

One- and Two-year Follow-up of a Randomized Trial of
Neck-specific Exercise with or without a Behavioural
Approach Compared with Prescription of Physical
Activity in Chronic Whiplash DisorderThis section is compiled by Frank M. Painter, D.C.
Send all comments or additions to: Frankp@chiro.org




FROM: J Rehabil Med 2016 (Jan); 48 (1): 56–64 ~ FULL TEXT
OPEN ACCESS Maria Landén Ludvigsson, MSc, Gunnel Peterson MSc, Ĺsa Dedering, PhD and Anneli Peolsson, PhD
Department of Medical and Health Sciences,
Division of Physiotherapy,
Linköping University,
SE-581 83 Linköping, Sweden.
Objective: To explore whether neck-specific exercise, with or without a behavioural approach, has benefits after 1 and 2 years compared with prescribed physical activity regarding pain, self-rated functioning/disability, and self-efficacy in management of chronic whiplash.
Patients A total of 216 volunteers with chronic whiplash-associated disorders, grades 2 or 3.
Methods: Participants were randomized to 1 of 3 exercise interventions: neck-specific exercise with or without a behavioural approach, or physical activity prescription. Self-rated pain (visual analogue scale), disability/functioning (Neck Disability Index/Patient Specific Functional Scale) and self-efficacy (Self-Efficacy Scale) were evaluated after 1 and 2 years.
Results: Both neck-specific exercise groups maintained more improvement regarding disability/functioning than the prescribed physical activity group at both time-points (p ≤ 0.02). At 1 year, 61% of subjects in the neck-specific group reported at least 50% pain reduction, compared with 26% of those in the physical activity prescription group (p < 0.001), but at 2 years the difference was not significant.
Conclusion: After 1-2 years, participants with chronic whiplash who were randomized to neck-specific exercise, with or without a behavioural approach, remained more improved than participants who were prescribed general physical activity.
Keywords: whiplash; chronic; exercise; randomized; follow-up study; spine; behaviour therapy.
Clinical Trial Registration: Clinical Trials.gov, NCT01528579
The FULL TEXT Article:
INTRODUCTION
At 1 year post-injury, 50% of people with whiplash-associated disorders (WAD) still report neck pain. [1] Despite the significant impact of WAD, there is still no clear evidence regarding which treatment is most effective. [2–4] Persistence of symptoms in individuals with WAD has been attributed to both physical and psychosocial factors. [5] It is therefore reasonable to assume that a behavioural approach may be of benefit in the management of chronic WAD, as in chronic back pain. [6] However, impairments and altered patterns of muscle activation [7–11] and muscle deformation [12, 13] in the cervical spine are also features of chronic WAD, suggesting that treatments aimed at improving muscle function might also be of importance. Although exercise is considered a safe treatment for neck pain, with temporary and benign side-effects, its efficacy in the context of chronic WAD remains unclear. [2, 3]
Short-term pain reduction may be achieved [14], but there is no evidence regarding the optimal exercise approach for WAD. [14] Although prescription of physical activity (PPA) (i.e. self-directed general physical activity outside the healthcare system) is often recommended for patients with chronic pain [15], the relative effectiveness of different exercise regimens in relieving chronic WAD remains unknown. [14] Regarding chronic WAD grades 1–2, Michaleff et al. found that a comprehensive exercise programme including neck-specific exercise was not more effective for pain reduction than advice alone. [16] Another randomized controlled trial previously reported by our group found that patients with chronic WAD grades 2–3 experienced greater reductions in neck pain and neck-related disability after neck-specific exercise, with or without the addition of a behavioural approach, compared with PPA. [17] However, those results were only analysed up to 6 months post-inclusion.
The aim of this study was to explore whether, after 1 and 2 years, neck-specific exercise with or without a behavioural approach has long-term benefits over PPA regarding pain, self-rated functioning/disability, and self-efficacy in the management of grade 2 or grade 3 chronic WAD.
METHODS
Design
This is a 1– and 2–year follow-up of a multi-centre, prospective, randomized clinical trial with assessor and group allocation blinding (Clinical Trials.gov, NCT01528579 [18]). Short-term results have been presented previously. [16] The study, conducted in accordance with the Declaration of Helsinki, was approved by the Regional Ethics Committee of Linköping University, Sweden.
