers (acupuncturist, naturopath, homeopath, Chinese medicine practitioner)).
Adverse events
We measured adverse events at each follow-up interview, defined as an unintended sign or symptom of the intervention (eg, neck pain, radiating pain in arms, feeling tired, headache, depression or other physical discomfort).
Sample size
We aimed to detect a 20% difference in rate of self-reported global recovery at 1 year using a log rank test with 80% power and a two-tail significance level of 0.05. [62] In our trial protocol, we specified 90% power. [33] We revised the power of the trial from 90% to 80% because of the challenges associated with recruitment. Using these parameters, we needed 86 participants per group. Assuming a 30% loss to follow-up per arm, we needed 336 participants (ie, 112 per arm).
Statistical analysis
We conducted analyses according to the intention-to-treat principle. We described participant demographic and clinical characteristics at baseline (eg, mean, 95% CI, median, range) and conducted inference testing as appropriate (eg, t-test, χ2 test, Kruskal-Wallis test).
Primary outcome
We used Kaplan-Meier estimates to derive median time to self-reported global recovery and 95% CI. Using the government-regulated group as the reference intervention, we quantified the relative effectiveness of interventions by computing the hazard rate ratio (HRR) and 95% CI using Cox proportional hazards models.63–67 We computed the Wald χ2 statistic to determine whether the difference between groups was significant (p<0.05). We used two methods to test the proportionality assumption of our model. First, we tested the significance of an interaction term between the intervention groups and log of time. Second, we fitted piecewise proportional hazards models.
Baseline characteristics that differed between groups and changed either of the regression coefficients by 10% or more were controlled for in the primary analysis.68 Observations were censored at 3 weeks for participants who dropped out prior to the first follow-up interview, or on the date of their last completed follow-up interview for those who provided follow-up data.
Secondary outcomes
We computed mean differences (and 95% CI) within and between groups from baseline to each follow-up point. We used standardised cut-off values to determine if clinically important differences were reached at each time point:1) two points on the 11-point Numeric Rating Scale [37];
2) 21.4 points on the Whiplash Disability Questionnaire (ie, the minimal detectable change) [46] and
3) 7.7 points for the SF-36 Physical Component Score. [69]The minimal clinically important differences for CES-D and SF-36 Mental Component Score have not been established in this population; therefore, we considered a 10% change from baseline to be clinically important. We used Generalised Estimating Equations models to account for effects due to study arm, different follow-up times and the interaction between study arm and follow-up times. We used an exchangeable correlation structure to account for within-subject correlation over time. Finally, we used Kaplan-Meier estimates to derive median time to claim closure and Cox proportional hazards models to analyse time on insurance benefits according to the methods described above. [63–67]
Patient and public involvement
Patients were not involved in the development of the research question, study design, choice of outcome measures or recruitment for the study. Participants did not assess the burden of the interventions. We will use social media and our university website to inform the public about the results of the study.
Results
Study sample
We received 1348 referrals and 422 individuals from 336 automobile collisions were clinically assessed for inclusion in the trial. Of these, 340 participants were randomised: 113 cars (115 participants) to the government-regulated guideline, 113 cars (113 participants) to the preferred-provider group and 110 cars (112 participants) to education and activation (figures 1 and 2; supplementary appendix 4). Overall, 86.7% of participants received the allocated intervention (at least one session): 83.5% for the government-regulated guideline, 84.1% for preferred-provider rehabilitation and 92.9% for the education and activation group.
Sample characteristics
Baseline characteristics were well balanced between groups (Table 1). The mean physical component score of the SF-36 and active coping score were higher in the government-regulated guideline group, but these differences were small and therefore not clinically meaningful. The education and activation group included a smaller proportion of employed participants and a larger proportion of participants with hypertension. Finally, the preferred-provider group included a smaller proportion of participants who expected to get better soon. Among these baseline characteristics, only expectation of recovery changed the regression coefficients by at least 10% (supplementary appendix 5). Therefore, expectation of recovery was adjusted for in the primary analysis.