Participants and settings

Table 1 A total of 216 individuals with chronic WAD were recruited between February 2011 and May 2012, including 142 (65%) women and 74 (35%) men with a mean age of 40 (range 18–63, SD 11.4) years (Table I). Inclusion criteria were age 18–63 years, and a grade 2 or 3 whiplash injury according to the Quebec Task Force [19] in the preceding 6–36 months that was nominated as the cause of current symptoms. Additional inclusion criteria were a Neck Disability Index score (NDI) [20] of at least 10/50 points, and/or an average pain rating on the visual analogue scale (VAS) of > 20/100 mm (where 0 = no pain and 100 = worst imaginable pain) [21] for the preceding week. Exclusion criteria were: signs of traumatic brain injury, previous neck trauma with unresolved symptoms, more dominant pain elsewhere, neck pain causing more than 1 month of absence from work in the year preceding the whiplash injury, myelopathy, spinal infection or tumour, previous neck surgery, conditions that were potentially detrimental to completing the study interventions (e.g. severe psychiatric disorders or known drug abuse) or insufficient knowledge of the Swedish language. Experienced physiotherapists conducted the interventions in a primary care setting. The physiotherapists were provided with standardized oral information about their interventions. Those in charge of physiotherapist-led interventions participated in a 1–day workshop of standardized practical and theoretical training held by the project leaders.

Figure 1 A total of 170 patients (79%) completed the 1–year follow-up, and 123 patients (57%) completed the 2–year follow-up (Figure 1). With imputed values (see statistics), data were available from 193 participants (89%) at 1 year and from 184 (85%) participants at 2 years. There was no baseline difference (p > 0.27 for all) between those who completed the questionnaires and drop-outs at either time-point regarding allocation, gender, WAD grade, pain or pain bothersomeness, NDI (1 year only), or age (2 years only). Drop-outs at 1 year were somewhat younger (age 37 (SD 11) years) than those who completed the study (age 41 (SD 11) years, p = 0.04). Drop-outs at 2 years reported more baseline disability than those who completed the study (NDI 17.9 (SD 6.9) vs NDI 15.7 (SD 6.5), p < 0.04). At 2 years, drop-outs and completers did not differ regarding preceding improvement from baseline to 1 year (NDI and neck pain VAS, p > 0.94).
Procedure
Potential participants were identified from the healthcare registries of 6 Swedish counties, including primary healthcare centres and hospital outpatient services. Participants were screened for eligibility through the following 4–step process (Fig. 1): (i) an initial screening letter that contained study information, basic inclusion/exclusion criteria (Fig.1), NDI [19] and Pain VAS (P-VAS) measures; (ii) a telephone interview with 1 of the project leaders; (iii) a review of medical records, if needed due to any uncertainties; and (iv) a physical examination by an experienced physiotherapist (mean 18 years’ experience) to confirm findings consistent with either WAD grade 2 (neck pain and clinical findings) or WAD grade 3 (addition of neurological signs). [19]
All participants received verbal and written information about the study. Informed consent and baseline measurements were collected before allocation. Allocation from a computer-generated randomization list was made by an independent researcher, who also put the individual results in sealed opaque envelopes for further distribution to the treating physiotherapists. Collection and entering of data were made by staff blinded to allocation.
Interventions
First, all patients were examined by their treating physiotherapist. All 3 interventions were undertaken during a 12–week period, and participants were encouraged to continue exercising on their own after the interventions. The interventions, as previously described in more detail [17], were: physiotherapist-led
- neck-specific exercise (NSE),
- NSE with the addition of a behavioural approach (NSEB), or
- prescribed physical activity (PPA).
No serious adverse events were reported.
Neck-specific exercise (NSE). Participants in the NSE group undertook supervised, neck-specific exercise twice weekly. They initially also practiced daily at home, focusing on activity of the deep cervical muscles. Next, gym exercise within participants’ symptom tolerance was gradually introduced, with progressive head resistance training that focused on low load endurance in flexion, extension, rotation, and lateral flexion. Exercise-related pain provocation was not accepted in this group. A detailed description of the exercises can be found at the Academic Archive On-line. [22] Participants also received a written individualized exercise programme that contained exercises from the interventions and general physical activity towards the end of the 12–week intervention.