Healthcare services
The mean number of visits during the first 3 weeks of care was 3.8 (SD 2.3) for the government-regulated guideline group and 2.7 (SD 1.9) for the preferred-provider rehabilitation group. Similarly, it was 2.8 visits (SD 2.4) for government-regulated guideline and 2.7 (SD 2.5) for the preferred-provider rehabilitation during the subsequent 3 weeks. The education and activation group had a mean of 1.5 visits to general practitioners (SD 0.8) during the first 6 weeks of care.
A total of 48 participants from the preferred-provider and education and activations groups were referred for multidisciplinary evaluation. Twenty-two of the 28 (24.8%) referred participants from the preferred-provider group attended their multidisciplinary evaluation. In the education and activation group, 20 participants (17.9%) were referred and 19 attended.
Compared with the government-regulated guideline group, a higher proportion of participants in the other two groups received treatment outside of the protocol (supplementary appendix 6). Specifically, they used more massage therapy, physiotherapy and chiropractic. Some participants visited their own general practitioner within the first 6 weeks of care (27.5% for government-regulated guideline group, 43.8% for the preferred-provider group, 34.8% for education and activation group).
Follow-up
Follow-up rates at 12 months were 80.9% for the government-regulated guideline group; 84.1% for the preferred-provider group and 71.4% for those receiving education and activation. The follow-up rate for the primary outcome was 74.1% at 6 weeks, 65.3% at 3 months, 61.8% at 6 months, 54.4% at 9 months and 78.8% at 1 year. Following the 9 month follow-up, we adapted our follow-up strategy to minimise selection bias due to increasing attrition. Trial coordinators called participants who could not be reached by the research assistant and invited to talk to the research assistant to complete the final interview. Overall, 91.1% of participants provided follow-up data and were included in the analysis (figures 1 and 2). Not providing follow-up data was associated with consulting a lawyer, direction of impact, expectation of recovery, self-reported cardiovascular problems, self-reported gastrointestinal problems and mental and emotional problems prior to the collision (supplementary appendix 7).
Self-reported global recovery

Figure 3 The median time to recovery was 59 days (95% CI 55 to 68) for the government-regulated group, 105 days (95% CI 61 to 126) for the preferred-provider rehabilitation group and 108 days (95% CI 93 to 206) for the education and activation group (Figure 3). The time to recovery between groups was not significant (χ2 = 3.96; 2 df: p = 0.138). Compared with the government-regulated group, rate of recovery was 13% slower in the preferred-provider rehabilitation group (adjusted HRR = 0.87; 95% CI 0.64 to 1.18) and 28% slower in the education and activation group (adjusted HRR = 0.72; 95% CI 0.53 to 1.00).
Proportionality assumptions of the model
Our analysis showed that the interaction between treatment groups and the log of time was not statistically significant (time×general practitioner group, p=0.08; time×preferred-provider group, p = 0.25). However, on observing the shape of the Kaplan-Meier curves, two possible inflection times were identified: the first one at 60 days and the second one at 80 days. Therefore, we built two post hoc piecewise proportional hazards models. The first model (split at 60 days) did not yield any substantial improvement compared with the original Cox model (likelihood ratio statistic = 3.74; 2 df: p = 0.15). However, the second model (split at 80 days) showed substantial improvement compared with the original Cox model (likelihood ratio statistic = 7.76; 2 df: p = 0.02). Compared with the government-regulated guideline group, the general practitioner (delivering education and activation) and preferred-provider groups had slower rates of recovery during the first 80 days (HRR = 0.51, 95% CI 0.34 to 0.77 and HRR = 0.67, 95% CI 0.46 to 0.96, respectively), but not beyond that (HRR = 1.26, 95% CI 0.74 to 2.16 and HRR = 1.33, 95% CI 0.78 to 2.27, respectively).
Secondary outcomes
Neck pain intensity, whiplash-related disability, depressive symptomatology and health-related quality of life improved in all groups during follow-up (Table 2), but there were no significant differences between groups (p>0.05; Table 3).
The median time on insurance benefits was similar between groups: 300 days (95% CI 256 to 373) for the government-regulated guideline group; 283 days (95% CI 221 to 393) for preferred-provider rehabilitation and 321 days (95% CI 250 to 417) for the education and activation group (supplementary appendix 8). Compared with the government-regulated guideline group, there were no differences in the rate of claim closure between groups (preferred-provider rehabilitation group: HRR = 1.01, 95% CI 0.71 to 1.37; education and activation group: HRR = 0.91, 95% CI 0.65 to 1.30).