Neck-specific exercise with a behavioural approach (NSEB). The protocol of exercises in the NSEB group was the same as that undertaken by the NSE group, with the addition of a behavioural approach. The behavioural approach aimed to be basic and manageable by experienced physiotherapists in primary care with some previous knowledge of behavioural approaches. In accordance with the concept of graded exercise, patients were encouraged not to focus on temporary increases in neck pain. They also received physiotherapist-guided behavioural interventions, including education and introduction to activities aimed at pain management and problem-solving. Time-frames and specific components of the interventions have been described previously. [17]
Prescribed physical activity (PPA). Participants in the PPA group initially underwent a short motivational interview with a physiotherapist. Based on this interview and a physical examination they were prescribed individualized general physical activity to be performed independently. The purpose of this prescription was to increase overall physical activity, either with individualized home exercise or activities performed in public gyms or elsewhere, outside the healthcare system. Neck-specific exercises that included any form of head resistance were not prescribed in this group. A single follow-up visit or phone call was encouraged. Participants in this group were also encouraged to continue exercise post-interventions.
Outcomes
All measurements were recorded at baseline and after 1 and 2 years.
The individually chosen activities were recorded verbally in the Patient-Specific Functional Scale (PSFS) by a blinded investigator in connection with other clinical tests, to ensure that they were individually standardized with regard to time and/or repetitions.
Disability and functioning. The primary outcome measurement was the Neck Disability Index (NDI) [20], which consists of 10 items that grade neck disability from 0 (no activity limitations) to 5 (major activity limitations), with a total maximum score of 50 points. [20] A higher score represents a greater level of disability. The NDI is considered a reliable and valid measurement of disability in patients with neck pain disorders. [23]
The PSFS was used to measure functioning. For the PSFS, each patient nominated 3 individual activities related to work, leisure, and physical activity/exercise that they were unable to do or experienced difficulty performing because of their neck condition. These activities were ranked according to functional level on a scale from 0 (unable to do) to 10 (functional level equal to pre-injury status), and the mean of the scores was calculated. The PSFS has been shown to have excellent reliability [24] and responsiveness in the chronic WAD population. [25]
Pain. Current neck pain intensity was measured using a Pain VAS (PVAS) anchored by 0 = no pain, and 100 = worst imaginable pain. [21] Bothersomeness of neck pain (B-VAS) was recorded for the preceding 24 h (anchored by 0 = not bothersome at all, 100 = extremely bothersome). Pain bothersomeness is reportedly more responsive than pain intensity in individuals with WAD. [25] Patients also recorded whether they used analgesics to manage their neck pain (yes/no).
Self-efficacy. The participants’ confidence in their ability to perform activities despite pain was evaluated using the Self-Efficacy Scale (SES). [26, 27] The SES is a reliable instrument in WAD populations [5, 28]; it consists of 20 different physical and psychosocial activity items that are scored from 0 = not confident at all, to 10 = very confident, thus generating a total score from 0–200.
Adherence. Participants were asked to estimate their adherence to their post-intervention prescribed exercise on a 4–point scale: full, fair, some, or no adherence. Participants who reported some to full adherence were classified as adherent in the analysis.
Clinical relevance. The Initiative on Methods, Measurement and Pain Assessment in Clinical Trials (IMMPACT) concluded that it is impossible to provide specific guidelines for determining whether a group difference is clinically meaningful. [29] Therefore, we also calculated the proportion of patients that achieved clinically important improvement where such cut-offs have been established. The minimal clinically important difference (MCID) of the NDI score is suggested to be 3.5–5/50 points [20], with a reduction of 5 set as the cut-off score in this study. This exceeds the measurement error in this study sample, as previously reported (minimum detectable change (MDC) of 3.3/50 points. [17] In the PSFS, the MCID is reported as 2.3 and the MDC is reported as 2.1. [30] An increase of 2.3 was set as the cut-off score in this study. A reduction in pain intensity of ≥ 50% is suggested to indicate substantial improvement or treatment success according to IMMPACT recommendations. [31] This level is also used in this study to define clinically important improvement. To our knowledge, the MCID has not been established in the SES.