Adverse events
There were no adverse events related to the study interventions. However, nine participants reported the following conditions during the trial:1) government-regulated guideline group: suicidal ideation (n = 1), otosclerosis (n = 1), transient vertigo (n = 1), one urinary retention and foot drop (n = 1);
2) preferred-provider rehabilitation group: detached retina (n = 1), arthroscopic knee surgery (n = 1) and lump in neck (n = 1) and
3) education and activation group: hip fracture (n = 1) and ankle fracture (n = 1).
Discussion
We conducted a pragmatic randomised controlled trial of the effectiveness of a government-regulated rehabilitation guideline for the management of acute WAD. We found that the government-regulated guideline was not associated with a statistically significant improvement in recovery compared with general practitioner education and activation or preferred-provider rehabilitation in patients with acute WAD grade I–II. Similarly, we did not find differences in secondary outcomes. However, our post hoc analysis suggests that the government-regulated rehabilitation guideline may have a short-term limited effect (first 80 days) on self-reported recovery. The reasons for this temporary effect are not known, but cannot be attributed to differential follow-up times. The median follow-up times (IQR) at the 6-week and 3-month follows-up were, respectively: 43 days (IQR 42–49) and 95 days (IQR 92–104) for the education and activation group; 44 days (IQR 41–51) and 96 days (IQR 91–107) for the preferred-provider group and 45 days (IQR 42–50) and 95 days (IQR 91–105) for the government-regulated guideline. While the role of chance cannot be ruled out, it is possible that additional care received by 41 participants in the preferred-provider and activation and education groups may have impacted perceived recovery. The median time for a multidisciplinary examination to occur was 55.5 days (IQR 47–70) for the preferred-provider group (n=22) and 55 days (IQR 35–85) days for the education and activation group (n=19). The median time to begin interdisciplinary rehabilitation was 64 days (IQR 57–782) and 65 days (IQR 49–157) from recruitment for the preferred provider and education and activation groups, respectively.
Our findings are partly consistent with the results of a previous randomised trial. Jull et al reported no differences in neck pain and disability (measured on Neck Disability Index) between participants allocated to multidisciplinary individualised treatments compared with usual care. [21] Similarly, we found no differences in secondary outcomes (including neck disability) between treatment arms. However, we found that government-regulated guideline may promote time-limited short-term faster self-perceived global recovery. Although these results may appear paradoxical, they are not contradictory; recovery for musculoskeletal injuries is not necessarily synonymous with resolution of symptoms; patients report recovery when they are able to adjust to their condition, or adapt to living with their condition. [70]
Our findings are significant because they suggest that guidelines developed and regulated by governments may improve self-perceived recovery from WAD. Although guidelines are developed to reduce the gap between research and clinical care, their use and adherence by clinicians is poor. [71, 72] Our study suggests that the implementation of guidelines by government agencies could improve early recovery from traffic injuries. [73] This finding has implications beyond North America because WAD is associated with a high burden of disability throughout the world. [11, 74, 75]
Our trial provides important clinical information regarding the effective dose of care necessary to promote recovery in patients with acute WAD. Participants randomised to the government-regulated guideline received an average of 6.5 treatments during the first 6 weeks of care. This finding agrees with the results of a recent systematic review, which reported that effective multimodal interventions include an average of six visits during the first 8 weeks of care. [22] Future research examining potential dose-response relationships with treatment visits under a government-regulated guideline scheme and recovery is warranted.
We did not confirm the results from cohort studies which suggested that low-intensity general practitioner-directed care may be superior to other conservative management. [6, 7, 17, 19] Several reasons may help explain this finding. First, previous results were from Saskatchewan in the mid-1990s when management of whiplash injuries was not guided by a treatment protocol, such as the government-regulated programme. A regulated management programme (especially when applied in a standardised manner from a randomised trial) may yield benefits over unguided usual care. Second, evidence-based knowledge translation strategies (since the mid-1990s in Canada) have mainly targeted rehabilitation practitioners (physiotherapists and chiropractors) rather than general practitioners. [29, 30, 32, 76, 77] This may have led to changes in the clinical management of WAD by the former groups of clinicians. Third, automobile insurance rehabilitation practices in Ontario may have created a culture where injured persons with WAD expect rehabiltation; one or two visits to a general practitioner may not be perceived as a form of rehabilitation. Patients may expect to receive rehabilitation care and may not perceive general practitioner-based activation and rehabilitation as sufficient. This may explain why more participants allocated to this group sought co-interventions. In contrast, the government-regulated guideline group did not receive multidisciplinary rehabilitation and sought fewer co-interventions outside of the study protocol. Finally, delivery of an educational intervention alone may be ineffective. Recent studies, as identified in a previous systematic review, reported that education interventions alone provide minimal or no benefit in the management of WAD. [15]
Study strengths and limitations
Our study had several strengths. First, we recruited a consecutive sample of participants early after the injury from a single insurer (median 5–6 days). Second, variability in the delivery of multidisciplinary care was minimised because treatment was provided at the same clinics in a geographic location, but by independent clinicians. Third, our trial was informed by a pilot study. A summary of the results of the pilot study are provided in the associated protocol paper. [33] Finally, we used a valid and reliable patient-centred outcome that provides a global measure of recovery.
Our study had some limitations.
First, it was not possible to blind participants to the received intervention.
Second, a higher proportion of participants allocated to preferred-provider rehabilitation and to general practitioner education and activation care reported using healthcare services outside the study protocol. However, it is likely that a considerable proportion of these participants received government-regulated rehabilitation outside of the study because this was the standard of care at the time of the study, which would reduce the contrast between groups. Moreover, fewer co-interventions in the government-regulated guideline group adds further weight that the government-regulated rehabilitation was more effective.
Third, the follow-up rate was 65.3% at 3 months, 61.8% at 6 months and 54.4% at 9 months for the primary outcome. However, the 12-month follow-up rate for the primary outcome was 78.8%. In addition, recovery was assessed at 3, 6, 9 and 12 months to calculate time to recovery, whereas participants may have recovered earlier during the interval periods. Moreover, those who consulted a lawyer about their claim at baseline or did not expect to get better/did not know about their recovery were more likely to drop out. However, we explored the confounding effect of expectation of recovery and consulting a lawyer, and these did not bias our analysis. Reasons reported for study withdrawal were: self-perceived lack of importance, dissatisfaction with care received and advised to withdraw by their lawyer. Finally, these results may not be generalisable to settings and other jurisdictions outside of Ontario.
Conclusion
The results of our trial suggest that a government-regulated guideline is not more effective than a physician-based education and activation or preferred-provider rehabilitation intervention in promoting global recovery of patients with acute WAD. Similarly, we found no differences in neck-specific outcomes, depression or quality of life between groups. However, the government-regulated guideline may be associated with temporary faster self-rated recovery in the first 80 days postinjury, but this finding needs to be validated in future research.
Acknowledgments
The authors would like to thank participants for their contribution to the study.
Funding
The study was supported by an unrestricted grant from AVIVA Canada to the University Health Network. The funding agency was not involved in the collection of self-reported data, data analysis, interpretation of data or writing of the manuscript.
Competing interests
PC reports grants from Aviva Canada, during the conduct of the study; other from European Spine Society, personal fees from European Spine Society, grants from Ontario Ministry of Finance, grants from Canadian Institutes of Health Research—Canada Research Chair Program, other from North American Spine Society, grants from Ontario Trillium Foundation, grants from French Chiropractic Association, other from International Academy of Independent Medical Evaluators, other from Griffith University—Whiplash Symposium 2017, other from World Federation of Chiropractic, personal fees from Canadian Chiropractic Protective Association, outside the submitted work. JDC and EB report grants from Aviva Canada, during the conduct of the study
References:
Cassidy JD , Carroll LJ , Côté P , et al .
Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury.
N Engl J Med Overseas Ed 2000;342:1179–86.
doi:10.1056/NEJM200004203421606Berglund A , Alfredsson L , Cassidy JD , et al .
The association between exposure to a rear-end collision and future neck or shoulder pain:.
J Clin Epidemiol 2000;53:1089–94.
doi:10.1016/S0895-4356(00)00225-0Berglund A , Alfredsson L , Jensen I , et al .
The association between exposure to a rear-end collision and future health complaints.