Statistical analysis
The required sample size for the original randomized controlled trial was determined on the basis of the expected difference between the 3 groups (alpha 5%, power 80%) for main outcome, NDI (3.5/50, SD 7), and allowing for a 10% drop-out rate, rendering a sample size of 216. If only 1 item of data was missing from the NDI scores or 2 items were missing from the SES, the missing data were substituted by the mean item score of the questionnaire for that participant. If more data items were missing, that particular score was omitted from the analysis. Missing scores were considered missing at random (MAR), such that the closest match is considered a reliable and efficacious imputation method in repeated measures data. Closest match replaces a participant’s missing time-point with a value obtained from another participant who has similar scores on the same measure assessed at other time-points. [32]
Only participants with complete measurements from 3 time-points served as possible donors, and participants with missing data served as recipients. The score obtained by the donor at that time-point was imputed to the missing time-point for the recipient. Closest match was defined as all donors with less than 15% absolute differences between the recipient’s scores and donor’s scores at all other time-points for which data were present, and with the same trend over time (better, worse, or unchanged). Priority was given to absolute matches, and each outcome was analysed and imputed separately. When more than one possible donor was identified, the computer (SPSS version 22) selected the closest match donor at random from the possible donors. Because baseline adherence data cannot be measured, these values were not imputed. The presented results are from the imputed data set. Use of imputed vs non-imputed values in the analysis did not cause a significant difference in the results.
The primary analysis was conducted using SPSS version 22 on an intent-to-treat basis, including all patients completing each measurement and imputed data. Descriptive statistics were calculated, and between-group comparisons were evaluated with the Kruskal– Wallis test for non-parametric data, with the Mann-Whitney U test for post-hoc, or with 1–way analysis of variance (ANOVA) for normally distributed parametric data. In binary outcomes, χ2 tests were used. Within-group differences at baseline, 6, 12 and 24 months were calculated using a Friedman’s ANOVA with post-hoc Wilcoxon’s signed rank test. Correlations were calculated using Spearman’s rho. To determine the proportion of responders in each group, sub-analyses of participants who had reached the predefined cut-off values were performed, as described previously. Statistical significance was set at p < 0.05 (with Bonferroni post-hoc correction at 0.017). To aid comparability to previous and other publications in this field, all outcomes are presented with both mean and median values, and data are also presented for separate WAD grades.
RESULTS
Disability and functioning

Table 2
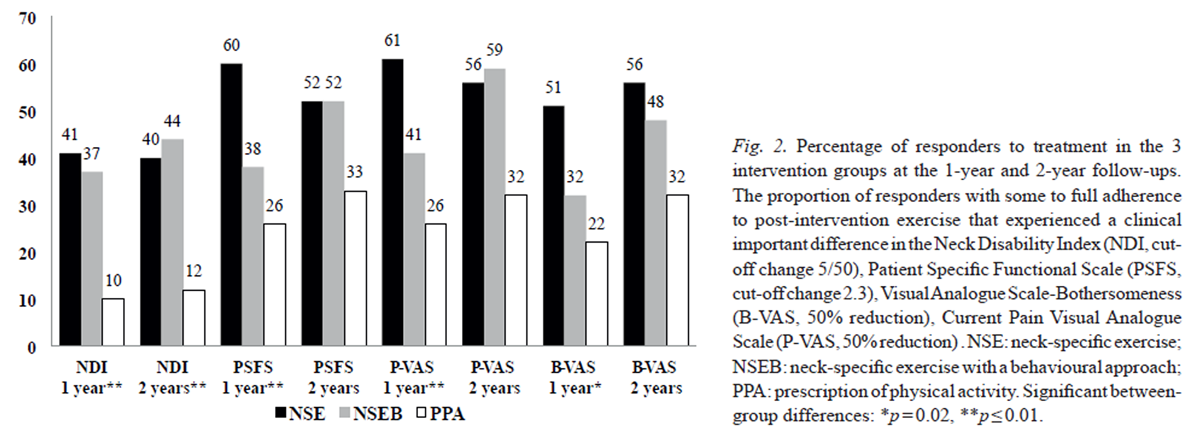
Figure 2

Table 3 Between-group analysis indicated that both physiotherapist-led neck-specific exercise groups reported greater reductions in neck disability and improved functioning (p < 0.01) than the PPA group at the 1–year follow-up. At 2 years, the NSEB group reported significant reduction in neck disability compared with the prescribed physical activity (PPA) group (p ≤ 0.02); however, the NSE group reported significant improvement in functioning compared with the PPA group (p = 0.02) (Table II). There was, however, no difference between the 2 physiotherapist-led groups. A greater proportion of individuals in the 2 physiotherapist-led neck-specific groups than in the PPA group experienced clinically relevant improvement in disability/functioning at 1 year (p < 0.01) and 2 years (disability p = 0.01); however, the difference regarding functioning was not statistically significant at 2 years (p = 0.32) (Figure 2).
Within-group results indicated that both neck-specific exercise groups (but not the PPA group) improved over time (disability p = NSE 0.01, NSEB < 0.001, PPA 0.13, functioning p = NSE/NSEB < 0.001, PPA 0.22). The improvements were gained in the first 6 months [17] and were maintained over time (Table III).