J Clin Epidemiol 2001;54:851–6.
doi:10.1016/S0895-4356(00)00369-3Côté P , Cassidy JD , Carroll L .
Is a lifetime history of neck injury in a traffic collision associated with prevalent neck pain.
headache and depressive symptomatology?
Accident; analysis and prevention 2000;32:151–9Nolet PS , Côté P , Cassidy JD , et al .
The Association Between a Lifetime History of Low Back Injury in a Motor Vehicle Collision
and Future Low Back Pain: A Population-based Cohort Study
European Spine Journal 2018 (Jan); 27 (1): 136–144Côté P , Hogg-Johnson S , Cassidy JD , et al .
Initial patterns of clinical care and recovery from whiplash injuries: a population-based cohort study.
Archives of internal medicine 2005;165:2257–63Côté P , Hogg-Johnson S , Cassidy JD , et al .
Early aggressive care and delayed recovery from whiplash: isolated finding or reproducible result?
Arthritis & Rheumatism 2007;57:861–8.
doi:10.1002/art.22775Quinlan KP , Annest JL , Myers B , et al .
Neck strains and sprains among motor vehicle occupants—United States, 2000.
Accident Analysis & Prevention 2004;36:21–7.
doi:10.1016/S0001-4575(02)00110-0Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining “Whiplash” and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Holm LW , Carroll LJ , Cassidy JD , et al .
Widespread pain following whiplash-associated disorders: incidence, course, and risk factors.
The Journal of rheumatology 2007;34:193–200.Carroll, LJ, Holm, LW, Hogg-Johnson, S et al.
Course and Prognostic Factors for Neck Pain in Whiplash-associated
Disorders (WAD): Results of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S83–92Walton DM , MacDermid JC , Giorgianni AA , et al .
Risk Factors for persistent problems following acute whiplash injury: update of a systematic review and meta-analysis.
Journal of Orthopaedic & Sports Physical Therapy 2013;43:31–43.
doi:10.2519/jospt.2013.4507Wiangkham T , Duda J , Haque S , et al .
The effectiveness of conservative management for acute Whiplash Associated Disorder (WAD) II:
a systematic review and meta-analysis of randomised controlled trials.
PLoS One 2015;10:e0133415.
doi:10.1371/journal.pone.0133415Wong JJ , Shearer HM , Mior S , et al .
Are Manual Therapies, Passive Physical Modalities, or Acupuncture
Effective for the Management of Patients with Whiplash-associated
Disorders or Neck Pain and Associated Disorders? An Update
of the Bone and Joint Decade Task Force on Neck Pain and
Its Associated Disorders by the OPTIMa Collaboration
Spine J. 2016 (Dec); 16 (12): 1598-1630Yu H , Côté P , Southerst D , et al .
Does Structured Patient Education Improve the Recovery and
Clinical Outcomes of Patients with Neck Pain?
A Systematic Review from the Ontario Protocol
for Traffic Injury Management
(OPTIMa) Collaboration
Spine J. 2016 (Dec); 16 (12): 1524–1540Southerst D, Nordin M, Côté P, et al.
Is Exercise Effective for the Management of Neck Pain and
Associated Disorders or Whiplash-associated Disorders?
A Systematic Review by the Ontario Protocol for Traffic
Injury Management (OPTIMa) Collaboration
Spine J 2016 (Dec); 16 (12): 1503–1523Cassidy JD , Carroll LJ , Côté P , et al .
Does multidisciplinary rehabilitation benefit whiplash recovery?:
results of a population-based incidence cohort study.
Spine 2007;32:126–31Scholten-Peeters GGM , Neeleman-van der Steen CWM , van der Windt DAWM , et al .
Education by general practitioners or education and exercises by physiotherapists for patients with
whiplash-associated disorders? A randomized clinical trial.
Spine 2006;31:723–31.
doi:10.1097/01.brs.0000206381.15224.0fSkillgate E , Côté P , Cassidy JD , et al .
Effect of early intensive care on recovery from whiplash-associated disorders:
results of a population-based cohort study.
Arch Phys Med Rehabil 2016;97:739–46.
doi:10.1016/j.apmr.2015.12.028Lamb SE , Gates S , Williams MA , et al .
Emergency department treatments and physiotherapy for acute whiplash:
a pragmatic, two-step, randomised controlled trial.
The Lancet 2013;381:546–56.
doi:10.1016/S0140-6736(12)61304-XJull G , Kenardy J , Hendrikz J , et al .
Management of acute whiplash: a randomized controlled trial of multidisciplinary stratified treatments.
Pain 2013;154:1798–806.
doi:10.1016/j.pain.2013.05.041Sutton DA , Côté P , Wong JJ , et al .
Is multimodal care effective for the management of patients with whiplash-associated disorders or
neck pain and associated disorders? A systematic review by the
Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration.
The Spine Journal 2016;16:1541–65.
doi:10.1016/j.spinee.2014.06.019Côté P , Soklaridis S .
Does early management of whiplash-associated disorders assist or impede recovery?
Spine 2011;36(25 Suppl):S275–S279.
doi:10.1097/BRS.0b013e3182388d32Guzman J, Haldeman S, Carroll LJ, et al.
Clinical Practice Implications of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders:
From Concepts and Findings to Recommendations
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S199–S212Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions: Results of the
Bone and Joint Decade 2000–2010 Task Force on Neck Pain
and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123–152Pinfold M , Niere KR , O’Leary EF , et al .
Validity and internal consistency of a whiplash-specific disability measure.
Spine 2004;29:263–8.
doi:10.1097/01.BRS.0000107238.15526.4CMoore A , Jackson A , Jordan J , et al .
Clinical guidelines for the physiotherapy management of whiplash associated disorders:
quick reference guide.
The Chartered Society of Physiotherapy 2005Motor Accidents Authority.
Guidelines for the management of acute whiplash disorders for health professionals. 3rd edn.
New South Wales, Australia: Motor Accidents Authority, 2014Financial Services Commission of Ontario.
Pre-approved framework guideline for whiplash-associated disorders Grade I injuries with or without
complaint of back symptoms.
Ontario: Financial Services Commission of Ontario, 2003Financial Services Commission of Ontario.
Pre-approved framework guideline for whiplash-associated disorders Grade II injuries with or without
complaint of back symptoms.
Ontario: Financial Services Commission of Ontario, 2003Wong JJ , Côté P , Shearer HM , et al .
Clinical practice guidelines for the management of conditions related to traffic collisions:
a systematic review by the OPTIMa Collaboration.
Disabil Rehabil 2015;37:471–89.
doi:10.3109/09638288.2014.932448Rebbeck T , Maher CG , Refshauge KM .
Evaluating two implementation strategies for whiplash guidelines in physiotherapy:
a cluster randomised trial.
Aust J Physiother 2006;52:165–74.
doi:10.1016/S0004-9514(06)70025-3Côté P , Cassidy JD , Carette S , et al .
Protocol of a randomized controlled trial of the effectiveness of physician education and activation
versus two rehabilitation programs for the treatment of Whiplash-associated Disorders:
The University Health Network Whiplash Intervention Trial.
Trials 2008;9:75.doi:10.1186/1745-6215-9-75Independent Insurance Agents & Brokers of America, Inc.
MSA Market Share Report 2013 Property and Casualty, 2013:222–30Elashoff JD .
nQuery Advisor. Version 7.0 User’s Guide:
Los Angeles, CA, 2007Financial Services Commission of Ontario.
Pre-approved framework guideline for Grade I and II Whiplash associated disorders.
Ontario: Financial Services Commission of Ontario, 2007Carroll LJ , Jones DC , Ozegovic D , et al .
How well are you recovering? The association between a simple question about recovery and patient reports
of pain intensity and pain disability in whiplash-associated disorders.
Disabil Rehabil 2012;34:45–52.
doi:10.3109/09638288.2011.587085Fischer D , Stewart AL , Bloch DA , Lorig K , Laurent D , Holman H .
Capturing the patient’s view of change as a clinical outcome measure.
JAMA 1999;282:1157–62.
doi:10.1001/jama.282.12.1157Ngo T , Stupar M , Côté P , et al .
A study of the test–retest reliability of the self-perceived general recovery and self-perceived change
in neck pain questions in patients with recent whiplash-associated disorders.
European Spine Journal 2010;19:957–62.
doi:10.1007/s00586-010-1289-xHoving JL , de Vet HC , Koes BW , et al .