Pain
There were no significant between-group differences (p ≥ 0.15) regarding reduction in neck pain or pain bothersomeness at the 1–year or 2–year follow-up (Table II). Although significantly fewer participants in the 2 neck-specific groups reported taking analgesics for neck pain (NSE 47%, NSEB 50%, PPA 69%, p = 0.04) at 1 year, the difference was non-significant at 2 years (NSE 44%, NSEB 53%, PPA 61%, p = 0.31). However greater proportions of individuals in the 2 physiotherapist-led neck-specific groups reported clinically relevant improvements in pain/pain bothersomeness after 1 year, as indicated by 50% pain reduction (p ≤ 0.02); but the difference was non-significant at 2 years (p ≥ 0.11; Fig. 2).
The within-group results showed that current pain and pain bothersomeness improved significantly over time in both neckspecific groups (p = NSE, NSEB ≤ 0.001). Pain bothersomeness improved in the PPA group (p = 0.02), although current pain did not (p = 0.07). The improvements were gained in the first 6 months (17) and maintained over time without significant changes thereafter for either outcome (Table III).
Self-efficacy
There were no significant between-group differences regarding self-efficacy (p < 0.17) at the 1–year or 2–year follow-up. The within-group results demonstrated improvement for the NSE group only over time (p = NSE 0.02, NSEB 0.07, PPA 0.86), and there were no changes in any of the groups after 6 months (p > 0.12) (Table III).
Adherence
At the 1–year follow-up, there was no between-group difference regarding self-reported adherence to post-intervention prescribed exercise (p = 0.23). Seventy-nine percent of the patients in the NSE and PPA group and 69% of patients in the NSEB group reported some to full adherence. At 2 years there was a significant difference (p = 0.02): the PPA group reported the highest percentage of some to full adherence to post-intervention exercise (NSE 69%, NSEB 60%, PPA 74%).
DISCUSSION
The results of this study indicate that a substantial number of individuals with chronic WAD (mean duration 20 months) can obtain long-lasting symptom reduction, particularly following neck-specific exercise. The 2 neck-specific exercise groups reported greater improvements regarding disability/functioning than the PPA group, which reported no improvement over time. Pain bothersomeness was reduced in all 3 groups over time, but current pain was reduced only in the NSE/NSEB groups; however, there was no difference among mean group results. However, regarding clinically important improvement, defined as the proportion of participants reaching the MCID of the NDI, PSFS, or VAS, greater proportions of participants in the 2 neck-specific groups displayed clinically important improvements regarding pain, disability, and functioning at 1 year; the NSE group reported the greatest proportion (up to 61%). At 2 years, the between-group difference was only significant regarding disability, although the 2 neck-specific groups exhibited clear trends toward greater proportions of participants with clinically important improvement in all outcomes (40–59%), compared with the PPA group (12–33%). The lack of significance may be because of the lower number of participants in this subanalysis after excluding non-adherent patients. Neck-specific exercise did not produce any significant differences regarding any outcomes when applied alone vs in combination with a behavioural approach.
Our findings are in contrast with those of Michaleff et al. [16], who observed similar improvements for both treatment arms, whereas in our study the improvements seen in the PPA group were generally smaller or non-existing. Stewart et al. observed only short-term differences between groups. [33] Possible reasons may be that Michaleff et al. included lower WAD grades (1–2) and did not include patients with WAD grade 3. WAD grade 3 has been associated with treatment success in neck-specific exercise. [34] Disability improvements also tended to be greater among patients with WAD grade 3 in the neck-specific groups, while there was a trend toward deterioration in the PPA group. The neck-specific exercise regimes may also have differed somewhat, as Stewart et al. [33] did not specify whether the endurance training was neck-specific. Although Michaleff et al. [46] reported progressive training in neck flexion/extension, it is unclear whether this included resistance. In our study, endurance training included headresisted neck exercise, and apart from flexion and extension, rotation and lateral flexion were also part of the programme. Consistent with our findings, the PSFS is reportedly more sensitive to change than the NDI. [25] This difference in sensitivity might be because the chosen activities are based on what is most important to each individual. Therefore, the results must be interpreted as changes of functioning regarding meaningful individual activities for each participant. Even so, the PSFS is suggested to be an appropriate measure for statistical comparisons between groups in clinical research [35], and can also complement the NDI.
The proportion of participants that reported clinical improvement even after 2 years was high among those who continued exercising to some degree, especially in the 2 neck-specific groups. Whether this was because improvement led to greater motivation to continue exercising, or continuous exercise postulated improvement is uncertain. However, whether all participants were included in the analysis (regardless of adherence), the results were the same, except for a tendency toward lower improvements and a significant between-group difference favouring the 2 neck-specific groups regarding PVAS in the complete set analysis.
Even though the PPA group reported better adherence to their prescribed exercise activity than the NSEB group at 2 years, the NSEB group still reported less disability. One reason might be that the behavioural approach included the discussion of strategies to handle relapse/periods of worsening. This may also be a reason why the proportion of responders tended to increase over time. It may also indicate that choice of exercise intervention is important even after 2 years, even when continuous adherence is not optimal. This is in accordance with findings by Ylinen et al., who reported that improvements achieved through long-term training in chronic neck pain were maintained at a 3–year follow-up despite faltering adherence. [36]
There were no improvements or between-group differences in self-efficacy at the 1– or 2–year follow-ups. There was a large variance that could not be explained by level of adherence. Selfefficacy has previously been reported to increase with the completion of an exercise programme [37]; however, there was no correlation between either baseline SES score or change in SES score and adherence (Spearman’s rho –0.10,–0.11, p > 0.23). One reason might be the relatively high baseline level of self-efficacy in this study, indicating that self-efficacy was not a major issue. This might be because participants were recruited mainly from primary care, not pain clinics. Patients in pain clinics reportedly have higher levels of functional impairment and psychosocial difficulties, but may thus not be as representative of individuals in general who suffer from chronic pain. [38]
Opinions differ regarding whether rating scales and larger scores from questionnaires should be analysed with nonparametric or parametric statistics. We also checked our results using parametric statistics, and observed no significant differences from the non-parametric results presented, in accordance with the policy of this journal.
Study limitations
Forty-three percent of the participants were lost to follow-up at 2 years, possibly because the clinical tests, in which they also participated for up to 1 year, ended, which may have reduced their motivation to continue answering questionnaires. This scenario introduces possible bias into the results. However, analysis indicated that the only difference between drop-outs and completers was that drop-outs at 1 year were somewhat younger than completers, and drop-outs at 2 years reported more baseline disability than completers. As reported previously, age was not associated with outcome; however, in this study sample a higher NDI score at baseline was associated with greater improvement regarding disability, but not pain. [34] Furthermore, the use of imputed vs non-imputed data in the analyses did not significantly affect the results.
The closest match imputation method used in this study did not substitute values in cases in which only baseline data were available. This approach resulted in some missing values, even after imputation. However, closest match is reported to perform well even when missing data are substantial, and is recommended over common methods such as last value carried forward, which are reported to perform poorly. [32] There was a small, but significant, baseline difference between randomization groups regarding gender and age; however, neither factor was associated with outcomes in this study sample. [34]
Although these results are promising, and the study sample was representative regarding age, gender, and level of pain compared with those who declined to participate in the study [17], the study should be repeated in another population. It is also important for future studies to identify predictors of which patients will benefit from which specific treatments. As seen in this study, there were participants who exhibited clinically important improvement in all groups (including the PPA group, in which the mean disability rather tended to worsen slightly). In conclusion, after 1–2 years, participants with chronic WAD grade 2 or 3 who were randomized to neck-specific exercise (with or without a behavioural approach) remained more improved than participants who were prescribed general physical activity. However, due to the loss to follow-up, the results must be interpreted with some caution.
ACKNOWLEDGEMENTS
The authors would like to thank all participants in this study, including WAD participants, physiotherapists, and staff involved at any stage of the study. Financial disclosure and conflicts of interest. This study was supported by funding from the Swedish government through the REHSAM Foundation, the Swedish Research Council, the regional Center for Clinical Research and the County Council of Östergötland, Centre for Clinical Research Sörmland at Uppsala University, the Medical Research Council of Southeast Sweden, and the Uppsala-Örebro Regional Research Council, Sweden. The authors declare no conflicts of interest.
REFERENCES
Carroll, LJ, Holm, LW, Hogg-Johnson, S et al.
Course and Prognostic Factors for Neck Pain in Whiplash-associated
Disorders (WAD): Results of the Bone and Joint Decade 2000-2010
Task Force on Neck Pain and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S83–92Hurwitz, EL, Carragee, EJ, van der Velde, G et al.