Manual therapy, physical therapy, or continued care by the general practitioner for patients with
neck pain: long-term results from a pragmatic randomized clinical trial.
The Clinical journal of pain 2006;22:370–7Hoving JL , Gross AR , Gasner D , et al .
A critical appraisal of review articles on the effectiveness of conservative treatment for neck pain.
Spine 2001;26:196–205.
doi:10.1097/00007632-200101150-00015Jensen MP , Karoly P , Braver S .
The measurement of clinical pain intensity: a comparison of six methods.
Pain 1986;27:117–26.
doi:10.1016/0304-3959(86)90228-9Wewers ME , Lowe NK .
A critical review of visual analogue scales in the measurement of clinical phenomena.
Res Nurs Health 1990;13:227–36.
doi:10.1002/nur.4770130405Ferrari R , Russell A , Kelly AJ .
Assessing whiplash recovery-the Whiplash Disability Questionnaire.
Australian family physician 2006;35:653–4.Willis C , Niere KR , Hoving JL , et al .
Reproducibility and responsiveness of the Whiplash Disability Questionnaire.
Pain 2004;110:681–8.
doi:10.1016/j.pain.2004.05.008Stupar M , Côté P , Beaton DE , et al .
A Test-retest reliability study of the whiplash disability questionnaire in patients with
acute whiplash-associated disorders.
J Manipulative Physiol Ther 2015;38:629–36.doi:10.1016/j.jmpt.2015.10.003Stupar M , Côté P , Beaton DE , et al .
Structural and construct validity of the Whiplash Disability Questionnaire in adults with
acute whiplash-associated disorders.
The Spine Journal 2015;15:2369–77.
doi:10.1016/j.spinee.2015.07.006Beaton DE , Hogg-Johnson S , Bombardier C .
Evaluating changes in health status: reliability and responsiveness of five generic health status
measures in workers with musculoskeletal disorders.
J Clin Epidemiol 1997;50:79–93.
doi:10.1016/S0895-4356(96)00296-XGarratt AM , Ruta DA , Abdalla MI , et al .
The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS?
BMJ 1993;306:1440–4.
doi:10.1136/bmj.306.6890.1440Haley SM , McHorney CA , Ware JE .
Evaluation of the mos SF-36 physical functioning scale (PF-10): I.
Unidimensionality and reproducibility of the Rasch Item scale.
J Clin Epidemiol 1994;47:671–84.
doi:10.1016/0895-4356(94)90215-1McHorney CA , Ware JE , Raczek AE .
The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests
of validity in measuring physical and mental health constructs.
Med Care 1993;31:247–63Cote P, Cassidy JD, Carroll L.
The Saskatchewan Health and Back Pain Survey.
The Prevalence of Neck Pain and Related Disability in Saskatchewan Adults
Spine (Phila Pa 1976). 1998 (Aug 1); 23 (15): 1689–1698Carroll LJ , Cassidy JD , Côté P .
Frequency, timing, and course of depressive symptomatology after whiplash.
Spine 2006;31:E551–E556.
doi:10.1097/01.brs.0000225979.26966.9eBoyd JH , Weissman MM , Thompson WD , et al .
Screening for depression in a community sample. Understanding the discrepancies between depression
symptom and diagnostic scales.
Archives of general psychiatry 1982;39:1195–200Radloff LS .
The CES-D scale: a self-report depression scale for research in the general population.
Applied Psychological Measurement 1977;1:385–401Blalock SJ , Devellis RF , Brown GK , et al .
Validity of the center for epidemiological studies depression scale in arthritis populations.
Arthritis & Rheumatism 1989;32:991–7.
doi:10.1002/anr.1780320808Orme JG , Reis J , Herz EJ .
Factorial and discriminant validity of the center for epidemiological studies depression (CES-D) scale.
J Clin Psychol 1986;42:28–33.
doi:10.1002/1097-4679(198601)42:1<28::AID-JCLP2270420104>3.0.CO;2-TZich JM , Attkisson CC , Greenfield TK .
Screening for depression in primary care clinics: the CES-D and the BDI.
The International Journal of Psychiatry in Medicine 1990;20:259–77.
doi:10.2190/LYKR-7VHP-YJEM-MKM2Devins GM , Orme CM , Costello CG , et al .