Treatment of Neck Pain: Noninvasive Interventions: Results of the
Bone and Joint Decade 2000–2010 Task Force on Neck Pain
and Its Associated Disorders
Spine (Phila Pa 1976). 2008 (Feb 15); 33 (4 Suppl): S123–152Southerst D, Nordin M, Côté P, et al.
Is Exercise Effective for the Management of Neck Pain and
Associated Disorders or Whiplash-associated Disorders?
A Systematic Review by the Ontario Protocol for Traffic
Injury Management (OPTIMa) Collaboration
Spine J 2016 (Dec); 16 (12): 1503–1523Soderlund A, Denison E.
Classification of patients with whiplash associated disorders (WAD):
reliable and valid subgroups based on the Multidimensional Pain Inventory (MPI-S).
Eur J Pain 2006; 10: 113–119.Chou R, Huffman LH; American Pain Society.
Nonpharmacologic Therapies for Acute and Chronic Low Back Pain:
A Review of the Evidence for an American Pain Society/
American College of Physicians Clinical Practice Guideline
Annals of Internal Medicine 2007 (Oct 2); 147 (7): 492–504Nederhand MJ, Hermens HJ, IJzerman MJ, Turk DC, Zilvold G.
Cervical muscle dysfunction in chronic whiplash-associated disorder
grade 2: the relevance of the trauma.
Spine (Phila Pa 1976) 2002; 27: 1056–1061.Sterling M, Jull G, Vicenzino B, Kenardy J, Darnell R.
Development of motor system dysfunction following whiplash injury.
Pain 2003; 103: 65–73.Jull G, Kristjansson E, Dall’Alba P.
Impairment in the cervical flexors:
a comparison of whiplash and insidious onset neck pain patients.
Man Ther 2004; 9: 89–94.Woodhouse A, Vasseljen O.
Altered motor control patterns in whiplash and chronic neck pain.
BMC Musculoskelet Disord 2008; 9: 90.Juul-Kristensen B, Clausen B, Ris I, Jensen RV, Steffensen RF, et al.
Increased neck muscle activity and impaired balance among females
with whiplash-related chronic neck pain: a cross-sectional study.
J Rehabil Med 2013; 45: 376–384.Landén Ludvigsson M, Peterson G, Jull G, Trygg J, Peolsson A.
Mechanical properties of the trapezius during scapular elevation in
people with chronic whiplash associated disorders -
A casecontrol ultrasound speckle tracking analysis.
Man Ther 2015 [Epub ahead of print].Peterson G, Dedering A, Andersson E, Nilsson D, Trygg J, Peolsson M, et al.
Altered ventral neck muscle deformation for individuals with whiplash
associated disorder compared to healthy controls – a case-control ultrasound study.
Man Ther 2015; 20: 319–327.Teasell RW, McClure JA, Walton D, Pretty J, Salter K, Meyer M, et al.
A research synthesis of therapeutic interventions for whiplashassociated
disorder (WAD): part 4 – noninvasive interventions for chronic WAD.
Pain Res Manag 2010; 15: 313–322.Professional Associations for Physical Activity, Swedish National Institute
of Public Health Physical activity in the prevention and treatment of disease.
Stockholm: Swedish National Institute of Public Health; 2010 [cited 2015 Feb 10]. Available from:
http://www.fyss.se/fyss-in-english/Michaleff ZA, Maher CG, Lin CW, Rebbeck T, Jull G, Latimer J, et al.
Comprehensive physiotherapy exercise programme or advice for chronic
whiplash (PROMISE): a pragmatic randomised controlled trial.
Lancet 2014: 12; 384: 133–141.Ludvigsson ML, Peterson G, O’Leary S, Dedering A, Peolsson A.
The effect of neck-specific exercise with, or without a behavioral
approach, on pain, disability, and self-efficacy in chronic
whiplash-associated disorders: a randomized clinical trial.
Clin J Pain 2015; 31: 294–303.Peolsson A, Ludvigsson ML, Overmeer T, Dedering A, Bernfort L, Johansson G, et al.
Effects of neck-specific exercise with or without a behavioural approach
in addition to prescribed physical activity for individuals with chronic
whiplash-associated disorders: a prospective randomised study.
BMC Musculoskel Dis 2013; 14: 311.Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, Zeiss E.
Scientific Monograph of the Quebec Task Force on Whiplash-Associated Disorders
Redefining Whiplash and its Management
Spine (Phila Pa 1976). 1995 (Apr 15); 20 (8 Suppl): S1-S73Vernon H.
The Neck Disability Index: State-of-the-Art, 1991-2008
J Manipulative Physiol Ther 2008 (Sep); 31 (7): 491–502Carlsson AM.
Assessment of chronic pain. I.
Aspects of the reliability and validity of the visual analogue scale.
Pain 1983; 16: 87–101.Landén Ludvigsson M, Peolsson A, Peterson G.
Neck-specific exercise program. [Cited 2015 Feb 9]. Available from:
http://liu.divaportal.org/smash/record.jsf?pid=diva2%3A785214&dswid=-3895MacDermid JC, Walton DM, Avery S, Blanchard A, Etruw E, McAlpine C, et al.
Measurement properties of the neck disability index: a systematic review.
J Orthop Sports Phys Ther 2009; 39: 400–417.Westaway MD, Stratford PW, Binkley JM.
The patient-specific functional scale:
validation of its use in persons with neck dysfunction.
J Orthop Sports Phys Ther 1998; 27: 331–338.Stewart M, Maher CG, Refshauge KM, Bogduk N, Nicholas M.
Responsiveness of pain and disability measures for chronic whiplash.
Spine (Phila Pa 1976) 2007; 32: 580–585.Altmaier EM, Russell DW, Kao CF, Lehmann TR, Weinstein JN.
Role of self-efficacy in rehabilitation outcome among chronic low back pain patients.
J Counsel Psychol 1993; 40: 335–339.Denison E, Ĺsenlöf P, Lindberg P.
Self-efficacy, fear avoidance, and pain intensity as predictors of disability
in subacute and chronic musculoskeletal pain patients in primary health care.
Pain 2004; 111: 245–252.Bunketorp L, Carlsson J, Kowalski J, Stener-Victorin E.
Evaluating the reliability of multi-item scales: a non-parametric approach
to the ordered categorical structure of data collected with the Swedish version
of the Tampa Scale for Kinesiophobia and the Self-Efficacy Scale.
J Rehabil Med 2005; 37: 330–334.Dworkin RH, Turk DC, McDermott MP, Peirce-Sandner S, Burke LB, et al.
Interpreting the clinical importance of group differences
in chronic pain clinical trials: IMMPACT recommendations.
Pain 2009; 146: 238–244.Cleland JA, Fritz JM, Whitman JM, Palmer JA.
The reliability and construct validity of the Neck Disability Index
and patient specific functional scale in patients with cervical radiculopathy.
Spine (Phila Pa 1976) 2006; 31: 598–602.Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, et al.
Interpreting the clinical importance of treatment outcomes
in chronic pain clinical trials: IMMPACT recommendations.
J Pain 2008; 9: 105–121.Elliott P, Hawthorne G.
Imputing missing repeated measures data:
how should we proceed?
Aust N Z J Psychiatry 2005; 39: 575–582.Stewart MJ, Maher CG, Refshauge KM, Herbert RD, Bogduk N, Nicholas M.
Randomized controlled trial of exercise for
chronic whiplash-associated disorders.
Pain 2007; 128: 59–68.Landén Ludvigsson M, Peterson G, Dedering Ĺ, Falla D, Peolsson A.
Factors associated with pain and disability reduction
following exercise interventions in chronic whiplash.
Eur J Pain 2015 May 29 [Epub ahead of print].Abbott JH, Schmitt JS.
The Patient-Specific Functional Scale was valid for
group-level change comparisons and between-group discrimination.
J Clin Epidemiol 2014; 67: 681–688.Ylinen J, Hakkinen A, Nykanen M, Kautiainen H, Takala EP.
Neck muscle training in the treatment of chronic neck pain:
a three-year follow-up study.
Eura Medicophys 2007; 43: 161–169.Jones F, Harris P, Waller H, Coggins A.
Adherence to an exercise prescription scheme: the role of expectations,
self-efficacy, stage of change and psychological well-being.
Br J Health Psychol 2005; 10: 359–378.Mailis-Gagnon A, Yegneswaran B, Lakha SF, Nicholson K, Steiman AJ, Ng D, et al.
Pain characteristics and demographics of patients attending
a university-affiliated pain clinic in Toronto, Ontario.
Pain Res Manag 2007; 12: 93–99.
Return to WHIPLASH
Return to EXERCISE AND CHIROPRACTIC
Since 10-05-2022


| Home Page | Visit Our Sponsors | Become a Sponsor |
Please read our DISCLAIMER |