Measuring depressive symptoms in illness populations: Psychometric properties of the Center for
Epidemiologic Studies Depression (CES-D) Scale.
Psychol Health 1988;2:139–56.doi:10.1080/08870448808400349Côté P , Hogg-Johnson S , Cassidy JD , et al .
The association between neck pain intensity, physical functioning, depressive symptomatology
and time-to-claim-closure after whiplash.
J Clin Epidemiol 2001;54:275–86.
doi:10.1016/S0895-4356(00)00319-XBoyle E , Cassidy JD , Côté P , et al .
The relationship between insurance claim closure and recovery after traffic injuries for individuals
with whiplash associated disorders.
Disabil Rehabil 2017;39:889–96.
doi:10.3109/09638288.2016.1170211Lakatos E .
Sample sizes based on the log-rank statistic in complex clinical trials.
Biometrics 1988;44:229–41.
doi:10.2307/2531910Murray DM , Varnell SP , Blitstein JL .
Design and analysis of group-randomized trials: a review of recent methodological developments.
Am J Public Health 2004;94:423–32.
doi:10.2105/AJPH.94.3.423Allison PD .
Survival analysis using the SAS system: a practical guide.
Cary, N.C.: SAS Institute, 1995Cox DR .
Regression models and life-tables, 1972Hosmer DW , Lemeshow S Hosmer DW , Lemeshow S .
Assessment of model adequacy.
In: Hosmer DW , Lemeshow S , eds.
Applied survival analysis: regression modeling of time to event data.
New York: John Wiley & Sons, 1999:196–240Lee KJ , Thompson SG .
The use of random effects models to allow for clustering in individually randomized trials.
Clin Trials 2005;2:163–73.
doi:10.1191/1740774505cn082oaGreenland S , Rothman KJ Greenland S , Rothman KJ .
Introduction to stratified analysis. In: Greenland S , Rothman KJ , eds.
Modern epidemiology.
Philadelphia: Lippincott-Raven, 1998:253–79Lauche R , Langhorst J , Dobos GJ , et al .
Clinically meaningful differences in pain, disability and quality of life for chronic nonspecific
neck pain – A reanalysis of 4 randomized controlled trials of cupping therapy.
Complement Ther Med 2013;21:342–7.
doi:10.1016/j.ctim.2013.04.005Beaton DE , Tarasuk V , Katz JN , et al .
Are you better?? A qualitative study of the meaning of recovery.
Arthritis & Rheumatism 2001;45:270–9.
doi:10.1002/1529-0131(200106)45:3<270::AID-ART260>3.0.CO;2-TAlonso-Coello P , Irfan A , Sola I , et al .
The quality of clinical practice guidelines over the last two decades: a systematic review
of guideline appraisal studies.
BMJ Qual Saf 2010;19:e58.
doi:10.1136/qshc.2010.042077Whitworth JA .
Best practices in use of research evidence to inform health decisions.
Health Res Policy Syst 2006;4:11.
doi:10.1186/1478-4505-4-11Kung J , Miller RR , Mackowiak PA .
Failure of clinical practice guidelines to meet institute of medicine standards:
two more decades of little, if any, progress.
Archives of internal medicine 2012;172:1628–33Holm LW , Carroll LJ , Cassidy JD , et al .
The Burden and Determinants of Neck Pain in Whiplash-associated Disorders after Traffic Collisions:
Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S52-59Chappuis G , Soltermann B .
Number and cost of claims linked to minor cervical trauma in Europe:
results from the comparative study by CEA, AREDOC and CEREDOC.
European Spine Journal 2008;17:1350–7.
doi:10.1007/s00586-008-0732-8Bussières AE , Stewart G , Al-Zoubi F , et al .
The Treatment of Neck Pain–Associated Disorders and Whiplash-Associated Disorders:
A Clinical Practice Guideline
J Manipulative Physiol Ther 2016 (Oct); 39: 523–64Dhopte P , Ahmed S , Mayo N , et al .
Testing the feasibility of a knowledge translation intervention designed to improve chiropractic care
for adults with neck pain disorders: study protocol for a pilot cluster-randomized controlled trial.
Pilot Feasibility Stud. 2016 Jul 20;2:33. eCollection 2016.
Return to WHIPLASH
Since 2-15-2019


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |